Abstract
Plasma is an ionized gas. It is typically formed at high temperature. As a result of both the development of low-temperature plasma sources and a better understanding of complex plasma phenomena over the last decade, “plasma medicine” has become a booming interdisciplinary research topic of growing importance that explores enormous opportunities at the interface of chemistry, plasma physics, and biomedical sciences with engineering. This review presents the latest development in plasma medicine in the area of the central nervous system and aims to introduce cutting-edge plasma medicine to clinical and translational medical researchers and practitioners.
Keywords: Cold plasma, Plasma medicine, Neuroscience, ROS/RNS
Main text
What is plasma?
If we mention the word “plasma,” the first thing a doctor might think of would be the yellowish liquid component of blood that normally suspends the blood cells in suspension. Of course, that definition is correct. However, a more common description for plasma should be a quasi-neutral gas of neutral and charged particles that exhibit collective behavioral pattern, which is also the most bountiful phase of matter in the vast expanse of the universe.
From the perspective of physics, plasma is regarded as the fourth state of matter along with solids, gases, and liquids. Plasma is the least recognized, but the most widespread form of the fourth state of matter, comprising more than 99% of the universe. Plasmas are in fact a “cosmic soup” of freely moving and fixed atoms, molecules, ions, and electrons of a variety of densities as well as temperatures ranging from cold to extremely hot (Fig. 1). Plasmas are highly conductive and can respond to magnetic and electric fields; thus, it can serve as an efficient energy source.
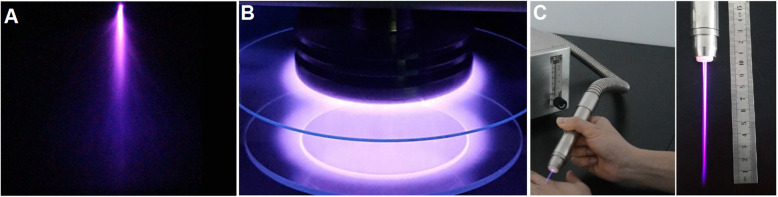
Fig. 1.
Four states of matter and various plasmas. Plasmas comprise charged and freely moving particles, such as electrons and ions. Plasmas are generated under high temperatures when electrons are detached from neutral atoms. Plasmas are prevalent in nature. For example, stars are mainly plasma. Due to unique physical properties, plasmas are indeed the “fourth state of matter” as distinguished from gases, solids, and liquids. Temperatures and densities of plasma vary extensively (use for reference from “Fusion - Physics of a fundamental energy source, Plasmas - the fourth state of matter, Characteristics of typical plasmas” at http://FusEdWeb.llnl.gov/CPEP/)
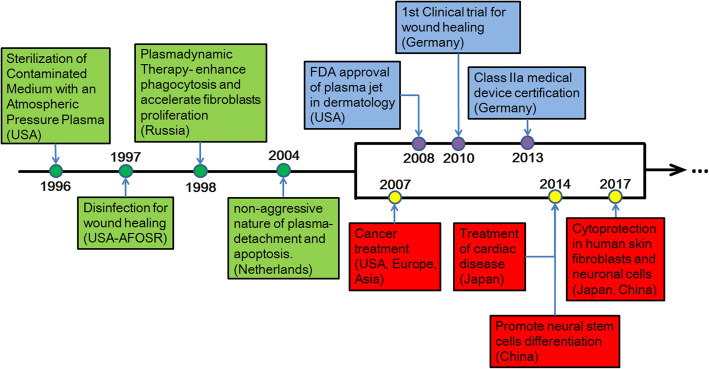
The majority of plasma forms, such as lightning, stars, and the sun, cannot be easily tested because they are tremendously hot or “superheated” and are difficult to handle. However, recently, researchers have been developing techniques to manufacture non-thermal plasmas that can be operated at atmospheric pressure and room temperature. One of the most important features is the non-equilibrium in that electrons are as hot as 104 K or above, but ions and neutrals are cool at approximately 300 K. The less dense forms of plasma at lower temperature are interrelated to auroras and stellar and solar winds. Moreover, the plasma produced by glow discharge results in the phenomena of colored light in the sky which are Aurora Australis in the southern hemisphere and Aurora Borealis in the northern hemisphere. In the laboratory, we also usually get plasma in the form of gas discharge. Typical electrical discharges that produce cold plasma at atmospheric pressure include corona, dielectric barrier discharge (DBD) and atmospheric-pressure plasma jet (APPJ) [1], and some other plasma sources (Fig. 2).
Fig. 2.
Typical measures to produce cold plasma at atmospheric pressure include corona (a), DBD (b), and APPJ (c)
Historical perspective of plasma medicine
Some previous applications of plasmas in the medicine industry were mainly on the basis of its thermal effects [2]. It has been decades since the clinical use of thermal plasma, in which plasma is applied in for cauterization as well as blood coagulation, as exemplified in the argon plasma coagulator [3]. In the early and mid-1990s, with the development in the generation of plasma with low temperature, large volume, and atmospheric pressure, most plasma applications in the medicine industry were related to the more gentle and non-thermal effects for simple and convenient use [4].
