The observed COVID-19 case-fatality rate varies widely across countries. This study determined how much of the variation in case-fatality rate was the result of country-specific age-related factors (that is, age distribution of the cases and population age distribution). The information is critical for making meaningful comparisons of COVID-19 case-fatality rates across countries.
Visual Abstract. Age Distributions of Cases and COVID-19 Case Fatality Across Countries.
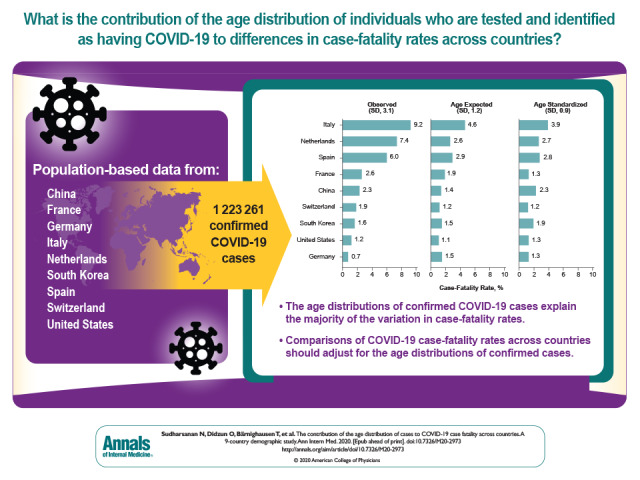
The observed COVID-19 case-fatality rate varies widely across countries. This study determined how much of the variation in case-fatality rate was the result of country-specific age-related factors (that is, age distribution of the cases and population age distribution). The information is critical for making meaningful comparisons of COVID-19 case-fatality rates across countries.
Abstract
Background:
There is wide variation in coronavirus disease 2019 (COVID-19) case-fatality rates (CFRs) across countries, leading to uncertainty about the true lethality of the disease. A large part of this variation may be due to the ages of individuals who are tested and identified.
Objective:
To measure the contribution of distortions from the age distributions of confirmed cases to CFRs within and across populations.
Design:
Cross-sectional demographic study using aggregate data on COVID-19 cases and deaths by age.
Setting:
Population-based data from China, France, Germany, Italy, the Netherlands, South Korea, Spain, Switzerland, and the United States.
Participants:
All individuals with confirmed COVID-19, as reported by each country as of 19 April 2020 (N = 1 223 261).
Measurements:
Age-specific COVID-19 CFRs and age-specific population shares by country.
Results:
The overall observed CFR varies widely, with the highest rates in Italy (9.3%) and the Netherlands (7.4%) and the lowest rates in South Korea (1.6%) and Germany (0.7%). Adjustment for the age distribution of cases explains 66% of the variation of across countries, with a resulting age-standardized median CFR of 1.9%. Among a larger sample of 95 countries, the observed variation in COVID-19 CFRs is 13 times larger than what would be expected on the basis of just differences in the age-composition of countries.
Limitation:
The age-adjusted rates assume that, conditional on age, COVID-19 mortality among diagnosed cases is the same as that among undiagnosed cases and that individuals of all ages are equally susceptible to severe acute respiratory syndrome coronavirus 2 infection.
Conclusion:
Selective testing and identifying of older cases considerably warps estimates of the lethality of COVID-19 within populations and comparisons across countries. Removing age distortions and focusing on differences in age-adjusted case fatality will be essential for accurately comparing countries' performance in caring for patients with COVID-19 and for monitoring the epidemic over time.
Primary Funding Source:
Alexander von Humboldt Foundation.
Coronavirus disease 2019 (COVID-19) has led to unprecedented disruptions to health systems and individuals' social, psychological, and economic lives (1–6). As the number of COVID-19 cases continues to increase worldwide (7), individuals are being exposed to a continuous flow of information (and misinformation) about the disease (8, 9). The lethality of COVID-19 in particular is highly discussed by the news media and general public, especially because wide differences have emerged in the COVID-19 case-fatality rate (CFR) across countries (7). This wide variation has contributed to confusion among the general public and also among scientists and policymakers as to how fatal infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) really is (10).
