Abstract
Introduction
Cardiovascular (CV) disease affects a high percentage of patients with type 2 diabetes mellitus (T2DM), especially in the hospital setting, impacting on mortality, complications, quality of life and use of health resources. The aim of this study was to estimate the incidence, mean length of hospital stay (LOHS) and costs attributable to hospital admissions due to CV events in patients with T2DM versus patients without diabetes mellitus (non-DM) in Spain.
Research design and methods
Retrospective observational study based on the Spanish National Hospital Discharge Database for 2015. Hospital admissions for patients aged ≥35 years with a diagnosis of CV death, non-fatal acute myocardial infarction (AMI), non-fatal stroke, unstable angina, heart failure and revascularization were evaluated. The International Classification of Diseases, Ninth Revision (250.x0 or 250.x2) coding was used to classify records of patients with T2DM. For each CV complication, the hospital discharges of the two groups, T2DM and non-DM, were precisely matched and the number of hospital discharges, patients, LOHS and mean cost were quantified. Additional analyses assessed the robustness of the results.
Results
Of the 276 925 hospital discharges analyzed, 34.71% corresponded to patients with T2DM. A higher incidence was observed in all the CV complications studied in the T2DM population, with a relative risk exceeding 2 in all cases. The mean LOHS (days) was longer in the T2DM versus the non-DM group for: non-fatal AMI (7.63 vs 7.02, p<0.001), unstable angina (5.11 vs 4.78, p=0.009) and revascularization (7.96 vs 7.57, p<0.001). The mean cost per hospital discharge was higher in the T2DM versus the non-DM group for non-fatal AMI (€6891 vs €6876, p=0.029) and unstable angina (€3386 vs €3304, p<0.001).
Conclusions
Patients with T2DM had a higher incidence and number of hospital admissions per patient due to CV events versus the non-DM population. This generates a significant clinical and economic burden given the longer admission stay and higher costs associated with some of these complications.
Keywords: type 2 diabetes, cardiovacsular disease(s), incidence, health care costs
Significance of this study.
What is already known about this subject?
Cardiovascular disease (CVD) affects a high percentage of patients with type 2 diabetes mellitus (T2DM), and this has major consequences on mortality, complications, quality of life and use of health resources.
In Spain, 7.8% of the adult population are diagnosed with T2DM and about 29.8% of these have CVD.
What are the new findings?
T2DM population had a higher incidence in all the cardiovascular (CV) complications studied compared with the population without diabetes mellitus (non-DM), with a relative risk exceeding 2 in all cases.
The mean length of hospital stay (LOHS) (days) was longer in the T2DM group compared with the non-DM group for non-fatal acute myocardial infarction (AMI), unstable angina and revascularization.
The mean cost per hospital discharge was higher in the T2DM versus the non-DM cohort for non-fatal AMI and unstable angina.
How might these results change the focus of research or clinical practice?
The results of this study will help in the understanding of incidence, LOHS and cost of the CV complications (classified considering major adverse cardiovascular events variable) in the real-world setting comparing T2DM and non-DM populations.
This study will provide complementary information on the most widely used intermediate variables in diabetes research, such as hemoglobin A1c and weight.
The findings of this study may support health decision-making by establishing the economic cost of CV events avoided.
Background
The International Diabetes Federation (IDF) estimates that globally type 2 diabetes mellitus (T2DM) affects around 9.3% of the adult population.1 Approximately 32.2% of these patients suffer cardiovascular disease (CVD).2 In Spain, 7.8% of the adult population are diagnosed with T2DM3 and about 23.2% of these have CVD,4 with this figure reaching 40.8% in hospitalized patients with T2DM.5
The IDF estimates that diabetes has an 132% increased risk of CVD death.1 In Spain, the probability of inpatient death from any cardiovascular (CV) event is higher in patients with T2DM compared with patients without this disease (OR 1.06; 95% CI 1.04 to 1.09).6 Furthermore, patients with T2DM have a higher risk of CV events compared with the population without T2DM.7–10 Both CVD and acute CV events have a major clinical impact and negatively affect patients’ quality of life.11
The Food and Drug Administration requires concrete evidence regarding CV safety when evaluating new treatments for diabetes. This evidence includes an assessment of major adverse cardiovascular events (MACE), that is, non-fatal stroke, non-fatal acute myocardial infarction (AMI) and CV death.12 Such evidence has had consequences on the consensus report by the American Diabetes Association and the European Association for the Study of Diabetes.13 This report recommends antidiabetic therapy such as glucagon-like peptide 1 receptor agonists or sodium-glucose cotransporter 2 inhibitors due to their proven CV benefit for patients with CVD. Also, reference T2DM clinical practice guidelines establish CV risk reduction as one of the main treatment goals and recommend adjusting this treatment on an individual basis based on the patient’s CV risk profile.12 14–21
CV complications in T2DM also have significant economic implications.22 23 Patients with T2DM and macrovascular complications consume more health resources,22 24 being even possible to double the use of resources in emergency department admissions (OR 2.69; 95% CI 1.56 to 4.65) and hospitalizations (OR 2.58; 95% CI 1.64 to 4.07) compared with patients with T2DM without such complications.22 In Spain, the annual direct cost per patient with T2DM and CVD was estimated at €4815.60, which is 82% higher than that in patients with T2DM without CVD (€2648.80) and 46% higher than that for patients without T2DM with CVD (€3306.80) (EUR 2011).23 Results from the Spain estimated cost Ciberdem-Cabimer in Diabetes (SECCAID) study25 showed that CVD generated 40% (€764 million) of the total hospital costs (€1934 million) associated with DM (EUR 2012).
Several studies have evaluated the clinical characteristics of patients with T2DM hospitalized due to CV events using the Spanish National Hospital Discharge Database (SNHDD) of the Ministry of Health, Consumer Affairs and Social Welfare (MoHCASW).5 6 8 9 26 The most prevalent CV event in hospitalized patients with T2DM is congestive heart failure (20.1%), followed by cerebrovascular disease (10.3%), coronary disease (9.4%) and peripheral arterial disease (9.1%).5
However, very few studies have evaluated the economic implications of CV events in patients with T2DM treated in the Spanish hospital setting.27 We have only identified internationally based studies that specifically examine the economic impact associated with clinical outcomes based on the MACE variable.28 29 Therefore, it is difficult to quantify the economic impact associated with the complications included in the MACE indicator in the Spanish context.
The aim of this study was to estimate the number of patients, hospital discharges, hospital stay and mean direct costs per hospitalization attributable to CV complications in Spain in 2015, based on whether the discharge was related to T2DM or non-diabetes mellitus (non-DM).