In 1996, the sterilization effects of cold plasma were demonstrated [5]. Since then, the medical and biological applications of cold plasma have attracted increasing attention. Based on the potential use of plasmas in soldiers’ wounds treatment and sterilization of abiotic and biotic surfaces, in 1997, a proof of principle research program was financially supported by the Physics and Electronics Directorate of the US Air Force Office of Scientific Research (AFOSR), which lasted for over 10 years [4]. In the meantime, comparable studies carried out in Russia indicated that nitric oxide (NO) generated by plasma is of paramount importance in enhancing phagocytosis and speeding up the proliferation of fibroblasts [6]. This was referred to as “plasmadynamic therapy” of wounds by Russian researchers and was demonstrated in experiments both in vivo and in vitro [6]. In 2002 and 2004, researchers from the Netherlands identified the non-aggressiveness of the plasma, which could be applied to detach mammalian cells without leading to necrosis, and they found that in some conditions, low-temperature plasma can result in apoptosis (programmed cell death) [7, 8].
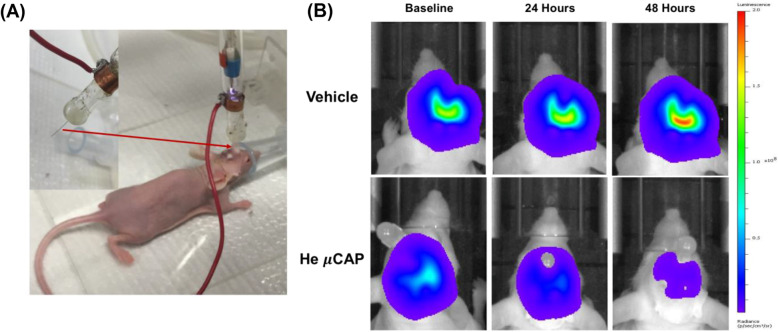
The aforementioned early breakthroughs in plasma studies by researchers paved the way for a nascent multidisciplinary field of study: the biomedical use of plasma at low temperature. By 2007, the International Conference on Plasma Medicine (ICPM), which was the first conference devoted to plasma medicine, was established and held every 2 years. In addition, the first workshop entirely committed to the applications of low-temperature plasma (LTP) in tumorous diseases, the International Workshop on Plasma for Cancer Treatment (IWPCT), was founded in 2014 [4]. Some important milestones were shown as a time line in Fig. 3, indicating the biomedical applications development of LTP, and a nascent field of study known today as “plasma medicine” was gradually formed, which mainly focused on the interaction between LTP and biological tissues, cells, and systems.
Fig. 3.
Timeline indicating some of the major breakthroughs in the nascent field of the biomedical applications of plasma at atmospheric pressure and low temperature. This timeline does not indicate the use of thermal plasmas, which have been employed for decades in medical applications that require heat, i.e., blood coagulation and cauterization (after Laroussi [9])
Basic knowledge on biological plasma effects
Plasma that lends itself to biomedical applications is mostly created in the open air. A number of reactive oxygen species (ROS) and reactive nitrogen species (RNS), like O, OH, O2−, O2 (1Δ), NO, and H2O2 (Fig. 4), are produced by the reaction of a small quantity of H2O, O2, and N2 with excited-state species, ions, and electrons in the plasma in the air. RNS and ROS are of importance in oxidation and reduction biochemistry in many living organisms with significant biological implications [11]. A previous publication by Yan et al. in 2012 reported that plasma treatment could lead to ROS and NO accumulation both intracellularly and extracellularly, which demonstrated a direct relationship between plasma physics and biology, as well as medicine [12]. Based on the biomedical interactions of ROS and RNS from plasma, plasma medicine covers a number of applications of LTP in medicine and biology, including sterilization, plasma-aided wound healing, plasma dentistry, plasma pharmacology, plasma oncology, and plasma treatment for implants to enhance biocompatibility. In the next section, the applications of plasma in neuro-protection, differentiation of neural stem cells, and tumors, particularly the glioma, will be summarized.
Fig. 4.
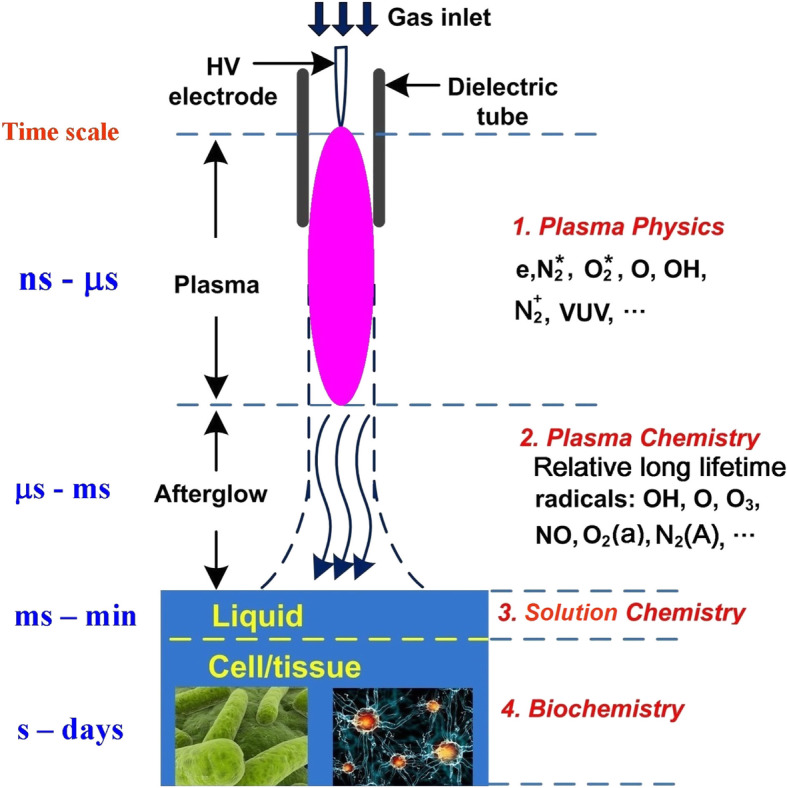
Following Lu et al. [10], the generation, interactions, and transport of reactive species among a variety of states of matter and spatial scales associated with interactions of plasma with biological objects
Anti-cancer activities of cold plasma-based on the nitrative and/or oxidative stress of plasma
On the bases of the oxidative stress and nitrative stress of plasma treatment on cells or tissues, the latest application that comes under the spotlight is the anti-cancer activities of cold plasma. The first report about the anti-cancer applications and the apoptosis of cancer cells in response to plasma treatment was published by Fridman et al. in 2007 [13]. Since then, a series of studies have confirmed the remarkable anticancer capacity of cold plasma and a number of cancer cell lines have been found vulnerable to CAP treatment, such as skin cancer cell lines [14], hepatoma [15], colorectal cancer cell lines [16], gastric cancer cell lines [17], breast cancer cell lines [18], pancreatic cancer cell lines [19], lung cancer cell lines [20], cervical cancer cell lines [21], head and neck cancer cell lines [22], leukemia [23], and even brain tumors. Glioblastoma is the most prevalent and one of the most aggressive main brain tumors with a devastatingly poor prognosis.