A large part of the variation in CFRs across countries may be due to the ages of individuals who are tested and identified. One consistent pattern across countries is that the COVID-19 CFR rises sharply over age (Supplement Figure 1) (11). This relationship means that small differences in the age distribution of cases can have a strong influence on the overall CFR observed in the population. Indeed, there has been discussion about the role that the age distribution of cases plays in observed CFR differences (12). For example, news sources and scientific journals have reported that lower CFRs in low- and middle-income countries could reflect younger population distributions and that the high CFR in Italy might be due to the large proportion of older individuals with confirmed COVID-19 (10, 13). However, the contribution of such age-based distortions on observed CFR differences across populations has not been empirically examined and quantified.
We measured how much of the wide variation in CFRs across countries is due to differences in the age distribution of cases rather than differences in the virulence of SARS-CoV-2, underlying health of cases (independent of age), and the ability of the health system to effectively care for patients with COVID-19. This information is important for comparing countries' performance in treating and caring for patients with COVID-19 and to measure progress over time. This information can also help policymakers and the public anticipate the likely CFR in their countries, particularly in resource-limited countries where the epidemic has not yet reached its peak.
Methods
Data Sources
We used data on COVID-19 cases and deaths by age for all countries for which this age-disaggregated data was available as of 19 April 2020 (N = 1 223 261): China, France, Germany, Italy, the Netherlands, South Korea, Spain, Switzerland, and the United States. For the United States, China, and South Korea, we obtained data from the Centers for Disease Control and Prevention or that country's equivalent agency (14–16). For other countries, we obtained data directly from official government reports (17–22).
These 9 countries are the focus of our analysis because they were the countries for which detailed age-disaggregated data were available at the time of the analysis. However, we also explored the role of age-structure among a larger sample of 95 countries (countries with at least 500 confirmed cases as of 19 April 2020) for which information on overall COVID-19 CFRs (not disaggregated by age) was available. For these countries, we extracted information on overall COVID-19 CFRs compiled by the European Centre for Disease Prevention and Control as of 19 April 2020 (23). We also drew information on the overall population age distribution for each country for 2020 from the United Nations World Population Prospects, 2019 revision database (24). Supplement Tables 1 to 16 show all of the input data used in this study.
Data on age-specific COVID-19 mortality for Italy, Spain, Switzerland, the Netherlands, China, and South Korea were published for common age groups (0-9 years, 10–19 years, 20–29 years, 30–39 years, 40–49 years, 50–59 years, 60–69 years, 70–79 years, ≥80 years). However, data for the United States, Germany, and France were published with a different set of age groups. For these countries, we converted from the published age groups to those used for the majority of the countries in our study. To do this, we first calculated the age-specific CFRs (the number of deaths in a given age group divided by the number of cases in that age group) within the published age groups. We then assumed that the values of the age-specific CFRs corresponded to the midpoint of the published age groups and used linear interpolation between the age groups to estimate the CFR at the midpoint of the age groups used in the other countries. For the United States, we conducted this process separately for COVID-19 cases and COVID-19 deaths since the data were from 2 different sources with different age groups. We graphically demonstrate this process for the United States, Germany, and France in Supplement Figures 2 to 5. Of note, our main conclusions remain unchanged if these 3 countries are omitted.
Demographic Analyses
Our main aim was to determine how much of the differences in the observed overall CFR across countries can be attributed to differences in the age distribution of cases. To explore this, our analysis had the following 3 steps. First, we calculated the observed overall CFR in each country by multiplying the age-specific CFRs by the corresponding age-specific share of cases in that age group and summing this product across age groups:
Here, is mi the age-specific CFR and is di the proportion of cases in age group i.
Second, we compared the observed overall CFR with 2 age-adjusted CFRs: the age-expected CFR and the age-standardized CFR. To estimate the age-expected CFR, we conducted the same procedure as for the observed overall CFR, except that instead of using the observed age-specific proportions of cases, di, we used the share of the overall population in age group

Third, we estimated the age-standardized CFR similarly, this time using a common age distribution of cases,

, across all countries (Supplement Table 14 shows the estimated standard distribution).
