Abstract
Brucellosis is one of the world's most widespread bacterial zoonoses caused by Brucella. It leads to considerable economic losses as a result of low productivity of infected animals and the long debilitating illness in humans. Despite its impact on human and animal health, little attention has been paid on Brucella infections in domestic animals. It is in this light that the prevalence of Brucella antibodies was determined in domestic animals with the overarching goal of improving our knowledge on brucellosis in southern Cameroon. During cross‐sectional studies conducted from December 2016 to August 2018 in five sites of southern Cameroon, blood samples were collected in cattle, sheep, goat, pig and dog. Plasma was obtained from each blood sample and Brucella antibodies were detected using the Rose Bengal test and the enzyme‐linked immunosorbent assay (ELISA). From 1873 animals that were sampled, the overall prevalence of Brucella antibodies using Indirect enzyme‐linked immunosorbent assay (i‐ELISA) was 6.35% (118/1873): 9.12% (78/855) in cattle; 8.04% (30/373) in sheep; 6.06% (2/33) in dog, 1.87% (3/160) in pig and 1.1% (5/452) in goat. Between animal species (p‐value < .0001, x 2 = 33.63) as well as sampling sites (p‐value = .0001, x 2 = 18.97), significant differences were observed in the prevalence of Brucella antibodies. Yoko and Noun localities have shown the highest prevalence of 8.6% (30/348) and 7.2% (78/1070), respectively. This prevalence was significantly higher (p = .03, x 2 = 1.25) in female than male cattle. Between adult (16.923%) and young cattle (7.8%), significant difference (p = .04, x 2 = 6.42) was observed in the prevalence of Brucella antibodies. This study shows that the prevalence of Brucella antibodies varies between animal species and localities. It also shows several domestic animals of southern Cameroon that have been in contact with Brucella. It enabled to identify villages where investigations on the transmission dynamic must be focused for the final goal of developing control measures for this neglected zoonotic disease.
Keywords: Brucella antibodies, brucellosis, Cameroon, domestic animals
Brucella infections can affect cattle, pigs, sheep, goats and dogs;As the results of Brucella infections, the prevalence Brucella antibodies varies not only between animal species, but also between localities for which each of them has specific environmental conditions;Understanding the epidemiology of brucellosis for the overarching objective of designing efficient control measures requires investigating such infections on human and animal in different epidemiological settings.

Impacts.
Brucella infections can affect cattle, pigs, sheep, goats and dogs;
As the results of Brucella infections, the prevalence Brucella antibodies varies not only between animal species, but also between localities for which each of them has specific environmental conditions;
Understanding the epidemiology of brucellosis for the overarching objective of designing efficient control measures requires investigating such infections on human and animal in different epidemiological settings.
1. INTRODUCTION
Brucellosis is a neglected anthropozoonotic disease caused by a group of bacteria of the genus Brucella (Aznar et al., 2015; Dean, Crump, Greter, Schelling, & Zinsstag, 2012). In livestock, Brucella infections cause abortion, premature birth and decreased productivity (Ayayi, Têko‐Agbo, & Koné, 2009; Havelaar et al., 2015). This infectious disease is one of the major constraints for livestock production in developing countries (Corbel, 1997; Fyumagwa, Wambura, Mellau, & Hoare, 2009). In sub‐Saharan Africa, brucellosis is considered as a serious public health problem which is responsible for tremendous economic losses estimated to be about 427 million USD per year (Mangen, Otte, Pfeiffer, & Chilonda, 2002). In this sub‐region, the prevalence of brucellosis ranges from sporadic cases to up to 41% in some affected areas (Bayemi, Webb, Nsongka, Unger, & Njakoi, 2009; Mazeri et al., 2013; Scolamacchia et al., 2010). Due to the lack of surveillance programme in many sub‐Saharan countries, many cases of Brucella infections are not detected (Ladbury et al., 2017). Therefore, the disease is neglected and poses an important public health threat (Ayayi et al., 2009). In most developing countries where the population growth increases steadily, the demand for livestock‐derived products such as the meat, milk and dairy products increases also in consequence (Abbasi, Abbasi, & Abbasi, 2016; Sibhatu, Krishna, & Qaim, 2015). To satisfy this demand requires improving animal production by fighting diseases that could jeopardize animal health and consequently, the quality and quantity of livestock‐derived products.
In Cameroon, previous studies have generated baseline information on cattle brucellosis in the northern part of the country (Awah‐Ndukum, Mouiche, Bayang, et al., 2018; Awah‐Ndukum, Mouiche, Kouonmo‐Ngnoyum, et al., 2018; Kelly et al., 2016; Mazeri et al., 2013; Scolamacchia et al., 2010). Despite the interesting data generated by these studies, no control strategy has been developed for brucellosis in Cameroon like in most sub‐Saharan countries. The development and implementation of control measures against brucellosis require deep investigations aiming to understand the current epidemiological situation of the disease. Although Brucella antibodies have been detected in cattle, no data has been published regarding Brucella infections in other domestic animals such as sheep, goats and pig. However, most of these animal species are susceptible to Brucella infections and they are also able to carry and transmit Brucella species that are responsible for human brucellosis.
In most sub‐Saharan countries where various domestic animal species are bred by inhabitants for which such animals constitute their main economic incomes; little attention has been paid on Brucella infections. Undertaking investigations on Brucella infections in different animal species as well as in different ecological settings could enable to generate data that will help to better understand the epidemiological situation of Brucella infections.
The present study was designed to improve our knowledge on Brucella infections in domestic animals from three agro‐ecological zones of southern Cameroon to generate data that could help to plan control strategies for brucellosis.
2. MATERIALS AND METHODS
2.1. Description of sampling sites
Domestic animals were sampled during cross‐sectional field surveys conducted in four regions (West, Central, South and South‐West) of southern Cameroon to determine the sero‐prevalence of Brucella antibodies in cattle, pigs and small ruminants. The first and second surveys were performed in December 2016 and June 2017 at Fontem, the third survey in August 2017 at Campo, the fourth in September 2017 at Bipindi, the fifth in November 2017 at Yoko and the sixth from April to June 2018 in the Noun Division.
The Noun division (between 4°95′ 6°30′N and 10°30′12°E) is situated in the western highlands (Agro ecological zone III) of Cameroon (Figure 1) (Silatsa et al., 2019). Its vegetation characterized by savannah and degraded forest offers favourable agro‐climatic conditions for cattle rearing. It is therefore, the main cattle breeding area of the western region of Cameroon (Bayemi et al., 2015). Its hydrographic network is dense with streams and rivers crossing the region and the dams that, in the dry season, make it as transhumance area for farmers. The cattle reared in this locality belong to breeds such as Zebu Goudali, Zebu White Fulani and Zebu Red Fulani with few cross breeds (indigenous and exotic). Indigenous sheep and goat breeds are also kept by inhabitants. For trade or transhumance purposes, animals can move from this locality to others and vice versa and even in neighbouring countries (Bayemi et al., 2015).
FIGURE 1.