Plasma treatment of glioblastoma
Cold plasma has been highlighted in the in vitro anti-glioblastoma activities in different kinds of glioblastoma cell lines for many years [24, 25]. Mechanistic research on the anti-glioblastoma activities of plasma has mainly focused on the apoptotic and survival signal pathways mediated by the reactive species from the plasma emissions [26] or the plasma-mediated medium (PAM) [27, 28]. For example, Tanaka et al. found that PAM could downregulate cell survival and proliferation pathways, such as extracellular regulated kinase (ERK), serine-threonine kinase AKT, and mammalian target of rapamycin (mTOR) signaling pathways [29]. Another interesting publication by Kaushik et al. found that plasma-induced reactive species induced cytotoxic RAW 264.7 macrophages to release TNF-α, which could block the growth of cancer cells when cocultured with the T98G human glioblastoma multiforme cell line [29]. Recently, Yan et al. [29] suggested that aquaporin 8 (AQP 8), a kind of H2O2 membrane channel in many types of cells, was closely related to the anticancer capacity of plasma-stimulated medium (PSM) in U87MG glioblastoma cell lines. Inhibiting the expression of AQP8 in U87MG cells played an important role in weakening the anti-glioblastoma effect of PSM.
Some researchers are more focused on the targeted killing effect on glioblastoma cell lines of plasma. Cheng et al. compared the parameters of plasma and the threshold of plasma treatment on a U87 glioblastoma cell line and human astrocytes in normal conditions (E6/E7); these authors found that a plasma treatment that lasted 30 s caused a threefold increase in the death of U87 cells as compared to the E6/E7 cells [26]. Another publication by Tanaka et al. found that, compared with the commercially available normal human astrocytes, U251SP glioblastoma cells were more easily induced to apoptosis by the plasma mediated medium (PAM), which was regulated by downregulating total AKT kinase expression and phosphorylated AKT (Ser473) [30].
The first-line glioblastoma chemotherapeutic drug is temozolomide (TMZ), which is an alkylating agent. Currently, standard GBM care consists of maximal surgical resection, and then radiotherapy along with adjuvant chemotherapy by virtue of TMZ [31]. Recurring issues with present chemotherapeutics employed in GBM treatment are the negative side effects as a result of the high toxic effect of the drugs, and the resistance to the therapy developed over time. In response, combinational therapies are adopted in order to reduce the possibility of drug resistance and the negative side effects related to therapies with a single agent. Recent research from Conway et al. showed that plasma could induce a JNK-, ROS-, and caspase-independent mechanisms of death of the U373MG GBM cell lines, which can be significantly enhanced by virtue of combining low doses of TMZ [32]. Koritzer et al. investigated the effect of plasma on TMZ-sensitive and TMZ-resistant cell lines in glioblastoma cell lines LN18, U87MG, and LN229. The combined treatment of TMZ and plasma resulted in cell cycle arrest and the inhibition of cell growth [33].
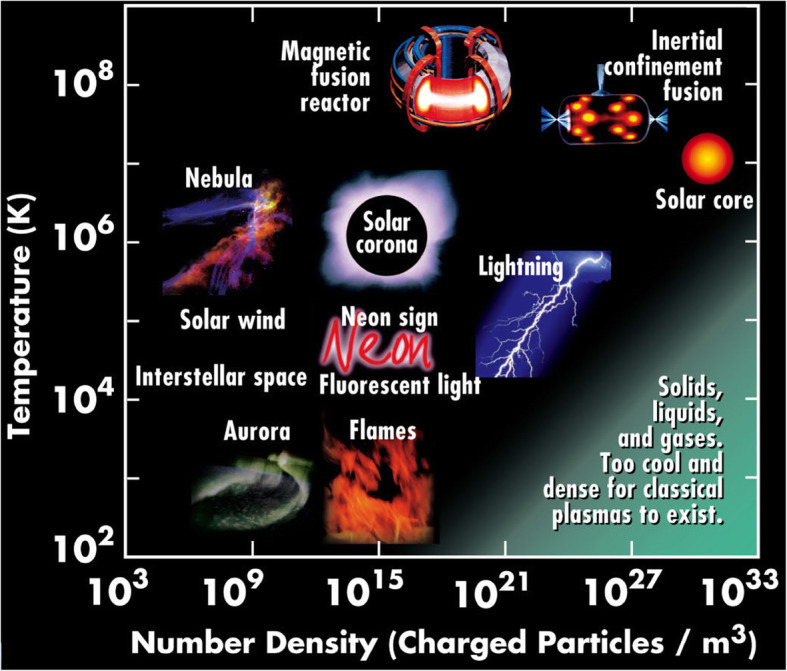
Some researchers have tried to translate the in vitro research about the anti-glioblastoma effect of plasma into animal studies. Research from Yan et al. also demonstrated the anti-glioblastoma effect of plasma both in the U87MG glioblastoma cell line and U87MG xenografts in rat brains. This research was based on a novel microsized CAP device (μCAP), of which the inner diameter of quartz tube was only 70 ± 3 μm, so the tube could be implanted into the mouse brain for the in vivo treatment of glioblastoma (Fig. 5). The results showed significant inhibition of tumor volume compared with the control animals [34]. Other research by Vandamme et al. also showed that plasma treatment could reduce subcutaneous glioma xenograft volume and prolong overall survival rate in rats [35].
