Abstract
Background
School closures have occurred globally during the COVID-19 pandemic. However, empiric data on transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) among children and in educational settings are scarce. In Australia, most schools have remained open during the first epidemic wave, albeit with reduced student physical attendance at the epidemic peak. We examined SARS-CoV-2 transmission among children and staff in schools and early childhood education and care (ECEC) settings in the Australian state of New South Wales (NSW).
Methods
Laboratory-confirmed paediatric (aged ≤18 years) and adult COVID-19 cases who attended a school or ECEC setting while considered infectious (defined as 24 h before symptom onset based on national guidelines during the study period) in NSW from Jan 25 to April 10, 2020, were investigated for onward transmission. All identified school and ECEC settings close contacts were required to home quarantine for 14 days, and were monitored and offered SARS-CoV-2 nucleic acid testing if symptomatic. Enhanced investigations in selected educational settings included nucleic acid testing and SARS-CoV-2 antibody testing in symptomatic and asymptomatic contacts. Secondary attack rates were calculated and compared with state-wide COVID-19 rates.
Findings
15 schools and ten ECEC settings had children (n=12) or adults (n=15) attend while infectious, with 1448 contacts monitored. Of these, 633 (43·7%) of 1448 had nucleic acid testing, or antibody testing, or both, with 18 secondary cases identified (attack rate 1·2%). Five secondary cases (three children; two adults) were identified (attack rate 0·5%; 5/914) in three schools. No secondary transmission occurred in nine of ten ECEC settings among 497 contacts. However, one outbreak in an ECEC setting involved transmission to six adults and seven children (attack rate 35·1%; 13/37). Across all settings, five (28·0%) of 18 secondary infections were asymptomatic (three infants [all aged 1 year], one adolescent [age 15 years], and one adult).
Interpretation
SARS-CoV-2 transmission rates were low in NSW educational settings during the first COVID-19 epidemic wave, consistent with mild infrequent disease in the 1·8 million child population. With effective case-contact testing and epidemic management strategies and associated small numbers of attendances while infected, children and teachers did not contribute significantly to COVID-19 transmission via attendance in educational settings. These findings could be used to inform modelling and public health policy regarding school closures during the COVID-19 pandemic.
Funding
NSW Government Department of Health.
Introduction
The global COVID-19 pandemic has been addressed through implementation of aggressive public health measures focused on restricting mobility and ensuring physical distancing. Most countries have enforced school closures to mitigate transmission.1 However, evidence suggests that COVID-19 is less prevalent in children and generally causes milder illness, when compared with adults.2, 3, 4, 5, 6 The extent to which children are asymptomatically infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and what role they have in virus transmission, particularly in schools, remains unclear. It appears children are less likely to be the primary infection source in household clusters, compared with adults.7, 8
School closures might be effective in controlling pandemic influenza because children are important in transmission, and have high hospitalisation rates and severe outcomes from influenza.9, 10 However, school closures have significant social and economic impacts on children and families, with widespread implications for national and global economies.11 Although past experiences of school closures might inform expectations of social and economic impacts, modelled effects of school closures have varied depending on the assumptions regarding children's role in SARS-CoV-2 transmission.12 In China, schools were already closed for school holidays and remained so for a number of months,13 and, to date, data on COVID-19 from school or childcare settings are scarce.14, 15, 16
Australian strategies to delay and reduce the impact of COVID-19 following the first case in a traveller from Wuhan, China, on Jan 25, 2020, included thorough incoming traveller and community surveillance, high testing rates, rapid case isolation and contact tracing, and border closures and quarantine.17 Major changes in population behaviour and a low infection rate have ensued.17 Consistent with national policy, most of Australia's eight states and territories, including the most populous state New South Wales (NSW), kept schools open during the pandemic.18 In NSW, guidance for physical distancing, hygiene measures, and educational facility cleaning was issued. At the epidemic peak on March 23, 2020, distance (online) learning was implemented, and physical attendance recommended to be limited to children who needed to attend in person (eg, children of health-care workers or those without other care options).18 Early childhood education and care (ECEC) settings for children aged 6 weeks to 5 years remained open.
Research in context.
Evidence before this study
Data on COVID-19 in schools are scarce, particularly given many schools have been closed in response to the pandemic. We searched PubMed and medRxiv on June 5, 2020, for studies published from Jan 1, 2020, reporting transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in educational settings since the start of the outbreak in China, using the search terms COVID-19, SARS-CoV-2, transmission, schools, and children, as well as manually searching the references used in other relevant papers. Terms were searched individually and in combination as necessary, and no language restrictions were used. We identified some studies that included mention of student cases as part of a larger outbreak. We identified one article that detailed transmission in a school setting in Ireland in children aged 10 years and older; however, this study had few participants, a short study period (10 days), no data on testing rates, or serological testing in follow-up.
Added value of this study
We examined SARS-CoV-2 transmission among children and adults in 25 educational settings (primary and secondary schools, and early childhood education and care settings) together with the rate and characteristics of all paediatric COVID-19 cases in the Australian state of New South Wales over a 3-month period. We found a low incidence of attendance of children and staff members with COVID-19 at educational facilities, and low rates of SARS-CoV-2 transmission in the 15 schools and childcare settings where a case occurred. The exception was an outbreak in a childcare centre. The use of enhanced surveillance and serological testing of close contacts within the educational setting enabled detection of a small number of asymptomatic SARS-CoV-2 secondary infections in schools and the childcare setting.
Implications of all the available evidence
This is the first comprehensive population-based assessment of SARS-CoV-2 transmission among children and adults in educational facilities. Our results show that where effective case-contact testing and epidemic control strategies exist for the population, children and teachers did not contribute significantly to COVID-19 transmission via attendance in educational settings. This study will assist modellers, policy makers, health-care providers, and the public to understand the risk of COVID-19 occurring in educational facilities and help in decision making around school closures and reopenings. Our data also provide insights that can assist in comparing the economic and community costs of school closures against the potential benefits of reduced virus transmission.
This study aimed to prospectively examine SARS-CoV-2 transmission among children and adults in educational settings and to provide real-time evidence for decision making on school-based policies related to COVID-19. We secondarily aimed to examine the rate and characteristics of NSW paediatric COVID-19 cases in both educational settings and the wider population.
