Abstract
Purpose of review
Increasingly, digital technologies, especially mobile telecommunications and smartphone apps, are seen as a novel tool for managing severe mental disorders (SMDs) in low- and middle-income countries (LMICs). However, there is a need to identify best practices in the use of digital technologies to effectively reach, support and manage care for patients living with SMDs. In this review, we summarize recent studies using digital technology to manage symptoms and support clinical care for this patient population and discuss new opportunities to advance digital psychiatry research and practice in LMICs.
Recent findings
Studies evaluating digital interventions for clinical populations living with SMDs in LMICs are limited. Yet, across recent articles surveyed, digital technology appears to yield diverse benefits for this at-risk patient population. These benefits include improved medication adherence, appointment adherence, reduced instances of relapse and fewer re-hospitalizations.
Summary
Continued rigorous research evaluating effectiveness and cost-effectiveness of digital technologies in reaching, treating and managing symptoms and supporting clinical care for patients with SMDs in LMICs is vital. The urgency for remote approaches for delivering specialized psychiatric care is particularly pronounced due to the immediate and long-term impact of the coronavirus (COVID-19) pandemic on access to in-person services. Future research should emphasize participatory approaches rooted in a process of co-design with target users, in order to achieve clinically effective remotely delivered digital mental health interventions.
Keywords: digital psychiatry, severe mental disorders, digital technology, global health, mental health, mHealth
Introduction
Although all countries can be viewed as ‘developing’ in the context of mental health provision, low and middle-income countries (LMICs) face unique challenges.[1] Their health systems are frequently fragmented by geography, undermined by inadequate legislation, and higher rates of poverty adversely impact individuals’ mental health.[2,3] Further, the supply-side constraints faced by higher income countries are more acute in LMICs. The ratio of mental health workers to the population is estimated to be nearly 200 times greater in high-income countries when compared to LMICs.[4] This shortage of providers means that up to 90% of individuals living with mental disorders in LMICs receive no mental health care.[5]
When considering mental health interventions, the goal of equity in service delivery demands that we focus on those living with Severe Mental Disorders (SMDs), as these individuals, when compared to the general population, are less likely to seek care, less likely to use digital technology, and more likely to experience discrimination, isolation, social disadvantage, and premature mortality.[1] SMDs are also a leading contributor to the global burden of disease.[6] Schizophrenia is one of the top 15 causes of disability worldwide and those living with the disorder die on average 15 years earlier than those without.[7,8] Similarly, bipolar disorder affects 45 million people worldwide.[9] The burden of disease also appears to fall disproportionately on LMICs; for instance, the Indian state of Bihar has more individuals suffering from schizophrenia than all of North America.[10]
Consequently, there is a clear need to build innovative care models to serve individuals with SMDs who reside in LMICs. In this paper, we review studies that have evaluated the use of digital technologies to reach patients with SMDs, support and manage their symptoms, and augment clinical care. This is a novel, yet pressing area of study, and our aim is to highlight key insights from the work conducted so far to inform future directions in the field. The scope of this review covers digital technology interventions targeting serious mental illness, defined as disorders characterized by psychotic symptoms such as schizophrenia and bipolar disorder, in low-income and middle-income countries (LMICs).[11] LMICs were defined based on the World Bank’s classification system. [12]
Rapid Proliferation of Mobile Telecommunications in LMICs
The rapid proliferation of digital technology, specifically mobile telecommunications and smartphone apps represents a chance to shift the status quo. In November 2019, there were 6.2 billion unique mobile broadband subscriptions globally.[13] Cellular phone subscriptions encompass 86% of the population in India, 114% of the population in China, and 82% and 101% of the population in Africa and Latin America, respectively.[13] In the third quarter of 2019, China, Indonesia and the Philippines added 14 million, 9 million and 6 million new mobile subscriptions respectively.[13] Additionally, as of 2020, cellular devices account for 53.3% of global web traffic.[14] It is evident that mobile technology has now achieved widespread adoption and use in LMICs. As such, opportunities for digital technology to support those living with SMDs through telepsychiatry, training lay providers, predicting relapse, challenging stigma, or improving adherence and treatment engagement, among other functions, need to be explored.
