Abstract
Background/objective
High-signal intensity changes in the glenohumeral joint capsule on T2-and proton density-weighted magnetic resonance imaging are known as characteristic finding that is often observed in patients with frozen shoulder. We investigated the associations between high-signal intensity changes in the joint capsule on magnetic resonance imaging and the presence of rotator cuff tears and shoulder symptoms in patients with shoulder pain.
Methods
The medical records of 230 patients with shoulder pain who underwent magnetic resonance imaging at our hospital were reviewed. Patients were divided into three groups according to the presence and/or degree of rotator cuff tears (none, partial, or complete). The frequency of high-signal intensity changes in the joint capsule and its relationship with shoulder symptoms and the severity of rotator cuff tears were assessed. By quantitatively evaluating the intensity on MRI, the ratio between the joint capsule and the long head of the biceps (HSIC ratio) was calculated and compared with 15 healthy subjects.
Results
High-signal intensity changes were diagnosed in 165 (72%) patients, and it was significantly associated with night pain and range of motion limitation (p < 0.01). High-signal intensity changes were present in 66 patients (70%) with no rotator cuff tears, in 69 (71%) with partial rotator cuff tears, and in 36 (80%) with complete rotator cuff tears, without differences in their occurrence (p = 0.60), but were significantly associated with night pain in all the groups (p < 0.01) without differences in tear severity (p = 0.63). The ratio in the high-signal intensity changes (HSIC) positive group was approximately six times higher than that in the HSIC-negative and control groups (P < 0.01). Multivariate logistic regression analysis revealed that night pain is significantly associated with high-signal intensity changes (p < 0.01).
Conclusion
Shoulder pain is a common and reliable clinical finding in patients with high–signal intensity changes, regardless of the presence and/or degree of rotator cuff tears, Such changes may indicate night pain and range of motion limitation in patients.
Keywords: Adhesive capsulitis, MRI, Shoulder joint, Rotator cuff injuries
Introduction
Range of motion (ROM) limitation is a characteristic symptom of shoulder joint disorder, along with motion pain and night pain (pain when lying either supine or laterally); e.g., frozen shoulder presenting with primary idiopathic stiff shoulder, occasionally known as adhesive capsulitis,1 causes both ROM limitation and night pain.2,3 The diagnosis of frozen shoulder has long been based on the comprehensive assessment of clinical findings and exclusion of other diseases with similar presentations.2,4 Recently, high-signal intensity changes (HSIC) in the glenohumeral joint capsule on T2-and proton density-weighted MRI were recently determined to have high sensitivity and specificity for the diagnosis of frozen shoulder with excellent inter-observer variability.5,6 Therefore, capsular signal intensity changes on magnetic resonance imaging (MRI) are carefully considered in patients with frozen shoulder.7,8
Rotator cuff injuries (tear) is a leading cause of shoulder pain along with night pain.9,10 The relationship between HSIC and rotator cuff tendon disease has not been studied to date. HSIC However, this finding remains to be investigated in relation to actual shoulder joint symptoms. We hypothesized that HSIC are relatively common finding in patients with rotator cuff tear (RCT), and HSIC that are identified on MRI are associated with night pain even in the patients with RCT.
This study investigated the occurrence of HSIC in patients with painful shoulder, reviewed the associations between HSIC in the glenohumeral joint capsule and clinical symptoms.
Materials and methods
Study design and participants
This retrospective cross-sectional study was conducted at our hospital from December 2014 to July 2016. We included patients with shoulder problems at their 30 years of age or older who consulted to the shoulder clinic at the hospital and were evaluated their shoulder by 3-T (3 T) MRI. Patients who had sports-related injuries, traumatic dislocations, collagen disease, or neoplastic lesions were excluded from this study. We compared shoulder symptoms according to the presence of RCT and HSIC on MRI. Additionally, a sample of 15 healthy and asymptomatic volunteers was used as a control group.
