Maintaining good general hygiene is an important aspect to prevent coronavirus disease (COVID-19), but there has been much controversy regarding face mask use in the community setting (1). The World Health Organization (WHO) does not recommend that healthy people wear a mask routinely (2), whereas the CDC has recently shifted to recommend wearing cloth face coverings in public (3) because of the evolving pandemic and new study findings on asymptomatic and presymptomatic virus transmission (4, 5). In many Asian countries such as China and Japan, the use of face masks in this pandemic is ubiquitous and is considered hygiene etiquette, whereas in many Western countries, its use in the public is less common. The discrepant behaviors between cultures have induced stigmatization and have even caused a rash of racism on several occasions.
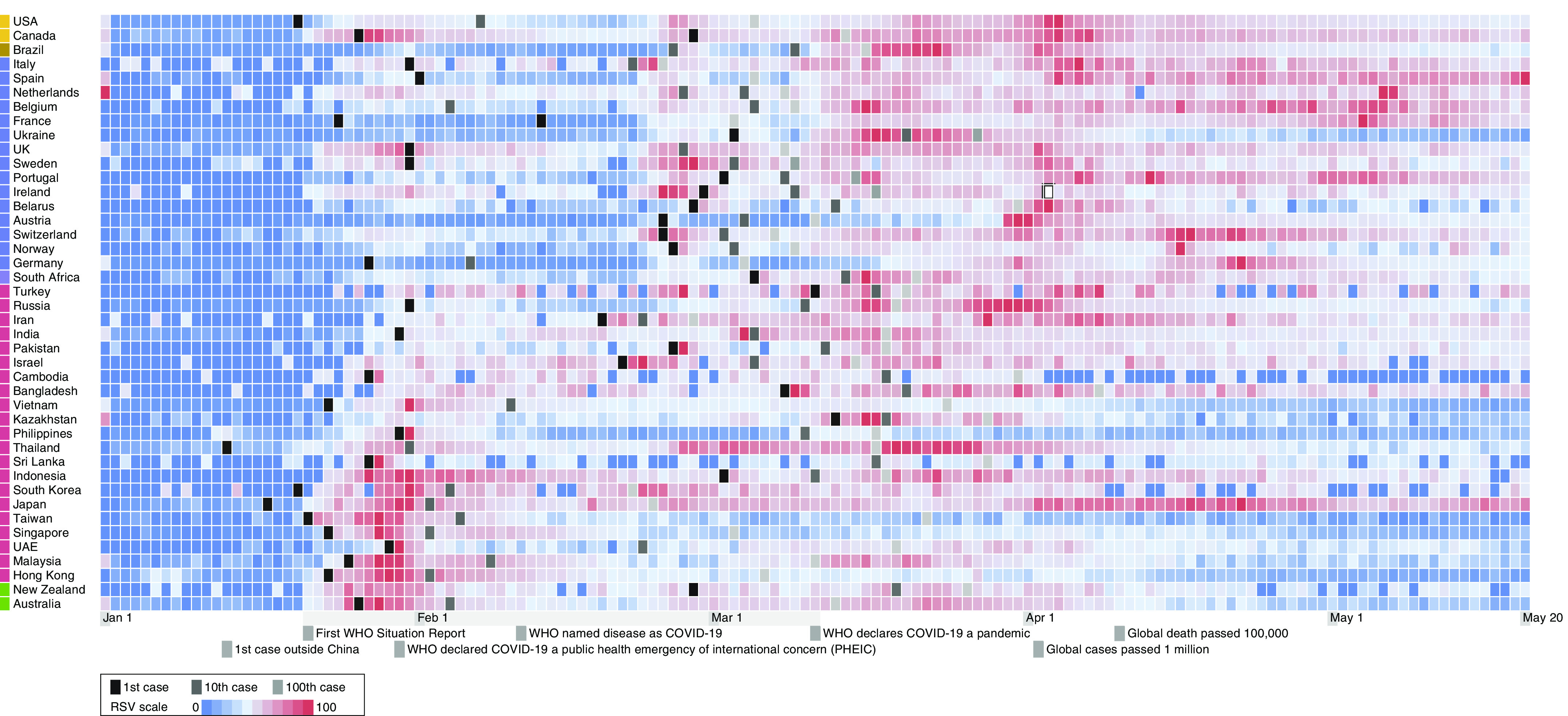
To explore the relationship between public interest in face masks and the COVID-19 epidemic, we retrieved the global incidence data and Google Trends relative search volume (RSV) data on the topic “surgical mask” until May 20, 2020. We observed a divergent pattern of RSV values along the timeline of COVID-19, with some geographical regions having peak RSV values early in the epidemic (Figure 1 and Table E1 in the online supplement). This led us to ask whether early awareness on face mask use could help contain the outbreak. We further retrieved the RSV data over the early epidemic period from January 21, 2020 (when WHO published the first Situation Report) to March 11, 2020 (when WHO officially declared a pandemic), and correlated with the epidemics in different regions indicated by the average daily number of COVID-19 cases (6). We observed a significant inverse correlation, with a Kendall rank correlation coefficient (τ) of −0.47 (P = 2.4 × 10−5) among 42 geographical regions from six continents. Notably, lower numbers of daily cases were seen in several Asian regions that correlated with high search volumes (Figure 2). Partial correlation analysis showed that this correlation remained independently significant after adjusting for RSV of related terms of hand washing and social distancing as well as government policy responses represented by the Oxford COVID-19 Government Response Tracker stringency index over the same period (7) (Table E2).
