Abstract
There has been a growing number of sexual health and blood-borne virus (SHBBV) surveys specifically administered to migrant populations. The purpose of this scoping review is to collate available information about how SHBBV surveys have been administered in migrant populations and the effect that mode of administration has on data quality, reliability and other practical considerations, e.g. response rates (RR) and social desirability bias. A methodological framework for scoping reviews was applied. SHBBV survey studies administered to international migrants published since 2000 were included if they contained some description of mode of administration. Ninety one studies were identified for inclusion from Embase, Medline, Web of Science, Google Scholar and supplementary grey literature. ‘Interview only’ was the most common mode of administration (n = 48), predominately comprising face-to-face interviews. Thirty six studies reported data from ‘self-completed’ surveys only, with pen-and-paper being most common (n = 17). Few studies (n = 7) combined interview and self-completed methods of survey administration. Sixty one studies did not report (or only partially reported) RR or the data necessary to calculate RR. Of the studies that reported RR, most were missing other key information including method of recruitment, consent procedures and whether incentives were offered. Strengths and limitations of all administration modes are summarised. Guidelines to inform future SHBBV survey research in migrant populations are presented.
Introduction
Migrants are a priority group for the prevention and control of HIV/AIDS [1]. Between 2007 and 2012, 42% of HIV diagnoses in Western Europe were in migrant populations [2]. Elsewhere such as in United States of America and Australia, migrants accounted for 19% and 38% of HIV diagnoses respectively [3, 4]. Existing research suggests that migrants may encounter legal, social, economic and cultural barriers to healthcare access in relation to HIV and other sexually transmissible infections and blood-borne viruses [5–7].
In spite of the priority for this population, migrants are often under-represented in research, including in the context of general population sexual health and blood-borne virus (SHBBV) surveys [8–10]. High quality data are needed to monitor whether strategic objectives relating to this population group are being met or need to be adjusted in response to changing circumstances. As such, there has been a growing number of SHBBV surveys specifically developed for migrant populations, including the African Health and Sex Survey in England, the Advancing Migrant Access to Health Services in Europe (aMASE) study and the HIV community survey in people from culturally and linguistically diverse backgrounds in New South Wales, Australia [11–13]. Additionally, the World Health Organisation is in the process of developing a standard instrument for measuring sexual health knowledge, practices and outcomes worldwide, and has sought submissions on implementation factors including survey administration channels [14, 15].
While there are a range of factors which can affect the quality of survey data (e.g. validity of survey constructs, sampling and recruitment methods), the focus of this article is the mode of survey administration. As a recent literature review shows, the manner of survey administration can greatly affect the quality of the data collected by influencing response rates, completion rates, respondent cognition and social desirability bias [16]. However, this review did not seek to determine whether certain modes of administration were more appropriate for specific topic areas, especially those of a sensitive nature. For instance, an Italian study on sexual behaviour in the general population compared results obtained via computer assisted telephone interviews (CATI) with self-answered questionnaires following interviews (SAQ-FI) and found that the SAQ-FI sample reported higher levels of early intercourse and same-sex attraction and had lower item non-response rates than the CATI sample [17].
How these differing modes of survey administration affect data quality can be even more complicated with respect to research in migrant populations. In culturally and linguistically diverse settings, self-administered questionnaires (SAQ) (which tend to be written) may be problematic because “languages spoken may not have a standard written form, or respondent literacy rates may be vastly different” [18]. Likely reflective of such concerns, a recent review of 550 empirical surveys of asylum seekers and minority groups found that over half (n = 293) were administered through face-to-face interviews, compared to 11% (n = 55) SAQ [19].
When collecting sensitive data from potentially vulnerable populations, researchers have an ethical imperative to ensure that any foreseeable harms are proportionate to the benefits that can flow from valid and reliable research outputs. However, there is still no strong/empirical guidance to determine appropriate modes of SHBBV survey administration among migrant populations. Therefore, we aimed to perform a scoping review of SHBBV surveys administered to international migrant populations in receiver countries to understand the effect that mode of administration has on key indicators of data quality and reliability, including response rates and social desirability bias. Practical and logistical considerations associated with the different modes of administration were also considered. The PRISMA extension for scoping reviews has been followed in the reporting of this study [20].
Materials and methods
An unregistered protocol was developed and is available on request from the corresponding author. The methodological framework for scoping reviews developed by Arksey and O’Malley [21] (set out in Table 1) was applied. The broad research objective was to determine what modes of survey administration have been used to conduct SHBBV surveys in migrant populations and to ascertain the strengths and limitations associated with each mode. The following sub-questions were set to meet the stated objective:
Table 1. Methodological framework for scoping studies, based on Arksey and O’Malley [21].
| STAGE | SUMMARY |
|---|---|
| 1. A research question is identified | Facets of the question (e.g. population, interventions, outcomes) are identified and defined. |
| 2. Potentially relevant studies are identified | A search strategy for a range of resources and databases is developed. The search is conducted within predefined parameters relating to factors such as language and date of publication/reporting. |
| 3. Relevant studies are selected | Studies identified in Stage Two are assessed against inclusion and exclusion criteria based on either a review of abstracts or the full study (if relevance cannot be established from the abstract). All studies which ‘pass’ this first screen are reviewed and assessed in full. |
| 4. Data are charted | Information relevant to the aims of the scoping review are extracted from each included study. |
| 5. Results are collated, summarized and reported | Data extracted in Stage Four are analyzed and findings are reported. |
With what frequency have different modes of administration been used to administer SHBBV surveys to migrants?
Is the mode of survey administration statistically associated with response rates, controlling for factors such as provision of recruitment incentives/gratuities and survey length?
What are the reported strengths and limitations of the different modes of survey administration, in terms of social desirability bias, project resources and other factors?
The review focussed on English-language papers published or released after 2000 (in light of the technological developments in survey administration). In order to be included, papers needed to contain: (a) primary analyses of data from SHBBV surveys administered to international migrants (i.e. people living in a country other than their birth country); and (b) some description of the mode of survey administration. General population surveys were excluded unless migrant and non-migrant responses were explicitly compared in the paper. Other exclusion criteria are set out in Table 2.
Table 2. Inclusion and exclusion criteria.
| Criteria | |
|---|---|
| Include if: | • Study is primary analysis of survey data |
| • Survey is aimed at or includes first-generation (externally-born) international migrants | |
| • Survey relates to the prevention, transmission or management of sexually transmissible infections and/or blood-borne viruses | |
| • Study contains some description of mode of survey administration | |
| Exclude if: | • Survey is aimed at migrant health professionals only |
| • Survey sample frame is the general population (unless the stated objective is to compare migrant and non-migrant responses) | |
| • Study relates to tourists / recreational travellers | |
| • Study seeks only to validate screening and diagnostic tools or tests used in clinical settings | |
| • Study is not in English language (although survey may be in another language) |
Searches were run in March and April 2019. The search strategy combined terms relating to three concepts–surveys, migrants and modes of survey administration. The terms were entered into the databases Embase, Medline and Web of Science (Core Collection) using database-specific subject headings and search syntax as set out in the Supplementary table (S1 Table). Supplementary searches were conducted in Google, Google Scholar, and ProQuest Theses and Dissertations with a view to locating grey literature and unindexed publications. These supplementary searches were more focussed given the search limitations of those platforms (Survey AND (Migrant OR Refugee OR Displaced OR Emigrant OR Immigrant OR "Foreign born" OR "Culturally and Linguistically diverse") AND (STI OR STD OR BBV OR Sexual OR HIV OR "Hepatitis B" OR "Hepatitis C")). Only the first 20 pages of results in Google and Google Scholar were reviewed, consistent with accepted practice [22].
Results were imported into Endnote and de-duplicated using the process developed by Bramer, Giustini et al. [23] for this purpose (e.g. tailored use of field settings and filters). One researcher screened the title and abstract of each identified study against the inclusion and exclusion criteria set out in Table 2 and categorised each study as ‘Potential Include’ or ‘Exclude’. The full text of all studies marked ‘Potential Include’ were then independently screened by two researchers and either marked for inclusion or exclusion with reasons. If the researchers reached different decisions, each researcher explained their rationale and, if consensus could not be reached, a third member of the research team assessed the item against the inclusion and exclusion criteria.
A charting form was developed in Excel by the second-named author and tested on the included studies identified through searches in Medline, Embase and Web of Science (see S2 Table). The form was revised for charting data in the remaining studies (i.e. those identified through Google, Google Scholar and ProQuest). The revisions involved reducing the number of charting categories and introducing fixed drop-down options into the Excel table (see S3 Table). Data were extracted by one researcher and cross-checked by a second researcher. Differences in coding decisions were resolved in the same manner as for screening (described above). The extracted data included information about the studies, including study setting, recruitment methods, sample size and characteristics, response rates, mode of survey administration, and reported information about the strengths and weaknesses of survey administration methods.
Following data extraction, it became apparent that different response rate calculation methods were being used in the included studies. As such, a decision was made to collect more detailed information relevant to response rate reporting. To that end, any studies in which a response rate was reported (or capable of being calculated) were reviewed and data extracted directly into Table 4 below, with a second researcher cross-checking for accuracy. Information on instrument validation was also collected post facto in response to a suggestion from one reviewer.
Table 4. Included studies with response rates reported or able to be calculated (n = 30), by other reported characteristics.
