Abstract
Background: Surgical site infections (SSIs) represent a major cause of morbidity and mortality in Ethiopia. Lack of post-discharge follow-up, including identification of SSIs, is a barrier to continued patient care, often because of financial and travel constraints. As part of a surgical quality improvement initiative, we aimed to assess patient outcomes at 30 days post-operative with a telephone call.
Patients and Methods: We conducted mobile telephone follow-up as part of Lifebox's ongoing Clean Cut program, which aims to improve compliance with intra-operative infection prevention standards. One urban tertiary referral hospital and one rural district general hospital in Ethiopia were included in this phase of the study; hospital nursing staff called patients at 30 days post-operative inquiring about signs of SSIs, health-care–seeking behavior, and treatments provided if patients had any healthcare encounters since discharge.
Results: A total of 701 patients were included; overall 77% of patients were reached by telephone call after discharge. The rural study site reached 362 patients (87%) by telephone; the urban site reached 176 patients (62%) (p < 0.001). Of the 39 SSIs identified, 19 (49%) were captured as outpatient during the telephone follow-up (p < 0.001); 22 (34%) of all complications were captured following discharge (p < 0.001). Telephone follow-up improved from 65%–78% in the first half of project implementation to 77%–89% in the second half of project implementation.
Conclusion: Telephone follow-up after surgery in Ethiopia is feasible and valuable, and identified nearly half of all SSIs and one-third of total complications in our cohort. Follow-up improved over the course of the program, likely indicating a learning curve that, once overcome, is a more accurate marker of its practicability. Given the increasing use of mobile telephones in Ethiopia and ease of implementation, this model could be practical in other low-resource surgical settings.
Keywords: low- and middle-income countries, patient follow-up, surgical outcomes
Surgical site infections (SSIs) are a primary factor of patient morbidity and mortality after surgical procedures [1], are more common in low-resource settings [2], and have enormous impact on financial well-being of patients and health systems [3,4]. Moreover, SSIs represent the leading hospital-acquired infection in sub-Saharan Africa [5]. Although there are few studies in Africa examining the impact of SSI prevention programs [6], evidence-based interventions focused on improving antibiotic administration, proper hair removal, glycemic control, and other targets have been shown to reduce surgical infections both in high- and low-income settings [7–10]. In Ethiopia, prior studies in Tigray [11] and Hawassa [12] using chart review and patient interviews have shown rates of SSIs from 11% to 19%. Additionally, SSI prevention is an expressed priority of the Federal Ministry of Health [13].
A major limitation of many large-scale studies of SSI is poor follow-up [2], particularly after discharge [14]. Several strategies are used commonly to obtain 30-day patient follow-up information after surgery, including direct observation in post-operative clinic visits or chart review, however, each has shortcomings, particularly in low-resource settings. In Cambodia, SSI identification by telephone call versus chart review showed a sensitivity of just 16% [15]. In Kenya, one study showed that less than 25% of patients attend their post-operative appointments [16].
Previous work from our group [17] found that in surgical patients in Ethiopia, loss to follow-up is high and chart review alone was not sufficient to determine outcomes. In this study, we aimed to assess the feasibility and ability to follow-up surgical patients using a telephone call to capture site infection and other complications in patients who would not have otherwise had any follow-up at all. We also aimed to determine the proportion of post-operative patient outcomes identified in inpatient versus the outpatient setting and determine any differences in urban and rural settings in our success of reaching patients by telephone.
