Abstract
Purpose
The following case describes a 28-year old African American male who presented with squamous cell carcinoma of the lacrimal duct. Despite its size and location, his tumor showed complete resolution with non-surgical treatment.
Observations
The patient presented with a 4-month history of dacryocystitis-like symptoms in the right eye, with no prior medical history and a history of tobacco smoking. Pathology indicated that SCC arose as nests within a benign sinonasal inverted papilloma. He received cisplatin chemotherapy and radiotherapy with tumor resolution in 4 months. Several months after the end of treatment, he experienced irreversible visual deterioration which led to enucleation of the right eye. The patient has remained in remission for 4 years following the treatment.
Conclusions
The complete resolution of the mass with non-surgical management supports the most recent literature endorsing a multidisciplinary approach for localized tumors. Our patient is the only African American identified in the literature and the youngest reported patient to present with this tumor. Most case studies have not emphasized race, ethnicity and demographics, although it is known that morbidity in malignancy is impacted by these factors.
Keywords: Lacrimal apparatus diseases, Eye neoplasms, Squamous cell carcinoma, Nasolacrimal duct pathology
1. Case report
A 28-year-old African American male with no known medical history presented to the emergency department with chief complaint of a progressively growing right eyelid mass over the course of 4 months. He initially presented to his PCP and was managed for what was thought to be a chalazion. He received multiple rounds of antibiotics and warm compresses with no resolution. After sustaining a mild trauma to the mass, he developed bleeding followed by intermittent nasal discharge for several weeks. This prompted him to present to our ED for further evaluation. In the ED, he reported no medications or past ocular history. Risk factors included family history of malignancy, and personal history of tobacco abuse.
On ophthalmic exam, best corrected visual acuity of 20/40 in the right eye and 20/20 in the left eye. Pupils, extraocular motility and intraocular pressure were all found to be normal OU. External examination of the right eye showed a large, firm, nodular mass along the medial aspect of the lower lid extending to the upper lid, associated with several indurated areas of exposed beefy red tissue (Fig. 1). No other findings were noted on anterior and posterior segment exam OU. The general physical exam was found to be normal. Labs showed moderate leukocytosis and mild microcytic anemia. HIV testing was negative.
Fig. 1.
Gross image demonstrating size of tumor at presentation.
The patient was admitted and underwent imaging on the day after admission. Noncontrast CT scan of the head and orbit showed a 3.2 cm × 3.4 cm heterogeneous enhancing soft tissue mass in the anterior medial right orbit (Fig. 2). The mass displaced the right globe laterally, abutting the anterior medial rectus muscle at its insertion into the globe. It also expanded and extended through the nasolacrimal duct with extension into the inferior nasal turbinate. No cortical destruction was noted.
Fig. 2.
CT scan with contrast showing a soft-tissue right orbital mass.
Biopsy and debulking took place on hospital day 2. Superficial surgical exploration showed it to have several large nodular lesions that were friable, highly vascularized, with purulent drainage. Pathology initially reported an inverted papilloma with mild focal dysplasia and cytologic atypia in some regions. Later, additional deeper sections (Fig. 3, Fig. 4) showed small nests of keratinized squamous epithelium infiltrating the stroma, confirming the diagnosis of secondary squamous cell carcinoma. The tumor was found to invade through subcutaneous soft tissues and focally ulcerated the overlying skin. In some areas the lesion had a cytology and architecture consistent with inverted/endophytic papilloma. Materials were also sent to Johns Hopkins Hospital for expert opinion and they concurred with the above diagnosis. After further work-up, including PET scan, the tumor was staged as T4bN0M0. Strong consideration was given to performing excisional surgery, given the size of the mass. Instead, a decision was made to pursue chemotherapy and radiation primarily due to patient preference.
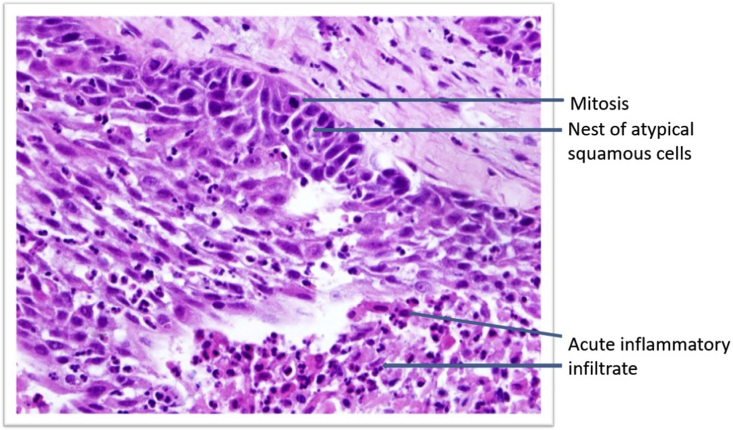
Fig. 3.