Compared with the observed overall CFR, the age-expected CFR corrects for within-country distortions by assuming that the age distribution of the entire population is a better estimate of the true underlying distribution of cases than the observed age distribution of COVID-19 cases, which is strongly influenced by who presented with the most salient symptoms and was thus tested. Another way of conceptualizing the age-expected CFR is that it is the CFR that would occur if, within a given population, individuals of all ages were equally likely to be infected regardless of who showed symptoms or was tested. Of note, because the age-expected CFR does not use the observed age distribution of cases, it is less dependent on the distribution of testing in a population. This approach of applying age-specific rates estimated from a subpopulation (in our case, only among those who have been tested and confirmed to have COVID-19) to the overall age distribution of a population to estimate population-level rates is often used in environments where high-quality mortality data are available for only a small subset of the population. For example, studies in India, where comprehensive cause-of-death registers do not exist, have estimated overall cause-specific mortality rates by applying age-and-cause–specific mortality rates from a mortality surveillance cohort to the overall population distributions (25).
The goal of age-expected CFRs is to attempt to correct for distortions in who was tested within populations and therefore provide a more accurate picture of the CFR in each country separately. In contrast, age-standardized rates provide a way to compare CFRs across countries. By standardizing the CFRs using a common case-distribution by age across countries, any differences that remain among countries are purely due to differences in their age-specific CFRs.
We estimated the contribution of these 2 age adjustments as the difference in the SD of CFRs across countries relative to the observed rates. For all estimated rates, the widths of the 95% Cis were within 7% of reported rate for most of the countries and within 14% of the reported rates for the Netherlands and South Korea.
Next, we used a form of indirect standardization to explore how much variation we would expect in the COVID-19 CFR across countries purely due to differences in population age distributions and how much “excess” variation we observe due to distortions caused by age distribution among the larger sample of 95 countries. We were unable to use this larger sample of countries for our primary analyses because they did not have information on COVID-19 mortality disaggregated by age. For each country in this analysis, we estimated an overall predicted CFR on the basis of the age distribution of the country and a common set of age-specific CFRs across countries. We constructed the common age-specific CFRs as the mean of the age-specific CFRs across the 9 countries in our first analyses, because they were the countries for which age-disaggregated data were available (Supplement Table 16 shows this common age pattern of COVID-19 mortality). This process completely removed the influence of country differences in age-specific COVID-19 mortality, thus allowing only differences in the age distribution to drive differences in the overall predicted CFRs (this procedure if often referred to as “indirect standardization” and can be thought of as standardizing the age-specific CFRs rather than standardizing the case distribution across ages). We then compared the across-country distribution and SD in these predicted CFRs with the across-country distribution and SD in actual reported CFRs. We were, unfortunately, unable to directly age-standardize the rates for this larger set of countries because we did not have age-disaggregated information on cases and deaths.
Results
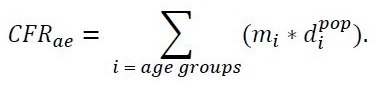
There was wide variation in the observed overall CFRs, with the highest rates in Italy (9.3%), the Netherlands (7.4%), and Spain (6.0%) and lowest rates in South Korea (1.6%), the United States (1.2%), and Germany (0.7%) (Figure 1). These wide differences led to an SD of the observed overall CFRs of 3.1%. The differences across countries attenuated substantially between the observed overall and age-expected CFRs. For example, Italy's high observed overall CFR decreased by half (to 4.6%) and the Netherlands' rate decreased by nearly two thirds (to 2.6%). Conversely, Germany's low rate doubled (to 1.5%). Not all countries had a large change between the observed overall and age-expected rates. For example, South Korea's rate only decreased by 0.1% to an age-expected rate of 1.5%. Overall, moving from the observed overall to age-expected CFRs decreased the SD of the CFRs across countries from 3.1% to 1.2%.
Figure 1. Observed, age-expected, and age-standardized coronavirus disease 2019 case-fatality rates.
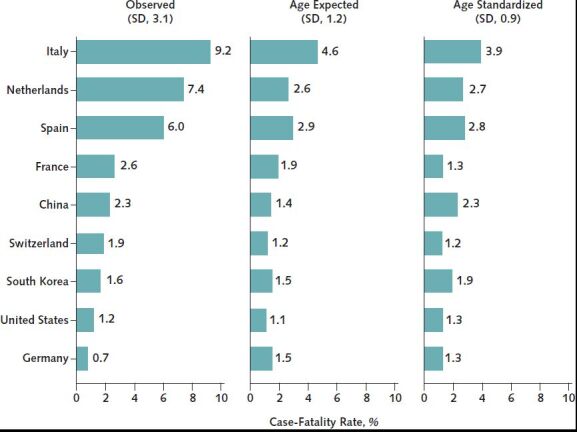
Age-expected rates use the age distribution of the country's general population; age-standardized rates use the mean age distribution of diagnosed severe acute respiratory system coronavirus 2 infections across the 9 countries as the standard.