Patients and Methods
As part of an ongoing, multimodal surgical quality improvement program, we collected data on operations performed at two hospitals over a six-month time period. The Clean Cut program is a quality improvement initiative to improve perioperative infection prevention practices and the methodology of this program has been described previously [18]. In brief, infection prevention behaviors were observed directly in the operating room by trained operating room nurses and anesthetists in six domains: hand scrubbing and patient skin preparation; antibiotic administration; gown and drape integrity; instrument sterility, gauze counting; and use of the Surgical Safety Checklist. Patients were followed daily on the wards with direct observation of surgical site and chart review by trained ward nurses; information on complications including surgical infection, re-operations, pneumonia, urinary tract infection, and mortality were recorded. After discharge, patients received a telephone call by a surgical ward nurse 30 days after their operation. The patient, or family member if patient was unable to communicate, was asked questions about signs of surgical infection, health-care–seeking behaviors, and mortality. Nurses performing data collection were also trained on the definition and diagnosis of SSI. Data collected were entered into Excel (Microsoft, Redmond, WA) and analysis was performed using Stata 15.1 (StataCorp, College Station, TX). Descriptive statistics, Student t-test, and χ2 tests for significance were performed; a two-sided α level <0.05 was considered to be significant. Because this was a quality improvement project incorporating evidence-based standards into practice, Institutional Review Board approval was not pursued; administrators and surgical department heads of each hospital approved the program.
SSI definition
We used a modified definition of SSIs as described previously by our group [18] as well as the GlobalSurg collaborative [2], modified from the U.S. Centers for Disease Control and Infection (CDC) definition [19]. Our definition of SSI included: purulent drainage from incision; abscess within the incision (or on imaging); a combination of erythema or fever; and opening of the incision (either spontaneously or deliberately by provider). Because our study hospitals do not routinely have microbiology laboratory services, we did not include incision culture in our diagnostic criteria; pain and heat from the incision were similarly removed from our definition of SSI because they are difficult to assess in our context and highly subjective.
Hospital settings
The urban hospital is a large referral center in Addis Ababa, Ethiopia, with 267 beds and four functioning operating rooms, staffed by general surgeons, obstetrics/gynecology, and other subspecialties including neurosurgery and orthopedic surgery. Surgical volume is an average of 72 cases per month. This hospital is a referral center for four hospitals and 11 health centers in the surrounding Addis Ababa and Oromia regions. In contrast, the rural hospital is a general hospital with 40 beds and two operating rooms staffed by one gynecologist and several mid-level general surgery providers (Integrated Emergency Surgical Officers; IESOs). Surgical volume is an average of 93 cases per month.
Telephone call mechanism
Ward nurses kept a log of inpatients after surgery with the date of surgery and the date of discharge, as well as several telephone numbers that the patients provided to be contacted. On or about the thirtieth post-operative day, one of the ward nurses placed a telephone call to the patients who were due for follow-up each day. Nurses called each patient on their follow-up due date to ask about any drainage from the surgical site and if so, the type of drainage, as well as any healthcare visits and type of care provided at such since discharge. If the patient had died, this was also recorded. Data were recorded on paper forms and entered into Excel by members of the Clean Cut team. Nurses were provided with the equivalent of $7.00 USD per month in mobile telephone data to place calls. Full details of the telephone call data collection form can be found in Appendix A.
Results
A total of 701 patients from two hospitals were enrolled over the six-month course of the program, 415 from the rural and 286 from the urban hospitals (Table 1). Overall, patients were young with a mean age of 29.5 years; patients at the urban hospital were slightly older (32 vs. 28, p < 0.001). Patients had low and similar rates of hypertension (0.7%) and diabetes (0.3%) and were predominantly female (84%); there were no substantial differences between these demographic features between the two facilities. Cases in the rural hospital were evenly split between obstetric and main operating rooms (48% vs. 52%), whereas more cases were done in the obstetric operating room in the urban hospital (65% vs. 35%, p < 0.001). Overall, the majority of cases were done on an emergency basis (78%), with the proportion of emergency cases being higher at the rural versus urban hospital (89% vs. 63%, p ≤ 0.001).
Table 1.
