Abstract
The study’s objectives were to assess diagnostic stability of initial autism spectrum disorder (ASD) diagnoses in community settings and identify factors associated with diagnostic instability using data from a national Web-based autism registry. A Cox proportional hazards model was used to assess the relative risk of change in initial ASD diagnosis as a function of demographic characteristics, diagnostic subtype, environmental factors and natural history. Autistic disorder was the most stable initial diagnosis; pervasive developmental disorder—not otherwise specified was the least stable. Additional factors such as diagnosing clinician, region, when in time a child was initially diagnosed, and history of autistic regression also were significantly associated with diagnostic stability in community settings. Findings suggest that the present classification system and other secular factors may be contributing to increasing instability of community-assigned labels of ASD.
Keywords: Diagnosis stability, Children, Autism spectrum disorders, Community settings
Introduction
The objective of this study was to identify factors associated with the stability of initial autism spectrum disorder diagnoses in community settings. An estimated one in 110 children in the US is diagnosed with an autism spectrum disorder (ASD; Autism and Developmental Disabilities Monitoring Network 2006 Principal Investigators 2009; Kogan et al. 2009); this figure reflects a 10-fold increase in diagnoses during the past half century (Johnson et al. 2007). Given the recent increase in diagnosed prevalence in addition to changing diagnostic criteria and other secular trends, knowledge about stability of ASD diagnoses in community settings is an important avenue for further research (Fombonne 2009; Rosenberg et al. 2009). While past studies examining diagnostic stability in research settings have improved our understanding of the natural history of this group of disorders, this paper will focus on community settings to assess how ASD labels have changed within children over time. The following standard Diagnostic and Statistical Manual of Mental Disorders (4th ed., text revision) diagnoses (American Psychiatric Association [APA], 2000)—autistic disorder (AD), Asperger’s disorder (AS), and pervasive developmental disorder-not otherwise specified (PDD-NOS)—and the nonstandard diagnoses of autism spectrum disorder (‘ASD’) and pervasive developmental disorder (‘PDD’) will be used in this paper.
Findings from studies conducted in controlled research settings show that the ASDs are fairly stable neuropsychiatric disorders (Cederlund et al. 2008; Charman et al. 2005; Chawarska et al. 2007; Kleinman et al. 2008; Lord et al. 2006; Lord and Luyster 2006; Moss et al. 2008; Scambler et al. 2006; Turner et al. 2006; Turner and Stone 2007; van Daalen et al. 2009) with diagnostic stability (maintaining the same diagnosis within the autism spectrum at times 1 and 2) estimates ranging from 69% (Lord et al. 2006) to 95% (Charman et al. 2005). A recent study, the first on a genetically homogeneous ASD group (fragile X syndrome) found diagnostic stability during a 3-year period to be *60% for AD and 20% for PDD-NOS (Hernandez et al. 2009). A summary of ASD diagnostic stability studies published from 2005 to the present is provided in the “Appendix”. Collectively, these studies found AD to be the most stable diagnosis and PDD-NOS, the least stable (Cederlund et al. 2008; Charman et al. 2005; Chawarska et al. 2007; Kleinman et al. 2008; Lord et al. 2006; Moss et al. 2008; Turner and Stone 2007; van Daalen et al. 2009). Diagnostic stability has also been linked to age of initial evaluation, cognition and language ability, and participation in early intervention (Itzchak and Zachor 2009; Stone et al. 1999; Turner and Stone 2007).
While studies of diagnostic stability in research settings have expanded the knowledge base with respect to the natural history of the disorder, there remains a gap in the broader understanding of how the use of community-based labels of ASD change within children over time as well as characteristics that may be associated with these changes. Recent studies have provided some insight into ASD diagnostic practices in community settings (Rosenberg et al. 2009; Wiggins et al. 2006; Williams et al. 2009). A 2006 study examining diagnostic patterns in a population-based sample of 8-year-old children found initial ASD diagnosis to vary by setting; while most children were diagnosed in non-school settings, children initially diagnosed with autistic disorder and PDD-NOS were less likely to be diagnosed in a non-school setting compared with children initially diagnosed with Asperger’s and general ASD (Wiggins et al. 2006). In a recent study of the classification of ASDs in community settings, initial diagnosis was also found to vary by evaluation setting; when compared to early childhood programs and regional centers, school settings were significantly more likely to diagnose a child as having autism versus other diagnoses on the ASD spectrum (Williams et al. 2009). In an examination of trends in ASD diagnoses from 1994 through 2007 using a web-based registry of children with ASD, investigators found that initial ASD diagnosis varied by region, race/ethnicity, initial evaluator and secular time (Rosenberg et al. 2009). Specifically, AS was less likely to be diagnosed by developmental pediatricians and more likely to be diagnosed by psychiatrists or clinical psychologists, whereas ‘PDD’/’ASD’ was less likely to be diagnosed by clinical psychologists (Rosenberg et al. 2009). The study also showed that the proportion of children being diagnosed with specific ASD diagnoses changed over time, suggesting secular changes in clinician preferences for and use of ASD labels (Rosenberg et al. 2009).
Despite an improved understanding of factors associated with initial diagnoses of ASD in the community and the stability of diagnoses in research settings, no studies have examined the stability of these initial diagnoses in community settings. That is, once an initial diagnosis is made by any evaluator, how likely is the diagnosis to change within a given child, and what factors influence this likelihood? Assessing the stability of initial ASD diagnoses in community settings is important for a number of reasons. First, a lack of stability may be a reflection of poor initial diagnostic procedures or a lack of clinician training on how to recognize and diagnose the disorder. Second, instability in diagnoses of ASD may reflect variations in clinical practice and use of the ASD label across clinician types and locations. Lastly, although not a focus of this study, changes in community diagnoses may reflect true changes to the natural history of the disorder. In sum, assessing the prevalence of ASD label stability in community settings and factors associated with diagnostic instability have important research and practice implications, especially in the context of growing diagnosed prevalence and future changes in diagnostic criteria.