| Study | Survey mode | Reported response rate (%) | Reported information relevant to RR | How many and what type of attempts were made to contact subjects?* | Who approached potential subjects?* | Where were potential subjects approached?* | How was informed consent obtained?* | How did those who agreed differ from those who did not agree?* | What was the average time taken to complete survey (minutes)? | Was an incentive to participation offered? |
|---|---|---|---|---|---|---|---|---|---|---|
| Ahmed [28] | F2F interview | 48 | Number invited: 425 Number consented: 205 |
NR | NR | Mosques, local cafes, restaurants | Verbal | NR | 60 | No |
| Alvarez-del Arco, Fakoya et al. [30] | Device | 70 | Number invited: 3251 Number eligible: 3152 Number consented: 2209 |
NR | Researcher or member of clinical care team | Clinic | NR | Participation higher in men, decreased with age and was higher in migrants from Latin America and Eastern Europe and lower in those from Sub-Saharan Africa | NR | NR |
| Asante, Körner et al. [33] | Paper | >95 in Thai, Ethiopian and Sudanese communities Less in Cambodian community |
Only reported for Cambodian community Number invited: 104 Number consented: 86 |
NR | Co-workers from the relevant language backgrounds, as well as some members of the reference groups, would lead the recruitment and assist participants to complete the questionnaires | Mainly at places of worship, community events and other social gatherings | NR | NR | 20–25 | NR |
| Bastani, Glenn et al. [34] | Paper Phone interview |
94 (B) 86 (F) |
Number screened: 1,866 Number eligible: 1,196 Number enrolled at baseline: 1,123 |
In-person on a single day | Staff members | Church | NR | NR | NR | NR |
| Coronado, Taylor et al. [40] | F2F interview | Figure not reported but relevant data presented (see next column) | Number screened: 1,902 Number enrolled: 436 (6 later excluded due to ineligibility) Number refused: 314 Number ineligible at screening: 628 households + 105 (non-residential) Number unable to be contacted: 419 |
Households received an introductory letter (traditional Chinese, simplified Chinese, and English versions). Called 2 weeks later. Up to 5 contact attempts made. | Chinese interviewer of same gender | Home | NR | NR | 30 | Calendar and $20 |
| Duan, Ding et al. [26] | F2F interview | Figure not reported but relevant data presented (see next column) | Among the total of 7656 mixed couples, 6269 Chinese spouses and 7092 Burmese immigrant spouses gave informed consent to participate including both spouses of 5742 couples. Only the 5742 couples with both spouses participating in the survey were included. | NR | Trained public health worker (or, where necessary, village or community clinical doctors who were able to speak and understand Burmese) | NR (but interviews principally conducted in homes) | NR | NR | NR | $10 |
| Evans, Suggs et al. [49] | Paper Online Phone Device (SMS) |
61 | Number invited: 281 Number consented: 172 (3 later excluded) |
Not reported for baseline | Community researchers | Voluntary sector groups and community venues | Written | NR | NR | GBP 5 shopping voucher |
| Foster, McCormack et al. [55] | Paper | 94 | Number distributed: 488 Number returned: 460 |
NR | Sexual health clinic staff and health education officers | Sexual health clinic and sex work parlours | Implied (consent form prefaced survey) | NR | NR | NR |
| Grieb, Flores-Miller et al. [59] | Paper | Figure not reported but relevant data presented (see next column) | Number screened: 135 Number eligible: 113 Number consented: 104 |
NR | Trained research assistants | Street- and community-based venues | Verbal | NR for non-response/refusals but noted that no differences in age, country of origin, education, time in the United States, or time in Baltimore were observed between those who were eligible and those who were not. | 10–15 | $10 |
| Hamdiui, Stein et al. [60] | Paper Online |
69.1 | Number invited: 350 Number participated: 242 (excluding 165 people recruited by participants who accepted the invitation–no RR reported for the total sample which included respondent-driven sampling methods) |
Number of attempts NR Online-recruited respondents were enrolled through advertisements on Moroccan-Dutch forums, Facebook, Instagram, websites. Recruiting peers online was enabled through indirect email, WhatsApp, Facebook, or by sharing a hyperlink. |
Peer (respondent-driven sampling) | Online and at community venues, such as community centres, day care centres, mosques, interest groups, and civil support foundations. | NR | NR | NR | Gift coupon when recruited at least three other respondents (value increased in three steps to enhance peer recruitment: €5, €10, and €25). |
| Hislop, Teh et al. [61] | F2F interview | 59 | Households selected: 1500 Number of non-residential: 41 Number unable to contact: 149 Number ineligible: 375 Number refused: 384 Number of interviews completed: 551 (504 when non-migrants excluded) |
Five door-to-door attempts | Trilingual Chinese interviewer | Home | NR | NR | 45 | $20 |
| Jenkins, McPhee et al. [63] | Phone interview | 93 | Call attempts: 12,094 Call attempts that reached eligible respondents: 1624 Number consented: 1508 |
Up to five attempts by phone | NR | Phone | NR | NR | NR | NR |
| Juon, Lee et al. [67] | Paper | 98 (B) 78 (F) |
Eligible program participants: 940 Number of no-shows: 47 Number who did not complete baseline or did not participate: 13 Number who participated in program in past year: 3 Number who completed baseline: 877 Number who completed follow-up: 688 |
NR | NR | Community based organisations, college cultural organisations, Asian grocery stores, restaurants, nail salons | NR | NR for baseline Differences at follow-up described | NR | NR |
| Kara [68] | Paper Online |
35 | Number of surveys distributed: 525 Number of surveys returned: 186 |
NR | Partners from member organisations made initial contact | Online | Electronic (for online survey) Implied (for written survey) | NR | 10–30 | NR |
| Lessard, Lebouche et al. [71] | Phone interview | 54 | Number eligible: 74 Number refused: 4 Number unable to be contacted: 30 Number participants: 40 |
NR | Service staff member made initial contact, followed up by researcher | Phone | Written | NR | 10–15 | None |
| Maxwell, Bastani et al. [76] | F2F interview Phone interview |
51 (B) 68 (F) |
Number recruited at clinic: 98 Number who attended workshop: 46 (+ 8 peer recruits) Number who completed baseline survey: 54 Number who completed follow-up survey: 44 workshop attenders and 28 non-attenders |
NR | Clinical phlebotomist briefly described study, researcher followed up with those interested | Clinic | Written | Participants who completed post-test reported significantly more years of schooling than those who did not complete. | NR | $5 for initial interview, $10 for workshop participation, $15 for post-test |
| Montealegre, Risser et al. [79] | F2F interview | Figure not reported but relevant data presented (see next column) | Number screened: 230 Number eligible: 222 Number consented: 221 (one did not complete interview and data from ten excluded from analysis or lost) |
Number of attempts NR Seeds and eligible participants were given three serially numbered study coupons to recruit peers. Study coupons provided recruits with the name and a short description of the study, project phone number, name and address of the interview sites, hours of operation, and the coupon’s expiration date. |
Peer (respondent-driven sampling) | NR | Verbal | NR | 60 | Seeds and participants were given $20 for completing the interview and $5 for each of up to three peers they recruited into the survey. |
| O'Connor, Shaw et al. [80] | Phone interview | 66 | Number invited: 761 Number consented: 506 (seven later excluded from analysis) |
NR | Men were telephoned by a Vietnamese speaking woman | Phone | NR | NR | NR | NR |
| Ogungbade [81] | Paper | 86 | Number of surveys distributed: 194 Number of surveys returned: 167 |
Flyers distributed. Researcher addressed potential participants at an event. Returned one week later to conduct survey. | Researcher (Nigerian migrant) | Faith-based organisations | Implied consent form given explaining that completion of survey was considered consent | NR | NR | NR |
| Organista and Kubo [82] | F2F interview | >90 | Notes from outreach workers indicate that less than 10% of men approached refused participation. | NR | Spanish-speaking project team members who introduced themselves as local public health outreach workers | Street corner | NR | NR | 45 | $20 fast food voucher |
| Ramanathan and Sitharthan [86] | Online | 42 | Number surveys attempted: 438 Number of surveys completed: 278 Number of completed surveys in which SHBBV section also completed: 184 |
Advertisements on Indian specific websites and social networking websites (e.g. Google, Facebook). | N/A (internet advertising) | Indian specific websites and social networking websites | NR | NR | NR | NR |
| Rangel, Martinez-Donate et al. [87] | Paper | 90 | Number invited: 1,606 Number consented: 1,429 |
NR | Trained Mexican interviewers | International airport, bus stations, deportation stations | Verbal | NR | NR | NR |
| Salabarria-Pena, Lee et al. [89] | F2F interview | 97 | Number invited: 222 Number ineligible: 42 Number refused: 5 |
In-person (quantity unclear) | NR | Clinic waiting room | Verbal | NR | 60 | NR |
| Santos-Hovener, Marcus et al. [91] | Paper F2F interview Phone interview |
Figure not reported but relevant data presented (see next column) | Surveys distributed: 950 Number returned: 649 Number eligible: 569 |
NR | Peer researchers | NR | Verbal | NR | NR | Key chain, shopping cart chip, referral to health promotion information sessions, condom, informational flyers and free testing services |
| Şimşek, Yentur Doni et al. [94] | F2F interview | 100 | A total of 961 married women were identified in 458 houses. One eligible woman from each selected house was randomly selected. A total of 458 women provided written and signed informed consent; the response rate among eligible women was 100.0 percent. | 12 attempts made to contact | Trained Syrian midwife research assistant, lab technician and a translator from the area | Home | Written and verbal | NA | NR | NR |
| Taylor, Jackson et al. [99] | Phone interview | 70 | Initial sampling frame: 161 Number unable to contact/ phone disconnected: 42 Number ineligible: 12 Number consented: 75 |
Number of attempts NR Introductory letter followed by telephone call |
Bilingual, bicultural Vietnamese survey workers | Home | NR | NR | NR | $10 voucher |
| Taylor, Jackson et al. [100] | F2F interview | 73 (B) 56 (F) |
NR for baseline Three hundred and twenty (77 percent) of the 413 women who participated in the baseline survey also completed the follow-up survey. Therefore, the estimated overall response rate with respect to the hepatitis B questions was 56 percent (i.e., 77 percent of 73 percent). |
NR | Bilingual, bicultural Cambodian women | Home | NR | NR | NR | Calendar at baseline, $5 at follow up |
| Taylor, Choe et al. [101] | F2F interview | 80–82 | Details obtained from related papers cited. Number of unsuccessful contact attempts: 41 (women); 47 (men) Number ineligible: 116 (women); 131 (men) Number eligible but refused: 66 (women); 70 (men) Number completed: 370 (women); 345 (men) Estimated proportion of eligible where eligibility was not established: 79% (women); assume proportion of eligible same as those not contactable (men) |
Five door-to-door attempts | Bilingual, bicultural interviewers (gender matched) | Home | NR | NR | 45 | Posters |
| Taylor, Tu et al. [102] | F2F interview | Figure not reported but relevant data presented (see next column) | Interviews completed: 436 Number of households refused: 314 Number of households ineligible: 628 Number of uncontactable households: 419 (plus 105 non-residential addresses) |
Introductory letter followed by five door-to-door attempts | Chinese interviewer of same gender | Home | NR | NR | NR | $20 |
| UNHCR [106] | F2F interview | Figure not reported but relevant data presented (see next column) |
Kala camp Number of forms completed: 828 Number of refusals: 34 Number unable to contact: 224 Kala communities Number of forms completed: 880 Number of refusals: 17 Number unable to contact: 169 Mwange camp Number of forms completed: 916 Number of refusals: 20 Number unable to contact: 389 Mwange communities Number of forms completed: 854 Number of refusals: 16 Number unable to contact: 349 |
In-person 1–3 times | Research assistants | Home | Oral (with interviewer’s signature) | NR | NR | NR |
Results
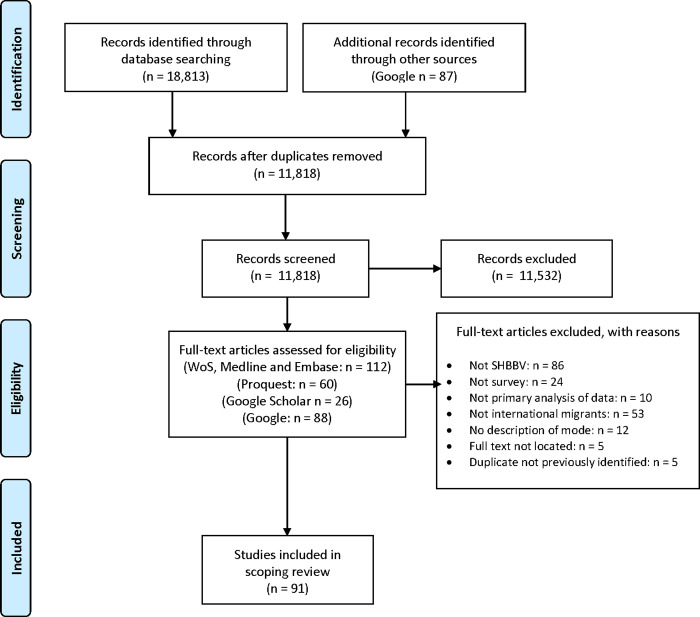
Ninety one studies were identified for inclusion following the search-and-screen process represented in Fig 1.