Methods
Study setting
This study was done in NSW, Australia, population 8·1 million, of which 1·8 million residents (23·0%) are aged 18 years or younger.19 Among laboratory-confirmed COVID-19 cases in NSW, we identified all children (aged ≤18 years) and staff who attended school or ECEC settings while considered infectious (defined as 24 h before symptom onset based on national guidelines during the study period20). All NSW schools (n=3103; public, independent, and Catholic) providing either primary (ages approximately 5–12 years), or secondary school education (ages approximately 13–18 years), or both, and any ECEC setting (approximately n=4600; ages approximately 6 weeks to 5 years) were eligible for inclusion. The estimated numbers of school staff and enrolled students state wide for 2020 were 143 084 and 1 232 367, respectively. Estimates of numbers of ECEC setting staffing and enrolment were not available.
The study period for index case identification was from Jan 25 (first NSW COVID-19 case notification) to April 9, 2020 (when the 10-week school term 1 ended and scheduled holidays commenced). From March 22, 2020, children were encouraged to stay home for distance learning until term 1 end; however, schools remained open if home schooling was not an option. The follow-up period for close contacts of COVID-19 cases extended to May 1, 2020.
The study was commissioned by the NSW Department of Health under the Public Health Act 2010 (NSW) and implemented in conjunction with approval and support from the NSW Department of Education.
Population-level data
All laboratory-confirmed COVID-19 cases in NSW, using SARS-CoV-2 nucleic acid testing,20 were recorded and monitored daily using the NSW Notifiable Conditions Information Management System. All cases (or their parent or carers) were interviewed at diagnosis to determine links to known COVID-19 cases, ascertain movements, and identify close contacts while infectious, including at educational facilities. Descriptive data for all laboratory-confirmed cases with onset from Jan 13 to May 1, 2020, were analysed.
School and ECEC setting case and close contact definitions and management
A COVID-19 school or ECECs index case was defined as the first identified laboratory-confirmed case who attended the facility while infectious. A school or ECEC setting primary case was defined as the initial infectious case or cases in that setting, and might or might not have been the index case. A secondary case was defined as a close contact with SARS-CoV-2 infection (detected through nucleic acid testing or serological testing, or both), which was considered likely to have occurred via transmission in that educational setting (based on no other epidemiological link or risk factor). Data on all cases' potential sources of infection and close contacts were obtained from interviews with cases, families, and school officials, and review of school timetables. Close contacts were defined as children or staff with face-to-face contact for at least 15 min, or who shared a closed indoor space for at least 40 min (generally the same class or lesson, typically consisting of 20–30 students) with a case during their infectious period. All close contacts quarantined at home for 14 days, had regular text message or telephone call contact to enquire about symptoms, and were instructed to be tested if they developed COVID-19-related symptoms at designated COVID-19 testing facilities. Schools and ECEC settings closed temporarily on case notification and generally reopened within 24–48 h after environmental cleaning and public health measures were instituted. We reviewed data for all close contacts for a minimum of 30 days from last exposure to the primary case, to ensure that any potential new cases were identified and investigated.
Targeted enhanced school and ECEC setting-based investigations
Selected educational settings were offered participation in enhanced investigations, in addition to routine public health management if logistically feasible and authorisation was provided by local public health and education authorities. Close contacts or their parents or carers were provided with information on enhanced investigations and informed consent was obtained (appendix). Participants could opt out at any time.
Enhanced investigations of close contacts included a survey requesting more details on extent of contact with the case, and symptoms before and during quarantine; upper respiratory tract (nasopharyngeal) swab for nucleic acid testing 5–10 days after last case contact if not previously collected and irrespective of symptoms; and serological testing after day 21 following last case contact. Swabs were collected at home either by visiting health-care workers, or by the case or parent or carer using written and video instructions. Blood was collected at home visits, dedicated school-based collection days, or pathology collection centres.
Laboratory testing
Ten public and three private NSW laboratories were validated and did SARS-CoV-2 nucleic acid testing during the study period. Blood and nasopharyngeal specimens for enhanced surveillance were tested by the NSW Pathology reference laboratory, the Institute for Clinical Pathology and Medical Research. Nucleic acid testing was done using an in-house real-time PCR as previously described.21 SARS-CoV-2-specific IgG, IgA, and IgM detection was done using an indirect immunofluorescence assay (IFA) that has a sensitivity compared with nucleic acid testing of detecting any of SARS-CoV-2-specific IgG, IgA, or IgM when samples were collected at least 14 days after illness onset of 91·3% (95% CI 84·9–95·6) and specificity of 98·9% (95% CI 98·4–99·3%; MVNO, personal communication).
Data analyses
Percentages were calculated to describe demographic, laboratory, and epidemiological characteristics of all NSW cases, school or ECEC setting cases, and close contacts. Attack rates were calculated for different transmission scenarios and with denominators including all close contacts or only close contacts who were tested for SARS-CoV-2. School attendance data were obtained from the NSW Department of Education. Population data were obtained from the Australian Bureau of Statistics. Data cleaning and analysis were done using Stata, version 14.2.
Role of the funding source
The funder of the study had no role in study design, data analysis, data interpretation, or writing of the report. The funder contributed to collection of data. KM, HEQ, AJP, AK, LD, NWi, ALK, MVNO, CD, and NWo had access to the raw data. The corresponding author had full access to all of the data and the final responsibility to submit for publication.
Results
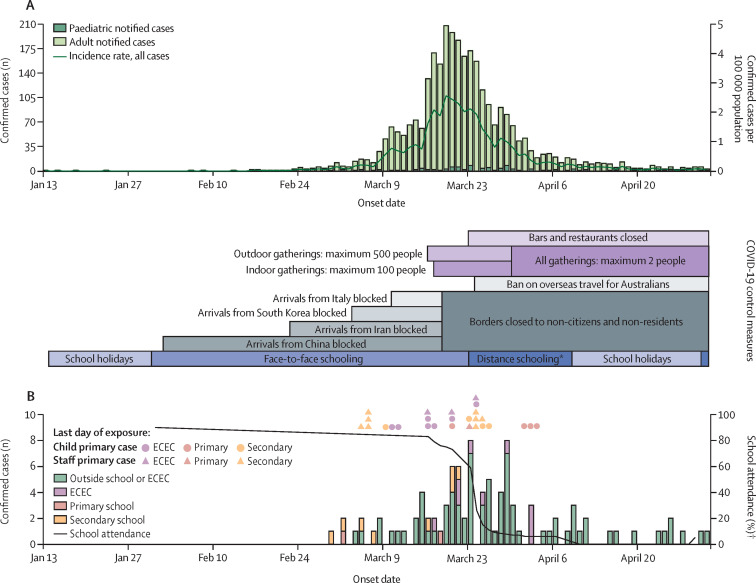
As of May 1, 2020, NSW had 3033 confirmed COVID-19 cases, representing 37·5 cases per 100 000 population and 44·8% of 6777 cases nationally (figure ). In NSW, 1760 (58·0%) of 3033 cases were acquired overseas and 54 (1·8%) of 3033 cases were acquired interstate. Of 1220 locally acquired cases, 416 (34·1%) had an unknown source or were under investigation. Children aged 18 years or younger accounted for 97 (3·2%) of 3033 cases in NSW. 9% (n=9) of children with COVID-19 were admitted to hospital (most for isolation purposes only), with one child, aged 18 years, admitted to intensive care (table 1 ).