Fig. 5.
In vivo targeting of glioblastoma tumors by He μCAP [34]. a A new μCAP device used in plasma delivery by means of an intracranial endoscopic tube to direct at glioblastoma tumors in the brain of the mouse. b Representative bioluminescence images in vivo demonstrating the volume of glioblastoma tumor (such as radiance or light emission) at baseline and 2 days after the treatment of He μCAP or vehicle (helium). Areas of low photon emission are indicated in blue and high are indicated in red
Neural stem cells differentiation and neuro-protection of plasma-based on the physiology functions of ROS and RNS from “suitable” low-dose plasma treatment
The RNS and ROS generated by the APPJ treatment have been regarded to associate the biomedical applications with plasma for a long time [36, 37]. Previous researches highlighted the inactivation effects of microorganisms (fungi, viruses, bacteria, etc.), cancer tissues, or cells as a result of the accumulation of nitrative stress and/or oxidative stress mediated by APPJ [10, 11, 38]. Nevertheless, RNS and ROS play more significant physiological roles in the human body [39, 40]. RNS and ROS at physiological concentrations can result in positive physiological advantages, including maintaining homeostasis [41], initiating immune responses [42], and regulating cell differentiation and proliferation [43], by means of functioning as intracellular signaling molecules which are engaged in the pathophysiological and physiological processes.
Among these active species produced by plasma, NO plays a critical role in the central nervous system (CNS). NO is a crucial signaling molecule that regulates a variety of biological processes and plays a double role in the human body, particularly in terms of CNS (i.e., neurotoxicity and neuroprotection). Excessive generation of NO not only induces apoptosis but also is involved in the pathophysiology of neurodegenerative disorders [44]. On the other hand, NO at physiologically low levels can function as a neuroprotective agent in the face of a variety of death challenges by regulation of the downstream signal pathways, like PI3 kinase/Akt and NO-cGMP-PKG pathways [45, 46]. A quantity of pharmacological researches have indicated that gaseous NO and various NO donor drugs have been widely used for a variety of vascular and CNS disorders or as a neuroprotective agent during brain injuries [46–51]. Furthermore, in vivo researches suggested that NO could also function as a powerful cerebral vasodilator to improve the supply of cerebral blood flow (CBF) into the infarcted area during hypoxic or ischemic brain injuries [52, 53].
Therefore, some researchers focus on the potential use of plasma on CNS disorders. Xiong et al. first reported that cold plasma could selectively promote the differentiation of neural stem cells into neuronal cells, which was regulated by the nitric oxide (NO) generation of plasma emissions [54]. The mechanism of the neuronal differentiation effect of plasma on neural stem cells was detailed by Jang et al. These authors found that plasma treatment could increase the extracellular NO concentration, which induced reversible inhibition of mitochondrial complex IV and produced large amounts of superoxide radical (•O2−). Cytosolic hydrogen peroxide, which is generated by •O2− dismutation, activated the Trk/Ras/ERK signaling pathway in specific by playing the role of an intracellular messenger. In addition, the authors also proved the differentiation effect of plasma in the living zebrafish in vivo (Fig. 6) [55].
Fig. 6.
