Abstract
Objective
This trial compared the efficacy and safety of transarterial chemoembolisation (TACE) plus sorafenib with TACE alone using a newly established TACE-specific endpoint and pre-treatment of sorafenib before initial TACE.
Design
Patients with unresectable hepatocellular carcinoma (HCC) were randomised to TACE plus sorafenib (n=80) or TACE alone (n=76). Patients in the combination group received sorafenib 400 mg once daily for 2–3 weeks before TACE, followed by 800 mg once daily during on-demand conventional TACE sessions until time to untreatable (unTACEable) progression (TTUP), defined as untreatable tumour progression, transient deterioration to Child-Pugh C or appearance of vascular invasion/extrahepatic spread. Co-primary endpoints were progression-free survival (PFS), which is not a conventional one but defined as TTUP, or time to any cause of death plus overall survival (OS). Multiplicity was adjusted by gatekeeping hierarchical testing.
Results
Median PFS was significantly longer in the TACE plus sorafenib than in the TACE alone group (25.2 vs 13.5 months; p=0.006). OS was not analysed because only 73.6% of OS events were reached. Median TTUP (26.7 vs 20.6 months; p=0.02) was also significantly longer in the TACE plus sorafenib group. OS at 1 year and 2 years in TACE plus sorafenib group and TACE alone group were 96.2% and 82.7% and 77.2% and 64.6%, respectively. There were no unexpected toxicities.
Conclusion
TACE plus sorafenib significantly improved PFS over TACE alone in patients with unresectable HCC. Adverse events were consistent with those of previous TACE combination trials.
Trial registration number
Keywords: transarterial chemoembolization, sorafenib, hepatocellular carcinoma, combination therapy with transarterial chemoembolisation and sorafenib, progression-free survival
Significance of this study.
What is already known about this subject?
Three trials conducted previously (Korea-Japan post-TACE trial, SPACE trial and TACE-2 trial) comparing PFS or TTP in TACE plus sorafenib with that in TACE alone could not show any clinical benefit by the addition of sorafenib to TACE.
It was demonstrated in the exploratory analysis of Korea-Japan post-TACE trial that longer treatment duration (31 weeks) of sorafenib in Korean patients is associated with significantly favourable TTP (HR=0.38, 95% CI, 0.18 to 0.81) as compared with TTP (HR=0.94, 95% CI, 0.75 to 1.19) in Japanese patients with shorter sorafenib treatment duration (16 weeks). Similarly, in SPACE trial, it was also shown that longer treatment duration with sorafenib in Asian patients (33.6 weeks) is associated with more favourable HR of TTP (HR=0.72, 95% CI, 0.457 to 1.135, p=0.078) than HR of TTP (HR=0.865, 95% CI, 0.576 to 1.300, p=0.243) in Non-Asian patients with shorter treatment duration (26.0 weeks). The design of these previous trials was based on RECIST1.1 or modified RECIST as a definition of the progression. Therefore, when tumour status becomes progression per RECIST1.1/mRECIST such as appearance of intrahepatic new lesions, protocol treatment had to be terminated at the time of progression, leading to a short treatment duration of sorafenib.
Significance of this study.
What is already known about this subject?
However, even when intrahepatic new lesion appears, repeated transarterial chemoembolisation (TACE) is still effective in intermediate stage hepatocellular carcinoma (HCC) in the routine clinical practice. In other words, progression per Response Evaluation Criteria in Solid Tumors (RECIST) 1.1/modified RECIST (mRECIST) does not always mean TACE treatment failure or does not suggest switching to next line of treatment in case of intermediate stage HCC different from advanced stage HCC, for which only systemic therapy is performed. Since intrahepatic metastasis/multicentric occurrence is a natural tumour biology in HCC, different endpoint to prolong the treatment duration may be necessary to demonstrate the clinical benefit of the addition of sorafenib. Authors felt that RECIST or mRECIST are not adequate for progression registration in the TACE realm and that we used a different progression endpoint, which was based on Response Evaluation Criteria in Cancer of the Liver (RECICL).
In addition, pre-treatment with molecular targeted agent before TACE had been proven in preclinical studies to normalise tumour vessels and suppress hypoxia (caused by TACE) inducible factor-1α, upregulating vascular endothelial growth factor, platelet-derived growth factor, or angiopoietin 2, which further enhance the HCC progression. Previous trials failed to show progression-free survival (PFS)/time to progression benefit due to the lack of pre-treatment of sorafenib as well as short treatment duration of sorafenib based on inadequate trial design for adjusting the TACE combination trial.
What are the new findings?
In this trial, RECIST1.1 or mRECIST was not used as a response evaluation criterion, but RECICL was used. PFS based on untreatable (unTACEble) progression plus death was defined as a trial endpoint based on a line of routine clinical practice in intermediate stage HCC. In this trial, intrahepatic new lesion was not regarded as a ‘progression’ and trial was continued until newly defined progression, resulting in very long treatment duration with sorafenib (38.7 weeks) as compared with previous trials (17–21 weeks).
Pre-treatment with sorafenib 2–3 weeks before initial TACE procedure was introduced in this trial, resulting in significantly longer interval between each TACE procedure in TACE plus sorafenib group than that in TACE alone group. In Sorfenib or Placebo in combination with TACE for intermediate stage hepatocellular carcinoma (SPACE) trial, pre-treatment with sorafenib before TACE was already introduced, but treatment duration before TACE was only 3–7 days, which is a bit different trial design as compared with current trial design.
This trial met its primary endpoint: PFS in TACE plus sorafenib group showed significantly longer (25.2 months) than that in TACE alone group (13.5 months) (HR, 0.59; 95% CI, 0.41 to 0.87). Furthermore, time to extrahepatic spread (EHS), time to vascular invasion and time to stage progression were significantly longer in TACE plus sorafenib group than those in TACE alone group.
This is the first ever positive trial of TACE in combination with a molecular targeted agent, sorafenib, in patients with unresectable HCC without vascular invasion or EHS. Thus, the combination of TACE plus sorafenib can improve clinical outcomes and may be a choice of treatment in patients with unresectable HCC.
How might it impact on clinical practice in the foreseeable future?
This trial clearly showed that TACE in combination with sorafenib should not be terminated at the point of intrahepatic tumour progression, when TACE is still deemed effective. The results in this trial also suggest that pre-treatment of sorafenib before TACE and continued use of sorafenib after TACE will prolong the PFS and prolong the interval between each TACE session, providing the prevention of liver function deterioration often caused by TACE repetition. Improvement of PFS and preservation of liver function will eventually lead to the prolongation of overall survival. However, further large-scaled validation randomised controlled trial is warranted to establish the real benefits of the combination use of targeted agents with TACE.