Methods
Study design and population
A retrospective study of hospital discharges recorded between January 1, 2015 and December 31, 2015, in the SNHDD generated by the MoHCASW was carried out. This data set compiles information on the characteristics of patients attended (age and sex), the hospitalization (type of admission/discharge and length of hospital stay (LOHS)) and the diagnoses coded according to the Spanish International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). Completion of the SNHDD is mandatory and must include all hospital discharges from acute hospitals belonging to the National Healthcare System. In 2015, the SNHDD included 93% of all hospital discharges in Spanish hospitals,30 of which 15% of all hospital discharges corresponded to private hospitals.31
The study population included all hospital discharges in which the main diagnosis or procedure was coded under any of the six CV complications included in the expanded MACE indicator (CV death, non-fatal myocardial infarction, non-fatal stroke, heart failure, revascularization and unstable angina).32 Online supplementary material table A1 displays the corresponding ICD-9-CM codes used to define each CV complication. Once the hospital discharge records were selected, six cohorts were defined (one for each CV complication under study).
bmjdrc-2019-001130supp001.pdf (309.4KB, pdf)
Hospital discharge records of patients of both sexes, aged 35 years or older, were included and classified according to diabetes status: T2DM (ICD-9-CM: 250.x0 or 250.x2) recorded as the primary or secondary diagnosis or non-DM. Hospital discharges coded as type 1 DM (T1DM) (ICD-9-CM: 250.x1 or 250.x3), secondary diabetes (ICD-9-CM: 249) or abnormal glucose tolerance (ICD-9-CM: 648.8) were excluded.
Matching
After grouping hospital discharges according to T2DM (cases) or non-DM (controls) for each CV complication, cases and controls were exactly matched (1:1) by age, sex and autonomous community (AC) in which the hospital was located. As there was more than one control for each case, control selection was carried out randomly.
Covariates
Records were stratified by comorbidity based on the Charlson Comorbidity Index (CCI),33 adapted for use with administrative databases.34 To calculate the CCI, 15 disease categories were used, excluding diabetes and the corresponding CV complication, as described by Thomsen et al.35
The presence of risk factors such as smoking, obesity, hypertension and lipid metabolism disorder was also analyzed based on the ICD-9-CM code (online supplementary material table A1).
Incidence estimation
A unique patient identifier was generated from the registry variables: recoded medical record number, recoded hospital, date of birth, sex and AC of residence.
The specific incidence rate of the CV complications in T2DM and non-DM adjusted by sex and age groups was estimated by dividing the number of patients by the corresponding number of people for that population group. For the estimation, the prevalence data of the Di@betes study3 and census data in 2015 from the Spanish Office for National Statistics36 were used.
Direct costs estimation
All Patients Refined-Diagnosis Related Groups direct costs estimated by the MoHCASW were used.37 All costs were expressed in Euros of 2019.
Stratification by patient age and sex
The number of hospital discharges, LOHS and mean direct cost attributable to the CV complications were described according to whether the hospitalization was related to T2DM or non-DM and stratified according to age groups (35–60 years; 61–70 years; 71–80 years; ≥81 years) and sex.
Additional analysis
To validate the results obtained in our analysis, we compared them against the database of the Spanish Network of Hospital Costs (Red Española de Costes Hospitalarios (RECH))38 made up of 16 Spanish hospitals whose cost system is based on activity (full-costing).37
The procedure was the same for this analysis; hospital discharges between 2013 and 2015 whose main diagnosis was any of the six CV complications under study and that met the defined study criteria. Cases (hospital discharges with T2DM) and controls (hospitalizations without DM) were matched according to sex, age and AC of hospital. The LOHS and mean direct costs attributable to the CV complications were described according to whether the hospital discharge was related to T2DM or non-DM.
Statistical analysis
The quantitative variables were described using the mean, SD, median and IQR. Qualitative variables were analyzed according to absolute and relative frequencies. For the comparisons, the Mann-Whitney U test was used for continuous variables and the χ2 test for categorical variables. A significance of 5% was assumed in all the tests performed.
All analyses were performed using the statistical package R V.3.5.1.
Results
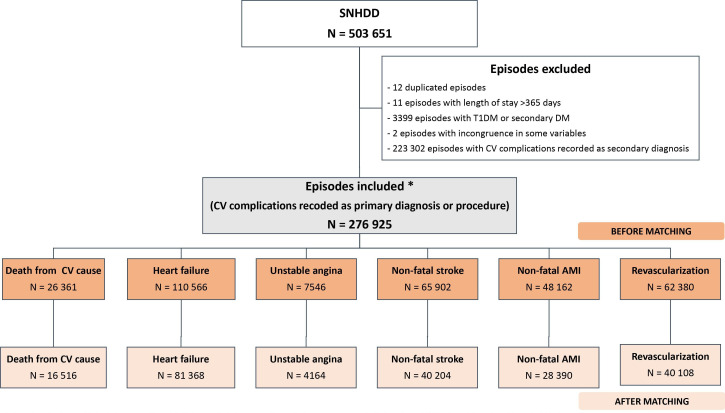
Of the total 503 651 hospital discharges registered in Spain in 2015 that met the selection criteria defined for the analysis, 226 726 records were excluded after data cleansing (figure 1). Therefore, the cohort to be analyzed before matching was 276 925 hospital discharges. CV complications were not considered mutually exclusive, in other words, the same record could be included in the analysis of more than one complication.
Figure 1.
Episodes valuable for analysis. *Mutually non-exclusive CV complications. AMI, acute myocardial infarction; CV, cardiovascular; DM, diabetes mellitus; N, hospital discharge; SNHDD, Spanish National Hospital Discharge Database; TIDM, type 1 diabetes mellitus.
Descriptive analysis of the unmatched study population
Of the total unmatched hospital discharges analyzed, 34.71% were patients with T2DM with a mean age of 75 years (SD: 10.91 years) and 56.93% were men. In the non-DM group, the mean age was 74 years (SD: 13.68 years) and 57.18% were men. There was a higher frequency of risk factors in the T2DM cohort compared with the non-DM cohort: obesity (17.25% vs 9.46%), hypertension (55.88% vs 45.44%) and lipid metabolism disorder (42.37% vs 27.54%), as well as of patients with high CCI (33.18% vs 25.90%). A higher mean (SD) LOHS was observed in the T2DM cohort (8.19 (7.98)) than in the non-DM cohort (8.02 (9.30)), whereas the non-DM cohort had a higher cost per hospitalization (5908 (4952) vs 6194 (6622), T2DM vs non-DM, respectively) (online supplementary material table A2).
On analyzing patients’ sociodemographic and epidemiological characteristics for each of the six CV complications evaluated, the proportion of patients with risk factors (obesity, hypertension and lipid metabolism disorder) was higher in the T2DM population compared with the non-DM group (table 1).
Table 1.
