Abstract
Oxidized zirconium was introduced as an alternative bearing surface to decrease polyethylene wear and reduce aseptic mechanical failure of hip and knee arthroplasties. Oxidized zirconium combines the strength of a metal with wear properties of ceramic, proposing increased survivorship of implant components, and possible decreased rate of revision. Despite a harder surface than cobalt-chromium, the substrate of zirconium is a softer metal. Although uncommon, prior reports have described accelerated wear and severe metallosis after femoral head dislocation in oxidized zirconium total hip arthroplasty; however, this has not been described in total knee arthroplasty. We report a case of an oxidized zirconium total knee arthroplasty failure in a patient with knee instability. This is the first report of catastrophic failure of an oxidized zirconium total knee arthroplasty implant.
Keywords: Oxidized zirconium, Total knee arthroplasty, Total knee replacement, Metallosis
Introduction
Total joint arthroplasty has been identified as one of the most commonly performed elective surgeries in the United States [[1], [2], [3]]. Various models have projected primary total knee arthroplasty (TKA) volumes to increase to numbers ranging from 1.26 to 3.48 million by 2030 [1,2,4]. The demand for arthroplasty is also growing among a younger (<65 years) and more active population, which poses a higher risk for revision secondary to their activity level and the higher demand placed on prostheses. Owing to the need for increased implant longevity, alternative bearing surfaces that exhibit improved wear resistance continue to be an area of development.
Oxidized zirconium has been used for femoral components in TKA since the 1980s and total hip arthroplasty (THA) since 2003 [5]. It is produced by heating a zirconium alloy in air (97.5% zirconium + 2.5% niobium), forming a hard 5-μm outer oxidized surface that is over twice the hardness of a cobalt-chromium alloy, giving it the strength of a metal while also avoiding the risk of brittle fracture that can occur with ceramic [[5], [6], [7]]. Oxidized zirconium implants were initially introduced as an alternative bearing surface to reduce polyethylene wear and aseptic loosening in TKA and have demonstrated improved survival rates [8]. Owing to its proposed benefits, oxidized zirconium has been used in patients with metal sensitivities [9,10] and in revision after metallosis [11].
There have been prior reports of accelerated wear and severe metallosis after dislocation of THA oxidized zirconium femoral heads and unicompartmental knee arthroplasties [7,[12], [13], [14], [15], [16]]; however, this has not been described in TKA. We report a case of mechanical failure and metallosis of an oxidized zirconium TKA in a patient with knee instability. To our knowledge, this is the first report of catastrophic failure of an oxidized zirconium TKA implant.
Case history
Informed consent was obtained from the patient. The patient is a 68-year-old female with multiple comorbidities including cerebellar ataxia, hypertension, hyperlipidemia, and major depressive disorder who underwent left TKA at an outside institution in 2014. After the index procedure, the patient presented in April 2019 endorsing pain, difficulty bearing weight, knee instability, and buckling. On examination, the incision was well healed, there was no erythema or swelling, but there was significant laxity to varus and valgus stress. Imaging demonstrated a widened and asymmetric joint space but no sign of perihardware lucency or hardware failure (Fig. 1). A knee aspirate was obtained and was notable for synovial leukocytosis >20,000 c/mm (automated count), with 5% polymorphonuclear cells. A manual cell count was not obtained. Aspiration cultures remained negative. Owing to the patient’s neurologic condition and inability to tolerate a two-stage procedure, the patient was indicated for a single-stage revision of her left knee with placement of a hinged prosthesis to optimize stability.
Figure 1.
Anteroposterior and lateral views of the left knee preoperatively demonstrating an asymmetric joint space. No sign of perihardware lucency or hardware failure.
Surgical intervention
The patient underwent left knee debridement and irrigation and revision TKA with a distal femoral replacing rotating hinge. Examination under anesthesia revealed gross instability with greater than 30 degrees laxity to varus and valgus stresses with soft end points. The knee was able to dislocate anteriorly and subluxate posteriorly. A medial parapatellar arthrotomy was performed, and no purulence was noted. However, abundant black metallosis was found (Fig. 2). An extensive synovectomy was performed removing all darkened synovium, as well as components, with minimal bone loss. Surrounding soft tissues and ligamentous structures were attenuated. The femoral component showed extensive wear and loss of the black appearance on the lateral aspect of the medial femoral condyle. The tibial component showed scratching along the posteromedial aspect of the tibial tray consistent with repeated anterior subluxation or dislocation (Fig. 3). After completion of debridement and synovectomy, the knee was prepared for implantation of the hinged prosthesis because of the ligamentous incompetence. The tibia required a 10-mm augment, and the tibial stem was 150 mm and fully cemented using third-generation techniques. The femoral implant was a 3-cm implant cemented distally, and the 200-mm stem was press fit in the diaphysis. A 14-mm polyethylene held the knee stable and well balanced. The rotating hinge was then assembled. The knee capsule and skin were then closed, and a negative-pressure wound dressing was placed over the incision. The patient tolerated the procedure well with no complications.
