Abstract
Introduction:
Drug adherence is a major factor in determining health outcomes of geriatric patients and is a growing concern for health-care systems as the geriatric population shows a steep rise due to improved health-care services in the UAE.
Aim:
We aimed to evaluate the adherence and beliefs of geriatric patients in the UAE toward their medicines and to explore the factors affecting them.
Methods:
A cross-sectional study was performed including 163 geriatric patients. Surveys, direct observations, and interviews were used for primary data collection. Demographic data were computed using descriptive statistics method. The Statistical Package for the Social Sciences (SPSS) program, Version 19.0, SPSS Inc., Chicago, IL, USA, was used to analyze and code the raw data, whereas chi-squared test was used to analyze the responses. Secondary data were also collected.
Results:
The results indicated that patient factors and medication factors are the main risk factors for medication nonadherence among geriatric patients in the UAE. The study found that drug regimen (91.4%, N = 149), forgetfulness (87.1%, N = 142), time constraints (67.5%, N = 110), and cost (55.2%, N = 90) were the main key factors affecting medication adherence. Also, poor communication (12.9%), the lack of trust (16.6%), confidence (20.2%), and patient involvement (43.6%) were shown to influence adherence behaviors to medication. The main habits, attitudes, and beliefs that were found to affect patient’s adherence were follow-ups (73%), inadequate knowledge of medicine (60.1%), the lack of perceived benefits (18.4%), and limited knowledge on health conditions (19.6%). The study showed 161 patients among the total 163 participants forget taking their medications and others cease from taking their medications. To conclude, nonadherence to medications is a substantial problem among the elderly in the UAE.
Conclusion:
The study findings confirm the need for further research to examine the perspectives of at-risk population with a focus on knowledge, beliefs, and attitudes on medication nonadherence.
KEYWORDS: Drug administration, geriatric patients, medication adherence, medication nonadherence, patient belief, United Arab Emirates
INTRODUCTION
Medicines that are prescribed to the elderly patients often have a multiple of issues and as a consequence, it is important for medical practitioners to ensure that the structures and the process of drug management among them are defined and described explicitly to optimize patients’ outcomes.[1] A broad array of practices, for example, prescribing, drug administration and monitoring, and promoting patient drug adherence are encompassed within the scope of the concept of medicines management.[1] The major roles of health-care experts in medicine management include developing drugs that are related to the patient care plans to support a suitable choice of drug therapy, educating health-care providers, families, and patients to encourage medicines adherence, monitoring the patients’ outcomes of drug use, and ensuring both drug safety and effectiveness.[2] Therefore, it is critical for health-care professionals across different countries, including the UAE, to adequately understand the key roles involved in the effective medicines management. Such practices increase the potential of patients to adhere to appropriate drugs, which, in turn, yields positive patient outcomes.
Research has revealed that medication adherence is a growing concern for health-care systems, caregivers, and several other sponsors in the health-care sector due to the growing evidence that nonadherence is dominant and often associated with negative patient outcomes and relatively higher costs of care.[3] One central point that impacts adherence is that the patient’s capacity to peruse and comprehend medication guidelines. Patients with low proficiency may experience issues understanding guidelines. This leads to diminished adherence and poor drug administration. It has additionally been observed that patients’ nonadherence fluctuates between people and also crosswise over time, prescribed practices, and illnesses. The adherence to medication and treatment fluctuates with age. A noteworthy problem behind nonadherence is a higher patient–doctor conflict, which causes patients to feel discomfort with health-care providers. Nonadherence can also occur when the pharmaceutical regimen is complex and there is poor planning in medication organization.
