Abstract
Background
Similar to the situation in other European countries, Danish wild boars may harbour a wide range of pathogens infectious to humans and domestic pigs. Although wild boars must be kept behind fences in Denmark, hunting and consumption of the meat may cause zoonotic transmission. Moreover, most infections of wild boars are transmissible to domestic pigs, which may have important economic consequences. The aim of this study was to investigate whether Danish wild boars were infected with bacteria and parasites transmissible to humans or domestic pigs: Brucella suis, methicillin-resistant Staphylococcus aureus (MRSA), Salmonella spp., Trichinella spp., lungworms and gastrointestinal parasites, especially Ascaris suum. This is the first study to investigate the prevalence of these important pathogens in Danish wild boars.
Results
Wild boars from eight enclosures were analysed over a 5-year period. All tested wild boars were negative for B. suis (n = 240), MRSA (n = 244), Salmonella spp. (n = 115) and Trichinella spp. (n = 232), while eight parasite genera were identified in the faeces (n = 254): Ascaris suum, Capillaria sp., Cystoisospora suis, Eimeria spp., Metastrongylus sp. (lungworm), Strongyloides ransomi, Trichuris suis and strongylid eggs, i.e. strongyles not identified to the genera. Eimeria spp. and Metastrongylus sp. had the highest prevalence (92.3 and 79.5%, respectively) and were identified in wild boars from all eight enclosures, while the remaining parasite genera were present more sporadically.
Conclusions
Wild boars from Denmark constitute a low risk of transmitting B. suis, MRSA, Salmonella spp. and Trichinella spp. to humans or domestic pigs, while economically important parasites transmissible to domestic pigs are highly prevalent in the wild boar population.
Keywords: Brucella, Gastrointestinal parasites, Metastrongylus, MRSA, Salmonella, Trichinella, Wild boars
Background
Wild boars (Sus scrofa) have an extensive worldwide distribution, and a significant increase in their population was observed in Europe in the last decades [1]. Wild boars have one of the largest geographical ranges of all terrestrial wild animal species [2]. In Denmark, free-living wild boars were extinguished in 1801 [3], and today, wild boars must be kept behind fences. In the Danish Central Livestock Register, 53 enclosures are currently listed for keeping wild boars [4], and officially, the wild boar population consist of 654 animals. However, the actual number is unknown. The enclosures include natural habitats up to 40 km2, where the wild boars are kept for hunting or farming. Free-living wild boars are sporadically reported, when they escape from enclosures or cross the border from Germany. However, hunters are encouraged to shoot these free-living wild boars all year round. In December 2019, a fence (1.5 m high and 70 km long) was built at the German–Danish border to prevent wild boars from crossing the Danish land border from Germany.
In general, wild boars are considered a potential risk for transmission of severe pathogens to humans and domestic pigs. Humans can come in contact with live or dead wild boars and become infected e.g. during hunting, recreational use of wild boar habitats or through consumption of wild boar meat, or exposure to the escaped wild boars. Moreover, humans or wild boars can transfer infections to domestic pigs [5–8]. Currently, domestic pigs from Denmark are free from important notifiable diseases such as classical- and African swine fever, Aujeszky’s disease, brucellosis and trichinellosis [9], but the risk of disease transmission from wild boars to domestic pigs is likely to increase due to the trend of converting pig production from indoor to outdoor housing. Pig production and export of pork meat is a major and important industry in Denmark with a production of around 20 million slaughter pigs per year [10]. Although the Danish wild boars are confined in enclosures, other wild animals can function as reservoir hosts for transmission of pathogens from wild boars to domestic swine, e.g. brown hares (Lepus europaeus) infected with Brucella suis [11] and rodents infected with Trichinella spp. [12].
This study focused on the bacteria and parasites, which in Denmark currently are considered most important to the pig industry and public health, i.e. B. suis, Salmonella spp., methicillin-resistant Staphylococcus aureus (MRSA), Trichinella spp., and various gastrointestinal parasites and lungworms.
The genus Brucella is a group of zoonotic bacteria causing brucellosis. Brucella spp. are infectious to several mammals including cattle, sheep, goats, pigs, and humans. In pigs, brucellosis caused by infection with B. suis manifests as abortion, orchitis, and lameness [13], while in humans, the disease has varying clinical manifestations, where the acute stage is characterized by nonspecific symptoms similar to a flu-like or septicaemic illness [14]. Brucellosis has not been detected in Danish pig herds since 1994 and 1999, where B. suis biovar 2 have been found in free-ranging pig herds [15].
Salmonella are widespread bacterial pathogens shared by humans, domestic- and wild animals including wild boars [16–18]. Human foodborne Salmonella outbreaks are common in Europe [19]. Wild boars can harbour several different serovars of Salmonella including S. typhimurium and S. enteritidis [17], both of which cause numerous salmonellosis cases in humans annually [19]. In humans, salmonellosis can cause severe disease and even death, while animals are often asymptomatic carriers of the infection. Salmonella infections occur in Danish pigs [20] as well as in wild animals including e.g. hedgehogs (Erinaceus europaeus), badgers (Meles meles) and harbour seals (Phoca vitulina) [21].
Lately, MRSA has become a problematic microorganism because of its resistance to almost all beta-lactams and the ability to transfer the resistance mechanism to other non-beta-lactamase producing pathogens. Previously, MRSA was a pathogen mostly associated with hospitals, but also people without contact to hospital environments are widely diagnosed with MRSA. MRSA has been recorded from Danish pigs [22], from retail meat [23], farmed mink [24], and horses [25]. Studies on MRSA in wild boars are currently scarce, but MRSA has been identified in wild boars from Germany and Spain [26, 27].
Denmark is officially recognised as a region with negligible risk of Trichinella in farmed pigs [28]. Currently, no systematic surveillance of Trichinella spp. in Danish wildlife occur, but previous surveillance projects have demonstrated presence of T. pseudospiralis in wild mink on the Island of Bornholm in 2007 (Data not published), and three cases of Trichinella spp. in red foxes (0.1%) in the mid-1990s [29]. Therefore, Danish wildlife, including wild boars, could potentially be infected with Trichinella spp.. Currently, all wild boars shot in Denmark or shot abroad and imported to Denmark for consumption must be tested for Trichinella spp.. Wild boars are asymptomatic carriers of Trichinella spp., while the symptoms of trichinellosis in humans include mild non-bloody diarrhoea, nausea, vomiting, abdominal discomfort, persistent fever, sweating, chills, periorbital oedema, urticarial rash, and conjunctival or splinter and ungual haemorrhages [30].