Figure 2.

Intraoperative photographs demonstrating abundant black metallosis during revision.
Figure 3.
Intraoperative photographs after explantation with evidence of a groove in the metal beneath the surface on the anteromedial aspect of the femoral component and the posterior aspect of the tibial plate.
Postoperative course
The patient’s postoperative course was uneventful and without complication. Tissue samples that were sent for culture intraoperatively were negative. The incisional wound vacuum was discontinued and transitioned to a waterproof dressing on postoperative day 8. She mobilized with physical therapy during the admission and was discharged with a well-appearing incision and adequate pain control.
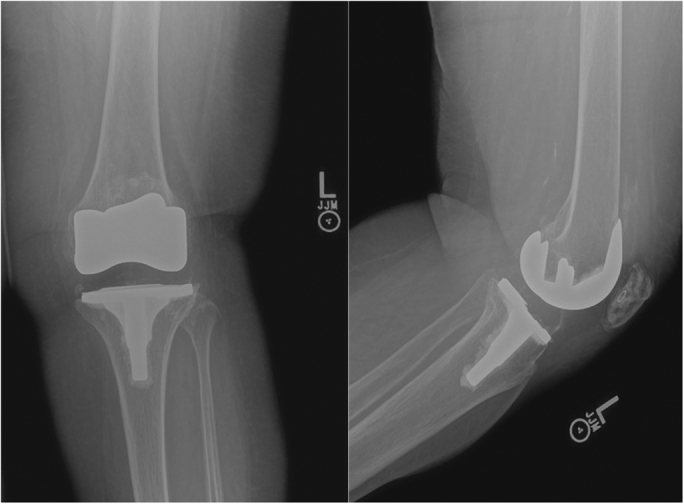
At follow-up, the patient reported markedly improved stability of her knee and endorsed being able to stand for short periods and ambulate short distances with physical therapy with no pain at 4 months. The patient’s knee remained stable with no pain at 9 months. However, secondary to progression of the patient’s neurologic disease, her functional status has since declined and she is unable to ambulate independently. Radiographs demonstrated no evidence of hardware compromise (Fig. 4).
Figure 4.

Anteroposterior and lateral radiographs of the left knee postoperatively.
Discussion
Metallosis is the infiltration of metallic-wear debris into the soft tissue and bony structures adjacent to a prosthesis. Although uncommon, it is a well-recognized complication of total joint arthroplasty. It is more common in hip arthroplasty than in knee arthroplasty and can arise from breakdown of either bearing or nonbearing surfaces. Chang et al. [17] reported a 5.3% incidence of metallosis of 418 THAs and recommended early revision in cases of metallosis to prevent rapid progression of osteolysis. Although less common in knee arthroplasty, it is recognized as a potential cause for failure. Schiavone Panni et al. [18] reported on four patients who developed metallosis, 1 unicompartmental knee replacement (UKA) and 3 TKAs, and noted that osteolysis results from the immune response to metallic particles and release of cytokines. In their series, one case of metallosis was the result of friction between the metal-back patellar component and anterior femoral component, which is prevented with the use of an all-polyethylene patellar component. The remaining three cases were caused by friction between the femoral and tibial prosthetic metal surfaces, resulting from full-thickness wear of the tibial polyethylene and progressive instability. The authors found that revision surgery rapidly eliminates pain and restores function in patients with metallosis.
Oxidized zirconium’s wear properties theoretically make it less prone to wear and catastrophic failure. The oxidized zirconium surface is noted to have twice the hardness of cobalt-chromium implants [10] and has been demonstrated to have lower friction, decreased wear rates, increased resistance to scratching, and reduced particle numbers compared with cobalt-chromium implants. A study conducted by Good et al. [6] demonstrated that oxidized zirconium femoral heads produced 61% less polyethylene wear and 45% fewer polyethylene particles than cobalt-chromium ones. Spector et al. [19] demonstrated that under clean conditions, femoral component polyethylene wear rates were more than sixfold lower than those of cobalt-chromium femoral components. Ries et al. [20] demonstrated under abrasive conditions, oxidized zirconium reduced the polyethylene wear rate by over eight times with a 44% reduction in particle numbers when compared with cobalt-chromium. The authors noted when components were roughened before wear testing, visual inspection of oxidized zirconium components also demonstrated shorter and shallower scratches to the surface and components were also less affected by the roughening procedure when compared with the cobalt-chromium components, suggesting oxidized zirconium has increased resistance to scratching.