Introduction
Transarterial chemoembolisation (TACE) has shown survival benefits in patients with intermediate stage hepatocellular carcinoma (HCC).1 Most clinical practice guidelines, including those of the Barcelona Clinic Liver Cancer (BCLC),2 the European Association for the Study of the Liver,3 the American Association for the Study of Liver Diseases (AASLD),4 5 the Asian Pacific Association for the Study of the Liver6 and the Japan Society of Hepatology (JSH),7 have recommended the use of TACE for these patients, with TACE becoming the standard of care. Because of the high tumour recurrence rate after TACE, this procedure is usually repeated many times. However, the repetition of TACE may lead to deterioration of liver function, resulting in poor patient prognosis.8 Furthermore, TACE increases tumour hypoxia, leading to the upregulation of hypoxia inducible factor-1α (HIF-1α).9–11 Increased HIF-1α, in turn, upregulates the expression of vascular endothelial growth factor (VEGF) and platelet-derived growth factor (PDGF) and increases tumour angiogenesis.9–11That is, administration of TACE to patients with unresectable HCC has been shown to lead to a spike in the intratumoural concentration of VEGF, suggesting that blockade of VEGF receptors may prevent the effects of a surge in proangiogenic factors.11 12 A preclinical model has shown that the combination of antiangiogenic therapy with TACE reduces tumour volume and vessel density, as well as prolonging survival, when compared with TACE alone.12
Sorafenib is an oral multikinase inhibitor targeting, among others, VEGF receptor, RAF and PDGF receptor, thereby exerting both antiangiogenic and direct antitumour effects. This activity profile suggests that sorafenib may suppress the surge of proangiogenic factors after TACE. Sorafenib has been shown to significantly prolong overall survival (OS) in patients with advanced HCC, resulting in a significant advance in the treatment of this disease.13 14 Sorafenib has since been approved worldwide and has become the standard treatment for patients with advanced unresectable HCC. Because TACE and sorafenib have each been shown to prolong survival in patients with unresectable HCC,13–17 their combination may improve clinical outcomes.18–21 To date, however, all five randomised controlled trials testing combinations of TACE with molecular targeted agents such as sorafenib, brivanib and orantinib have failed to show clinical benefits of these combinations.22–27
Trials assessing the combination of TACE plus sorafenib in patients with unresectable HCC have yielded inconsistent results. Several single-arm trials have shown that this combination is safe, effective and feasible in patients with unresectable HCC.19–21 In contrast, three previous randomised controlled trials failed to show the benefits of this combination of TACE plus sorafenib.22–24 Subgroup analyses of two of these trials, however, the Japan-Korea Post-TACE trial and the SPACE trial, suggested that longer duration of treatment with sorafenib in combination with TACE may improve clinical outcomes.22 23 Based on the three negative clinical trials, the parameter TACE-specific progression was defined as a study outcome in the current trial. The present study reports the results of the TACE Therapy In Combination with Sorafenib as compared with TACE alone in patients with hepatocellular carcinoma (TACTICS) trial, comparing the safety and efficacy of the combination of TACE plus sorafenib with TACE alone in patients with unresectable HCC who were not candidates for resection or ablation.
Patients and methods
Patients
This randomised, open label, multicentre trial was conducted at 33 institutions in Japan and included patients who had been diagnosed with unresectable HCC by biopsy, cytology or diagnostic imaging, such as dynamic CT or MRI, according to the criteria of the AASLD. Patients were included if they were aged≥20 years, had a life expectancy≥12 weeks and had tumours confined to the liver without vascular invasion/extrahepatic spread (EHS) and treatable by TACE. Maximum tumour diameter was 10 cm, and maximum number of nodules was 10. The maximum number of TACE procedures allowed before enrolment was 2, with at least 6 months since prior TACE. All of those patients who had a history of prior TACE achieved complete response by previous TACE, but recurred more than 6 months later at the study entry. All patients had an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1, Child-Pugh scores≤7 points and adequate organ function. Prior resection or ablation was allowed; however, any prior systemic therapy was not allowed.
Patients were excluded if they had another previous or current malignant tumour, except for early-stage cancer with low risk of recurrence or a malignant tumour curatively treated>3 years prior to enrolment with no recurrence. Patients were also excluded if they had cardiac disease or a serious and active infection, except for hepatitis B virus (HBV) and hepatitis C virus (HCV). Patients with diffuse tumour lesions, extrahepatic metastases, vascular invasion, hepatic encephalopathy, uncontrolled ascites or pleural effusion were also excluded, as were patients previously treated for advanced HCC, including systemic chemotherapy, and those treated with CYP3A4-inducing agents. Patients with uncontrollable ascites or decompensated liver function were also excluded.
All patients provided written informed consent prior to enrolment.
Randomisation and masking
Patients were randomised 1:1 to treatment with TACE plus sorafenib or TACE alone. Randomisation was performed centrally via an interactive Web response system involving a computer-generated sequence and Electric Data Capture System Software (Viedeoc, Uppsala, Sweden). Patients were stratified by study centre, by their meeting or not meeting Milan criteria (one nodule≤5 cm in diameter or ≤3 nodules ≤3 cm in diameter) and by number of prior TACE sessions (0 vs 1–2).
Treatment protocol
Patients randomised to TACE plus sorafenib were started on 400 mg/day sorafenib 2–3 weeks prior to first TACE to confirm tolerability to sorafenib, to normalise tumour neovasculature for efficient TACE response and to suppress the VEGF increase after the TACE procedure. Sorafenib was discontinued for 2 days before and 2 days after each TACE session.
TACE in both groups consisted of intra-arterial injection of lipiodol plus epirubicin or miriplatin,28followed by injection of an embolic agent (Gelpart) to interrupt blood flow. Selection of anticancer agent (epirubicin or miriplatin) was decided by the sites/investigators; however, the same agent must be used at the repeated TACE sessions. Therefore, sites were included in the one of the stratification factors to avoid any imbalance. When necessary in treating very large tumours, split TACE was allowed within 4–6 weeks of the first TACE session. First image was taken 4 weeks after split TACE was performed. Repeat TACE with the same anticancer agent was recommended when the two-dimensional measurement of the viable lesion was >50% that of the baseline tumour. TACE was repeated for intrahepatic new lesions measuring >10 mm, which show arterial enhancement with venous washout. If venous washout is not associated with arterial enhancement even in lesions >10 mm, TACE was waited until the time venous washout is confirmed.
Patients in the TACE plus sorafenib group resumed taking 400 mg/day sorafenib 3 days after TACE. If this dose was tolerated, dose increases were allowed to 800 mg/day in a stepwise manner at the discretion of the investigator. At the same dose before re-TACE sorafenib was started after the on-demand TACE. The dose of sorafenib in patients who experienced adverse events (AEs) due to this agent was reduced to 400 mg/day or 400 mg every other day, with patients requiring further dose reduction undergoing dose interruption or discontinued from sorafenib treatment.
Beginning 4 weeks after TACE, tumours were assessed by dynamic CT or MRI every 8 weeks, with tumour marker tests performed at the same times. Treatment was continued until untreatable (unTACEable) progression, progression to meet the TACE refractoriness criteria, unacceptable toxicity or withdrawal of consent.
Study endpoints
The co-primary endpoint of this trial consisted of progression-free survival (PFS)/OS, an endpoint determined using a gatekeeping strategy for multiplicity adjustments, such that OS was calculated only if PFS was statistically significant.29 PFS was defined as the time from randomisation to progression or death from any cause, and OS was defined as the time from randomisation to death from any cause.