In an effort to address this gap, this study will build upon findings from Rosenberg and colleagues’ study and, using the same data source (Rosenberg et al. 2009), specifically a large sample (>7,000) of children with professionally-diagnosed ASD, assess and identify factors associated with the stability of initial ASD diagnoses in community settings over time. After controlling for child demographic and natural history characteristics, we hypothesize that initial diagnoses of AD will be more stable than initial diagnoses of PDD-NOS. Based on previous findings from studies examining community-based diagnoses of ASD (Rosenberg et al. 2009; Wiggins et al. 2006; Williams et al. 2009), we further expect type of initial diagnosing clinician, location of initial diagnosis and secular time of initial diagnosis to significantly affect diagnostic stability.
Methods
Data Source
Data for this study come from the Interactive Autism Network (IAN) Research database, a voluntary national (US) online registry for individuals with ASD and their families. Families are recruited to participate in IAN Research through a number of mechanisms including direct marketing, media campaigns and conferences, and through families’ interaction with clinicians, doctor’s offices and advocacy groups who have knowledge of the IAN Project. Individuals are eligible for IAN Research if they live in the United States and have been professionally diagnosed with an ASD, excluding Rett syndrome, as an online registry for this population already exists for Rett syndrome research. At registration, eligible parents consent for their child to participate and, if appropriate, affected children assent. As of February 2010, more than 11,000 children with ASD were registered in IAN Research. A more detailed description of the data source can be found at www.ianproject.org.
This study was approved by the Johns Hopkins Medical Institutions Institutional Review Board (#NA_00002750).
Sample
Children with an ASD diagnosis whose parents completed the Child with an ASD Questionnaire (“registered”) as of June 26, 2009, and ranged in age from 6 months to 18 years at the time of registration were included in this study (n = 7,106). Children with a first or current diagnosis of childhood disintegrative disorder (n = 16), a current diagnosis defined as “my child has fully recovered and no longer has an ASD (according to a professional)” (n = 42), or a missing a first or current diagnosis (n = 13) were excluded from the analysis. Children first diagnosed younger than age 6 months also were excluded from this study (n = 34). The mean age of the sample at the time of IAN registration was 7.6 years (SD = 3.9). Eighty-three percent of the sample was male (n = 5,869), 87% was White (n = 6,216), 3% was African-American, (n = 202), and 4% (n = 270) and 6% (n = 418) belonged to multiple and other racial groups, respectively. Eight percent of the sample was Hispanic (n = 582).
Measures
ASD Diagnoses
Diagnostic, developmental, and medical histories of children with ASD were extracted from the Child with an ASD Questionnaire (available at http://www.iancommunity.org/cs/ian_research_questions/child_with_asd_questionnaire). Parents were asked, “What was [display_name]’s FIRST autism spectrum disorder (ASD) diagnosis?” and were provided with the following options: “Autism or Autistic disorder”; “Asperger’s Syndrome”; “Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS)”; “Childhood Disintegrative Disorder (CDD)”; “Pervasive Developmental Disorder (‘PDD’) (choose only if none of the above apply)”; or “Autism Spectrum Disorder (‘ASD’) (choose only if none of the above apply).” Parents were then asked to provide information about when and where the diagnosis was made, and by whom. For this study, only children with a first or current diagnosis of AD, AS, PDD-NOS, ‘PDD’ or ‘ASD’ were included. ‘PDD’ and ‘ASD’ were combined into one category due to small sample size and on the basis that the groups were qualitatively similar when the relationships between ‘PDD’ and key risk factors and ‘ASD’ and key risk factors were compared (data not shown). An era of initial diagnosis variable was created using exact date of initial diagnosis and was divided into the following three categories (based loosely on major historical changes to the DSM): Before 1995, 1995–2001, and After 2001. Parents reported whether their child’s current diagnosis was different from his or her first diagnosis. If yes, they were asked to provide the current diagnosis and describe when and where the diagnosis was made, and by whom. Time to change in initial ASD diagnosis is the primary dependent variable of this study.
Demographic Characteristics
Information on gender, race, ethnicity, and location was obtained from parent report at registration. A mutually exclusive race variable using the following four categories was created: White, African American, Multiple, and Other. Information on mother’s highest level of education was obtained from the biological or adoptive mother report, and the following three categories were created: Up to high school graduate or equivalent, Some college or associate’s degree, and Bachelor’s degree or higher. The following urbanicity categories were created using the year 2000 rural-urban commuting area codes: Metropolitan, Micropolitan, and Small towns/rural (University of Washington 2009). A region variable was created using the United States Census Bureau Regions and Divisions and included the following categories: Northeast, Midwest, South, and West (United States Census Bureau 2009).
Natural History
Age of first concern was collapsed from 22 categories into the following three categories: Under 1 year; 1–2 years; and Over 2 years. Parents also were asked about skill loss; positive history of autistic regression was assigned for moderate to severe loss of social and/or communication skills prior to age 3.
Statistical Analyses
Means and proportions were calculated for each variable as a function of whether a child’s current diagnosis differed from his or her initial diagnosis, and differences were tested using Student’s t tests and χ2 tests. The relative risk of a change in ASD diagnosis was estimated using a Cox proportional hazards model. This is a type of survival model that compares the risk of change in diagnosis among participants using time until change in initial ASD diagnosis as the outcome variable (Cox 1972). The amount of time that individuals contribute to the analysis was defined by taking the difference between age at initial diagnosis and either (a) current age (i.e., age at registration) for those censored or not experiencing a change or (b) age at change in initial diagnosis.
Based on a review of existing literature, a preliminary multivariable model included era of initial diagnosis, age of initial diagnosis, initial ASD diagnosis, clinician assigning initial diagnosis and location of initial diagnosis. Demographic and natural history characteristics that were statistically related (p < .25) to change in ASD diagnosis were subsequently added to the model one at a time, after which likelihood ratio tests were performed to assess whether the addition of each new covariate improved model fit. All covariates improved the fit of the multivariable model except age of first concern, which was thus excluded. Potential collinearity was examined using the Variance Inflation Factor and was found not to be an issue (VIF < 2).