Ethical approval was obtained from our institution’s Research Ethics Committee (Ref: 15-J024).
Shoulder symptoms
Night pain was defined as the presence of pain in the supine or lateral position.10,11 Passive ROM was measured for shoulder forward flexion (FF), external rotation at 0° (ER1) and 90° (ER2), abduction, and internal rotation (IR). FF, ER1, and ER2 were measured with a goniometer by a shoulder consultant. IR was assessed at four levels: level 1, the buttocks; level 2, 5th to 3rd lumbar vertebrae; level 3, 3rd to 1st lumbar vertebrae; and level 4, thoracic spine and above. Muscular weakness was assessed by the manual muscle strength testing (MMT) of shoulder abduction, and external and IR was assessed by a shoulder consultant.
Evaluations of shoulder on MRI
The RCT and HSIC were diagnosed by both the board-certificated musculoskeletal radiologist and shoulder consultant. The consistency in diagnosis was statistically evaluated. When there was discrepancy in diagnosis between the orthopedic shoulder consultant and radiologist differed, the final diagnosis was reached by discussion. Fat-suppressed proton density- and T2-weighted MR images were made in diagonal–coronal and diagonal–sagittal planes, respectively (TR/TE = 2500/37, FOV 180 mm, section thickness 3 mm; 3 T unit, Magnetom Verio, Siemens, Erlangen, Germany). The signal intensity of the joint capsule (inferior glenohumeral ligament) was evaluated based on the signal intensity of the vertical portion of the long head of the biceps tendon (LHB).5 HSIC was considered positive if the intensity of in the joint capsule in either image was higher than that in the LHB and surrounding muscle fibers (Fig. 1, Fig. 2, Fig. 3). The inter-tester reliability of positive MRI findings between the shoulder consultant and musculoskeletal radiologist was assessed in 50 consecutive patients. Intra-tester reliability between the two examiners was similarly assessed at a 3-month interval.
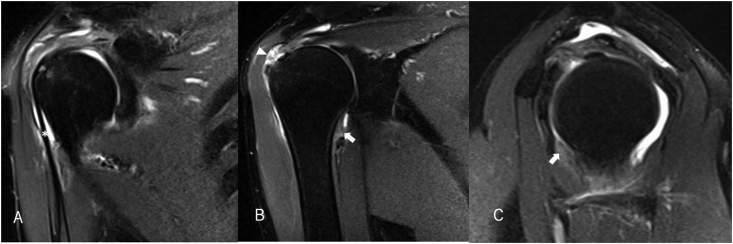
Fig. 1.
Proton density-weighted fat-suppressed images in the coronal plane (A, B) and T2-weighted images in the sagittal plane (C) of the left shoulder of a 52-year-old male revealed high-signal intensity changes (HSIC) in the joint capsule (arrow) without rotator cuff tear. Asterisk indicates the long head of the biceps tendon (LHB).
Fig. 2.
Proton density-weighted fat-suppressed images in the coronal plane (A, B) and T2-weighted images in the sagittal plane (C) of the right shoulder of a 54-year-old male revealed high-signal intensity changes (HSIC) (arrow) in the joint capsule with a partial-thickness bursal side tear in the supraspinatus muscle (arrowhead). Asterisk indicates LHB.
Fig. 3.
Proton density-weighted fat-suppressed images in the coronal plane (A, B) and T2-weighted images in the sagittal plane (C) of the right shoulder of a 61-year-old male revealed high-signal intensity changes (HSIC) (arrow) in the joint capsule with a full-thickness bursal side tear in the supraspinatus muscle (arrowhead). Asterisk indicates LHB.