Fig 1. PRISMA flow diagram of scoping review stages [24].
Key characteristics of the studies are set out in Table 3. The majority of studies (n = 51) were conducted in North America, followed by Europe/Eurasia (n = 22), Australia (n = 8), Asia (n = 6), Africa (n = 2) and Latin America and the Caribbean (LAC) (n = 2). Globally, the majority of SHBBV surveys were administered to migrants born in Asia (n = 40), LAC (n = 31) or Africa (n = 28). Only four included studies reported data from SHBBV surveys administered to migrants from Middle Eastern countries. Sample sizes ranged from six migrant participants [25] to 11,484 participants [26].
Table 3. Included studies (n = 91), by key characteristics.
| # | Author(s) and year | Country of study | Migrant region of origin | Mode of administration | SHBBV instrument used | Sample size |
|---|---|---|---|---|---|---|
| 1 | Agbemenu, Terry et al. [27] | USA | Africa | Paper | New instrument developed (not clear if tested) | 15 |
| Online | ||||||
| 2 | Ahmed [28] | USA | Africa | F2F interview | New instrument developed (not clear if tested) | 201 |
| 3 | Alber, Cohen et al. [29] | USA | Asia | Online | Based on / used an existing instrument | 418 |
| 4 | Alvarez-del Arco, Fakoya et al. [30] | Europe(9 countries) | Africa | Device | Based partly on / used an existing instrument | 2,209 |
| LAC | ||||||
| Europe | ||||||
| 5 | Amadi [31] | USA | Africa | Paper | Based partly on / used an existing instrument | 395 |
| 6 | Arevalo [32] | USA | LAC | Paper | Based on / used existing instrument | 80 |
| F2F interview | ||||||
| 7 | Asante, Körner et al. [33] | Australia | Africa Asia | Paper | New instrument developed (not clear if tested) | 286 |
| 8 | Bastani, Glenn et al. [34] | USA | Asia | Paper | Based on / used existing instruments | 1,123 |
| Phone interview | ||||||
| 9 | Beltran, Simms et al. [35] | USA | Asia | Online | Based on / used existing instruments | 192 |
| Paper | ||||||
| 10 | Burns, Fenton et al. [36] | UK | Africa | F2F interview | Based partly on / used existing instruments | 385 (incl. ~25% UK born) |
| Device | ||||||
| 11 | Chamratrithirong, Boonchalaksi et al. [37] | Thailand | Asia | F2F interview | New instrument developed + pretested | 3,426 |
| 12 | Chen, Guthrie et al. [38] | USA | Asia | Device | Based on / used existing instruments | 50 |
| 13 | Cohen [39] | USA | Asia | Paper | New instrument developed + pilot tested | 2,004 (excl. US born) |
| F2F interview | ||||||
| 14 | Coronado, Taylor et al. [40] | USA | Asia | F2F interview | New instrument developed + pretested | 430 (may include US-born) |
| 15 | Dean, Mitchell et al. [41] | Australia | Africa | Paper | Based on / used existing instruments | 229 |
| 16 | Delgado, Lundgren et al. [42] | USA | LAC | F2F interview | NR | 200 |
| 17 | Demeke [43] | USA | Africa | F2F interview | Based on / used existing instruments | 37 (excl. US born) |
| 18 | Dennis, Wheeler et al. [44] | USA | LAC | F2F interview | NR | 127 |
| 19 | Dias, Gama et al. [45] | Portugal | Africa | F2F interview | NR | 1,513 |
| Asia | ||||||
| Europe | ||||||
| LAC | ||||||
| 20 | Duan, Ding et al. [26] | China | Asia | F2F interview | Based on / used existing instruments | 11,484 |
| 21 | Elford, Doerner et al. [46] | UK | Africa | Online | NR | 1,334 |
| Asia | ||||||
| Europe | ||||||
| LAC | ||||||
| 22 | Elford, McKeown et al. [47] | UK | Africa | Online | Based on / used existing instruments | 1,241 |
| Asia | ||||||
| Europe | ||||||
| LAC | ||||||
| 23 | Evans, Hart et al. [48] | UK | Europe | Online | NR | 206 |
| 24 | Evans, Suggs et al. [49] | UK | Africa | Paper | New instrument developed + pilot tested | 169 |
| Online | ||||||
| Phone | ||||||
| Device (SMS) | ||||||
| 25 | Fakoya, Alvarez-Del Arco et al. [50] | Europe (multiple) | Africa | Online | Based partly on / used existing instruments | 1,637 |
| LAC | ||||||
| 26 | Fenton, Chinouya et al. [51] | UK | Africa | Paper | New instrument developed (not clear if tested) | 720 (excl. UK born) |
| 27 | Fernandez-Esquer, Atkinson et al. [52] | USA | LAC | F2F interview | Based partly on / used an existing instrument | 152 |
| 28 | Fitzgerald, Chakraborty et al. [53] | USA | LAC | F2F interview | New instrument developed (not clear if tested) | 19 (excl. US born) |
| 29 | Ford and Chamrathrithirong [54] | Thailand | Asia | F2F interview | New instrument developed + pretested | 3,426 |
| 30 | Foster, McCormack et al. [55] | Australia | Asia | Paper | Based on / used instruments | 435 |
| 31 | Getrich, Broidy et al. [56] | USA | LAC | F2F interview | NR | 6 (excl. US-born) |
| 32 | Goldade and Nichter [57] | Costa Rica | LAC | F2F interview | NR | 33 |
| 33 | Gray, Crawford et al. [58] | Australia | Africa | Paper | Based on / used existing instruments | 209 |
| Asia | Device | |||||
| Online | ||||||
| 34 | Grieb, Flores-Miller et al. [59] | USA | LAC | Paper | NR | 104 |
| 35 | Hamdiui, Stein et al. [60] | Netherlands | Africa | Paper | New instrument developed + pretested | 193 (excl. Dutch born) |
| Online | ||||||
| 36 | Hislop, Teh et al. [61] | Canada | Asia | F2F interview | New instrument developed + pretested | 503 |
| 37 | Hwang, Huang et al. [62] | USA | Asia | Paper | Based on / used existing instruments | 128 (excl. US born) |
| 38 | Jenkins, McPhee et al. [63] | USA | Asia | Phone interview | New instrument developed + pretested | 1508 |
| 39 | Johnston [64] | Armenia | Europe | F2F interview | New instrument developed + piloted | 945 |
| Azerbaijan | ||||||
| Georgia | ||||||
| 40 | Joseph, Belizaire et al. [65] | USA | LAC | F2F interview | New instrument developed (not clear if tested) | 20 (excl. US born) |
| 41 | Juon, Strong et al. [66] | USA | Asia | Paper | NR | 232 |
| 42 | Juon, Lee et al. [67] | USA | Asia | Paper | NR | 877 |
| 43 | Kara [68] | USA | Africa | Paper | Based on / used existing instruments | 164 |
| Online | ||||||
| 44 | Kuehne, Koschollek et al. [69] | Germany | Africa | Paper | Based on / used existing instruments | 2,720 |
| F2F interview | ||||||
| 45 | Leite, Buresh et al. [70] | USA | LAC | F2F interview | New instrument developed (not clear if tested) | 200 (excl. US born) |
| 46 | Lessard, Lebouche et al. [71] | Canada | Africa | Phone interview | Based on / used existing instruments | 40 |
| Asia | ||||||
| Europe | ||||||
| LAC | ||||||
| Middle East | ||||||
| 47 | Lin, Simoni et al. [72] | USA | Asia | Online | Based partly on / used existing instruments | 144 |
| 48 | Lofters, Vahabi et al. [73] | Canada | Asia | Paper | NR | 30 |
| 49 | Loos, Manirankunda et al [74] | Belgium | Africa | Paper | NR | 139 |
| LAC | ||||||
| 50 | McGregor, Mlambo et al. [13] | Australia | Africa | Paper | Based on / used existing instruments + pilot tested | 1,406 |
| Asia | ||||||
| 51 | Manoyos, Tangmunkongvorakul et al. [75] | Thailand | Asia | F2F interview | Based on / used existing instruments | 442 |
| 52 | Maxwell, Bastani et al. [76] | USA | LAC | F2F interview | Based partly on / used existing instruments | 106 |
| Phone interview | ||||||
| 53 | Miller, Guarnaccia et al. [77] | USA | LAC | Phone interview | Based on / used existing instruments | 85 (excl. US born) |
| 54 | Montealegre [78] | USA | LAC | F2F interview | NR | 210 |
| 55 | Montealegre, Risser et al. [79] | USA | LAC | F2F interview | NR | 210 |
| 56 | O'Connor, Shaw et al. [80] | Australia | Asia | Phone interview | Based on / used existing instruments | 499 |
| 57 | Ogungbade [81] | USA | Africa | Paper | Based on / used existing instruments | 167 |
| 58 | Organista and Kubo [82] | USA | LAC | F2F interview | Based on / used existing instruments | 102 |
| 59 | Pannetier, Ravalihasy et al. [83] | France | Africa | F2F interview | Based on / used existing instruments | 980 |
| 60 | Platt, Grenfell et al. [84] | UK | Europe | Device | NR | 268 |
| 61 | Plewes, Lee et al. [85] | Thailand | Asia | F2F interview | NR | 109 |
| 62 | Ramanathan and Sitharthan [86] | Australia | Asia | Online | Based on / used existing instruments | 184 |
| 63 | Rangel, Martinez-Donate et al. [87] | Mexico | LAC | Paper | New instrument developed (not clear if tested) | 1,429 |
| 64 | Saenz [88] | USA | LAC | F2F interview | Based on / used existing instruments | 141 |
| 65 | Salabarria-Pena, Lee et al. [89] | USA | LAC | F2F interview | New instrument developed (not clear if tested) | 175 |
| 66 | Salehi [90] | Canada | Various (unspecified) | Paper | Based on / used existing instruments | 141 |
| 67 | Santos-Hovener, Marcus et al. [91] | Germany | Africa | Paper | Based on / used existing instruments + pretested | 596 |
| F2F interview | ||||||
| Phone interview | ||||||
| 68 | Selvey, Lobo et al. [92] | Australia | Asia | Paper | Based on / used existing instruments | 94 (excl. non-Asian born) |
| Online | ||||||
| 69 | Shiau, Bove et al. [93] | USA | Asia | F2F interview | New instrument developed (not clear if pretested) | 270 (excl. US born) |
| Phone interview | ||||||
| 70 | Şimşek, Yentur Doni et al. [94] | Turkey | Middle East | F2F interview | Based on / used existing instruments | 458 |
| 71 | Spadafino, Martinez et al. [95] | USA | LAC | F2F interview | NR | 176 |
| Phone interview | ||||||
| 72 | Srithanaviboonchai, Choi et al. [96] | Thailand | Asia | F2F interview | NR | 429 |
| 73 | Stromdahl, Liljeros et al. [97] | Sweden | Africa | Online | New instrument developed + piloted | 244 |
| Asia | ||||||
| Europe | ||||||
| LAC | ||||||
| 74 | Sumari-de Boer, Sprangers et al. [98] | Netherlands | Africa | F2F interview | Based on / used existing instruments | 112 |
| Europe | ||||||
| 75 | Taylor, Jackson et al. [99] | USA | Asia | Phone interview | Based on / used existing instruments | 75 |
| 76 | Taylor, Jackson et al. [100] | USA | Asia | F2F interview | Based on / used existing instruments | 413 |