The proportional hazards assumption was assessed through examination of graphical displays of the survival function versus survival time (Kaplan-Meier curves) and Schoenfeld residuals of each covariate as well as covariate-specific and global tests of the proportional hazards assumption (Hosmer et al. 2008). All covariate-specific tests for proportionality as well as the global test on the multivariable model were non-significant, indicating that the proportional hazards assumption was acceptable. As an additional check for violation of the proportional hazards assumption, new variables modeling the interaction between each era of initial diagnosis category and log time were added to the model. A similar procedure was conducted with age of initial diagnosis categories, and the interaction terms were not significant. Taken together, these tests suggested that the proportional hazard assumption was not violated.
Kaplan-Meier survival curves were used to illustrate time to change in ASD diagnosis as a function of initial ASD diagnosis and era of initial ASD diagnosis categories. Log-rank tests were used to test the difference in the survival distributions by the aforementioned groups. All analyses were performed using Stata Statistical Software, Version 10.0 (StataCorp., College Station, TX, 2007).
Results
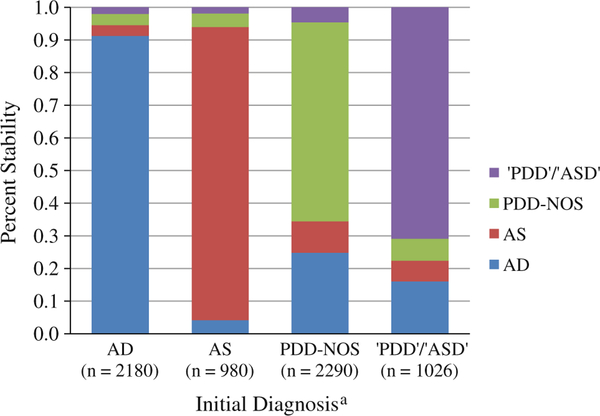
Of the entire sample (n = 7,106), 22% had a current ASD diagnosis that differed from their first (n = 1,540). The distribution of current diagnoses by initial diagnosis is presented in Fig. 1. Of children with an initial AD diagnosis (n = 2,810), 9% (n = 264) had a different current diagnosis, most commonly PDD-NOS (n = 96). Of children with an initial AS diagnosis (n = 980), 10% (n = 100) had a different current diagnosis, most commonly AD (n = 41) and PDD-NOS (n = 41). Of children with an initial PDD-NOS diagnosis (n = 2,290), 39% (n = 895) had a different current diagnosis, most commonly AD (n = 568). Finally, of children with an initial ‘PDD’/’ASD’ diagnosis (n = 1,026), 29% (n = 299) had a different current diagnosis, most commonly AD (n = 165).
Fig. 1.
Unadjusted distribution of current ASD diagnosis by initial ASD diagnosis. a AD = autism or autistic disorder; AS = Asperger’s syndrome; PDD-NOS = pervasive developmental disorder-not otherwise specified; ‘PDD’ = pervasive developmental disorder; ‘ASD’ = autism spectrum disorder
In the unadjusted analyses (Table 1), children who experienced a change in initial ASD diagnosis were on average 1.5 years older (p < .001) and were less likely to be female (p = .040). These children were also more likely to have mothers with at least a bachelor’s-level education (p = .044), and be from the Northeast or Southern regions of the US (p = .013). With respect to diagnostic history, a change in initial ASD diagnosis was less likely in children diagnosed after 2001 (p < .001) and more likely in children diagnosed before age 4 (p < .001). Children with an initial diagnosis of PDD-NOS or ‘PDD’/’ASD’ were also significantly more likely to experience a change initial diagnosis (p < .001). Children whose diagnosis changed were less likely to have been initially diagnosed by a team of health professionals, developmental pediatrician, or clinical psychologist and more likely to have been diagnosed by a pediatrician, psychiatrist, neurologist, or speech and language pathologist (p < .001). Children with a history of autistic regression were significantly more likely to experience a change in initial ASD diagnosis (p = .005).
Table 1.
Characteristics of children with current autism spectrum disorder (ASD) diagnosis
| No change in ASD diagnosis (n = 5,566) | Change in ASD diagnosis (n = 1,540) | p Value | |
|---|---|---|---|
| Demographic characteristics | |||
| Current age in years, mean (SD) | 7.3 (3.8) | 8.8 (4.0) | <.001 |
| Females | 18% | 16% | .040 |
| Race | |||
| White | 87% | 89% | .067 |
| African American | 3% | 3% | |
| Multiple | 4% | 3% | |
| Other | 6% | 5% | |
| Hispanic | 8% | 8% | .287 |
| Mother’s highest level of education (n = 6,629) | |||
| ≤High school diploma | 13% | 11% | .044 |
| Associate’s degree or some college | 39% | 37% | |
| ≥Bachelor’s degree | 48% | 52% | |
| Urbanicity (n = 7,043) | |||
| Metropolitan | 84% | 85% | .450 |
| Micropolitan | 9% | 8% | |
| Small town | 7% | 7% | |
| US region | |||
| Northeast | 25% | 27% | .013 |
| Midwest | 23% | 22% | |
| South | 34% | 35% | |
| West | 18% | 16% | |
| Autism spectrum disorder history | |||
| Era of initial diagnosis | |||
| After 2001 | 85% | 68% | <.001 |
| 1995–2001 | 13% | 28% | |
| Before 1995 | 2% | 4% | |
| Age of initial diagnosis | |||
| Under 4 years | 47% | 51% | <.001 |
| 4–8 years | 44% | 42% | |
| Over 8 years | 9% | 6% | |
| Initial ASD diagnosisb | |||
| AD | 46% | 16% | <.001 |
| AS | 16% | 6% | |
| PDD-NOS | 25% | 58% | |
| ‘PDD’/‘ASD’ | 13% | 19% | |
| Clinician(s) assigning initial diagnosis | |||
| Team of health professionals | 15% | 10% | <.001 |
| Pediatrician | 4% | 6% | |
| Developmental pediatrician | 22% | 20% | |
| Psychiatrist | 9% | 10% | |
| Clinical psychologist | 19% | 17% | |
| Neurologist | 15% | 20% | |
| Team of professionals in a school system | 10% | 10% | |
| Speech and language pathologist | 1% | 2% | |
| Other | 5% | 5% | |
| Location of initial ASD diagnosis (n = 7,101) | |||
| Health care system | 63% | 61% | .161 |
| Public school system | 10% | 10% | |
| Early intervention program | 15% | 17% | |
| Other | 11% | 12% | |
| Natural history | |||
| Age of first concern (n = 7,075) | |||
| Under 1 year | 25% | 28% | .008 |
| 1–2 years | 62% | 61% | |
| Over 2 years | 13% | 11% | |
| History of autistic regression (n = 7,103) | 27% | 31% | .005 |
Information available on entire sample (n = 7,106) unless otherwise specified
AD = autism or autistic disorder; AS = Asperger’s syndrome; PDD-NOS = pervasive developmental disorder—not otherwise specified; ‘PDD’ = pervasive developmental disorder; ‘ASD’ = autism spectrum disorder
Table 2 presents results from the adjusted Cox regression analysis. Children who were initially diagnosed before 1995 and from 1995 to 2001 had a 32 and 29% decreased risk of experiencing a change in diagnosis as compared to children initially diagnosed after 2001, respectively (95% CI, 0.62, 0.81, and 0.51, 0.89). Living in the Southern or Western regions of the United States was associated with a 1.20 and 1.26 increased risk of a change in ASD diagnosis, respectively, as compared with living in the Northeast (95% CI, 1.13, 1.48, and 1.07, 1.49).