Besides Trichinella spp., wild boars can harbour many parasites of zoonotic and economic importance. Gastrointestinal parasites and lungworms are commonly detected in European wild boars [31–34], and they can infect domestic pigs and vice versa. Parasitic infections in domestic pigs are commonly subclinical, but weight loss, diarrhoea, reduced growth, depression, fatalities, reduced carcass quality and chronic and paroxysmal coughing can appear [35–38], depending on the parasite genera and infection dose. Hence, parasitic infections may cause significant economic losses to the pig production. Additionally, the helminths A. suum and Metastrongylus are zoonotic [39–41] and the same may be true for Trichuris suis [35]. In humans, A. suum infection may cause severe visceral larval migrans causing liver and lung lesions [42].
The aim of this study was to investigate the prevalence of B. suis, MRSA, Salmonella spp., Trichinella spp., gastrointestinal parasites and lungworms in wild boars from Denmark to assess if they pose a risk of transmitting these pathogens to humans and domestic pigs. Surveillance of wild boars for African- and classical swine fever as well as Aujeszky’s disease is mandatory in Denmark and testing for these pathogens were therefore not included in this study.
Methods
Study area and sample collection
The Danish Veterinary and Food Administration funded the study, and decided on the yearly sample size. The Veterinary Institute (now Centre for Diagnostic), Technical University of Denmark selected the study enclosures based on the size of the actual enclosure and the willingness of the owners to participate. The aim was to sample five large enclosures per hunting season. Since the sampling was based on voluntary participation by hunters, this was not always possible (Table 1). Altogether, eight separate outdoor enclosures in mainland Denmark were included in the study (Fig. 1).
Table 1.
Overview of wild boars included in the study according to hunting seasons and enclosure
| Enclosure | Hunting season | |||||
|---|---|---|---|---|---|---|
| 2014/2015 | 2015/2016 | 2016/2017 | 2017/2018 | 2018/2019 | Total | |
| A | 8 | 21 | 10 | 16 | 55 | |
| B | 19 | 19 | 15 | 14 | 67 | |
| C | 10 | 7 | 12 | 10 | 39 | |
| D | 11 | 10 | 12 | 33 | ||
| E | 11 | 11 | ||||
| F | 11 | 14 | 25 | |||
| G | 15 | 15 | ||||
| H | 10 | 10 | ||||
| Total | 59 | 21 | 47 | 61 | 67 | 255 |
Fig. 1.
Map of Denmark showing the geographical origin of the wild boar enclosures included in the study
The enclosures are natural habitats with forest, lakes and/or moor covering up to 40 km2. The wild boars were typically fed supplemental feed at permanent feeding sites or on the ground. If severe clinical disease was observed, the animals were euthanized for welfare reasons. The sampling took place during the hunting seasons (1st October to 31st January) 2014/2015 to 2018/2019. Each enclosure was sampled once during each hunting season. The samples were collected during one to four hunting seasons from each enclosure (Table 1). No animals were hunted for the purpose of this study.
Between seven and 20 wild boars were sampled per sampling day and enclosure (Table 1). Faecal samples from rectum (min. 30 g), diaphragm (approx. 5 × 5 cm), uterus or one testicle, spleen (approx. 5 × 5 cm) and nose swabs were collected immediately post mortem and transported in cooling boxes directly to the laboratory for analyses.
Analysis
Table 2 shows the number of wild boars analysed for each pathogen. Some samples were unsuited for analyses due to severe tissue damage after passage of the bullet. If possible, the approximate age was assessed by the hunters and recorded for each animal.
Table 2.
Overview of the number of wild boars in Denmark (2014–2019) examined for pathogens that can be transferred between wild boars, domestic pigs and humans
| Pathogen | Number of wild boars analysed |
|---|---|
| Brucella spp. | 240 |
| Parasite eggs/oocysts | 254 |
| Methicillin-resistant Staphylococcus aureus (MRSA) | 244 |
| Salmonella spp. | 115a |
| Trichinella spp. | 232 |
aWild boars sampled in in the hunting seasons 2017/2018 and 2018/2019 were not analysed for Salmonella spp.
The diaphragms were analysed for Trichinella spp. larvae by the magnetic stirrer method for pooled sample digestion according to Mayer-Scholl et al. [43]. Briefly, individual diaphragm samples (20 g from each animal from up to 10 animals from the same enclosure) were mixed and digestion fluid was added. The mixture was then stirred for a maximum of 60 min at 45 °C, subsequently sieved and allowed to sediment for 30 min. The sediment was collected and allowed to sediment for another 10 min. The supernatant was removed and the sediment was analysed for presence of Trichinella spp. larvae by stereomicroscopy at ×20 magnification.
The faecal samples were analysed for parasite eggs/oocysts and Salmonella spp.. Parasite eggs/oocysts were quantified using the modified McMaster technique [44] with a sensitivity of 5 eggs/oocysts per g faeces. Briefly, 4 g of faeces was suspended in 56 mL tap water, sieved through gauze, and 10 mL was centrifuged at 178 × g for 10 min. The supernatant was removed, the pellet was re-suspended in 3 mL of flotation fluid (saturated saline with glucose, 50 g/100 mL, specific gravity 1.27 g/mL) and a disposable McMaster chamber was filled with the mixture. The McMaster disposable chambers were prepared in our laboratory by gluing two small glass slides (38 × 26 × 1 mm) onto a larger glass slide (76 × 38 × 1 mm) separated by 24 mm space, and finally, a microscopic cover glass (50 × 25 × 0.2 mm) was glued onto the two small glass slides to create a counting chamber holding 0.6 mL. All eggs/oocysts in the whole chamber were identified by microscopy at ×100 magnification.
Salmonella spp. were analysed by faecal culture; 225 mL peptone buffer (Oxoid, Hampshire, UK) was added to 25 g of faeces in a plastic cup, homogenised by stirring and incubated at 37 °C for 16–20 h. Following incubation, 1 mL of the faecal mixture was collected; three drops of the mixture was inoculated onto Modified Semisolid Rappaport Vassiliadis agar (MSRV) (Oxoid, Hampshire, UK), while the remaining was added to 9 mL of Selenit broth (Oxoid, Hampshire, UK). Both were incubated for 18–24 h at 41.5 °C. Suspected Salmonella spp. colonies from the MSRV agar plate and 10 µL of the Selenit broth were plated onto a Xylose Lysine Deoxycholate agar (Oxoid, Hampshire, UK) and a Brilliant Green Agar (Oxoid, Hampshire, UK) and incubated at 37 °C in 18–24 h.