Although oxidized zirconium could lengthen implant life and possibly decrease the need for revision on the basis of these studies, there is increasing evidence of accelerated wear and metallosis with oxidized zirconium THA implants after dislocation or reduction, leading to catastrophic failure [5,7,[12], [13], [14],21]. In addition, there have been at least 2 reports of catastrophic failure in patients with UKA secondary to dislocation of fixed polyethylene bearings [15,16].
The oxidized surface of oxidized zirconium is 5-μm thick, and although it possesses characteristics of an all-ceramic component with low friction, resistance to scratching, and decreased roughening while maintaining the hardness of a metal, the outer layer is a transformation of the underlying metal. Kop et al. [12] demonstrated that the underlying zirconium alloy core is a softer metal than cobalt-chromium and remains soft after the oxidation process, lending itself to plastic deformation, accelerated wear, and metallosis if left exposed.
Moussa et al. [22] also assessed the damage and characterized the roughness profile of oxidized zirconium femoral heads after dislocation. The authors demonstrated a substantial increase in surface roughness compared with a ceramic bearing surface when subjected to dislocation in vivo. The integrity of oxidized zirconium layer was compromised when exposed to unintended contact (ie, dislocation or reduction), and thus, subsequent accelerated wear and metallosis can ensue with exposure of the softer metal alloy.
In the case of our patient, it is unclear if knee instability was present immediately after the index procedure, subsequently leading to scratching of the oxidized zirconium surface and accelerated wear or vice versa. During the revision, visible scratches were noted on the femoral component and tibial tray (Fig. 3) that likely coincided with the episodes of buckling the patient reported, which then led to accelerated wear and metallosis. The patient’s automated cell count was elevated >20,000 c/mm; however, metal ions can falsely elevate automated cell counts [[23], [24], [25]]. A manual cell count should be considered in cases where metal ions may be present. Owing to her history of knee instability, low baseline physical demand, and comorbidities, she was revised to a hinge knee prosthesis, as this would optimally stabilize her knee. We recommend surgeons ensure proper balancing has been achieved, particularly when using oxidized zirconium components for TKA.
Summary
There have been prior reports of catastrophic oxidized zirconium failure in THA and unicompartmental knee arthroplasty; however, this is the first report of catastrophic failure of an oxidized zirconium TKA implant. Although it has been demonstrated to have lower friction, reduced wear, and higher resistance to scratching than cobalt-chromium implants, if the integrity of the 5-μm oxidized zirconium surface is violated either from dislocation or some other mechanism that causes scratching, these implants are at risk of accelerated wear and metallosis. The findings of this report highlight the importance of recognizing this as a mode of failure in oxidized zirconium implants and ensuring proper balancing and limit instability when these components are used. In addition, surgeons should consider catastrophic failure when evaluating patients presenting with instability and pain after TKA using oxidized zirconium.
Conflict of interest
The authors declare there are no conflicts of interest.
Footnotes
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of Defense or the US Government.
Appendix A. Supplementary data
References
- 1.Sloan M., Premkumar A., Sheth N.P. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018;100:1455. doi: 10.2106/JBJS.17.01617. [DOI] [PubMed] [Google Scholar]
- 2.Kurtz S.M., Lau E., Ong K., Zhao K., Kelly M., Bozic K.J. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Learmonth I.D., Young C., Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 4.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 5.Tribe H., Malek S., Stammers J., Ranawat V., Skinner J.A. Advanced wear of an OxiniumTM femoral head implant following polyethylene liner dislocation. Ann R Coll Surg Engl. 2013;95:e133. doi: 10.1308/003588413X13629960047876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Good V., Ries M., Barrack R.L., Widding K., Hunter G., Heuer D. Reduced wear with oxidized zirconium femoral heads. J Bone Joint Surg Am. 2003;85-A(Suppl 4):105. doi: 10.2106/00004623-200300004-00013. [DOI] [PubMed] [Google Scholar]