Table 2.
Adjusted relative risk (RR) of a change in autism spectrum disorder (ASD) diagnosis
| RR | 95% Confidence interval | p value | |
|---|---|---|---|
| Female | 0.88 | 0.76–1.01 | .069 |
| Mother’s highest level of education | |||
| ≤High school diploma | 1.00 | - | - |
| Associate’s degree or some college | 1.02 | 0.86–1.22 | .807 |
| ≥Bachelor’s degree | 0.99 | 0.84–1.18 | .943 |
| Race | |||
| White | 1.00 | - | - |
| African American | 1.01 | 0.75–1.35 | .944 |
| Multiple | 1.00 | 0.75–1.35 | .955 |
| Other | 0.88 | 0.68–1.13 | .313 |
| US region | |||
| Northeast | 1.00 | - | - |
| Midwest | 1.15 | 0.99–1.34 | .076 |
| South | 1.29 | 1.13–1.48 | <.001 |
| West | 1.26 | 1.07–1.49 | .007 |
| Era of initial diagnosis | |||
| After 2001 | 1.00 | - | - |
| 1995–2001 | 0.71 | 0.62–0.81 | <.001 |
| Before 1995 | 0.68 | 0.51–0.89 | .005 |
| Initial ASD diagnosisa | |||
| AD | 1.00 | - | - |
| AS | 1.34 | 1.04–1.74 | .026 |
| PDD-NOS | 5.65 | 4.86–6.57 | <.001 |
| ‘PDD’/‘ASD’ | 4.63 | 3.88–5.52 | <.001 |
| Age of initial diagnosis | |||
| Under 4 years | 1.00 | - | - |
| 4—8 years | 0.92 | 0.82–1.03 | .133 |
| Over 8 years | 1.00 | 0.78–1.27 | .989 |
| Clinician(s) assigning initial diagnosis | |||
| Team of health professionals | 1.00 | - | - |
| Pediatrician | 1.73 | 1.31–2.29 | <.001 |
| Developmental pediatrician | 1.39 | 1.13–1.69 | .001 |
| Psychiatrist | 1.67 | 1.33–2.11 | <.001 |
| Clinical psychologist | 1.38 | 1.11–1.69 | .003 |
| Neurologist | 1.47 | 1.21–1.80 | <.001 |
| Team of professionals in a school system | 1.32 | 1.01–1.72 | .040 |
| Speech and language pathologist | 1.55 | 1.07–2.04 | .020 |
| Other | 1.47 | 1.11–1.95 | .008 |
| Location of initial diagnosis | |||
| Healthy system | 1.00 | - | - |
| School system | 1.24 | 1.00–1.55 | .052 |
| Early intervention | 1.11 | 0.95–1.30 | .181 |
| Other | 1.02 | 0.86–1.20 | .833 |
| History of autistic regression | 1.15 | 1.02–1.29 | .022 |
AD = autism or autistic disorder; AS = Asperger’s syndrome; PDD-NOS = pervasive developmental disorder—not otherwise specified; ‘PDD’ = pervasive developmental disorder; ‘ASD’ = autism spectrum disorder
While children initially diagnosed with AS were modestly more likely to have a change in diagnosis compared to those with an initial AD diagnosis (RR1.34, 95% CI, 1.04,1.74), children initially diagnosed with PDD-NOS or ‘PDD’/’ASD’ were at much higher risk for diagnostic change (RR 5.65, 95% CI, 4.86, 6.87 and RR 4.63, 95% CI, 3.88, 5.52, respectively).
A significant increased risk in change in diagnosis was associated with every clinician type in comparison with an initial diagnosis made by a team of health professionals; relative risks ranged from 1.32 for teams of professionals in school systems to (95% CI, 1.01, 1.72) to 1.73 for pediatricians (95% CI, 1.31, 2.29). Finally, children who regressed were at 15% increased risk of experiencing a change in initial diagnosis compared to children who did not regress (95% CI, 1.02, 1.29).