By quantitatively evaluating the signal intensity on MRI, the ratio between the joint capsule and the LHB (HSIC ratio) was calculated and compared with 15 healthy subjects. A region of interest (ROI) was placed in the joint capsule (inferior glenohumeral ligament) and LHB tendon on the coronal section of fat-saturated proton-density weighted images in asymptomatic volunteers, patients with HSIC, and patients without HSIC (Fig. 4). The HSIC ratio was calculated as SJoint capsule/SLHB. Finally, the existence of HSIC was determined based on qualitative evaluation conducted via a consultation.
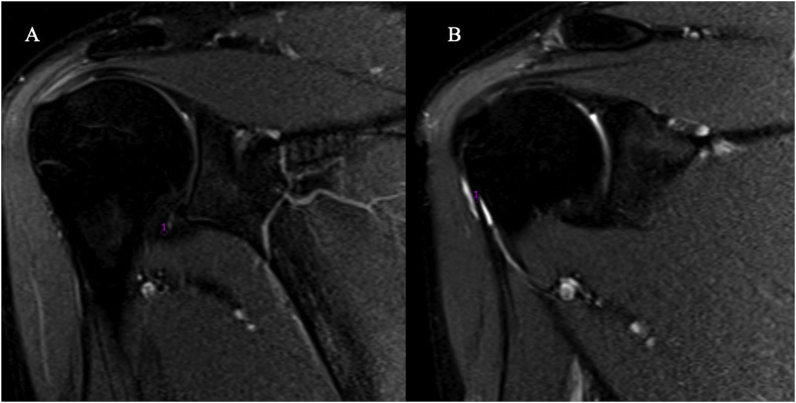
Fig. 4.
Measurement of the HSIC: Case of articular side partial thickness rotator cuff tear, 51-year-old male, Rt. shoulder. A ROI was placed in the joint capsule (A) and LHB tendon (B) on the coronal section of fat-saturated proton density-weighted fat-suppressed images in the coronal plane.
The same MRIs were used to divide the patients into three groups according to the presence and/or degree of rotator cuff tears (no RCT, partial RCT, or full RCT). The period from symptom onset to MRI investigation was also recorded.
Statistical analyses
In terms of diagnosis on MRI, intra- and inter-tester reproducibility was assessed based on the kappa values. Then, we compared patient’s demographics and shoulder symptoms between groups according to the presence of HISC and between groups according to the degree of RCT. After that, we examined the association between RCT and night pain, stratifying by degree of RCT Finally, we performed multivariate logistic regression to evaluate associated factors to HISC among demographics and symptoms, adjusting for variables which were clinically important or had significant results in bivariate analyses.
Statistical analyses were done with IBM® SPSS® Statistics Version 22.0 (SPSS, Inc., Chicago, IL). Chi-squared test, Mann-Whitney test, Kruskal-Wallis test, one-way analysis of variance with Bonferroni correction, and logistics regression analysis were used for analysis. Kappa values were used to assess intra– and inter–tester reproducibility. p < 0.05 was considered significant.
Results
Study population
In total 302 consecutive patients with shoulder problems, 28 with sports-related injuries, 22 with traumatic dislocations, 20 with collagen disease, and 2 with neoplastic lesions were excluded. On the other and 230 patients [108 (47%) males and 122 (53%) females; median age: 65 (37–81) years] were included in the study (Fig. 5). The groups were composed as follows: no RCT = 94 patients, partial RCT = 91 patients, and full RCT = 45 patients. The median period from the symptom onset to MRI evaluation was 6 (0–192) months.
Fig. 5.
Flow diagram of the study.
Association between HSIC and night pain and ROM
HSIC in the joint capsule were observed on MRI in 165 (72%) of the 230 patients and was significantly more prevalent in females (96/122 females vs. 69/108 males; p < 0.01). Night pain was significantly associated with positive HSIC findings (p < 0.01, Table 1), and passive ROM was significantly decreased in all directions in patients with HSIC (p < 0.01). Conversely, HSIC were not significantly associated with MMT. Synovial fluid was observed in the glenohumeral joint, subacromial space, and around the LHB and rotator interval in 191 patients (83%).