(Above) Atypical squamous epthelial cells infiltrating the stroma and the subcutaneous tissue. Mitotic figures are seen in addition to acute inflammatory cell infiltrate. Well-differentiated.
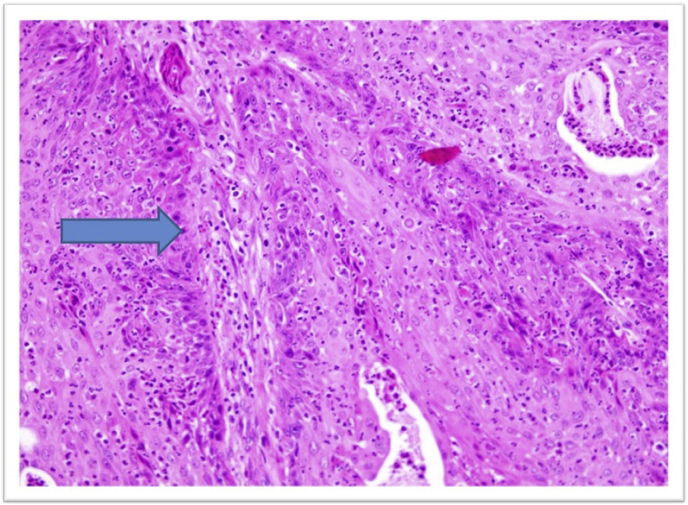
Fig. 4.
The arrow points to the transformation of the squamous cells lining the periphery to become atypical neoplastic cells; i.e. increased N/C ratio, pleomorphism and presence of mitotic figures.
The patient received Cisplatin for 3 cycles over the course of 3 months. His radiation regimen consisted of an intensity-modulated radiotherapy (IMRT) with an initial dose of 50 Gy (Gy) in 25 fractions. By month two, the mass was found to have been reduced to 1.5 cm × 1.4 cm. Thereafter, he received an additional reduced dose of 10 Gy in 5 fractions, for a total of 60 Gy in 30 fractions over 61 days. The tumor completely resolved after 4 months as seen clinically and on MRI. Radiation was discontinued at 60 Gy, largely due to worsening eye discomfort.
Several months after completion of his 4-month treatment, the patient returned to the ophthalmology department with severe eye pain, hand motion vision with a large epithelial defect and cicatricial membrane formation in the inferior fornix of the right eye. Despite management for several months with Prokera grafts and bandage contact lenses, he continued to have recurrent epithelial defects, elevated intraocular pressure due to neovascular glaucoma, severe eye pain and progression to phthisis bulbi with light perception vision. Thus, comfort care measures were taken, and enucleation was performed with implantation of a prosthesis. The patient did well following the enucleation. He has remained in remission since the completion of his radiation and chemotherapy for 4 years.
2. Discussion
Cases of squamous cell carcinoma of the lacrimal sac have been reported all over the world.1, 2, 3, 4 Several reports specific to SCC are available,4,5 as are several literature reviews referring to the more general category of epithelial neoplasms of the lacrimal sac.3,6,7 An estimated 300–775 lacrimal sac tumors have been reported in the literature.1,4,7 They are classified into epithelial and non-epithelial tumors, and studies estimate the percentage of epithelial tumors to be anywhere from 25% to 73% of total cases.1,3 Squamous cell carcinomas appear to be the most common variant, and may arise as primary or secondary tumors.
Sinonasal inverted papilloma (SIP), from which the SCC in our patient appears to have arisen, is uncommon, though benign. It is prone to recurrence, local invasion and malignant transformation, as occurred in this case.8 SIP has been associated with HPV infection, occupational exposure to smoke, dust and aerosols, chronic inflammation and tobacco exposure.8 Our patient was a smoker, but the length and amount of tobacco exposure is unknown.
Overall, given the relative rarity of lacrimal sac tumors, demographic correlation (i.e. race, gender, age group) has not been well-established. A recent retrospective study of 65 patients in Taiwan suggests that patients with malignant lacrimal sac tumors had a younger mean age at the time of diagnosis than patients with benign and secondary lacrimal sac tumors. It also indicated that primary malignant and secondary malignant tumors have higher prevalence in females and males respectively.9 This corresponds with our findings; our patient is male with a secondary, malignant SCC.