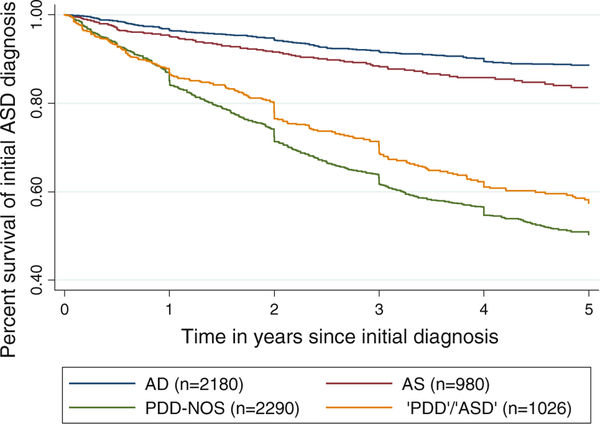
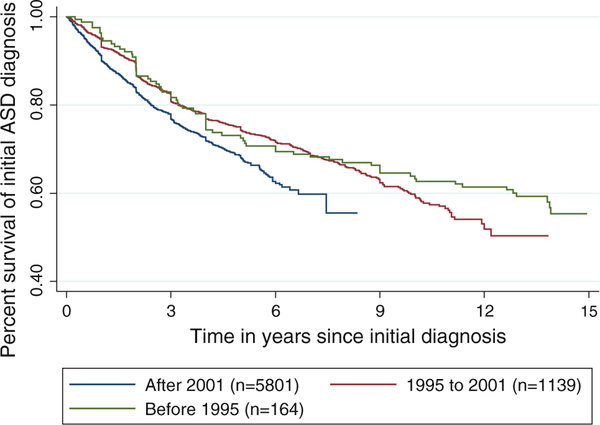
As seen in Fig. 2, the Kaplan-Meier survival curve of change in ASD diagnosis stratified by initial diagnosis shows significant differences in diagnostic survival (log-rank test p < .001). A test of the difference between survival curves between era of diagnosis categories (Fig. 3) indicates that the cumulative stability of an initial ASD diagnosis is significantly decreased for children diagnosed after 2001, as compared to children initially diagnosed prior to 1995 and between 1995 and 2001 (log-rank test p < .001).
Fig. 2.
Kaplan-Meier survival curve of time to change in initial ASD diagnosis by initial ASD diagnosis. AD = autism or autistic disorder; AS = Asperger’s syndrome; PDD-NOS = pervasive developmental disorder-not otherwise specified; ‘PDD’ = pervasive developmental disorder; ‘ASD’ = autism spectrum disorder
Fig. 3.
Kaplan-Meier survival curve of time to change in initial ASD diagnosis by era of initial diagnosis
Discussion
This study used data from a large, national web-based registry to identify factors associated with the stability of initial community-based diagnoses of ASD among children on the autism spectrum. Twenty-two percent of participants had a current diagnosis that was different from their initial diagnosis, consistent with the range of stability estimates reported in past clinical studies (Cederlund et al. 2008; Charman et al. 2005; Chawarska et al. 2007; Kleinman et al. 2008; Lord et al. 2006; Moss et al. 2008; Turner and Stone 2007).
Confirming the first hypothesis and consistent with past studies conducted in research settings, ASD label stability depended in part on specific initial diagnosis, and PDD-NOS was the least stable. The high rate of instability among an initial diagnosis of PDD-NOS is not entirely surprising given the ambiguous and widely debated nature of the American Psychiatric Association’s current DSM-IV-TR criteria, as well as changes in criteria between DSM-IV (APA, 1994) and DSM-IV-TR (APA 2000) (Bristol et al. 1996; Mahoney et al. 1998; Szatmari 2000; Walker et al. 2004). Another possible explanation for the low diagnostic stability of both PDD-NOS and ‘PDD’/’ASD’ may be that clinicians are assigning either diagnosis as a “placeholder” for patients with mild or atypical ASD, particularly those younger than 5 years, waiting to see how the child develops and/or responds to early intervention and thus anticipating a label change.
The adjusted decreased stability of AS compared with an initial AD diagnosis may be due to the recent addition of AS to the DSM-IV (APA 1994). A later mean age of initial diagnosis may explain some of the relative stability of a first AS diagnosis compared to the initial diagnoses of PDD-NOS or ‘PDD’/’ASD’; while the mean age of initial diagnosis for AS in this sample was 7.1 years, compared with 3.7 and 3.4 years for PDD-NOS and ‘PDD’/’ASD’, respectively, age of initial diagnosis was not significant in the multivariable model. An additional explanation for the relatively high stability of AS in comparison with other ASD diagnoses could be that parents or clinicians prefer a diagnosis of AS to other ASDs, most notably autism, because they believe that AS is associated with a more positive outcome.
The second hypothesis, which purported that diagnostic stability in community settings would vary as a function of the clinician assigning the initial diagnosis, setting of initial diagnosis and secular time, was supported by these results. In this study, an initial diagnosis by any other evaluator, in comparison with one assigned by a team of health professionals, was associated with an increased risk of a change in initial ASD diagnosis, although most experts recommend evaluation by a team of health professionals (Charman and Baird 2002; Johnson et al. 2007). Possible explanations for this finding may be that timely access to professional teams is limited and teams often assess children at later stages in the natural history of ASD and hence later chronological ages than alternative evaluators; however, there was no statistical difference in age at initial diagnosis by diagnostic change status.
Alternatively, health care team diagnoses may truly be more “accurate” because of the increased sensitivity and specificity resulting from multiple sources of information/observation. A recent study on the assessment of ASD in community settings found that a majority of professionals did not follow best practices or use diagnostic instruments when assigning initial diagnosis (Williams et al. 2009; Wiggens et al. 2009). Variation in clinician practices may help to explain relative differences in the stability of community labels of ASD across clinician types when compared to those assigned by a team of health professionals.
While the present study did not find difference in diagnostic stability in community-settings by physical location of initial ASD diagnosis, most likely a result of confounding by diagnosing clinician, stability of initial ASD diagnosis did vary as a function of geographic setting. Children living in the US South and West regions were significantly more likely to experience a change in initial ASD diagnosis as compared with children living in the Northeast. These differences may depend in part on regional variations in population sociodemographic characteristics, diagnostic facilities, evaluator preferences, and secular trends in diagnostic nosology as reported previously (Rosenberg et al. 2009).
Findings from this study suggest that secular time may be influencing the stability of initial ASD diagnoses in community settings. Results of the Kaplan-Meier curve of time to change in ASD diagnosis stratified by era of initial diagnosis and adjusted Cox analysis show that there are changes over time in the stability of initial diagnoses in community settings, with children who were diagnosed most recently (after 2001) being more susceptible to diagnostic instability. One possible explanation for this finding is that children diagnosed around the time of the publication of DSM-IV-TR (APA 2000) may have been reassigned up to several years after the change in diagnostic criteria, depending on how long it took to disseminate the new guidelines. Another possibility is that children were reassigned based on secular trends in diagnosis, as different specific diagnoses have become more popular (such as ‘ASD’) while others (such as PDD-NOS) may be less so (Rosenberg et al. 2009). A more likely explanation for this finding is that children are initially diagnosed at younger ages than they were in the recent past (Autism and Developmental Disabilities Monitoring Network 2006 Principal Investigators 2009), leading to longer intervals for natural history changes and/or early intervention, which then may impact ultimate diagnosis. Interestingly, after adjusting for other factors, chronological age at initial diagnosis was no longer significantly associated with change in initial diagnosis. This finding could suggest that factors such as when in time a child was diagnosed may play a greater role in predicting diagnostic stability than the age at which a child was diagnosed. However, it is likely that a number of additional factors, such as initial ASD diagnosis and history of autistic regression played a role in the attenuation of the observed relationship between age of initial diagnosis and diagnostic stability.