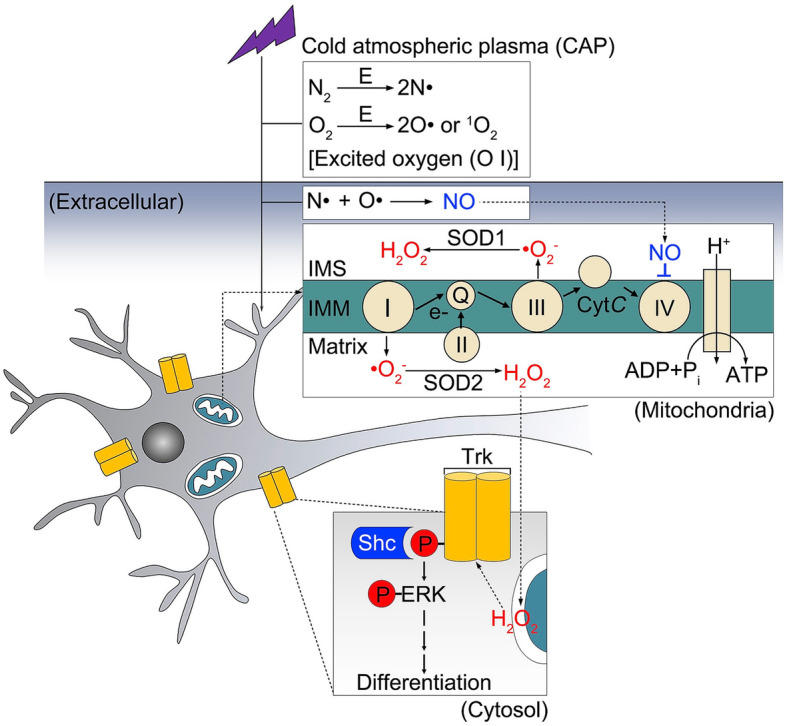
Following Jang et al. regarding the neural differentiation mechanism of cold plasma. Plasma treatment directly induced an increase in extracellular NO and targeted mitochondria. NO contends with O2 for binding to the active site of the cytochrome c oxidase, mitochondrial electron transport chain complex IV, and reversibly impeding its activity. Mitochondrial •O2− is generated by virtue of an electron reduction of O2 by means of obstructing electron transfer in the electron transport chain. Then, mitochondrial •O2− further leads to the production of intracellular H2O2, which could activate the Trk/Ras/ERK signaling pathway in specific by playing the role of an intracellular messenger, and finally resulted in neural differentiation
Then, some researchers focused on the treatment effect of plasma using in vitro disease models of the central nervous system (CNS). Oxidative stress-induced cell damage has long been implicated in both the physiological process of aging and neurodegenerative disorders, including Alzheimer’s disease (AD) and Parkinson’s disease (PD). Yan et al. pretreated SH-SY5Y cells, which is a cell line commonly used for neurotoxicity or neuroprotection research in vitro by an atmospheric pressure plasma jet (APPJ), and then subjected the cells to oxidative stress injuries. These authors found that pretreatment by APPJ could rescue SH-SY5Y cells from the harm of oxidative stress by decreasing cell apoptosis, which could be associated with the reactive nitrogen species that were induced by the treatment of APPJ [56]. Two researchers from the same group also found that APPJ pretreatment could protect against glucose deprivation (to stimulate glucose metabolism dysfunction diseases in CNS) [57] and hypoxia-induced injury (to simulate ischemia diseases in CNS, especially stroke) [58] in the SH-SY5Y cells. In addition, the authors also found that APPJ treatment could reduce the hypoxia microenvironment induced by an over-proliferation of cells, using a real-time cell viability recording system, namely, the electric cell-substrate impedance sensing system [58], suggesting a new mechanism of the anti-tumor capacity of APPJ that deserves further investigation.
Conclusions
Plasma medicine is a multidisciplinary field of study, coupling plasma physics, medicine, biology, plasma chemistry, and engineering, grown from studies in the application of atmospheric plasmas under low-temperature (or cold) in biomedicine. The current review summarized some applications of plasma medicine in neuroscience, especially in anti-glioblastoma, neuro-differentiation, and neuroprotection, based on the biological production of RNS and ROS in response to plasma emissions. In future studies, identifying key plasma-generated ROS/RNS and tracking their influence on different cells in the brain and even on neoplastic cells will be of growing importance. Issues like the origin of these species, their transportation to and within cells, what reactions are involved in these processes, and ultimately, how their effects permeate other cells will be of vital importance to be studied in the future. The current level of studies suffices to prove that plasmas can (eventually) achieve special use in the CNS in direct molecular transportation of medical substances. By controlling the parameters, plasmas may ultimately be able to produce specific species that propagate into the cellular tissues and cause the desired biological and medical effects.
Acknowledgements
Not applicable
Abbreviations
- AD
Alzheimer’s disease
- AFOSR
Air Force Office of Scientific Research
- APPJ
Atmospheric-pressure plasma jet
- AQP 8
Aquaporin 8
- CBF
Cerebral blood flow
- CNS
Central nervous system
- DBD
Dielectric barrier discharge
- ECIS
Electric cell-substrate impedance sensing
- ERK
Extracellular regulated kinase
- ICPM
International Conference on Plasma Medicine
- IWPCT
International Workshop on Plasma for Cancer Treatment
- LTP
Low-temperature plasma
- mTOR
Mammalian target of rapamycin
- NO
Nitric oxide
- PAM
Plasma-mediated medium
- PD
Parkinson’s disease
- PSM
Plasma-stimulated medium
- RNS
Reactive nitrogen species
- ROS
Reactive oxygen species
- TMZ
Temozolomide
- μCAP
Microsized CAP device
Authors’ contributions
XY and JO were the main contributors for designing and preparing this review. CZ, ZS, and BW collected the data and prepared the figures. KO reviewed and made any modifications for this review. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (nos. 51707012 and 11475019).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Contributor Information
Xu Yan, Email: devil-yx@163.com.
Jiting Ouyang, Email: jtouyang@bit.edu.cn.
Chenyang Zhang, Email: 916717268@163.com.
Zhongfang Shi, Email: shizhongfangbj@163.com.
Boran Wang, Email: ttboran@163.com.
Kostya ( Ken) Ostrikov, Email: kostya.ostrikov@qut.edu.au.