Sociodemographic and epidemiological characteristics of hospitalized patients according to CV complications and presence of T2DM: unmatched T2DM and non-DM groups
| Death from CV cause | Non-fatal AMI | Non-fatal stroke | |||||||
| T2DM | Non-DM | P value | T2DM | Non-DM | P value | T2DM | Non-DM | P value | |
| Hospital discharges— N (%) |
8644 (32.80%) | 17 717 (67.20%) | NA | 14 714 (30.60%) | 33 448 (69.40%) | NA | 20 326 (30.80%) | 45 576 (69.20%) | NA |
| Patients—n | 8644 | 17 717 | 14 049 | 32 347 | 19 578 | 44 216 | |||
| Hospital discharges/patient | 1.00 | 1.00 | 1.05 | 1.03 | 1.04 | 1.03 | |||
| Gender—n (%)* | 0.550 | <0.001 | <0.001 | ||||||
| Men | 4114 (47.59%) | 8362 (47.20%) | 10 082 (68.52%) | 24 637 (73.66%) | 11 548 (56.81%) | 24 521 (53.80%) | |||
| Women | 4528 (52.38%) | 9354 (52.80%) | 4632 (31.48%) | 8810 (26.34%) | 8778 (43.19%) | 21 053 (46.20%) | |||
| Age (years) | <0.001 | <0.001 | <0.001 | ||||||
| Mean (SD) | 81.13 (15.42) | 82.31 (10.73) | 70.73 (12.91) | 65.75 (14.02) | 74.98 (13.57) | 73.68 (13.25) | |||
| Median (Q1; Q3) | 83.00 (77.00; 87.00) | 85.00 (78.00; 89.00) | 72.00 (62.00; 80.00) | 65.00 (55.00; 78.00) | 77.00 (68.00; 83.00) | 77.00 (65.00; 84.00) | |||
| Age (years)—n (%) | <0.001 | <0.001 | <0.001 | ||||||
| 35–60 | 292 (3.38%) | 975 (5.50%) | 3186 (21.65%) | 13 170 (39.37%) | 2207 (10.86%) | 8250 (18.10%) | |||
| 61–70 | 790 (9.14%) | 1289 (7.28%) | 3614 (24.56%) | 7356 (21.99%) | 4029 (19.82%) | 7918 (17.37%) | |||
| 71–80 | 2339 (32.39%) | 3486 (19.68%) | 4382 (29.78%) | 6680 (19.97%) | 7012 (34.50%) | 12 522 (27.47%) | |||
| ≥81 | 5223 (60.42%) | 11 967 (67.55%) | 3532 (24.00%) | 6242 (18.66%) | 7078 (34.82%) | 16 886 (37.05%) | |||
| Smoker—n (%) | 1076 (12.45%) | 2191 (12.37%) | 0.860 | 5546 (37.69%) | 17 244 (51.55%) | <0.001 | 4538 (22.33%) | 11 274 (24.74%) | <0.001 |
| Obesity—n (%) | 1022 (11.82%) | 994 (5.61%) | <0.001 | 2729 (18.55%) | 3831 (11.45%) | <0.001 | 2356 (11.59%) | 2852 (6.26%) | <0.001 |
| Hypertension—n (%) | 4152 (48.03%) | 6683 (37.72%) | <0.001 | 8641 (58.73%) | 14 643 (43.78%) | <0.001 | 13 539 (66.61%) | 23 939 (52.53%) | <0.001 |
| Disorders of lipid metabolism—n (%) | 2821 (32.64%) | 2930 (16.54%) | <0.001 | 7132 (48.47%) | 11 554 (34.54%) | <0.001 | 8664 (42.63%) | 12 569 (27.58%) | <0.001 |
| Charlson Comorbidity Index† | <0.001 | <0.001 | <0.001 | ||||||
| Low | 3577 (41.38%) | 8298 (46.84%) | 8206 (55.77%) | 23 670 (70.77%) | 10 464 (51.48%) | 25 394 (55.72%) | |||
| Medium | 3726 (43.11%) | 6846 (38.64%) | 4492 (30.53%) | 7446 (22.26%) | 7486 (36.83%) | 15 569 (34.16%) | |||
| High | 1341 (15.51%) | 2573 (14.52%) | 2016 (13.70%) | 2332 (6.97%) | 2376 (11.69%) | 4613 (10.12%) | |||
| Unstable angina | Heart failure | Revascularization | |||||||
| T2DM | Non-DM | P value | T2DM | Non-DM | P value | T2DM | Non-DM | P value | |
| Hospital discharges— N (%) |
2488 (32.00%) | 5058 (67.00%) | NA | 42 738 (38.70%) | 67 828 (61.30%) | NA | 20 544 (32.90%) | 41 836 (67.10%) | NA |
| Patients—n | 2392 | 4907 | 34 844 | 57 268 | 19 682 | 40 465 | |||
| Hospital discharges/patient | 1.04 | 1.03 | 1.23 | 1.18 | 1.04 | 1.03 | |||
| Gender—n (%)* | 0.220 | <0.001 | <0.001 | ||||||
| Men | 1473 (59.20%) | 3070 (60.70%) | 20 955 (49.03%) | 31 407 (46.30%) | 15 199 (73.98%) | 32 678 (78.11%) | |||
| Women | 1015 (40.80%) | 1988 (39.30%) | 21 783 (50.97%) | 36 421 (53.70%) | 5344 (26.01%) | 9155 (21.88%) | |||
| Age (years) | <0.001 | <0.001 | <0.001 | ||||||
| Mean (SD) | 71.96 (13.29) | 69.18 (12.92) | 78.53 (15.07) | 80.72 (10.66) | 68.59 (11.84) | 65.15 (12.38) | |||
| Median (Q1; Q3) | 73.00 (65.00; 80.00) | 70.00 (59.00; 80.00) | 80.00 (73.00; 85.00) | 83.00 (76.00; 88.00) | 69.00 (61.00; 77.00) | 65.00 (56.00; 75.00) | |||
| Age (years)—n (%) | <0.001 | <0.001 | <0.001 | ||||||
| 35–60 | 402 (16.16%) | 1355 (26.79%) | 2281 (5.34%) | 4003 (5.90%) | 4818 (23.45%) | 15 737 (37.62%) | |||
| 61–70 | 665 (26.73%) | 1225 (24.22%) | 5936 (13.89%) | 6357 (9.37%) | 6361 (30.96%) | 10 925 (26.11%) | |||
| 71–80 | 807 (32.43%) | 1335 (26.40%) | 13 651 (31.94%) | 15 795 (23.29%) | 6542 (31.84%) | 10 002 (23.91%) | |||
| ≥81 | 614 (24.68%) | 1143 (22.60%) | 20 870 (48.83%) | 41 673 (61.44%) | 2823 (13.74%) | 5172 (12.36%) | |||
| Smoker—n (%) | 700 (28.14%) | 1770 (34.99%) | <0.001 | 7088 (16.58%) | 10 922 (16.10%) | 0.040 | 8465 (41.20%) | 21 187 (50.64%) | <0.001 |
| Obesity—n (%) | 467 (18.77%) | 558 (11.03%) | <0.001 | 8503 (19.90%) | 7352 (10.84%) | <0.001 | 3886 (18.92%) | 4727 (11.30%) | <0.001 |
| Hypertension—n (%) | 1544 (62.06%) | 2486 (49.15%) | <0.001 | 20 201 (47.27%) | 27 385 (40.37%) | <0.001 | 12 813 (62.37%) | 19 411 (46.40%) | <0.001 |
| Disorders of lipid metabolism—n (%) | 1290 (51.85%) | 1917 (37.90%) | <0.001 | 15 903 (37.21%) | 14 314 (21.10%) | <0.001 | 10 913 (53.12%) | 15 828 (37.83%) | <0.001 |
| Charlson Comorbidity Index† | <0.001 | <0.001 | <0.001 | ||||||
| Low | 1252 (50.32%) | 3098 (61.25%) | 15 168 (35.49%) | 28 872 (42.57%) | 3890 (18.93%) | 7243 (17.31%) | |||
| Medium | 928 (37.30%) | 1560 (30.84%) | 20 096 (47.02%) | 28 687 (42.29%) | 13 334 (64.90%) | 30 656 (73.28%) | |||
| High | 308 (12.38%) | 400 (7.91%) | 7474 (17.49%) | 10 269 (15.14%) | 3320 (16.16%) | 3937 (9.41%) | |||
*No data on eight hospital discharges.
