Abstract
Rationale. Incarceration carries several negative ramifications for population health, while diverting scarce resources from other public goods. At a time when health care systems around the world are strained, the current study investigates the long-term relationship between incarceration and health care infrastructure. Objective. We investigated the longitudinal association between incarceration rates and hospital beds per capita for 36 countries between 1971 and 2015. Method. Fixed effects regression analyses were employed to examine the effect of within-country changes in incarceration rates on hospital beds per capita. Results. Findings demonstrated that increases in national incarceration rates over time were associated with declines in hospital beds per capita, net of controls for socio-demographic and economic factors. Conclusions. Increased incarceration negatively impacts hospital bed availability at the cross-national level.
Keywords: Incarceration, Health care, Hospital beds, Health, Punishment
Highlights
-
•
Incarceration is associated with worse population health.
-
•
Limited research assesses spillover effects of incarceration for health care.
-
•
Cross-national incarceration is inversely associated with hospital beds per capita.
-
•
Incarceration may carry negative implications for health care infrastructure.
1. Introduction
A growing body of research documents that incarceration carries negative ramifications for population health (Blankenship et al., 2018; Jahn et al., 2020; Stuckler et al., 2008; Testa et al., 2020; Weidner and Schultz, 2019; Wildeman, 2016; Wildeman and Wang, 2017) and shows increased incarceration has spillover effects that negatively impact other institutions including labor markets (Western and Beckett, 2001) and political institutions (Uggen and Manza, 2002). While the influence of incarceration on population health and other social institutions has received considerable attention, less research has focused on how incarceration effects the wider functioning of health care systems (Schnittker et al., 2015). Even so, previous research has drawn attention to this issue, noting, “consideration of the [impact on the] health care system is essential to evaluating the total social costs of incarceration” (Schnittker et al., 2015: p. 518). This consideration is particularly relevant in light of the COVID-19 pandemic, which has increased awareness of the spread of infectious diseases within correctional institutions (Rubin, 2020), and the capacity of hospital and health care infrastructure worldwide (Cavallo et al., 2020).
Thus far, existing research has focused on the relationship between incarceration and a single measure of health care infrastructure: psychiatric hospitalization (Kim, 2016). This line of research stems from Penrose's (1939) hypothesis and subsequent observation of an inverse relationship between prison populations and psychiatric bed capacity in 18 European countries. This hypothesis received increased attention during the latter half of the 20th century as many countries began undergoing a period of psychiatric deinstitutionalization (Mundt, 2019). While this relationship has been observed in other parts of the world including South America (Mundt et al., 2015) and the United States (Harcourt, 2011), there are a variety of issues surrounding data and methodology that prevent any firm conclusions from being made in regard to the Penrose hypothesis (Kalapos, 2016; Kim, 2016; Mundt, 2019).
The focus on psychiatric hospitalization leaves open the question of whether the inverse relationship between incarceration and health care infrastructure extends beyond that of mental health care capacity alone. The exclusive focus on the tradeoff in the relationship between incarceration and psychiatric hospitalization neglects the possibility that investment in social control via incarceration may be offset by broader reductions in health care infrastructure across public, private, general, and specialized hospitals (Schnittker et al., 2015). Indeed, one plausible hypothesis is that the inverse relationship between incarceration and psychiatric hospitalization is that it is just one reflection of the broader extent to which a society emphasizes social support relative to social control (Cullen, 1994). That is, increased emphasis on social control through incarceration will be associated with broader reductions in social support that extend beyond just psychiatric hospitalization and negatively impact other forms of social support including general health care infrastructure.
According to prior research, countries that emphasize greater social support expenditures are likely to be characterized by a stronger emphasis on investing in public health (Papanicolas et al., 2019) and less investment in institutions of social control such as incarceration (Sutton, 2000). At the same time, greater investment in social control via incarceration may be offset by reduced investment in the broader health care infrastructure. As one example, Schnittker et al. (2015) found that U.S. states with a higher percentage of former prisoners have a weaker health care infrastructure characterized by a higher percentage of uninsured residents and higher rates of emergency room visitations.
