Dear Editor:
We read with great interest the letter by Rotzinger et al. [1], discussing the role of chest computed tomography (CT) in the management of COVID-19 pneumonia.
They comment that CT has become a cornerstone in both the diagnostic workup and follow-up of COVID-19 pneumonia and highlight the incidence of acute pulmonary embolism in patients diagnosed with COVID-19. They also comment that CT is usually performed without intravenous contrast agent injection, and in patients with elevated D-dimer levels on admission or sudden clinical worsening, CT pulmonary angiography should be considered since pulmonary embolism is a life-threatening but potentially treatable condition [1].
The predominant CT findings of Covid-19 pneumonia are multifocal, bilateral ground-glass opacities, with or without the crazy-paving pattern, and/or consolidation. Another tomographycal finding recently related to Covid-19 pneumonia is the reversed halo sign (RHS).
The reversed halo sign (RHS) has gained prominence recently as a tomographic sign observed in patients with COVID-19 pneumonia (Fig. 1 ). The Radiological Society of North America, Society of Thoracic Radiology, and American College of Radiology recently published an Expert Consensus Statement on the reporting of COVID-19–related CT findings [2], with the aim of helping radiologists recognize findings potentially attributable to COVID-19 pneumonia. In this statement, the RHS is characterized as a typical feature of the infection, that is, a commonly reported imaging finding of greater specificity for COVID-19 pneumonia.
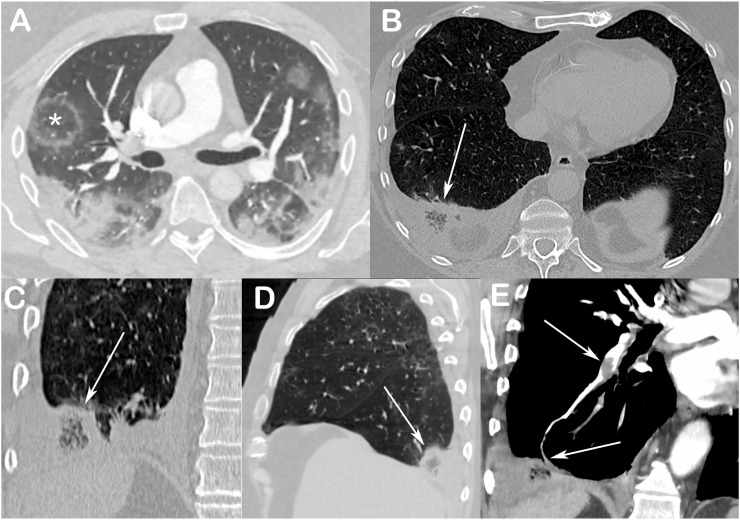
Fig. 1.
(A) Enhanced axial chest CT image of a 48-year-old man with confirmed COVID-19 pneumonia, showing bilateral consolidations and ground-glass opacities, and a reversed halo sign (asterisk) in the right lung. Reconstructed axial (B), coronal (C), and sagittal (D) chest CT images of a 54-year-old man with confirmed COVID-19 pneumonia show a reversed halo sign in the basal posterior segment of the right lung, with internal reticulation (arrows); pulmonary CT angiography (E) showed emboli in arterial branches of the basal posterior segment of the right lower lobe (arrow).
The tomographic presentation of the RHS in most patients with COVID-19 is the same as that of the RHS secondary to organizing pneumonia: a focal, rounded area of ground-glass opacity surrounded by a nearly complete ring of consolidation. This similarity can be explained easily, as the organization of diffuse alveolar damage is the most likely mechanism of RHS appearance in patients with COVID-19. Histopathological reports have demonstrated the presence of organizing pneumonia in patients with COVID-19, with the RHS appearing at later stages, after symptom onset [3]. Bernstein et al. [3] found that the RHS was absent in the early phase of COVID-19 and appeared in the late phase, and hypothesized that the frequency of certain findings depended on the time course of infection.