†Low: no disease; medium: one to two diseases; high: three or more diseases.
AMI, acute myocardial infarction; CV, cardiovascular; DM, diabetes mellitus; NA, not applicable; Q1, first quartile; Q3, third quartile; T2DM, type 2 diabetes mellitus.
The non-DM population had a higher percentage of smokers in four of the complications (non-fatal AMI, non-fatal stroke, unstable angina and revascularization). Also, statistically significant differences were found in the sociodemographic characteristics (age and sex) between both groups in all CV complications except for the sex variable in death due to CV event and unstable angina. In general, a greater proportion of patients under 60 years was observed in the non-DM group, both aggregately (online supplementary material table A2) and for each individual CV complication (table 1). A higher percentage of women was observed in the T2DM group in three CV complications: non-fatal AMI, unstable angina and revascularization. For all CV complications, a higher number of hospital discharges per patient was observed in the T2DM group, especially in heart failure (table 1). Online supplementary material table A3 describes the sociodemographic and epidemiological characteristics of hospitalized patients with matched cohorts for each of the complications studied.
Incidence rate
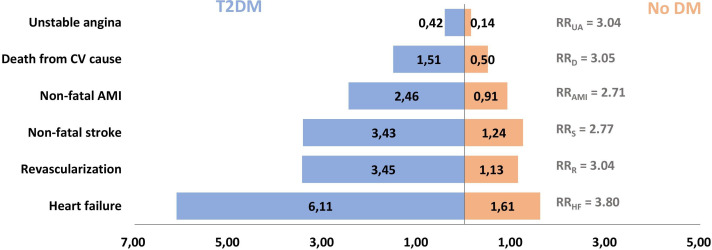
The incidence of T2DM in CV complications ranged between 0.42 hospital discharges/1000 inhabitants in unstable angina and 6.11 hospital discharges/1000 inhabitants in heart failure. The T2DM population had a higher incidence for all CV complications versus the non-DM population, observing an incidence rate at least two times higher in T2DM. CV complications with the greatest difference were heart failure (rate ratio (RR)=3.80), death due to CV event (RR=3.05), unstable angina (RR=3.04) and revascularization (RR=3.04) (figure 2).
Figure 2.
Incidence rate of patients hospitalized due to CV complications per 1000 inhabitants and RR: unmatched T2DM and non-DM groups. AMI, acute myocardial infarction; CV, cardiovascular; DM, diabetes mellitus; RRAMI, non-fatal myocaridal infarction rate ratio; RRD, death from CV cause rate ratio; RRHI, heart failure rate ratio; RRR, revascularization ratio; RRUA, unstable angina rate ratio; T2DM, type 2 diabetes mellitus.
Hospital stay
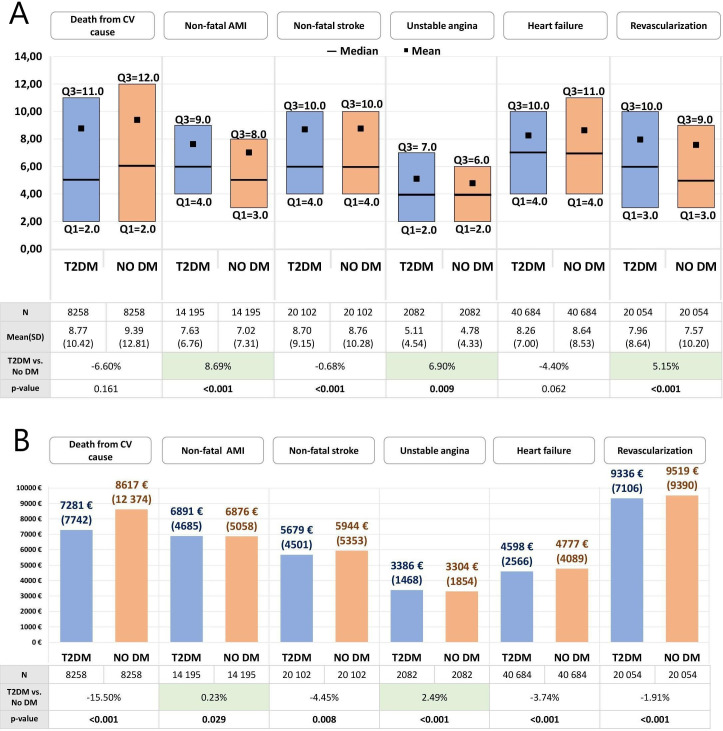
In three CV complications, a higher mean (SD) LOHS was observed in T2DM: 7.63 (6.76) vs 7.02 (7.31) in non-fatal AMI; 5.11 (4.54) vs 4.78 (4.33) in unstable angina and 7.96 (8.64) vs 7.57 (10.20) in revascularization, in T2DM versus non-DM, respectively, all statistically significant (figure 3A). Conversely, a lower mean (SD) LOHS was observed in the T2DM versus the non-DM group in death due to CV event: 8.77 (10.42) vs 9.39 (12.81); non-fatal stroke: 8.70 (9.15) vs 8.76 (10.28) and heart failure: 8.26 (7.00) vs 8.64 (8.53).
Figure 3.
(A) LOHS and (B) direct hospital costs (mean [SD]) attributable to CV complications by presence of T2DM: matched T2DM and non-DM groups. Euros 2019. AMI, acute myocardial infarction; CV, cardiovascular; DM, diabetes mellitus; LOHS, length of hospital stay; T2DM, type 2 diabetes mellitus; Q1, first quartile; Q3, third quartile.