Potential Impact of Digital Technology
In LMICs, the supply of care for individuals with SMDs is hampered by the limited numbers of mental health workers and inequitable distribution of providers. In India for instance, there is approximately one trained psychiatrist for every 250,000 people, and the total mental health workforce (including psychiatrists, clinical psychologists, and psychiatric social workers) available is <1 provider per 100,000 people.[15] Furthermore, these few providers and specialized psychiatric facilities are concentrated in major cities.[15] In such a context, digital technology could play a vital role in bridging the care gap by either extending the reach of this limited number of providers, or connecting patients with remote services delivered by non-specialized providers.[16]
Digital technology could benefit patients with SMDs across the entire continuum of care. This includes augmenting prevention activities, enabling the delivery of treatment, symptom management, fostering patient adherence, and providing an outlet for social interaction. On the other hand, recent studies suggest that commercially available digital platforms, such as apps, are not often rigorously tested and could even harm an at-risk population.[17] A 2015 review that assessed 82 commercially available smartphone apps to manage bipolar disorder concluded that in general, the content was not in line with practice guidelines or established self-management principles.[18] A recent study found that only 14% of a sample of 73 smartphone apps involved individuals with lived experience in the design or development process.[19*]
Methods Used
The study selection and data extraction process involved searching Medline/PubMed and Google Scholar to find pertinent studies. Findings from previous literature reviews on use of digital technology for mental health care in LMICs also informed our search. [20–23] Only studies that implemented and evaluated digital interventions for SMDs are profiled. Data extraction involved collection of study characteristics, including country of origin, study design, sample description, intervention description, and primary outcome.
Reviewing the Evidence:
Studies using digital technology to manage SMDs in LMICs
In Table 1, we present 7 studies [24–30] from LMICs that leverage digital technology to reach, treat and manage SMDs. Although this is not a systematic review, it is evident from the findings that the field remains nascent. Interestingly, 5 out of 7 studies used text messages to facilitate medication adherence, improve clinic attendance and improve patient functioning. Thomas et al. and Maiga et al. reported that text message reminders improved appointment attendance for patients with psychosis in two countries in sub-Saharan Africa.[24,25] Sibeko et al. conducted formative work in South Africa and found that text messaging could boost clinic attendance, but loss of handsets due to misplacement and theft proved challenging during the trial.[26]
Table 1:
Studies using digital technology to manage SMDs in LMICs
| Authors | Country | Study Aim | Design | Participants | Findings |
|---|---|---|---|---|---|
| Chen et al (2007)[29] | China | Comparative study of relapse prevention in schizophrenia by network |
Randomized control trial with one year follow up. Online psychoeducation for relapse prevention combined with drug treatment for non-acute schizophrenia; compared with general rehabilitation control group |
71 patients with schizophrenia | Intervention group showed a significant decrease in positive and negative symptoms and relapse incidence compared with control group (p<0.01) Intervention group had better medication adherence and social function than the control group (p<0.01). |
| Fang et al. (2011)[28] | China | Effects of daily short message reminder for preventing schizophrenia recrudescence |
Randomized control trial with a two year follow up. Mobile SMS text-messages sent daily as reminders for medication adherence combined with antipsychotic treatment and telephone follow-up; compared with control group with antipsychotic treatment and telephone follow-up only |
91 patients with clinically stable schizophrenia | At two-year follow-up, relapse rates were 36% in the intervention group compared with 61% in the control group (p=0.03). Daily SMS text-message reminders appear effective for reducing relapse in schizophrenia. |
| Maiga et al (2011)[25] | Niger | Impact of mobile technology on follow up visit attendance among patients with psychosis | Randomized control trial with a two year follow up. Reminder SMS text-messages and phone calls two days before monthly follow-up appointments; compared with control without appointment reminders |
100 participants with psychosis | The intervention group attended significantly more monthly follow-up visits than the control group (p<0.05) |
| Ozkan et al.[30] (2013) | Turkey | Effect of psychoeducation and telepsychiatric follow up given to the caregiver of the schizophrenic patient on family burden, depression and expression of emotion |