Progression in this trial was determined as untreatable (UnTACEable) progression, defined as the inability of a patient to further receive or benefit from TACE for reasons that included intrahepatic tumour progression (25% increase vs baseline) according to Response Evaluation Criteria in Cancer of the Liver (RECICL),30 transient deterioration of liver function to Child-Pugh C right after TACE, macrovascular invasion (MVI) or EHS. When ascites is not controllable or liver function is decompensated, TACE was not performed in both arms since TACE is contraindicated in such cases. In this trial, new intrahepatic lesions were NOT regarded as ‘progressive disease’, as they are indicative of the natural tumour biology of HCC and do not imply treatment failure or moving to the next line of treatment. Therefore, neither Response Evaluation Criteria in Solid Tumors (RECIST) 1.1 nor modified RECIST criteria were used in this trial. Rather, tumour response was evaluated using RECICL.30 Lipiodol retention area in the nodule after 1 month following TACE was regarded as necrosis.31 Therefore, complete tumour response to TACE was defined as complete lipiodol retention within the nodule and partial tumour response was defined as 50%–100% lipiodol retention within the nodule throughout the trial. Progression in this trial also included progression that met the JSH criteria for TACE failure/refractoriness,32 defined as two or more consecutive insufficient responses of the treated tumour (viable lesion>50%) or two or more consecutive unnumbered increases in liver tumour number, even after changing the chemotherapeutic agents and/or reanalysis of the feeding artery, as determined by CT/MRI 8 weeks after adequate performance of selective TACE.
Secondary endpoints of this trial included time to untreatable (unTACEable) progression (TTUP), defined as the time from randomisation to Child-Pugh grade C, intrahepatic tumour progression (>25% increase vs baseline), with new lesions NOT defined as tumour progression, MVI or EHS (diameter>10 mm); and time to progression (TTP), defined as the time from randomisation to unTACEable progression or progression to TACE failure/refractoriness. Other secondary endpoints included objective response rate (ORR) after the first session of TACE; serum concentrations of the tumour markers AFP, AFP-L3 and PIVKA-II; and safety.
Statistical methods
All statistical analyses were performed using the data obtained by the cut-off date of 2 November 2017, at which time point 118 patients had experienced disease progression. Efficacy data were analysed on an intention-to-treat basis. To adjust for multiple comparisons, hierarchical statistical testing was performed in a pre-specified fixed-order, first for PFS and then for OS. OS was formally compared only when the difference in PFS was significant (p<0.15). The primary endpoints were compared using stratified log-rank tests. The Kaplan-Meier method was used to estimate survival curves, from which medians were calculated. HRs and CIs were estimated using Cox proportional hazards models. Safety analysis included all patients who received at least one dose of the assigned treatment, irrespective of eligibility or duration of treatment. All statistical analyses were performed using SAS (SAS Institute, Cary, NC, USA), V.9.4.
We originally designed this trial such that a total of 125 TTUP events would give the trial an 80% power to detect an HR of 0.71 with a one-sided alpha of 0.15. The required number of events was anticipated to be reached by monitoring 168 patients. In November 2015, with the investigators and statisticians still blinded to all patient data, the protocol was amended due to slow recruitment. The primary endpoint was amended to the co-primary endpoints, PFS and OS, because extension of the recruitment period made it possible to observe sufficient numbers of PFS and OS events, not only TTUP events that do not require long-term follow-up. As such, a total of 125 PFS and OS events were required to maintain an 80% power to detect a HR of 0.71 with a one-sided alpha of 0.15.
Results
Patient characteristics
A total of 197 patients were screened from February 2011 to March 2016; of these, 156 met the inclusion criteria and were enrolled and randomised. In contrast, 41 patients did not meet the inclusion criteria, for reasons that included Child-Pugh score, prior TACE number and laboratory test results (figure 1). Of the 156 enrolled patients, 60 (38%) were categorised as BCLC stage A, with most having a single large (>5 cm) unresectable tumour and regarded as good candidates for TACE. Similarly, 18 patients (12%) were categorised as BCLC stage C because they had performance status 1, but without EHS or vascular invasion. The remaining 78 patients (50%) were categorised as BCLC stage B.
Figure 1.
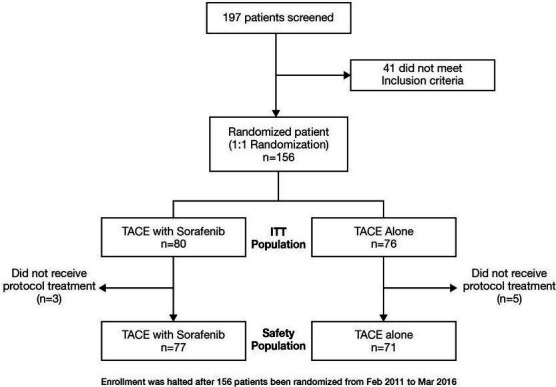
Patientflow chart (consort diagram). TACE, transarterial chemoembolisation.
In all, 80 patients were randomised to the TACE plus sorafenib group and 76 to the TACE alone group; of these, three and five patients, respectively, were withdrawn prior to protocol treatment. The three patients in the TACE plus sorafenib and two of the five patients in the TACE alone group did not receive protocol treatment (TACE) because of worsening liver function; the other three patients in the TACE alone group were withdrawn because they were found not to meet eligibility criteria after randomisation. The baseline demographic and clinical characteristics were similar in the TACE plus sorafenib and TACE alone groups (table 1).
Table 1.
Baseline demographic and clinical characteristics of patients enrolled in this study results reported as N (%), unless otherwise indicated
| Characteristic | TACE plus sorafenib (n=80) | TACE alone (n=76) |
| Age, median (range), years | 72.0 (36–85) | 73.0 (53–86) |
| Sex | ||
| Male | 63 (78.8) | 55 (72.4) |
| Female | 17 (21.2) | 21 (27.6) |
| Performance status | ||
| 0 | 71 (88.8) | 67 (88.2) |
| 1 | 9 (11.3) | 9 (11.8) |
| Aetiology | ||
| Hepatitis B | 10 (12.5) | 2 (2.6) |
| Hepatitis C | 38 (47.5) | 53 (69.7) |
| Non-B Non-C | 32 (40.0) | 21 (27.6) |
| Child-Pugh score | ||
| 5 | 64 (80.0) | 54 (71.1) |
| 6 | 15 (18.8) | 17 (22.4) |
| 7 | 1 (1.3) | 5 (5.6) |
| Ascites | 0 (0) | 0 (0) |
| Treatment with diuretics | 10 (12.5) | 9 (11.8) |
| AFP | ||
| <200 ng/mL | 64 (80.0) | 60 (78.9) |
| ≥200 ng/mL | 16 (20.0) | 16 (21.1) |
| Tumour burden | ||
| Within Milan criteria | 28 (35.0) | 35 (46.1) |
| Outside Milan criteria | 52 (65.0) | 41 (53.9) |
| Up to T7 criteria | ||
| Within | 54 (67.5) | 50 (65.8) |
| Outside | 26 (32.5) | 26 (34.2) |
| BCLC stage | ||
| A | 27 (33.8) | 33 (43.4) |
| B | 44 (55.0) | 34 (44.7) |
| C | 9 (11.3) | 9 (11.8) |
| Prior TACE | ||
| 0 | 45 (56.3) | 48 (63.2) |
| 1–2 | 35 (43.8) | 28 (36.8) |
BCLC, Barcelona Clinic Liver Cancer; TACE, transarterial chemoembolisation.