A review of the pathophysiology of lung injury is important to gain an understanding of RHS formation in patients with COVID-19. The few published studies addressing the histopathological aspects of COVID-19 have revealed the basic evolution of initial lesions (diffuse alveolar damage) to an early stage of organization [[4], [5], [6]]. After the first week, the organizing phase of diffuse alveolar damage predominates, and is characterized by organizing fibroblastic tissue and fibrosis. The term “organizing pneumonia” is used to describe a histological pattern that is a nonspecific response to lung injury, namely the organization of fibroblastic tissue plugs composed of spindle-shaped cells in a pale-staining matrix [4]. Zhang et al. [6] described the histopathological findings of a lung biopsy performed postmortem in a patient who died 3 weeks after being diagnosed with COVID-19. The study revealed diffuse alveolar damage in the organizing phase. The authors noted the presence of loose intra-alveolar fibrous plugs of organizing pneumonia, with intra-alveolar organizing fibrin at most foci [6]. These findings suggest that COVID-19, like other viral infections [e.g., influenza A (H1N1)], may progress early in the disease course to a pattern of organizing pneumonia, explaining the presence of the RHS.
Another possible mechanism of virus aggression has attracted researchers' attention. A series of publications has addressed the relationship between COVID-19 and thrombogenesis [1]. Among patients with acute respiratory distress syndrome referred to intensive care units, Helms et al. [7] found that patients with this syndrome secondary to COVID-19 developed significantly more thrombotic complications, mainly pulmonary embolism, than did those without COVID-19 (11.7% versus 2.1%, p < 0.008), and that >95% of patients with COVID-19 had elevated D-dimer and fibrinogen levels. The mechanisms involved in this manifestation of thrombosis remain unclear. The pathophysiology of vascular disease in patients with COVID-19 is controversial, and could involve in situ microvascular thrombosis or pulmonary embolism originating from pelvic or lower-limb veins. As pulmonary vascular disease in COVID-19 involves mainly the segmental and subsegmental arteries, some authors have suggested that the development of pulmonary thromboembolism in COVID-19 is attributable to pulmonary artery thrombosis caused by severe lung inflammation and hypercoagulability, rather than thromboembolism [8,9]. In this situation, we hypothesize that the RHS could be interpreted as an indirect sign of pulmonary embolism. In a minimally invasive autopsy study including 10 patients with COVID-19, Dolhnikoff et al. [5] found a variable number of small fibrinous thrombi in the small pulmonary arterioles. They concluded that the pathological observations supported the current concept of hypercoagulative status in these critically ill patients, with a high frequency of pulmonary microthrombosis. These pathological findings have been matched in imaging studies. Chest CT angiography has revealed the presence of pulmonary thrombi, including the formation of pulmonary infarctions [10]. Pulmonary CT angiography demonstrated acute pulmonary emboli in 32 of 106 (30%; 95% confidence interval, 22–40%) patients with COVID-19 infection [11].
In this context, we must recognize that the RHS, atypical non-contrast CT finding among patients with COVID-19, may be related not only to the organization of the infectious process, but also to pulmonary infarction. This differential diagnosis is extremely important, as different therapeutic approaches will be taken in the presence of thromboembolic disease. The reported frequency of the RHS in patients with COVID-19 ranges from 2% to 5% [[12], [13], [14], [15]]. In patients with pulmonary embolism and no COVID-19, the frequency of the RHS ranges from 16% to 18% [16,17]. The morphological characteristics of the RHS may help to narrow its origin. Areas of low attenuation inside the halo, with or without reticulation, strongly suggest pulmonary infarction. Subpleural and lower-lung localization, as well as pleural effusion in association with the RHS, may also favor pulmonary infarction [16]. These chest CT findings indicate the need for additional examination by pulmonary CT angiography in patients with unsuspected pulmonary embolism. Given the significant rate of acute kidney injury in patients with COVID-19, however, intravenous contrast injection for imaging should be used with caution. Duplex ultrasonography, echocardiography, and even clinical suspicion alone can play larger roles in these cases.
In conclusion, the RHS is a common COVID-19–related non-contrast CT finding, and may be related to either of two distinct pathophysiological events with different imaging characteristics. The RHS with homogeneous internal ground-glass density is more common, and suggests the diagnosis of organizing pneumonia. Alternatively, the presence of low-attenuation areas inside the halo, with or without reticulation, should prompt consideration of pulmonary infarction, especially when accompanied by pleural effusion, D-dimer elevation, or sudden clinical worsening. In these conditions, unless contraindicated, the use of pulmonary CT angiography should be considered.