Underuse, abuse, and inappropriate utilization of medication keeps on being the most widely recognized reasons for poor adherence to treatment. In an empirical investigation that explored adherence to antidiabetic medications in patients at a hospital in Ajman, UAE, Koprulu et al.[4] revealed that forgetfulness is the most common reason for medication nonadherence. The study investigated both medication adherence and the factors that induce the behaviors of patients with type 2 diabetes to have poor adherence to medications.[4] The study addressed the factors that are usually associated with noncompliance to medicine for treating type 2 diabetes in the regions of North UAE.[4] The study concluded that patient adherence to diabetes medication is quite poor in the Northern Region of the UAE.[4] A different research examined the relationship between knowledge and drug adherence in patients with hypertension in the UAE. The researchers reported that in the UAE, there is a positive relationship between knowledge and drug adherence among them.[5]
MATERIALS AND METHODS
Data collection methods
After obtaining the approval of the ethical committee of Ajman University (F-H-18-1-04), a cross-sectional study was performed. One hundred sixty-three geriatric patients were included in the study. The study was explained to the participants and their written consent was obtained. Then, the structured questionnaires were distributed and interviews with the participants were conducted. In this study, the focus was on selecting data collection method that could help in assessing the level of adherence and beliefs toward medication among the elderly patients in the UAE, understanding the factors that influence the compliance to medication by the elderly patients in the UAE, and developing possible solutions to the issue of adherence. Primary and secondary methods were used to collect the needed data. Primary sources and procedures such as surveys, direct observations, and interviews were used as the sources of collecting data.[6,7] The first primary qualitative data collection method in this study was interviews. In this case, the researcher interviewed older patients and their family members and their physicians in Sharjah. Interviews were carried out to retrieve first-hand qualitative information regarding the patients.
The second primary data collection method in this study was semi-structured questionnaires. Questionnaires refer to research forms that were handed or sent to the patient and collected later after they have been filled.[6] The questionnaire forms contained a set of questions related to the issues under investigation in the study.
Secondary data were extracted from other scholarly works examining adherence or noncompliance to medication by the geriatric population. To address the proposed theoretical perspective in the study, secondary sources played an essential role. These sources provided a multi-perspective understanding of the elderly patients’ adherence to medication in the UAE.
Sampling of 163 geriatric patients
Inclusion criteria included the following:
Participants were elderly patients from the UAE
The 163 participants were geriatric patients aged 55 years and older.
All the geriatric patients who signed informed consent participated in the study.
Exclusion criteria included the following:
Geriatric patients outside the UAE.
Elderly patients aged below 55 years.
A stratified probability sampling strategy was used to select the participants from a particular group. In this probability sampling method, the study population is grouped separately based on their knowledge and background to the study problem. The intention is to guarantee that the selected sample represents a given subgroup.[8] Using stratified method, the study population in this study were geriatric patients and were selected because they had enough background to the phenomenon. Hence, they were appropriate to provide information that can help in exploring the issue of medication adherence.
Data analysis
In this study, the raw data acquired from the field were systematically organized for analysis. The data collected, both qualitatively and quantitatively, were analyzed differently in this study.
Analysis in qualitative study involves the interpretation of the collected data by using the context of information collected through face-to-face discussions to understand people’s understanding of the phenomenon.[9] In this study, qualitative analysis of data was conducted by interviewing geriatric patients, their family members, and their physicians. The quantitative data were examined through numerical interpretation and interpreting figures gathered in the course of the study to determine the rationale behind the emergence of the primary findings. The Statistical Package for the Social Sciences (SPSS) program, Version 19.0, SPSS Inc., Chicago, IL, USA was used to analyze and code the raw data. The SPSS program helped in determining whether the variables of the study were related to each other in answering the questions. Graphs, pie charts, and tables were generated to present the analyzed data. Finally, the secondary data were used to make further sense of the results of the qualitative and quantitative procedures undertaken in this study.
Ethics
All the followed procedures were in accordance with the ethical standards of the research ethical committee of Ajman University. Ethical approval number (F-H-18-1-04) was obtained.