Figure 2 shows pairwise comparisons of what the age-expected CFR of any country would be if they had the age distribution of another country. The figure reveals the strong influence that age has on comparisons between countries with very different age structures. For example, China's comparatively low age-expected CFR of 1.4% would increase to 2.5% if China had the age distribution of Germany, and 2.4% if it had the age distribution of Spain. Similarly, South Korea's age-expected CFR would increase from just 1.5% to 2.4% if it had the age distribution of Italy. Conversely, Italy's high age-expected CFR of 4.6% would decrease to 3.2% under South Korea's age distribution and halve to 2.3% under China's age distribution.
Figure 2. Estimates of the case-fatality rate for each country under the age distribution of other countries.
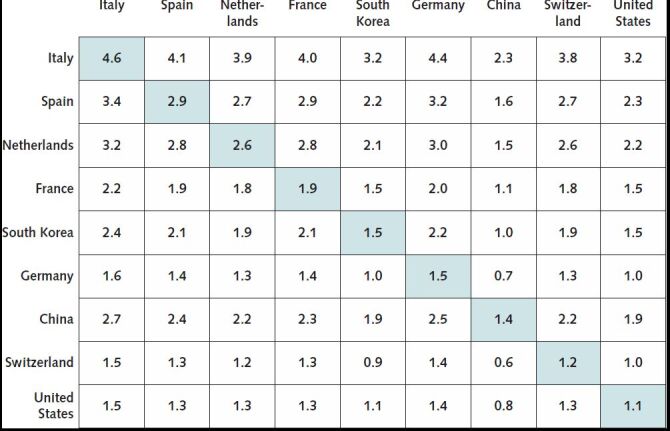
Diagonal boxes are the age-expected case-fatality rates for each country. Off-diagonal estimates are interpreted as, “What would the age-expected case-fatality rate for country X be if it had the age-distribution of country Y?”.
The differences across countries further attenuated between the age-expected and age-standardized CFRs, with a further reduction in the SD to 1.0%, and a median age-adjusted CFR of 1.9%. Given that the SD for the observed CFR between countries is 3.1 and the SD for the age-standardized CFR 1.0, we conclude that differences in the age distribution of cases are responsible for two thirds of the variation in the observed CFRs across countries. Of note, although age standardization reduced the differences in CFRs across countries, even after age standardization, Italy (3.9%), Spain (2.8%), and the Netherlands (2.7%) still had the highest CFRs. Adjustment for age differences, however, affected which countries have the lowest rates. Switzerland became the best-performing country, with an age standardized CFR of just 1.2%, whereas South Korea went from the third- to fifth-best performing country. Germany's considerable advantage among the observed CFRs also disappeared, with an age-standardized CFR on par with the United States and France.
Among the larger analysis of 95 countries, there was large variation in observed overall CFRs, with a difference of 28.6 percentage points between the highest rates in Sudan (28.6%) and Angola (25.0%) and the lowest rates in Eritrea (0.0%) and Cambodia (0.0%) (Figure 3). The variation for the predicted CFRs was substantially smaller, with a difference of just 1.9 percentage points between the highest rate (2.1% in Malta) and the lowest rate (0.24% in Uganda). Overall, the SD of CFRs decreased markedly, from 6.4 among the observed overall CFRs to just 0.5 among the predicted CFRs.
Figure 3. Distribution of observed and predicted case-fatality rates across 95 countries.