References
- 1.Rotzinger D.C., Beigelman-Aubry C., von Garnier C., Qanadli S.D. Pulmonary embolism in patients with COVID-19: time to change the paradigm of computed tomography. Thromb. Res. 2020 Jun;190:58–59. doi: 10.1016/j.thromres.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simpson S., Kay F.U., Abbara S., Bhalla S., Chung J.H., Chung M. Radiological society of North America Expert Consensus statement on reporting chest CT findings related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA. Radiology: Cardiothoracic Imaging. 2020;2(2) doi: 10.1148/ryct.2020200152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bernheim A., Mei X., Huang M., Yang Y., Fayad Z.A., Zhang N. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020 Feb 20:200463. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kligerman S.J., Franks T.J., Galvin J.R. Organization and fibrosis as a response to lung injury in diffuse alveolar damage, organizing pneumonia, and acute fibrinous and organizing pneumonia. Radiographics. 2013;33:1951–1975. doi: 10.1148/rg.337130057. [DOI] [PubMed] [Google Scholar]
- 5.Dolhnikoff M., Duarte-Neto A.N., de Almeida Monteiro R.A., Ferraz da Silva L.F., Pierre de Oliveira E., Nascimento Saldiva P.H. Pathological evidence of pulmonary thrombotic phenomena in severe COVID-19. J. Thromb. Haemost. 2020 Apr 15 doi: 10.1111/jth.14844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang H., Zhou P., Wei Y., Yue H., Wang Y., Hu M. Histopathologic changes and SARS-CoV-2 immunostaining in the lung of a patient with COVID-19. Ann. Intern. Med. 2020 Mar 12 doi: 10.7326/M20-0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Helms J., Tacquard C., Severac F., Leonard-Lorant I., Ohana M., Delabranche X. High risk of thrombosis in patients in severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020 doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cavagna E., Muratore F., Ferrari F. Pulmonary thromboembolism in COVID-19: venous thromboembolism or arterial thrombosis? Radiology: Cardiothoracic Imaging. Jul 9 2020 doi: 10.1148/ryct.2020200289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Desborough M.J.R., Doyle A.J., Griffiths A., Retter A., Breen K.A., Hunt B.J. Image-proven thromboembolism in patients with severe COVID-19 in a tertiary critical care unit in the United Kingdom. Thromb. Res. 2020 May 29;193:1–4. doi: 10.1016/j.thromres.2020.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moreira B.L., Santana P.R.P., Zanetti G., Marchiori E. COVID-19 and acute pulmonary embolism: what should be considered to indicate a computed tomography pulmonary angiography scan? Rev. Soc. Bras. Med. Trop. 2020;53 doi: 10.1590/0037-8682-0267-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Leonard-Lorant I., Delabranche X., Severac F., Helms J., Pauzet C., Collange O. Acute pulmonary embolism in COVID-19 patients on CT angiography and relationship to D-dimer levels. Radiology. 2020 Apr 23:201561. doi: 10.1148/radiol.2020201561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bernheim A., Mei X., Huang M., Yang Y., Fayad Z.A., Zhang N., Diao K., Lin B., Zhu X., Li K., Li S., Shan H., Jacobi A., Chung M. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020 Feb 20:200463. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bai H., Hsieh B., Xiong Z. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT. Radiology. 2020 doi: 10.1148/radiol.2020200823. published online ahead of print, 2020 Mar 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li Y., Xia L. Coronavirus disease 2019 (COVID-19): role of chest CT in diagnosis and management. Am. J. Roentgenol. 2020;214(6):1280–1286. doi: 10.2214/AJR.20.22954. [DOI] [PubMed] [Google Scholar]
- 15.Wu J., Pan J., Teng D., Xu X., Feng J., Chen Y.-C. Interpretation of CT signs of 2019 novel coronavirus (COVID-19) pneumonia. Eur. Radiol. 2020 May 4:1–8. doi: 10.1007/s00330-020-06915-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marchiori E., Menna Barreto M., Pereira Freitas H.M., Hochhegger B., Soares Souza A. Jr, Zanetti G., Dias Mançano A., Souza Rodrigues R. Morphological characteristics of the reversed halo sign that may strongly suggest pulmonary infarction. Clin. Radiol. 2018;73:503.e7–503.e13. doi: 10.1016/j.crad.2017.11.022. [DOI] [PubMed] [Google Scholar]
- 17.Mançano A.D., Rodrigues R.S., Menna Barreto M., Zanetti G., Moraes T.C., Marchiori E. Incidence and morphological characteristics of the reversed halo sign in patients with acute pulmonary embolism and pulmonary infarction undergoing computed tomography angiography of the pulmonary arteries. J. Bras. Pneumol. 2019;45 doi: 10.1590/1806-3713/e20170438. [DOI] [PMC free article] [PubMed] [Google Scholar]