RESULTS AND DISCUSSION
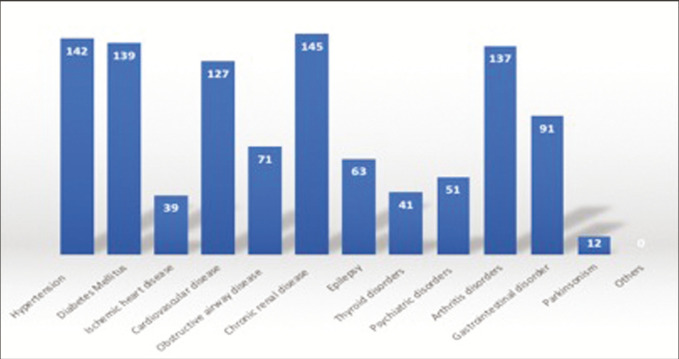
The aim of the research was to assess the level of adherence and beliefs toward medication among the elderly patients in the UAE. The respondents were asked to share details regarding the medical illnesses they have with the option to select multiple illnesses in case if they have to. The top four reported medical illnesses include chronic renal disease, hypertension, diabetes mellitus, and arthritis disorders. The medical illnesses receiving the lowest response include parkinsonism, ischemic heart disease, and psychiatric disorders as indicated in Figure 1.
Figure 1.
Medical illnesses reported by respondents
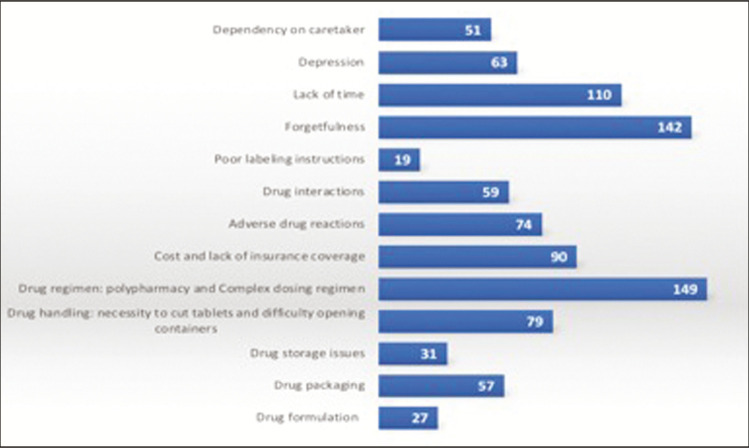
Patients’ factors as indicated in Figure 2 were highly responsible for the cause of nonadherence to medications. Forgetfulness, lack of time, and cost of drugs prevented more than half of the patients from efficiently adhering to their medications regimen. Many patients had difficulties remembering to take their pills at the right time, whereas complex drug regimen, the high cost of medicines, and drug handling also appeared to be a difficult task. Patients found it difficult opening containers and cutting their drugs, which is understandable, especially with their old age ranging from 55 years and above. A previous research found that socioeconomic factors such as support from family members on purchasing medication and remembering to take medications lead to a lower readmission due to high adherence to drugs.[10] Patients who have poor compliance to drugs are likely to develop more complications, experience more hospital readmissions, and cause an increase in the cost of care.[11] Also, factors such as health literacy, old age, low level of education, the male gender, and mental and physical status influence adherence to medication.[11] Medication factors such as inadequate instruction labeling, complicated regimen, high cost, and provider–patient’ relationship such as the lack of patient involvement, the lack of trust, and the lack of follow-up were also found to hinder patients from adhering to medications. A study by Roy et al.[12] on adherence to medications by elderly patients showed that taking many pills, forgetfulness, and the inability to remember taking pills was affecting medication adherence of more than 50% of the 240 patients surveyed. Forgetfulness, old age, and taking many pills have a great association in affecting medical adherence by patients.[13] Forgetfulness ranks among the most common factors in various studies.
Figure 2.
Factors that may affect medication adherence
Health-care providers factors affecting medication adherence
The factors of education level for patients and health-care providers also affect the extent to which patients adhere to medications. A previous study found a significant association between patients’ lack of knowledge on their condition and nonadherence to medications.[13] In this study, the lack of confidence on health-care provider was the provider’s factor that affected patients most, though not in great numbers as expected. As most of the patients in this study were highly educated, poor labeling instructions, packaging, and formulation were not common problems that affected the adherence to medication but most had the association with patients’ factors mainly related to old age. A high level of education is not enough to prevent nonadherence but physical and mental factors have a great deal in affecting patient’s adherence to drugs.[14] This was also evident when 99% of the patients agreeing to follow the doctor’s instructions but still, 99% stated they often forget to take their medications.