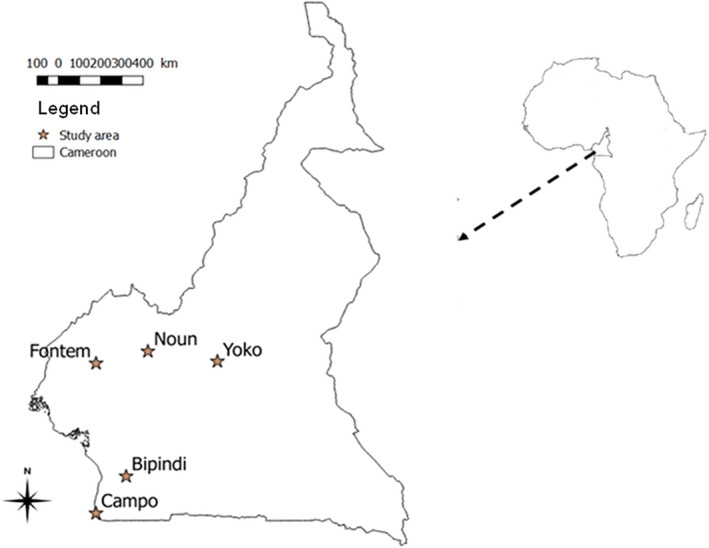
Map of Cameroon showing localities where sampling was undertaken
Fontem (5°40′00″N, 9°55′00″E) is located in Lebialem division in south‐west region of Cameroon (Figure 1). It belongs to the agro ecological zone IV with a relief made mainly of mountains and hills (Silatsa et al., 2019). Its altitude ranges from 300 to 2,500 m above sea level. In addition to agriculture, the population also practises breeding of cattle, pigs, goats and sheep. All pigs and dogs were of local breed, originating from a mixture of different breeds.
Bipindi (3°82′00″N, 10°82′20″E) and Campo (2°82′00″N, 9°85′20″E) (Figure 1) are located in the southern region of Cameroon. They belong to agro ecological zone IV characterized by a humid forest (Silatsa et al., 2019). The main source of livelihood for people in these two localities is hunting, but inhabitants practice also small breeding of pig, sheep and goat. Cattle breeding is not developed in this area due to unfavourable climatic conditions and also animal trypanosomiasis which occurs in these areas (Nimpaye et al., 2011; Njiokou et al., 2010). The sheep and goats reared are dwarf breeds (Djallonke west‐African dwarf for sheep and Guinea goat), which are known to be trypanotolerant. Local animals live in close contact with wild animals because of their proximity with forest. Some pigs were kept in pigsties whereas other move around villages. The other domestic animal species move freely around villages.
Yoko (05°30.895′N and 012°18.830′E) is situated in the Central region of Cameroon. It is part of the agro ecological zone V (Figure 1). Considered as the large basin for cattle and small ruminants production of the centre region, its vegetation is mainly constituted by forest and savannah. Its favourable climatic conditions for animals breeding (pasture, streams and river) favour uncontrolled movements of livestock from different regions of the country as well as from neighbouring country like the Central African Republic (Motta et al., 2018; Seignobos, 2008). In this locality, sheep, goats and cattle are reared together and these animals share the same pasture and water point. The breeding system is essentially free grazing and to a lesser extent, a combination between free grazing and stall‐feeding.
2.2. Sample size estimation
The prevalence of Brucella antibodies was determined in cattle, small ruminants, pigs and dogs in Southern Cameroon. For this study, a stratified sampling strategy was applied to select herds and then, individual cattle per herd. The sample size for cattle was estimated as described by Thrusfield (2007) using the bovine brucellosis prevalence of 5.2% previously reported by Bayemi et al. (2015) in the Northwest Region of Cameroon. For this estimation, the sensitivity and specificity of the tests used were 85% and 90%, respectively as given by the manufacturer, with a precision of 0.05 and 95% confidence intervals. Only herds with a minimum of 10 cattle that were older than 6 months at the time of sampling were included. Cattle were sampled by herd and in each herd, blood samples were collected in about 20% of animals. However, more than 20% of animals of some herds were sampled due to the interests (administration of vitamins and anthelminthic to animals) and cooperation of some farmers and advices from veterinarians. From each chosen herd, the selection of cattle to be sampled was done on the basis of a systematic random sampling technique as described by Asgedom, Damena, and Duguma (2016). A total of 38 farms were enrolled in 16 villages for a sample size of 855 cattle.
For the other animal species including pigs, sheep, goats and dogs for which there is no published data on the brucellosis prevalence in Cameroon, an expected prevalence of 50% was used to estimate the sampling size. Because of the small number of goats, sheep, dogs and pigs found in each village, all of them were sampled irrespective of the number of animals presented by each household. In consequence, 452 goats, 368 sheep, 160 pigs and 33 dogs from four divisions of four regions of Cameroon were sampled.
2.3. Blood collection and plasma preparation
After approval from each owner, the farm characteristics and information regarding each animal including the name of the village (where each sample was collected), the geographical coordinates of each sampling site, the animal species found in farm (cattle, goat, sheep), the origin, sex, age, breed and the feeding system were recorded. Blood sample was collected from each animal by a veterinarian. Anthelmintic and vitamin were administered to these animals following advice of the veterinarian. From each animal, about 5 ml of blood was collected into EDTA‐coated tubes. This collection was performed from the jugular vein in goats, pigs, sheep and cattle and from the saphenous vein in dogs. Tubes were labelled and carefully packed to avoid crossed contamination. In the field, the blood samples were stored at 4°C in an electric cooler before being transported to the laboratory where each sample was centrifuged at 8,000 × g for 10 min. After this centrifugation, 500 µl of plasma was collected from each tube and then, transferred into sterile labelled micro‐tube that was subsequently stored at −20°C until use.
2.4. Detection of Brucella antibodies
Brucella antibodies were detected using the Rose Bengal plate test (RBPT) which is a rapid test, and the i‐ELISA test. These two tests were used to improve the accuracy or the ability to detect Brucella antibodies.
2.4.1. Detection of Brucella antibodies by RBPT
The detection of Brucella antibodies in the plasma of domestic animals was performed with the RBPT (ID.Vet, Innovative Diagnostics) as described by Alton, Jones, Angus, and Verger (1988). Before each test, an aliquot of each plasma sample as well as the RBPT reagents were removed from the freezer and left to thaw at room temperature (22 ± 4°C) for approximately 25 min as recommended by the manufacturer. Thereafter, 30 μl of plasma and equal volume of RBPT antigen were put in each circle of the RBPT plate, and then mixed. Each plate has been allowed to rotate at room temperature for 4 min and the result was appreciated by examining the degree of agglutination. Any visible agglutination on the plate was considered positive (presence of Brucella antibodies in the plasma) (Nielsen & Yu, 2010). If no visible agglutination (no antibodies against Brucella) was observed, the test was considered negative.
2.4.2. Detection of Brucella antibodies by i‐ELISA
The i‐ELISA test was carried out as confirmation test on all samples that were positive to RBPT to confirm RBPT results. Samples tested negative to RBPT were grouped in pool of 10 before their confirmation by i‐ELISA test. Samples from positive pools were tested individually to identify the sample that induced the positive reaction. The i‐ELISA tests were performed in polystyrene plate of 96‐wells pre‐coated with purified Brucella spp. antigens. Plasma samples were tested for the presence of antibodies against Brucella spp. (B. arbortus, B. melitensis, B. suis and B. canis) using multi species commercial i‐ELISA test kit (ID‐Screen Brucellosis Serum Indirect Multispecies, ID VET, product code BRUS‐MS‐1014, Gabrels, France). The tests were performed according to the instructions of the manufacturer (ID‐VET, 2008). Before each i‐ELISA test, reagents and plasma samples were equilibrated at room temperature (22 ± 4°C) and 100 µl of diluted buffer was added to each well. Ten microlitres of positive control and equal volume of negative control provided by the manufacturer were introduced into two different wells of the plate and 10 µl of each plasma sample was introduced in the remaining wells. Each plate was sealed and homogenized. After incubation at room temperature for 45 min, each plate was washed three times with PBS‐Tween and 100 µl of multispecies horseradish peroxidase (HRP) conjugate was added to each well. Each plate was subsequently incubated for 30 min at room temperature and washed three times to eliminate the excess of conjugate. Thereafter, 100 µl of the substrate solution (tetramethylbenzidine in substrate buffer containing H2O2) was added to each well and the plate was incubated in the dark for 15 min at room temperature. The reaction was stopped by addition of 100 μl of 1 N hydrochloric acid (HCl). The optical density in each well was measured at 450 nm using a micro plate photometer (Bio Tek ELX800 absorbance reader). For each sample tested, its results were expressed as a percentage of optical density (%OD). This percentage OD (%OD) was calculated using the following formula:
where S, N and P are ODs of the sample, the negative and positive controls, respectively. Sample with a % OD ≥ 120% where considered positive.