However, extant research has only begun to consider the general relationship between incarceration and health care infrastructure. Existing research that has examined this relationship has largely been conducted at sub-national levels within the United States. Wildeman (2016: p. 361) notes that “virtually all existing research on the macro-level consequences of incarceration has to date focused solely on the United States … which is problematic because there are several reasons to expect changes in the incarceration rate in the United States and in other developed democracies to yield qualitatively different results.” Indeed, incarceration rates vary substantially across countries, with the United States being particularly unique in this regard having an especially steep rise in incarceration rates between the 1970s and 2010s relative to other countries (Travis et al., 2014).
In this study, we use longitudinal data for a sample of 36 countries from 1971 to 2015 to assess the longitudinal relationship between incarceration and health care infrastructure. Specifically, we address the following research question:
Is there a longitudinal association between incarceration rates and hospital beds per capita?
2. Method
2.1. Sample
Data for this study were compiled from a variety of international organizations including the World Health Organization (WHO), United Nations (UN), and World Bank. The study was restricted to countries with available data beginning during the 1970s and 1980s – a key phase in the buildup of incarceration in many countries (Walmsley, 2003). Because several variables used in the analysis were not collected every year, we used a five-year average of variables which is a common practice in cross-national incarceration research (Weiss et al., 2020). The final analytic sample is comprised of nine (T) 5-year waves (1971–1975, 1976–1980, 1981–1985, 1986–1990, 1991–1995, 1996–2000, 2001–2005, 2006–2010, 2011–2015) for 36 (N) countries resulting in a sample size of 254 country-waves (N x T). Appendix A details the sample selection process and Appendix B provides the countries and years included in the sample.
2.2. Dependent variable
Hospital beds per capita measures the number of inpatient beds available in public, private, general, and specialized hospitals and rehabilitation centers, including both acute and chronic care per 1,000 population. Hospital bed data are compiled by the WHO and are supplemented by the World Bank. Hospital beds are a key measure of health care infrastructure as they indicate the availability of inpatient services in each country. Hospital beds per capita is transformed using the natural logarithm to account for the positive skew.
2.3. Independent variable
Incarceration rate measures the average number of incarcerated persons in prison and jail per 100,000 population. Incarceration rates are collected from the World Prison Brief, which is hosted by the Institute for Crime & Justice Policy Research (Walmsley, 2018). Incarceration rates are based on national government statistics, as well as other official sources. The incarceration rate is log transformed to adjust for positive skew.
2.4. Control variables
Several control variables are included to account for relevant socio-demographic characteristics of a country. Percent male represents the percentage of a country's population that is male and is obtained from the from the UN World Population Prospects. The Gini Index is used to control for economic inequality and ranges from a hypothetical value of 0 (completely equal) to 1 (completely unequal) and is obtained from the Standardized World Income Inequality Database (SWIID) (Solt, 2016). For analyses, we mutliplied the orignal Gini Index by 100, thereby rescaling the index to 0–100. To account for cross-national differences in crime, we include the homicide rate per 100,000 obtained from WHO Mortality Database. Homicide rate is log transformed to account for the positive skew. To adjust for differences in the age structure of a population, we include an ordinal variable for the percentage of the population in each of five age groupings (0–14 [reference], 15–29, 30–44, 45–59, and 60 and older). Data on age-structure were obtained from the UN World Population Prospects. We measure the system of governance in a country using data from the Polity database, which produces a 21-point scale (−10 to +10) (Marshall and Jaggers, 2004). Following prior research, we collapse the scale into three categories: full democracy (10 points on the Polity scale), transitional democracy (1–9 points), and autocracy (−10 to 0 points) (LaFree and Tseloni, 2006). Finally, to adjust for socio-economic development, we generate a development index using four highly correlated items from the World Bank: gross domestic product per capita, infant mortality rate, life expectancy, and percentage of a country's population that lives in urban areas. The development index is created using principal components analysis and is set to a standardized scale ranging from 0 to 100, where higher scores equate to more socio-economic development (Cronbach's α = 0.862; Eigenvalue = 2.85).
2.5. Analytic approach
The longitudinal association between incarceration and hospital bed rates is assessed using fixed-effects linear regression. Fixed-effects modeling assesses within-country changes in incarceration and hospital beds, while controlling for the influence of any unobserved time-invariant measures that may confound this association. Also, the observed controls account for the influence of several time-varying variables. The coefficients from fixed-effects models provide an estimate of how contemporaneous changes in incarceration rates over time correspond with changes in hospital beds per capita over time (Kropko and Kubinec, 2020). A Hausman test revealed that the fixed-effects model is a preferred estimation method compared to random-effects (χ2 = 27.80, p < .001). Standard errors are clustered by country to account for dependence of observations within countries (Wooldridge, 2002). A statistical power analysis performed using G*Power 3.1 (Faul et al., 2009) indicates adequate sample size to detect a small effect size and a 0.05 significance level for a multivariable fixed-effects regression (two-tailed test).