Randomized-controlled experimental study |
62 participants with schizophrenia and their caregivers assigned to experiment (n=32) and control (n=30) groups |
Mean scores of caregivers in the experiment group with regards to family burden, emotional expression and depression decreased after education and after telephone follow-up. The difference was significant (p<0.001). |
| Sibeko et al.[26] (2017) | South Africa | Improving adherence in mental health service users with severe mental illness in South Africa | A pilot randomized controlled trial of a treatment partner and text message intervention vs treatment as usual (TAU). Intervention pairs underwent treatment-partner contracting, psychoeducation and received monthly text message reminders of clinic appointments. | 77 participants were recruited from a psychiatric hospital in Cape Town. 42 randomized to receive the intervention and 35 to TAU. |
Formative work by the researchers found support for text message reminders. Yet, during the trial, a range of challenges were encountered Both participants and fieldworkers reported loss of handsets and fieldworkers faced software-related challenges. The text message component was deemed acceptable but not feasible in its current form. Factoring in contextual socio-economic factors and minimizing the complexity of software used is key to boosting the utility of text message prompts in this setting. |
| Thomas et al.[24] (2017) | Nigeria | Effect of short message service reminders on clinic attendance among outpatients with psychosis at a psychiatric hospital in Nigeria |
Patients seeking treatment for a psychotic episode for the first time were randomly assigned to a control group or intervention group. Both groups received appointment dates on appointment cards, and the intervention group also received SMS text reminders of their appointments. |
A total of 192 patients were included in a per-protocol analysis |
Participants who received the SMS reminders were almost twice as likely to attend their appointment compared with the control group. The analysis showed that receiving an SMS reminder independently reduced the risk of a missed next appointment by 50%. |
| Xu et al.[27] (2019) |
China | Lay health supporters aided by mobile text messaging to improve adherence, symptoms, and functioning among schizophrenia patients in a resource-poor community in rural China (LEAN) |
The control group received a free antipsychotic medication under the public ‘686 Program’ (also known as the National Continuing Management and Intervention Program for Psychoses), while the intervention group received the 686 Program plus LEAN. | There were 278 participants in total and 271 out of 278 were successfully followed up for outcome assessment. All participants were community-dwelling villagers from 9 townships of Hunan, China. |
Significant improvement in medication adherence (27% improvement in adherence in the intervention group) Substantial reduction in risk of relapse in the intervention group (21.7%) versus the control (34.7%) Substantial reduction in rehospitalization in the intervention group (7.3%) versus the control (20.5%) Texting effectively addressed the low adherence at marginal cost. |
A key study due to the broad range of outcomes assessed is the Xu et al. study based in China. Psychosis patients were provided with a ‘lay health supporter’ and text message communication was used for medication reminders, health education, monitoring of early signs of relapse, and linkage to primary healthcare. [27**] Outcomes assessed included medication adherence, patient symptoms, functioning, relapses, and re-hospitalizations. The intervention contributed to improvement in medication adherence and reduction in risk of relapse and rehospitalization.[27] Similarly, Fang et al. recorded that text message reminders to foster medication adherence can result in lower relapse rates for schizophrenia patients. [28]
Potential Benefits and Challenges of Using Digital Technology for SMDs
Benefits of Digital Technology Use
In high-income settings, there is a growing body of evidence highlighting the range of benefits catalyzed by digital interventions for individuals living with SMDs. A 2019 article by Ben-Zeev et al. outlines the demonstrated potential of digital health platforms to act as sources of information, communities of support, modes of clinical service delivery, psychoeducation, self-management and medication adherence tools for individuals living with psychosis.[31**] Although similar research in lower resource settings is limited, study findings summarized in Table 1 and graphically illustrated in Figure 1 reflect that digital technology can yield important benefits for individuals living with SMDs in LMICs. In the current scenario, the evidence base is strongest for the use of text message prompts to facilitate medication and treatment adherence.