The lack of patients’ involvement appeared as the most common health provider factor that affected drug adherence. One study showed that high health-care provider involvement in their patients’ welfare such as the provision of counseling helps in improving patients’ adherence to medication a lot.[11] In this study, 53% of clinicians cited the lack of confidence on the health providers as a factor related to their professionalism that affected patient’s adherence to medication. These two factors seem to be related as understanding and the lack of involvement in patients’ affairs will lead them to have low confidence and trust on health-care providers. Jin et al.[11] further showed that patients’ adherence to medication was highly enhanced by great satisfaction in the services provided by their health-care providers. Therefore, health-care providers have a role to play in enhancing patients’ drug adherence by providing quality services, follow-up services, and responding to the need of the patients. The health-care provider factors are presented in Figure 3.
Figure 3.
Health-care provider factors affecting medication adherence
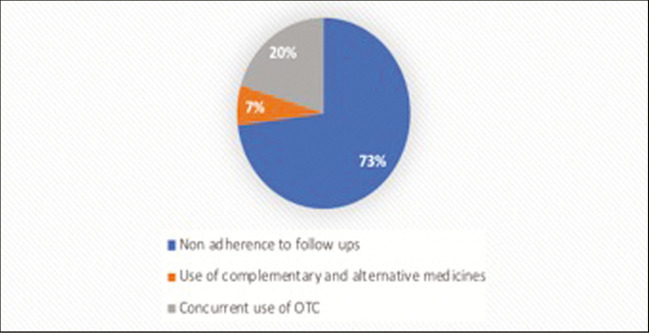
Attitude, habits, knowledge, and belief toward medication adherence
To assess the attitude and habits of the patients toward adherence to medication, they were asked to share their response on what attitude or habit affects their medication adherence. As shown in Figure 4, a majority of the participants indicated that nonadherence to follow-ups is their main attitude/habit affecting their medication adherence.
Figure 4.
Attitude and habits toward medication adherence
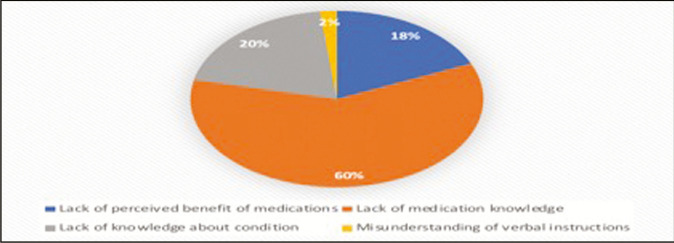
In terms of the knowledge and beliefs affecting medication adherence, it was found that the lack of medication knowledge (N = 98, 60.1%) was the main factor followed by the lack of perceived benefit of medications (18.4%) and the lack of knowledge about condition (19.6%) as shown in Figure 5.
Figure 5.
Knowledge and belief affecting medication adherence
Medication factors and conditions
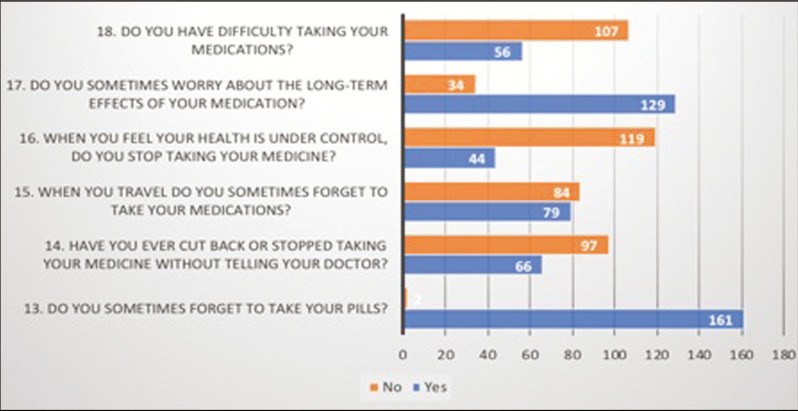
The participants were asked a series of questions to assess their current adherence to medication. As shown in Figure 6, the respondents indicated that they are forgetful in taking the pills on time (N = 161) and have discontinued the medication without prior consent from the doctor (N = 66). Even during travel, 79 respondents indicated that they forget to take their medication. Though a majority (N = 107) indicated that they do not have difficulty in taking their medication, 129 of 163 respondents shared that they worry about the long-term effect of the medication on their health. In terms of whether the participants discontinue their medication if they feel their health is under control, a majority (N = 119) denied, which reflects their worry about their health and willingness to take their medication for a better outcome. The respondents were also asked about the amount of medication being consumed currently to which a majority (N = 85) indicated as 5–9, followed by 10–14 (N = 63).