Direct costs
A slightly higher mean (SD) cost was observed for the cohort with T2DM compared with the non-DM cohort for non-fatal AMI (€6891 (4685) vs €6876 (5058)) and unstable angina (€3386 (1468) vs €3304 (1854)) (figure 3B). In death from CV cause, a lower cost was observed in the T2DM group compared with non-DM group (€7281 (7742) vs €8617 (12 374)). In the other complications, the non-DM cohort presented a slightly higher cost per hospitalization (percentage difference <5%). All differences were statistically significant (figure 3B).
LOHS and costs according to age group
Online supplementary material table A4 shows the mean direct cost and LOHS stratified by age group. Both the mean LOHS and mean cost continued to be higher in the T2DM group in non-fatal AMI (except for the cost in the 71–80 and ≥81 age groups) and unstable angina (except for cost in the ≥81 age group). Likewise, the mean LOHS and cost continued to be higher in the non-DM group in death due to CV event, non-fatal stroke (except for LOHS in the ≥81 age group) and heart failure.
LOHS and costs according to sex
Online supplementary material table A5 shows the stratification of LOHS and direct cost by sex. The mean LOHS continued to be higher in the T2DM group for non-fatal AMI, unstable angina and revascularization. For non-fatal stroke, the mean LOHS in the T2DM group was higher in women (8.85 T2DM vs 8.73 non-DM). The mean direct cost continued to be higher in T2DM group for non-fatal AMI (only in men) and unstable angina.
Additional analyses
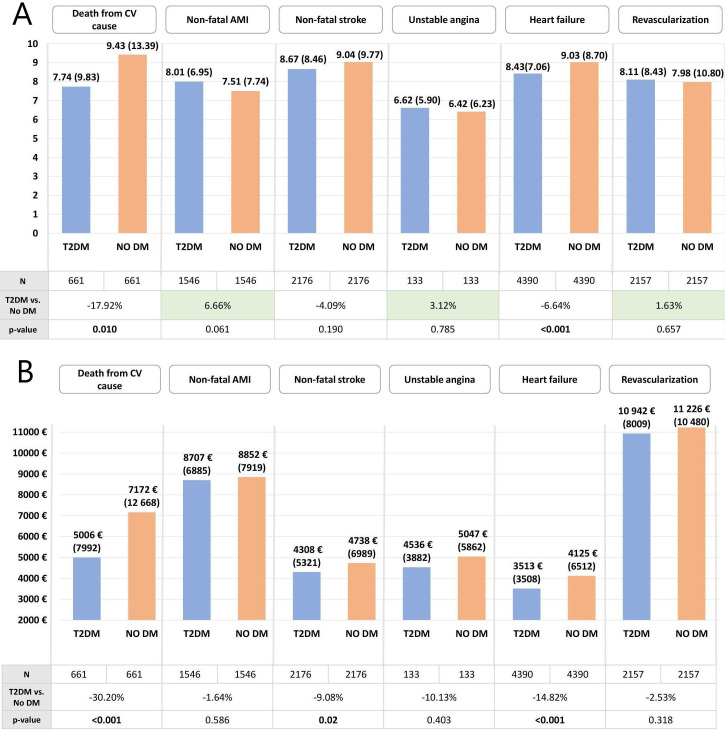
RECH database
In line with the results presented, a higher mean LOHS was observed in the T2DM group versus the non-DM group for non-fatal AMI (8.01 vs 7.51, respectively), unstable angina (6.62 vs 6.42, respectively) and revascularization (8.11 vs 7.98, respectively) (figure 4A). While the mean direct cost was higher in the non-DM group for the six CV complications evaluated (figure 4B).
Figure 4.
(A) LOHS and (B) direct hospital costs attributable to CV complications by presence of T2DM (mean (SD)) (Red Española de Costes Hospitalarios database): matched T2DM and non-DM groups. Euros 2019. AMI, acute myocardial infarction; CV, cardiovascular; DM, diabetes mellitus; LOHS, length of hospital stay; T2DM, type 2 diabetes mellitus.
Discussion
The results of this study highlight the clinical and economic burden of hospital admissions due to CV events in patients with T2DM. In the group of patients with T2DM, a higher incidence was observed for all CV complications evaluated compared with the non-DM group, with a RR over 3 for heart failure (RR=3.80), death due to CV event (RR=3.05), unstable angina (RR=3.04) and revascularization (RR=3.04). Also, for three of the six CV complications evaluated (non-fatal AMI, unstable angina and revascularization), the mean LOHS increased between 5% and 9% in the group with T2DM. This, consequently, has economic implications given the fact that a reduction in LOHS may result in a decrease in the hospital costs and also provide free hospital-bed-days to be used for other patients.39
Among the main results, a shorter LOHS was observed in patients with T2DM in the complication death due to CV event (reduction of 6.60%; p=0.161). Patients with T2DM have more comorbidities and CV risk factors.6 Moreover, they present greater severity and worse clinical characteristics, which would be associated with higher inpatient mortality after a CV event. Furthermore, the LOHS was shorter for death due to CV complication in women in both study cohorts, which could be related to a poorer prognosis compared with men. In a Spanish study in women hospitalized for ischemic stroke, an increased risk of mortality was observed in women with T2DM versus non-DM (OR 1.07; 95% CI 1.05 to 1.11).9
Regarding costs, the results of our analysis show a slightly higher cost for the population with T2DM in unstable angina and non-fatal AMI. A Spanish study that evaluated hospitalized patients with a primary diagnosis of AMI found a slightly lower cost in patients with DM versus non-DM, €6228 and €6283, respectively (Euro 2006).27 In line with our study, the differences between the two cohorts were minimal. A study in the USA40 found that the total average cost was 2.2 times higher in patients with T2DM versus non-DM. However, although the incidence of vascular complications was higher in the T2DM group, the average cost per CV event was similar between groups. Another study that included 4657 Australian patients, although the association with CVD was not described,41 found that the presence of DM comorbidity increased both the cost of hospitalization (1.22-fold; 95% CI 1.12 to 1.33, p<0.001) and LOHS (OR 1.19; 95% CI 1.06 to 1.33, p=0.002).
Our results showed a lower hospital cost in the population with T2DM for three complications: non-fatal stroke, heart failure and revascularization. Other Spanish studies when evaluating hospitalized patients for transcatheter aortic valve implantation or surgical aortic valve replacement also found this same trend: lower costs in the T2DM population versus the non-DM, which they attributed to shorter LOHS for patients with T2DM.42 However, the increase of hospitalization due heart failure in Spain in the last years43 and the large difference in incidence means that the overall cost remains clearly higher in people with diabetes.