Figure.
Onset date of total (A) and paediatric (B) confirmed COVID-19 cases in NSW, Jan 13–May 1, 2020, relative to control measures and school attendance
Nucleic acid testing used for confirmation of severe acute respiratory syndrome coronavirus 2 infection, and definition of COVID-19 case. If people were asymptomatic, specimen positive date was used. ECEC=early childhood education and care settings. NSW=New South Wales. *Distance (remote) learning recommended, but schools also remained open for face-to-face attendance as required. After school holidays, preference for distance learning continued for 2 weeks before resumption of full face-to-face learning. †Excluding ECEC.
Table 1.
Demographic and clinical data on all paediatric and adult COVID-19 cases in NSW, Australia, from Jan 13 to May 1, 2020, including links to an educational setting as either a primary or secondary case
|
Sex |
Age group |
Existing medical condition | Hospitalisation | ICU admission | Total (rate per 100 000 population) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | 0 to <5 years | 5 to <13 years | 13 to ≤18 years | 19 to ≤39 years | 40 to ≤59 years | ≥60 years | ||||||
| Paediatric cases | |||||||||||||
| Within school or ECEC | 13 (68%) | 6 (32%) | 9 (47%) | 3 (16%) | 7 (37%) | .. | .. | .. | 5 (26%) | 3 (16%) | 0 | 19 | |
| Primary case | 6 (50%) | 6 (50%) | 3 (25%) | 2 (17%) | 7 (58%) | .. | .. | .. | 4 (33%) | 3 (25%) | 0 | 12 | |
| Secondary case | 7 (100%) | 0 | 6 (86%) | 1 (14%) | 0 | .. | .. | .. | 1 (14%) | 0 | 0 | 7 | |
| Outside school or ECEC | 35 (44%) | 43 (55%) | 11 (14%) | 27 (34%) | 40 (51%) | .. | .. | .. | 9 (12%) | 6 (8%) | 1 (1%) | 78 | |
| All | 48 (49%) | 49 (51%) | 21 (21%) | 30 (31%) | 47 (48%) | .. | .. | .. | 14 (14%) | 9* (9%) | 1 (1%) | 97 (5) | |
| Adult cases | |||||||||||||
| Within school or ECEC | 1 (5%) | 21 (95%) | .. | .. | .. | 12 (55%) | 9 (41%) | 1 (5%) | 4 (18%) | 4 (18%) | 2 (9%) | 22 | |
| Primary case | 1 (7%) | 14 (93%) | .. | .. | .. | 8 (53%) | 6 (40%) | 1 (7%) | 3 (20%) | 2 (13%) | 0 | 15 | |
| Secondary case | 0 | 7 (100%) | .. | .. | .. | 4 (57%) | 3 (43%) | 0 | 1 (14%) | 2 (29%) | 2 (29%) | 7 | |
| Outside school or ECEC | 1450 (50%) | 1463 (50%) | .. | .. | .. | 1156 (40%) | 821 (28%) | 937 (32%) | 849 (29%) | 296 (10%) | 75 (3%) | 2914 | |
| All | 1451 (49%) | 1484 (51%) | .. | .. | .. | 1168 (40%) | 830 (28%) | 938 (32%) | 853 (29%) | 300 (10%) | 77 (3%) | 2936 (47) | |
Data are n (%), unless otherwise stated. ECEC=early childhood education and care setting. ICU=intensive care unit. NSW=New South Wales.
Most were hospitalised early in the epidemic response for isolation purposes only and had mild symptoms.
Notification of the first COVID-19 case in an educational setting was on March 5, 2020 (figure). Among 97 nucleic acid testing-confirmed cases in children to April 9, 2020, 19 (19·6%) attended an educational setting while infectious and were included in the study (table 1; figure). Of the other 78 paediatric cases, 44 (56·4%) were locally acquired from contact with a confirmed case, mostly from their household (70·5%; table 1).
The timing of measures implemented to ensure physical distancing and decrease population movement and school attendance rates are shown in the figure. Rates declined from approximately 90·0% to 5·0% after recommendations for distance learning were made on March 23, 2020, and immediately before school holidays commenced on April 10, 2020. Cases peaked in late March, with primary cases in schools occurring earlier in the outbreak and primary cases in ECEC settings occurring later in the outbreak (figure).
There were 27 primary cases identified in 25 schools (n=15) and ECEC settings (n=10); of 27 cases, 15 (55·6%) were staff and 12 (44·4%) were children (Table 1, Table 2 ). Of the child cases, eight (median age 15 years; range 14–16) were in secondary schools, with one (age 10 years) in primary school. Three ECEC setting primary cases were children (median age 2 years; range 2–3). Staff (median age 38 years; range 31–50) were the primary cases in four (40·0%) of ten secondary schools, four (80·0%) of five primary schools, and seven (70·0%) of ten ECEC settings. The median time that primary cases attended the setting while infectious was 2 days (range 1–10). Infection was locally acquired for all primary cases, but the source was unknown for many (12 [44·4%] of 27). Where known, a household member was usually the source, especially for children (table 2).
Table 2.