Figure 6.
Current adherence to medication
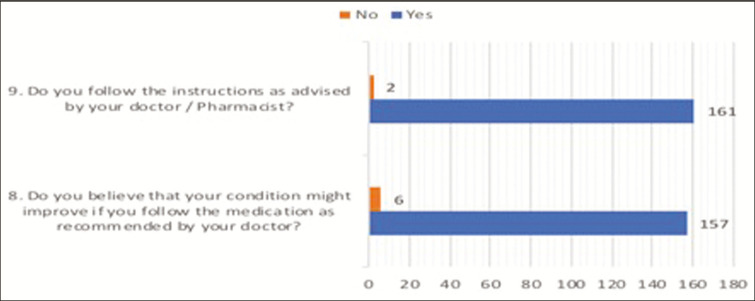
When asked if the participants adhere to the instructions given by the doctor or pharmacist, a majority (N = 163) replied in affirmation [Table 1]. Similarly, when asked if the participants believed that their condition might improve due to medication adherence as recommended by their doctor, a majority agreed (N = 157) as presented in Figure 7.
Table 1.
Relationship between knowledge and belief and demographics
| Test statistics | |
|---|---|
| N | 163 |
| χ2 | 224.84 |
| df | 2 |
| Asymp. sig. | 0.030* |
*Statistically significant difference
Figure 7.
Following medication instructions
Relationship between knowledge and belief and demographics
A linear independent sample test was conducted to understand if there is a statistically significant relationship between demographics and knowledge and belief of patients toward medication adherence. The relationship displayed a chi-square value of 224.84 with two degrees of freedom (df) as shown in Table 1. The relationship was found to be statistically significant as P = 0.03 (<0.05). This indicates that demographics (gender, age, marital status, and education) significantly affect the knowledge and belief of patients toward medication adherence.
Relationship between knowledge and belief and medication illnesses
A linear independent sample test was conducted to understand if there is a statistically significant relationship between medical illnesses reported by patients and the knowledge and belief of the respondents toward medication adherence [Table 2]. The relationship displayed a chi-square value of 271.04 with 2 df. The relationship was found to be statistically significant as P = 0.02 (<0.05). This indicates that medical illnesses reported by patients significantly affect the knowledge and belief of the participants toward medication adherence.
Table 2.
Relationship between knowledge and belief and medication illnesses
| Test statistics | |
|---|---|
| N | 163 |
| χ2 | 271.04 |
| df | 2 |
| Asymp. sig. | 0.020 |
Relationship between knowledge and belief and patient factors
A linear independent sample test was conducted to understand if there is a statistically significant relationship between factors reported by the patients affecting medication adherence and the knowledge and belief of patients toward medication adherence [Table 3]. The relationship displayed a chi-square value of 265.6 with 5 df. The relationship was found to be statistically significant as P = 0.01 (<0.05). This indicates that patient factors reported by the participants significantly affect the knowledge and belief of the patients toward medication adherence.
Table 3.
Relationship between knowledge and belief and patient factors
| Test statistics | |
|---|---|
| N | 163 |
| χ2 | 265.6 |
| df | 5 |
| Asymp. sig. | 0.010 |
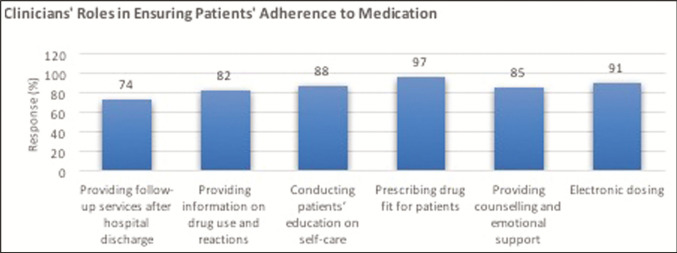
Clinicians’ role in adherence
There were similar but varied responses in the study where clinicians gave various ways of ensuring patients adherence to their medication regimen. The prescription of the right drugs to patients, using electronic dosing, providing counseling and emotional support, and education to patients on self-care were among the methods that clinicians highly use in ensuring patients take their medicines. The clinician’s role in controlling patients’ adherence to medications is presented in Table 4.