Table 1.
Relation between HSIC and night pain, ROM and MMT.
| Night pain, n (%) | Those without HSIC (n = ) |
Those with HSIC (n = ) |
Total |
p value |
|---|---|---|---|---|
| 27 (41.5) | 139 (84.2) | 166 (72.2) | <0.01 | |
| Range of motion, mean (SD) | ||||
| Forward flexion | 157 (14) | 141 (30) | <0.01 | |
| External rotation with arm at side | 52 (13) | 46 (16) | <0.01 | |
| External rotation with arm at 90° abduction | 75 (13) | 71 (18) | <0.01 | |
| Internal rotation | 2.8 (1.0) | 2.2 (1.0) | <0.01 | |
| Manual muscle testing, median (IQR) | ||||
| Abduction | 5 (4–5) | 5 (4–5) | 0.18 | |
| External rotation. | 5 (4–5) | 5 (5–5) | 0.46 | |
| Internal rotation. | 5 (5–5) | 5 (5–5) | 0.19 | |
ROM FF:forward flexion, ER1:external rotation with arm at side, ER2:external rotation with arm at 90° abduction, IR:internal rotation, MMT Abd: abduction, ER: external rotation.
ROM of IR indicated 4 levels, 1: the buttocks, 2: 5th to 3rd lumbar spine, 3: 3rd to 1st lumbar spine, 4: thoracic spine and above, SD: standard deviation, %:percentile.
HSIC: High signal intensity changes in the joint capsule in MRI.
Qualitative and quantitative evaluation of HSIC
The inter–tester reliability for detecting HSIC on MRI between the shoulder consultant and radiologist was 0.813. The intra–tester reliability was 0.833 and 0.882 for the shoulder consultant and radiologist, respectively.
HSIC–positive was found in 64 patients in the no RCT group, 65 patients in the partial RCT group, and 36 patients in the full RCT group (Table 2). HSIC–negative was found in 71 patients (no RCT = 30 patients, partial RCT = 26 patients, and full RCT = 15 patients, 38 males and 29 females, average age = 61 (32–74) years), and 71 patients with the same number of HSIC positive groups (40 males and 31 females, average age = 65 years: selected from early entry), and comparing the HSIC ratio of control cases, the HSIC positive group was significantly higher ratio (p < 0.001) (Fig. 6). There were also significant differences in each group. Also, in the comparison between positive HSIC and negative HSIC in each group, the negative and positive HSIC were 1.52 ± 0.76 vs 7.05 ± 2.98 for no RCT, 1.72 ± 1.02 vs 7.02 ± 3.67 for partial RCT, and 1.49 ± 0.47 vs 6.56 ± 2.83 for full RCT. Significant differences were recognized (p < 0.001).
Table 2.
Patient characteristics by rotator cuff diagnosis.
| Diagnosis |
No tear |
PTT |
FTT |
p-value |
|
|---|---|---|---|---|---|
| cases (%) | 94 (41%) | 91 (40%) | 45 (19%) | ||
| Age (year) (median, 25%–75%) | 63 (50–70) | 64 (55–71) | 70 (66–74)) | 0.03 | |
| Gender N (%) | male | 45 (48%) | 48 (53%) | 14 (31%) | 0.22 |
| female | 49 (52%) | 43 (47%) | 31 (69%) | ||
| Passive RO Mean ± SD | FF | 144 ± 29 | 149 ± 25 | 145 ± 29 | 0.33 |
| ER1 | 46 ± 15 | 48 ± 16 | 50 ± 14 | 0.50 | |
| ER2 | 71 ± 18 | 73 ± 19 | 77 ± 12 | 0.26 | |
| IR | 2.4 ± 1.1 | 2.6 ± 1.1 | 2.1 ± 0.9 | 0.07 | |
| HSIC N (%) | + | 64 (70%) | 65 (72%) | 36 (80%) | 0.43 |
| Night pain N (%) | + | 66 (70%) | 69 (76%) | 31 (69%) | 0.60 |
PTT = partial thickness rotator cuff tear, FTT = full thickness rotator cuff tear.