Figure 1:
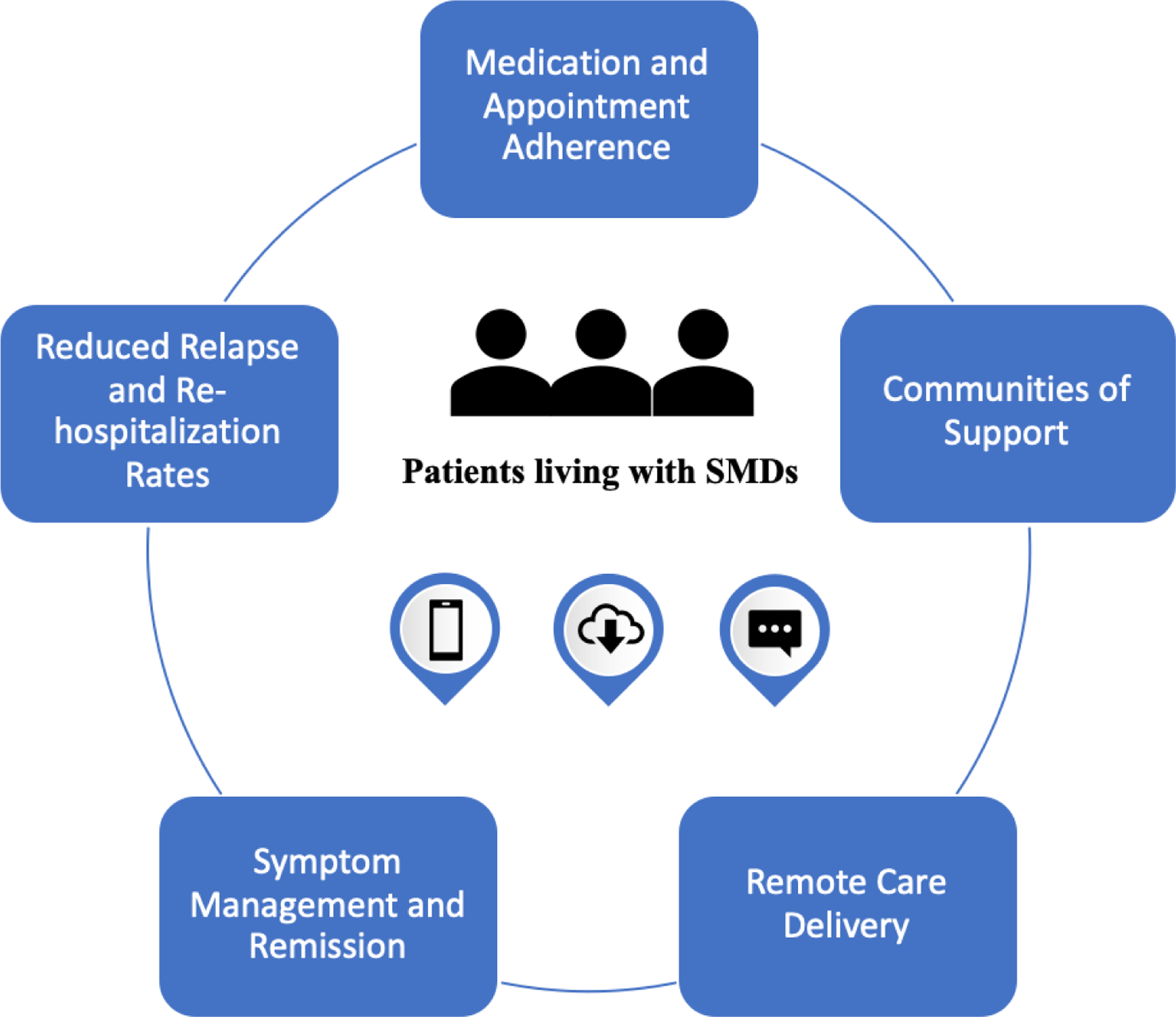
As depicted in this illustration, digital technology could yield important benefits for individuals living with SMDs in LMICs across the care continuum
Studies in low-income settings also suggest that there is increased caregiver demand for digital mental health interventions. A cross-sectional survey by Deb et al. in India studied the use of smartphone-based interventions in patients with SMDs and their caregivers. Their findings suggest that caregivers are interested in mobile apps that could automate routine caregiving activities and democratize information regarding resources for people with SMDs.[32] These preliminary findings suggest the importance of considering the family members of persons with SMDs when designing or implementing digital interventions for this high-risk patient group.