| 77 | Taylor, Choe et al. [101] | USA | Asia | F2F interview | Based on / used existing instruments | 715 |
| 78 | Taylor, Tu et al. [102] | USA | Asia | F2F interview | New instrument developed + pretested | 395 |
| 79 | Taylor, Seng et al. [103] | USA | Asia | Phone interview | NR | 111 |
| 80 | Thompson, Taylor et al. [104] | USA | Asia | F2F interview | Based on / used existing instruments | 116 (excl. North American born) |
| 81 | Tu, Li et al. [105] | USA | Asia | F2F interview | New instrument developed (not clear if pretested) | 945 (excl. USA and Can. born) |
| Canada | ||||||
| 82 | UNHCR [106] | Zambia | Africa | F2F interview | Based on / used existing instruments | 822 |
| 83 | UNHCR [107] | Kenya | Africa | F2F interview | Based on / used existing instruments | 1,646 |
| 84 | Uribe, Darrow et al. [108] | USA | LAC | Phone | NR | 1,266 (excl. US born) |
| 85 | van der Veen, Voeten et al. [109] | Netherlands | Middle East | Paper | Based partly on / used existing instruments | 174 (excl. Dutch born) |
| 86 | Viadro and Earp [110] | USA | LAC | F2F interview | NR | 43 |
| 87 | Villarreal, Wiley et al. [111] | USA | LAC | Paper | New instrument developed + piloted | 24 (excl. US born) |
| 88 | Westmaas, Kok et al. [112] | Netherlands | Europe | Paper | Based on / used existing instruments | 753 |
| Online | ||||||
| 89 | Yau, Ford et al. [113] | Canada | Asia | Phone interview | New instrument developed (not clear if tested) | 1,013 overall (may include Canadian born) |
| 90 | Zellner, Martínez-Donate et al. [114] | USA | LAC | Device | NR | 647, excl. US born |
| 91 | Zhussupov, McNutt et al. [115] | Kazakhstan | Middle East | F2F interview | NR | 422 |
F2F = face-to-face
NR = not reported
LAC = Latin America and the Caribbean
NR = Not reported
In 44 studies, existing SHBBV instruments were adapted or used. These instruments included the Brief HIV Screener [116], the Perceived Susceptibility to HIV Scale [117], the AIDS Health Belief Scale [118], the National Survey of Australian Secondary Students and Sexual Health [119], the Survey of Latino Adults [120, 121], the African Health and Sex Survey [12], the Bass Line Survey [122], UN Behavioral Surveillance Surveys [123] and the National Health Interview Survey Supplement on AIDS Knowledge and Attitudes [124]. For the remaining studies, either the origin of the survey items was not reported (n = 23) or new survey instruments were developed (n = 24). Of the studies in which new survey instruments were developed, half (n = 12) did not explicitly report whether the instrument had been pretested or piloted.
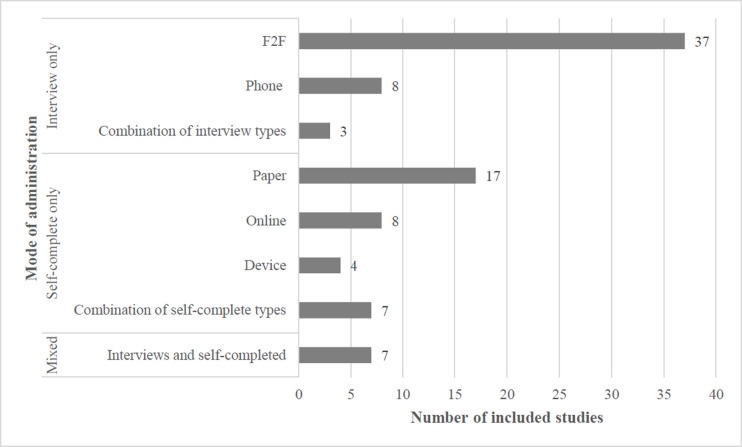
As shown in Fig 2, ‘interview only’ was the most common mode of survey administration (n = 48), with face-to-face (n = 37) being the most common interview technique. Of the thirty six studies reporting data from ‘self-completed’ surveys only, pen-and-paper was the most common method of self-completion (n = 17). Few studies (n = 7) combined interview and self-completed methods of survey administration.
Fig 2. Included studies (n = 91), by mode of survey administration.
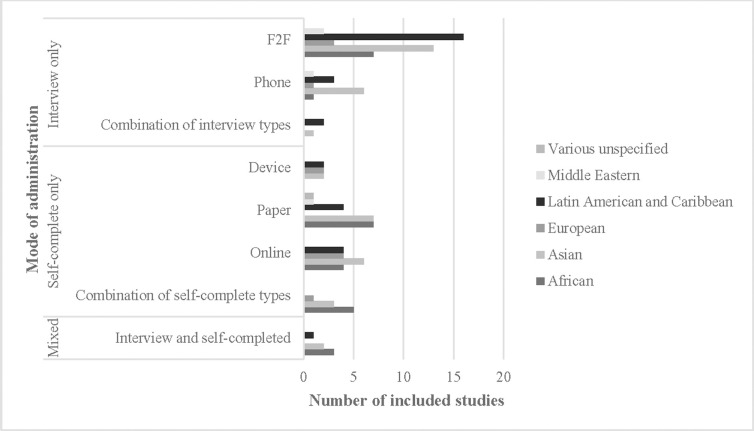
Fig 3 shows that some modes of SHBBV survey administration have been implemented more in some populations, compared to others. For instance, face-to-face only interviews were more commonly administered to LAC (n = 16) and Asian (n = 13) migrants; by contrast, pen-and-paper only surveys were used less frequently in LAC communities (n = 4). The small number of ‘online only’ and ‘device only’ surveys were relatively evenly distributed across LAC, Asian, African and European migrant populations.
Fig 3. Included studies (n = 91), by mode of administration and migrants’ region of origin.
Given the level of reporting in the included studies, it was not possible to determine whether certain modes of administration were associated with higher response rates, controlling for other factors. Sixty one studies (67%) either: (a) did not report response rates or the data necessary to calculate response rates; or (b) partially reported them (e.g. did not specifically report for overseas-born sample members or did not report response rates for all modes of administration).
Of the 30 studies where response rates were reported or able to be calculated (Table 4), the most common mode of administration was face-to-face interview only (n = 12), followed by pen-and-paper only (n = 6). By contrast, online administration was only used in four studies and was used in combination with other modes in three of those cases. Several studies noted the difficulties associated with determining the denominator required to calculate response rates when administering surveys online (e.g. Elford, Doerner et al. [46], Fakoya, Alvarez-Del Arco et al. [50], Gray, Crawford et al. [58]). Additionally, Ramanathan and Sitharthan [86] noted that noneligible persons could participate in online surveys and that the same respondent could complete the survey multiple times unless identifying data (e.g. IP addresses) were collected and stored.
The majority of the 30 studies reported response rates exceeding 50 percent, although the methods for calculating response rates varied. Generally, response rates were calculated by dividing the number of complete (and, in some cases, partial) eligible surveys by the sum of the number of ineligible cases, refusals, unsuccessful contact attempts and all cases of unknown eligibility. However, in other studies, attempts were made to estimate the number of cases of unknown eligibility which were ineligible and those cases were excluded from the denominator. For instance, Taylor, Choe et al. [101] reported “the overall estimated response rate was 80% among men and 82% among women (assuming the same proportions of eligible men and women among those who could and could not be contacted)”.
Additionally, there was a general lack of reporting on data relevant to assessing the quality of the response rates. For instance, 14 studies (47%) did not report whether incentives to participation were offered, 14 studies (47%) did not report on the method for obtaining informed consent, and 27 studies (90%) did not provide data to enable the characteristics of participants to be compared to non-responders.
The strengths and limitations of the various methods were discussed in the examined literature. Face-to-face interviews were considered useful when surveying populations with low levels of literacy [52, 89]. However, this method of administration was often human resource intensive and associated with logistical issues, including the need to find accessible and sufficiently private interview sites at mutually convenient times for multiple researchers and participants [64, 78, 79, 106].
While one study considered face-to-face interaction to be an important element of building trust [70], several noted the potentially increased risk of social desirability bias when disclosing sensitive information in-person [32, 35, 44, 51, 52, 83, 89, 110], and it was noted that consideration should be given to the characteristics of the interviewer. For instance, in a study of the health knowledge, attitudes and behaviours of U.S. Latino men who have sex with men, Arevalo [32] warned that “[s]ocial desirability may have been magnified by the interviewer, given that he was relatively more verbal, educated and overall healthier than the average participant.” A study of the sexual behaviour of male Mexican migrants to the United States observed that extramarital sex may have been underreported to female interviewers who lived in the respondents’ community or were casually known to the respondents’ wives [110].
Although telephone interviews have the potential to increase respondents’ sense of ‘anonymity’, the risk of social desirability bias may still remain because telephone respondents might be unable to answer questions in a private location away from other household residents [108]. The included studies also report that telephone interviews may result in selection bias [40, 63, 77, 100, 113]. For instance, Miller, Guarnaccia et al. [77] observed that recent Latino migrants to New Jersey were less likely to have residential telephones or may have “rapid turnover of telephone numbers” due to high residential mobility.
The risk of selection bias was also reported in the studies which utilised online surveys [29, 49, 92, 97]. Online surveys have the potential to exclude respondents who lack internet access or technological proficiency, or who are wary of disclosing sensitive information online. Selvey, Lobo, et al. [92] found that only a minority of Asian sex workers in Australia completed online versions of a survey, with most preferring pen-and-paper (although the difference may have been attributable to the recruitment methods associated with each). A study of HIV testing among African migrants living in the UK found that none of the 169 respondents completed an online follow-up survey, although 60 subsequently agreed to participate in a telephone interview; this led the authors to conclude that online data collection “was not feasible in this population group” [49]. However, online recruitment and administration was considered advantageous in studies of migrant men who have sex with men (MSM) in Britain [46, 47]. According to Elford, McKeown, et al. [47], “[u]sing an online survey we were able to survey MSM across Britain from a diverse range of backgrounds.”
One study recommended the use of computer-assisted self-interviews (CASI) in future research as a means of “address[ing] the need for privacy and the low literacy levels” in some migrant populations [52]. Empirical data on the strengths and limitations of this mode of survey administration were not presented in any of the included studies.