Case Mix and Patient Demographics
| Facility |
Rural Hospital |
Urban Hospital |
Overall |
|
|---|---|---|---|---|
| n | 415 | 286 | 701 | p |
| Patient age, mean (SD) | 27.9 (11.2) | 31.9 (12.9) | 29.5 (12.1) | <0.001 |
| Hypertension | 1 (0.2%) | 4 (1.4%) | 5 (0.7%) | 0.073 |
| Diabetes | 1 (0.2%) | 1 (0.3%) | 2 (0.3%) | 0.79 |
| Patient gender | 0.79 | |||
| Female | 348 (83.9%) | 242 (84.6%) | 590 (84.2%) | |
| Male | 67 (16.1%) | 44 (15.4%) | 111 (15.8%) | |
| Location of surgery | <0.001 | |||
| Main operating room | 214 (51.6%) | 99 (34.6%) | 313 (44.7%) | |
| obstetric operating room | 201 (48.4%) | 187 (65.4%) | 388 (55.3%) | |
| Urgency of case | <0.001 | |||
| Elective | 47 (11.3%) | 104 (36.4%) | 151 (21.5%) | |
| Emergency | 368 (88.7%) | 182 (63.3%) | 550 (78.3%) |
SD = standard deviation.
Completion of follow-up and patient outcomes
Mean hospital length of stay was 3.7 days at the urban hospital and 4.6 days at the rural hospital (p < 0.001; Table 2). Four patients (0.6%) required re-operation, all of whom were at the urban facility. At the rural facility, six (1.4%) patients developed a urinary tract infection post-operatively, and 14 (3.4%) developed pneumonia, compared with the urban facility that had no urinary tract infections (p = 0.04) and one (0.3%) pneumonia (p = 0.007). Surgical site infections were fairly low, with overall rate of 5.6%. Of the 39 total SSI diagnosed, 20 (51%) were diagnosed in the inpatient setting, whereas 19 (49%) were diagnosed after discharge (p < 0.001). The urban site had higher SSI incidence (7.7%) compared with the rural hospital (4.1%, p = 0.04). There were five (0.7%) total deaths in the cohort during the study period, three of which occurred in the outpatient setting and were captured by telephone follow-up. When measuring all complications including surgical infections, other hospital-acquired infections and deaths, 22 of the 64 identified complications (34%) were reported after hospital discharge.
Table 2.
Completion of Follow-Up and Patient Outcomes
| Factor |
Rural Setting |
Urban Setting |
Overall |
|
|---|---|---|---|---|
| n | 415 | 286 | 701 | p |
| LOS, mean (SD) | 4.6 (2.1) | 3.7 (2.6) | 4.3 (2.4) | <0.001 |
| Re-operation | 0 (0.0%) | 4 (1.4%) | 4 (0.6%) | 0.016 |
| Endometritis | 0 (0.0%) | 2 (0.7%) | 2 (0.3%) | 0.088 |
| Chorioamnionitis | 0 (0.0%) | 3 (1.0%) | 3 (0.4%) | 0.037 |
| Meningitis | 0 (0.0%) | 1 (0.3%) | 1 (0.1%) | 0.23 |
| Urinary tract infection | 6 (1.4%) | 0 (0.0%) | 6 (0.9%) | 0.041 |
| Pneumonia | 14 (3.4%) | 1 (0.3%) | 15 (2.1%) | 0.007 |
| Pelvic inflammatory disease | 0 (0.0%) | 1 (0.3%) | 1 (0.1%) | 0.23 |
| All infectious complications | 32 (7.7%) | 29 (10.1%) | 61 (8.7%) | 0.26 |
| Inpatient SSI | 7 (1.7%) | 13 (4.5%) | 20 (2.9%) | 0.025 |
| Outpatient SSI | 10 (2.4%) | 9 (3.1%) | 19 (2.7%) | 0.55 |
| Overall SSI | 17 (4.1%) | 22 (7.7%) | 39 (5.6%) | 0.041 |
| Inpatient deaths | 0 (0.0%) | 2 (0.7%) | 2 (0.3%) | 0.088 |
| Outpatient deaths at 30 d | 1 (0.2%) | 2 (0.7%) | 3 (0.4%) | 0.36 |
| Total deaths | 1 (0.2%) | 4 (1.4%) | 5 (0.7%) | 0.073 |
| All inpatient complications | 22 (5.3%) | 20 (7.0%) | 42 (6.0%) | 0.35 |
| All outpatient complications | 11 (2.7%) | 11 (3.8%) | 22 (3.1%) | 0.37 |
| Overall complications | 33 (8.0%) | 31 (10.8%) | 64 (9.1%) | 0.19 |
| Completed inpatient follow up | 407 (98.1%) | 261 (91.3%) | 668 (95.3%) | <0.001 |
| Completed phone follow up | 362 (87.2%) | 176 (61.5%) | 538 (76.7%) | <0.001 |
LOS = length of stay; SD = standard deviation; SSI = surgical site infection.