The spleen and the genital organs were analysed for B. suis by culture. The spleen and genital tissues (2 g of each) were pooled, 2.5 mL sterile water was added and the sample was homogenised for 2 min in a Stomacher® laboratory blender. Two drops of the resulting broth were then inoculated onto Brucella agar plates and incubated at 37 °C with CO2 for a maximum of 10 days.
Presence of MRSA was investigated by adding 3–4 mL Mueller–Hinton bouillon with 6.5% NaCl (SSI Diagnostica, Hillerød, Denmark) to a 15 mL tube containing the nasal swab, followed by incubation on a shaker table at 37 °C for 24 h. A loopful of broth was inoculated onto a MRSA 2 agar (Oxoid, Hampshire, UK) and incubated at 37 °C for 24–48 h, following which suspected colonies were subcultured onto a C-cattle blood agar (SSI Diagnostica, Hillerød, Denmark).
Data analysis
The prevalence and the 95% confidence intervals (CI) were calculated for each parasite species for the total study population. The prevalence, median and mean intensity (95% CI), min and max FEC/FOC were also calculated for wild boars ≤1 and >1 year for each parasite species. Differences in prevalence between age groups were determined using a binary logistic regression model with the parasite genera (Cystoisospora suis and Strongyloides ransomi were not tested) as the dependent variable and age groups (≤1 or >1 year) as the independent variable. The age was not assessed for 36.1% of the wild boars, and therefore excluded from the analysis. The differences in mean A. suum, Metastrongylus sp. and strongyle faecal egg count (FEC) and Eimeria spp. faecal oocyst count (FOC) for wild boars positive and negative for T. suis were determined by a one-way ANOVA with the log-transformed FEC/FOC as dependent variable and T. suis infection status (positive/negative) as independent categorical variable to determine if T. suis positive wild boars had higher FEC and FOC than T. suis negative wild boars. A P-value of ≤0.05 was considered significant. All statistical analyses were done in SAS for windows version 9.4 (SAS institute Inc., Cary, NC, USA).
Results
Altogether, 255 wild boars were sampled. Of these, 56.5% were males and 40.4% were females, while sex was not recorded for 3.1% of the wild boars. Of the wild boars where age was noted, 32.2% were ≤1 year and 31.8% were >1 year. The age was not assessed for 36.1% of the wild boars.
All tested wild boars were negative for Trichinella spp. larvae, Salmonella spp., B. suis, and MRSA, while parasite eggs/oocysts were identified from 0.4–92.3% of the wild boars (Table 3). The following parasite eggs/oocysts were identified: Ascaris suum, Capillaria sp., C. suis, Eimeria spp. (the oocysts were not identified to species level, but based on morphology, a mixture of different species was present), Metastrongylus sp., strongylids not identified to species level, S. ransomi and T. suis.
Table 3.
Overview of parasites detected coproscopically in wild boars in Denmark in 2014–2019 (n = 254)
| Parasite genera | No. of positive | Prevalence 95% CI | No. of enclosures with positive wild boars | Age ≤1a | Age >1a | ||||
|---|---|---|---|---|---|---|---|---|---|
| Prevalence 95% CI |
Median egg/oocyst excretion [min – max] |
95% CI of mean intensity | Prevalence 95% CI |
Median egg/oocyst excretion [min – max] |
95% CI of mean intensity | ||||
| Eimeria spp. | 234 |
92.3 88.8; 95.5 |
8 |
92.1 85.2; 99.0 |
2760 [10−200,000] |
5,021; 23,257 |
87.9 81.3; 84.4 |
7,980 [10 - 378,000] |
15,884; 39,009 |
| Metastrongylus sp. | 202 |
79.5 74.5; 84.5 |
8 |
90.5 83.0; 98.0 |
130 [10−11,100] |
429; 1,512 |
66.7 57.2; 76.1 |
83 [10 - 16,500] |
184; 1,409 |
| Strongyles | 150 |
59.1 53.0; 65.1 |
7 |
52.4 39.7; 65.1 |
120 [10 – 3,900] |
217; 984 |
56.6 46.7; 66.5 |
48 [10 – 1,600] |
72; 250 |
| Capillaria sp. | 28 |
11.1 7.1; 14.9 |
3 |
14.3 5.4; 23.2 |
10.0 [10 - 20] |
8.8; 15.7 |
14.1 7.2; 21.1 |
10.0 [10 - 20] |
9.7; 14.6 |
| Ascaris suum | 27 |
10.6 6.8; 14.4 |
6 |
12.7 4.2; 21.2 |
3540 [0 – 10,740] |
0; 92,416 |
8.1 2.6; 13.5 |
953 [0 - 239] |
0; 2,969 |
| Trichuris suis | 22 |
8.7 5.2; 12.1 |
4 |
12.7 4.2; 21.2 |
25 [0 - 10.7] |
0; 83 |
20.2 0; 4.8 |
15 [0 - 0.7] |
0-79 |
| Cystoisospora suis | 1 | 0.4 | 1 | – | – | - | – | ||
| Strongyloidesransomi | 1 | 0.4 | 1 | – | – | – | - | ||
aA total of 36.1% of the examined wild boars were not included in the calculation of excretion per age
Eimeria spp. were the most commonly identified parasite, followed by Metastrongylus sp., strongyles, Capillaria sp., A. suum and T. suis, while C. suis and S. ransomi were identified from only one wild boar each (Table 3). Eimeria spp. oocysts and Metastrongylus sp. eggs were identified in faeces from wild boars from all eight enclosures (Table 3).
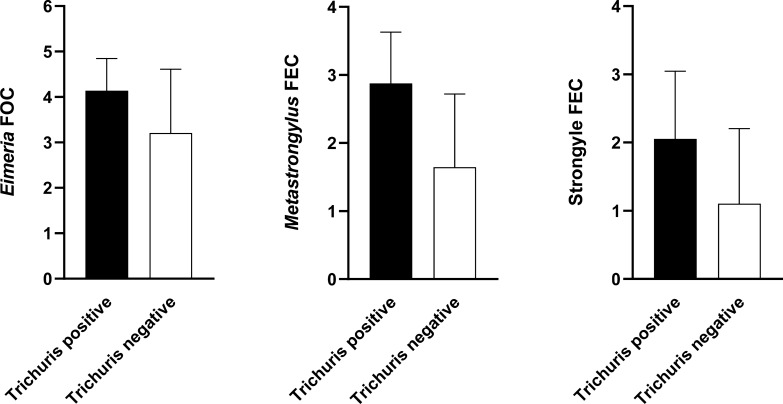
Wild boars positive for T. suis had significantly higher Metastrongylus sp. FEC (P < 0.0001), Eimeria spp. FOC (P = 0.0024), and strongyle FEC (P < 0.0001) compared to wild boars negative for T. suis infection (Fig. 2). Ascaris suum FECs were not significant different between T. suis positive and negative wild boars. Metastrongylus sp. were significantly more prevalent in the young wild boars (P < 0.0001) compared to the adult animals (Table 3. Age related differences in the prevalence were not detected for any of the other parasites.