Current standards of care for ASD diagnosis incorporate information on developmental milestones, including the presence of autistic regression (Filipek et al. 2000). In this study children who had a history of regression were at greater risk for a change in initial diagnosis as compared to children who did not. Given that children who experience regression have a more labile developmental trajectory, it is not entirely surprising that diagnosing children around the time they experience regression would result in an increased likelihood that their diagnosis may change after such time as their developmental course stabilizes.
Limitations
Although this is the largest study to date of changes in ASD stability in community settings over time, the novel form of data collection—parent-reported Web-based registry—does necessitate some caution in interpreting the results. Nonetheless, the validity and reliability of Internet-based research have been extensively studied and supported (Evans and Mathur 2005; Gosling et al. 2004; Huang 2006; Wilson and Laskey 2003). Parent-reported ASD diagnoses have been validated against the Social Communication Questionnaire (Rutter et al. 2003), which also is administered to families via IAN Research. A previous study showed sensitivity of parent-reported ASD diagnoses in this sample to range from 91% for AS to 95% for AD, using ASD screens as the gold standard (Rosenberg et al. 2009). In addition, preliminary results of the IAN Research Diagnosis Validation study, which uses a clinical record review to validate parent-reported diagnoses, show that >98% of IAN parents are able to corroborate their child’s ASD diagnosis. Furthermore, while the validity of ASD diagnoses is a common concern in the research community, this study is not the first to produce findings from parent-report data (i.e. National Survey of Children’s Health; US Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau, 2009).
Since parents provide data on initial and current diagnoses rather than all interim diagnoses, it is possible that children whose current diagnosis is the same as their first diagnosis may have had a change in diagnosis several times in between these two time points. Conversely, children whose current diagnosis is different from their first may have had several changes to their diagnostic label between these two time points. Similarly, among children whose parents reported no change, the extent to which this reflects a “stable” diagnosis or rather the result of a single assessment is unknown because the children may not have been reevaluated; the interval between diagnoses is also not standardized as it might be in a research setting (i.e., every 12 months). Additionally, a change in ASD diagnosis, as a function of the type and quantity of services received is an important question from both a public health and policy perspective and deserves further study; this study did not address the association between service use and diagnostic stability in this analysis. Similarly, because our data are based on only those currently with an ASD, we were unable to examine patterns off the spectrum. However, ongoing data collection within IAN may address some of these constraints with time.
Last, there are concerns about selection bias and generalizability. Although Web-based data collection is likely to reduce or at least achieve results that are no more biased than center-based studies (Gosling et al. 2004), they are skewed toward certain populations (e.g., White or higher socioeconomic status), and individuals who participate in research are likely different from those who choose not to participate, therefore limiting the generalizability of our findings. Nonetheless, the use of the Internet has allowed IAN to gather information on a large sample of children with ASD and their families from throughout the country and presumably among families who were previously precluded from participating in research because of geography.
Conclusion
Findings from this study are consistent with past research that suggest ASD diagnostic stability in community settings depends in large part on the specific initial ASD diagnosis (Cederlund et al. 2008; Charman et al. 2005; Chawarska et al. 2007; Kleinman et al. 2008; Lord et al. 2006; Moss et al. 2008; Turner and Stone 2007). This study has expanded the research base with respect to changes in ASD diagnoses assigned in the community as well as additional factors that may contribute to diagnostic instability, such as type of initial evaluator. Finally, there is also evidence to suggest that community labels of ASD are becoming less stable over time.
Acknowledgments
This study was supported by Autism Speaks. The funder had no role in determining content. We thank Ms. Teresa Foden for providing assistance with editing and Mr. Alden Gross and Ms. Janet Kuramoto for their assistance with the statistical analyses. We gratefully acknowledge the contributions of IAN families without which this research would not be possible.
Appendix
See Table 3.
Table 3.