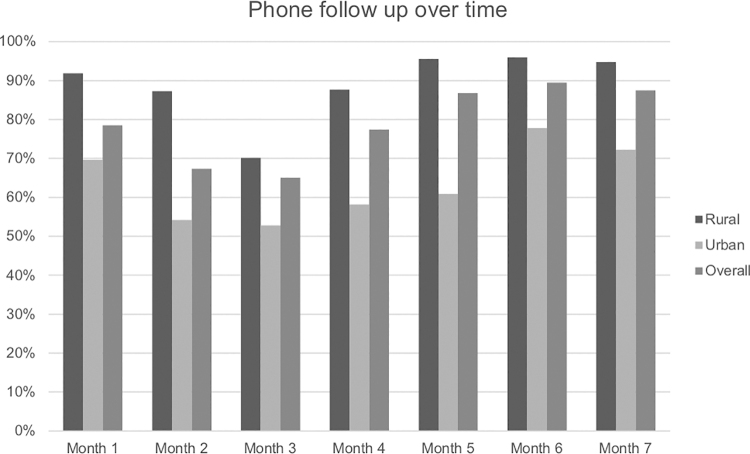
More than 95% (n = 668) of patients enrolled intra-operatively were followed to discharge with greater success at the rural hospital (261 [91%] urban, 407 [98%] rural, p < 0.001; Table 3). Overall, 538 of the 701 patients (77%) were reached by telephone for follow-up at 30 days after surgery. Successful telephone follow-up was greater at the rural hospital (87% vs. 62%, p < 0.001). The proportion of patients reached by telephone also improved over the course of the program, with between 53% and 70% of patients reached at the urban site in the first half of the program, and 61%–78% reached in the latter half of the program (p < 0.001; Fig. 1). The rural site performed better overall at 30-day follow-up, but also improved over the course of the program, from 70%–92% of patients reached in the first half, and 87%–96% reached in the latter half (p < 0.001).
Table 3.
Telephone Follow-Up Over Time
| Factor |
|
Month 1 |
Month 2 |
Month 3 |
Month 4 |
Month 5 |
Month 6 |
Month 7 |
|
|---|---|---|---|---|---|---|---|---|---|
| n | Hospital | 93 | 138 | 123 | 124 | 91 | 76 | 56 | p |
| Follow to discharge | Urban | 53 (95%) | 70 (84%) | 34 (94%) | 40 (93%) | 20 (87%) | 26 (96%) | 18 (100%) | |
| Rural | 36 (97%) | 52 (95%) | 83 (95) | 81 (100%) | 68 (100%) | 49 (100%) | 38 (100%) | ||
| Overall | 89 (96%) | 122 (88%) | 117 (95%) | 121 (98%) | 88 (97%) | 75 (99%) | 56 (100%) | 0.002 | |
| 30-d telephone call | Urban | 39 (70%) | 45 (54%) | 19 (53%) | 25 (58%) | 14 (61%) | 21 (78%) | 13 (72%) | |
| Rural | 34 (92%) | 48 (87%) | 61 (70%) | 71 (88%) | 65 (96%) | 47 (96%) | 36 (95%) | ||
| Overall | 73 (78.5%) | 93 (67.4%) | 80 (65.0%) | 96 (77.4%) | 79 (86.8%) | 68 (89.5%) | 49 (87.5%) | <0.001 |
FIG. 1.