Fig. 2.
Log-transformed Eimeria spp. faecal oocyst counts (FOC) and, Metastrongylus sp.- and strongyle faecal egg counts (FEC) according to the Trichuris suis infection status (error bars represent the standard deviation)
Discussion
In this study, we investigated 255 Danish wild boars for bacteria and parasites relevant for the public health and the pig production. This is the first study to document these infections in wild boars in Denmark, which prevents comparison of our results with historic Danish data.
The prevalence of A. suum (10.4%) was consistent with the prevalence in wild boars in northern Iran (4.8%) and Estonia (9.0%) [45, 46], while in studies from Turkey and western Iran, Ascaris spp. were absent [33, 47], and yet others recorded a higher prevalence (Italy, 88%) [48]. The differences in prevalence may reflect the different age composition of the studied populations. Age-related resistance against A. suum is recognized [49]. Different sampling seasons and diverse environmental conditions such as e.g. presence or absence of agricultural fields applied with slurry from domestic pigs may also contribute to the different A. suum prevalences reported from various countries. Ascaris suum infection is relatively common in domestic pigs [50], but the parasite is mainly important due to the economic losses caused by liver condemnations and the need for anthelmintic treatment. The long-lived A. suum eggs is a great challenge for outdoor pig production and even a 2–3 year pasture rotation programme may be insufficient to avoid infection since the eggs can remain infective for up to 7 years [51]. In this study, all samples were collected during the hunting season (October to January) corresponding to late autumn and winter. There may be seasonal variations in the egg/oocyst excretion, as development of most parasite species are temperature-dependent. For example, A. suum eggs only embryonate at temperature >14.5 °C, equalling late spring and summer in northern Europe [52]. With a prepatent period of 6–8 weeks [53], a peak in egg excretion might occur during autumn and winter compared to the rest of the year. This also applies for T. suis [52] and Eimeria spp.. Since these parasite eggs/oocysts can remain viable for several years [51, 54], seasonal differences in egg excretion in this study was not expected. Our results indicate that due to the zoonotic risk of A. suum infection, wild boar hunters should take precautions to avoid infection. The main precaution is to avoid contact with faecal material, since A. suum is transmitted through oral intake of embryonated eggs, which may stick to the carcasses.
Besides A. suum, eight parasite genera were identified in the study, including the zoonotic T. suis and Metastrongylus. The predominant species were Eimeria spp. (92.5%) and Metastrongylus sp. (79.5%), which were identified from all sampled enclosures. Wild boars can harbour several Metastrongylus species, including M. asymmetricus, M. confusus, M. elongatus, M. apri, M. pudendotectus and M. salmi [55–57]. Of these, M. elongatus and M. salmi have been identified in humans as well as wild boars [41, 58]. Metastrongylids were not identified to species level, and it is therefore unknown if zoonotic species were present. Metastrongylids have been absent from Danish domestic pigs for decades [59, 60], while historic data for wild boars is non-existent. Metastrongylids are widespread in European wild boars with prevalences of 28.8–60.0% [34, 48, 61], considerably lower than in our study (79.5%). One important exception though, is a prevalence of >80% reported in wild boars from the Estonian Island Saaremaa [45]. The high prevalences reported in this part of Estonia and in Denmark could result from accumulation of eggs in the soil when wild boars inhabit isolated areas, consequently increasing the infection rate in the intermediate hosts. Nagy et al. [62] showed significantly higher Metastrongylus sp. prevalence and infection rate in earthworms in enclosures compared to areas inhabited by free-ranging wild boars. Likewise, feeding sites seemingly constitute a highly infectious reservoir for Metastrongylus sp. in wild boars as egg-containing faeces accumulate and increase the infection rate in earthworms significantly compared to other areas [62]. This was supported by a Spanish study, where feeders were built on concrete bases and Metastrongylus sp. prevalence in wild boars was independent of feeder density [63].
Hunters reported high piglet fatality rates in two enclosures during preceding years in our study. The high mortality might be associated with Metastrongylus sp., and Eimeria spp., considering the high prevalence. In domestic pigs, infections with metastrongylids can be exacerbated by co-existing factors such as secondary bacterial and viral infections [64]. In our study, we observed significantly higher metastrongylid egg counts in wild boars concurrently infected with T. suis compared to T. suis-negative wild boars. This finding indicates that T. suis infection might have the same exacerbating effect on Metastrongylus infection in wild boars as bacteria and viruses. Likewise, wild boars positive for T. suis infection had significantly higher Eimeria spp. FOC and strongyle FEC demonstrating that several parasitic infections in wild boars can be exacerbated by co-infection with T. suis or vice versa; wild boars infected with other parasites are more likely to be infected with T. suis. However, the study design does not allow us to conclude further.
Eimeria spp. infections were also substantially more prevalent (92.5%) in this study than in other studies (7.5–64.2%) [34, 61, 65, 66]. The Eimeria spp. oocysts are environmentally resistant and can survive in the environment for a long time, subsequently leading to accumulation of infective oocysts in enclosures. Thus, the high Eimeria spp. prevalence in Danish wild boars could (Table 3), as for Metastrongylus sp., result from restricting the wild boars in enclosures, and from the close contact between wild boars at the permanent feeding sites.
Although the meat-borne nematode Trichinella spp. was absent in the examined wild boars, total absence of Trichinella spp. in wild boars in Denmark cannot be proven based on our results, as the prevalence may be very low. A Danish study from 2000, identified three Trichinella spp. positive red foxes (0.1%) out of 3133 shoot in 1995–1996 [29]. However, no Trichinella spp. infections have been demonstrated in domestic pigs in Denmark since 1930, and for more than 50 years, no autochthonous human Trichinella spp. infections have been diagnosed in Denmark. This is in contrast to the neighbouring countries (Germany and Sweden), where Trichinella spp. positive wild animals occur [67–69]. The newly built fence along the German–Danish border (finished in 2019) can possibly decrease the risk of Trichinella spp. positive wild boars entering Denmark from Germany.