Summary of ASD diagnostic stability studies published from 2005 through 2009
| Study | Total N | Age | Measurea | Diagnosisb | N | Stability, %c | ||
|---|---|---|---|---|---|---|---|---|
| Time 1 | Time 2 | Time 1 | Time 2 | |||||
| Charman et al. (2005) | 20 | 2 years | 7 years | ADI-R | AD | AD | 19 | 95 |
| ADOS | AD | PDD-NOS | 1 | |||||
| Clinical diagnosis (ICD-10) | ||||||||
| Lord et al. (2006) | 124 | 2 years | 9 years | ADI-R | AD | AD | 71 | 69 |
| ADOS | AD | PDD-NOS | 12 | |||||
| Clinical diagnosis | PDD-NOS | PDD-NOS | 14 | |||||
| PDD-NOS | AD | 27 | ||||||
| Turner et al. (2006) | 22 | 2 years | 9 years | ADI-R | AD | AD | 16 | 82 |
| ADOS-G | PDD-NOS | AD | 3 | |||||
| PDD-NOS | PDD-NOS | 2 | ||||||
| PDD-NOS | AS | 1 | ||||||
| Chawarska et al. (2007) | 31 | <2 years | 3 years | ADI-R | AD | AD | 19 | 81 |
| ADOS-G | AD | PDD-NOS | 2 | |||||
| Clinical diagnosis | PDD-NOS | PDD-NOS | 6 | |||||
| DD | DD | 3 | ||||||
| DD | PDD-NOS | 1 | ||||||
| Turner and Stone (2007) | 30 | 2 years | 4 years | ADI-R | AD | AD | 20 | 77 |
| ADOS | AD | PDD-NOS | 6 | |||||
| Clinical diagnosis | PDD-NOS | PDD-NOS | 3 | |||||
| PDD-NOS | AS | 1 | ||||||
| Cederlund et al. (2008) | 131 | >5 years | 16–38 years | Clinical diagnosis | AS | AS | 52 | 84 |
| DISCO | AS | Atypical | 3 | |||||
| AS | AD | 7 | ||||||
| AD | AD | 58 | ||||||
| AD | Atypical | 11 | ||||||
| Kleinman et al. (2008) | 46 | 16–35 months | 42–82 months | ADI-R | AD | AD | 32 | 80 |
| ADOS | AD | PDD-NOS | 7 | |||||
| CARS | PDD-NOS | PDD-NOS | 5 | |||||
| Clinical diagnosis | PDD-NOS | AD | 2 | |||||
| (DSM-IV) | ||||||||
| Moss et al. (2008) | 30 | 3.5 years | 10.5 years | ADI-R | AD | AD | 28 | 93 |
| AD | ASD | 2 | ||||||
| van Daalen et al. (2009) | 46 | 23 months | 42 months | ADOS-G | AD | AD | 25 | 70 |
| Clinical diagnosis | AD | PDD-NOS | 13 | |||||
| PDD-NOS | PDD-NOS | 7 | ||||||
| PDD-NOS | AD | 1 | ||||||
ADI-R = Autism Diagnostic Interview—Revised; ADOS = Autism Diagnostic Observation Schedule; ICD-10 = International Classification of Disease-10; ADOS-G = Autism Diagnostic Observation Schedule-Generic; DISCO = Diagnostic Interview for Social and Communication Disorder; CARS = Childhood Autism Rating Scale; DSM-IV = Diagnostic and Statistical Manual (4th ed.)
AD = autistic disorder; PDD-NOS = pervasive developmental disorder—not otherwise specified; AS = Asperger’s syndrome; DD = developmental delay; ASD = autism spectrum disorder
Stability, % refers to keeping the same ASD diagnosis at Time 1 and Time 2
Contributor Information
Amy M. Daniels, Department of Medical Informatics, Kennedy Krieger Institute, 3825 Greenspring Avenue, Painter Building 1st Floor, Baltimore, MD 21211, USA Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA.
Rebecca E. Rosenberg, Department of Medical Informatics, Kennedy Krieger Institute, 3825 Greenspring Avenue, Painter Building 1st Floor, Baltimore, MD 21211, USA
J. Kiely Law, Department of Medical Informatics, Kennedy Krieger Institute, 3825 Greenspring Avenue, Painter Building 1st Floor, Baltimore, MD 21211, USA; Department of Pediatrics, Johns Hopkins University School of Medicine, Johns Hopkins Medical Institutions, Baltimore, MD, USA.
Catherine Lord, University of Michigan Autism and Communication Disorders Center (UMACC), University of Michigan, Ann Arbor, MI, USA.
Walter E. Kaufmann, Center for Genetic Disorders of Cognition & Behavior, Kennedy Krieger Institute, Baltimore, MD, USA Departments of Pathology, Neurology, Pediatrics, Psychiatry, and Radiology, Johns Hopkins University School of Medicine, Johns Hopkins Medical Institutions, Baltimore, MD, USA.
Paul A. Law, Department of Medical Informatics, Kennedy Krieger Institute, 3825 Greenspring Avenue, Painter Building 1st Floor, Baltimore, MD 21211, USA Department of Pediatrics, Johns Hopkins University School of Medicine, Johns Hopkins Medical Institutions, Baltimore, MD, USA.
References
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington, DC: American Psychiatric Association. [Google Scholar]
- Autism and Developmental Disabilities Monitoring Network 2006 Principal Investigators. (2009). Prevalence of autism spectrum disorders—Autism and developmental disabilities monitoring network, United States, 2006. Morbidity and Mortality Weekly Report, 58(SS-10), 1–21. [PubMed] [Google Scholar]
- Bristol MM, Cohen DJ, Costello EJ, Denckla M, Eckberg TJ, Kallen R, et al. (1996). State of the science in autism: Report to the National Institutes of Health. Journal of Autism and Developmental Disorders, 26(2), 121–154. [DOI] [PubMed] [Google Scholar]
- Cederlund M, Hagberg B, Billstedt E, Gillberg IC, & Gillberg C (2008). Asperger’s syndrome and autism: A comparative longitudinal follow-up study more than four years after original diagnosis. Journal of Autism and Developmental Disorders, 38, 72–85. [DOI] [PubMed] [Google Scholar]
- Charman T, & Baird G (2002). Practitioner review: Diagnosis of autism spectrum disorder in 2- and 3-year-old children. Journal of Child Psychology and Psychiatry, 43(3), 289–305. [DOI] [PubMed] [Google Scholar]
- Charman T, Taylor E, Drew A, Cockerill H, Brown J, & Baird G (2005). Outcome at 7 years of children diagnosed with autism at age 2: Predictive validity of assessments conducted at 2 and 3 years of age and pattern of symptom change over time. Journal of Child Psychology and Psychiatry, 46(5), 500–513. [DOI] [PubMed] [Google Scholar]
- Chawarska K, Klin A, Paul R, & Volkmar F (2007). Autism spectrum disorder in the second year: Stability and change in syndrome expression. Journal of Child Psychology and Psychiatry, 48(2), 128–138. [DOI] [PubMed] [Google Scholar]
- Cox DR (1972). Regression models and life-tables. Journal of the Royal Statistical Society. Series B (Methodological), 34(2), 187220. [Google Scholar]
- Evans JR, & Mathur A (2005). The value of online surveys. Internet Research, 15(2), 195–219. [Google Scholar]
- Filipek PA, Accardo PJ, Ashwal S, Baranek GT, Cook EH, Dawson G, et al. (2000). Practice parameter: Screening and diagnosis of autism: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Child Neurology Society. Neurology, 55(4), 468–479. [DOI] [PubMed] [Google Scholar]