Regarding heart failure, no statistically significant differences were observed in this study in the LOHS between the two groups and the cost per hospitalization was slightly lower in the cohort with T2DM at €179 (reduction of 3.74%, p<0.001). These results corroborate those from Muñoz-Rivas et al44 who, for the 2013–2015 period, found both a shorter mean LOHS due to heart failure for the T2DM versus non-DM population (8.43 vs 8.48, respectively) and a slightly lower mean cost per hospitalization in the T2DM versus the non-DM group (€4184 (€2575) and €4209 (€2822), respectively). Although these results could be a priori associated with some extent to the higher inpatient mortality in patients with T2DM for this complication, Muñoz-Rivas, et al44 found that inpatient mortality was lower in the T2DM (8.15%) group compared with the non-DM group (10.54%). In fact, diabetes was associated with a lower inpatient mortality (OR 0.84; 95% CI 0.83 to 0.86). Possible underdiagnosis of T2DM in patients hospitalized for heart failure could also affect these results.45
Moreover, the burden of the heart failure complication must be placed in context bearing in mind that in our study it is the complication that shows the largest differences in the incidence between the T2DM and non-DM cohorts (RR=3.80). Muñoz-Rivas et al44 estimated a fivefold higher risk (IRR 4.93; 95% CI 4.91 to 4.95) in patients with T2DM. Finally, in another Spanish study based on data from the National Heart Failure Registry (Registro Nacional de Insuficiencia Cardiaca)46 in which patients hospitalized for heart failure were followed up for 1 year, the presence of T2DM was statistically significantly associated with all-cause mortality (HR 1.54; 95% CI 1.20 to 1.97, p=0.001) and with a higher probability of readmissions (HR 1.46; 95% CI 1.18 to 1.80, p<0.001).
Among the main strengths of this study is that it is the first time that LOHS and cost of the CV complications, classified considering MACE variable, are evaluated in the Spanish setting. The study also provides data on the incidence, hospital stays and costs comparing T2DM and non-DM populations stratified by age and sex. The data used are representative of the entire Spanish context, as the SNHDD from the MoHCASW pools data from all the Spanish AC.
The results of this study could serve to support health decision-making by establishing the economic cost of CV events avoided in Spain, and providing complementary information on the most widely used intermediate variables, such as hemoglobin A1c (HbA1c) and weight.29
The main limitation of this study is related with the use of the administrative SNHDD, as the results are conditioned by the quality of the data record in the discharge reports. While this database is an extremely useful tool in hospital management, it lacks relevant information to assess the impact on the results obtained, such as left ventricular ejection fraction, medication, like statins or aspirin, taken by patients prior to or during hospitalization or other variables of interest in the patient’s medical history.39 Other limitations include possible undercoding of T2DM in the hospital setting as HbA1c is not determined during hospitalization or that recording of T2DM diagnoses in the SNHDD is low.5 27 44 Additionally, there is often some difficulty in correctly coding the type of diabetes as T1DM being sometimes reported if the patient uses multiple doses of insulin and T2DM if being treated with antidiabetics and/or basal insulin. Nonetheless, the SNHDD is widely used in the study of hospital discharges in patients with T2DM,5 6 8 9 25–27 39 42 44 and the diagnosis of diabetes in SHNDD was validated in a previous study, where a sensitivity of 55% was observed and a specificity of close to 97%, which would indicate that may be some patients with T2DM who are not encoded in the discharge report, but that most patients not diagnosed with T2DM do not have T2DM, as suggested by the high specificity.47
Another limitation is due to the methodology used for matching. After a thorough review of the literature and evaluation by the clinical coordinators of the study, the exact matching between T2DM and non-DM according to sex, age and AC of the hospital seemed correct. While it is true that other covariates in the matching such as smoking, obesity, hypertension and lipid metabolism could have been considered, it was decided not to include them, given the nature of the database used, which was designed for administrative purposes rather than research. Thus, these conditions may not have been adequately recorded in the database.47 Previous studies in Spain and other countries found that smoking, obesity are frequently not coded in administrative database.9 47 48
Additionally, we could also have evaluated trends in the cost and prevalence of CV complications in recent years. However, the objective was not to evaluate temporal trends but rather to carry out a cross-sectional study to estimate the cost of these complications in the most recent year available in Spain at the time of the study.
A further limitation would be that the costs obtained from the SNHDD correspond to the cost per DRG which implies a series of limitations as it represents an equal cost for each DRG code. It is not possible to differentiate the cost depending on whether the patient had a longer LOHS or required more procedures while admitted.27 To overcome this, the results based on the SNHDD were checked against the RECH38 database which provides more detailed information on hospitalization costs, making it possible to differentiate the cost based on the actual resource used during hospitalization.
Only direct hospital costs were considered in this analysis, which represent one of the main direct cost item associated with CV events,49 reaching up to 48.6% of the mean direct health cost in the case of stroke.50 Other relevant cost categories would be non-healthcare direct costs, for example, informal care that represents 60% of the total average cost.50 Other studies have also estimated the cost associated with MACE events including only the cost of the event the first time it occurs or the year of the event.28 However, it is far to notice that CV complications can have clinical and economic repercussions in both the medium-term and long-term.
Conclusion
CV complications associated with T2DM represent a major burden for the Spanish healthcare system as LOHS are longer or equivalent in patients with T2DM compared with the non-DM population. Both the incidence and number of hospital discharges per patient for all the CV complications are higher in the T2DM population. Finally, in terms of the unstable angina and revascularization complications, the cost per hospitalization is higher in patients with T2DM than in the non-DM group.
This is the first study evaluating the clinical and economic impact of CV complications (defined as MACE) comparing T2DM and non-DM populations and including representative data from the national Spanish setting.
Acknowledgments
The authors would like to thank Elisenda Pomares who helped in the data analysis and interpretation.
Footnotes
Contributors: All authors contributed to the study conception and design, data interpretation and the drafting of the manuscript. EU and RP contributed to the analysis of the study. All authors gave final approval for this version to be published.
Funding: This study was funded by Novo Nordisk Pharma SA. Oblikue Consulting received funding from Novo Nordisk Pharma SA for the development and analysis of this study. Oblikue Consulting performed the analysis independently.
Competing interests: EU, NL-M and RP are employees of Oblikue Consulting. EJ, SA and XG-M received an honorarium from the sponsor and participated as independent consultants. VM is a Novo Nordisk Pharma SA employee.
Patient consent for publication: Not required.
Ethics approval: This study does not contain any studies with human participants or animals performed by any of the authors. It is exclusively based on the exploitation of information from the Spanish National Hospital Discharge Database (SNHDD), which is hosted by the Ministry of Health, Consumer Affairs and Social Welfare (MoHCASW). The SNHDD is regulated by the Spanish law and both dissociation and anonymization of all the records enclosed in it are guaranteed. The data were requested to the MoHCASW, which evaluated our study and concluded that it complied with all ethical aspects in accordance with the Spanish legislation.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data may be obtained from a third party and are not publicly available. According to the agreement signed with the Spanish Ministry of Health, Consumer Affairs and Social Welfare, which provided access to the databases from the Spanish National Hospital Discharge Database (Conjunto Mínimo Basico de Datos; CMBD), the authors cannot share the databases with any other investigator, and the databases have to be destroyed once the investigation has concluded. Consequently, the authors cannot upload the databases to any public repository. However, any investigator can apply for access to the databases by filling out the questionnaire available at: https://www.mscbs.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SolicitudCMBDdocs/2018_Formulario_Peticion_Datos_RAE_CMBD.pdf. All other relevant data are included in the paper.