All the examined wild boars tested negative for B. suis. However, Brucella spp. have been reported in wild boars in other European countries such as Germany, Sweden, Italy, Latvia, and Switzerland [70–72]. In Germany, Al Dahouk et al. [73] found that 22% of wild boar sera were Brucella sp. seropositive, while Swedish wild boars were sero-negative for Brucella sp. in 2013–2015 [74]. The brown hare (Lepus europaeus) may become infected with B. suis biovar 2 [75] as observed for two Danish brown hares that were diagnosed with B. suis biovar 2 in 2002 [76]. Brown hares can thereby act as reservoir for wild boar infection. To our knowledge, brucellosis in Danish brown hares has not been documented since 2002, and it is currently unknown if Danish brown hares constitute a risk for transmission of brucellosis to wild boars.
All wild boars examined in this study tested negative for MRSA. However, MRSA is frequently diagnosed in Danish domestic pigs. In 2018, the screening for MRSA in Denmark showed 20% of the organic pig herds and 89% of the conventional pig farms were positive for MRSA [77]. Outdoor access, lack of antimicrobial usage, and the feed composition was suggested as influencers of low MRSA prevalence in organic pigs [78]. Wild boars are all exclusively housed outdoor and not treated with antimicrobials, but MRSA has previously been diagnosed from wild boars in Portugal [79]. Likewise, all examined wild boars tested negative for Salmonella spp.. In Danish pig herds, Salmonella spp. cases increased substantially in 2010–2013 following low levels in 2004–2009, primarily in piglets [20]. Routine wildlife disease surveillance in 2003–2018 revealed low prevalence of Salmonella spp., with none of the positive animals being wild boars [21]. Salmonella spp. infections are, however, reported in wild boars in other European countries such as Sweden [18], Switzerland [80], and Germany [81]. Overall, Danish wild boars constitute an insignificant risk for transmission of MRSA and Salmonella spp. to domestic pigs or humans. It is more likely that wild boars may acquire these pathogens from the Danish domestic pigs.
Conclusions
Of the examined pathogens, only gastrointestinal parasites and lungworms were identified from the Danish wild boars. The most prevalent parasites were Eimeria spp. (92.3%) and Metastrongylus sp. (79.5%), both of which can be transmitted to domestic pigs. Although human infections are rare, Metastrongylus species are considered potentially zoonotic. Relatively few (10.6 and 8.7%, respectively) of the wild boars were infected with the zoonotic parasites A. suum and T. suis. Therefore, Danish wild boars represent a low risk of transmission to humans, while economically important parasites of domestic pigs were highly prevalent in the wild boars.
Acknowledgements
We thank the local hunters for their collaboration. Furthermore, the laboratory technicians from the parasitology and bacteriology department at the National Veterinary Institute, Technical University of Denmark are acknowledged for their skilled technical assistance.
Prior publication
Data have not been published previously.
Authors’ contributions
HHP collected the samples from 2016–2019, analysed these samples for parasites and was the major contributor in writing the manuscript. HLE and NT collected and analysed the samples for parasites from 2014–2015. STN collected and analysed the samples for parasites in 2019. GL analysed all the samples for Brucella, Salmonella and MRSA. MC made substantial contributions to the conception, designed the study, contacted and got the agreements with the hunters in place and applied for the funding, and participated in the sampling in 2014–2016. All authors read and approved the final manuscript.
Funding
The study was funded by the Danish Veterinary and Food Administration.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval
This study did not require official or institutional ethical approval as no animals were hunted for the purpose of this study. Certified hunters shot the wild boars during the official hunting seasons, and the samples were collected post mortem for a national surveillance program of infectious diseases in wild boars. The data were handled confidentially.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Heidi Huus Petersen, Email: hhpet@vet.dtu.dk.
Nao Takeuchi-Storm, Email: naonow_t@hotmail.com.
Heidi Larsen Enemark, Email: heidi.enemark@vetinst.no.
Stine Thorsø Nielsen, Email: stine.thorso@sund.ku.dk.
Gitte Larsen, Email: gitte_rav_larsen@hotmail.com.
Mariann Chriél, Email: machr@mst.dk.
References
- 1.Massei G, Kindberg J, Licoppe A, Gačić D, Šprem N, Kamler J, et al. Wild boar populations up, numbers of hunters down? A review of trends and implications for Europe. Pest Manag Sci. 2015;71:492–500. doi: 10.1002/ps.3965. [DOI] [PubMed] [Google Scholar]
- 2.Ballari SA, Barrios-García MN. A review of wild boar Sus scrofa diet and factors affecting food selection in native and introduced ranges. Mamm Rev. 2014;44:124–134. [Google Scholar]
- 3.Weismann C. Wildlife and hunting history in Denmark [In Danish] 1. Copenhagen: C.A Reitzels forlag; 1931. [Google Scholar]
- 4.Danish Central Livestock Register. 2019. https://chr.fvst.dk/chri/faces/frontpage?_adf.ctrl-state=yieuuu3rn_3
- 5.Pavic S, Andric A, Sofronic-Milosavljevic LJ, Gnjatovic M, Mitić I, Vasilev S, et al. Trichinella britovi outbreak: epidemiological, clinical, and biological features. Médecine Mal Infect. 2019 doi: 10.1016/j.medmal.2019.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Li TC, Chijiwa K, Sera N, Ishibashi T, Etoh Y, Shinohara Y, et al. Hepatitis E virus transmission from wild boar meat. Emerg Infect Dis. 2005;11:1958–1960. doi: 10.3201/eid1112.051041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cvetnic Z, Mitak M, Ocepek M, Lojkic M, Terzic S, Jemersic L, et al. Wild boars (Sus scrofa) as reservoirs of Brucella suis biovar 2 in Croatia. Acta Vet Hung. 2003;51:465–473. doi: 10.1556/AVet.51.2003.4.4. [DOI] [PubMed] [Google Scholar]