References
- 1.Yan KP, Jin QK, Zheng C, Deng GL, Yin SY, Liu Z. Pulsed cold plasma-induced blood coagulation and its pilot application in stanching bleeding during rat hepatectomy. Plasma Sci Technol. 2018;20(4):044005. doi: 10.1088/2058-6272/aa9b79. [DOI] [Google Scholar]
- 2.Fridman G, Friedman G, Gutsol A, Shekhter AB, Vasilets VN, Fridman A. Applied plasma medicine. Plasma Processes Polym. 2008;5(6):503–533. doi: 10.1002/ppap.200700154. [DOI] [Google Scholar]
- 3.Vargo JJ. Clinical applications of the argon plasma coagulator. Gastrointest Endosc. 2004;59(1):81–88. doi: 10.1016/S0016-5107(03)02296-X. [DOI] [PubMed] [Google Scholar]
- 4.Laroussi M, Lu X, Keidar M. Perspective: the physics, diagnostics, and applications of atmospheric pressure low temperature plasma sources used in plasma medicine. J Appl Phys. 2017;122(2):020901. doi: 10.1063/1.4993710. [DOI] [Google Scholar]
- 5.Laroussi M. Sterilization of contaminated matter with an atmospheric pressure plasma. Ieee T Plasma Sci. 1996;24(3):1188–1191. doi: 10.1109/27.533129. [DOI] [Google Scholar]
- 6.Shekhter AB, Kabisov RK, Pekshev AV, Kozlov NP, Perov YL. Experimental and clinical validation of plasmadynamic therapy of wounds with nitric oxide. Bull Exp Biol Med. 1998;126(8):829–834. doi: 10.1007/BF02446923. [DOI] [PubMed] [Google Scholar]
- 7.Stoffels E, Flikweert AJ, Stoffels WW, Kroesen GMW. Plasma needle: a non-destructive atmospheric plasma source for fine surface treatment of (bio)materials. Plasma Sources Sci Technol. 2002;11(4):383–388. doi: 10.1088/0963-0252/11/4/304. [DOI] [Google Scholar]
- 8.Stoffels E, Sladek REJ, Kieft IE. Gas plasma effects on living cells. Phys Scr. 2004;T107:79–82. doi: 10.1238/Physica.Topical.107a00079. [DOI] [Google Scholar]
- 9.Laroussi M. Plasma medicine: a brief introduction. Plasma. 2018;1(1):5. doi: 10.3390/plasma1010005. [DOI] [Google Scholar]
- 10.Lu X, Naidis GV, Laroussi M, Reuter S, Graves DB, Ostrikov K. Reactive species in non-equilibrium atmospheric-pressure plasmas: generation, transport, and biological effects. Phys Rep. 2016;630:1–84. doi: 10.1016/j.physrep.2016.03.003. [DOI] [Google Scholar]
- 11.Graves DB. The emerging role of reactive oxygen and nitrogen species in redox biology and some implications for plasma applications to medicine and biology. J Phys D Appl Phys. 2012;45(26):263001. doi: 10.1088/0022-3727/45/26/263001. [DOI] [Google Scholar]
- 12.Yan X, Xiong Z, Zou F, Zhao S, Lu X, Yang G, et al. Plasma-induced death of HepG2 cancer cells: intracellular effects of reactive species. Plasma Processes Polym. 2012;9(1):59–66. doi: 10.1002/ppap.201100031. [DOI] [Google Scholar]
- 13.Fridman G, Shereshevsky A, Jost MM, Brooks AD, Fridman A, Gutsol A, et al. Floating electrode dielectric barrier discharge plasma in air promoting apoptotic behavior in melanoma skin cancer cell lines. Plasma Chem Plasma P. 2007;27(2):163–176. doi: 10.1007/s11090-007-9048-4. [DOI] [Google Scholar]
- 14.Gay-Mimbrera J, Garcia MC, Isla-Tejera B, Rodero-Serrano A, Garcia-Nieto AV, Ruano J. Clinical and biological principles of cold atmospheric plasma application in skin cancer. Adv Ther. 2016;33(6):894–909. doi: 10.1007/s12325-016-0338-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gweon B, Kim M, Kim DB, Kim D, Kim H, Jung H, et al. Differential responses of human liver cancer and normal cells to atmospheric pressure plasma. Appl Phys Lett. 2011;99(6):063701. doi: 10.1063/1.3622631. [DOI] [Google Scholar]
- 16.Kim CH, Bahn JH, Lee SH, Kim GY, Jun SI, Lee K, et al. Induction of cell growth arrest by atmospheric non-thermal plasma in colorectal cancer cells. J Biotechnol. 2010;150(4):530–538. doi: 10.1016/j.jbiotec.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 17.Torii K, Yamada S, Nakamura K, Tanaka H, Kajiyama H, Tanahashi K, et al. Effectiveness of plasma treatment on gastric cancer cells. Gastric Cancer. 2015;18(3):635–643. doi: 10.1007/s10120-014-0395-6. [DOI] [PubMed] [Google Scholar]
- 18.Wang M, Holmes B, Cheng XQ, Zhu W, Keidar M, Zhang LG. Cold atmospheric plasma for selectively ablating metastatic breast cancer cells. PLoS One. 2013;8(9):e73741. doi: 10.1371/journal.pone.0073741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brulle L, Vandamme M, Ries D, Martel E, Robert E, Lerondel S, et al. Effects of a non thermal plasma treatment alone or in combination with gemcitabine in a MIA PaCa2-luc orthotopic pancreatic carcinoma model. PLoS One. 2012;7(12):e52653. doi: 10.1371/journal.pone.0052653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim JY, Ballato J, Foy P, Hawkins T, Wei YZ, Li JH, et al. Apoptosis of lung carcinoma cells induced by a flexible optical fiber-based cold microplasma. Biosens Bioelectron. 2011;28(1):333–338. doi: 10.1016/j.bios.2011.07.039. [DOI] [PubMed] [Google Scholar]