Discussion
The primary objective of this scoping review was to determine best practices from the published literature to ensure that future SHBBV surveys are conducted both effectively and efficiently in migrant populations. However, the widespread lack of reporting on key survey characteristics made it difficult to appraise which mode of survey administration is likely to collect the most reliable data to inform future migrant SHBBV service provision and planning. Researchers are thus limited in their ability to avoid past missteps and replicate successes in study design, creating the risk of both resources and participants’ time being wasted.
Only a minority of studies in this scoping review reported response rates and, of those, few provided a comprehensive description of other key survey characteristics. The findings are consistent with a recent review of empirical surveys of asylum-related migrants and minority groups which found that “information on methodological aspects, such as response/cooperation/participation rate, sampling frames, sampling strategies … are often missing or are not specified and discussed” [19]. These findings emphasise the need for greater adherence to (or awareness of) reporting standards [125]. For instance, the STROBE checklist for observational studies requires details about setting (e.g. recruitment sites and sources), eligibility criteria, method of recruitment, and numbers of individuals at each stage of the study, and reasons for non-participation at each stage [126]. Survey-specific checklists also recommend reporting additional details including description of the survey instrument and its development, pretesting processes, instrument reliability and validity, sample representativeness, mode of administration, number of attempts made to contact subjects, whether incentives were offered, methods for analysis of nonresponse error and descriptions of consent procedures (see data extraction tool published by Bennett, Khangura, et al. [127]).
There are also ethical implications associated with the lack of transparency. The principles of beneficence and non-maleficence require researchers “to seek the greatest benefit for research participants while minimizing harm” [128]. When examining a sensitive subject matter (e.g. sexual knowledge and behaviours) with potentially vulnerable participants (e.g. migrants), researchers must feel confident that any potential discomfort to participants is outweighed by the expected benefits which, at the very least, should take the form of valid and reliable findings. In order to weigh the potential harms against the potential benefits, researchers need to understand how SHBBV information has been collected from migrant populations in the past, and whether those methods produced valid and reliable data (and, if not, why not). This ethical arithmetic is not easily performed based on the information reported in the studies included in this review.
The information that we have about the use of online SHBBV surveys in migrant populations offers a case in point. There has been an increase in the use of online surveys for SHBBV research in migrant populations since 2010, as is evident in Table 3; this reflects increased general access to the internet and the development of a number of affordable and accessible survey software development tools [129, 130]. However, the included studies in this scoping review broach some important considerations about the appropriateness of online SHBBV surveys in migrant settings. For instance, Selvey, Lobo et al. [92] and Evans, Suggs et al. [49] had limited success in using online surveys to obtain data from Asian Australian sex workers and African migrants living in the UK respectively. By contrast, Elford et al. [46, 47] considered SHBBV online surveys a useful tool. Based on the available information, future researchers are faced with a dilemma as to whether they can reasonably expect valid and reliable SHBBV data from online surveys in migrant populations. More data are needed to provide guidance to researchers considering the use of this mode of survey administration. As Poynton, DeFouw, et al. [131] note, online survey methods “will continue to be poorly understood until researchers plan for and more thoroughly report information related to response rates.” Their specific recommendations for the conduct and reporting of online survey research should be heeded (e.g. create separate links to the survey for each mode of invitation or dissemination; document undeliverable emails; keep records of the number of people on electronic mailing lists and in online discussion boards) [131].
Despite the dearth of data reported in the included studies, the following principles are suggested to guide the administration of SHBBV surveys in migrant contexts:
SHBBV survey researchers should begin the survey design process with a clear profile of their sample population. The profile can either be created by drawing upon existing data or in consultation with informed community stakeholders. Where possible, the profile should include information about: (a) languages spoken; (b) written literacy; (c) access to relevant technology (e.g. internet, phones) and technological proficiency; (d) social customs governing researcher/participant interactions (e.g. gender/class considerations); and (e) perceived attitudes to the subject areas that are the focus of the survey.
The sample profile should inform the choice of survey administration mode, based on mode-specific considerations which include those set out in Table 5.
Where possible, consideration should be given to mixed-modes of survey data collection to overcome the limitations associated with using each mode in isolation [19]. However, mixed-mode survey administration is not, in itself, a magic bullet and care still needs to be taken to avoid measurement (and other) errors that may affect the validity and reliability of the findings [132, 133].
In the absence of clear guidance on best practice in the administration of SHBV surveys in specific migrant populations, pre-testing and pilot testing are essential. Pre-testing will enable “the capabilities of the selected mode[s] of data collection” to be evaluated, while pilot testing can be used to estimate response rates and ascertain whether a proposed mode of administration is appropriate for meeting research objectives [134]. Where issues are identified through pre-testing and piloting, appropriate revisions should be made in line with relevant guidelines (e.g. the Guidelines for Best Practice in Cross-Cultural Surveys [135]).
Table 5. Advantages, disadvantages and considerations, by mode survey administration.
| Mode | Possible advantages | Possible disadvantages | Considerations and significance | |
|---|---|---|---|---|
| Self-completed | • Versions of the survey can be prepared in multiple languages • Allows for greater anonymity which can reduce social desirability response bias, especially when asking sensitive questions • Can be completed at participants’ own convenience and does not have to be completed in full in one sitting |
• Less control over manner in which survey is completed (e.g. missing data, external assistance) • Requires literacy (unless innovative audio-visual techniques used) • If delivered online/via device, requires access to technology and user proficiency |
Are instructions for completion clear? | If no, may result in response or non-response errors |
| Are measures in place to minimise number of missed questions? | If no, may result in item non-response error | |||
| Is the survey available in places that are convenient for / accessible to the target population? | If no, may result in sampling error | |||
| Are there sufficient resources to ensure the survey is translated in languages required to obtain a representative of the target population? | If no, may result in sampling error | |||
| Interviewer-led | • Can facilitate rapport- and trust-building • Enables greater control over the manner in which the survey is completed by participants Quality of responses is not dependent on participant literacy |
• Lack of anonymity may increase social desirability response bias, especially when asking sensitive questions • Requires participants to be present / available at the time the interviewers are able to collect data If delivered by telephone, requires eligible participants to have access Personnel costs May limit ability to collect data from places if interviewers need to travel long distances • Limited to languages spoken by interviewers |
Is the interview able to be offered at times that are convenient to the eligible population? | If no, may result in sampling error |
| Are the interviewers appropriately trained? | If no, may result in interviewer error or processing error | |||
| Are the characteristics of the available interviewers (e.g. gender) suitable given the characteristics of the participant and survey subject matter? | If no, may result in response error (social desirability), sampling error, interviewer error | |||
| Are the interviews able to be conducted/offered in a private place? | If no, may result in response error (social desirability bias), sampling error | |||
The main limitation of this scoping review is that it relied solely on information reported in the included studies. It is possible that a larger number of studies and data may have been included if authors had been approached to provide more information about the way in which their surveys were administered. Better reporting in the form of adherence to checklists such as STROBE [136] for observational studies and survey-specific guidelines (see Bennett, Khangura et al. [127]) will assist future researchers to undertake more comprehensive reviews into this subject area and facilitate their ability to produce rigorous meta-syntheses. Future reviews of survey research in migrant populations would also benefit from using appropriate tools to critically appraise the quality of included studies (e.g. checklists developed by the Joanna Briggs Institute or the Critical Appraisal Skills Program) [137, 138].
As Méndez and Font [139] note, “[t]he demand for more data about immigrants and ethnic minorities from national and supra-national bodies makes us confident that the number of surveys addressed to these populations will increase in the future.” The challenge for researchers is to ensure that future SHBBV surveys are designed with reference to, and with a view to building on, the evidence base about which mode of survey administration is best suited to collecting valid and reliable evidence about migrants’ knowledge, behaviours and practices. Additionally, other factors influencing quality should also be examined, including sampling methods, survey translation and instrument validation. Research in this area is particularly salient, given the World Health Organizations current project to develop a “standard, globally-recognized instrument to measure sexual practices, behaviours and sexual health related outcomes” [15] which would facilitate comparisons across populations.
Supporting information
(PDF)
(DOCX)
(DOCX)
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
AR, BM, RL, DV and MR received funding from the Australia Research Council: https://www.arc.gov.au/. Additional project funding was provided by the Department of Health Western Australia (https://ww2.health.wa.gov.au/), the Department of Health South Australia (https://www.sahealth.sa.gov.au/), the Department of Health and Human Services Victoria (https://www.sahealth.sa.gov.au/) and SHine SA (https://www.shinesa.org.au/) The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.UNAIDS. UNAIDS 2016–2021 Strategy: On the fast-track to end AIDS. Geneva: 2015. [Google Scholar]
- 2.Hernando V, Alvarez-del Arco D, Alejos B, Monge S, Amato-Gauci A, Noori T, et al. HIV infection in migrant populations in the European Union and European Economic Area in 2007–2012: an epidemic on the move. Journal of Acquired Immune Deficiency Syndrome. 2015;70(2):204–11. [DOI] [PubMed] [Google Scholar]
- 3.Gunaratnam P, Heywood A, McGregor S, Jamil MS, McManus H, Mao L, et al. HIV diagnoses in migrant populations in Australia—a changing epidemiology. PLoS ONE. 2019;14(2):e0212268 10.1371/journal.pone.0212268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prosser AT, Tang T, Hall H. HIV in persons born outside the United States, 2007–2010. Journal of the American Medical Association. 2012;308(6):601–7. 10.1001/jama.2012.9046 [DOI] [PubMed] [Google Scholar]
- 5.Suphanchaimat R, Sommanustweechai A, Khitdee C, Thaichinda C, Kantamaturapoj K, Leelahavarong P, et al. HIV/AIDS health care challenges for cross- country migrants in low- and middle-income countries: a scoping review. HIV/AIDS—Research and Palliative Care. 2014;6:19–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UNAIDS. The Gap Report. Geneva: 2014. [Google Scholar]
- 7.Agu J, Lobo R, Crawford G, Chigwada B. Migrant sexual health help-seeking and experiences of stigmatization and discrimination in Perth, Western Australia: exploring barriers and enablers. International Journal of Environmental Research and Public Health. 2016;13(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richters J, Badcock P, Simpson J, Shellard D, Rissel C, Visser Rd, et al. Design and methods of the second Australian study of health and relationships. Sexual Health. 2014;11:383–96. 10.1071/SH14115 [DOI] [PubMed] [Google Scholar]
- 9.Erens B, Phelps A, Clifton S, Mercer CH, Tanton C, Hussey D, et al. Methodology of the third British national survey of sexual attitudes and lifestyles (Natsal-3). 2014;90(2):84–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rogers W, Lange MM. Rethinking the vulnerability of minority populations in research. American Journal of Public Health. 2013;103(12):2141–6. 10.2105/AJPH.2012.301200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fakoya I, Álvarez-del Arco D, Monge S, Copas AJ, Gennotte A-F, Volny-Anne A, et al. Advancing migrant access to health services in Europe (AMASE): Protocol for a cross-sectional study. JMIR Research Protocols. 2016;5(2):e74 10.2196/resprot.5085 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bourne A, Reid D, Weatherburn P. African health and sex survey 2013–2014: headline findings. London: 2014. [Google Scholar]
- 13.McGregor S, Mlambo E, Gunaratnam P, Wilson D, Guy R. HIV knowledge, risk behaviour and testing: a community survey in people from culturally and linguistically diverse (CALD) backgrounds in NSW, Australia. Sydney: 2016. [Google Scholar]
- 14.World Health Organization. Seeking feedback to develop a population-representative sexual health survey instrument 2019 [Available from: https://www.who.int/news-room/detail/21-10-2019-seeking-feedback-to-develop-a-population-representative-sexual-health-survey-instrument].