Monthly telephone call rates by site.
Discussion
As part of implementation of a multimodal surgical quality improvement program in Ethiopia, we noted high rates of telephone follow-up in this cohort of surgical patients from both urban and rural environments and were able to reach more than 75% of patients by telephone after discharge. The information obtained from telephone follow-up was meaningful to the program: nearly half of SSIs diagnosed were captured in the outpatient setting, as were more than one-third of all post-operative complications. Furthermore, our success in reaching patients improved from 65% to 95% over the course of the program, indicating that incorporating this strategy into the nursing and hospital workflow requires some adaption, training, and modification of daily routine. Telephone call follow-up appears to be a practical and effective way to communicate with Ethiopian patients after discharge.
Surgical infections are a major contributor to morbidity and mortality, particularly in severely resource-limited environments such as Ethiopia. The African Surgical Outcomes Study [20] found that of 11,000 surgical cases performed in sub-Saharan African countries, 10.2% developed SSI in the first seven days after surgery and of those, 9.7% died. Prior bundled SSI reduction interventions have resulted in substantially reduced rates of SSI, but follow-up has been challenging, requiring a combination of chart review, clinic visits, and telephone calls [21]. Our approach used telephone calls only, which does not include the element of clinical evaluation but also is not reliant on patients returning to the treatment hospital and allows for more complete follow-up. Another study in Cambodia combined strategies of providing patients with a standardized follow-up card at discharge that could be completed by any provider, and a telephone call from the surgical hospital at 30 days [22]. This study found that, similar to our population, 87% of patients were able to be reached by telephone and 17% of patients had SSIs (as defined by purulent drainage) that had not been diagnosed in the inpatient setting. Of these, approximately 30% of SSIs that were reported by patients were not reported by clinicians, but no SSIs were diagnosed on the follow-up card only and not reported by the patient themselves.
Chart review in a prior study in one Ethiopian hospital [17] yielded a surgical infection rate of 5% and a 28% loss to follow-up, whereas prospective direct observation showed the SSI rate was 14% in this cohort. However, in this cohort, follow-up after hospital discharge was also performed by chart review of any follow-up clinic visits, and also may not capture complications adequately. Another study in the Sudan [23] investigating the use of post-discharge telephone calls for patients after surgery found that 78% of patients were contacted successfully after discharge, and the vast majority of surgical infections (6.8% outpatient vs. 0.8% inpatient) were detected during the telephone call. These findings are important because patients often need to travel long distances for care and, once they return home, have difficulty coming back to the hospital where they received care. Following patients by telephone is cost effective and more practical for the majority of patients involved.
There are a number of important limitations to our study. We did not corroborate our findings of diagnosed SSIs on telephone call with a clinical assessment, there is a chance that patients may have described signs and symptoms incorrectly leading to missed diagnoses of SSIs. Additionally, patients were not randomized to any other follow-up mechanism to determine if a telephone call was indeed the most successful strategy. However, without a telephone call many patients would have had no follow-up at all. Patients reporting signs and symptoms of surgical infection or other worrisome clinical finding were counseled to see health care, however, we had no assurance that patients counseled to seek care did so. Furthermore, the provision of mobile telephone data was a cost covered by the Clean Cut program and made calling hundreds of patients feasible. At subsequent sites a hospital landline has been designated for patient telephone call follow-up, however, whatever strategy is used is not completely free for the hospital and must be considered practically. There seemed to be a learning curve to the telephone call follow-up workflow, Initially, it was viewed as an additional burden to the nursing staff, and attention must be paid to integrating the telephone follow-up into the typical nursing responsibilities and workflow. Additionally, the knowledge and practice of nurses in Ethiopia related to SSI prevention have been studied previously and found to be unsatisfactory [24], particularly among junior nurses. It is possible that training and experience in this role of outpatient communication with patients would benefit nurses' clinical acumen and other behaviors in the workplace. A qualitative study of the Clean Cut program [25] revealed themes supporting this concept previously, with nurses reporting increased job satisfaction and a sense of value in reaching out to patients after discharge.