ROM FF:forward flexion, ER1:external rotation with arm at side, ER2:external rotation with arm at 90° abduction, IR:internal rotation, ROM of IR indicated 4 levels, 1: the buttocks, 2: 5th to 3rd lumbar spine, 3: 3rd to 1st lumbar spine, 4: thoracic spine and above.
HSIC: High signal intensity changes in the joint capsule on MRI.
Fig. 6.
Comparison of HSIC ratio. The ratio of positive HSIC was significantly higher (p < 0.001) than those of the other groups.
Patient characteristics on rotator cuff diagnosis
Patients were evaluated based on the presence and/or degree of RCT. Patients with full RCT were significantly older than those with no or partial RCT (p = 0.03; Table 2). No significant differences were noted in passive ROM according to rotator cuff diagnosis. No significant differences were observed in the frequency of HSIC in the joint capsule on MRI and night pain according to rotator cuff diagnosis.
HSIC were significantly associated with night pain in all groups (p < 0.01), but there were no differences between the groups in the strength of the associations (p = 0.63, Table 3). Logistic regression analysis identified only night pain as a significant factor associated with HSIC [p < 0.01, odds ratio: 5.98 (0.98–1.05), Table 4].
Table 3.
Comparison of the relation between HSIC and night pain within the rotator cuff injuries.
| Diagnosis | HSIC | P-value | Interaction P-value | |||
| – | + | |||||
| No tear 94 cases | night pain | - | 17 (18%) | 11 (12%) | <0.01 | |
| + | 13 (14%) | 53 (56%) | ||||
| PTT 91 cases | night pain | - | 15 (16%) | 7 (8%) | <0.01 | |
| + | 11 (12%) | 58 (64%) | ||||
| FTT 45 cases | night pain | - | 6 (13%) | 8 (18%) | <0.01 | 0.63 |
| + | 3 (7%) | 28 (62%) | ||||
PTT = partial thickness rotator cuff tear, FTT = full thickness rotator cuff tear.
HSIC: High signal intensity changes in the joint capsule on MRI.
Table 4.
Logistic regression analysis of factors related to high signal intensity change in joint capsule.
| Factor | Odds ratio (95% conf. interval) | p-value |
|---|---|---|
| Age | 1.01 (0.98–1.05) | 0.45 |
| Gender | 1.62 (0.80–3.28) | 0.18 |
| Night pain | 5.98 (2.95–12.15) | <0.01 |
| ROM: FF | 0.99 (0.97–1.02) | 0.51 |
| ROM: ER1 | 1.00 (0.97–1.04) | 0.88 |
| ROM: ER2 | 0.99 (0.95–1.02) | 0.44 |
| ROM: IR | 0.69 (0.45–1.04) | 0.08 |
| No teara | ||
| PTT | 1.20 (0.57–2.55) | 0.63 |
| FTT | 1.77 (0.63–4.92) | 0.28 |
FF:forward flexion, ER1:external rotation with arm at side, ER2:external rotation with arm at 90° abduction, IR:internal rotation.
ROM of IR indicated 4 levels, 1: the buttocks, 2: 5th to 3rd lumbar spine, 3: 3rd to 1st lumbar spine, 4: thoracic spine and above.
PTT = partial thickness rotator cuff tear, FTT = full thickness rotator cuff tear.
No tear was used as a comparison with other rotator cuff injuries (PTT and FTT).
Discussion
The current study demonstrated that HSIC in the joint capsule in fat-suppressed proton density- and T2-weighted images were present in 72% of patients with shoulder symptoms and that HSIC were associated with shoulder night pain in the shoulder and ROM limitation, regardless of the presence and/or severity of RCT. HSIC were clinically reliable finding that the capsule/LHB ratio in the HSIC-positive group was approximately six times higher than that in the HSIC-negative group and the control group. Logistic regression analysis revealed that HSIC are associated with night pain.