- 8.Franco-Paredes C, Chastain D, Taylor P, Stocking S, Sellers B. Boar hunting and brucellosis caused by Brucella suis. Travel Med Infect Dis. 2017;16:18–22. doi: 10.1016/j.tmaid.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 9.The Danish Veterinary and Food Administration . Animal health in Denmark 2018. 1. Copenhagen: Ministry of Environment and Food of Denmark; 2019. [Google Scholar]
- 10.Danish Agriculture and Food Council. Statistics 2018 pigmeat. Copenhagen. 2019. https://agricultureandfood.dk/prices-and-statistics/annual-statistics
- 11.Gyuranecz M, Erdélyi K, Makrai L, Fodor L, Szépe B, Mészáros ÁR, et al. Brucellosis of the European Brown Hare (Lepus europaeus) J Comp Pathol. 2011;145:1–5. doi: 10.1016/j.jcpa.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 12.Loutfy NF, Awad OM, El-Masry AG, Kandil GM. Study on rodents infestation in Alexandria and prevalence of Trichinella spiralis infection among them. J Egypt Soc Parasitol. 1999;29:897–909. [PubMed] [Google Scholar]
- 13.Poester FP, Samartino LE, Santos RL. Pathogenesis and pathobiology of brucellosis in livestock. Rev Sci Tech Off Int Epiz. 2013;32:105–115. doi: 10.20506/rst.32.1.2193. [DOI] [PubMed] [Google Scholar]
- 14.De Massis F, Zilli K, Di Donato G, Nuvoloni R, Pelini S, Sacchini L, et al. Distribution of Brucella field strains isolated from livestock, wildlife populations, and humans in Italy from 2007 to 2015. PLoS ONE. 2019;14:e0213689. doi: 10.1371/journal.pone.0213689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Godfroid J, Käsbohrer A. Brucellosis in the European Union and Norway at the turn of the twenty-first century. Vet Microbiol. 2002;90:135–145. doi: 10.1016/s0378-1135(02)00217-1. [DOI] [PubMed] [Google Scholar]
- 16.Vieira-Pinto M, Morais L, Caleja C, Themudo P, Torres C, Igrejas G, et al. Salmonella sp. in Game (Sus scrofa and Oryctolagus cuniculus) Foodborne Pathog Dis. 2011;8:739–740. doi: 10.1089/fpd.2010.0742. [DOI] [PubMed] [Google Scholar]
- 17.Chiari M, Zanoni M, Tagliabue S, Lavazza A, Alborali LG. Salmonella serotypes in wild boars (Sus scrofa) hunted in northern Italy. Acta Vet Scand. 2013;55:42. doi: 10.1186/1751-0147-55-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sannö A, Aspán A, Hestvik G, Jacobson M. Presence of Salmonella spp., Yersinia enterocolitica, Yersinia pseudotuberculosis and Escherichia coli O157:H7 in wild boars. Epidemiol Infect. 2014;142:2542–2547. doi: 10.1017/S0950268814000119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.EFSA. The European Union One Health 2018 Zoonoses report. EFSA J. 2019. https://doi.wiley.com/10.2903/j.efsa.2019.5926 [DOI] [PMC free article] [PubMed]
- 20.Pedersen KS, Haugegaard S, Svensmark B. Experiences with Salmonella as a cause of disease in piglets. 2013. https://svineproduktion.dk/publikationer/kilder/notater/2013/1321
- 21.National Veterinary Institute. Annual report of diseases in Danish wildlife 2003–2018. https://www.vildtsundhed.dk/om-vildtsundhed-dk/aarsrapporter
- 22.Guardabassi L, Stegger M, Skov R. Retrospective detection of methicillin resistant and susceptible Staphylococcus aureus ST398 in Danish slaughter pigs. Vet Microbiol. 2007;122:384–386. doi: 10.1016/j.vetmic.2007.03.021. [DOI] [PubMed] [Google Scholar]
- 23.Tang Y, Larsen J, Kjeldgaard J, Andersen PS, Skov R, Ingmer H. Methicillin-resistant and -susceptible Staphylococcus aureus from retail meat in Denmark. Int J Food Microbiol. 2017;249:72–76. doi: 10.1016/j.ijfoodmicro.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 24.Fertner M, Pedersen K, Jensen VF, Larsen G, Lindegaard M, Hansen JE, et al. Within-farm prevalence and environmental distribution of livestock-associated methicillin-resistant Staphylococcus aureus in farmed mink (Neovison vison) Vet Microbiol. 2019;231:80–86. doi: 10.1016/j.vetmic.2019.02.032. [DOI] [PubMed] [Google Scholar]
- 25.Islam MZ, Espinosa-Gongora C, Damborg P, Sieber RN, Munk R, Husted L, et al. Horses in Denmark are a reservoir of diverse clones of methicillin-resistant and -susceptible Staphylococcus aureus. Front Microbiol. 2017;8:543. doi: 10.3389/fmicb.2017.00543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kraushaar B, Fetsch A. First description of PVL-positive methicillin-resistant Staphylococcus aureus (MRSA) in wild boar meat. Int J Food Microbiol. 2014;186:68–73. doi: 10.1016/j.ijfoodmicro.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 27.Porrero MC, Mentaberre G, Sánchez S, Fernández-Llario P, Gómez-Barrero S, Navarro-Gonzalez N, et al. Methicillin resistant Staphylococcus aureus (MRSA) carriage in different free-living wild animal species in Spain. Vet J. 2013;198:127–130. doi: 10.1016/j.tvjl.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 28.Danish Veterinary and Food Administration. Trichinella. https://www.foedevarestyrelsen.dk/english/Food/Trichinella/Pages/default.aspx
- 29.Enemark HL, Bjørn H, Henriksen SA, Nielsen B. Screening for infection of Trichinella in red fox (Vulpes vulpes) in Denmark. Vet Parasitol. 2000;88:229–237. doi: 10.1016/s0304-4017(99)00219-8. [DOI] [PubMed] [Google Scholar]
- 30.McIntyre L, Pollock SL, Fyfe M, Gajadhar A, Isaac-Renton J, Fung J, et al. Trichinellosis from consumption of wild game meat. CMAJ. 2007;176:449–451. doi: 10.1503/cmaj.061530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barutzki D, Schoierer R, Gothe R. Helminth infections in wild boars in enclosures in southern Germany: species spectrum and infection frequency. Tierarztl Prax. 1990;18:529–534. [PubMed] [Google Scholar]