3. Results
Table 1 provides the summary statistics for the analytic sample. The mean incarceration rate is 136 per 100,000 population and ranges from a low of 33.14 (Greece; 1976–1980) to a high of 751.19 (United States; 2006–2010). The average hospital bed rate is 5.10 per 1,000 population, and ranges from a low of 0.34 (Venezuela; 1971–1975) to a high of 15.6 (Finland; 1976–1980).
Table 1.
Descriptive statistics (N = 254).
| Variables | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| Hospital Beds Per Capita | 5.10 | 3.52 | .34 | 15.60 |
| Hospital Beds Per Capita (Ln) | 1.36 | .78 | −1.09 | 2.75 |
| Incarceration Rate | 136.00 | 108.40 | 33.15 | 751.20 |
| Incarceration Rate (Ln) | 4.72 | .57 | 3.50 | 6.62 |
| Development Index | 63.44 | 21.76 | 0 | 100 |
| GDP per Capita | 23993.49 | 17829.23 | 1010.50 | 89546.11 |
| Infant Mortality Rate | 13.99 | 14.14 | 2.08 | 96.56 |
| Life Expectancy | 75.26 | 4.48 | 56.31 | 83.28 |
| Percent Urban | 73.12 | 14.71 | 22.59 | 100.00 |
| Percent Male | 49.38 | .70 | 47.45 | 52.33 |
| Homicide Rate (Ln) | 5.70 | 10.37 | 0.23 | 80.02 |
| Homicide Rate | .91 | 1.18 | −1.49 | 4.38 |
| Gini Index | 35.02 | 8.80 | 20.56 | 53.54 |
| Polity | ||||
| Autocracy | .07 | .26 | 0 | 1 |
| Transitional Democracy | .37 | .49 | 0 | 1 |
| Full Democracy | .55 | .50 | 0 | 1 |
| Age Composition | ||||
| Percent ages 0 to 14 | 24.11 | 8.13 | 13.16 | 46.18 |
| Percent ages 15 to 29 | 23.57 | 3.68 | 15.17 | 33.23 |
| Percent ages 30 to 44 | 20.79 | 2.57 | 13.83 | 29.76 |
| Percent ages 45 to 59 | 16.08 | 3.92 | 7.87 | 25.13 |
| Percent ages 60 or more | 15.45 | 6.29 | 4.54 | 31.89 |
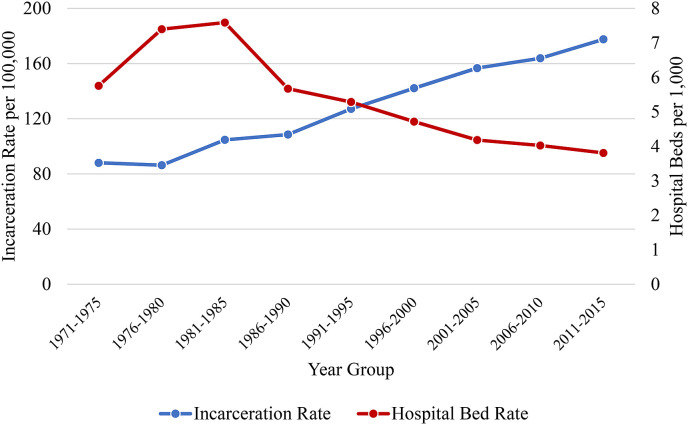
Fig. 1 displays the trends in the incarceration and hospital bed rates from 1971 to 2015. During this time period, the average incarceration rate among countries in the sample has doubled from 88 (1971–1975) to 177 per 100,000 population (2011–2015), while the average hospital bed rate has decreased from 5.75 in 1971–1975 to 3.80 per 1,000 population in 2011–2015.
Fig. 1.
Trends in incarceration rates and hospital bed rates (1971–2015).