- 15.World Health Organization. Seeking feedback to develop a population-representative sexual health survey instrument: An open call from the WHO—Additional information for participation 2019 [Available from: https://drive.google.com/file/d/1f33Eustjgoqq4cY34kknc9UMvw_NIP3c/view].
- 16.Bowling A. Mode of questionnaire administration can have serious effects on data quality. Journal of Public Health. 2005;27:281–91 10.1093/pubmed/fdi031 [DOI] [PubMed] [Google Scholar]
- 17.Caltabiano M, Dalla-Zuanna G. A comparison of survey techniques on sensitive sexual behavior in Italy. The Journal of Sex Research. 2013;50(6):537–47. 10.1080/00224499.2012.674573 [DOI] [PubMed] [Google Scholar]
- 18.De Jong J. Data collection: Self-administered surveys. In: Survey Research Center, editor. Guidelines for best practice in cross-cultural surveys. Ann Arbor: Survey Research Center 2016. p. 550–75. [Google Scholar]
- 19.European Asylum Support Office. A review of empirical surveys of asylum-related migrants. EASO; 2018. [Google Scholar]
- 20.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of Internal Medicine. 2018,169(7):467–473. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 21.Arksey H, O'Malley L. Scoping studies: towards a methdological framework International Journal of Social Research Methodology 2005;8(1):19–32. [Google Scholar]
- 22.Haddaway NR, Collins AM, Coughlin D, Kirk S. The role of Google Scholar in evidence reviews and its applicability to grey literature searching. PLOS ONE. 2015;10(9):e0138237 10.1371/journal.pone.0138237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. Journal of the Medical Library Association 2016;104(3):240–3. 10.3163/1536-5050.104.3.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine. 2009;6(7):e1000097-e. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Getrich CM, Broidy LM, Kleymann E, Helitzer DL, Kong AS, Sussman AL, et al. Different models of HPV vaccine decision-making among adolescent girls, parents, and health-care clinicians in New Mexico. Ethnicity and Health. 2014;19(1):47–63. 10.1080/13557858.2013.857767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duan S, Ding Y, Yang Y, Lu L, Sun J, Wang N, et al. Prevalence and correlates of HIV discordance and concordance among Chinese-Burmese mixed couples in the Dehong prefecture of Yunnan province, China. Sexual Health. 2012;9(5):481–7. 10.1071/SH12065 [DOI] [PubMed] [Google Scholar]
- 27.Agbemenu K, Terry MA, Hannan M, Kitutu J, Doswell W. Attitudes and beliefs of African immigrant mothers living in the US towards providing comprehensive sex education to daughters aged 12–17 Years: a Pilot Study. Journal of Immigrant Minority Health. 2016;18:1053–9. 10.1007/s10903-015-0292-z [DOI] [PubMed] [Google Scholar]
- 28.Ahmed M. Determinants of condom use and HIV prevention among East African immigrants in Minnesota. PhD [dissertation]. El Paso: University of Texas; 2013.
- 29.Alber JM, Cohen C, Nguyen GT, Ghazvini SF, Tolentino BT. Exploring communication strategies for promoting hepatitis B prevention among young Asian American adults. Journal of Health Communication. 2018;23(12):977–83. 10.1080/10810730.2018.1534904 [DOI] [PubMed] [Google Scholar]
- 30.Alvarez-del Arco D, Fakoya I, Thomadakis C, Pantazis N, Touloumi G, Gennotte AF, et al. High levels of postmigration HIV acquisition within nine European countries. AIDS. 2017;31(14):1979–88. 10.1097/QAD.0000000000001571 [DOI] [PubMed] [Google Scholar]
- 31.Amadi RN. Perceptions, attitudes, and acceptability of HIV testing among sub-Saharan African immigrants in Chicago. PhD [dissertation]. Chicago: Loyola University; 2012.
- 32.Arevalo IA. The influence of discrimination, substance use, acculturation, and mental health on HIV-related sexual behaviors: The case of immigrant Latino men who have sex with men. PhD [dissertation]. Washington DC: Howard University; 2016.
- 33.Asante A, Körner H, McMahon T, Sabri We, Kippax S. Periodic survey of HIV knowledge and use of health services among people from culturally and linguistically diverse backgrounds, 2006–2008. Sydney: National Centre in HIV Social Research, 2009. [Google Scholar]
- 34.Bastani R, Glenn BA, Maxwell AE, Jo AM, Herrmann AK, Crespi CM, et al. Cluster-randomized trial to increase hepatitis B testing among Koreans in Los Angeles. Cancer Epidemiology Biomarkers and Prevention. 2015;24(9):1341–9. 10.1158/1055-9965.EPI-14-1396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beltran R, Simms T, Lee HY, Kwon M. HPV literacy and associated factors among Hmong American immigrants: Implications for reducing cervical cancer disparity. Journal of Community Health. 2016;41(3):603–11. 10.1007/s10900-015-0135-9 [DOI] [PubMed] [Google Scholar]
- 36.Burns F, Fenton K, Morison L, Mercer C, Erens B, Field J, et al. Factors associated with HIV testing among black Africans in Britain. Sexually Transmitted Infections. 2005;81:494–500. 10.1136/sti.2004.013755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chamratrithirong A, Boonchalaksi W, Yampeka P. Prevention of HIV/AIDS among migrant workers in Thailand (PHAMIT): The baseline survey 2004. Salaya: Mahidol University, 2005. [Google Scholar]
- 38.Chen WT, Guthrie B, Shiu CS, Wang L, Weng Z, Li CS, et al. Revising the American dream: how Asian immigrants adjust after an HIV diagnosis. Journal of Advanced Nursing. 2015;71(8):1914–25. 10.1111/jan.12645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cohen CA. Chronic HBV infection and community-based services for high-risk Asians and Pacific Islanders. PhD [dissertation]. Philadelphia: Drexel University; 2015.
- 40.Coronado GD, Taylor VM, Tu SP, Yasui Y, Acorda E, Woodall E, et al. Correlates of hepatitis B testing among Chinese Americans. Journal of Community Health. 2007;32(6):379–90. 10.1007/s10900-007-9060-x [DOI] [PubMed] [Google Scholar]
- 41.Dean J, Mitchell M, Stewart D, Debattista J. Sexual health knowledge and behaviour of young Sudanese Queenslanders: a cross-sectional study. Sexual Health. 2017;14(3):254–60. 10.1071/SH16171 [DOI] [PubMed] [Google Scholar]
- 42.Delgado M, Lundgren LM, Deshpande A, Lonsdale J, Purington T. The association between acculturation and needle sharing among Puerto Rican injection drug users. Evaluation and Program Planning. 2008;31(1):83–91. 10.1016/j.evalprogplan.2007.05.010 [DOI] [PubMed] [Google Scholar]
- 43.Demeke HB. Relationships between HIV-related stigma, coping, social support and health-related quality of life in people living with HIV/AIDS. PhD [dissertation]. Atlanta: Emory University; 2013.
- 44.Dennis AM, Wheeler JB, Valera E, Hightow-Weidman L, Napravnik S, Swygard H, et al. HIV risk behaviors and sociodemographic features of HIV-infected Latinos residing in a new Latino settlement area in the Southeastern United States. AIDS Care. 2013;25(10):1298–307. 10.1080/09540121.2013.764964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dias S, Gama A, Severo M, Barros H. Factors associated with HIV testing among immigrants in Portugal. International Journal of Public Health. 2011;56(5):559–66. 10.1007/s00038-010-0215-7 [DOI] [PubMed] [Google Scholar]
- 46.Elford J, Doerner R, McKeown E, Nelson S, Anderson J, Low N. HIV infection among ethnic minority and migrant men who have sex with men in Britain. Sexually Transmitted Diseases. 2012;39(9):678–86. 10.1097/OLQ.0b013e31825c8018 [DOI] [PubMed] [Google Scholar]
- 47.Elford J, McKeown E, Doerner R, Nelson S, Low N, Anderson J. Sexual health of ethnic minority MSM in Britain (MESH project): design and methods. BMC Public Health. 2010;10:419 10.1186/1471-2458-10-419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Evans AR, Hart GJ, Mole R, Mercer CH, Parutis V, Gerry CJ, et al. Central and east European migrant men who have sex with men: an exploration of sexual risk in the U.K. Sexually Transmitted Infections. 2011;87(4):325–30. 10.1136/sti.2010.046409 [DOI] [PubMed] [Google Scholar]
- 49.Evans C, Suggs LS, Turner K, Occa A, Juma A, Blake H. Mobile phone messaging to promote uptake of HIV testing among migrant African communities in the UK. Health Education Journal. 2019;78(1):24–37. 10.1177/0017896918785928 [DOI] [Google Scholar]
- 50.Fakoya I, Alvarez-Del Arco D, Copas AJ, Teixeira B, Block K, Gennotte AF, et al. Factors associated with access to HIV testing and primary care among migrants living in Europe: cross-dectional survey. JMIR Public Health and Surveillance. 2017;3(4):e84 10.2196/publichealth.7741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fenton KA, Chinouya M, Davidson O, Copas A. HIV testing and high risk sexual behaviour among London’s migrant African communities: a participatory research study. Sexually Transmitted Infections. 2002;78:241–5. 10.1136/sti.78.4.241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fernandez-Esquer ME, Atkinson J, Diamond P, Useche B, Mendiola R. Condom use self-efficacy among U.S. and foreign-born Latinos in Texas. Journal of Sex Research. 2004;41(4):390–9. 10.1080/00224490409552246 [DOI] [PubMed] [Google Scholar]
- 53.Fitzgerald K, Chakraborty J, Shah T, Khuder S, J. D. HIV/AIDS knowledge among female migrant farm workers in the Midwest. Journal of Immigrant Health 2003;5:29–36. 10.1023/a:1021000228911 [DOI] [PubMed] [Google Scholar]
- 54.Ford K, Chamrathrithirong A. Sexual partners and condom use of migrant workers in Thailand. AIDS and Behavior. 2007;11(6):905–14. 10.1007/s10461-007-9207-x [DOI] [PubMed] [Google Scholar]