Further, the extensive period of physical distancing triggered by the coronavirus (COVID-19) pandemic, highlights the value of robustly tested remote interventions that leverage digital technology. Individuals living with SMDs may need to attend regular outpatient visits for evaluations and prescriptions.[33] Worldwide policies of physical isolation coupled with increased social and economic stressors mean that outpatients with SMDs may find it difficult to access maintenance treatment, leading to relapse and uncontrollable behaviors.[34**] In this context, digital technologies are key to reach patients and deliver evidence-based services to maintain care continuity and respond to relapse. Beyond the immediate mental health needs resulting from periods of lockdown and distancing, it is likely that a second mental health crisis will emerge in the near future as a result of the severe economic consequences of the pandemic. [35*] Economic recessions are often associated with a high prevalence of mental health disorders. [36] A slowdown in the post-COVID-19 context is likely to disproportionately affect patient populations that require long-term management and access to specialized services, such as individuals living with SMDs. The availability of essential services for individuals living with SMDs may also be compromised, as health systems shift priorities towards addressing COVID-19 and preparing for response to future pandemics. Therefore, telehealth and digital technologies will play an important role for ensuring the delivery of remote support and services necessary for reaching and managing care for patients with SMDs, while maintaining the safety and well-being of the clinician.[37**]
Challenges of Digital Technology Use
A key challenge is alluded to in the Sibeko et al. study mentioned in Table 1. Cellular devices can be lost or misplaced, and the challenges with the required software can occur. [26] Further, the Xu et al. study found that 28.8% and 47.9% of patients could not master the task of reading and replying to messages, respectively.[27] The cross-sectional study by Deb et al. also found that health app usage among study participants was low and that the language of the medium hindered adoption.[31] Low digital literacy of patient populations can hamper the effectiveness of a digital health intervention and as such, committing to a rigorous process of co-design with patients, caregivers and clinicians is vital. Co-design is particularly relevant when creating apps and other digital interventions for individuals living with SMDs as there is a need to accommodate any potential cognitive limitations or challenges with motor functioning caused by their illness.
Gaps in access to and use of digital technologies remain in many settings, especially among women compared to men, and among those who are most impoverished.[22] This is particularly pertinent for individuals living with SMDs, as this population is more likely to experience homelessness, marginalization and poorer living standards.[1,38] Furthermore, in regions with poor or variable wireless connectivity, it may be difficult to realize the full potential of many digital psychiatry apps that require continuous online access.[21]
More generally, there is mounting evidence that digital technologies impact our mental health in both positive and negative ways.[39–43] For instance, a nationally representative survey of American adolescents by Twenge et al. in 2017, found that adolescents who spent more time on new media (including social media and electronic devices such as smartphones) were more likely to report mental health issues.[39] As patients living with SMDs are already an at-risk group, it is vital to develop an evidence-based understanding of the use and scope of different digital technologies for each clinical sub-group.
Conclusion
In all countries, and particularly LMICs, supply-side constraints with regards to service infrastructure mean that we cannot accommodate all individuals who require care.[44*] This reality is coupled with the immediate and long-term impact of the COVID-19 pandemic. Given this backdrop, and the need that patients living with SMDs have for long-term management and access to specialized services, digital technologies must play a larger role in care delivery.
As discussed in this paper, digital technologies could contribute to improved medication adherence, appointment adherence, reduced relapse and fewer re-hospitalizations among patients with SMDs. These technologies also afford the scope to catalyze a broader range of benefits, but continued research is necessary. This review found only three studies in the last three years evaluating digital interventions for clinical populations living with SMDs in LMICs. Relative to other mental disorders such as depression or anxiety, research on the effectiveness of digital interventions aimed at this patient population in LMICs appears to be scarce, and there is a demonstrated need to accelerate research in this area. [20,21,22]
In future efforts, it is necessary to closely involve target users across the development, testing, and implementation stages of a digital intervention.[23*] Referred to as participatory approaches, these methods allow target users to share insights through a series of focus groups, interviews, iterative workshops and prototype testing.[45] Additionally, successfully leveraging technology in to drive benefits for patients requires integrating effective interventions into local healthcare systems, cultural contexts and social settings.[44*] Future research should concurrently consider how to achieve clinically effective digital mental health interventions as well as how to integrate these interventions into LMIC health systems to advance care for individuals living with SMDs.
Key Points:
Chronic supply-side shortages coupled the imperatives of a post-coronavirus world, mean that there is an urgent need for more research on leveraging remotely delivered digital platforms to reach, support and manage patients living with SMDs in LMICs.
Digital technology can drive benefits for patients across a range of outcomes including improved medication adherence, appointment adherence as well as reduced relapse and re-hospitalizations.
Adopting participatory approaches that emphasize the co-design of a digital intervention and involve patients, caregivers and clinicians is vital to ensure contextual and cultural relevance of the intervention and uptake and adoption among the target patient population.