2.5. Data analysis
Statistical analyses were carried out using the Statistical Package for Social Sciences (SPSS) for Windows® version 22.0 (SPSS Inc.). Kappa Cohen test was used to evaluate the concordance between RBPT and i‐ELISA tests. Chi‐squared test was used to compare the prevalence of Brucella antibodies between sampling areas and different animal species (pig, goat, sheep and dog) except cattle. The difference was considered significant if the p‐value was lower than .05.
For cattle where about 20% of animals of each herd was selected, the mixed‐effect model analysis was performed using the R package lme4. This model was performed only in cattle because they were the only animal species for which the sampling was done at the level of the herds. Pigs, goats, sheep or dogs were kept alone or by group of two or three animals in the sampled villages. For these analyses, the Bayesian Information Criterion (BIC) and log‐likelihood (logLik) for comparing models and assessing fit were considered. From these criteria; a significant fitting model was obtained when the variance of RBPT and i‐ELISA test were compared with a BIC and logLik. Results of this comparison were confirmed by analysing variance type III that was undertaken for both RBPT and i‐ELISA tests with Satterthwaite's method. The correlation was done with the analysis of variance.
3. RESULTS
3.1. Prevalence of Brucella antibodies in different domestic animals
A total of 1873 domestic animals containing 855 cattle, 452 goats, 373 sheep, 160 pigs and 33 dogs (Table 2) was investigated. The RBPT revealed 6.94% (130/1873) of animals with Brucella antibodies (Table 1). The prevalence of Brucella antibodies was 9.7% [95% CI: 9.6–16.4] in cattle, 9.4% [95% CI: 9.2–18.5] in sheep, 9.1% [95% CI: 2.6–18.1] in dogs, 1.87% [95% CI: 0.42–3.07] in pigs and 1.3% [95% CI: 0.48–2.90] in goats.
TABLE 2.
Prevalence of Bucella antibodies according to domestic animal species
| Animal species | Number of animals tested | Brucella infections | |||
|---|---|---|---|---|---|
| Number of animals positive for RBPT (%) | 95% CI | Number of animals positive for i‐ELISA (%) | 95% CI | ||
| Cattle | 855 | 83 (9.7) | 9.6–16.4 | 78 (9.12) | 8.9–14.3 |
| Sheep | 373 | 35 (9.4) | 9.2–18.5 | 30 (8.04) | 7.5–16.4 |
| Dog | 33 | 3 (9.1) | 2.6–18.1 | 2 (6.06) | 3.1–19.2 |
| Pig | 160 | 3 (1.87) | 0.42–3.07 | 3 (1.87) | 0.36–2.59 |
| Goat | 452 | 6 (1.3) | 0.48–2.90 | 5 (1.1) | 0.37–2.65 |
| Total | 1,873 | 130 (6.9) | 118(6.3) | ||
| X 2 | 39.42 | 33.63 | |||
| p value | <.0001* | <.0001* | |||
Abbreviations: CI, confidence interval; i‐ELISA, Indirect Enzyme‐linked immunosorbent assay; RBPT, Rose Bengal plate test.
Significant difference in the sero‐prevalence of Brucella antibodies.
TABLE 1.
Prevalence of Brucella antibodies according to sampling sites
| Sampling sites | Number of animal tested | Brucella antibodies | |||
|---|---|---|---|---|---|
| Number of animals positive for RBPT (%) | 95% CI | Number of animals positive for i‐ELISA (%) | 95% CI | ||
| Yoko | 348 | 35 (10.05) | 9.2–18.5 | 30 (8.6) | 7.7–16.3 |
| Noun | 1,070 | 85 (7.9) | 6.8–16.4 | 78 (7.2) | 6.9–14.3 |
| Campo | 54 | 3 (5.5) | 4.8–29.0 | 3 (5.5) | 3.1–29.2 |
| Bipindi | 118 | 5 (4.2) | 4.2–30.7 | 5 (4.2) | 3.6–23.6 |
| Fontem | 283 | 2 (0.7) | 0.16–4.81 | 2 (0.5) | 0.13–4.01 |
| Total | 1,873 | 130 (6.94) | 118 (6.3) | ||
| X 2 | 26.08 | 18,97 | |||
| p value | <.0001* | <.001* | |||
Abbreviations: CI, confidence interval; i‐ELISA, Indirect Enzyme‐linked immunosorbent assay; RBPT, Rose Bengal plate test.
Significant difference in the sero‐prevalence of Brucella antibodies.
The i‐ELISA revealed 6.35% (118/1873) of animals with Brucella antibodies (Table 1). The prevalence was estimated at 9.12% [95% CI: 8.9–14.3] in cattle, 8.04% [95% CI: 7.5–16.4] in sheep, 6.06% [95% CI: 3.1–19.2] in dogs, 1.87% [95% CI: 0.36–2.59] in pigs and 1.1% [95% CI: 0.37–2.65] in goats.
The overall prevalence of Brucella antibodies was 6.94% (130/1873) for RBPT against 6.35% (118/1873) for i‐ELISA. Although these two tests revealed a slight difference in the prevalence of Brucella antibodies, the statistical analysis comparing their performance revealed a high Kappa Cohen coefficient of 0.87 with a significant p value (p < .0001); indicating a good concordance between the two tests. For its higher specificity in comparison to RBPT, the prevalence of Brucella antibodies in the subsequent analyses will be based on data generated by i‐ELISA test.
3.2. Prevalence of Brucella antibodies according to sampling sites
In each location of the three agro‐ecological zones where this study was carried out, at least one animal was tested positive for the presence of Brucella antibodies. The highest prevalence of Brucella antibodies of 8.6% [95% CI 7.7–16.3] was found at Yoko followed by the Noun division with a prevalence of 7.2% [95% CI 6.9–14.3]. The lowest prevalence of 0.5% [95% CI 0.13–4.01] was observed in animals sampled in villages of Fontem in Southwest region (Table 1). Between different sampling sites, a significant difference (p = .001, x 2 = 18.97) was observed in the prevalence of Brucella antibodies (Table 1).
3.3. Prevalence of Brucella antibodies according to domestic animal species
Brucella antibodies were detected in at least one animal of each species that were investigated in this study (Table 2). Cattle, sheep and dog were reported with the highest prevalence of Brucella antibodies, while the lowest prevalence was observed in goats (Table 2). The prevalence of Brucella antibodies were 8.04% [95% CI: 7.5–16.] in sheep, 6.06% [95% CI: 3.1–19.2] in dog and 1.87% [95% CI: 0.36–2.59] in pigs. Between animal species, significant differences (p < .05, x 2 = 33.63) were observed in the prevalence of Brucella antibodies (Table 2).
3.4. Prevalence of Bucella antibodies according to intrinsic factors of animals
The prevalence of Brucella antibodies were 9.61% [95% CI: 7.0–13.3]) for Zebu Goudali, 11.48% [95% CI: 5.1–15.8] for Zebu Red Fulani and 7.21% [95% CI: 3.4–9.3] for Zebu White fulani (Table 3). Between cattle breeds, no significant difference (p = 0.78, x 2 = 0.49) was found in the prevalence of Brucella antibodies. However, a significant difference was observed (p = 0.03, x 2 = 1.25) in the prevalence of Brucella antibodies revealed by i‐ELISA test between female [9.94%; 95% CI: 6.5–11.1] and male [5.5%; 95% CI: 3.8–13.0] cattle. In other domestic animal species, no significant difference was observed between male and female (Table 3).