Conclusion
In resource-limited settings, where in-person post-operative follow-up is challenging and often prohibitively expensive for patients, we found that a telephone call for follow-up was an effective and affordable strategy for contacting patients and capturing complications after surgery. This strategy allowed us to identify nearly half of surgical infections in our cohort and one-third of overall complications and had the added benefit of increased engagement and satisfaction of nurses involved in patient care. We found that follow up with 30-day telephone call after surgery is feasible even in rural and low-resource settings and assert that this strategy is important for improving data quality on surgical outcomes. Post-discharge telephone calls after surgery may be useful to utilize in other resource-limited environments and beyond and could provide a simple and effective way for more accurate measurement of surgical complications, as well as an opportunity to connect with and triage patients to appropriate care.
Acknowledgments
The authors extend their sincere thanks to the entire team of nurses, physicians and other hospital staff engaged in the Clean Cut program, as well as the Ethiopian Federal Ministry of Health for their institutional support of the program.
Appendix A.
Telephone Call Data Collection Form
Funding Information
The Clean Cut program was funded in part by the GE Foundation. NS is supported by NIH T32 DK007573 grant.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Allegranzi B, Bagheri Nejad S, Combescure C, Graafmans W, Attar H, Donaldson L, et al. Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. Lancet 2011;377:228–241 [DOI] [PubMed] [Google Scholar]
- 2. GlobalSurg Collaborative. Surgical site infection after gastrointestinal surgery in high-income, middle-income, and low-income countries: A prospective, international, multicentre cohort study. Lancet Infect Dis 2018;18:516–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shepard J, Ward W, Milstone A, et al. Financial impact of surgical site infections on hospitals: The hospital management perspective. JAMA Surg 2013;148:907–914 [DOI] [PubMed] [Google Scholar]
- 4. Jha AK, Larizgoitia I, Audera-Lopez C, et al. The global burden of unsafe medical care: Analytic modelling of observational studies. BMJ Qual Saf 2013; 22:809–815 [DOI] [PubMed] [Google Scholar]
- 5. Rothe C, Schlaich C, Thompson S. Healthcare-associated infections in sub-Saharan Africa. J Hosp Infect 2013;85:257–267 [DOI] [PubMed] [Google Scholar]
- 6. Aiken AM, Karuri DM, Wanyoro AK, Macleod J. Interventional studies for preventing surgical site infections in sub-Saharan Africa—A systematic review. Int J Surg 2012;10:242–249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Munday GS, Deveaux P, Roberts H, et al. Impact of implementation of the Surgical Care Improvement Project and future strategies for improving quality in surgery. Am J Surg 2014;208:835–840 [DOI] [PubMed] [Google Scholar]
- 8. Kilan R, Moran D, Eid I, et al. Improving antibiotic prophylaxis in gastrointestinal surgery patients: A quality improvement project. Ann Med Surg (Lond) 2017;20:6–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cataife G, Weinberg DA, Wong H-H, Kahn KL. The effect of Surgical Care Improvement Project (SCIP) compliance on surgical site infections (SSI). Med Care 2014;52(2 Suppl 1):S66–73 [DOI] [PubMed] [Google Scholar]
