To the Editor:
We would like to thank Chowdhary et al for their constructive comments1 regarding our recent publication describing mortality rates in a cohort of patients with coronavirus disease 2019 (COVID-19) with a history of radiotherapy.2 We wholeheartedly agree that additional potential risk factors, including comorbid medical conditions,3 should be included in future analyses on this topic. We are currently sharing patient data with large national and international consortia4,5 to enable more definitive analyses.
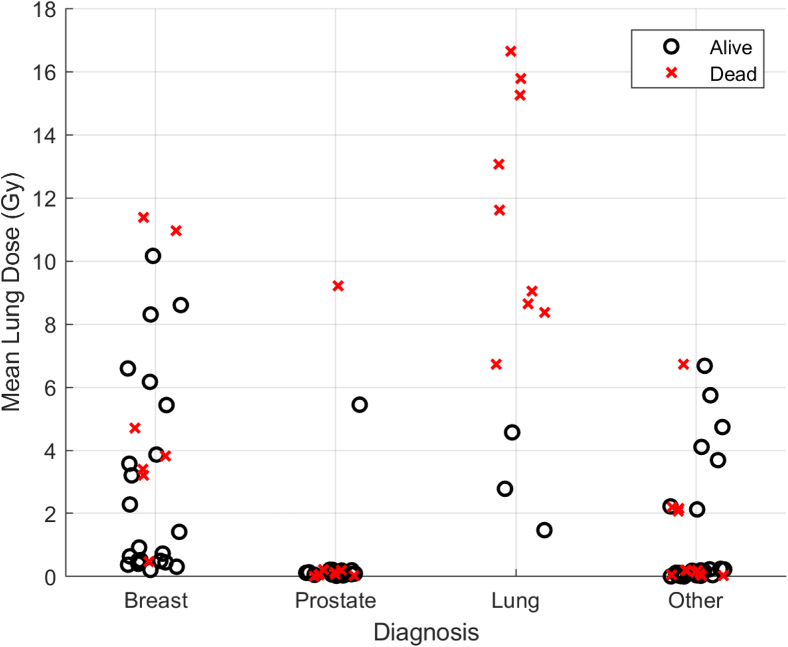
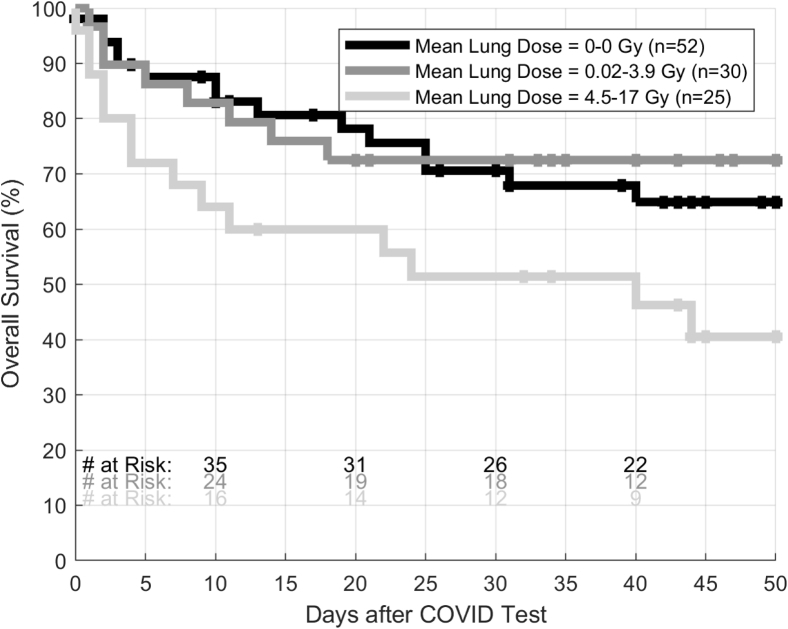
To try to address other concerns about our analysis, we now present updated data. Additional deaths have unfortunately occurred in our cohort of 107 patients, including deaths more than 14 days after COVID-19 diagnosis. The actuarial 14-day survival rate is now 75%, and the 45-day survival rate is now 61%. Figure 1 depicts the relationship between primary cancer type, mean lung radiation therapy dose, and vital status in our data set. Figure 2 contains updated Kaplan-Meier survival curves.
Figure 1.
Scatter plot depicting primary cancer diagnosis, mean lung radiation therapy dose, and vital status for patients who contracted coronavirus disease 2019 (COVID-19).
Figure 2.
Updated Kaplan-Meier overall survival curves for patients grouped by mean lung radiation therapy dose.
We invite readers to make their own interpretations of our data. We find it plausible that patients with a history of significant lung irradiation may be at increased risk for complications when faced with a serious viral pneumonia. Until more conclusive data are available, we hope that all patients with thoracic cancers/tumors receive appropriate guidance and social support to minimize their risk of contracting COVID-19.
Footnotes
Sources of support: This work had no specific funding.
Disclosures: none.
References
- 1.Chowdhary M., Greco L., McFarlane M. In regard to Kabarriti et al. Adv Radiat Oncol. 2020 doi: 10.1016/j.adro.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kabarriti R., Brodin N.P., Maron M.I. Extent of prior lung irradiation and mortality in COVID-19 patients with a cancer history. Adv Radiat Oncol. 2020;5:707–710. doi: 10.1016/j.adro.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehta V., Goel S., Kabarriti R. Case fatality rate of cancer patients with COVID-19 in a New York hospital system. Cancer Disc. 2020;10:935–941. doi: 10.1158/2159-8290.CD-20-0516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rubinstein S., Steinharter J.A., Warner J. The COVID-19 & Cancer Consortium (CCC19): A collaborative effort to understand the effects of COVID-19 on patients with cancer. Cancer Cell. 2020;37:738–741. doi: 10.1016/j.ccell.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whisenant J.G., Trama A., Torri V. TERAVOLT: Thoracic Cancers International COVID-19 collaboration. Cancer Cell. 2020;37:742–745. doi: 10.1016/j.ccell.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]