Table 4.
Clinician’s role in controlling patients’ adherence to medications
| Clinicians’ roles | Responses | % |
|---|---|---|
| Providing follow-up services after hospital discharge | 25 | 74 |
| Providing information on drug use and reactions | 28 | 82 |
| Conducting patients’ education on self-care | 30 | 88 |
| Prescribing drug fit for patients | 33 | 97 |
| Providing counseling and emotional support | 29 | 85 |
| Others | 15 | 44 |
The percentages of their responses are also presented in bar graph as shown in Figure 8.
Figure 8.
Clinicians’ roles in ensuring patients’ adherence to medication
A review on the best means of enhancing drug adherence by health-care providers was conducted and it was found out that the practitioners can overcome the barriers that prevent patients from adhering to their medications through providing support.[15] Patients receiving ongoing and constant support from doctors, nurses, and family members can stick to their drugs for long. Encouragements in the form of assistance, daily treatment support, counseling in the form of cognitive behavior therapy, and motivational counseling and great education lead to improvement in adherence.[15] The study showed that even though the provision of support improved a patient’s adherence to medication, the improvement was not significant to lead to better outcomes.[15] In a study that sought to identify the effects of interventions toward drug adherence, it was found out that providing feedback on improved adherence by 19.8% increased by 16.1% when cognitive education became part of the program.[16] The researchers found out that although these interventions had the ability of promoting medical adherence, their effectiveness showed a reduction of 1.1% per month.[16] Another research found out that the use of electronic reminders was effective in enhancing the patient’s ability to adhere to their medications as it allowed patients not to miss any dosage.[17] The study showed that there is a remarkable improvement in drug adherence in the short-term, especially for elderly patients as most of them forget to take their drugs. As 87% and 76% of the patients and clinicians, respectively, cited forgetfulness as affecting medication adherence, this method can be very useful.
Some studies showed that many of the clinicians’ interventions may not be effective in the long term.[15,16] Another study provided a better approach to the problem where the researchers identified that using a combination of these interventions was effective in improving medication adherence.[18] The combination of family therapy, counseling, self-monitoring, information, reminders, and electronic dosing enhances a patient’s adherence to medications.[18] However, the researchers found out that these interventions were complicated and had no prediction of effectiveness. Therefore, the use of a more innovative response would make the process easier.
CONCLUSION
Patient and health-care provider factors influence medication adherence in geriatric patients. Factors such as drug regimen, forgetfulness, time constraints, cost, poor communication, the lack of trust, the lack of confidence, and the lack of patient involvement influence the ability of elderly patients to adhere to their medications. The main habits, attitudes, and beliefs that affect adherence include nonadherence follow-ups, limited medication knowledge, the lack of perceived benefits, and the lack of knowledge on health condition. The beliefs and knowledge of geriatric patients about adherence to medications is significantly affected by their medical conditions. There is a significant relationship between demographics, knowledge, and beliefs of geriatric patients and their adherence to pharmacological therapies. Clinicians have a key role in promoting the adherence of geriatric patients to their drug regimens. Clinicians ensure patient’s follow-up, provide information on uses of drugs and their effects, offer patient education, prescribe relevant drugs to the patients, and provide emotional support and counseling.
Implications for future research
The issue of collaboration between clinicians and family members in enhancing adherence to pharmaceutical treatments has not been adequately explored. Therefore, future studies should seek to determine how collaborative relationships influence the attitudes of geriatric patients on the adherence to their drug regimens. Future studies should also focus on exploring the impact of innovative technologies such as electronic dosing systems on the adherence of geriatric patients to medications. Such studies will inform the adoption and implementation of emerging technologies during the dispensing process of drugs to the elderly patients.