TABLE 3.
Prevalence of Bucella antibodies according to intrinsic factors of animals
| Animal species | Variable | Number of animals tested | Brucella infections | X 2 | p‐Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| RBPT positive (%) | 95% CI | i‐ELISA positive (%) | 95% CI | ||||||
| Cattle | Sex | Female | 694 | 69 (9.94) | 4.5–13.1 | 69 (9.94) | 6.5–11.1 | 1.25 | .03* |
| Male | 161 | 14 (8.69) | 4.1–11.2 | 9 (5.5) | 3.8–13.0 | ||||
| Breed | Goudali | 416 | 41 (9.8) | 6.9–14.3 | 40 (9.61) | 7.0–13.3 | 0.49 | .78 | |
| W. Fulani | 291 | 24 (8.24) | 3.1–8.3 | 21 (7.21) | 3.4–9.3 | — | — | ||
| R. Fulani | 148 | 18 (12.16) | 6.1–14.4 | 17 (11.48) | 5.1–15.8 | — | — | ||
| Age group | ≤4 years | 388 | 35 (9.02) | 5.6–14.6 | 31 (7.8) | 5.6–11.6 | 6.42 | .04* | |
| 5−8 years | 402 | 39 (9.7) | 4.6–13.5 | 36 (8.95) | 5.6–11.5 | — | — | ||
| ≥9 years | 65 | 9 (13.84) | 3.1–18.1 | 11 (16.92) | 4.3–22.1 | — | — | ||
| Sheep | Sex | Female | 302 | 26 (8.6) | 4.6–14.2 | 24 (7.94) | 4.8–11.4 | 0.02 | .8 |
| Male | 71 | 6 (8.45) | 3.0–13.4 | 6 (8.45) | 2.2–16.4 | — | — | ||
| Age group | <1 year | 29 | 3 (10.34) | 2.0–32.2 | 3 (10.34) | 2.1–30.2 | 0.3 | .5 | |
| >1 year | 344 | 32 (9.3) | 2.1–12.2 | 27 (7.84) | 4.7–10.7 | — | — | ||
| Goat | Sex | Female | 401 | 5 (1.24) | 0.0–2.7 | 4 (0.99) | 0.0–2.5 | 0.3 | .5 |
| Male | 51 | 1 (1.96) | 0.0–11.1 | 1 (1.96) | 0.0–10.9 | — | — | ||
| Age group | <1 year | 27 | 0 (0.00) | 0.0–9.2 | 0 (0.00) | 0.0–13.6 | 0.3 | .5 | |
| >1 year | 425 | 6 (1.4) | 0.0–1.9 | 5 (1.17) | 0.0–2.7 | — | — | ||
Abbreviations: CI, confidence interval; i‐ELISA, Indirect Enzyme‐linked immunosorbent assay; RBPT, Rose Bengal plate test.
Significant difference in the sero‐prevalence of Brucella antibodies
To see if the herd level may have a random effect or if there is a lack of independence in animals from the same herd, the mixed‐effect model analysis was done of data obtained from cattle. From this model, a significant fitting model was obtained when the variance of RBPT and i‐ELISA test were compared with a BIC and log‐likelihood (logLik) of‐886.5 and −154.08, a Chi‐squared test value of 68.4 and a p‐value of 2.2e‐16 with an intercept variance of 7.8e‐05 (CI: 0.001 ± 0.025) for the random effect on herd. These results were confirmed by variance type III analysis that revealed the statistical probability values as 2.2e‐16, F‐stat value of 2,657 and correlation of fixed effect of variance of −0.294. These results show that the herd factor has no real effect on the prevalence of Brucella antibodies in cattle. It is for this reason that the chi‐squared test was used above to compare the prevalence of Brucella antibodies between different sampling sites.
Between adult (≥9 years) [16.923%; 95% CI: 4.3%–22.1%] and young cattle (≤4 years) [7.8% 95%; CI: 5.6–13.3], a significant difference (p = .04, x 2 = 6.42) was found in the prevalence of Brucella antibodies (Table 3).
4. DISCUSSION
This study was designed to improve our knowledge on brucellosis by determining the prevalence of Brucella antibodies in domestic animals. The RBPT and i‐ELISA used here are the standard and common serological tests recommended for epidemiological study on brucellosis (Leuenberger et al., 2007). Although i‐ELISA showed higher specificity, the RBPT and i‐ELISA tests revealed a high KAPA value of 0.87 (K = 0.87); thus showing a good concordance between RBPT and i‐ELISA for the detection of Brucella antibodies. Our results are in line with those of Madut et al. (2018) who also observed a perfect concordance between these tests.
The significant differences (p < .0001, x 2 = 18.97) in the prevalence of Brucella antibodies between sampling sites could be explained by the variation of risk factors in various agro ecological zones. The higher prevalence of Brucella antibodies in animals of Yoko (agro ecological zone V) and Noun (agro ecological zone III) could be explained by the environmental conditions that are more favourable for the breeding and mixing of animals from different herds. Indeed, herd size, movement and congregation of animals for access to pastures, water or marketing figure among the well‐known risk factors of brucellosis (Berhe, Belihu, & Asfaw, 2007; Kadohira, McDermott, Shoukri, & Kyule, 1997; Megersa, Biffa, Abunna, et al., 2011; Megersa, Biffa, Niguse, et al., 2011; Mekonnen, Shewit, & Kyule, 2010; Muma, Samui, Oloya, Munyeme, & Skjerve, 2007; Sanogo et al., 2012). In the Noun division, the presence of many water streams, rivers (Noun, Mapé, Nshi, Mfû and Chiémbùh) and dams offer, especially during the dry season where water points are scarce, favourable breeding conditions that induce migration of pastoralists and their animals. This creates conditions that increase the transmission risk of Brucella between animals of different herds. This hypothesis is in line with observations of Khuzaima et al. (2018) reporting that when animals of different herds share temporally the same pasture zone or water point, the chance of transmission of brucellosis from infected to uninfected herds increases.
At Yoko where environmental conditions are also favourable for animal breeding, the transhumance phenomenon occurring there create favourable conditions for Brucella transmission due to mix up of animals from other herds or regions of Cameroon and neighbouring countries like the Central African Republic. This is in line with observations of Awah‐Ndukum, Mouiche, Bayang, et al. (2018) reporting that the mixing of large numbers of animals, the movement of animals in search of pasture, the sharing of grazing areas with wildlife, the concentration of animals around water points and the contact with other infected animals are risk factors for brucellosis spread. Sharing the same environment constitutes therefore a risk factor for Brucella infections and can facilitate the dissemination of brucellosis (Kaindi et al., 2012; Shimeles & Andualem, 2018).
Although the domestic animal species analysed in this study have shown susceptibilities to Brucella infections, significant differences (p < .0001, x 2 = 33.63) was observed in the prevalence of Brucella antibodies between different animal species. The low prevalence of Brucella antibodies in goat and pig could be explained by their large‐scale slaughtering for meat consumption; phenomenon that reduce the number of infected animals. Another reason will be the involvement of these animals in the intensive production systems in which they are not often in contact with infected animals or contaminated products (Kaindi et al., 2012).