- Gosling SD, Vasire S, Srivastava S, & John OP (2004). Should we trust Web-based studies? A comparative analysis of six preconceptions about the Internet questionnaires. AmericanPsychologist, 59(2), 93–104. [DOI] [PubMed] [Google Scholar]
- Hernandez RN, Feinberg RL, Vaurio R, Passanante NM, Thompson RE, & Kaufmann WE (2009). Autism spectrum disorder in fragile x syndrome: A longitudinal evaluation. American Journal of Medical Genetics, Part A, 149A, 11251137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S, & May S (2008). Applied survival analysis: Regression modeling of time to event data (2nd ed.). New York: Wiley-Interscience. [Google Scholar]
- Huang H (2006). Do print and web surveys provide the same results? Computers in Human Behavior, 22, 334–350. [Google Scholar]
- Itzchak EB, & Zachor DA (2009). Changes in autism classification with early intervention: Predictors and outcomes. Research in Autism Spectrum Disorders, 3, 967–976. [Google Scholar]
- Johnson CP, Myers SM, & The Council on Children with Disabilities. (2007). Clinical report: Identification and evaluation of children with autism spectrum disorders. Pediatrics, 120(5), 1183–1215. [DOI] [PubMed] [Google Scholar]
- Kleinman JM, Ventola PE, Pandy J, Verbalis AD, Barton M, Hodgson S, et al. (2008). Diagnostic stability in very young children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 38, 606–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogan MD, Blumberg SJ, Schieve LA, Boyle CA, Perrin JM, Ghandour RM, et al. (2009). Prevalence of parent-reported diagnosis of autism spectrum disorder among children in the US, 2007. Pediatrics, 124(4), 1–9. [DOI] [PubMed] [Google Scholar]
- Lord C, & Luyster R (2006). Early diagnosis of children with autism spectrum disorders. Clinical Neuroscience Research, 6, 189–194. [Google Scholar]
- Lord C, Risi S, DiLavor PS, Shulman C, Thurn A, & Pickles A (2006). Autism from 2 to 9 years of age. Archives of General Psychiatry, 63, 694–701. [DOI] [PubMed] [Google Scholar]
- Mahoney W, Szatmari P, Maclean JE, Bryson SE, Bartolucci G, Walter SD, et al. (1998). Reliability and accuracy of differentiating between pervasive developmental disorder subtypes. Journal ofthe American Academy of Child and Adolescent Psychiatry, 37(3), 278–285. [DOI] [PubMed] [Google Scholar]
- Moss J, Magiati I, Charman T, & Howlin P (2008). Stability of the Autism diagnostic interview-revised from pre-school to elementary school age in children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 38, 1081–1091. [DOI] [PubMed] [Google Scholar]
- Rosenberg RE, Daniels AM, Law JK, Law PA, & Kaufmann WE (2009). Trends in autism spectrum disorder diagnoses: 1994–2007. Journal of Autism and Developmental Disorders, 39(8), 1099–1111. [DOI] [PubMed] [Google Scholar]
- Rutter M, Bailey A, & Lord C (2003). Social communication questionnaire (SCQ). Los Angeles: Western Psychological Services. [Google Scholar]
- Scambler DJ, Hepburn SL, & Rogers SJ (2006). A two-year follow-up on risk status identified by the checklist for Autism in Toddlers. Journal of Developmental and Behavioral Pediatrics, 27(2), S104–S110. [DOI] [PubMed] [Google Scholar]
- StataCorp. (2007). Stata statistical software (Release 10) [Computer software]. College Station, TX: StataCorp LP. [Google Scholar]
- Stone WL, Lee EB, Ashford L, Brissie J, Hepburn SL, Coonrod EE, et al. (1999). Can autism be diagnosed accurately in children under three years? Journal of Child Psychology and Psychiatry, 40, 219–226. [PubMed] [Google Scholar]
- Szatmari P (2000). The classification of autism, Asperger’s syndrome, and pervasive developmental disorder. Revue Canadienne de Psychiatrie, 45(8), 731–738. [DOI] [PubMed] [Google Scholar]
- Turner LM, & Stone WL (2007). Variability in outcome for children with ASD diagnosis at age 2. Journal of Child Psychology and Psychiatry, 48(8), 793–802. [DOI] [PubMed] [Google Scholar]
- Turner LM, Stone WL, Pozdol SL, & Coonrod EE (2006). Follow-up of children with autism spectrum disorders from age 2 to age 9. Autism, 10, 243–264. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. (2009). Census regions and divisions of the United States. Retrieved February 1, 2009, from http://www.census.gov/geo/www/us_regdiv.pdf. [Google Scholar]
- U.S. Department of Health, Human Services, Health Resources, Services Administration, Maternal, Child Health Bureau. (2009). The National Survey of Children’s Health 2007. Rockville, Maryland: U.S. Department of Health and Human Services. [Google Scholar]
- University of Washington. (2009). Rural health research center rural-urban commuting area codes. Retrieved February 1, 2009, from http://depts.washington.edu/uwruca/download2006.html.
- van Daalen E, Kemner C, Dietz C, Swinkles SHN, Buitelaar JK, & van Engeland H (2009). Inter-rater reliability and stability of diagnoses of autism spectrum disorder in children identified through screening at very young age. European Child and Adolescent Psychiatry, 18, 663–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker DR, Thompson A, Zwaigenbaum L, Goldberg J, Bryson SE, Mahoney WJ, et al. (2004). Specifying PDD-NOS: A comparison of PDD-NOS, Asperger syndrome, and autism. Journal of the American Academy of Child and Adolescent Psychiatry, 43(2), 172–180. [DOI] [PubMed] [Google Scholar]
- Wiggins LD, Baio J, & Rice C (2006). Examination of the time between first evaluation and first autism spectrum diagnosis in a population—based sample. Developmental and Behavioral Pediatrics, 27(2), S79–S87. [DOI] [PubMed] [Google Scholar]
- Williams ME, Atkins M, & Soles T (2009). Assessment of Autism in community settings: Discrepancies n classification. Journal of Autism and Developmental Disorders, 39, 660–669. [DOI] [PubMed] [Google Scholar]
- Wilson A, & Laskey N (2003). Internet based marketing research: A serious alternative to traditional research methods? Marketing Intelligence & Planning, 21(2), 79–84. [Google Scholar]