Doses of study drugs
At a median follow-up of 122.3 weeks, the median duration of sorafenib treatment in the TACE plus sorafenib group was 38.7 weeks (range, 0.3–245.9 weeks), and the mean±SD duration of sorafenib treatment was 57.1±53.3 weeks. Only in 42 of 80 patients in combination group, sorafenib dose was increased up to 800 mg after initial TACE procedure; however, sorafenib dose was eventually reduced during the protocol treatment in all of these 42 patients and also other patients who do not increase the sorafenib dose up to 800 mg due to AEs, patients’ requests or physician’s decision. The median actual daily dose of sorafenib was 355.2 mg (range, 86.8–792.9 mg), and the mean±SD actual daily dose of sorafenib was 353.6±172.0 mg. The median interval between TACE sessions was 21.1 weeks (range, 15.8–39.0 weeks) in the TACE plus sorafenib group and 16.9 weeks (range, 10.1–32.1 weeks) in the TACE alone group (p=0.018).
Efficacy outcomes
The first co-primary endpoint, median PFS, specifically defined for TACE-specific PFS based on unTACEable progression was significantly longer in the TACE plus sorafenib than in the TACE only group (25.2 vs 13.5 months; HR=0.59; 95% CI, 0.41 to 0.87; p=0.006; figure 2A). In TACE naïve group, there was no statistical difference between median PFS based on unTACEable progression in the combination group and that in TACE alone group (HR=0.741; 95% CI, 0.45, 1.22; p=0.23) (online supplementary figure 1A). However, in prior TACE 1–2 group, median PFS based on unTACEable progression in the combination group was significantly longer than that in TACE alone group (HR=0.570; 95% CI, 0.33 to 0.99; p=0.04) (online supplementary figure 1B). The second co-primary endpoint, median OS, was not analysed because only 92 of 125 (73.6%) of OS events were mature on the study cut-off date of 2 November 2017. Independent review committee declared that OS was not mature at the PFS manuscript submission on 15 September 2019; therefore, final analysis could not have been performed yet. However, survival rates in TACE plus sorafenib group and TACE alone group were 96.2% and 82.7% at 1 year and 77.2% and 64.6% at 2 years at the last data cut-off (2 November 2017), respectively, although statistical analysis was not allowed based on the protocol regulation.
Figure 2.
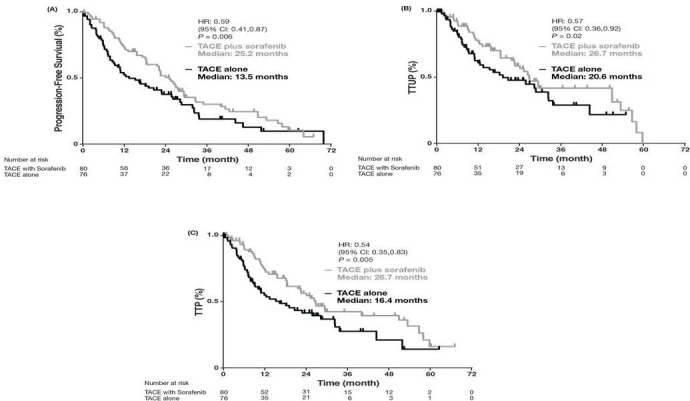
Kaplan-Meier plots of median (A) progression-free survival, (B) TTUP and (C) TTP in the TACE plus sorafenib and TACE alone groups. TACE, transarterial chemoembolisation; TTP, time to progression; TTUP, time to untreatable (unTACEable) progression.
gutjnl-2019-318934supp001.pdf (27.8KB, pdf)
Analysis of secondary efficacy outcomes showed that median TTUP (26.7 vs 20.6 months; HR=0.57; 95% CI, 0.36 to 0.92; p=0.02; figure 2B) and median TTP (26.7 vs 16.4 months; HR=0.54; 95% CI, 0.35 to 0.83; p=0.005; figure 2C) were also significantly longer in the TACE plus sorafenib than in the TACE alone group. Exploratory subgroup analyses showed that PFS based on unTACEable progression was longer in all subgroups treated with TACE plus sorafenib than with TACE alone (figure 3). In contrast, tumour responses, disease control rate (DCR) and ORR 4 weeks after the first TACE session were similar in the two groups (table 2).
Figure 3.
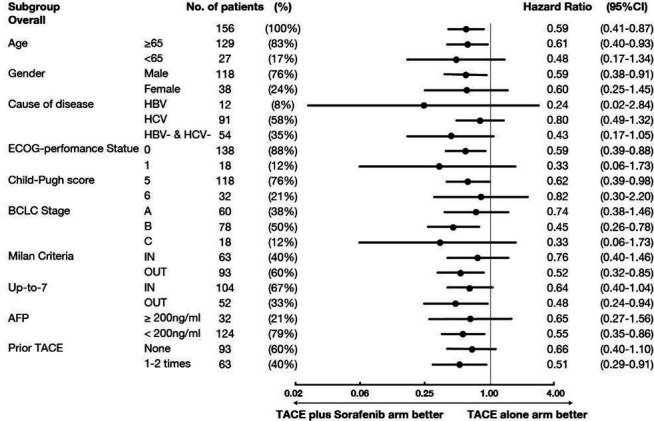
Forest plot of PFS in subgroups of patients treated with TACE plus sorafenib and TACE alone. PFS, progression-free survival; TACE, transarterial chemoembolisation.
Table 2.
Tumour responses 4 weeks after first TACE in patients randomised to the TACE plus sorafenib and TACE alone groups results reported as N (%)
| TACE plus sorafenib (n=80) | TACE alone (n=76) | P value* | |
| Best response | 0.77 | ||
| Complete response (CR) | 23 (28.8) | 21 (27.6) | |
| Partial response (PR) | 34 (42·.5) | 26 (34.2) | |
| Stable disease (SD) | 10 (12.5) | 12 (15.8) | |
| Progressive disease (PD) | 2 (2.5) | 3 (3.9) | |
| Not evaluable | 11 (13.8) | 14 (18.4) | |
| ORR (CR+PR) | 57 (71.3) | 47 (61.8) | 0.23 |
| DCR (CR+PR+SD) | 67 (83.8) | 59 (77.6) | 0.42 |
*By two-sided Fisher’s exact tests.
DCR, disease control rate; ORR, objective response rate; TACE, transarterial chemoembolisation.