It is well‐established that the dominance and overlapping nature of the C epitope of smooth brucellae (Alonso‐Urmeneta et al., 1998) makes it impossible to ascertain the infecting Brucella species using serological methods, irrespective of the antigen (melitensis or abortus) or host species tested (Ariza, 1999; OIE, 2013a, 2013b; Spink, 1956). Nevertheless, the presence of Brucella antibodies highlights contact with at least one Brucella species. The low prevalence (1.87%) of Brucella antibodies in pig is in line with previous results (Cadmus, Ijagbone, Oputa, Adesokan, & Stack, 2006; Nwanta et al., 2011; Onunkwo et al., 2011; Stafford, Tafford, Paton, & Gamble, 1992). In Nigeria for instance, the prevalence of porcine brucellosis was 0.6% (Nwanta et al., 2011; Onunkwo et al., 2011) while, in Uganda and Zambia, it was reported to be 0% (Cadmus et al., 2006; Stafford et al., 1992). Considering pig as the main host for B. suis, it is likely that this Brucella species is not highly prevalent in the sampling villages. Pig breeding could be probably not too affected by brucellosis and, like in other African countries, B. suis infections seem of little epidemiological importance.
Our results showing Brucella antibodies in dogs are the first ones reporting the possibility of dog brucellosis in Cameroon. If we consider dog as the main host of B. canis, our results would be in line with those of Gous et al. (2005) who reported B. canis in two dogs sampled in South Africa. Further investigations on B. canis are required to confirm this hypothesis. The probability for dogs to be infected by Brucella could be explained by the fact that in rural areas of most African countries where dogs are kept for many years by inhabitants for different purposes like hunting activities, these animals are in contact with wild animals. They have therefore, the possibility to become infected from wild animals that carry Brucella infections (Cross et al., 2018; Mick et al., 2014; Mohandoss et al., 2012).
Our results showing 9.12% of cattle with Brucella antibodies are in line with 8.4% reported one decade ago in the Northwest Region of Cameroon (Bayemi et al., 2009). They are lower than 31% reported in South Sudan (Madut et al., 2018), but higher than 6.8% found in Tanzania (Assenga, Matemba, Muller, Malakalinga, & Kazwala, 2015). These differences could be related to variations in the cattle management systems as previously reported elsewhere (Bayemi et al., 2015; Kaindi et al., 2012). In central Africa, most studies on brucellosis used serological tests and consequently, information related to Brucella species that infect cattle and small ruminants remains unknown. From data generated on bovine brucellosis in other parts of sub‐Saharan Africa, it is likely that most cattle found with Brucella antibodies have been in contact with B. abortus, the most commonly species that have been isolated and characterized in cattle from sub‐Saharan countries (Ducrotoy et al., 2017). However, it is important to point out that cattle and small ruminants share the same environment in most of our sampling sites. In such context, the transmission of different Brucella species can occur between cattle and small ruminants. Taking into consideration this probability, it is likely that some cattle found with Brucella antibodies have been in contact with B. melitensis. This hypothesis is in agreement with previous observations reporting the transmission of B. melitensis to cattle in countries where cattle and small ruminants are kept together (Benkirane, 2006; Refai, 2002). Indeed, the presence of larger herds and mixed crop‐livestock production system (cattle, goat and sheep) favours inter and intra‐species transmission of Brucella (Ariza et al., 2007; Mohamed et al., 2018).
The prevalence of Brucella antibodies in small ruminants (goats and sheep) are in line with 1.6% and 1.2% reported in Tanzania (Assenga et al., 2015) and Bangladesh (Rahman et al., 2011, 2013), but lower than the 11.4% and 5.3%, respectively reported in Sudan (Mohamed et al., 2018) and Ethiopia (Tadesse, 2016). These differences may result from the variations of risk factors such as the nomadic movements, the use of communal grazing lands and watering points for animals (Kaindi et al., 2012; Khuzaima et al., 2018). Compared to goats (1.1%), the higher prevalence of Brucella antibodies in sheep (8.04%) may be due to the larger herd sizes of sheep in the studied areas. Most small ruminants found with Brucella antibodies have been probably in contact with B. melitensis because, in most sub‐Saharan countries, this bacterial species have been reported as the most prevalent in these animals. However, we could not rule out the fact that B. abortus can be also found in small ruminants because it has been isolated several times from milk and abortion products of sheep and goat (Bertu et al., 2015; Okoh, 1980). Searching also for B. ovis, a non‐zoonotic species restricted to sheep, will be interesting because it has been reported to exist in several sub‐Saharan countries (Ate, Bello, Nenshi, Allam, & Rashidat, 2011; Cameron, Carles, & Lauerman, 1971; De Wet & Erasmus, 1984; Van Rensburg, Heerden, Roux, Snyders, & Heerden, 1958).
The proportion of female cattle (9.65%) with Brucella antibodies was significantly higher (p = .03, x 2 = 1.25) than male. Moreover significantly higher (p = .04, x 2 = 6.42) prevalence of Brucella antibodies was found in adult compared to young animals. These results are in agreement with those obtained in Tanzania and Pakistan (Gul, Khan, Rizvi, & Hussain, 2014; Shafee et al., 2012). These differences may result from the fact that females are kept longer in the herd for reproduction and therefore, are more exposed to infections than males (Dinka & Chala, 2009; Solorio‐Rivera, Segura‐Correa, & Sanchez‐Gil, 2007).
The main limitations of this study rely on the fact that no Brucella species was identified or isolated and therefore, the bacterial species circulating in different agro‐ecological zones remain unknown. However, hot spot villages were identified for subsequent investigations on brucellosis. Understanding the transmission dynamics within and between villages and between different animal species could enable to efficiently plan control operations against brucellosis. Data on this transmission could help to identify areas presenting high risk where investigations on human brucellosis could be undertaken for the overarching objective of designing efficient control programme for this neglected zoonotic disease.
5. CONCLUSION
The findings of this study have shown that the prevalence of Brucella antibodies varies between animal species and localities. Our results indicate that brucellosis can affect a variety of domestic animals from different regions of Cameroon. These results could help to identify villages where investigations on the transmission dynamic should be focused in order to improve animal health and boost peasant economy. Investigations aiming to determine the prevalence of human brucellosis and to identify Brucella genotypes could help to better understand the transmission dynamics of Brucella.
CONFLICT OF INTEREST
The authors of this manuscript declare that they have no competing interests concerning this research.
AUTHOR CONTRIBUTIONS
Rolin M. N. Kamga: contributed to conceptualization, formal analysis, methodology and writing‐original draft. Barberine A. Silatsa: contributed to conceptualization, investigation, methodology and writing‐original draft. Oumarou Farikou: contributed to data curation, investigation and methodology. Jules‐Roger Kuiate: contributed to conceptualization and supervision. Gustave Simo: contributed to conceptualization, funding acquisition, methodology, project administration, supervision and Writing‐review & editing.
ETHICS STATEMENT
The protocol of this study was approved by the divisional delegation of the Ministry of livestock, fisheries and animals Industries of Cameroon with the reference number Ref N°015/16/L/DDEPIA.NN. The local administrative and traditional authorities of each sampling site were also informed and gave their approval. Subsequently, the review board of the molecular parasitology and entomology subunit of the Department of Biochemistry of the Faculty of Science of the University of Dschang gave its approval. Verbal consent was obtained from each owner after providing detailed explanation of the aim and objective of the study.
ACKNOWLEDGEMENTS
The authors thank the support of inhabitants of different localities as well as the staff of different divisional delegations of the Ministry of livestock, fisheries and animals Industries of Cameroon. The authors also thank the anonymous reviewers for helpful comments on the manuscript.
Kamga RMN, Silatsa BA, Farikou O, Kuiate J‐R, Simo G. Detection of Brucella antibodies in domestic animals of southern Cameroon: Implications for the control of brucellosis. Vet Med Sci. 2020;6:410–420. 10.1002/vms3.264
The peer review history for this article is available at https://publons.com/publon/10.1002/vms3.264
Funding information
This work was supported by the University of Dschang of Cameroon through the Molecular Parasitology and Entomology subunit of the Faculty of Science.