Table 2 presents the results of the fixed effects regression of hospital beds per capita regressed on incarceration rates. Model 1 demonstrates that incarceration rates yield a strong negative bivariate association with hospital beds per capita (β = −0.403, 95% CI = −0.624, −0.182). After adding the controls in Model 2, we find that the inverse association between incarceration and hospital beds per capita remains similar (β = −0.427, 95% CI = −0.751, −0.102). Substantively, the results indicate that each 1% increase in the incarceration rate is associated with a 0.4% decline in hospital beds per capita. Appendix C displays this inverse association: Thus, a country with an incarceration rate of 100 persons per 100,000 is predicted to have 4.1 hospital beds per 1,000 persons. However, this predicted rate falls to 2.6 hospital beds per capita for countries with an incarceration rate of 300 per 100,000. A robustness analysis that removed the United States from the analytic sample produced substantively similar findings (results available as an online appendix).
Table 2.
Fixed Effects Regression Models Predicting Hospital Beds Per Capita (per 1,000 population).
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Variables | β | 95% CI | β | 95% CI |
| Incarceration Rate (Ln) | -.403*** | (-.624; −.182) | -.427* | (-.751; −.102) |
| Development Index | -.031*** | (-.046; −.016) | ||
| Percent Male | -.060 | (-.233; .113) | ||
| Homicide Rate (Ln) | -.042 | (-.187; .102) | ||
| Gini Index | -.042** | (-.069; −.014) | ||
| Autocracy (Reference) | ||||
| Transitional Democracy | .285† | (-.023; .594) | ||
| Full Democracy | .233 | (-.176; .641) | ||
| Percent ages 0 to 14 (Reference) | ||||
| Percent ages 15 to 29 | .054* | (.013; .094) | ||
| Percent ages 30 to 44 | .096*** | (.053; .140) | ||
| Percent ages 45 to 59 | .052* | (.013; .091) | ||
| Percent ages 60 or more | .046† | (-.009; .101) | ||
| Constant | 3.266*** | (2.223; 4.309) | 4.824 | (-3.996; 13.645) |
| Observations | 254 | 254 | ||
| R-squared | .133 | .437 | ||
| Number of Countries | 36 | 36 | ||
†p<.10; *p < .05; **p < .01; ***p < .001.
4. Discussion
The global spread of COVID-19 has drawn attention to the importance of population health, the vulnerability of prison systems across the world to the spread of infectious disease, and how under-resourced health care systems are in many countries. Drawing from a growing body of research that suggests incarceration is a key social institution that impacts population health (Wildeman and Wang, 2017), as well as a smaller body of research suggesting that incarceration may have spillover effects on health care (Schnittker et al., 2015), the current study investigated whether increases in incarceration rates within countries over time are associated with changes in the number of hospital beds per capita. Results suggest that there is an inverse association between incarceration and hospital beds per capita at the country level. While this is the first study to examine the relationship between incarceration and hospital bed availability, this result is consistent with the Penrose (1939) hypothesis which is specific to psychiatric hospitalization, as well as prior research on incarceration and health care infrastructure at the sub-national level in the United States (Schnittker et al., 2015).
These findings also expand upon efforts to understand how incarceration is related to population health by suggesting that incarceration may increase the strain placed on national health care systems by contributing to adverse health outcomes while simultaneously reducing the capacity of the systems that treat these health problems. In this sense, the findings highlight broader societal consequences that result from increased incarceration. Sampson (2011) previously proposed that research should evaluate the full ramifications of the benefits of incarceration (i.e. crime reduction) against any unintended and hidden costs. On this point, recent work has suggested the one fruitful avenue is “to more fully assess the incarceration ledger and the potential offsetting consequences of the prison boom for health inequalities.” (Light and Marshall, 2018: p. 15). Our study highlights the degree to which prison booms may contribute to a weakening of health care infrastructure, which in turn may generate greater vulnerabilities for population health.