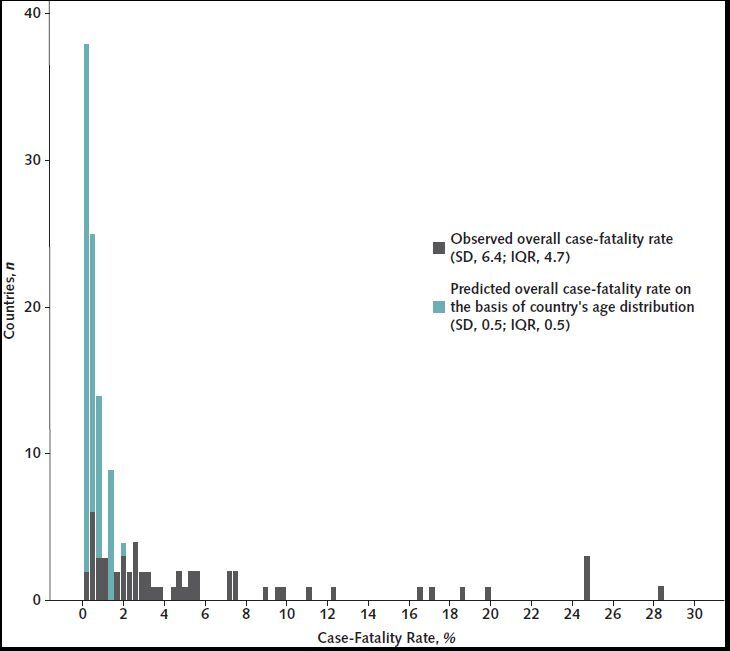
The predicted case-fatality rates use the age distribution of the country and the average age-specific case-fatality rates of the 9 countries in Figure 2. IQR = interquartile range.
Discussion
We found that distortions from the ages of individuals who were tested and identified as having COVID-19 explains two thirds of the variation in overall CFRs across countries. This suggests that selective testing and identification of older patients and age-distribution differences among countries considerably warp estimates of differences in the lethality of COVID-19. This distortion is especially salient for pairwise comparisons of countries with very different age structures, such as Italy and China, where changes to the age distribution of cases drastically affects the difference in CFRs between countries. We observed a similar phenomenon among our larger sample of 95 countries and found that observed differences among countries in overall COVID-19 CFRs are far larger than what we would expect on the basis of just age-composition differences across countries.
Compared with the observed overall CFRs, our age-expected rates make the assumption that individuals of all ages have an equal likelihood of being infected regardless of whether they are symptomatic or tested. This means the age-expected rates are a product of the overall age structure of a country and its age-specific CFRs. Therefore, changes between the observed overall and age-expected CFRs within a country reflect the extent to which the observed age distribution of cases is older or younger than the overall population distribution. For example, we found that the CFR in Germany doubled when moving from the observed to the age-expected CFR, whereas the CFR in Italy, the Netherlands, and Spain approximately halved. This reveals that in Germany, the distribution of individuals who were tested and confirmed as having COVID-19 was substantially younger than the overall population, implying that testing was disproportionately done among younger individuals. Conversely, in Italy, the Netherlands, and Spain, the distribution of confirmed cases was far older than the overall population distribution, suggesting that identification was disproportionately done among older individuals. This may reflect differences in testing strategies. For example, countries where testing was done primarily among those who exhibit severe symptoms and seek care are likely to disproportionately identify older cases, leading the observed overall CFR to be much higher than the age-expected CFR.
Compared with age-expected CFRs, the age-standardized CFRs provide a way to compare COVID-19 mortality across countries while filtering out any differences between countries in both the age distributions of COVID-19 cases and the age distributions of their populations. For example, whereas the observed overall and age-expected rates gave the impression that China and South Korea had much lower CFRs than the other countries, this difference narrowed considerably after age standardization. This change reveals that the comparatively younger distribution of these 2 countries gave a skewed impression of how they were faring relative to countries with older age distributions. Of note, however, age-standardized CFRs are primarily a tool for comparing countries with one another. Indeed, changes within a country between the age-expected and age-standardized rates do not provide any information other than that the age distribution of a country is different from the standard distribution.
After age standardization, the highest CFRs were still observed in Italy, Spain, and the Netherlands, and the lowest CFR occurred in Switzerland, followed closely by France, the United States, and Germany. Several factors are likely to explain these residual differences across countries, including differences in the underlying health of the populations; timely identification of and care for COVID-19; health care quality, especially for treatment of chronic conditions; and, more broadly, the general preparedness of health systems for COVID-19 care (26–29). An important future area of research will be to identify the contribution of each of these pathways to ultimately prepare health systems for future waves of the epidemic.
Our study has limitations. First, the age-expected CFR relies on the assumption that all individuals in the population are equally likely to be infected (regardless of whether they show symptoms or are ultimately tested). This assumption could be violated for clinical reasons, such as if persons with preexisting chronic conditions are more susceptible to infection, and social reasons, if age is related to the likelihood that an individual congregates in groups or engages in preventive behavior. Evidence in support of both these potential pathways is still emerging with some indication, for example, that individuals with diabetes may be more susceptible to infection (30), and that the high rate of infection among older Italians relative to other age groups was not just a distortion from testing but was instead related to cultural practices, whereby older Italians were more likely to live in the same household with younger generations (12). Ultimately, evidence on the true susceptibility and how it varies across the population is still emerging; in the interim, however, we believe our approach of assuming a uniform infection rate by age provides a better estimate of the true infection distribution than the distribution of identified cases.