DATA AVAILABILITY STATEMENT
All data generated and/or analysed are included in this article.
REFERENCES
- Abbasi, T. , Abbasi, T. , & Abbasi, S. A. (2016). Reducing the global environmental impact of livestock production: The mini livestock option. Journal of Cleaner Production, 112, 1754–1766. 10.1016/j.jclepro.2015.02.094 [DOI] [Google Scholar]
- Alonso‐Urmeneta, B. , Marin, C. M. , Aragon, V. , Blasco, J. M. , Díaz, R. , & Moriyón, I. (1998). Evaluation of lipopolysaccharides and polysaccharides of different epitopic structures in the indirect enzyme‐linked immunosorbent assay for diagnosis of brucellosis in small ruminants and cattle. Clinical and Diagnostic Laboratory Immunology, 5, 749–754. 10.1128/CDLI.5.6.749-754.1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alton, G. G. , Jones, L. M. , Angus, R. D. , & Verger, J. M. (1988). Technics for the brucellosis laboratory, Institut National de la Recherche Agronomique, Paris. 10.12691/ajidm-4-5-1 [DOI]
- Ariza, J. (1999). Brucellosis: An update: The perspective from the Mediterranean basin. Review of Medical Microbiology, 10, 125–135. [Google Scholar]
- Ariza, J. , Bosilkovski, M. , Cascio, A. , Colmenero, J. D. , Corbel, M. J. , Falagas, M. E. , … Pappas, G. (2007). Perspectives for the treatment of brucellosis in the 21st century: TheIoannina recommendations. PLoS Medicine, 4, e317 10.1371/journal.pmed.0040317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asgedom, H. , Damena, D. , & Duguma, R. (2016). Seroprevalence of Bovine Brucellosis and associated risk factors in and around alage district, Ethiopia. Springer Plus, 5(1), 851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assenga, J. A. , Matemba, L. E. , Muller, S. K. , Malakalinga, J. J. , & Kazwala, R. R. (2015). Epidemiology of Brucella infection in the human, livestock and wildlife interface in the Katavi‐Rukwa ecosystem, Tanzania. BMC Veterinary Research, 11(1), 1–11. 10.1186/s12917-015-0504-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ate, I. U. , Bello, A. , Nenshi, P. M. , Allam, L. , & Rashidat, M. (2011). Foetal maceration associated with Brucella ovis infection in a Yankassa ewe. Revista Electrónica De Veterinaria, 12, 1–6. [Google Scholar]
- Awah‐Ndukum, J. , Mouiche, M. M. , Bayang, H. N. , Ngu Ngwa, V. , Assana, E. , Feussom, K. J. M. , … Zoli, P. A. (2018). Seroprevalence and associated risk factors of brucellosis among indigenous cattle in the Adamawa and North Regions of Cameroon. Veterinary Medicine International, 2018, 1–10. 10.1155/2018/3468596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awah‐Ndukum, J. , Mouiche, M. M. M. , Kouonmo‐Ngnoyum, L. , Bayang, H. N. , Manchang, T. K. , Poueme, R. S. N. , … Zoli, A. P. (2018). Seroprevalence and risk factors of brucellosis among slaughtered indigenous cattle, abattoir personnel and pregnant women in Ngaoundéré, Cameroon. BMC Infectious Diseases, 18(1), 611 10.1186/s12879-018-3522-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayayi, J. A. , Têko‐Agbo, A. , & Koné, P. (2009). The impact of brucellosis on the economy and public health in Africa Inter‐State School of Veterinary Sciences and Medicine1 Conf. OIE (pp.85–98).
- Aznar, M. N. , Linares, F. J. , Cosentino, B. , Sago, A. , La Sala, L. , León, E. , … Perez, A. (2015). Prevalence and spatial distribution of bovine brucellosis in San Luis and La Pampa, Argentina. BMC Veterinary Research, 11(1), 1–7. 10.1186/s12917-015-0535-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayemi, P. H. , Mah, G. D. , Ndamukong, K. , Nsongka, V. M. , Leinyuy, I. , Unger, H. , … Luogbou, N. D. (2015). Bovine brucellosis in cattle production systems in the Western Highlands of Cameroon. International Journal of Animal Biology, 1(2), 38–44. Retrieved from http://www.publicscienceframework.org/journal/ijab [Google Scholar]
- Bayemi, P. H. , Webb, E. C. , Nsongka, M. V. , Unger, H. , & Njakoi, H. (2009). Prevalence of Brucella abortus antibodies in serum of Holstein cattle in Cameroon. Tropical Animal Health and Production, 41, 141–144. 10.1007/s11250-008-9184-8 [DOI] [PubMed] [Google Scholar]
- Benkirane, A. (2006). Ovine and caprine brucellosis: World distribution and control/eradication strategies in West Asia/North Africa region. Small Ruminant Research, 62(19), 25 10.1016/j.smallrumres.2005.07.032 [DOI] [Google Scholar]
- Berhe, G. , Belihu, K. , & Asfaw, Y. (2007). Seroepidemiological investigation of bovine brucellosis in the extensive cattle production system of Tigray region of Ethiopia. The International Journal of Applied Research in Veterinary Medicine, 5, 65–71. [Google Scholar]
- Bertu, W. J. , Ducrotoy, M. J. , Munoz, P. M. , Mick, V. , Zuniga Ripa, A. , Bryssinckx, W. , … Ocholi, R. A. (2015). Phenotypic and genotypic characterization of Brucella strains isolated from autochthonous livestock reveals the dominance of B. abortus biovar 3a in Nigeria. Veterinary Microbiology, 180, 103–108. 10.1016/j.vetmic.2015.08.014 [DOI] [PubMed] [Google Scholar]
- Cadmus, S. I. B. , Ijagbone, I. F. , Oputa, H. E. , Adesokan, H. K. , & Stack, J. A. (2006). Serological survey of brucellosis in livestock animals and workers in Ibadan, Nigeria. African Journal of Biomedical Research, 9, 163–168. [Google Scholar]
- Cameron, R. D. , Carles, A. B. , & Lauerman, L. H. J. (1971). The incidence of Brucella ovis in some Kenya flocks and its relationship to clinical lesions and semen quality. Veterinary Record, 89, 552–557. 10.1136/vr.89.21.552 [DOI] [PubMed] [Google Scholar]
- Corbel, M. J. (1997). Brucellosis: An overview. Emerging Infectious Diseases, 3, 213–221. 10.3201/eid0302.970219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross, A. R. , Baldwin, V. M. , Roy, S. , Essex‐Lopresti, A. E. , Prior, J. L. , & Harmer, N. J. (2018). Zoonoses under our noses. Microbes and Infection, 21, 10–19. 10.1016/j.micinf.2018.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Wet, J. A. , & Erasmus, J. A. (1984). Epididymitis of rams in the central and southern districts of the Orange Free State. Journal of the South African Veterinary Association, 55, 173–179. [PubMed] [Google Scholar]
- Dean, A. S. , Crump, L. , Greter, H. , Schelling, E. , & Zinsstag, J. (2012). Global burden of human brucellosis: A systematic review of disease frequency. PLoS Neglected Tropical Diseases, 6(10), e1865 10.1371/journal.pntd.0001865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinka, H. , & Chala, R. (2009). Sero‐prevalence study of bovine brucellosis in Pastoral and Agro‐Pastoral Areas of East Showa Zone, Oromia Regional State, Ethiopia. American Eurasian Journal Agricultural Environmental Sciences, 6(5), 508–512. [Google Scholar]
- Ducrotoy, M. , Bertu, W. J. , Matope, G. , Cadmus, S. , Conde‐Álvarez, R. , Gusi, A. M. , … Moriyón, I. (2017). Brucellosis in Sub‐Saharan Africa: Current challenges for management, diagnosis and control. Acta Tropica, 165, 179–193. 10.1016/j.actatropica.2015.10.023 [DOI] [PubMed] [Google Scholar]
- Fyumagwa, R. D. , Wambura, P. N. , Mellau, L. S. B. , & Hoare, R. (2009). Sero‐prevalence of Brucella abortus in buffaloes and wildebeests in the Serengeti ecosystem: A threat to humans and domestic ruminants. Tanzania Veterinary Journal, 26(2), 62–67. 10.4314/tvj.v26i2.53803 [DOI] [Google Scholar]