- 10. Tanner J, Padley W, Assadian O, et al. Do surgical care bundles reduce the risk of surgical site infections in patients undergoing colorectal surgery? A systematic review and cohort meta-analysis of 8,515 patients. Surgery 2015;158:66–77 [DOI] [PubMed] [Google Scholar]
- 11. Weldu MG, Berhane H, Berhe N, et al. Magnitude and eeterminant factors of surgical site infection in Suhul Hospital Tigrai, Northern Ethiopia: A cross-sectional study. Surg Infect 2018;19:684–690 [DOI] [PubMed] [Google Scholar]
- 12. Legesse Laloto T, Hiko Gemeda D, Abdella SH. Incidence and predictors of surgical site infection in Ethiopia: Prospective cohort. BMC Infect Dis 2017;17:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Burssa D, Teshome A, Iverson K, et al. Safe surgery for all: Early lessons from implementing a national government-driven surgical plan in Ethiopia. World J Surg 2017;41:3038–3045 [DOI] [PubMed] [Google Scholar]
- 14. Biccard BM, Madiba TE, Kluyts H-L, et al. Perioperative patient outcomes in the African Surgical Outcomes Study: A 7-day prospective observational cohort study. Lancet 2018;391:1589–1598 [DOI] [PubMed] [Google Scholar]
- 15. Guerra J, Guichon C, Isnard M, et al. Active prospective surveillance study with post-discharge surveillance of surgical site infections in Cambodia. J Infect Public Health 2015;8:298–301 [DOI] [PubMed] [Google Scholar]
- 16. Aiken AM, Wanyoro AK, Mwangi J, et al. Evaluation of surveillance for surgical site infections in Thika Hospital, Kenya. J Hosp Infect 2013;83:140–145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Forrester JA, Koritsanszky L, Parsons BD, et al. Development of a surgical infection surveillance program at a tertiary hospital in Ethiopia: Lessons learned from two surveillance strategies. Surg Infect 2018;19:25–32 [DOI] [PubMed] [Google Scholar]
- 18. Forrester JA, Koritsanszky LA, Amenu D, et al. Developing process maps as a tool for a surgical infection prevention quality improvement initiative in resource-constrained settings. J Am Coll Surg 2018;226:1103–1116 [DOI] [PubMed] [Google Scholar]
- 19. Centers for Disease Control. 9 Surgical Site Infection (SSI) Event. 2020;36
- 20. Biccard BM, Madiba TE, Kluyts H-L, et al. Perioperative patient outcomes in the African Surgical Outcomes Study: A 7-day prospective observational cohort study. Lancet 2018;391:1589–1598 [DOI] [PubMed] [Google Scholar]
- 21. Allegranzi B, Aiken AM, Zeynep Kubilay N, et al. A multimodal infection control and patient safety intervention to reduce surgical site infections in Africa: A multicentre, before-after, cohort study. Lancet Infect Dis 2018;18:507–515 [DOI] [PubMed] [Google Scholar]
- 22. Guerra J, Isnard M, Guichon C. Postdischarge surveillance of surgical site infections using telephone calls and a follow-up card in a resource-limited setting. J Hosp Infect 2017;96:16–19 [DOI] [PubMed] [Google Scholar]
- 23. Elbur AI, Ma Y, Elsayed ASA, Abdel-Rahman ME. Post-discharge surveillance of wound infections by telephone calls method in a Sudanese Teaching Hospital. J Infect Public Health 2013;6:339–346 [DOI] [PubMed] [Google Scholar]
- 24. Woldegioris T, Bantie G, Getachew H. Nurses' knowledge and practice regarding prevention of surgical site infection in Bahir Dar, Northwest Ethiopia. Surg Infect 2019;20:71–77 [DOI] [PubMed] [Google Scholar]
- 25. Mattingly AS, Starr N, Bitew S, et al. Qualitative outcomes of Clean Cut: Implementation lessons from reducing surgical infections in Ethiopia. BMC Health Serv Res 2019;19:579. [DOI] [PMC free article] [PubMed] [Google Scholar]