Primary COVID-19 cases and close contacts who attended 25 educational settings from March 5 to April 9, 2020, in NSW, Australia
|
Primary cases |
Days when contacts' NAT done post last exposure* |
Child close contacts |
Staff close contact |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years), sex (M or F) | Source of infection (all acquired locally) | Days infectious at school* | Age (years) | n | Contacts' NAT done† | NAT positive of contacts tested† | Age (years) | n | Contacts' NAT done† | NAT positive of contacts tested† | |||
| SS | |||||||||||||
| SS 1 | 16, M | Household | 4 | 3 (2–5) | 16 (16–16) | 58 | 19 (33%) | 0 | 51 (48–53) | 11 | 2 (18%) | 0 | |
| SS 2‡ | 14, M; 15, F | Household | Unknown§; 5 | 5 (3–8) | 15 (15–15) | 193 | 117 (61%) | 0 | 41 (27–49) | 18 | 12 (67%) | 0 | |
| SS 3 | 12, F | Household | 4 | 4 (4–5) | 12 (12–12) | 66 | 20 (30%) | 0 | 38 (34–39) | 11 | 5 (46%) | 0 | |
| SS 4 | 48, F | Source unknown | 1 | 6 (5–7) | 15 (13–15) | 46 | 15 (33%) | 0 | 47 (42–53) | 11 | 6 (54%) | 0 | |
| SS 5 | 53, F | Source unknown | 1 | 4 (4–4) | 14 (13–15) | 4 | 1 (25%) | 0 | 38 (36–46) | 6 | 5 (83%) | 0 | |
| SS 6‡ | 13, F; 15, M | Household | 5; 2 | 10 (8–13) | 15 (13–15) | 65 | 13 (20%) | 0 | 41 (30–45) | 9 | 2 (22%) | 0 | |
| SS 7 | 16, M | Household | 3 | 11 (11–12) | 16 (16–16) | 131 | 9 (7%) | 0 | 55 (48–64) | 8 | 1 (13%) | 0 | |
| SS 8 | 18, M | Household | 2 | 14 (11–14) | 17 (16–17) | 8 | 1 (13%) | 0 | 44 (31–56) | 7 | 3 (43%) | 0 | |
| SS 9 | 34, F | Source unknown | 1 | NA | 16 (16–16) | 10 | 0 | 0 | NA | 0 | 0 | 0 | |
| SS 10 | 65, F | Source unknown | 4 | 12 (10–15) | 13 (13–15) | 19 | 1 (5%) | 0 | 50 (44–53) | 15 | 3 (20%) | 0 | |
| All SSs | 8, 4¶ | NA | 3 (2–4)‖ | 5 (4–8) | 15 (14–16) | 600 | 196 (33%) | 0 | 44 (34–53) | 96 | 39 (41%) | 0 | |
| PS | |||||||||||||
| PS 1‡** | 46, F | Non-household contact | 1 | 6 (6–7) | 7 (6–10) | 66 | 28 (42%) | 1 (4%) | 45 (37–52) | 15 | 8 (53%) | 1 (13%)¶ | |
| PS 2† | 10, F | Source unknown | 10 | 12 (11–12) | 10 (10–10) | 43 | 6 (14%) | 0 | 60 (60–61) | 2 | 1 (50%) | 0 | |
| PS 3 | 31, F | Household | 3 | 7 (7–8) | 10 (10–11) | 15 | 1 (7%) | 0 | 32 (31–47) | 7 | 5 (71%) | 0 | |
| PS 4 | 21, M | Non-household contact | 4 | 7 (5–8) | 7 (5–9) | 27 | 4 (15%) | 0 | 24 (23–24) | 2 | 2 (100%) | 0 | |
| PS 5 | 19, F | Non-household contact | 5 | 7 (6–10) | 7 (6–8) | 28 | 3 (11%) | 0 | 25 (20–29) | 13 | 4 (31%) | 0 | |
| All PSs | 1, 4¶ | NA | 4 (3–5)‖ | 6 (6–11) | 9 (7–10) | 179 | 42 (23%) | 1 (2%) | 36 (26–52) | 39 | 20 (51%) | 1 (5%) | |
| ECEC | |||||||||||||
| ECEC 1‡ | 36, F | Non-household contact | 1 | 10 (8–13) | 4 (4–4) | 16 | 16 (100%) | 0 | NA | 0 | 0 | 0 | |
| ECEC 2 | 50, F | Non-household contact | 2 | 5 (3–6) | 4 (3–4) | 43 | 18 (42%) | 0 | 47 (42–50) | 6 | 2 (33%) | 0 | |
| ECEC 3‡ | 56, F | Acquired locally, source unknown | 9 | 7 (7–9) | 2 (1–3) | 151 | 79 (52%) | 0 | 30 (26–36) | 25 | 19 (76%) | 0 | |
| ECEC 4 | 30, F | Source unknown | 1 | 8 (7–8) | 2 (1–3) | 31 | 13 (42%9) | 0 | 32 (26–39) | 9 | 2 (22%) | 0 | |
| ECEC 5 | 3, F | Source unknown | 1 | 18 (15–19) | 3 (3–4) | 34 | 1 (3%) | 0 | 26 (22–32) | 18 | 3 (17%) | 0 | |
| ECEC 6‡ | 49, F | Source unknown | 1 | 16 (14–17) | 1 (2–3) | 25 | 23 (92%) | 6 (26%) | 38 (31–43) | 12 | 11 (92%) | 6 (55%) | |
| ECEC 7 | 2, M | Source unknown | 1 | 17 (15–17) | 3 (2–4) | 43 | 11 (26%) | 0 | 40 (38–50) | 14 | 5 (36%) | 0 | |
| ECEC 8 | 21, F | Non-household contact | 2 | 4 (4–4) | N/A | 0 | 0 | 0 | 31 (25–36) | 15 | 9 (60%) | 0 | |
| ECEC 9 | 1, F | Source unknown | 1 | 3 (3–3) | 1 (1–1) | 8 | 5 (63%) | 0 | 23 (20–31) | 5 | 3 (60%) | 0 | |
| ECEC 10 | 38, F | Source unknown | 2 | 5 (5–7) | 3 (2–3) | 55 | 16 (29%) | 0 | 29 (27–36) | 24 | 9 (38%) | 0 | |
| All ECEC | 3, 7¶ | NA | 1 (1–2)‖ | 8 (6–12) | 3 (2–4) | 406 | 182 (45%) | 6 (3%) | 34 (26–41) | 128 | 63 (49%) | 6 (10%) | |
| All settings | 12 (14), 15 (38)†† | 9 household; 6 non-household contact; 12 source unknown | 2 (1–4)‖ | 7 (5–10) | 10 (3–15) | 1185 | 420 (35%) | 7 (2%) | 37 (27–48) | 263 | 122 (46%) | 7 (6%) | |
Data are n; median (IQR); or n (%), unless otherwise stated. M=male. F=female. NAT=nucleic acid test. SS=secondary school. PS=primary school. NA=Not applicable. ECEC=early childhood education and care setting. NSW=New South Wales.