- Gous, T. A. , van Rensburg, W. J. , Gray, M. , Perrett, L. L. , Brew, S. D. , Young, E. J. , … Picard, J. (2005). Brucella canis in South Africa. The Veterinary Record, 157(21), 668 10.1136/vr.157.21.668 [DOI] [PubMed] [Google Scholar]
- Gul, S. T. , Khan, A. , Rizvi, F. , & Hussain, I. (2014). Sero‐prevalence of brucellosis in food animals in the Punjab, Pakistan. Pakistan Veterinary Journal, 34, 454–458. [Google Scholar]
- Havelaar, A. H. , Kirk, M. D. , Torgerson, P. R. , Gibb, H. J. , Hald, T. , Lake, R. J. , … Devleesschauwer, B. (2015). World Health Organization global estimates and regional comparisons of the burden of food‐borne disease in 2010. PLoS Medicine, 12(12), e1001923 10.1371/journal.pmed.1001923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadohira, M. , McDermott, J. J. , Shoukri, M. M. , & Kyule, M. N. (1997). Variations in the prevalence of antibody to Brucella infection in cattle by farm, area and district in Kenya. Epidemiology and Infection, 118, 35–41. 10.1017/s0950268896007005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaindi, D. W. , Schelling, E. , Wangoh, J. M. , Imungi, J. K. , Farah, Z. , & Meile, L. (2012). Risk factors for symptoms of gastrointestinal illness in rural town Isiolo, Kenya. Zoonoses and Public Health, 59(2), 118–125. 10.1111/j.1863-2378.2011.01425.x [DOI] [PubMed] [Google Scholar]
- Kelly, R. F. , Hamman, S. M. , Morgan, K. L. , Nkongho, E. F. , Ngwa, V. N. , Tanya, V. , … Bronsvoort, B. M. D. C. (2016). Knowledge of bovine tuberculosis, cattle husbandry and dairy practices amongst pastoralists and small‐scale dairy farmers in Cameroon. PLoS ONE, 11(1), e0146538 10.1371/journal.pone.0146538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khuzaima, B. A. , Hatim, H. I. , Shuaib, Y. A. , Mohamed Noor, S. E. , Elgadal, A. A. , Shigidi, M. T. , & Nimir, A. H. (2018). Sero‐prevalence of anti‐brucella antibodies in goats in El‐Gedarif state, Eastern Sudan. Journal of Animal Veterinary Science, 4, 1–8. 10.14202/vetworld.2018.511-518 [DOI] [Google Scholar]
- Ladbury, G. , Allan, K. J. , Cleaveland, S. , Davis, A. , De Glanville, W. A. , Forde, T. L. , … Zadoks, R. N. (2017). One health research in Northern Tanzania–challenges and progress. East African Health Research Journal, 1(1), 8–18. 10.24248/EAHRJ-D-16-00379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leuenberger, R. , Boujon, P. , Thür, B. , Miserez, R. , GarinBastuji, B. , Rüfenacht, J. , & Stärk, K. D. (2007). Prevalence of classical swine fever, Aujeszky’s disease and brucellosis in a population of wild boar in Switzerland. Veterinary Record, 160, 362–368. 10.1136/vr.160.11.362 [DOI] [PubMed] [Google Scholar]
- Madut, N. A. , Muwonge, A. , Nasinyama, G. W. , Muma, J. B. , Godfroid, J. , Jubara, A. S. , … Kankya, C. (2018). The sero‐prevalence of brucellosis in cattle and their herders in Bahrel Ghazal region, South Sudan. Plos Neglected Tropical Diseases, 12(6), e0006456 10.1371/journal.pntd.0006456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangen, M. J. , Otte, J. , Pfeiffer, D. , & Chilonda, P. (2002). Bovine brucellosis in Sub‐Saharan Africa: Estimation of sero‐prevalence and impact on meat and milk offtake potential. Rome, Italy: Food and Agriculture Organisation of the United nations. [Google Scholar]
- Mazeri, S. , Scolamacchia, F. , Handel, I. G. , Morgan, K. L. , Tanya, V. N. , & Bronsvoort, B. M. D. C. (2013). Risk factor analysis for antibodies to Brucella, Leptospira and C. burnetii among cattle in the Adamawa Region of Cameroon: A cross‐sectional study. Tropical Animal Health and Production, 45, 617–623. 10.1007/s11250-012-0268-0 [DOI] [PubMed] [Google Scholar]
- Megersa, B. , Biffa, D. , Abunna, F. , Regassa, A. , Godfroid, J. , & Skjerve, E. (2011). Seroprevalence of brucellosis and its contribution to abortion in cattle, camel, and goat kept under pastoral management in Borana, Ethiopia. Tropical Animal Health and Production, 43, 651–656. 10.1007/s11250-010-9748-2 [DOI] [PubMed] [Google Scholar]
- Megersa, B. , Biffa, D. , Niguse, F. , Rufael, T. , Asmare, K. , & Skjerve, E. (2011). Cattle brucellosis in traditional livestock husbandry practice in Southern and Eastern Ethiopia, and its zoonotic implication. Acta Veterinaria Scandinavica, 53, 24 10.1186/1751-0147-53-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mekonnen, H. , Shewit, K. , & Kyule, M. (2010). Serological survey of bovine brucellosis in barka and arado breeds (Bosindicus) of western Tigray, Ethiopia. Preventive Veterinary Medicine, 9(4), 28–35. 10.1016/j.prevetmed.2009.12.001 [DOI] [PubMed] [Google Scholar]
- Mick, V. , Le Carrou, G. , Corde, Y. , Game, Y. , Jay, M. , & Garin‐Bastuji, B. (2014). Brucella melitensis in France: Persistence in wildlife and probable spillover from Alpine ibex to domestic animals. PLoS ONE, 9, e94168 10.1186/s13690-017-0207-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohamed, E. M. , Mohamed, E. A. A. , El‐Sanousi, E. M. , Ibrahaem, H. H. , Mohamed‐Noor, S. E. , Abdalla, M. A. , & Shuaib, Y. A. (2018). Seroprevalence and risk factors of caprine brucellosis in Khartoum state, Sudan. Veterinary World, 11(4), 511–518. 10.14202/vetworld.2018.511-518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motta, P. , Porphyre, T. , Hamman, S. M. , Morgan, K. L. , Ngwa, V. N. , Tanya, V. N. , … Bronsvoort, B. M. (2018). Cattle transhumance and agropastoral nomadic herding practices in Central Cameroon. BMC Veterinary Research, 14(1), 214 10.1186/s12917-018-1515-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muma, J. B. , Samui, K. L. , Oloya, J. , Munyeme, M. , & Skjerve, E. (2007). Risk factors for brucellosis in indigenous cattle reared in livestock‐wildlife interface areas of Zambia. Preventive Veterinary Medicine, 80, 306–317. 10.1016/j.prevetmed.2007.03.003 [DOI] [PubMed] [Google Scholar]
- Nagalingam, M. , Shome, R. , Balamurugan, V. , Shome, B. R. , NarayanaRao, K. , Vivekananda, … Prabhudas, K. (2012). Molecular typing of Brucella species isolates from livestock and human. Tropical Animal Health and Production, 44(1), 5–9. 10.1007/s11250-011-9886-1 [DOI] [PubMed] [Google Scholar]
- Nielsen, K. , & Yu, W. L. (2010). Serological diagnosis of brucellosis. Prilozi, 31(1), 65–89. [PubMed] [Google Scholar]
- Nimpaye, H. , Njiokou, F. , Njine, T. , Njitchouang, G. R. , Cuny, G. , Herder, S. , … Simo, G. (2011). Trypanosome vivax, T. congolence forest type and T. simiae: Prevalence in domestic animals of sleeping sickness foci of Cameroon. Parasite, 18, 171–179. 10.1051/parasite/2011182171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Njiokou, F. , Nimpaye, H. , Simo, G. , Njitchouang, G. R. , Asonganyi, T. , Cuny, G. , & Herder, S. (2010). Domestic animals as potential reservoir hosts of Trypanosoma brucei gambiense in sleeping sickness foci in Cameroon. Parasite, 17, 61–66. 10.1051/parasite/2010171061 [DOI] [PubMed] [Google Scholar]
- Nwanta, J. A. , Shoyinka, S. V. O. , Chah, K. F. , Onunkwo, J. I. , Onyenwe, I. W. , Eze, J. I. , … Oladimeji, K. T. (2011). Production characteristics, disease prevalence, and herdhealth management of pigs in Southeast Nigeria. Journal of Swine Health and Production, 19(6), 331–339. [Google Scholar]
- OIE . (2013a). Bovine brucellosis. In Manual of Diagnostic Tests and Vaccines for Terrestrial Animals (pp. 1–35).