Pattern of unTACEable progression
The patterns and frequency of progression did not differ significantly in the TACE plus sorafenib and TACE alone groups (online supplementary table 1). However, in the analysis considering the timing of event occurrence, time to MVI (31.3 months vs 4.0 months; HR=0.26, 95% CI, 0.09 to 0.75, p=0.008) and time to EHS (15.7 months vs 6.9 months; HR=0.21, 95% CI, 0.006 to 0.70, p=0.006) were significantly longer in the TACE plus sorafenib than in the TACE alone group (online supplementary figure 2). Time to stage progression, which was defined as appearance of MVI and/or EHS was also significantly longer in the TACE plus sorafenib (22.5 months) than in the TACE alone (6.3 months) group (HR=0.31, 95% CI, 0.15 to 0.63, p=0.001) (online supplementary figure 3). Discontinuation of protocol treatment due to transient liver function deterioration to Child-Pugh C right after TACE was seen only in four cases; two in combination group and two in TACE alone group. Liver function in those four patients returned to Child-Pugh B seven or eight later, but dropped out from the trial due to protocol specification.
gutjnl-2019-318934supp002.pdf (50.4KB, pdf)
gutjnl-2019-318934supp003.pdf (122.2KB, pdf)
gutjnl-2019-318934supp004.pdf (94KB, pdf)
Safety outcomes
Table 3 shows the treatment emergent AEs with frequency≥10% in either group and their corresponding Grades 3 and 4 AEs within 4 weeks after first TACE. All grade AEs more frequent in the TACE plus sorafenib group than in the TACE alone group included hand-foot skin reaction (HFSR) (53.2% vs 0%), hypertension (51.9% vs 39.4%), increased lipase (49.4% vs 25.4%), fatigue (24.7% vs 9.9%), diarrhoea (14.3% vs 0%), erythemia multiforme (11.7% vs 0%), weight loss (11.7% vs 2.8%) and hoarseness (11.7% vs 0%). Grade 3 AEs more frequent in the TACE plus sorafenib group than in the TACE alone group included thrombocytopaenia (13.0% vs 2.8%), HFSR (5.2% vs 0%), hypertension (10.4% vs 4.2%), increased lipase (14.3% vs 2.8%), increased amylase (7.8% vs 1.4%), neutropaenia (5.2% vs 0%), fatigue (2.6% vs 0%), diarrhoea (2.6% vs 0%) and erythema multiforme (2.6% vs 0%). AEs more frequent in the TACE plus sorafenib group were likely due to the effects of sorafenib.
Table 3.
All-grade treatment-emergent AEs within 4 weeks after first TACE with frequency≥10% in either group and corresponding Grades 3 and 4 AEs
| n (%) | TACE plus sorafenib (n=77) | TACE alone (n=71) | ||||||
| All grade | Grades 1–2 | Grade 3 | Grade 4 | All grade | Grades 1–2 | Grade 3 | Grade 4 | |
| Elevated AST | 72 (93.5) | 50 (64.9) | 17 (22.1) | 5 (6.5) | 65 (91.5) | 50 (70.4) | 14 (19.7) | 1 (1.4) |
| Elevated ALT | 69 (89.6) | 50 (64.9) | 18 (23.4) | 1 (1.3) | 55 (77.5) | 42 (59.2) | 13 (18.3) | 0 (0.0) |
| Thrombocytopaenia | 67 (87.0) | 57 (74.0) | 10 (13.0) | 0 (0.0) | 53 (74.6) | 51 (71.8) | 2 (2.8) | 0 (0.0) |
| Elevated bilirubin | 55 (71.4) | 54 (70.1) | 1 (1.3) | 0 (0.0) | 39 (54.9) | 37 (52.1) | 2 (2.8) | 0 (0.0) |
| Anaemia | 50 (64.9) | 49 (63.6) | 1 (1.3) | 0 (0.0) | 35 (49.3) | 34 (47.9) | 1 (1.4) | 0 (0.0) |
| Hand-foot skin reaction | 41 (53.2) | 37 (48.1) | 4 (5.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Hypertension | 40 (51.9) | 32 (41.6) | 8 (10.4) | 0 (0.0) | 28 (39.4) | 25 (35.2) | 3 (4.2) | 0 (0.0) |
| Elevated lipase | 38 (49.4) | 26 (33.8) | 11 (14.3) | 1 (1.3) | 18 (25.4) | 16 (22.5) | 2 (2.8) | 0 (0.0) |
| Elevated serum amylase | 32 (41.6) | 26 (33.8) | 6 (7.8) | 0 (0.0) | 19 (26.8) | 18 (25.4) | 1 (1.4) | 0 (0.0) |
| Neutropaenia | 29 (37.7) | 25 (32.5) | 4 (5.2) | 0 (0.0) | 29 (40.8) | 29 (40.8) | 0 (0.0) | 0 (0.0) |
| Decreased WBC count | 29 (37.7) | 28 (36.4) | 1 (1.3) | 0 (0.0) | 26 (36.6) | 26 (36.6) | 0 (0.0) | 0 (0.0) |
| Malaise | 20 (26.0) | 20 (26.0) | 0 (0.0) | 0 (0.0) | 9 (12.7) | 9 (12.7) | 0 (0.0) | 0 (0.0) |
| Fatigue | 19 (24.7) | 17 (22.1) | 2 (2.6) | 0 (0.0) | 7 (9.9) | 7 (9.9) | 0 (0.0) | 0 (0.0) |
| Fever | 15 (19.5) | 14 (18.2) | 1 (1.3) | 0 (0.0) | 18 (25.4) | 18 (25.4) | 0 (0.0) | 0 (0.0) |
| Anorexia | 11 (14.3) | 9 (11.7) | 2 (2.6) | 0 (0.0) | 8 (11.3) | 7 (9.9) | 1 (1.4) | 0 (0.0) |
| Diarrhoea | 11 (14.3) | 9 (11.7) | 2 (2.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Erythema multiforme | 9 (11.7) | 7 (9.1) | 2 (2.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Weight loss | 9 (11.7) | 9 (11.7) | 0 (0.0) | 0 (0.0) | 2 (2.8) | 2 (2.8) | 0 (0.0) | 0 (0.0) |
| Hoarseness | 9 (11.7) | 9 (11.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
AEs, adverse events; ALT, alanine aminotransaminase; AST, aspartate aminotransferase; TACE, transarterial chemoembolisation; WBC, white blood cell.
Discussion
The TACTICS trial was a randomised, open label, multicentre trial comparing the safety and efficacy of the combination of TACE plus sorafenib with TACE alone in patients with unresectable HCC who were not candidates for resection or ablation. This study, which assessed one of the co-primary endpoints, median PFS based on unTACEable progression, found that the combination of TACE plus sorafenib resulted in significantly longer PFS based on unTACEable progression than TACE alone (25.2 vs 13.5 months; HR=0.59; 95% CI, 0.41 to 0.87; p=0.006). Moreover, times to vascular invasion, EHS and stage progression were much longer in the TACE plus sorafenib than in the TACE alone group, indicating that the combination of TACE plus sorafenib markedly prevented the progression of intermediate to advanced stage HCC. In addition, the interval between pairs of TACE sessions was significantly longer in the TACE plus sorafenib than in the TACE alone group, suggesting that TACE-associated deterioration of liver function is lower in the TACE plus sorafenib than in the TACE alone group. ORR was relatively high in both the TACE plus sorafenib (71.3%) and TACE alone (61.8%) groups, probably because of the high response to TACE performed in a superselective manner. Because OS events are not yet mature in this trial, the second co-primary endpoint, median OS, could not be analysed.