Capsular signal intensity changes on MRI are characteristic findings in patients with frozen shoulder.5,6 Clinically, frozen shoulder presentation is classified into three distinct stages: painful (freezing), frozen, and thawing.4,5,12 Synovial proliferation and hypervascular changes as an inflammatory reaction in joint capsule are typical of the initial stage, whereas fibrosis is typical of the later stages of the disease.4,12 Okuno et al. has reported that abnormal neovessels at rotator interval were found in all patients with frozen shoulder, along with improved night pain control with catheter embolization of the newly formed vessels.13 Also, using Doppler ultrasonography, anterior humeral circumflex artery hemodynamics appears to be a pathology related to night pain in patients with rotator cuff tear and normal subjects.10 Once tissue damage of the joint capsule is induced by causes such as ischemia, injured tendons and ligaments should be managed according to a prescribed tissue repair process.14 Generally, soft tissue damage is manifested by an inflammatory response with resultant hematoma and neutrophil infiltration.14 Fibroblastic proliferation subsequently occurs. Finally, collagen remodeling takes place at 6–12 months after injury. During the such a soft tissue healing process in the joint capsules, posture changes—such as changing from the standing position to the supine position—with rotation induce extensive stress to the joint capsule. This may be recognized as “night pain.” Although the cause of HSIC of the joint capsule is still unclear, HSIC may reflect soft tissue damage and its repair process.
Furthermore, ROM limitation was associated with HSIC on univariate analysis, but not on logistic regression analysis. Hagiwara et al. found that the expression of genes related to inflammation and fibrosis of the joint capsule is significant findings in frozen shoulder, and that chondrogenesis has a critical role in the pathogenesis of frozen shoulder.7 It is likely that the ROM limitation that is associated with HSIC is a result of pain caused by inflammation of the joint capsule, since fibrosis and chondrogenesis changes of the joint capsule may shows low signal intensity change in MRI findings. Therefore, it is theorized that HSIC only has a subtle statistical relationship statistically with the cause of limitation of joint mobility.
The frequency of HSIC in the joint capsule did not differ according to the degree of RCT. Yamaguchi et al. and Dunn et al. reported that the presence and degree of RCT have little association with shoulder pain and ROM.15,16 HSIC findings in the current study suggest that these symptoms are caused by capsular pathology rather than rotator cuff pathology. Night pain and ROM limitation typically abate over time with conservative treatment.17 Non-surgical treatment is an attractive option, regardless of RCT, because night pain and ROM limitation as symptoms of frozen shoulder may be an independent pathological condition.17,18
Limitations
This study has several limitations. First, though consecutive patients who visited the shoulder clinic at our hospital were enrolled to minimize selection bias, it is possible that confounding factors were not comprehensively examined because of the nature of retrospective reviews of medical records.19,20
Second, HSIC in the joint capsule on MRI were classified as frozen shoulder based on the literature. However, HSIC were identified in 27 (12%) patients with night pain, whereas they were not identified in 26 (11%) without night pain. Therefore, studies clarifying the duration from the onset of shoulder symptoms to HSIC appearance and disappearance are warranted.
In the future, assessing the relationship between HSIC severity and clinical symptoms, as well as the degree and location of joint capsule thickening, will enhance the understanding of the relationship between this change and pathology. A longitudinal assessment of how HSIC changes over time would be interesting to assess different clinical phases of frozen shoulder.