- 32.Foata J, Mouillot D, Culiolo J-L, Marchand B. Influence of season and host age on wild boar parasites in Corsica using indicator species analysis. J Helminthol. 2006;80:41–41. doi: 10.1079/joh2005329. [DOI] [PubMed] [Google Scholar]
- 33.Senlik B, Cirak VY, Girisgin O, Akyol CV. Helminth infections of wild boars (Sus scrofa) in the Bursa province of Turkey. J Helminthol. 2011;85:404–408. doi: 10.1017/S0022149X1000074X. [DOI] [PubMed] [Google Scholar]
- 34.Panayotova-Pencheva M, Dakova V. Studies on the gastrointestinal and lung parasite fauna of wild boars (Sus scrofa scrofa L.) from Bulgaria. Ann Parasitol. 2018;64:379–384. [PubMed] [Google Scholar]
- 35.Roepstorff A, Mejer H, Nejsum P, Thamsborg SM. Helminth parasites in pigs: new challenges in pig production and current research highlights. Vet Parasitol. 2011;180:72–81. doi: 10.1016/j.vetpar.2011.05.029. [DOI] [PubMed] [Google Scholar]
- 36.Knecht D, Popiołek M, Zaleśny G. Does meatiness of pigs depend on the level of gastro-intestinal parasites infection? Prev Vet Med. 2011;99:234–239. doi: 10.1016/j.prevetmed.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 37.Patra G, Prasad H, Lalsiamtha J, Kataria JL, Malsawmkim D, Lalrinkima H. Lungworm infestation in piglets in different parts of Mizoram. India Res J Parasitol. 2013;8:37–44. [Google Scholar]
- 38.Karamon J, Ziomko I, Cencek T. Prevalence of Isospora suis and Eimeria spp. in suckling piglets and sows in Poland. Vet Parasitol. 2007;147:171–175. doi: 10.1016/j.vetpar.2007.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nejsum P, Betson M, Bendall RP, Thamsborg SM, Stothard JR. Assessing the zoonotic potential of Ascaris suum and Trichuris suis: looking to the future from an analysis of the past. J Helminthol. 2012;86:148–155. doi: 10.1017/S0022149X12000193. [DOI] [PubMed] [Google Scholar]
- 40.Leles D, Gardner SL, Reinhard K, Ĩiguez A, Araujo A. Are Ascaris lumbricoides and Ascaris suum a single species? Parasit Vectors. 2012;5:42. doi: 10.1186/1756-3305-5-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Calvopina M, Caballero H, Morita T, Korenaga M. Case report: human pulmonary infection by the zoonotic metastrongylus salmi nematode. The first reported case in the Americas. Am J Trop Med Hyg. 2016;95:871–873. doi: 10.4269/ajtmh.16-0247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kakihara D, Yoshimitsu K, Ishigami K, Irie H, Aibe H, Tajima T, et al. Liver lesions of visceral larva migrans due to Ascaris suum infection: CT findings. Abdom Imaging. 2004;29:598–602. doi: 10.1007/s00261-003-0153-4. [DOI] [PubMed] [Google Scholar]
- 43.Mayer-Scholl A, Pozio E, Gayda J, Thaben N, Bahn P, Nöckler K. Magnetic stirrer method for the detection of Trichinella larvae in muscle samples. J Vis Exp. 2017;121:e55354. doi: 10.3791/55354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Roepstorff A, Nansen P. Epidemiology, diagnosis and control of helminth parasites of swine. Rome: FAO Animal Health Manual; 1998. [Google Scholar]
- 45.Järvis T, Kapel C, Moks E, Talvik H, Mägi E. Helminths of wild boar in the isolated population close to the northern border of its habitat area. Vet Parasitol. 2007;150:366–369. doi: 10.1016/j.vetpar.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 46.Dodangeh S, Azami D, Daryani A, Gholami S, Sharif M, Mobedi I, et al. Parasitic helminths in wild boars (Sus scrofa) in Mazandaran Province, northern Iran. Iran J Parasitol. 2018;13:416–422. [PMC free article] [PubMed] [Google Scholar]
- 47.Solaymani-Mohammadi S, Rezaian M, Hooshyar H, Mowlavi GR, Babaei Z, Anwar MA. Intestinal protozoa in wild boars (Sus scrofa) in western Iran. J Wildl Dis. 2004;40:801–803. doi: 10.7589/0090-3558-40.4.801. [DOI] [PubMed] [Google Scholar]
- 48.Castagna F, Musella V, Esposito L, Poerio A, Rinaldi L, Bosco A, et al. Helminths of wild boar (Sus scrofa) in the Calabrian region of Southern Italy. J Wildl Dis. 2019;55:416. doi: 10.7589/2018-02-028. [DOI] [PubMed] [Google Scholar]
- 49.Pedersen S, Saeed I. Acquired immunity to Trichuris suis infection in pigs. Parasitology. 2001;123:95–101. doi: 10.1017/s0031182001007934. [DOI] [PubMed] [Google Scholar]
- 50.Roepstorff A, Nilsson O, Oksanen A, Gjerde B, Richter SH, Örtenberg E, et al. Intestinal parasites in swine in the Nordic countries: prevalence and geographical distribution. Vet Parasitol. 1998;76:305–319. doi: 10.1016/s0304-4017(97)00223-9. [DOI] [PubMed] [Google Scholar]
- 51.Thamsborg SM, Roepstorff AK, Monrad J. Veterinary parasitology, helmintology for veterinary students [In Danish]. 7th edition. Sygdomsbiologi I for V. Frederiksberg, Denmark: Academic books; 2013.
- 52.Larsen MN, Roepstorff A. Seasonal variation in development and survival of Ascaris suum and Trichuris suis eggs on pastures. Parasitology. 1999;119:209–220. doi: 10.1017/s0031182099004503. [DOI] [PubMed] [Google Scholar]
- 53.Roepstorff A, Eriksen L, Slotved HC, Nansen P. Experimental Ascaris suum infection in the pig: worm population kinetics following single inoculations with three doses of infective eggs. Parasitology. 1997;115:443–452. doi: 10.1017/s0031182097001480. [DOI] [PubMed] [Google Scholar]
- 54.Kates KC. Observations on the viability of eggs of lungworms of swine. J Parasitol JSTOR. 1941;27:265–272. [Google Scholar]
- 55.García-González AM, Pérez-Martín JE, Gamito-Santos JA, Calero-Bernal R, Alonso MA, Carrió EM. Epidemiologic study of lung parasites (Metastrongylus spp.) in wild boar (Sus scrofa) in southwestern Spain. J Wildl Dis. 2013;49:157–162. doi: 10.7589/2011-07-217. [DOI] [PubMed] [Google Scholar]
- 56.Eslami A, Farsad-Hamdi S. Helminth parasites of wild boar, Sus scrofa, in Iran. J Wildl Dis. 1992;28:316–318. doi: 10.7589/0090-3558-28.2.316. [DOI] [PubMed] [Google Scholar]