- 7.Evangelista G.T., Fulkerson E., Kummer F., Di Cesare P.E. Surface damage to an Oxinium femoral head prosthesis after dislocation. J Bone Joint Surg Br. 2007;89:535. doi: 10.1302/0301-620X.89B4.17557. [DOI] [PubMed] [Google Scholar]
- 8.Civinini R., Matassi F., Carulli C., Sirleo L., Lepri A.C., Innocenti M. Clinical results of oxidized zirconium femoral component in TKA. A review of long-term survival. HSS J. 2017;13:32. doi: 10.1007/s11420-016-9512-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lachiewicz P.F., Watters T.S., Jacobs J.J. Metal hypersensitivity and total knee arthroplasty. J Am Acad Orthop Surg. 2016;24:106. doi: 10.5435/JAAOS-D-14-00290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hunter G., Dickinson J., Herb B., Graham R. Creation of oxidized zirconium orthopaedic implants. J ASTM Int. 2005;2:1. [Google Scholar]
- 11.Vivegananthan B., Shah R., Karuppiah A.S., Karuppiah S.V. Metallosis in a total knee arthroplasty. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2013-202801. bcr2013202801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kop A.M., Whitewood C., Johnston D.J.L. Damage of oxinium femoral heads subsequent to hip arthroplasty dislocation three retrieval case studies. J Arthroplasty. 2007;22:775. doi: 10.1016/j.arth.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 13.Jaffe W.L., Strauss E.J., Cardinale M., Herrera L., Kummer F.J. Surface oxidized zirconium total hip arthroplasty head damage due to closed reduction effects on polyethylene wear. J Arthroplasty. 2009;24:898. doi: 10.1016/j.arth.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 14.Zou A.H., Novikov D., Feng J.E., Anoushiravani A.A., Schwarzkopf R., Vigdorchik J.M. Liner dissociation leading to catastrophic failure of an Oxinium femoral head. Arthroplast Today. 2019;5:21. doi: 10.1016/j.artd.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Greco N., Berend K. Polyethylene liner dislocation of fixed-bearing medial oxinium unicompartmental arthroplasty with severe metallosis. Knee. 2018;25:341. doi: 10.1016/j.knee.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Luyet A., Fischer J.-F., Jolles B.M., Lunebourg A. Unexpected wear of an unicompartimental knee arthroplasty in oxidized zirconium. Acta Orthop Belg. 2015;81:790. [PubMed] [Google Scholar]
- 17.Chang J.-D., Lee S.-S., Hur M., Seo E.-M., Chung Y.-K., Lee C.-J. Revision total hip arthroplasty in hip joints with metallosis: a single-center experience with 31 cases. J Arthroplasty. 2005;20:568. doi: 10.1016/j.arth.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 18.Schiavone Panni A., Vasso M., Cerciello S., Maccauro G. Metallosis following knee arthroplasty: a histological and immunohistochemical study. Int J Immunopathol Pharmacol. 2011;24:711. doi: 10.1177/039463201102400317. [DOI] [PubMed] [Google Scholar]
- 19.Spector B.M., Ries M.D., Bourne R.B., Sauer W.S., Long M., Hunter G. Wear performance of ultra-high molecular weight polyethylene on oxidized zirconium total knee femoral components. J Bone Joint Surg Am. 2001;83-A(Suppl 2 Pt 2):80. doi: 10.2106/00004623-200100022-00004. [DOI] [PubMed] [Google Scholar]
- 20.Ries M.D., Salehi A., Widding K., Hunter G. Polyethylene wear performance of oxidized zirconium and cobalt-chromium knee components under abrasive conditions. J Bone Joint Surg Am. 2002;84-A(Suppl 2):129. doi: 10.2106/00004623-200200002-00018. [DOI] [PubMed] [Google Scholar]
- 21.Carli A., Koch C.N., Esposito C.I., Wright T.M., Padgett D.E. Polyethylene wear increases in liners articulating with scratched oxidized zirconium femoral heads. Clin Orthop Relat Res. 2018;476:182. doi: 10.1007/s11999.0000000000000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moussa M.E., Esposito C.I., Elpers M.E., Wright T.M., Padgett D.E. Hip dislocation increases roughness of oxidized zirconium femoral heads in total hip arthroplasty: an analysis of 59 retrievals. J Arthroplasty. 2015;30:713. doi: 10.1016/j.arth.2014.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lombardi A.V., Jr., Barrack R.L., Berend K.R. The Hip Society: algorithmic approach to diagnosis and management of metal-on-metal arthroplasty. J Bone Joint Surg Br. 2012;94-B:14. doi: 10.1302/0301-620X.94B11.30680. [DOI] [PubMed] [Google Scholar]
- 24.Wyles C.C., Larson D.R., Houdek M.T., Sierra R.J., Trousdale R.T. Utility of synovial fluid aspirations in failed metal-on-metal total hip arthroplasty. J Arthroplasty. 2013;28:818. doi: 10.1016/j.arth.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 25.Yi P.H., Cross M.B., Moric M. Do serologic and synovial tests help diagnose infection in revision hip arthroplasty with metal-on-metal bearings or corrosion? Clin Orthop Relat Res. 2015;473:498. doi: 10.1007/s11999-014-3902-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