- OIE . (2013b). Caprine and ovine brucellosis (excluding Brucella ovis). In Manual of Diagnostic Tests and Vaccines for Terrestrial Animals (pp. 1–10).
- Okoh, A. E. (1980). An investigation of abortion in sheep in Rano L.I.B.C. near Kano, Nigeria. Bulletin of Animal Health and Production in Africa, 28, 135–138. [PubMed] [Google Scholar]
- Onunkwo, J. I. , Njoga, E. O. , Nwanta, J. A. , Shoyinka, S. V. O. , Onyenwe, I. W. , & Eze, J. I. (2011). Serological survey of porcine brucella infection in South East, Nigeria. Nigerian Veterinary Journal, 32(1), 60–62. [Google Scholar]
- Rahman, A. K. M. , Saegerman, C. , Berkvens, D. , Fretin, D. , Gani, M. O. , Ershaduzzaman, M. , … Emmanuel, A. (2013). Bayesian estimation of true prevalence, sensitivity and specificity of indirect ELISA, Rose Bengal Test and Slow Agglutination Test for the diagnosis of brucellosis in sheep and goats in Bangladesh. Preventive Veterinary Medicine, 110, 242–252. 10.1016/j.prevetmed.2012.11.029 [DOI] [PubMed] [Google Scholar]
- Rahman, M. S. , Faruk, M. O. , Her, M. , Kim, J. Y. , Kang, S. I. , & Jung, S. C. (2011). Prevalence of brucellosis in ruminants in Bangladesh. Veterinary Medicine, 56, 379–385. 10.17221/1555-VETMED [DOI] [Google Scholar]
- Refai, M. (2002). Incidence and control of brucellosis in the Near East region. Veterinary Microbiology, 90, 81–110. 10.1016/S0378-1135(02)00248-1 [DOI] [PubMed] [Google Scholar]
- Sanogo, M. , Abatih, E. , Thys, E. , Fretin, D. , Berkvens, D. , & Saegerman, C. (2012). Risk factors associated with brucellosis seropositivity among cattle in the central savannah‐forest area of Ivory Coast. Preventive Veterinary Medicine, 107, 51–56. 10.1016/j.prevetmed.2012.05.010 [DOI] [PubMed] [Google Scholar]
- Scolamacchia, F. , Handell, I. G. , Fèvre, E. M. , Morgan, K. L. , Tanya, V. N. , & Bronsvoort, B. M. D. C. (2010). Serological patterns of brucellosis, leptospirosis and Q fever in Bos indicus cattle in Cameroon. PLoS ONE, 5(1), e8623 10.1371/journal.pone.0008623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ID‐VET . (2008). ID Screen Brucellosis Serum Indirect Multi‐species factsheet (pp. 1–6). France: ID‐VET. [Google Scholar]
- Seignobos, C. (2008). La Question mbororo. Réfugiés de la RCA au Cameroun, Yaoundé/Paris (HCR/SCAC/IRD).
- Shafee, M. , Rabbani, M. , Ahmad, M. U. D. , Muhammad, K. , Sheikh, A. A. , & Awan, M. A. (2012). Sero‐prevalence of bovine brucellosis using indirect ELISA in Quetta Balochistan, Pakistan. Journal of Animal and Plant Science Plant, 22(3), 125–127. [Google Scholar]
- Shimeles, A. A. , & Andualem, Y. D. (2018). Comparative seroepidemiological study of brucellosis in sheep under smallholder farming and governmental breeding ranches of Central and North East Ethiopia. Journal of Veterinary Medicine Article, 2018(7239156), 12 10.1155/2018/7239156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibhatu, K. T. , Krishna, V. V. , & Qaim, M. (2015). Farm production diversity and dietary diversity in developing countries. Proceedings of the National Academy of Sciences, 112, 10657–10662. 10.1073/pnas.1510982112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silatsa, A. B. , Kuiate, J. R. , Njiokou, F. , Simo, G. , Feussom, J. M. K. , Tunrayo, A. , … Pelle, R. (2019). A countrywide molecular survey leads to a seminal identification of the invasive cattle tick Rhipicephalus (Boophilus) microplus in Cameroon, a decade after it was reported in Cote d’Ivoire. Ticks and Tick‐borne Diseases, 10(3), 585–593. 10.1016/j.ttbdis.2019.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solorio‐Rivera, J. L. , Segura‐Correa, J. C. , & Sanchez‐Gil, L. G. (2007). Seroprevalence and risk factors for brucellosis of goats in herds of Michoacan Mexico. Preventive Veterinary Medicine, 82, 282–290. 10.1016/j.prevetmed.2007.05.024 [DOI] [PubMed] [Google Scholar]
- Spink, W. W. (1956). The diagnosis of human brucellosis The nature of brucellosis (pp. 191–215). Minneapolis, MN: The University of Minnesota Press. [Google Scholar]
- Stafford, K. , Tafford, Y. , Paton, D. , & Gamble, P. (1992). Antibodies to some swine disease in commercial piggeries in Central Zambia. Revue D‘élevage Et De Médecine Vétérinaire Des Pays Tropicaux, 45(34), 229–230. [PubMed] [Google Scholar]
- Tadesse, G. (2016). Brucellosis seropositivity in animals and humans in Ethiopia: A meta‐analysis. Plos Neglected Tropical Diseases, 10(10), e0005006 10.1371/journal.pntd.0005006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrusfield, M. (2007). Veterinary epidemiology (Vol. 610, p. 610). Oxford, UK: Blackwell Science Ltd, a Blackwell. [Google Scholar]
- Van Rensburg, S. W. , Van Heerden, K. M. , Le Roux, D. J. , Snyders, A. J. , & Van Heerden, K. M. (1958). Infectious infertility in sheep. Journal of the South African Veterinary Association, 29, 223–233. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated and/or analysed are included in this article.