DISCLOSURE OF FUNDING
Funding for this study was received from Wellcome Trust (Grant number: WT215843/Z/19/Z). Additional support was received from the National Institute of Mental Health (Grant number: 5U19MH113211). The funders played no role in the study design; collection, analysis, or interpretation of data; writing of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Conflicts of Interest
Rutvij Merchant declares that he has no conflict of interest
John Torous declares that he has no conflict of interest.
Elena Rodriguez-Vila declares that she has no conflict of interest.
John A. Naslund declares that he has no conflict of interest.
References and Recommended Reading
Papers of particular interest, published within the annual period of review, have been highlighted as:
* Papers of special interest
**Papers of outstanding interest
- 1.Patel V, Saxena S. Achieving universal health coverage for mental disorders. BMJ 2019; 366:l4516 doi: 10.1136/bmj.l4516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rathod Shanaya, Pinninti Narsimha, Irfan Muhammed, et al. Mental health service provision in low-and middle-income countries. Health Serv Insights. 2017; 10: 1178632917694350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lund Crick, Breen Alison, Flisher Alan J, et al. Poverty and common mental disorders in low- and middle-income countries: A systematic review. Soc Sci Med. 2010. August; 71(3): 517–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007. September 8; 370(9590):878–89. [DOI] [PubMed] [Google Scholar]
- 5.Patel V, Maj M, Flisher AJ, et al. Reducing the treatment gap for mental disorders: a WPA survey. World Psychiatry. 2010; 9:169–76. doi: 10.1002/j.2051-5545.2010.tb00305.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vigo D, Thornicroft G, Atun R, 2016. Estimating the true global burden of mental illness. The Lancet Psychiatry 3(2), 171–178 [DOI] [PubMed] [Google Scholar]
- 7.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017. September 16;390(10100):1211–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis. Lancet Psychiatry. 2017. Apr;4(4):295–301. doi: 10.1016/S221-0366(17)30078-0 [DOI] [PubMed] [Google Scholar]
- 9.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018; 392: 1789–858. DOI: 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adams CE, Tharyan P, Coutinho ES, Stroup TS. The schizophrenia drug-treatment paradox: pharmacological treatment based on best possible evidence may be hardest to practise in high-income countries. British Journal of Psychiatry, 189(5), 391–392. doi: 10.1192/bjp.bp.106.029983 [DOI] [PubMed] [Google Scholar]
- 11.Nguyen T, Tran T, Tran H, et al. The burden of clinically significant symptoms of common and severe mental disorders among adults in Vietnam: a population-based cross-sectional survey. BMC Public Health 19, 1173 (2019). 10.1186/s12889-019-7513-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The World Bank. [accessed Mar 28, 2020]; World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519.
- 13.Jonsson P, Carson S, Blennerud G, et al. Ericsson Mobility Report. 2019. [accessed Mar 28, 2020] https://www.ericsson.com/4acd7e/assets/local/mobility-report/documents/2019/emr-november-2019.pdf [Google Scholar]
- 14.Digital Kemp S. 2020: Global Digital Overview. 2020. [accessed April 18, 2020] https://wearesocial.com/uk/blog/2020/01/digital-2020-3-8-billion-people-use-social-media
- 15.Lahariya C Strengthen mental health services for universal health coverage in India. J Postgrad Med. 2018;64(1):7–9. doi: 10.4103/jpgm.JPGM_185_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pathare S, Brazinova A, Levav I. Care gap: a comprehensive measure to quantify unmet needs in mental health. Epidemiol Psychiatr Sci. 2018. October;27(5):463–467. doi: 10.1017/S2045796018000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Naslund JA, Marsch LA, McHugo GJ, Bartels SJ. Emerging mHealth and eHealth interventions for serious mental illness: a review of the literature. J Ment Health. 2015;24(5):321–332. doi: 10.3109/09638237.2015.1019054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nicholas J, Larsen ME, Proudfoot J, Christensen H. Mobile Apps for Bipolar Disorder: A Systematic Review of Features and Content Quality. J Med Internet Res. 2015;17(8): e198 Published 2015 Aug 17. doi: 10.2196/jmir.4581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *19.Larsen ME, Huckvale K, Nicholas J. et al. Using science to sell apps: Evaluation of mental health app store quality claims. npj Digit. Med 2, 18 (2019). 10.1038/s41746-019-0093-1 [DOI] [PMC free article] [PubMed] [Google Scholar]; * This study examined the app descriptions of 73 of the top ranked mental health apps publicly available and found that direct evidence from app-specific studies was often. lacking, involvement of end users with lived experience was limited and engagement with formal accreditation processes was also inadequate.