References
- 1.International Diabetes Federation IDF diabetes atlas. 9th edn Brussels, Belgium: International Diabetes Federation, 2019. [Google Scholar]
- 2.Einarson TR, Acs A, Ludwig C, et al. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol 2018;17:83. 10.1186/s12933-018-0728-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soriguer F, Goday A, Bosch-Comas A, et al. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: the Di@bet.es Study. Diabetologia 2012;55:88–93. 10.1007/s00125-011-2336-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mata-Cases M, Franch-Nadal J, Real J, et al. Prevalence and coprevalence of chronic comorbid conditions in patients with type 2 diabetes in Catalonia: a population-based cross-sectional study. BMJ Open 2019;9:e031281. 10.1136/bmjopen-2019-031281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zapatero-Gaviria A, Gómez-Huelgas R, Canora-Lebrato J, et al. Analysis of hospitalizations by cardiovascular disease in the population with diabetes in Spain. Rev Clin Esp 2019;219:124–9. 10.1016/j.rce.2018.09.012 [DOI] [PubMed] [Google Scholar]
- 6.de Miguel-Yanes JM, Jiménez-García R, Hernández-Barrera V, et al. Impact of type 2 diabetes mellitus on in-hospital-mortality after major cardiovascular events in Spain (2002-2014). Cardiovasc Diabetol 2017;16:126. 10.1186/s12933-017-0609-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dinesh Shah A, Langenberg C, Rapsomaniki E, et al. Type 2 diabetes and incidence of a wide range of cardiovascular diseases: a cohort study in 1·9 million people. Lancet 2015;385:S86. 10.1016/S0140-6736(15)60401-9 [DOI] [PubMed] [Google Scholar]
- 8.Muñoz-Rivas N, Méndez-Bailón M, Hernández-Barrera V, et al. Type 2 diabetes and hemorrhagic stroke: a population-based study in Spain from 2003 to 2012. J Stroke Cerebrovasc Dis 2016;25:1431–43. 10.1016/j.jstrokecerebrovasdis.2016.02.031 [DOI] [PubMed] [Google Scholar]
- 9.Muñoz-Rivas N, Méndez-Bailón M, Hernández-Barrera V, et al. Time trends in ischemic stroke among type 2 diabetic and non-diabetic patients: analysis of the Spanish national hospital discharge data (2003-2012). PLoS One 2015;10:e0145535. 10.1371/journal.pone.0145535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martín-Timón I, Sevillano-Collantes C, Segura-Galindo A, et al. Type 2 diabetes and cardiovascular disease: have all risk factors the same strength? World J Diabetes 2014;5:444–70. 10.4239/wjd.v5.i4.444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peña-Longobardo LM, Rodríguez-Sánchez B, Mata-Cases M, et al. Is quality of life different between diabetic and non-diabetic people? the importance of cardiovascular risks. PLoS One 2017;12:e0189505. 10.1371/journal.pone.0189505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cosentino F, Ceriello A, Baeres FMM, et al. Addressing cardiovascular risk in type 2 diabetes mellitus: a report from the European Society of cardiology cardiovascular roundtable. Eur Heart J 2018:1–13. [DOI] [PubMed] [Google Scholar]
- 13.Davies MJ, D'Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American diabetes association (ADA) and the European association for the study of diabetes (EASD). Diabetes Care 2018;41:2669–701. 10.2337/dci18-0033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diabetes Canada Clinical Practice Guidelines Expert Committee Diabetes Canada 2018 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes 2018;42:S1–326.29650079 [Google Scholar]
- 15.Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm - 2019 executive summary. Endocr Pract 2019;25:69–100. 10.4158/CS-2018-0535 [DOI] [PubMed] [Google Scholar]
- 16.Reyes-García R, Moreno-Pérez Óscar, Tejera-Pérez C, et al. Document on a comprehensive approach to type 2 diabetes mellitus. Endocrinol Diabetes Nutr 2019;66:443–58. 10.1016/j.endinu.2018.10.010 [DOI] [PubMed] [Google Scholar]
- 17.Gomez-Peralta F, Escalada San Martín FJ, Menéndez Torre E, et al. Spanish diabetes Society (SED) recommendations for the pharmacologic treatment of hyperglycemia in type 2 diabetes: 2018 update. Endocrinol Diabetes Nutr 2018;65:611–24. 10.1016/j.endinu.2018.08.004 [DOI] [PubMed] [Google Scholar]
- 18.Artola Menéndez S, Práctica D. Actualización del algoritmo de hiperglucemia 2017. Diabetes Práctica 2017;08:57. [Google Scholar]
- 19.American Diabetes Association Standards of medical care in diabetes - 2019. Diabetes Care 2019;42:1–187.30811333 [Google Scholar]
- 20.Arrieta F, Iglesias P, Pedro-Botet J, et al. Diabetes mellitus and cardiovascular risk: update of the recommendations of the diabetes and cardiovascular disease Working group of the Spanish diabetes Society (SED, 2018). Clin Investig Arterioscler 2018;30:137–53. 10.1016/j.artere.2018.05.002 [DOI] [PubMed] [Google Scholar]
- 21.Ruiz-García A, Arranz-Martínez E, Morón-Merchante I, et al. Consensus document of the Spanish Society of arteriosclerosis (sea) for the prevention and treatment of cardiovascular disease in type 2 diabetes mellitus. Clin Investig Arterioscler 2018;30:1–19. 10.1016/j.arteri.2018.06.006 [DOI] [PubMed] [Google Scholar]
- 22.Fu AZ, Qiu Y, Radican L, et al. Impact of concurrent macrovascular co-morbidities on healthcare utilization in patients with type 2 diabetes in Europe: a matched study. Diabetes Obes Metab 2010;12:631–7. 10.1111/j.1463-1326.2010.01200.x [DOI] [PubMed] [Google Scholar]
- 23.Mata-Cases M, Casajuana M, Franch-Nadal J, et al. Direct medical costs attributable to type 2 diabetes mellitus: a population-based study in Catalonia, Spain. Eur J Health Econ 2016;17:1001–10. 10.1007/s10198-015-0742-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehta S, Ghosh S, Sander S, et al. Differences in all-cause health care utilization and costs in a type 2 diabetes mellitus population with and without a history of cardiovascular disease. J Manag Care Spec Pharm 2018;24:280–90. 10.18553/jmcp.2018.24.3.280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crespo C, Brosa M, Soria-Juan A, et al. Costes directos de la diabetes mellitus Y de Sus complicaciones en España (estudio SECCAID: Spain estimated cost Ciberdem-Cabimer in diabetes). Avances en Diabetología 2013;29:182–9. 10.1016/j.avdiab.2013.07.007 [DOI] [Google Scholar]
- 26.López-de-Andrés A, Perez-Farinos N, de Miguel-Díez J, et al. Impact of type 2 diabetes mellitus in the utilization and in-hospital outcomes of surgical aortic valve replacement in Spain (2001-2015). Cardiovasc Diabetol 2018;17:135. 10.1186/s12933-018-0780-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lopez-de-Andres A, Hernández-Barrera V, Carrasco-Garrido P, et al. Trends of hospitalizations, fatality rate and costs for acute myocardial infarction among Spanish diabetic adults, 2001-2006. BMC Health Serv Res 2010;10:59. 10.1186/1472-6963-10-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kamstra R, Durkin M, Cai J, et al. Economic modelling of costs associated with outcomes reported for type 2 diabetes mellitus (T2DM) patients in the canvas and EMPA-REG cardiovascular outcomes trials. J Med Econ 2019;22:280–7. 10.1080/13696998.2018.1562817 [DOI] [PubMed] [Google Scholar]
- 29.McAdam-Marx C. Economic implications with newer agents to reduce cardiovascular risk in diabetes. Am J Manag Care 2018;24:S279–85. [PubMed] [Google Scholar]
- 30.Ministerio de Sanidad Consumo y Bienestar Social Registro de Altas – CMBD estatal. manual de definiciones Y glosario de términos, 2019. Available: https://pestadistico.inteligenciadegestion.mscbs.es/publicoSNS/Comun/DescargaDocumento.aspx?IdNodo=6415
- 31.Ministerio de Sanidad Consumo y Bienestar Social Instituto de Información Sanitaria. Registro de Altas 2015- CMBD, 2019. Available: http://pestadistico.inteligenciadegestion.msssi.es/publicoSNS/comun/DefaultPublico.aspx [Accessed 11 Oct 2019].