- 21.Li W, Yu KN, Bao LZ, Shen J, Cheng C, Han W. Non-thermal plasma inhibits human cervical cancer HeLa cells invasiveness by suppressing the MAPK pathway and decreasing matrix metalloproteinase-9 expression. Sci Rep. 2016;6:19720. doi: 10.1038/srep19720. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 22.Guerrero-Preston R, Ogawa T, Uemura M, Shumulinsky G, Valle BL, Pirini F, et al. Cold atmospheric plasma treatment selectively targets head and neck squamous cell carcinoma cells. Int J Mol Med. 2014;34(4):941–946. doi: 10.3892/ijmm.2014.1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barekzi N, Laroussi M. Dose-dependent killing of leukemia cells by low-temperature plasma. J Phys D Appl Phys. 2012;45(42):422002. doi: 10.1088/0022-3727/45/42/422002. [DOI] [Google Scholar]
- 24.Kaushik NK, Kim YH, Han YG, Choi EH. Effect of jet plasma on T98G human brain cancer cells. Curr Appl Phys. 2013;13(1):176–180. doi: 10.1016/j.cap.2012.07.002. [DOI] [Google Scholar]
- 25.Vermeylen S, De Waele J, Vanuytsel S, De Backer J, Van der Paal J, Ramakers M, et al. Cold atmospheric plasma treatment of melanoma and glioblastoma cancer cells. Plasma Processes Polym. 2016;13(12):1195–1205. doi: 10.1002/ppap.201600116. [DOI] [Google Scholar]
- 26.Cheng XQ, Sherman J, Murphy W, Ratovitski E, Canady J, Keidar M. The effect of tuning cold plasma composition on glioblastoma cell viability. PLoS One. 2014;9(5):e98652. doi: 10.1371/journal.pone.0098652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yan DY, Nourmohammadi N, Bian K, Murad F, Sherman JH, Keidar M. Stabilizing the cold plasma-stimulated medium by regulating medium’s composition. Sci Rep. 2016;6:26016. doi: 10.1038/srep26016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kurake N, Tanaka H, Ishikawa K, Kondo T, Sekine M, Nakamura K, et al. Cell survival of glioblastoma grown in medium containing hydrogen peroxide and/or nitrite, or in plasma-activated medium. Arch Biochem Biophys. 2016;605:102–108. doi: 10.1016/j.abb.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 29.Tanaka H, Mizuno M, Ishikawa K, Nakamura K, Utsumi F, Kajiyama H, et al. Cell survival and proliferation signaling pathways are downregulated by plasma-activated medium in glioblastoma brain tumor cells. Plasma Med. 2012;2(4):207–220. doi: 10.1615/PlasmaMed.2013008267. [DOI] [Google Scholar]
- 30.Tanaka H, Mizuno M, Ishikawa K, Nakamura K, Kajiyama H, Kano H, et al. Plasma-activated medium selectively kills glioblastoma brain tumor cells by down-regulating a survival signaling molecule, AKT kinase. Plasma Med. 2011;1(3–4):265–277. doi: 10.1615/PlasmaMed.2012006275. [DOI] [Google Scholar]
- 31.Adamson C, Kanu OO, Mehta AI, Di CH, Lin NJ, Mattox AK, et al. Glioblastoma multiforme: a review of where we have been and where we are going. Expert Opin Investig Drugs. 2009;18(8):1061–1083. doi: 10.1517/13543780903052764. [DOI] [PubMed] [Google Scholar]
- 32.Conway GE, Casey A, Milosavljevic V, Liu YP, Howe O, Cullen PJ, et al. Non-thermal atmospheric plasma induces ROS-independent cell death in U373MG glioma cells and augments the cytotoxicity of temozolomide. Br J Cancer. 2016;114(4):435–443. doi: 10.1038/bjc.2016.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koritzer J, Boxhammer V, Schafer A, Shimizu T, Klampfl TG, Li YF, et al. Restoration of sensitivity in chemo - resistant glioma cells by cold atmospheric plasma. PLoS One. 2013;8(5):e64498. doi: 10.1371/journal.pone.0064498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen ZT, Simonyan H, Cheng XQ, Gjika E, Lin L, Canady J, et al. A novel micro cold atmospheric plasma device for glioblastoma both in vitro and in vivo. Cancers (Basel) 2017;9(6):61. doi: 10.3390/cancers9060061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vandamme M, Robert E, Dozias S, Sobilo J, Lerondel S, Le Pape A, et al. Response of human glioma U87 xenografted on mice to non thermal plasma treatment. Plasma Med. 2011;1(1):27–43. doi: 10.1615/PlasmaMed.v1.i1.30. [DOI] [Google Scholar]
- 36.Laroussi M. Low-temperature plasma jet for biomedical applications: a review. Ieee T Plasma Sci. 2015;43(3):703–712. doi: 10.1109/TPS.2015.2403307. [DOI] [Google Scholar]
- 37.Von Woedtke T, Reuter S, Masur K, Weltmann K-D. Plasmas for medicine. Phys Rep. 2013;530(4):291–320. doi: 10.1016/j.physrep.2013.05.005. [DOI] [Google Scholar]
- 38.Weltmann KD, Kindel E, Brandenburg R, Meyer C, Bussiahn R, Wilke C, et al. Atmospheric pressure plasma jet for medical therapy: plasma parameters and risk estimation. Contrib Plasma Physics. 2009;49(9):631–640. doi: 10.1002/ctpp.200910067. [DOI] [Google Scholar]