In addition, both the age-expected and age-standardized CFRs make the additional assumption that the age-specific CFRs among individuals who were identified as having COVID-19 are the same as those who had undiagnosed disease. The extent to which this assumption holds probably varies with country-specific testing approaches. In countries with widespread and early testing, such as South Korea and Germany, the observed age-specific CFRs are likely to be more representative of the true age-specific CFRs because they are based on a broader population sample. However, in countries where testing was less comprehensive and more likely to be done among severe cases, such as in the United States and Italy, the observed age-specific CFRs may be higher than the true values because more severe cases were likely to be detected. Similarly, attribution of deaths to COVID-19 may bias age-specific CFRs if countries define COVID-19 deaths differently. In these circumstances, neither the age-expected nor age-standardized rates will correct for this source of bias. Continuously evaluating and reestimating CFRs as countries expand testing will be crucial for alleviating these biases and developing a better understanding of the lethality of the condition.
Our study reveals the strong and important role that the age distribution of cases can have on COVID-19 case fatality. However, even after we corrected for age distortions, important differences in CFRs remained across countries. This suggests that differences in the underlying health of a country's population and how effectively the health system cares for identified COVID-19 cases have meaningful effects on the share of individuals diagnosed with COVID-19 who survive. Removing the noise from age distortions and focusing on why age-adjusted CFRs are higher in some countries than in others, and why they change within countries over time, will be essential for formulating best case strategies for preventing and reducing COVID-19 mortality.
Supplementary Material
Footnotes
This article was published at Annals.org on 22 July 2020
*Dr. Sudharsanan and Mr. Didzun contributed equally.
References
- 1. Armocida B, Formenti B, Ussai S, et al. The Italian health system and the COVID-19 challenge [Letter]. Lancet Public Health. 2020;5:e253. [PMID: 32220653] doi:10.1016/S2468-2667(20)30074-8 [DOI] [PMC free article] [PubMed]
- 2. Saglietto A, D'Ascenzo F, Zoccai GB, et al. COVID-19 in Europe: the Italian lesson [Letter]. Lancet. 2020;395:1110-1111. [PMID: 32220279] doi:10.1016/S0140-6736(20)30690-5 [DOI] [PMC free article] [PubMed]
- 3. Tan BYQ, Chew NWS, Lee GKH, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020. [PMID: 32251513] doi:10.7326/M20-1083 [DOI] [PMC free article] [PubMed]
- 4. Baker SR, Bloom N, Davis SJ, et al. COVID-induced economic uncertainty. National Bureau of Economic Research. Working Paper 26983. April 2020. DOI:10.3386/w26983
- 5. Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly [Letter]. Lancet Public Health. 2020;5:e256. [PMID: 32199471] doi:10.1016/S2468-2667(20)30061-X [DOI] [PMC free article] [PubMed]
- 6. Dorn AV, Cooney RE, Sabin ML. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395:1243-1244. [PMID: 32305087] doi:10.1016/S0140-6736(20)30893-X [DOI] [PMC free article] [PubMed]
- 7. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time [Letter]. Lancet Infect Dis. 2020;20:533-534. [PMID: 32087114] doi:10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed]
- 8. Cinelli M, Quattrociocchi W, Galeazzi A, et al. The COVID-19 social media infodemic. arXiv. Preprint posted online 10 March 2020. arXiv:2003.05004 [DOI] [PMC free article] [PubMed]
- 9. Garfin DR, Silver RC, Holman EA. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol. 2020;39:355-357. [PMID: 32202824] doi:10.1037/hea0000875 [DOI] [PMC free article] [PubMed]
- 10. Henriques M. Coronavirus: Why death and mortality rates differ. BBC. 2 April 2020. Accessed at www.bbc.com/future/article/20200401-coronavirus-why-death-and-mortality-rates-differ on 20 April 2020.