- 55.Foster R, McCormack L, Thng C, Wand H, McNulty A. Cross-sectional survey of Chinese-speaking and Thai-speaking female sex workers in Sydney, Australia: factors associated with consistent condom use. Sexual Health. 2018;15(5):389–95. 10.1071/SH17205 [DOI] [PubMed] [Google Scholar]
- 56.Getrich CM, Broidy LM, Kleymann E, Helitzer DL, Kong AS, Sussman AL. Different models of HPV vaccine decision-making among adolescent girls, parents, and health-care clinicians in New Mexico. Ethnicity and Health. 2014;19(1):47–63. 10.1080/13557858.2013.857767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Goldade K, Nichter MA. Risk perceptions and knowledge of sexually transmitted infections (STIs) and HIV among undocumented Nicaraguan migrant women in Costa Rica. Annals of Anthropological Practice. 2010;34(1):195–212. 10.1111/j.1556-4797.2010.01059.x [DOI] [Google Scholar]
- 58.Gray C, Crawford G, Reid A, Lobo R. HIV knowledge and use of health services among people from South-East Asia and sub-Saharan Africa living in Western Australia. Health Promotion Journal of Australia. 2018;29(3):274–81. 10.1002/hpja.168 [DOI] [PubMed] [Google Scholar]
- 59.Grieb SMD, Flores-Miller A, Page KR. Solo Se Vive Una Vez! (You Only Live Once): A pilot evaluation of individually tailored video modules aiming to increase HIV testing among foreign-born Latino men. Journal of Acquired Immune Deficiency Syndromes. 2017;74:S104–S12. 10.1097/QAI.0000000000001239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hamdiui N, Stein M, Timen A, Timmermans D, Wong A, van den Muijsenbergh M, et al. Hepatitis B in Moroccan-Dutch: a quantitative study into determinants of screening participation. BMC Medicine. 2018;16(1):47 10.1186/s12916-018-1034-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hislop TG, Teh C, Low A, Li L, Tu SP, Yasui Y, et al. Hepatitis B knowledge, testing and vaccination levels in Chinese immigrants to British Columbia, Canada. Canadian Journal of Public Health 2007;98(2):125–9. 10.1007/BF03404323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hwang JP, Huang CH, Yi JK. Knowledge about hepatitis B and predictors of hepatitis B vaccination among Vietnamese American college students. Journal of American College Health. 2008;56(4):377–82. 10.3200/JACH.56.44.377-382 [DOI] [PubMed] [Google Scholar]
- 63.Jenkins CN, McPhee SJ, Wong C, Nguyen T, Euler GL. Hepatitis B immunization coverage among Vietnamese-American children 3 to 18 years old. Pediatrics. 2000;106(6):E78 10.1542/peds.106.6.e78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Johnston LG. Regional migrant health survey on tuberculosis and HIV and health service response for migrants in Armenia, Azerbaijan and Georgia. Switzerland: 2019. [Google Scholar]
- 65.Joseph NP, Belizaire M, Porter CL, Walsh JP, Esang M, Goff G, et al. Ethnic differences in perceived benefits and barriers to HPV vaccine acceptance: a qualitative analysis of young African American, Haitian, Caucasian, and Latino men. Clinical Pediatrics. 2014;53(2):177–85. 10.1177/0009922813515944 [DOI] [PubMed] [Google Scholar]
- 66.Juon HS, Strong C, Kim F, Park E, Lee S. Lay health worker intervention improved compliance with hepatitis B vaccination in Asian Americans: randomized controlled trial. PLoS ONE. 2016;11(9):e0162683 10.1371/journal.pone.0162683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Juon HS, Lee S, Strong C, Rimal R, Kirk GD, Bowie J. Effect of a liver cancer education program on hepatitis B screening among Asian Americans in the Baltimore-Washington metropolitan area, 2009–2010. Preventing Chronic Disease. 2014;11:130258 10.5888/pcd11.130258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kara RG. Predicting HIV testing intention among recent African immigrants. PhD [dissertation]. Minneapolis: Walden University; 2012.
- 69.Kuehne A, Koschollek C, Santos-Hövener C, Thorlie A, Müllerschön J, Tshibadi CM, et al. Impact of HIV knowledge and stigma on the uptake of HIV testing–Results from a community-based participatory research survey among migrants from sub-Saharan Africa in Germany. PLoS ONE. 2018;13(4):1–19. 10.1371/journal.pone.0194244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Leite L, Buresh M, Rios N, Conley A, Flys T, Page KR. Cell phone utilization among foreign-born Latinos: a promising tool for dissemination of health and HIV information. Journal of Immigrant & Minority Health. 2014;16(4):661–9. 10.1007/s10903-013-9792-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lessard D, Lebouche B, Engler K, Thomas R, Machouf N. Explaining the appeal for immigrant men who have sex with men of a community-based rapid HIV-testing site in Montreal (Actuel sur Rue). AIDS Care. 2015;27(9):1098–103. 10.1080/09540121.2015.1028880 [DOI] [PubMed] [Google Scholar]
- 72.Lin P, Simoni JM, Zemon V. The health belief model, sexual behaviors, and HIV risk among Taiwanese immigrants. AIDS Education and Prevention. 2005;17(5):469–83. 10.1521/aeap.2005.17.5.469 [DOI] [PubMed] [Google Scholar]
- 73.Lofters AK, Vahabi M, Fardad M, Raza A. Exploring the acceptability of human papillomavirus self-sampling among Muslim immigrant women. Cancer Management and Research. 2017;9:323–9. 10.2147/CMAR.S139945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Loos J, Manirankunda L, Platteau T, Albers L, Fransen K, Vermoesen T, et al. Acceptability of a community-based outreach HIV-testing intervention using oral fluid collection devices and web-based HIV test result collection among sub-Saharan African migrants: A mixed-method study. JMIR Public Health and Surveillance. 2016;2(2):e33 10.2196/publichealth.5519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Manoyos V, Tangmunkongvorakul A, Srithanaviboonchai K, Yangyuenkul S, Grimes RM. Sexual risk-behaviors for HIV infections among young cross-border migrant workers living in urban Chiang Mai, Thailand. Journal of Health Research. 2016;30(5):347–53. 10.14456/jhr.2016.47 [DOI] [Google Scholar]
- 76.Maxwell AE, Bastani R, Warda US. Pilot test of a single-session AIDS workshop for young Hispanic U.S. immigrants. Journal of Immigrant Health. 2002;4(2):73–9. 10.1023/A:1014594408471 [DOI] [PubMed] [Google Scholar]
- 77.Miller J, Guarnaccia P, Fasina A. AIDS knowledge among Latinos: the roles of language, culture, and socioeconomic status. Journal of Immigrant Health,. 2002;4:63–72. 10.1023/A:1014542324401 [DOI] [PubMed] [Google Scholar]
- 78.Montealegre JR. Prevalence of HIV risk-related behaviors among undocumented Central American immigrant women in Houston, Texas, 2010. PhD [dissertation]. Texas: University of Texas; 2011.
- 79.Montealegre J, Risser J, Selwyn B, McCurdy S, Sabin K. Effectiveness of respondent driven sampling to recruit undocumented Central American immigrant women in Houston, Texas for an HIV behavioral survey. AIDS and Behavior. 2013;17(2):719–27. 10.1007/s10461-012-0306-y [DOI] [PubMed] [Google Scholar]
- 80.O'Connor CC, Shaw M, Wen LM, Quine S. Low knowledge and high infection rates of hepatitis in Vietnamese men in Sydney. Sexual Health. 2008;5(3):299–302. 10.1071/sh07084 [DOI] [PubMed] [Google Scholar]
- 81.Ogungbade G. Social capital variables as predictors of HIV risk-taking behaviors among sub-Saharan African immigrants in the United States. PhD [dissertation]. Minneapolis: Walden University; 2010.
- 82.Organista K, Kubo A. Pilot survey of HIV risk and contextual problems and issues in Mexican/Latino migrant day laborers. Journal of Immigrant and Minority Health. 2005;7(4):269–81. 10.1007/s10903-005-5124-0 [DOI] [PubMed] [Google Scholar]
- 83.Pannetier J, Ravalihasy A, Lydié N, Lert F, Desgrées Du Loû A. Prevalence and circumstances of forced sex and post-migration HIV acquisition in sub-Saharan African migrant women in France: an analysis of the ANRS-PARCOURS retrospective population-based study. The Lancet Public Health. 2018;3(1):e16–e23. 10.1016/S2468-2667(17)30211-6 [DOI] [PubMed] [Google Scholar]
- 84.Platt L, Grenfell P, Bonell C, Creighton S, Wellings K, Parry J, et al. Risk of sexually transmitted infections and violence among indoor-working female sex workers in London: the effect of migration from Eastern Europe. Sexually Transmitted Infections. 2011;87(5):377–84. 10.1136/sti.2011.049544 [DOI] [PubMed] [Google Scholar]
- 85.Plewes K, Lee T, Kajeechewa L, Thwin MM, Lee SJ, Carrara VI, et al. Low seroprevalence of HIV and syphilis in pregnant women in refugee camps on the Thai-Burma border. International Journal of STD and AIDS. 2008;19(12):833–7. 10.1258/ijsa.2008.008034 [DOI] [PubMed] [Google Scholar]
- 86.Ramanathan V, Sitharthan G. Safe sex practices of Indian immigrant men living in Australia: an exploratory research. Indian Journal of Public Health. 2014;58(4):274–7. 10.4103/0019-557X.146295 [DOI] [PubMed] [Google Scholar]
- 87.Rangel MG, Martinez-Donate AP, Hovell MF, Santibanez J, Sipan CL, Izazola-Licea JA. Prevalence of risk factors for HIV infection among Mexican migrants and immigrants: Probability survey in the north border of Mexico. Salud Publica De Mexico. 2006;48(1):3–12. 10.1590/s0036-36342006000100003 [DOI] [PubMed] [Google Scholar]
- 88.Saenz CD. Health risks and health-seeking behaviors of migrant and seasonal farmworkers on the US-Mexico border. PhD [dissertation]. Texas: University of Texas; 2010.
- 89.Salabarria-Pena Y, Lee JW, Montgomery SB, Hopp HW, Muralles AA. Determinants of female and male condom use among immigrant women of Central American descent. AIDS and Behavior. 2003;7(2):163–74. 10.1023/a:1023998308892 [DOI] [PubMed] [Google Scholar]
- 90.Salehi R. Indicators of access to sexual health services for Toronto newcomer youth. PhD [dissertation]. Canada: York University; 2011.