Day test done post last day of exposure (D0) to the infectious cases.
Close contacts were managed in home quarantine and instructed to be tested if symptoms developed; also includes some asymptomatic cases (see table 3).
Settings where enhanced surveillance was done (see table 3).
Unknown exposure duration as asymptomatic case.
Data are number of children, number of staff.
Data are median (IQR).
The primary case notification was late after exposure and symptom onset and occurred shortly before notification of the secondary staff case. Close contact follow-up for the primary case was incomplete and probably reduced the total number of primary case contacts having an NAT test. Close contacts of the secondary case included the child who was a tertiary case in this setting (see table 3).
Data are number of children (median), number of staff (median).
Secondary transmission occurred in four of 25 settings: three schools (five cases), and one ECEC setting that had an outbreak (table 2). In total, 663 (43·7%) of 1448 close contacts were tested by nucleic acid testing or serology, or both; 18 secondary cases were identified among the total 1448 close contacts (attack rate 1·2%). Among close child and staff contacts who had laboratory testing done, the attack rate was 2·8% (Table 3, Table 4 ).
Table 3.
Details of secondary cases resulting from COVID-19 transmission in seven NSW educational settings where enhanced surveillance of symptomatic and asymptomatic close contacts was done
|
Symptomatic (n=65) |
Asymptomatic (n=223) |
Symptoms unknown (n=352)* |
Total secondary cases | Percentage of contacts tested | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | NAT | Serology | Any test | n | NAT | Serology | Any test | n | NAT* | Serology | Any test | ||||
| Child contacts | |||||||||||||||
| SS 2 | 20 | 0/19 | 1/16 (6%) | 1/20 (5%) | 90 | 0/51 | 0/52 | 0/74 | 83 | 0/47 | 0/3 | 0/47 | 1 | 73% | |
| SS 6 | 4 | 0/4 | 0/3 | 0/4 | 43 | 0/5 | 1/36 (3%) | 1/36 (3%)† | 18 | 0/4 | 0/4 | 0/6 | 1 | 70% | |
| PS 1 | 2 | 1/2 (50%) | 1/2 (50%) | 1/2 (50%) | 18 | 0/18 | 0/13 | 0/18 | 46 | 0/8 | 0/1 | 0/8 | 1 | 42% | |
| PS 2 | 1 | 0/1 | 0/1 | 0/1 | 8 | 0/1 | 0/6 | 0/6 | 34 | 0/4 | 0/8 | 0/12 | 0 | 44% | |
| ECEC 1 | 0 | 0/0 | 0/0 | 0/0 | 0 | 0/0 | 0/0 | 0/0 | 16 | 0/16 | 0/5 | 0/16 | 0 | 100% | |
| ECEC 3 | 21 | 0/18 | 0/4 | 0/20 | 22 | 0/6 | 0/7 | 0/11 | 108 | 0/55 | 0/4 | 0/59 | 0 | 60% | |
| ECEC 6 | 7 | 3/6 (50%) | 3/6 (50%) | 4/7 (57%) | 13 | 3/13 (23%) | 2/8 (25%) | 3/13 (23%) | 5 | 0/4 | 0/2 | 0/4 | 7 | 96% | |
| All | 55 | 4/50 (8%) | 5/32 (16%) | 6/54 (11·%) | 194 | 3/94 (3%) | 3/122 (3%) | 4/158 (3%) | 310 | 0/138 | 0/27 | 0/152 | 10 | 65% | |
| Adult contacts | |||||||||||||||
| SS 2 | 1 | 0/1 | 0/0 | 0/1 | 8 | 0/4 | 0/3 | 0/5 | 9 | 0/7 | 0/2 | 0/7 | 0 | 72% | |
| SS 6 | 0 | 0/0 | 0/0 | 0/0 | 7 | 0/1 | 1/5 (20%) | 1/5 (20%) | 2 | 0/1 | 0/1 | 0/1 | 1 | 67% | |
| PS 1 | 1 | 1/1 (100%) | 0/0 | 1/1 (100%) | 5 | 0/3 | 0/4 | 0/5 | 9 | 0/4 | 0/1 | 0/4 | 1 | 67% | |
| PS 2 | 0 | 0/0 | 0/0 | 0/0 | 0 | 0/0 | 0/0 | 0/0 | 2 | 0/1 | 0/2 | 0/2 | 0 | 100% | |
| ECEC 1 | 0 | 0/0 | 0/0 | 0/0 | 0 | 0/0 | 0/0 | 0/0 | 0 | 0/0 | 0/0 | 0/0 | 0 | 100% | |
| ECEC 3 | 2 | 0/2 | 0/1 | 0/2 | 4 | 0/1 | 0/1 | 0/1 | 19 | 0/16 | 0/2 | 0/17 | 0 | 80% | |
| ECEC 6 | 6 | 6/6 (100%) | 2/2 (100%) | 6/6 (100%) | 5 | 0/4 | 0/2 | 0/4 | 1 | 0/1 | 0/1 | 0/1 | 6 | 92% | |
| All | 10 | 7/10 (70%) | 2/3 (67%) | 7/10 (70%) | 29 | 0/13 | 1/15 (7%) | 1/20 (5%) | 42 | 0/30 | 0/9 | 0/32 | 8 | 77% | |
| Total | 65 | 11/60 (18%) | 7/35 (20%) | 13/64 (20%) | 223 | 3/107 (3%) | 4/137 (3%) | 5/178 (3%) | 352 | 0/168 | 0/36 | 0/184 | 18 | 67% | |
Data are n/N (% positive of those contacts tested), unless otherwise stated. NAT=nucleic acid test. SS=secondary school. PS=primary school. ECEC=early childhood education and care setting. NSW=New South Wales.
55% of all contacts did not complete a detailed symptom questionnaire and other data on symptoms at time of testing could not be obtained.
Asymptomatic in post-exposure period but reported influenza-like illness in period before primary case onset.
Table 4.