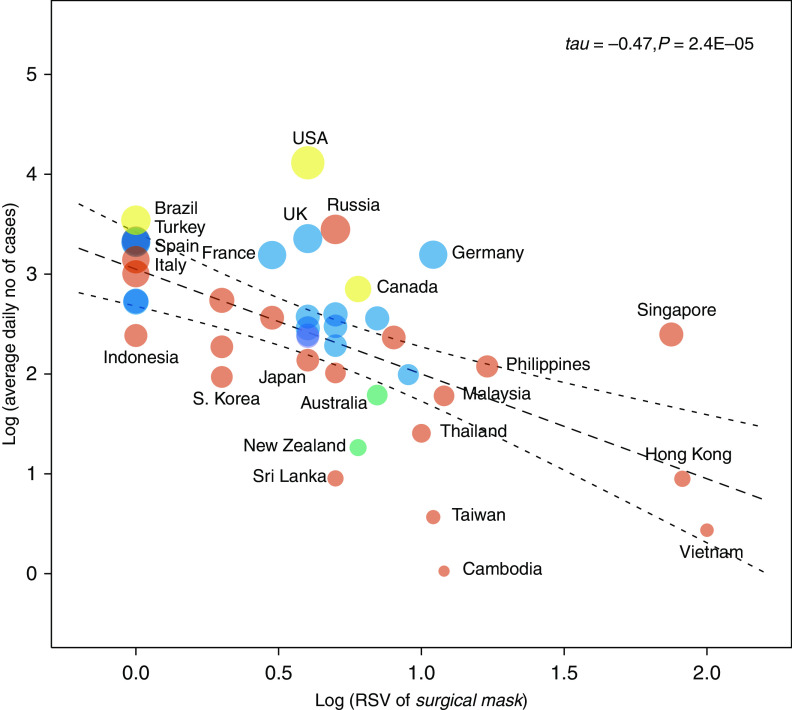
Figure 1.
Heat-map showing RSV of surgical mask over the epidemic period until May 20, 2020. The color gradients indicate the RSV values, and the striped/cross-hatched boxes indicate the dates of the 1st, 10th, and 100th coronavirus disease (COVID-19) cases in the respective region. RSV = relative search volume; WHO = World Health Organization.
Figure 2.
Diagram showing the relationship between RSV of surgical mask in the early epidemic period and the average daily number of cases. A significant correlation was observed (τ = −0.47; P = 2.4 × 10−5), and it remained robust after removal of outliers (P = 9.1 × 10−5) in sensitivity analysis. The dot colors indicate continents of the respective regions, and the dot sizes correspond to the total cumulative number of coronavirus disease (COVID-19) cases as of May 20, 2020. RSV = relative search volume.
These results suggest that early public interest with face mask may be an independently important factor in controlling the COVID-19 epidemic on a population scale. One illustrative region is Hong Kong, where the public interest in a face masks is among the highest. Paralleling the high RSV index, a recent survey showed that a face mask was used in 98.8% of the respondents to prevent COVID-19, a proportion higher than other measures of hand washing or crowd avoidance (8). Being one of the first cities inflicted by the severe acute respiratory syndrome (SARS) virus, residents in Hong Kong saw COVID-19 with an uncanny resemblance and quickly equipped themselves with protective wear early in the epidemics. Despite the close proximity and heavy passenger traffic with mainland China, the rise in case numbers in the city was relatively modest. At 16 days after having the first patient with COVID-19, there were only 12 confirmed local cases before the city imposed mandatory quarantine for individuals arriving at the border. During that period, the RSV value has reached its peak (Figure E1) as the city received 294,883 arrivals from mainland China (9). Although the RSV values do not necessarily equate mask purchase or its actual use, we observed significant correlations with global e-commence sales volumes and public opinion surveys (Table E3 and Figure E2). These suggest that the RSV index may serve as a good surrogate to reflect public interest even without absolute search volume data and population size adjustment (10).