- 57.Humbert J-F, Henry C. Studies on the prevalence and the transmission of lung and stomach nematodes of wild boar (Sus scrofa) in France. J Wildl Dis. 1989;25:335–341. doi: 10.7589/0090-3558-25.3.335. [DOI] [PubMed] [Google Scholar]
- 58.Miloshev B. Case of triple infection with Metastrongylus elongatus, Thaeniarhynchus saginatus and Enterobius vermicularis [In Bulgarian] Suvr Med (Sofiia) 1956;7:94–97. [PubMed] [Google Scholar]
- 59.Carstensen L, Vaarst M, Roepstorff A. Helminth infections in Danish organic swine herds. Vet Parasitol. 2002;106:253–264. doi: 10.1016/s0304-4017(02)00080-8. [DOI] [PubMed] [Google Scholar]
- 60.Roepstorff A, Jorsal SE. Prevalence of helminth infections in swine in Denmark. Vet Parasitol. 1989;33:231–239. doi: 10.1016/0304-4017(89)90133-7. [DOI] [PubMed] [Google Scholar]
- 61.Oja R, Velström K, Moks E, Jokelainen P, Lassen B. How does supplementary feeding affect endoparasite infection in wild boar? Parasitol Res. 2017;116:2131–2137. doi: 10.1007/s00436-017-5512-0. [DOI] [PubMed] [Google Scholar]
- 62.Nagy G, Csivincsik Á, Sugár L. Wild boar density drives Metastrongylus infection in earthworm. Acta Parasitol. 2015;60:35–39. doi: 10.1515/ap-2015-0005. [DOI] [PubMed] [Google Scholar]
- 63.Navarro-Gonzalez N, Fernández-Llario P, Pérez-Martín JE, Mentaberre G, López-Martín JM, Lavín S, et al. Supplemental feeding drives endoparasite infection in wild boar in Western Spain. Vet Parasitol. 2013;196:114–123. doi: 10.1016/j.vetpar.2013.02.019. [DOI] [PubMed] [Google Scholar]
- 64.Marruchella G, Paoletti B, Speranza R, Di Guardo G. Fatal bronchopneumonia in a Metastrongylus elongatus and Porcine circovirus type 2 co-infected pig. Res Vet Sci. 2012;93:310–312. doi: 10.1016/j.rvsc.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 65.Pilarczyk B, Balicka-Ramisz A, Cisek A, Szalewska K, Lachowska S. Prevalence of Eimeria and intestinal nematodes in wild boar in north-west Poland. Wiad Parazytol. 2004;50:637–640. [PubMed] [Google Scholar]
- 66.Molnár L, Beregi A, Gyurkovszky M, Farkas R, Molnar L, Heltai M. Coccidiosis in wild boars shot in the south region of Mátra in Hungary [In Hungarian] Magy Állatorvosok Lapja. 2013;135:622–624. [Google Scholar]
- 67.Chmurzyńska E, Rózycki M, Bilska-Zajac E, Nöckler K, Mayer-Scholl A, Pozio E, et al. Trichinella nativa in red foxes (Vulpes vulpes) of Germany and Poland: Possible different origins. Vet Parasitol. 2013;198:254–257. doi: 10.1016/j.vetpar.2013.07.034. [DOI] [PubMed] [Google Scholar]
- 68.Pannwitz G, Mayer-Scholl A, Balicka-Ramisz A, Nöckler K. Increased prevalence of Trichinella spp., northeastern Germany, 2008. Emerg Infect Dis. 2010;16:936–942. doi: 10.3201/eid1606.091629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.EFSA The European Union summary report on trends and sources of zoonoses, zoonotic agents and food-borne outbreaks in. EFSA J. 2018;16:e05500. doi: 10.2903/j.efsa.2018.5500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Leuenberger R, Boujon P, Thür B, Miserez R, Garin-Bastuji B, Rüfenacht J, et al. Prevalence of classical swine fever, Aujeszky’s disease and brucellosis in a population of wild boar in Switzerland. Vet Rec. 2007;160:362–368. doi: 10.1136/vr.160.11.362. [DOI] [PubMed] [Google Scholar]
- 71.Grantina-Ievina L, Avsejenko J, Cvetkova S, Krastina D, Streikisa M, Steingolde Z, et al. Seroprevalence of Brucella suis in eastern Latvian wild boars (Sus scrofa) Acta Vet Scand. 2018;60:19. doi: 10.1186/s13028-018-0373-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Di Sabatino D, Garofolo G, Di Provvido A, Zilli K, Foschi G, Di Giannatale E, et al. Brucella suis biovar 2 multi locus sequence type ST16 in wild boars (Sus scrofa) from Abruzzi region, Italy. Introduction from Central-Eastern Europe? Infect Genet Evol. 2017;55:63–67. doi: 10.1016/j.meegid.2017.08.031. [DOI] [PubMed] [Google Scholar]
- 73.Al Dahouk S, Nöckler K, Tomaso H, Splettstoesser WD, Jungersen G, Riber U, et al. Seroprevalence of brucellosis, tularemia, and yersiniosis in wild boars (Sus scrofa) from North-Eastern Germany. J Vet Med Ser B. 2005;52:444–455. doi: 10.1111/j.1439-0450.2005.00898.x. [DOI] [PubMed] [Google Scholar]
- 74.Malmsten A, Magnusson U, Ruiz-Fons F, González-Barrio D, Dalin AM. A serologic survey of pathogens in wild boar (Sus scrofa) in Sweden. J Wildl Dis. 2018;54:229–237. doi: 10.7589/2017-05-120. [DOI] [PubMed] [Google Scholar]
- 75.Godfroid J. Brucellosis in wildlife. Rev Sci Tech l’OIE. 2002;21:277–286. doi: 10.20506/rst.21.2.1333. [DOI] [PubMed] [Google Scholar]
- 76.The National Veterinary Institute. Annual report of diseases in Danish wildlife 2003 [In Danish]. 2003. https://www.vildtsundhed.dk/om-vildtsundhed-dk/aarsrapporter
- 77.Danish Veterinary and Food Administration. The results of screening for domestic MRSA in pigs in 2018 [In Danish]. 2019.
- 78.van de Vijver LPL, Tulinski P, Bondt N, Mevius D, Verwer C. Prevalence and molecular characteristics of methicillin-resistant Staphylococcus aureus (MRSA) in organic pig herds in the Netherlands. Zoonoses Public Health. 2014;61:338–345. doi: 10.1111/zph.12076. [DOI] [PubMed] [Google Scholar]
- 79.Sousa M, Silva N, Manageiro V, Ramos S, Coelho A, Gonçalves D, et al. First report on MRSA CC398 recovered from wild boars in the north of Portugal. Are we facing a problem? Sci Total Environ. 2017;596–597:26–31. doi: 10.1016/j.scitotenv.2017.04.054. [DOI] [PubMed] [Google Scholar]
- 80.Wacheck S, Fredriksson-Ahomaa M, König M, Stolle A, Stephan R. Wild boars as an important reservoir for foodborne pathogens. Foodborne Pathog Dis. 2010;7:307–312. doi: 10.1089/fpd.2009.0367. [DOI] [PubMed] [Google Scholar]
- 81.Methner U, Heller M, Bocklisch H. Salmonella enterica subspecies enterica serovar Choleraesuis in a wild boar population in Germany. Eur J Wildl Res. 2010;56:493–502. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.