Conclusion
HSIC is a reliable clinical finding that was common in patients with shoulder pain, regardless of the presence and/or degree of rotator cuff tears, and can be considered as an indicator of night pain and range of motion limitation.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
AT and TN performed data collection and each contributed to sections of the manuscript.AT and DK were responsible for statistical analysis. WM, BBP and NK were responsible for generation of the research question and implementation of the study. Each was involved in writing and editing of the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was reviewed and approved by the Research Ethics Committee of St. Luke’s International Hospital (Ref: 15-J024).
Declaration of competing interest
All authors report no competing interests. None of the authors have financial or institutional disclosures to report related to the research in this paper.
Acknowledgements
The authors are deeply grateful for the editorial assistance given by Kay Daugherty, Campbell Foundation, Memphis TN.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.asmart.2020.06.001.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Bain G.I., Clitherow D.S. The pathogenesis and classification of shoulder stiffness. In: Itoi E., Arce G., Bain G.L., editors. Shoulder Stiffness. Springer; New York, USA: 2015. pp. 3–20. [Google Scholar]
- 2.Brue S., Valentin A., Forssblad M., Werner S., Mikkelsen C., Cerulli G. Idiopathic adhesive capsulitis of the shoulder: a review. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):1048–1054. doi: 10.1007/s00167-007-0291-2. Aug. PubMed PMID: 17333122. Epub 2007/03/03. [DOI] [PubMed] [Google Scholar]
- 3.Mengiardi B., Pfirrmann C.W., Gerber C., Hodler J., Zanetti M. Frozen shoulder: MR arthrographic findings. Radiology. 2004;233(2):486–492. doi: 10.1148/radiol.2332031219. Nov. PubMed PMID: 15358849. Epub 2004/09/11. [DOI] [PubMed] [Google Scholar]
- 4.Neviaser A.S., Hannafin J.A. Adhesive capsulitis: a review of current treatment. Am J Sports Med. 2010;38(11):2346–2356. doi: 10.1177/0363546509348048. Nov. PubMed PMID: 20110457. Epub 2010/01/30. [DOI] [PubMed] [Google Scholar]
- 5.Gondim Teixeira P.A., Balaj C., Chanson A., Lecocq S., Louis M., Blum A. Adhesive capsulitis of the shoulder: value of inferior glenohumeral ligament signal changes on T2-weighted fat-saturated images. AJR Am J Roentgenol. 2012;198(6):W589–W596. doi: 10.2214/AJR.11.7453. Jun. PubMed PMID: 22623575. Epub 2012/05/25. [DOI] [PubMed] [Google Scholar]
- 6.Sofka C.M., Ciavarra G.A., Hannafin J.A., Cordasco F.A., Potter H.G. Magnetic resonance imaging of adhesive capsulitis: correlation with clinical staging. HSS J. 2008;4(2):164–169. doi: 10.1007/s11420-008-9088-1. Sep. PubMed PMID: 18815860. Pubmed Central PMCID: PMC2553174. Epub 2008/09/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hagiwara Y., Ando A., Onoda Y. Coexistence of fibrotic and chondrogenic process in the capsule of idiopathic frozen shoulders. Osteoarthritis Cartilage. 2012;20(3):241–249. doi: 10.1016/j.joca.2011.12.008. Mar. PubMed PMID: 22233812. Epub 2012/01/12. [DOI] [PubMed] [Google Scholar]