The combination of TACE plus sorafenib was clinically feasible and safe. Many AEs were more frequent in the TACE plus sorafenib than in the TACE alone group, with these AEs likely to result from treatment with sorafenib. None of the AEs in either group was unexpected, and rates of Grades 3 and 4 AEs were relatively low.
These findings differ markedly from those of previous trials testing the combination of TACE plus sorafenib in patients with HCC. For example, the Japan-Korea post-TACE and SPACE trials reported median TTPs of 5.4 and 5.6 months, respectively, with the criteria for disease progression determined using RECICL 2004 and mRECIST criteria, respectively.22 23 The TACE 2 trial reported a median PFS of 8.5 months, with the criteria for disease progression determined using RECIST 1.1 criteria.24 RECIST and mRECIST criteria may not be good measures of capturing the ‘progression’ of intermediate stage HCC, as regrowth of the original tumour or appearance of a new intrahepatic lesion is not indicative of treatment (TACE) failure and does not suggest the need to move to a next line of treatment.
In contrast, the TACTICS trial reported a median PFS of 25.2 months, with the criteria for progression being unTACEable progression/TACE failure. New intrahepatic lesions in the TACTICS trial were not regarded as progressive disease. The better outcomes observed in the TACTICS trial may be due to the much longer median duration of sorafenib treatment (38.7 weeks), owing to the TACE-specific trial design. In contrast, the median durations of sorafenib treatment in the post-TACE, SPACE, and TACE 2 trials ranged from 17.0 to 21.0 weeks.22–24 Another possible explanation would be sorafenib was given 2–3 weeks before initial TACE was performed. This pre-treatment with sorafenib might have led to the normalisation of tumour vessel, resulting in enhancement of TACE efficacy by dense accumulation of lipiodol mixed with anticancer agent and gelatine sponges. In fact, interval between each TACE session was significantly prolonged in TACE plus sorafenib group than TACE alone group. The third explanation would be sorafenib might have stabilised disease progression after each TACE session, leading to a prolonged PFS.
This study, however, had several limitations, including the relatively small number of patients included. Moreover TACE-specific PFS, PFS based on unTACEable progression, which was applied in this trial based on lessons learnt from previous negative trials, had rarely been used in previous trials, except that ‘unTACEable progression’ was used in the SPACE trial. Actually, this concept that progression after TACE may not mean treatment failure and that treatment could be maintained until untreatable progression was first proposed by Bruix et al 33 and therefore tested in SPACE trial. Thus, we believe that this new TACE-specific endpoint should be tested and validated in future TACE combination trials as well.
In summary, this is the first ever positive trial of TACE in combination with a molecular targeted agent, sorafenib, in patients with unresectable HCC, providing important results in the practice. In contrast to the three negative trials, the present trial assessed the efficacy of TACE plus sorafenib using an endpoint more suitable for a TACE combination trial, with this endpoint being consistent with those used in clinical practice. Furthermore, pre-treatment with sorafenib 2–3 weeks before initial TACE was introduced in this trial similar to, but longer period than SPACE trial. Pre-treatment with sorafenib before TACE will enhance the treatment effect of TACE through tumour vessel normalisation leading to homogeneous distribution of lipiodol mixed with anticancer drugs and gelatine sponge particle within the tumours. Furthermore, pre-treatment with sorafenib before initial TACE will suppress the HIF-1α induced VEGF or PDGFR, which is regarded as the factor responsible for further tumour progression. The results of the TACTICS trial indicate that new intrahepatic lesions may not be regarded as progressive disease or as a reason for halting treatment in TACE combination trials. Thus, we strongly believe that the definition of treatment success or failure by TACE should use a different criteria from RECIST or mRECIST.
In TACTICS trial, among unTACEable progression transient liver function deterioration to Child-Pugh C was observed only in 4 of 99 patients, which means many patients were discontinued TACE after TACE refractoriness. This event was included in the category of intrahepatic tumour growth>25% or TACE refractoriness in online supplementary table 2. The reason why for this is that the study protocol clearly specified TACE should not be continued once tumour status become refractory to TACE.
In conclusion, this trial clearly showed that the combination of TACE plus sorafenib can improve clinical outcomes and may be a choice of treatment in patients with unresectable HCC without vascular invasion or EHS, who are good candidates for TACE.
Acknowledgments
We thank the patients, their families, the investigators, the site staff and the teams who participated in this study. This study was supported by Japan Liver Oncology Group with funding from Bayer Yakuhin, Ltd., Japan, under a research contract.
Footnotes
MK and KU contributed equally.
Collaborators: The following members are the TACTICS trial group: Masatosi Kudo, Kazuomi Ueshima, Takuji Torimura, Masafumi Ikeda, Nobukazu Tanabe, Hiroshi Aikata, Namiki Izumi, Takahiro Yamasaki, Shunsuke Nojiri, Keisuke Hino, Hidetaka Tsumura, Teiji Kuzuya, Norio Isoda, Kohichiroh Yasui, Hajime Aino, Akio Ido, Naoto Kawabe, Kazuhiko Nakao, Yohiyuki Wada, Osamu Yokosuka, Kenichi Yoshimura, Takashi Okusaka, Junji Furuse, Norihiro Kokudo, Kiwamu Okita, Philip James Johnson, Yasuaki Arai, Masao Fujimoto, Masahiko Koda, Eiichi Tomita, Yukio Osaki, Hisashi Hidaka, Hiroshi Ogawa, Takayuki Kogure, Atsuhiro Nakatsuka, Nobuyuki Enomoto, Katsuaki Tanaka, Masataka Seike, Toru ishikawa, Tetsuro Inokuma, Manabu Morimoto.
Contributors: Masatoshi Kudo and Kazuomi Ueshima contributed to the study design, data collection, study analysis, manuscript writing, critical review of the manuscript and final approval of the manuscript submission. Masafumi Ikeda, Takuji Torimura, Nobukazu Tanabe, Hiroshi Aikata, Namiki Izumi, Takahiro Yamasaki, Shunsuke Nojiri, Keisuke Hino, Hidetaka Tsumura, Teiji Kuzuya, Norio Isoda, Kohichiroh Yasui, Hajime Aino, Akio Ido, Naoto Kawabe, Kazuhiko Nakao, Yoshiyuki Wada, Osamu Yokosuka, Takuji Okusaka, Junji Furuse, Norihiro Kokudo, Kiwamu Okita and Yasuaki Arai contributed to data collection, critical review of the manuscript and final approval of the manuscript submission. Philip Johnson contributed to interpretation of the data, critical review of the manuscript and final approval of the manuscript submission. Ken-ichi Yoshimura did the statistical analysis, critical review of the manuscript and final approval of the manuscript.
Funding: This study was supported by the Japan Liver Oncology Group with funding from Bayer Yakuhin, Ltd., Japan, under a research contract.