- 39.Valko M, Leibfritz D, Moncol J, Cronin MTD, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol. 2007;39(1):44–84. doi: 10.1016/j.biocel.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 40.Fransen M, Nordgren M, Wang B, Apanasets O. Role of peroxisomes in ROS/RNS-metabolism: implications for human disease. BBA-Mol Basis Dis. 2012;1822(9):1363–1373. doi: 10.1016/j.bbadis.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 41.Gupta KJ, Igamberdiev AU, Mur LAJ. NO and ROS homeostasis in mitochondria: a central role for alternative oxidase. New Phytol. 2012;195(1):1–3. doi: 10.1111/j.1469-8137.2012.04189.x. [DOI] [PubMed] [Google Scholar]
- 42.Wink DA, Hines HB, Cheng RYS, Switzer CH, Flores-Santana W, Vitek MP, et al. Nitric oxide and redox mechanisms in the immune response. J Leukoc Biol. 2011;89(6):873–891. doi: 10.1189/jlb.1010550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Droge W. Free radicals in the physiological control of cell function. Physiol Rev. 2002;82(1):47–95. doi: 10.1152/physrev.00018.2001. [DOI] [PubMed] [Google Scholar]
- 44.Shahani N, Sawa A. Nitric oxide signaling and nitrosative stress in neurons: role for S-nitrosylation. Antioxid Redox Signal. 2011;14(8):1493–1504. doi: 10.1089/ars.2010.3580. [DOI] [PubMed] [Google Scholar]
- 45.Martinez-Ruiz A, Cadenas S, Lamas S. Nitric oxide signaling: classical, less classical, and nonclassical mechanisms. Free Radic Biol Med. 2011;51(1):17–29. doi: 10.1016/j.freeradbiomed.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 46.Ha KS, Kim KM, Kwon YG, Bai SK, Nam WD, Yoo YM, et al. Nitric oxide prevents 6-hydroxydopamine-induced apoptosis in PC12 cells through cGMP-dependent PI3 kinase/Akt activation. FASEB J. 2003;17(9):1036–1047. doi: 10.1096/fj.02-0738com. [DOI] [PubMed] [Google Scholar]
- 47.Garry PS, Ezra M, Rowland MJ, Westbrook J, Pattinson KTS. The role of the nitric oxide pathway in brain injury and its treatment - from bench to bedside. Exp Neurol. 2015;263:235–243. doi: 10.1016/j.expneurol.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 48.Arandarcikaite O, Jokubka R, Borutaite V. Neuroprotective effects of nitric oxide donor NOC-18 against brain ischemia-induced mitochondrial damages: role of PKG and PKC. Neurosci Lett. 2015;586:65–70. doi: 10.1016/j.neulet.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 49.Li Y-S, Shemmer B, Stone E, Nardi MA, Jonas S, Quartermain D, et al. Brain Res. 2013;1507(Supplement C):134–145. doi: 10.1016/j.brainres.2013.02.031. [DOI] [PubMed] [Google Scholar]
- 50.Lundberg JO, Gladwin MT, Weitzberg E. Strategies to increase nitric oxide signalling in cardiovascular disease. Nat Rev Drug Discov. 2015;14(9):623. doi: 10.1038/nrd4623. [DOI] [PubMed] [Google Scholar]
- 51.Zhu C, Sun Y, Gao J, Wang X, Plesnila N, Blomgren K. Inhaled nitric oxide protects males but not females from neonatal mouse hypoxia–ischemia brain injury. Transl Stroke Res. 2013;4(2):201–207. doi: 10.1007/s12975-012-0217-2. [DOI] [PubMed] [Google Scholar]
- 52.Buchanan JE, Phillis JW. The role of nitric oxide in the regulation of cerebral blood flow. Brain Res. 1993;610(2):248–255. doi: 10.1016/0006-8993(93)91408-K. [DOI] [PubMed] [Google Scholar]
- 53.Dormanns K, Brown RG, David T. The role of nitric oxide in neurovascular coupling. J Theor Biol. 2016;394:1–17. doi: 10.1016/j.jtbi.2016.01.009. [DOI] [PubMed] [Google Scholar]
- 54.Xiong Z, Zhao S, Mao X, Lu X, He G, Yang G, et al. Selective neuronal differentiation of neural stem cells induced by nanosecond microplasma agitation. Stem Cell Res. 2014;12(2):387–399. doi: 10.1016/j.scr.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 55.Jang JY, Hong YJ, Lim J, Choi JS, Choi EH, Kang S, et al. Cold atmospheric plasma (CAP), a novel physicochemical source, induces neural differentiation through cross-talk between the specific RONS cascade and Trk/Ras/ERK signaling pathway. Biomaterials. 2018;156:258–273. doi: 10.1016/j.biomaterials.2017.11.045. [DOI] [PubMed] [Google Scholar]
- 56.Xu Y, Yajun Q, Jiting O, Mei J, Jiaxin L, Fang Y. Protective effect of atmospheric pressure plasma on oxidative stress-induced neuronal injuries: an in vitro study. J Phys D Appl Phys. 2017;50(9):095401. doi: 10.1088/1361-6463/aa5622. [DOI] [Google Scholar]
- 57.Yan X, Meng Z, Ouyang J, Qiao Y, Yuan F. New application of an atmospheric pressure plasma jet as a neuro-protective agent against glucose deprivation-induced injury of SH-SY5Y cells. J Vis Exp. 2017;(128):e56323. [DOI] [PMC free article] [PubMed]
- 58.Yan X, Meng ZZ, Ouyang JT, Qiao YJ, Li JX, Jia M, et al. Cytoprotective effects of atmospheric-pressure plasmas against hypoxia-induced neuronal injuries. J Phys D Appl Phys. 2018;51(8):085401. doi: 10.1088/1361-6463/aaa867. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.