- 32.Marso SP, Holst AG, Vilsbøll T. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2017;376:891–2. 10.1056/NEJMc1615712 [DOI] [PubMed] [Google Scholar]
- 33.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 34.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43:1130–9. 10.1097/01.mlr.0000182534.19832.83 [DOI] [PubMed] [Google Scholar]
- 35.Thomsen RW, Nielsen JS, Ulrichsen SP, et al. The Danish centre for strategic research in type 2 diabetes (DD2) study: collection of baseline data from the first 580 patients. Clin Epidemiol 2012;4:43–8. 10.2147/CLEP.S30083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Instituto Nacional de Estadística [INE] Censo poblacional España, 2018. Available: www.ine.es [Accessed 1 May 2018].
- 37.Ministerio de Sanidad Consumo y Bienestar Social Norma Estatal CMBD 2015, 2019. Available: http://www.mscbs.gob.es/estadEstudios/estadisticas/docs/NORMAGRD2015/Nota_dif_Norma_Est_2015.pdf
- 38.Cots F, Chiarello P, Carreras M, et al. Red Española de Costes Hospitalarios (RECH): bases para Una gestión clínica basada en La evidencia. Gestión y Evaluación Costes Sanit 2012;13:369–83. [Google Scholar]
- 39.Méndez-Bailón M, de Miguel Yanes JM, Jiménez-García R, et al. National trends in incidence and outcomes of acute pancreatitis among type 2 diabetics and non-diabetics in Spain (2001-2011). Pancreatology 2015;15:64–70. 10.1016/j.pan.2014.11.004 [DOI] [PubMed] [Google Scholar]
- 40.Fitch K, Engel T, Sander S, et al. Cardiovascular event incidence and cost in type 2 diabetes mellitus: a Medicare claims-based actuarial analysis. Curr Med Res Opin 2017;33:1795–801. 10.1080/03007995.2017.1346595 [DOI] [PubMed] [Google Scholar]
- 41.Karahalios A, Somarajah G, Hamblin PS, et al. Quantifying the hidden healthcare cost of diabetes mellitus in Australian hospital patients. Intern Med J 2018;48:286–92. 10.1111/imj.13685 [DOI] [PubMed] [Google Scholar]
- 42.Mendez-Bailon M, Lorenzo-Villalba N, Muñoz-Rivas N, et al. Transcatheter aortic valve implantation and surgical aortic valve replacement among hospitalized patients with and without type 2 diabetes mellitus in Spain (2014-2015). Cardiovasc Diabetol 2017;16:144. 10.1186/s12933-017-0631-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Méndez-Bailón M, Jiménez-García R, Hernández-Barrera V, et al. Significant and constant increase in hospitalization due to heart failure in Spain over 15 year period. Eur J Intern Med 2019;64:48–56. 10.1016/j.ejim.2019.02.019 [DOI] [PubMed] [Google Scholar]
- 44.Muñoz-Rivas N, Jiménez-García R, Méndez-Bailón M, et al. Type 2 diabetes increases the risk of hospital admission for heart failure and reduces the risk of in hospital mortality in Spain (2001-2015). Eur J Intern Med 2019;59:53–9. 10.1016/j.ejim.2018.08.011 [DOI] [PubMed] [Google Scholar]
- 45.Flores-Le Roux JA, Comin J, Pedro-Botet J, et al. Seven-Year mortality in heart failure patients with undiagnosed diabetes: an observational study. Cardiovasc Diabetol 2011;10:39. 10.1186/1475-2840-10-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carrasco-Sánchez FJ, Gomez-Huelgas R, Formiga F, et al. Association between type-2 diabetes mellitus and post-discharge outcomes in heart failure patients: findings from the Rica registry. Diabetes Res Clin Pract 2014;104:410–9. 10.1016/j.diabres.2014.03.015 [DOI] [PubMed] [Google Scholar]
- 47.Ribera A, Marsal JR, Ferreira-González I, et al. Predicting in-hospital mortality with coronary bypass surgery using hospital discharge data: comparison with a prospective observational study. Rev Esp Cardiol 2008;61:843–52. [PubMed] [Google Scholar]
- 48.Salinero-Fort MA, San Andrés-Rebollo FJ, Gómez-Campelo P, et al. Body mass index and all-cause mortality among type 2 diabetes mellitus patients: findings from the 5-year follow-up of the MADIABETES cohort. Eur J Intern Med 2017;43:46–52. 10.1016/j.ejim.2017.06.021 [DOI] [PubMed] [Google Scholar]
- 49.Johnston SS, Sheehan JJ, Shah M, et al. Cardiovascular event costs in patients with type 2 diabetes mellitus. J Med Econ 2015;18:1032–40. 10.3111/13696998.2015.1074078 [DOI] [PubMed] [Google Scholar]
- 50.Alvarez-Sabín J, Quintana M, Masjuan J, et al. Economic impact of patients admitted to stroke units in Spain. Eur J Health Econ 2017;18:449–58. 10.1007/s10198-016-0799-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjdrc-2019-001130supp001.pdf (309.4KB, pdf)