Competing interests: KM: Honoraria from Bayer, Eisai, MSD, Ajinomoto. Consulting or advisory role for Kowa, MSD, BMS, Bayer, Chugai, Taiho. Research funding from Chugai, Otuka, Takeda, Taiho, Sumitomo Dainippon, Daiichi Sankyo, MSD, Eisai, Bayer, Abbvie. IM: Honoraria from Novartis Pharma, Bayer Yakuhin, Bristol-Myers Squibb, Abbott Japan, Eisai, Taiho Pharmaceutical, Eli Lilly Japan, Daiichi-Sankyo, Yakult, Otsuka Pharmaceutical, Nobelpharma, EA Pharma, Teijin Pharma. Consulting or advisory role for Nano Carrier, Bayer Yakuhin, Eisai, Kyowa Hakko Kirin, Novartis Pharma, Shire, MSD, Bristol Myers Sqiibb, Eli Lilly Japan, Sumitomo Dainippon, Daiichi-Sankyo, Teijin Pharma, Takara Bio. Research funding from Bayer Yakuhin, Kyowa Hakko Kirin, Yakult, Taiho Pharmaceutical, Eli Lilly Japan, Ono Pharmaceutical, Eisai, AstraZeneca, Zeria Pharmaceutical, Chugai, Bristol Myers Sqiibb, Merck Serono, Kowa, Nano Carrier, ASLAN, Daiichi-Sankyo., Sumitomo Dainippon, Novartis Pharma, Baxalta, Boehringer Ingelheim, Takara Bio. Board membership: ASLAN, Chugai. IN: Honoraria from Bayer, Gilead, Abbvie, Otuka. IN: Research funding from Abbvie GK. HK: Honoraria from MSD, Abbvie, Bristrol-Myers Squibb, Dainippon Sumitomo and Otsuka, Research funding from Gilead, Bristrol-Myers Squibb, MSD. IA: Honoraria from AbbVie GK, Bristol Myers Squibb, Gilead, Eisai. Research funding from AbbVie GK, Otsuka, MSD, Chugai, Eisai, Astellas, Takeda. KN: Research funding from Abbvie GK.Nakao K: Honoraria from Gilead. YO: Research funding from AstraZeneca, Asteras, Ajinomoto, AsahiKasei-Kurare Medical, Bayer Yakuhin, Bristol Myers Sqiibb, Chugai, Daiichi-Sankyo, Eisai, Kyowa Hakko Kirin, Kowa, Nihon Kayaku, MSD, Otsuka, Ono, Taiho, Tanabe-Mitsubishi, Takeda, Torii, Tsumura, Zeria. YK: Honoraria from Chugai, Eli Lilly, Taiho, Nippon Shinyaku. OT: Honoraria from Novartis, Taiho, Eli Lilly, Dainippon Sumitomo, Bayer, Yakult, FUJIFILM, AstraZeneca, Ono Pharmaceutical, EA Pharma, Nippon Chemiphar, Celgene, Chugai, Bristol Myers, Eisai, Pfizer, Teijin, Daiichi Sankyo, MSD, Shire, AbbVie, Takeda. Consulting or advisory role for Eli Lilly, Dainippon Sumitomo, Taiho, Zeria Pharmaceutical, Daiichi Sankyo, Bristol Myers. Research Funding from Eli Lilly, Eisai, Novartis, Yakult Honsha, Taiho, Kowa, Kyowa Hakko Kirin, Merck Serono, Ono Pharmaceutical, Bayer, Pfizer Japan, AstraZeneca, Dainippon Sumitomo, Chugai, Bristol Myers, Zeria Pharmaceutical. KN: Honoraria from Eisai. AY: Royalties from Sumitomo Bakelite. Research funding from Canon Medical Systems, Taiho Pharmaceutical, Eisai. Honoraria from Merit Medical Systems., Fuji Pharma, Terumo International Systems, Nippon Kayaku, Canon Medical Systems, Bristol Meyer Squibb, Sumitomo Bakelite, Bayer Pharmaceuticals, Boston Scientific Japan, Taiho Pharmaceutical, Guerbet Japan, Guerbet Asia Pacific.
Patient consent for publication: Not required.
Ethics approval: The study conformed to the Declaration of Helsinki. The protocol was approved by the ethics committee of each participating institution.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
Contributor Information
on behalf of the TACTICS study group:
Masatosi Kudo, Kazuomi Ueshima, Takuji Torimura, Masafumi Ikeda, Nobukazu Tanabe, Hiroshi Aikata, Namiki Izumi, Takahiro Yamasaki, Shunsuke Nojiri, Keisuke Hino, Hidetaka Tsumura, Teiji Kuzuya, Norio Isoda, Kohichiroh Yasui, Hajime Aino, Akio Ido, Naoto Kawabe, Kazuhiko Nakao, Yohiyuki Wada, Osamu Yokosuka, Kenichi Yoshimura, Takashi Okusaka, Junji Furuse, Norihiro Kokudo, Kiwamu Okita, Philip James Johnson, Yasuaki Arai, Masao Fujimoto, Masahiko Koda, Eiichi Tomita, Yukio Osaki, Hisashi Hidaka, Hiroshi Ogawa, Takayuki Kogure, Atsuhiro Nakatsuka, Nobuyuki Enomoto, Katsuaki Tanaka, Masataka Seike, Toru Ishikawa, Tetsuro Inokuma, and Manabu Morimoto
References
- 1. Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology 2003;37:429–42. 10.1053/jhep.2003.50047 [DOI] [PubMed] [Google Scholar]
- 2. Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet 2018;391:1301–14. 10.1016/S0140-6736(18)30010-2 [DOI] [PubMed] [Google Scholar]
- 3. European association for the study of the liver. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2018;69:182–236. [DOI] [PubMed] [Google Scholar]
- 4. Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 2018;67:358–80. 10.1002/hep.29086 [DOI] [PubMed] [Google Scholar]
- 5. Bruix J, Sherman M. American association for the study of liver diseases. management of hepatocellular carcinoma: an update. Hepatology 2011;53:1020–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Omata M, Cheng A-L, Kokudo N, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int 2017;11:317–70. 10.1007/s12072-017-9799-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kudo M, Trevisani F, Abou-Alfa GK, et al. Hepatocellular carcinoma: therapeutic guidelines and medical treatment. Liver Cancer 2017;6:16–26. 10.1159/000449343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hiraoka A, Kumada T, Kudo M, et al. Real-Life practice experts for HCC (RELPEC) Study Group and HCC 48 group (hepatocellular carcinoma experts from 48 clinics). hepatic function during repeated TACE procedures and prognosis after introducing sorafenib in patients with unresectable hepatocellular carcinoma: multicenter analysis. Dig Dis 2017;35:602–10. [DOI] [PubMed] [Google Scholar]
- 9. Li X, Feng G-S, Zheng C-S, et al. Expression of plasma vascular endothelial growth factor in patients with hepatocellular carcinoma and effect of transcatheter arterial chemoembolization therapy on plasma vascular endothelial growth factor level. World J Gastroenterol 2004;10:2878–82. 10.3748/wjg.v10.i19.2878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Carmeliet P, Jain RK. Angiogenesis in cancer and other diseases. Nature 2000;407:249–57. 10.1038/35025220 [DOI] [PubMed] [Google Scholar]
- 11. Wang B, Xu H, Gao ZQ, et al. Increased expression of vascular endothelial growth factor in hepatocellular carcinoma after transcatheter arterial chemoembolization. Acta Radiol 2008;49:523–9. 10.1080/02841850801958890 [DOI] [PubMed] [Google Scholar]