Secondary attack rates of SARS-CoV-2 infection by educational setting and testing approach
| Secondary attack | ||
|---|---|---|
| All settings, all contacts, including single ECEC outbreak | 1·2% (18/1448) | |
| All settings, all contacts, excluding single ECEC outbreak* | 0·4% (5/1411) | |
| All settings, all child case to child contacts | 0·3% (2/649) | |
| All settings, all child case to staff member contacts | 1·0% (1/103) | |
| All settings, all staff member case to child contacts | 1·5% (8/536) | |
| All settings, all staff member case to staff member contacts | 4·4% (7/160) | |
| All settings, all staff member case to child contact, excluding single ECEC outbreak* | 0·2% (1/511) | |
| All settings, all staff member case to staff member contacts, excluding single ECEC outbreak* | 0·7% (1/148) | |
| All settings, tested population | 2·8% (18/633) | |
| All settings, tested population, excluding single ECEC outbreak | 0·8% (5/598) | |
| All schools, all contacts | 0·5% (5/914) | |
| All schools, tested population | 1·3% (5/375) | |
| Single ECEC outbreak,* all contacts | 35·1% (13/37) | |
| Child close contacts | 28·0% (7/25) | |
| Staff close contacts | 50·0% (6/12) | |
Data are rate % (n/N). SARS-CoV-2=severe acute respiratory syndrome coronavirus 2. ECEC=early childhood education and care.
This outbreak resulted in at least four generations of infection and there was no evidence of child to child or child to staff transmission (unpublished).
Seven of the 25 educational settings (four schools; three ECEC settings) participated in enhanced investigations (table 3). Among contacts who completed symptom questionnaires (44·9%), 65 (22·6%) of 288 developed symptoms consistent with COVID-19 during the 14-day quarantine, such as fever, sore throat, cough, or rhinorrhea. In these seven settings, 426 (66·6%) of 640 close contacts had nucleic acid testing or serological testing, or both. Secondary attack rates among symptomatic and asymptomatic contacts are shown in table 3.
Five secondary cases occurred in schools: one child in one secondary school; one child and one staff member in another secondary school; and one staff member, followed by one child in one primary school (table 3). This primary school was the only school to have a second-generation infection. Overall, two children were symptomatic and had nucleic acid testing (one positive on day 6 and the other negative on day 4 after last exposure), whereas one child and one staff member were asymptomatic and did not have nucleic acid testing. One symptomatic staff member had nucleic acid testing only (table 3). The attack rate in the tested population in schools was five (1·3%) of 375.
No SARS-CoV-2 transmission occurred in two of the three ECEC settings that participated in enhanced surveillance (25 staff and 167 child contacts). The third ECEC setting had a large outbreak first recognised via an index case in a child aged 2 years, but subsequently found related to a primary case in one staff member (infection source unknown; Table 2, Table 3). Overall, six other staff and seven children were infected (attack rate 35·1%). Among the infected close contacts, three of 13 were infants (age 1 year) who remained asymptomatic.
The overall child to child transmission rate was 0·3%, and the attack rate for child to staff member was 1·0% (table 4). The rate of staff member to child transmission was lower (1·5%) than staff to staff transmission (4·4%). Excluding the single ECEC setting with the large outbreak, staff member to child (0·2%) and staff member to staff member (0·7%) transmission rates were lower compared with all settings.
Discussion
This study of SARS-CoV-2 transmission in schools and early childcare settings in a defined population of 8·1 million Australians shows low case rates and secondary infections among children and staff attending educational facilities throughout the first epidemic wave of the COVID-19 pandemic. School closures during the COVID-19 pandemic have affected more than 90% of the world's student population,1 and contributed to reducing overall population mobility, including via reduced parent and carer workforce participation. However, the insufficiency of data on age-specific and setting-specific susceptibility and transmissibility of SARS-CoV-2 has limited our understanding of what school closure, or reopening, might contribute to COVID-19 control.9, 12 Our data provide multiple insights that need to be viewed in the context of our setting. First, and related to overall epidemic activity in NSW, the reported incidence of an infectious child or staff member attending an educational facility was low, occurring in only 25 of 7700 NSW facilities. Second, despite only 10·0% of school attendees being staff during the first part of the epidemic, when student attendance was high, overall, primary COVID-19 cases were staff members in 56·0% of educational settings; this is consistent with higher population-based rates of COVID-19 in adults than children. Third, secondary transmission of SARS-CoV-2 only occurred in three of 15 schools and one of ten ECEC settings. Only one setting, an ECEC setting, had a sustained outbreak of COVID-19 following infection in a staff member, which was not apparent until investigation of a child index case. Excluding this single ECEC setting outbreak, the overall attack rate was five (0·4%) in 1411, or one in every 282 contacts. Continued operation of schools throughout the moderate first epidemic wave in NSW, albeit with reduced face-to-face attendance in line with public health guidance, did not appear to contribute significantly to SARS-CoV-2 transmission (attack rate 0·5%). Attendance rates were still high during the period when transmission, in the two secondary and one primary schools, occurred. This finding was in contrast to other settings in NSW, where multiple outbreaks were contemporaneously identified, including aged-care facilities and mass gatherings, such as weddings and religious services.22
An important component of our study was enhanced follow-up in a subset of educational settings, including in both asymptomatic and symptomatic adult and child contacts. This resulted in laboratory testing in two-thirds of close contacts. The use of serology facilitated identification of four additional secondary cases, including an asymptomatic student and staff member, who were not detected using routinely deployed nucleic acid testing and increased secondary case numbers from that in our preliminary report23 to the NSW and Australian Government (n=2). By comparison, a small study16 from Ireland of six COVID-19 cases in three schools, over less than 2 weeks, suggested no transmission to 1115 close contacts. However, children aged younger than 10 years and data on testing rates were not included. In our study, the attack rate among the tested population across all schools was low (1·3%) and was zero in nine of the ten ECEC settings. The single ECEC setting outbreak was complex and occurred early on in the epidemic in NSW. 13 (35·1%) of 37 contacts in this small centre were infected; three of the seven infected children (all aged <3 years) remained asymptomatic and the others had mild disease. Transmission chains between staff and from staff to children were apparent. Child to child or child to staff transmission appeared unlikely to have occurred but could not be excluded. In addition, delayed primary case diagnosis, due to adherence to narrow nucleic acid testing criteria recommended at the time, close mixing of staff and children and shared physical amenities, probably contributed to the several generations of transmission (data not shown; unpublished). In summary, our findings add to emerging data7, 9 on the direction of transmission from household and similar settings, such as ECEC settings, that suggest children are unlikely to initiate, or propagate, outbreaks.