- 20.Jiménez-Molina Á, Franco P, Martínez V, et al. Internet-Based Interventions for the Prevention and Treatment of Mental Disorders in Latin America: A Scoping Review. Front Psychiatry. 2019;10:664 Published 2019 Sep 13. doi: 10.3389/fpsyt.2019.00664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaonga NN, Morgan J. Common themes and emerging trends for the use of technology to support mental health and psychosocial well-being in limited resource settings: a review of the literature. Psychiatry Res. 2019. November;281:112594. doi: 10.1016/j.psychres.2019.112594 [DOI] [PubMed] [Google Scholar]
- 22.Naslund JA, Aschbrenner KA, Araya R, et al. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: a narrative review of the literature. Lancet Psychiatry. 2017;4(6):486–500. doi: 10.1016/S2215-0366(17)30096-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *23.Naslund JA, Gonsalves PP, Gruebner O, Pendse SR, Smith SL, Sharma A, Raviola G. Digital Innovations for Global Mental Health: Opportunities for Data Science, Task Sharing, and Early Intervention. Current Treatment Options in Psychiatry 2019;6(4):337 DOI 10.1007/s40501-019-00186-8 [DOI] [PMC free article] [PubMed] [Google Scholar]; * This paper describes three emerging areas where digital technology will play a prominent role in global mental health. The areas identified include supporting methods in data science to improve our understanding of mental health, enabling task shifting, and facilitating opportunities for earlier intervention in young people in low resource settings.
- 24.Thomas IF, Lawani AO, James BO. Effect of short message service reminders on clinic attendance among outpatients with psychosis at a psychiatric hospital in Nigeria. Psychiatr Serv. 2017;68:75–80. doi: 10.1176/appi.ps.201500514 [DOI] [PubMed] [Google Scholar]
- 25.Maiga DD. Intérêt de l’utilisation du téléphone mobile dans la réponse aux rendez-vous des patients atteints de psychoses aiguës fonctionnelles au service de psychiatrie de l’Hôpital national de Niamey. Inf Psychiatr. 2011;87:127–32. [Google Scholar]
- 26.Sibeko G, Temmingh H, Mall S, et al. Improving adherence in mental health service users with severe mental illness in South Africa: a pilot randomized controlled trial of a treatment partner and text message intervention vs. treatment as usual. BMC Res Notes. 2017; 10: 584. doi: 10.1186/s13104-017-2915-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- **27.Xu DR et al. Lay health supporters aided by mobile text messaging to improve adherence, symptoms, and functioning among people with schizophrenia in a resource-poor community in rural China (LEAN): A randomized controlled trial. PLoS Med. 2019. April 23;16(4):e1002785. doi: 10.1371/journal.pmed.1002785 [DOI] [PMC free article] [PubMed] [Google Scholar]; ** This study describes the first randomized controlled trial showing that text messaging coupled with lay health worker support can improve medication adherence, symptoms, and functioning among schizophrenia patients in community-based settings in China.
- 28.Fang C-x Ye M-j, Yang Y-f Chen S-l. Effects of daily short message reminder for preventing schizophrenia recrudescence. Nurs J Chin PLA. 2011;7:74–76. [Google Scholar]
- 29.Ozkan B, Erdem E, Ozsoy SD, Zararsiz G. Effect of psychoeducation and telepsychiatric follow up given to the caregiver of the schizophrenic patient on family burden, depression and expression of emotion. Pak J Med Sci. 2013;29:1122–127. doi: 10.12669/pjms.295.2613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen L, Li Z, Chen Y. Comparative study of relapse prevention in schizophrenia by network. J ClinPsychol Med. 2007;17:234–36. [Google Scholar]
- **31.Ben-Zeev D, Buck B, Kopelovich S, and Meller S. A technology-assisted life of recovery from psychosis. NPJ Schizophr. 2019. doi: 10.1038/s41537-019-0083-y [DOI] [PMC free article] [PubMed] [Google Scholar]; ** This perspective piece outlines examples of innovations in digital health that are designed for individuals with schizophrenia spectrum illness. It also provides a snapshot of how digital technologies can support a young adult’s efforts to manage this illness.