- 12. Jiang H, Meng Q, Tan H, et al. Antiangiogenic therapy enhances the efficacy of transcatheter arterial embolization for hepatocellular carcinomas. Int J Cancer 2007;121:416–24. 10.1002/ijc.22655 [DOI] [PubMed] [Google Scholar]
- 13. Llovet JM, Ricci S, Mazzaferro V, et al. Sharp Investigators Study Group. sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008;359:378–90. [DOI] [PubMed] [Google Scholar]
- 14. Cheng A-L, Kang Y-K, Chen Z, et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol 2009;10:25–34. 10.1016/S1470-2045(08)70285-7 [DOI] [PubMed] [Google Scholar]
- 15. Yen C, Sharma R, Rimassa L, et al. Treatment stage migration maximizes survival outcomes in patients with hepatocellular carcinoma treated with sorafenib: an observational study. Liver Cancer 2017;6:313–24. 10.1159/000480441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Parsons HM, Chu Q, Karlitz JJ, et al. Adoption of sorafenib for the treatment of advanced-stage hepatocellular carcinoma in oncology practices in the United States. Liver Cancer 2017;6:216–26. 10.1159/000473862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Piscaglia F, Ogasawara S. Patient selection for transarterial chemoembolization in hepatocellular carcinoma: importance of benefit/risk assessment. Liver Cancer 2018;7:104–19. 10.1159/000485471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pawlik TM, Reyes DK, Cosgrove D, et al. Phase II trial of sorafenib combined with concurrent transarterial chemoembolization with drug-eluting beads for hepatocellular carcinoma. J Clin Oncol 2011;29:3960–7. 10.1200/JCO.2011.37.1021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cabrera R, Pannu DS, Caridi J, et al. The combination of sorafenib with transarterial chemoembolisation for hepatocellular carcinoma. Aliment Pharmacol Ther 2011;34:205–13. 10.1111/j.1365-2036.2011.04697.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sieghart W, Pinter M, Reisegger M, et al. Conventional transarterial chemoembolisation in combination with sorafenib for patients with hepatocellular carcinoma: a pilot study. Eur Radiol 2012;22:1214–23. 10.1007/s00330-011-2368-z [DOI] [PubMed] [Google Scholar]
- 21. Park J-W, Koh YH, Kim HB, et al. Phase II study of concurrent transarterial chemoembolization and sorafenib in patients with unresectable hepatocellular carcinoma. J Hepatol 2012;56:1336–42. 10.1016/j.jhep.2012.01.006 [DOI] [PubMed] [Google Scholar]
- 22. Kudo M, Imanaka K, Chida N, et al. Phase III study of sorafenib after transarterial chemoembolisation in Japanese and Korean patients with unresectable hepatocellular carcinoma. Eur J Cancer 2011;47:2117–27. 10.1016/j.ejca.2011.05.007 [DOI] [PubMed] [Google Scholar]
- 23. Lencioni R, Llovet JM, Han G, et al. Sorafenib or placebo plus TACE with doxorubicin-eluting beads for intermediate stage HCC: the space trial. J Hepatol 2016;64:1090–8. 10.1016/j.jhep.2016.01.012 [DOI] [PubMed] [Google Scholar]
- 24. Meyer T, Fox R, Ma YT, et al. Sorafenib in combination with transarterial chemoembolisation in patients with unresectable hepatocellular carcinoma (TACE 2): a randomised placebo-controlled, double-blind, phase 3 trial. Lancet Gastroenterol Hepatol 2017;2:565–75. 10.1016/S2468-1253(17)30156-5 [DOI] [PubMed] [Google Scholar]
- 25. Kudo M, Han G, Finn RS, et al. Brivanib as adjuvant therapy to transarterial chemoembolization in patients with hepatocellular carcinoma: a randomized phase III trial. Hepatology 2014;60:1697–707. 10.1002/hep.27290 [DOI] [PubMed] [Google Scholar]
- 26. Kudo M, Cheng A-L, Park J-W, et al. Orantinib versus placebo combined with transcatheter arterial chemoembolisation in patients with unresectable hepatocellular carcinoma (Oriental): a randomised, double-blind, placebo-controlled, multicentre, phase 3 study. Lancet Gastroenterol Hepatol 2018;3:37–46. 10.1016/S2468-1253(17)30290-X [DOI] [PubMed] [Google Scholar]
- 27. Kudo M, Arizumi T. Transarterial chemoembolization in combination with a molecular targeted agent: lessons learned from negative trials (Post-TACE, BRISK-TA, space, Oriental, and TACE-2). Oncology 2017;93:127–34. 10.1159/000481243 [DOI] [PubMed] [Google Scholar]
- 28. Ikeda M, Kudo M, Aikata H, et al. Transarterial chemoembolization with miriplatin vs. epirubicin for unresectable hepatocellular carcinoma: a phase III randomized trial. J Gastroenterol 2018;53:281–90. 10.1007/s00535-017-1374-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dmitrienko A, Offen WW, Westfall PH. Gatekeeping strategies for clinical trials that do not require all primary effects to be significant. Stat Med 2003;22:2387–400. 10.1002/sim.1526 [DOI] [PubMed] [Google Scholar]
- 30. Kudo M, Kubo S, Takayasu K, et al. Response evaluation criteria in cancer of the liver (RECICL) proposed by the liver cancer Study group of Japan (2009 revised version). Hepatol Res 2010;40:686–92. 10.1111/j.1872-034X.2010.00674.x [DOI] [PubMed] [Google Scholar]
- 31. Takayasu K, Arii S, Matsuo N, et al. Comparison of CT findings with resected specimens after chemoembolization with iodized oil for hepatocellular carcinoma. AJR Am J Roentgenol 2000;175:699–704. 10.2214/ajr.175.3.1750699 [DOI] [PubMed] [Google Scholar]
- 32. Kudo M, Izumi N, Kokudo N, et al. Management of hepatocellular carcinoma in Japan: consensus-based clinical practice guidelines proposed by the Japan Society of hepatology (JSH) 2010 updated version. Dig Dis 2011;29:339–64. 10.1159/000327577 [DOI] [PubMed] [Google Scholar]
- 33. Bruix J, Reig M, Rimola J, et al. Clinical decision making and research in hepatocellular carcinoma: pivotal role of imaging techniques. Hepatology 2011;54:2238–44. 10.1002/hep.24670 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
gutjnl-2019-318934supp001.pdf (27.8KB, pdf)
gutjnl-2019-318934supp002.pdf (50.4KB, pdf)
gutjnl-2019-318934supp003.pdf (122.2KB, pdf)
gutjnl-2019-318934supp004.pdf (94KB, pdf)