We report a correspondingly low rate of paediatric disease (97 cases among 1·8 million aged 18 years or younger; 5·2 per 100 000; 3·2% of total) across NSW, providing additional evidence of reduced transmission resulting in clinical disease to and between children. Studies from multiple countries have consistently shown lower rates of COVID-19 and mild disease in children compared with adults, even in settings with much higher population-based disease rates than Australia.2, 3, 4, 5, 24 Multiple hypotheses are being explored to explain the decreased susceptibility of children to SARS-CoV-2, including differences in immune responses25 and age-dependent expression of the angiotensin converting enzyme 2 (ACE2) virus receptor;26 however, the mechanisms responsible for this phenomenon remain unclear.
The low case and transmission rates in NSW schools and childcare settings reported here were underpinned by rapid and effective state and national public health, and community, responses.17 Although community-based transmission occurred in some areas, particularly in Sydney (based on the proportion of cases [34·2%] with a local or unknown source of infection despite intensive contact tracing, and an effective reproductive number above 1 until mid-March, 2020), the NSW epidemic was smaller and of shorter duration compared with that seen in many other countries.17, 27 Tracking SARS-CoV-2 transmission was possible in this epidemic context because frequent simultaneous case introductions to schools and ECEC settings were not occurring, and enabled by continued operation of educational facilities throughout the epidemic period, albeit with reduced face-to-face attendance in the weeks before school holidays. Higher SARS-CoV-2 primary case and transmission rates might have occurred in schools and ECEC settings if the epidemic had escalated or if extensive testing, tracing, quarantine of exposed close contacts, and other public health mitigation measures were not simultaneously and effectively implemented. Although there are no specific data on adherence to these measures by the public in NSW, several strategies were in place to support a high compliance rate, including for quarantine of close contacts identified in this study. These strategies included regular wellbeing calls by public health staff to facilitate access to essential goods without breaching isolation, and issuing of fines to people found in breach of isolation requirements during random house calls by NSW police. Interpretation of our findings needs to be made in the context of the epidemic characteristics and COVID-19 response in NSW.
Our study is also limited by several factors. First, the majority of close contacts were tested after developing symptoms, so infected contacts with no or mild symptoms might have been missed. Symptom data were also incomplete and might have been affected by participant recall bias. Additional enhanced surveillance was limited by geographical location and school or ECEC settings' willingness to participate during a challenging time. Second, transmission rates reported might have been affected by the sensitivity and specificity of assays (nucleic acid testing and the IFA for virus-specific antibody) used for the detection of SARS-CoV-2 infection. When compared with nucleic acid testing for the diagnosis of SARS-CoV-2 infection, the IFA is reported to have high sensitivity and specificity in a mixed patient population (asymptomatic individuals to patients requiring intensive care unit admission). We did not attempt transmission rates to adjust for test performance characteristics, given the non-uniform application of diagnostic testing methods in this study. Third, variation in close contact definitions used across settings, declining school attendance rates in the 2 weeks before school holidays, and differing types of contact could not be controlled for and might have influenced attack rates. However, although face-to-face attendance declined rapidly later in the study period in response to public health advice, the number of close contacts monitored (1411; 1185 children and 263 adults) was still substantial. The national public health definition of the infectious period for cases was extended from 24 h to 48 h before symptom onset after our study period based on the latest evidence. It is probable that additional close contacts would have been identified in our study had the 48-h presymptomatic contact definition been operational before the commencement of our study. Future studies in school settings in Australia or other countries using this criteria for the potential infectious period will build on our findings. Finally, we were unable to assess adherence to or the effect on transmission of recommendations regarding hygiene or physical distancing in educational settings, and these progressively increased in magnitude over the study period.
The possible benefits of school closures on SARS-CoV-2 transmission reduction must be considered against the adverse effects on child wellbeing, including the potential to exacerbate inequality.28 Although this study did not aim to assess the impact of school operation on the NSW epidemic, and it is unlikely that the effect of school closure alone can be disentangled from other broader pandemic control measures,29 our findings provide evidence that SARS-CoV-2 transmission in educational settings can be kept low and manageable in the context of an effective epidemic response. These data should inform modelling and decision making regarding planned return of children and teachers to classrooms as pandemic control evolves. Where pandemic mitigation measures result in strong disease control, we anticipate that schools can be open in a safe way, for the educational, social, and economic good of the community as we adapt to living with COVID-19.
Acknowledgments
Acknowledgments
NSW Health funded the National Centre for Immunisation Research and Surveillance for the COVID-19 schools transmission study entitled, Enhanced investigation and analysis of education setting-related COVID-19 in NSW. We thank all schools, staff, and student contacts and their families who participated in this work, especially those who assisted with the enhanced investigations. We acknowledge the following people who contributed to this work: Kerri Basile, at the Institute of Clinical Pathology and Medical Research, Westmead/NSW Pathology; and Lisa McCallum, Caroline Sharpe, Paula Spokes, and Jeremy McAnulty at the NSW Ministry of Health.
Contributors
KM, HEQ, AK, LD, NWi, ALK, CD, and NWo contributed to the study design. KM, HEQ, AJP, AK, LD, NWi, ALK, and NWo contributed to the literature review. KM, HEQ, AJP, AK, LD, NWi, MVNO, and NWo analysed the data. KM, HEQ, AJP, AK, LD, NWi, and NWo contributed to writing of the Article. KM, HEQ, AJP, AK, LD, NWi, ALK, and NWo contributed to the preparation of the Article. ALK contributed to data collection and MVNO contributed to laboratory testing. All authors contributed to data interpretation and Article review. The NSW COVID-19 Schools Study Team contributed to the study design, study recruitment, specimen collection, and participant interviews and follow-up.
NSW COVID-19 Schools Study Team
Deidre Brogan, Catherine Glover, Nicole Dinsmore, Andrew Dunn, Ajay Jadhav, Rosemary Joyce, Rama Kandasamy, Kathryn Meredith, Lisa Pelayo, Laura Rost, Gemma Saravanos (National Centre for Immunisation Research and Surveillance); Shopna Bag, Stephen Corbett (Western Sydney Public Health Unit [PHU]); Michael Staff (Northern Sydney PHU); Kate Alexander, Stephen Conaty (South Western Sydney PHU); Kate Leadbeater (Hunter New England PHU); Brad Forssman, Sheena Kakar (Nepean-Blue Mountains PHU); Dominic E Dwyer, Jen Kok (Institute for Clinical Pathology and Microbiology, NSW Health Pathology); and Kerry Chant (Ministry of Health, NSW Government).