It is reasonable to suggest that face masks can mitigate the current pandemic, as it may reduce coronavirus in aerosols and respiratory droplets (11). Multiple studies have demonstrated their protective role in preventing respiratory viral illnesses in health care (12) and household settings (13), acknowledging user adherence as an important factor. Furthermore, studies based on fluid dynamics unrelated to virus suggested that a cough turbulent gas cloud could propel to 7–8 m (14), and the SARS coronavirus 2 (SARS-CoV-2) may survive in environmental aerosols for 3 hours after deliberate jet nebulization (15), challenging the WHO and CDC recommendations on a social distance of 1–2 m. Advocacy to broaden the use of face masks in the community, both for source control and individual protection, should be considered, especially given the high viral load in asymptomatic or minimally symptomatic patients with COVID-19 (16).
The COVID-19 pandemic continues to inflict losses in different countries, yet we do not seem to have a highly effective method to control this disease. The healthcare systems worldwide are heavily burdened by the increase in case numbers, and the mortality rate can climb even higher when the systems become overloaded. We believe broader mask use is key to control the pandemic of COVID-19, apart from hand hygiene, social distancing, and other public policy measures. Although universal masking may seem tedious and is criticized by the lack of high-quality supporting evidence, we think it is reasonable to reconsider such a measure in all but sparse areas in the public. As the saying goes, “better safe than sorry,” and is it not better to adopt a possibly imperfect protective measure than to wait for more evidence at the expense of human lives?
Footnotes
Author Contributions: Conception and design: S.H.W. and J.Y.C.T. Analysis and interpretation: S.H.W., J.Y.C.T., C.-H.L., B.H.K.Y., and M.C.S.W. Drafting the manuscript for important intellectual content: S.H.W., J.Y.C.T., W.K.K.W., and D.S.C.H.
This letter has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Originally Published in Press as DOI: 10.1164/rccm.202004-1188LE on June 15, 2020
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ. Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med. 2020;8:434–436. doi: 10.1016/S2213-2600(20)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Coronavirus disease (COVID-19) advice for the public: When and how to use masks. 2020 [accessed 2020 May 27]. Available from: www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks.
- 3.Centers for Disease Control and Prevention (CDC) How to protect yourself & others. 2020 [accessed 2020 May 27]. Available from: www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html.
- 4.Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323:1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kimball A, Hatfield KM, Arons M, James A, Taylor J, Spicer K, et al. Public Health – Seattle & King County; CDC COVID-19 Investigation Team. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility - King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:377–381. doi: 10.15585/mmwr.mm6913e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hale T, Webster S, Petherick A, Philips T, Kira B Blavatnik School of Government. Oxford COVID-19 government response tracker. 2020 doi: 10.1038/s41562-021-01079-8. [accessed 2020 May 27]. Available from: www.bsg.ox.ac.uk/covidtracker. [DOI] [PubMed]
- 8.Cowling BJ, Ali ST, Ng TWY, Tsang TK, Li JCM, Fong MW, et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5:e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Hong Kong Special Administrative Region Government Immigration Department. Statistics on passenger traffic. 2020 [accessed 2020 May 27]. Available from: www.immd.gov.hk/eng/message_from_us/stat_menu.html.
- 10.Schootman M, Toor A, Cavazos-Rehg P, Jeffe DB, McQueen A, Eberth J, et al. The utility of Google Trends data to examine interest in cancer screening. BMJ Open. 2015;5:e006678. doi: 10.1136/bmjopen-2014-006678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leung NHL, Chu DKW, Shiu EYC, Chan KH, McDevitt JJ, Hau BJP, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Radonovich LJ, Jr, Simberkoff MS, Bessesen MT, Brown AC, Cummings DAT, Gaydos CA, et al. ResPECT Investigators. N95 respirators vs medical masks for preventing influenza among health care personnel: a randomized clinical trial. JAMA. 2019;322:824–833. doi: 10.1001/jama.2019.11645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cowling BJ, Chan KH, Fang VJ, Cheng CK, Fung RO, Wai W, et al. Facemasks and hand hygiene to prevent influenza transmission in households: a cluster randomized trial. Ann Intern Med. 2009;151:437–446. doi: 10.7326/0003-4819-151-7-200910060-00142. [DOI] [PubMed] [Google Scholar]
- 14.Bourouiba L.Turbulent gas clouds and respiratory pathogen emissions: potential implications for reducing transmission of COVID-19 JAMA[online ahead of print] 26 Mar 2020 [DOI] [PubMed] [Google Scholar]
- 15.van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]