- 91.Santos-Hovener C, Marcus U, Koschollek C, Oudini H, Wiebe M, Ouedraogo OI, et al. Determinants of HIV, viral hepatitis and STI prevention needs among African migrants in Germany: a cross-sectional survey on knowledge, attitudes, behaviors and practices. BMC Public Health. 2015;15:753 10.1186/s12889-015-2098-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Selvey LA, Lobo RC, McCausland KL, Donovan B, Bates J, Hallett J. Challenges facing Asian sex workers in Western Australia: implications for health promotion and support services. Frontiers in Public Health. 2018;6:171 10.3389/fpubh.2018.00171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Shiau R, Bove F, Henne J, Zola J, Fang T, Fernyak S. Using survey results regarding hepatitis B knowledge, community awareness and testing behavior among Asians to improve the San Francisco hep B free campaign. Journal of Community Health. 2012;37(2):350–64. 10.1007/s10900-011-9452-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Şimşek Z, Yentur Doni N, Gül Hilali N, Yildirimkaya G. A community-based survey on Syrian refugee women's health and its predictors in Şanliurfa, Turkey. Women and Health. 2018;58(6):617–31. 10.1080/03630242.2017.1321609 [DOI] [PubMed] [Google Scholar]
- 95.Spadafino JT, Martinez O, Levine EC, Dodge B, Munoz-Laboy M, Fernandez MI. Correlates of HIV and STI testing among Latino men who have sex with men in New York City. AIDS Care. 2016;28(6):695–8. 10.1080/09540121.2016.1147017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Srithanaviboonchai K, Choi K, van Griensven F, Hudes E, Visaruratana S, Mandel J. HIV-1 in ethnic Shan migrant workers in northern Thailand. AIDS. 2002;16(1):929–31. [DOI] [PubMed] [Google Scholar]
- 97.Stromdahl S, Liljeros F, Thorson AE, Persson KI, Forsberg BC. HIV testing and prevention among foreign-born men who have sex with men: an online survey from Sweden. BMC Public Health. 2017;17(1):139 10.1186/s12889-016-3992-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sumari-de Boer IM, Sprangers MA, Prins JM, Nieuwkerk PT. HIV stigma and depressive symptoms are related to adherence and virological response to antiretroviral treatment among immigrant and indigenous HIV infected patients. AIDS and Behavior. 2012;16(6):1681–9. 10.1007/s10461-011-0112-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Taylor VM, Jackson JC, Pineda M, Pham P, Fischer M, Yasui Y. Hepatitis B knowledge among Vietnamese immigrants: implications for prevention of hepatocellular carcinoma. Journal of Cancer Education. 2000;15(1):51–5. 10.1080/08858190009528654 [DOI] [PubMed] [Google Scholar]
- 100.Taylor VM, Jackson JC, Chan N, Kuniyuki A, Yasui Y. Hepatitis B knowledge and practices among Cambodian American women in Seattle, Washington. Journal of Community Health. 2002;27(3):151–63. 10.1023/a:1015229405765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Taylor VM, Choe JH, Yasui Y, Li L, Burke N, Jackson JC. Hepatitis B awareness, testing, and knowledge among Vietnamese American men and women. Journal of Community Health. 2005;30(6):477–90. 10.1007/s10900-005-7282-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Taylor VM, Tu SP, Woodall E, Acorda E, Chen H, Choe J, et al. Hepatitis B knowledge and practices among Chinese immigrants to the United States. Asian Pacific Journal of Cancer Prevention. 2006;7(2):313–7. [PubMed] [Google Scholar]
- 103.Taylor VM, Seng P, Acorda E, Sawn L, Li L. Hepatitis B knowledge and practices among Cambodian immigrants. Journal of Cancer Education. 2009;24(2):100–4. 10.1080/08858190802664750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Thompson MJ, Taylor VM, Jackson JC, Yasui Y, Kuniyuki A, Tu SP, et al. Hepatitis B knowledge and practices among Chinese American women in Seattle, Washington. Journal of Cancer Education. 2002;17(4):222–6. 10.1080/08858190209528842 [DOI] [PubMed] [Google Scholar]
- 105.Tu RS, Li L, Tsai JH, Yip MP, Terasaki G, Teh C, et al. A cross-border comparison of hepatitis B testing among Chinese residing in Canada and the United States. Asian Pacific Journal of Cancer Prevention. 2009;10(3):483–90. [PMC free article] [PubMed] [Google Scholar]
- 106.UNHCR. HIV and AIDS behavioral surveillance survey (BSS) refugee camps and hosting communities in Kawambwa and Mporokoso, Zambia. Zambia: 2006.
- 107.UNHCR. Behavioural Surveillance Surveys among refugees and surrounding host population: Kakuma, Kenya. 2004.
- 108.Uribe CL, Darrow WW, Villanueva LP, Obiaja KC, Sanchez-Brana E, Gladwin H. Identifying HIV risk-reduction strategies for Hispanic populations in Broward County. Annals of Epidemiology. 2009;19(8):567–74. 10.1016/j.annepidem.2009.04.006 [DOI] [PubMed] [Google Scholar]
- 109.Van der Veen YJJ, Voeten H, de Zwart O, Richardus JH. Awareness, knowledge and self-reported test rates regarding hepatitis B in Turkish-Dutch: a survey. BMC Public Health. 2010;10:7 10.1186/1471-2458-10-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Viadro CI, Earp JA. The sexual behavior of married Mexican immigrant men in North Carolina. Social Science and Medicine. 2000;50(5):723–35. 10.1016/s0277-9536(99)00305-6 [DOI] [PubMed] [Google Scholar]
- 111.Villarreal KM, Wiley DC, Housman J, Martinez-Ramos G. Attitudes about partner communication regarding contraceptive use among Hispanic male college students. Journal of American College Health. 2016;64(4):279–87. 10.1080/07448481.2015.1117467 [DOI] [PubMed] [Google Scholar]
- 112.Westmaas AH, Kok G, Vriens P, Gotz H, Richardus JH, Voeten H. Determinants of intention to get tested for STI/HIV among the Surinamese and Antilleans in the Netherlands: results of an online survey. BMC Public Health. 2012;12:961 10.1186/1471-2458-12-961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Yau AHL, Ford JA, Kwan PWC, Chan J, Choo Q, Lee TK, et al. Hepatitis B awareness and knowledge in Asian communities in British Columbia. Canadian Journal of Gastroenterology and Hepatology. 2016:8 10.1155/2016/4278724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zellner JA, Martínez-Donate AP, Sañudo F, Fernández-Cerdeño A, Sipan CL, Hovell MF, et al. The interaction of sexual identity with sexual behavior and its influence on HIV risk among Latino men: results of a community survey in northern San Diego County, California. American Journal of Public Health. 2009;99(1):125–32. 10.2105/AJPH.2007.129809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zhussupov B, McNutt LA, Gilbert L, Terlikbayeva A, El-Bassel N. Migrant workers in Kazakhstan: gender differences in HIV knowledge and sexual risk behaviors. AIDS and Behavior. 2015;19(7):1298–304. 10.1007/s10461-014-0914-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gerbert B, Bronstone A, McPhee S, Pantilat S, Allerton M. Development and testing of an HIV-risk screening instrument for use in health care settings. American Journal of Preventive Medicine. 1998;15(2):103–13. 10.1016/s0749-3797(98)00025-7 [DOI] [PubMed] [Google Scholar]
- 117.Lux KM, Petosa R. Preventing HIV infection among juvenile delinquents: educational diagnosis using the health belief model. International Quarterly of Community Health Education. 1994;15(2):145–64. 10.2190/WTBA-HVC1-R16N-RRT5 [DOI] [PubMed] [Google Scholar]
- 118.Zagumny MJ, Brady DB. Development of the AIDS Health Belief Scale (AHBS). AIDS Education and Prevention. 1998;10(2):173–9. [PubMed] [Google Scholar]
- 119.Smith A, Agius P, Dyson SM, A, Pitts M. Secondary students and sexual health 2002: Results of the 3rd national survey of Australian secondary students HIV/AIDS and sexual health. Melbourne: Australian Research Centre in Sex, Health and Society, 2003. [Google Scholar]
- 120.Marín BV, Gómez CA, Tschann JM, Gregorich SE. Condom use in unmarried Latino men: a test of cultural constructs. Health Psychology. 1997;16(5):458–67. 10.1037//0278-6133.16.5.458 [DOI] [PubMed] [Google Scholar]
- 121.Marín BV, Tschann JM, Gómez CA, Gregorich S. Self-efficacy to use condoms in unmarried Latino adults. American Journal of Community Psychology. 1998;26(1):53–71. 10.1023/a:1021882107615 [DOI] [PubMed] [Google Scholar]
- 122.Dodds C, Hickson F, Weatherburn P, Reid D, Hammond G, Jessup K, et al. BASS Line 2007 survey: Assessing the sexual HIV prevention needs of African people in England. London: London School of Hygiene and Tropical Medicine, 2008. [Google Scholar]
- 123.World Health Organization. Behavioral surveillance surveys (BSS) [Available from: https://www.who.int/hiv/strategic/pubbss/en/].
- 124.National Archive of Computerized Data on Aging. National health interview survey series 2020. [Available from: https://www.icpsr.umich.edu/web/NACDA/series/40].
- 125.Kelley K, Clark B, Brown V, Sitzia J. Good practice in the conduct and reporting of survey research. International Journal for Quality in Health Care. 2003;15(3):261–6. 10.1093/intqhc/mzg031 [DOI] [PubMed] [Google Scholar]
- 126.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLOS Medicine. 2007;4(10):e297 10.1371/journal.pmed.0040297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bennett C, Khangura S, Brehaut JC, Graham ID, Moher D, Potter BK, et al. Reporting guidelines for survey research: an analysis of published guidance and reporting practices. PLOS Medicine. 2011;8(8):e1001069 10.1371/journal.pmed.1001069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Draucker CB, Martsolf DS, Poole C. Developing distress protocols for research on sensitive topics. Archives of Psychiatric Nursing. 2009;23(5):343–50. 10.1016/j.apnu.2008.10.008 [DOI] [PubMed] [Google Scholar]
- 129.Groves RM. Three eras of survey research. Public Opinion Quarterly. 2011;75(5):861–71. 10.1093/poq/nfr057 [DOI] [Google Scholar]
- 130.Smyth J, Pearson J. Internet survey methods: a review of strengths, weaknesses, and innovation In: Das M, Ester P, Kaczmirek L, editors. Social and behavioral research and the internet: advances in applied methods and research strategies. New York: Routledge; 2011. p. 11–44. [Google Scholar]
- 131.Poynton TA, DeFouw ER, Morizio LJ. A systematic review of online response rates in four counseling journals. Journal of Counseling and Development. 2019;97(1):33–42. 10.1002/jcad.12233 [DOI] [Google Scholar]
- 132.Martin P. A good mix? Mixed mode data collection and cross-national surveys. ASK Research and Methods. 2011;20(1):5–26. [Google Scholar]
- 133.De Leeuw E. To mix or not to mix data collection modes in surveys. Journal of Official Statistics. 2005;21(2):233–55. [Google Scholar]
- 134.Caspar R, Peytcheva E, Yan T, Lee S, Liw M, Hu M. Pretesting In: Centre for Social Research, editor. Guidelines for best-practice in cross-cultural surveys. Ann Arbor: Survey Research Centre; 2016. [Google Scholar]
- 135.Survey Research Center. Guidelines for best practice in cross-cultural surveys. Ann Arbor: 2016. [Google Scholar]
- 136.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS medicine. 2007;4(10):e296 10.1371/journal.pmed.0040296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Joanna Briggs Institute. Critical Appraisal Tools 2017. [Available from: https://joannabriggs.org/ebp/critical_appraisal_tools].
- 138.CASP UK. CASP Checklists 2020. [Available from: https://casp-uk.net/casp-tools-checklists/].
- 139.Méndez M, Font J. Surveying immigrant populations: Methodological strategies, good practices and open questions In: Méndez M, Font J, editors. surveying ethnic minorities and immigrant populations. Methodological challenges and research strategies: Amsterdam University Press; 2013. p. 271–90. [Google Scholar]