Limitations of the study
The limitations of this study can be addressed by future researchers such as the use of larger sample sizes. The study did not determine the influence of specific cultural and social factors on nonadherence to medication among geriatric patients with chronic illnesses. The study, however, captured the age aspect of the participants, which was essential for the research. Future research should investigate into other unexplored areas, such as collaboration between patients’ family members and health providers in providing follow-up and medication adherence.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Al Shemeili SK. Exploring structures and processes of medicines management in elderly hospitalised patients in the United Arab Emirates. J Pharm Pract Res. 2015;36:58–66. doi: 10.1111/jep.12542. [DOI] [PubMed] [Google Scholar]
- 2.Fillit H, Rockwood K, Woodhouse KW, Brocklehurst JC. Brocklehurst’s textbook of geriatric medicine and gerontology. Philadelphia, PA: Saunders/Elsevier; 2010. [Google Scholar]
- 3.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 4.Koprulu F, Bader RJ, Hassan NA, Abduelkarem AR, Mahmood DA. Evaluation of adherence to diabetic treatment in Northern Region of United Arab Emirates. Trop J Pharm Res. 2014;13:989–95. [Google Scholar]
- 5.Gaili AA, Al-Ebraheem SQ, Metwali ZM, Abdalla N, Al-Akshar S. The relationship between knowledge and drug adherence in hypertensive patients: a cross sectional study in UAE. Am J Adv Drug Deliv. 2016;4:1–11. [Google Scholar]
- 6.Bajpai N. Business research methods. New Delhi, India: Pearson Education India; 2011. [Google Scholar]
- 7.Myers MD. Qualitative research in business & management. Los Angeles, CA: SAGE Publications; 2008. [Google Scholar]
- 8.Walliman N. Your research project: designing and planning your work. London, UK: SAGE Publications; 2011. [Google Scholar]
- 9.Collins H. Creative research: the theory and practice of research for the creative industries. London, UK: AVA Publications; 2010. [Google Scholar]
- 10.Hsu C, Lemon JM, Wong ES, Carson-Cheng E, Perkins M, Nordstrom MS, et al. Factors affecting medication adherence: patient perspectives from five veterans affairs facilities. BMC Health Serv Res. 2014;14:533. doi: 10.1186/s12913-014-0533-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jin H, Kim Y, Rhie SJ. Factors affecting medication adherence in elderly people. Patient Prefer Adherence. 2016;10:2117–25. doi: 10.2147/PPA.S118121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roy NT, Sajith M, Bansode MP. Assessment of factors associated with low adherence to pharmacotherapy in elderly patients. J Young Pharm. 2017;9:272–6. [Google Scholar]
- 13.Karakurt P, Kaşikçi M. Factors affecting medication adherence in patients with hypertension. J Vasc Nurs. 2012;30:118–26. doi: 10.1016/j.jvn.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Kalogiani A. Factors affecting patient adherence to medication regimen. J Health Sci. 2011;5:157–8. [Google Scholar]
- 15.Nieuwlaat R, Wilczynski N, Navarro T, Hobson N, Jeffery R, Keepanasseril A, et al. Interventions for enhancing medication adherence. Cochrane Library. 2014;11:1–172. doi: 10.1002/14651858.CD000011.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Demonceau J, Ruppar T, Kristanto P, Hughes DA, Fargher E, Kardas P, et al. Identification and assessment of adherence-enhancing interventions in studies assessing medication adherence through electronically compiled drug dosing histories: a systematic literature review and meta-analysis. Drugs. 2013;73:545–62. doi: 10.1007/s40265-013-0041-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vervloet M, Linn AJ, van Weert JC, de Bakker DH, Bouvy ML, van Dijk L. The effectiveness of interventions using electronic reminders to improve adherence to chronic medication: a systematic review of the literature. J Am Med Inform Assoc. 2012;19:696–704. doi: 10.1136/amiajnl-2011-000748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA. 2002;288:2868–79. doi: 10.1001/jama.288.22.2868. [DOI] [PubMed] [Google Scholar]