Declaration of interests
KM, HEQ, AJP, AK, LD, NWi, and NWo report receiving a grant from NSW Government Department of Health for the conduct of this study. NWo also reports other funding from the University of Sydney and the Sydney Children's Hospital Network outside of the submitted work. All National Centre for Immunisation Research and Surveillance-based members of the Study Team (DB, CG, ND, AD, AJ, RJ, RK, KMe, LP, LR, and GS) also report receiving a grant from the NSW Government Department of Health for the conduct of this study. RK also reports an Emerging Leader Fellowship from the National Health and Medical Research Council. All other authors declare no competing interests.
Contributor Information
NSW COVID-19 Schools Study Team:
D Brogan, C Glover, N Dinsmore, A Dunn, A Jadhav, R Joyce, R Kandasamy, K Meredith, L Pelayo, L Rost, G Saravanos, S Bag, S Corbett, M Staff, K Alexander, S Conaty, K Leadbeater, B Forssman, S Kakar, D Dwyer, J Kok, and K Chant
Supplementary Material
References
- 1.UNESCO . UNESCO; Paris: 2020. COVID-19 educational disruption and response.https://en.unesco.org/covid19/educationresponse [Google Scholar]
- 2.Bialek S, Gierke R, Hughes M, McNamara LA, Pilishvili T, Skoff T. Coronavirus disease 2019 in children - United States, February 12–April 2, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:422–426. doi: 10.15585/mmwr.mm6914e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dong Y, Mo X, Hu Y. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145 doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 4.Gudbjartsson DF, Helgason A, Jonsson H. Spread of SARS-CoV-2 in the Icelandic population. N Engl J Med. 2020;382:2302–2315. doi: 10.1056/NEJMoa2006100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lu X, Zhang L, Du H. SARS-CoV-2 infection in children. N Engl J Med. 2020;382:1663–1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qiu H, Wu J, Hong L, Luo Y, Song Q, Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis. 2020;20:689–696. doi: 10.1016/S1473-3099(20)30198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhu Y, Bloxham CJ, Hulme KD. Children are unlikely to have been the primary source of household SARS-CoV-2 infections. medRxiv. 2020 doi: 10.1101/2020.03.26.20044826. published online March 30. (preprint) [DOI] [Google Scholar]
- 8.Viner RM, Mytton OT, Bonell C. Susceptibility to and transmission of COVID-19 amongst children and adolescents compared with adults: a systematic review and meta-analysis. medRxiv. 2020 doi: 10.1101/2020.05.20.20108126. published online May 24. (preprint) [DOI] [Google Scholar]
- 9.Viner RM, Russell SJ, Croker H. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020;4:397–404. doi: 10.1016/S2352-4642(20)30095-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jackson C, Vynnycky E, Hawker J, Olowokure B, Mangtani P. School closures and influenza: systematic review of epidemiological studies. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2012-002149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen WC, Huang AS, Chuang JH, Chiu CC, Kuo HS. Social and economic impact of school closure resulting from pandemic influenza A/H1N1. J Infect. 2011;62:200–203. doi: 10.1016/j.jinf.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 12.Prem K, Liu Y, Russell TW. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fontanet A, Tondeur L, Madec Y. Cluster of COVID-19 in northern France: a retrospective closed cohort study. medRxiv. 2020 doi: 10.1101/2020.04.18.20071134. published online April 23. (preprint) [DOI] [Google Scholar]
- 15.Danis K, Epaulard O, Bénet T. Cluster of coronavirus disease 2019 (COVID-19) in the French Alps, 2020. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa424. published online April 11. (preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heavey L, Casey G, Kelly C, Kelly D, McDarby G. No evidence of secondary transmission of COVID-19 from children attending school in Ireland, 2020. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.21.2000903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McAnulty JM, Ward K. Suppressing the epidemic in New South Wales. N Engl J Med. 2020;382:e74. doi: 10.1056/NEJMc2011592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Australian Government Department of Health Australian Health Protection Principal Committee (AHPPC) coronavirus (COVID-19) statement on 17 March 2020. 2020. https://www.health.gov.au/news/australian-health-protection-principal-committee-ahppc-coronavirus-covid-19-statement-on-17-march-2020-0
- 19.Australian Bureau of Statistics Australian demographic statistics, December 2019. Estimated resident population by single year of age, New South Wales. 2020. https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3101.0Dec%202019?OpenDocument
- 20.Australian Government Department of Health Coronavirus disease 2019 (COVID-19) Communicable Diseases Network Australia (CDNA) national guidelines for public health units—COVID-19. 2020. https://www1.health.gov.au/internet/main/publishing.nsf/Content/cdna-song-novel-coronavirus.htm
- 21.Rahman H, Carter I, Basile K. Interpret with caution: an evaluation of the commercial AusDiagnostics versus in-house developed assays for the detection of SARS-CoV-2 virus. J Clin Virol. 2020;127 doi: 10.1016/j.jcv.2020.104374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.New South Wales Government Department of Health 2020 media releases from NSW Health. 2020. https://www.health.nsw.gov.au/news/Pages/2020-nsw-health.aspx
- 23.New South Wales Government Department of Health COVID-19 schools transmission investigation project team. COVID-19 in schools—the experience in NSW. 2020. http://ncirs.org.au/sites/default/files/2020-04/NCIRS%20NSW%20Schools%20COVID_Summary_FINAL%20public_26%20April%202020.pdf
- 24.Lavezzo E, Franchin E, Ciavarella C. Suppression of COVID-19 outbreak in the municipality of Vo, Italy. medRxiv. 2020 doi: 10.1101/2020.04.17.20053157. published online April 18. (preprint) [DOI] [Google Scholar]
- 25.Carsetti R, Quintarelli C, Quinti I. The immune system of children: the key to understanding SARS-CoV-2 susceptibility? Lancet Child Adolesc Health. 2020;4:414–416. doi: 10.1016/S2352-4642(20)30135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bunyavanich S, Do A, Vicencio A. Nasal gene expression of angiotensin-converting enzyme 2 in children and adults. JAMA. 2020;323:2427–2429. doi: 10.1001/jama.2020.8707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Price DJ, Shearer FM, Meehan MT. Early analysis of the Australian COVID-19 epidemic. medRxiv. 2020 doi: 10.1101/2020.04.25.20080127. published online April 30. (preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Armitage R, Nellums LB. Considering inequalities in the school closure response to COVID-19. Lancet Glob Health. 2020;8:e644. doi: 10.1016/S2214-109X(20)30116-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cowling BJ, Ali ST, Ng TWY. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5:e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.