- 8.Sridharan R., Engle M.P., Garg N., Wei W., Amini B. Focal uptake at the rotator interval or inferior capsule of shoulder on (18)F-FDG PET/CT is associated with adhesive capsulitis. Skeletal Radiol. 2017;46(4):533–538. doi: 10.1007/s00256-017-2587-8. Apr. PubMed PMID: 28161721. Pubmed Central PMCID: PMC5381154. Epub 2017/02/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitchell C., Adebajo A., Hay E., Carr A. Shoulder pain: diagnosis and management in primary care. BMJ. 2005;331(7525):1124–1128. doi: 10.1136/bmj.331.7525.1124. Nov 12. PubMed PMID: 16282408. Pubmed Central PMCID: PMC1283277. Epub 2005/11/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Terabayashi N., Watanabe T., Matsumoto K. Increased blood flow in the anterior humeral circumflex artery correlates with night pain in patients with rotator cuff tear. J Orthop Sci. 2014;19(5):744–749. doi: 10.1007/s00776-014-0604-5. Sep. PubMed PMID: 25069807. Epub 2014/07/30. [DOI] [PubMed] [Google Scholar]
- 11.Codman E.A. Thomas; 1934. The Shoulder. [Google Scholar]
- 12.Neviaser R.J., Neviaser T.J. The frozen shoulder. Diagnosis and management. Clin Orthop Relat Res. 1987;Oct(223):59–64. PubMed PMID: 3652593. Epub 1987/10/01. [PubMed] [Google Scholar]
- 13.Okuno Y., Oguro S., Iwamoto W., Miyamoto T., Ikegami H., Matsumura N. Short-term results of transcatheter arterial embolization for abnormal neovessels in patients with adhesive capsulitis: a pilot study. J Shoulder Elbow Surg. 2014;23(9):e199–206. doi: 10.1016/j.jse.2013.12.014. Sep. PubMed PMID: 24618195. Epub 2014/03/13. [DOI] [PubMed] [Google Scholar]
- 14.Eming S.A., Wynn T.A., Martin P. Inflammation and metabolism in tissue repair and regeneration. Science. 2017;356(6342):1026–1030. doi: 10.1126/science.aam7928. Jun 9. PubMed PMID: 28596335. Epub 2017/06/10. [DOI] [PubMed] [Google Scholar]
- 15.Dunn W.R., Kuhn J.E., Sanders R. Symptoms of pain do not correlate with rotator cuff tear severity: a cross-sectional study of 393 patients with a symptomatic atraumatic full-thickness rotator cuff tear. J Bone Joint Surg Am. 2014;96(10):793–800. doi: 10.2106/JBJS.L.01304. May 21. PubMed PMID: 24875019. Pubmed Central PMCID: PMC4018774. Epub 2014/05/31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamaguchi K., Ditsios K., Middleton W.D., Hildebolt C.F., Galatz L.M., Teefey S.A. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88(8):1699–1704. doi: 10.2106/JBJS.E.00835. Aug. PubMed PMID: 16882890. Epub 2006/08/03. [DOI] [PubMed] [Google Scholar]
- 17.Lorbach O., Anagnostakos K., Scherf C., Seil R., Kohn D., Pape D. Nonoperative management of adhesive capsulitis of the shoulder: oral cortisone application versus intra-articular cortisone injections. J Shoulder Elbow Surg. 2010;19(2):172–179. doi: 10.1016/j.jse.2009.06.013. Mar. PubMed PMID: 19800262. Epub 2009/10/06. [DOI] [PubMed] [Google Scholar]
- 18.Ueda Y, Sugaya H, Takahashi N, et al. Rotator cuff lesions in patients with stiff shoulders: a prospective analysis of 379 shoulders. J Bone Joint Surg Am. 2015 Aug 5;97(15):1233-1237. PubMed PMID: 26246257. Epub 2015/08/08. [DOI] [PubMed]
- 19.Liem D., Bartl C., Lichtenberg S., Magosch P., Habermeyer P. Clinical outcome and tendon integrity of arthroscopic versus mini-open supraspinatus tendon repair: a magnetic resonance imaging-controlled matched-pair analysis. Arthroscopy. 2007;23(5):514–521. doi: 10.1016/j.arthro.2006.12.028. May. PubMed PMID: 17478283. Epub 2007/05/05. [DOI] [PubMed] [Google Scholar]
- 20.Galatz L.M., Ball C.M., Teefey S.A., Middleton W.D., Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-A(2):219–224. doi: 10.2106/00004623-200402000-00002. Feb. PubMed PMID: 14960664. Epub 2004/02/13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.