- 32.Deb Sinha K, Tuli A, Sood M, et al. Is India ready for mental health apps (MHApps)? A quantitative-qualitative exploration of caregivers’ perspective on smartphone-based solutions for managing severe mental illnesses in low resource settings. PLoS One. 2018; 13(9): e0203353. doi: 10.1371/journal.pone.0203353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yao H, Chen Jian-Hua, Xu Yi-Feng. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry. April 2020. DOI: 10.1016/S2215-0366(20)30090-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- **34.Li W, Yang Y, Liu ZH, et al. Progression of Mental Health Services during the COVID-19 Outbreak in China. Int J Biol Sci. 2020;16(10):1732–1738. Published 2020 Mar 15. doi: 10.7150/ijbs.45120 [DOI] [PMC free article] [PubMed] [Google Scholar]; ** This paper throws a spotlight on mental health issues during the COVID-19 outbreak in China and discusses the provision of clinical services for mental health patients with SMDs during the outbreak.Specific measures that have been adopted to provide mental health services during the outbreak are also reviewed and discussed.
- *35.Torous J, Jän Myrick K, Rauseo-Ricupero N, Firth J. Digital Mental Health and COVID-19: Using Technology Today to Accelerate the Curve on Access and Quality Tomorrow. JMIR Ment Health 2020;7(3):e18848 DOI: 10.2196/18848 [DOI] [PMC free article] [PubMed] [Google Scholar]; * This article discusses that the context of the COVID-19 pandemic has made digital mental health’s role in increasing access and quality clearer. However, workforce training, digital equity and a focus on high-quality evidence are presented as key focus areas to enhance the uptake of digital interventions.
- 36.Frasquilho D, Matos MG, Salonna F, et al. Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health. 2016;16:115 Published 2016 Feb 3. doi: 10.1186/s12889-016-2720-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- **37.Druss BG. Addressing the COVID-19 Pandemic in Populations With Serious Mental Illness. JAMA Psychiatry. Published online April 03, 2020. doi: 10.1001/jamapsychiatry.2020.0894 [DOI] [PubMed] [Google Scholar]; ** This paper outlines the disproportionate effect that the COVID-19 pandemic will have on populations with serious mental illness. The author also discusses four high-level strategies that span the clinical, policy and system-level platforms to mitigate the impact of the pandemic.
- 38.Hailemichael Y, Hanlon C, Tirfessa K, et al. Mental health problems and socioeconomic disadvantage: a controlled household study in rural Ethiopia. Int J Equity Health. 2019;18(1):121 Published 2019 Jul 31. doi: 10.1186/s12939-019-1020-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Twenge JM, Joiner TE, Rogers ML and Martin GN. Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time. Clin Psychol Sci. 2018;6(1):3–17. [Google Scholar]
- 40.Primack BA, Shensa A, Escobar-Viera CG, et al. Use of multiple social media platforms and symptoms of depression and anxiety: a nationally-representative study among US young adults. Comput Hum Behav. 2017;69:1–9. [Google Scholar]
- 41.Orben A, Przybylski AK. The association between adolescent well-being and digital technology use. Nat Hum Behav. 2019;3(2):173–82. [DOI] [PubMed] [Google Scholar]
- 42.Orben A, Dienlin T, Przybylski AK. Social media’s enduring effect on adolescent life satisfaction. Proc Natl Acad Sci. 2019;116(21):10226–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Firth J, et al. The “online brain”: how the Internet may be changing our cognition. World Psychiatry. 2019;18(2):119–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *44.Lipschitz J, Hogan Timothy P, Bauer Mark S, Mohr David C. Closing the Research-To-Practice Gap in Digital Psychiatry: The Need to Integrate Implementation Science. The Journal of Clinical Psychiatry. Vol 80, No 3. [DOI] [PubMed] [Google Scholar]; * This paper emphasizes that advancing mental health treatment for patients using digital technologies requires us to move beyond an almost exclusive focus on intervention effectiveness research and also factor in implementation research. This would involve studying how to integrate effective digital interventions into local systems and routine patient care.
- 45.Chancellor S, et al. A taxonomy of ethical tensions in inferring mental health states from social media in Proceedings of the Conference on Fairness, Accountability, and Transparency. 2019. ACM. [Google Scholar]