4.1. Limitations and future directions
Several limitations in the current study may be expanded upon in future research. First, the study was limited to 36 mostly developed countries due to limitations in the availability of longitudinal data. As more longitudinal data emerge, future research can investigate the relationship between incarceration and health care infrastructure in a broader sample of both developed and developing countries. Second, the current study used five-year averages and could not assess annual changes in incarceration and hospital beds per capita because data on key variables are not collected annually. Third, this study focused on the impact of incarceration on hospital beds per capita only. Future research can investigate the link between incarceration and other metrics of health care infrastructure such as the number of doctors per capita, the percentage of uninsured citizens, and the frequency of emergency room visitations. Fourth, because detailed measures on crime rates are not available cross-nationally, we used national homicide rates to control for differences in crime. While homicide rates are considered the most reliable and available indicator of crime in a cross-national context, incarceration rates may be influenced by rates of property and violent crime beyond that of homicide. Fifth, the measure of hospital beds per capita combines a variety of inpatient beds including public, private, general, and specialized hospitals. Thus, we cannot disentangle the specific hospital bed types in each country. Sixth, while the focus of this study was on incarceration, future research could explore other measures of punitiveness, such as the number of police, the use of alternative punishments aside from incarceration, and the prevalence of capital punishment. Finally, countries have numerous budgetary considerations in any given year, which were not fully accounted for, including national infrastructure investment, social welfare programs, and national security.
5. Conclusions
The COVID-19 pandemic highlights challenges in the tradeoff between investment in public goods including public health and public safety. As the effects of the virus strain the existing resources of national health care systems by requiring high levels of hospitalization, large populations in jails and prisons can contribute to the further spread of contagions while placing an even greater strain on existing resources. Countries should take a holistic approach to public welfare by considering the potential negative ramifications of prioritizing one public good at the expense of others.
Author contribution
Alexander Testa: Conceptualization; Formal analysis; Methodology; Writing - original draft; reviewing and editing, Mateus Rennó Santos: Data curation; Formal analysis; Methodology; Writing original draft; reviewing and editing, Douglas B. Weiss: Conceptualization; Methodology; Writing - original draft; reviewing and editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2020.113262.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Blankenship K.M., del Rio Gonzalez A.M., Keene D.E., Groves A.K., Rosenberg A.P. Mass incarceration, race inequality, and health: expanding concepts and assessing impacts on well-being. Soc. Sci. Med. 2018;215:45–52. doi: 10.1016/j.socscimed.2018.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavallo J.J., Donoho D.A., Forman H.P. Hospital capacity and operations in the coronavirus disease 2019 (COVID-19) pandemic—planning for the Nth patient. JAMA Health Forum. 2020;1(3) doi: 10.1001/jamahealthforum.2020.0345. e200345-e200345. [DOI] [PubMed] [Google Scholar]
- Cullen F.T. Social support as an organizing concept for criminology: presidential address to the academy of criminal justice sciences. Justice Q. JQ. 1994;11(4):527–559. [Google Scholar]
- Faul F., Erdfelder E., Buchner A., Lang A.G. Statistical power analyses using G* Power 3.1: tests for correlation and regression analyses. Behav. Res. Methods. 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- Harcourt B.E. Reducing mass incarceration: lessons from the deinstitutionalization of mental hospitals in the 1960s. Ohio State Journal of Criminal Law. 2011;9(1):53–88. [Google Scholar]
- Jahn J.L., Chen J.T., Agénor M., Krieger N. Social Science & Medicine; 2020. County-level Jail Incarceration and Preterm Birth Among Non-hispanic Black and White US Women, 1999–2015; p. 112856. [DOI] [PubMed] [Google Scholar]
- Kalapos M.P. Penrose's law: methodological challenges and call for data. Int. J. Law Psychiatr. 2016;49:1–9. doi: 10.1016/j.ijlp.2016.04.006. [DOI] [PubMed] [Google Scholar]
- Kim D.-Y. Psychiatric deinstitutionalization and prison population growth: a critical literature review and its implications. Crim. Justice Pol. Rev. 2016;27(1):3–21. [Google Scholar]