- 11. Goldstein JR, Lee RD. Demographic perspectives on mortality of Covid-19 and other epidemics. National Bureau of Economic Research. Working Paper 27043. April 2020. DOI:10.3386/w27043 [DOI] [PMC free article] [PubMed]
- 12. Dowd JB, Andriano L, Brazel DM, et al. Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc Natl Acad Sci U S A. 2020;117:9696-9698. [PMID: 32300018] doi:10.1073/pnas.2004911117 [DOI] [PMC free article] [PubMed]
- 13. Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in italy. JAMA. 2020. [PMID: 32203977] doi:10.1001/jama.2020.4683 [DOI] [PubMed]
- 14. Division of Risk Assessment and International Cooperation, KCDC. The updates on COVID-19 in Korea as of 30 March. 30 March 2020. Accessed at www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030 on 31 March 2020.
- 15. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19): cases in the US. Accessed at www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html on 19 April 2020.
- 16. Zhang Y. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Weekly. Accessed at http://weekly.chinacdc.cn/en/article/id/e53946e2-c6c4-41e9-9a9b-fea8db1a8f51 on 29 March 2020. [PMC free article] [PubMed]
- 17. Santé publique France. COVID-19: point épidémiologique du 15 mars 2020. 18 March 2020. Accessed at www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/documents/bulletin-national/covid-19-point-epidemiologique-du-15-mars-2020 on 29 March 2020.
- 18. Istituto Superiore di Santia. Edidemia COVID-19: Aggiornamento nazionale. 26 March 2020. Accessed at www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_26-marzo%202020.pdf on 29 March 2020.
- 19. Schweizerische Eidgenossenschaft. Daten des Coronavirussituationberichts, Stand 2020-03-29. Accessed at www.bag.admin.ch/bag/de/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/situation-schweiz-und-international.html on 29 March 2020.
- 20. Rijksinstituut voor Volksgezondheid en Milieu. Ontwikkeling COVID-19 in grafieken. www.rivm.nl/coronavirus-covid-19/grafieken on 31 March 2020.
- 21. Ministerio de Sanidad, Gobierno de Espana. Actualización no 60. Enfermedad por el coronavirus (COVID-19). www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov-China/documentos/Actualizacion_61_COVID-19.pdf on 1 April 2020.
- 22.NPGEO Corona. RKI COVID19. https://npgeo-corona-npgeo-de.hub.arcgis.com/datasets/dd4580c810204019a7b8eb3e0b329dd6_0/data?selectedAttribute=AnzahlTodesfall on 29 March 2020.
- 23. European Centre for Disease Prevention and Control. Download today's data on the geographic distribution of COVID-19 cases worldwide. Accessed at www.ecdc.europa.eu/en/publications-data/download-todays-data-geographic-distribution-covid-19-cases-worldwide on 4 April 2020.
- 24. United Nations Department of Economic and Social Affairs. World Population Prospects: The 2019 Revision. New York: United Nations; 2019.
- 25. Bassani DG, Kumar R, Awasthi S, et al; Million Death Study Collaborators. Causes of neonatal and child mortality in India: a nationally representative mortality survey. Lancet. 2010;376:1853-60. [PMID: 21075444] doi:10.1016/S0140-6736(10)61461-4 [DOI] [PMC free article] [PubMed]
- 26. Guan WJ, Liang WH, Zhao Y, et al; China Medical Treatment Expert Group for COVID-19. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55. [PMID: 32217650] doi:10.1183/13993003.00547-2020 [DOI] [PMC free article] [PubMed]
- 27. NCD Risk Factor Collaboration (NCD-RisC). Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet. 2019;394:639-651. [PMID: 31327564] doi:10.1016/S0140-6736(19)31145-6 [DOI] [PMC free article] [PubMed]
- 28. Sun Q, Qiu H, Huang M, et al. Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu Province [Letter]. Ann Intensive Care. 2020;10:33. [PMID: 32189136] doi:10.1186/s13613-020-00650-2 [DOI] [PMC free article] [PubMed]
- 29. Patanavanich R, Glantz SA. Smoking is associated with COVID-19 progression: a meta-analysis. Nicotine Tob Res. 2020. [PMID: 32399563] doi:10.1093/ntr/ntaa082 [DOI] [PMC free article] [PubMed]
- 30. Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? [Letter]. Lancet Respir Med. 2020;8:e21. [PMID: 32171062] doi:10.1016/S2213-2600(20)30116-8 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