- Kropko J., Kubinec R. Interpretation and identification of within-unit and cross-sectional variation in panel data models. PloS One. 2020;15(4) doi: 10.1371/journal.pone.0231349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaFree G., Tseloni A. Democracy and crime: a multilevel analysis of homicide trends in forty-four countries, 1950-2000. Ann. Am. Acad. Polit. Soc. Sci. 2006;605:25–49. [Google Scholar]
- Light M.T., Marshall J. On the weak mortality returns of the prison boom: comparing infant mortality and homicide in the incarceration ledger. J. Health Soc. Behav. 2018;59(1):3–19. doi: 10.1177/0022146517748412. [DOI] [PubMed] [Google Scholar]
- Marshall M.G., Jaggers K. Center for International Development and Conflict Management, University of Maryland; College Park: 2004. Polity IV Project: Political Regime Characteristics and Transitions, 1800-2004. [Google Scholar]
- Mundt A.P. Asylums and deinstitutionalization: the Penrose hypothesis in the twenty-first century. In: Vollm B., Braun P., editors. Long-term Forensic Psychiatric Care: Clinical, Ethical and Legal Challenges. Springer Nature; Cham, Switzerland: 2019. pp. 7–13. [Google Scholar]
- Mundt A.P., Chow W.S., Arduino M., Barrionuevo H., Fritsch R., Girala N., Minoletti A., Mitkiewicz F., Rivera G., Tavares M., Priebe S. Psychiatric hospital beds and prison populations in South America since 1990: does the Penrose hypothesis apply? JAMA psychiatry. 2015;72(2):112–118. doi: 10.1001/jamapsychiatry.2014.2433. [DOI] [PubMed] [Google Scholar]
- Papanicolas I., Woskie L.R., Orlander D., Orav E.J., Jha A.K. The relationship between health spending and social spending in high-income countries: how does the US compare? Health Aff. 2019;38(9):1567–1575. doi: 10.1377/hlthaff.2018.05187. [DOI] [PubMed] [Google Scholar]
- Penrose L.S. Mental disease and crime: outline of a comparative study of European statistics. Br. J. Med. Psychol. 1939;18(1):1–15. [Google Scholar]
- Rubin R. The challenge of preventing COVID-19 spread in correctional facilities. J. Am. Med. Assoc. 2020;323(18):1760–1761. doi: 10.1001/jama.2020.5427. [DOI] [PubMed] [Google Scholar]
- Sampson R.J. The incarceration ledger: toward a new era in assessing societal consequences. Criminol. Publ. Pol. 2011;10:819–828. [Google Scholar]
- Schnittker J., Uggen C., Shannon S.K., McElrath S.M. The institutional effects of incarceration: spillovers from criminal justice to health care. Milbank Q. 2015;93(3):516–560. doi: 10.1111/1468-0009.12136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solt F. The standardized world income inequality database. Soc. Sci. Q. 2016;97(5):1267–1281. [Google Scholar]
- Stuckler D., Basu S., McKee M., King L. Mass incarceration can explain population increases in TB and multidrug-resistant TB in European and central Asian countries. Proc. Natl. Acad. Sci. Unit. States Am. 2008;105(36):13280–13285. doi: 10.1073/pnas.0801200105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutton J.R. Imprisonment and social classification in five common-law democracies, 1955–1985. Am. J. Sociol. 2000;106(2):350–386. [Google Scholar]
- Testa A., Jackson D.B., Vaughn M.G., Bello J.K. Incarceration as a unique social stressor during pregnancy: implications for maternal and newborn health. Soc. Sci. Med. 2020;246:112777. doi: 10.1016/j.socscimed.2019.112777. [DOI] [PubMed] [Google Scholar]
- Travis J., Western B., Redburn F.S. National Academies Press; Washington, DC: 2014. The Growth of Incarceration in the United States: Exploring Causes and Consequences. [Google Scholar]
- Walmsley R. Global incarceration and prison trends. Forum on Crime and Society. 2003;3(2):65–78. [Google Scholar]
- Walmsley R. International Centre for Prison Studies; London, UK: 2018. World Prison Population List. [Google Scholar]
- Weiss D.B., Testa A., Rennó Santos M. Criminology; 2020. Institutional Anomie and Cross‐national Differences in Incarceration. [Google Scholar]
- Weidner R.R., Schultz J. Examining the relationship between US incarceration rates and population health at the county level. SSM-Population Health. 2019;9:100466. doi: 10.1016/j.ssmph.2019.100466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wildeman C. Incarceration and population health in wealthy democracies. Criminology. 2016;54(2):360–382. [Google Scholar]
- Wildeman C., Wang E.A. Mass incarceration, public health, and widening inequality in the USA. Lancet. 2017;389(10077):1464–1474. doi: 10.1016/S0140-6736(17)30259-3. [DOI] [PubMed] [Google Scholar]
- Wooldridge J.M. MIT Press; Cambridge, MA: 2002. Econometric Analysis of Cross Section and Panel Data. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.