Lacrimal sac tumors typically present with symptoms of lacrimal duct obstruction and can easily be misdiagnosed as dacryocystitis during initial encounters.5 To differentiate, inflammation in chronic dacryocystitis often occurs below the medial canthal tendon whereas lacrimal sac tumors may occur above or below the tendon.10 Presenting symptoms include pain and epiphora (with or without spontaneous retrocanalicular bleeding). Patients may also experience a palpable canthal mass, mucocele and/or punctal regurgitation. Lesions can extend into the deep soft tissue of the orbit and affect adjoining structures, including the lacrimal sac fossa and parts of maxillary bone and ethmoidal sinuses. This can cause patients to develop nasal obstruction and bleeding.3
Mortality rates may vary amongst lacrimal sac tumors, depending on tumor histology and spread to local lymph nodes. In our patient, the mass extended directly to adjoining structures. In an analysis of 82 lacrimal sac tumors, direct extension was the mode of tumor spread in 89% of cases, and metastasis to local lymph nodes occurred in 27% of patients.6 Seeding may occur from the paranasal sinus or nasal cavity and signs of malignancy may appear on imaging in the form of bone erosion or infiltrative lesions. When a lacrimal sac tumor extends beyond the lacrimal duct, exenteration, lateral rhinotomy, and cervical lymph node dissection are generally advised.
Low rates of recurrence have been observed with globe-sparing treatments such as chemotherapy and radiotherapy.3 Cisplatin is a common regimen for lacrimal sac tumors and was used as the primary treatment for our patient. The use of chemotherapy has traditionally been reserved for inoperable tumors or during postoperative radiotherapy but has now become more commonplace.
Our patient responded very well to chemoradiation and experienced a complete resolution of his tumor. This is consistent with the course of other tumors involving the nasolacrimal drainage system.6 In a 2018 case series of 90 patients in Shanghai, physicians used a multidisciplinary approach similar to ours.2 They found that patients tolerated radiotherapy well, with multiple benefits related to preventing recurrence and metastasis. However, researchers found it a challenge to aim precisely and shield adequately during radiation, as was the case with our patient.
Ionizing radiation is known to cause dose-dependent side effects; complications increase steeply with doses of 40 Gy and above.11 External beam radiation is more likely to cause side effects such as xerophthalmia, blepharitis, loss of lashes and cataracts. With protective shielding, posterior segment complications are less likely, but still occur. In a study analyzing external beam irradiation of nasal and paranasal cancer, 8 of 25 patients (9 of 43 eyes) experienced complications such as neovascular glaucoma, retinopathy and central retinal artery occlusion. Late retinal complications tended to appear at a median post-treatment time of 22 months and in patients with higher doses (50 Gy+) of radiation.12 With cisplatin, dose-dependent ocular toxicity may occur. It is generally mild, occurring after 2–3 cycles. At higher doses, the risk of optic nerve and retinal toxicity increases significantly.13
As mentioned, previous reports rarely mention race and demographics in regard to SCC. African Americans have the highest death rate of any racial and ethnic group in the US for most cancers.14 Moreover, African Americans are more likely to experience delays in diagnosis and treatment of cancer, contributing to higher mortality rates.15 Our patient is the only African American identified in the literature and the youngest reported patient to present with SCC of the lacrimal duct, with most patients being 45+ years old at the time of presentation. Although he presented with a large mass, he showed complete resolution of his tumor with non-surgical treatment and has remained in remission.
2.1. Patient consent
Written consent was obtained from patient to use photographs for scientific purposes. No sensitive details are shared, and images and photographs used have no identifying details.
Funding
No funding was received for this work.
Intellectual property
We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
Research ethics
We further confirm that any aspect of the work covered in this manuscript that has involved human patients has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
Written consent to publish potentially identifying information, such as details or the case and photographs, was obtained from the patient(s) or their legal guardian(s).
Declaration of competing interest
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Acknowledgements
No acknowledgements. The authors have no conflicts of interest, financial disclosures, funding or grant support. All authors attest that they meet the current ICMJE criteria for Authorship.
Contributor Information
Nathan Kanyinda, Email: Nkanyinda15@gmail.com.
Simran Soni, Email: simran.soni@bison.howard.edu.
References
- 1.Parmar D.N., Rose G.E. Management of lacrimal sac tumours. Eye. 2003;17:599–606. doi: 10.1038/sj.eye.6700516. [DOI] [PubMed] [Google Scholar]
- 2.Song X., Wang J., Wang S., Wang W., Wang S., Zhu W. Clinical analysis of 90 cases of malignant lacrimal sac tumor. Graefes Arch Clin Exp Ophthalmol. 2018;256(7):1333–1338. doi: 10.1007/s00417-018-3962-4. [DOI] [PubMed] [Google Scholar]
- 3.El-Sawy T, Frank SJ, Hanna E, et al. Multidisciplinary management of lacrimal sac/nasolacrimal duct carcinomas. Ophthalmic Plast Reconstr Surg. 29(6):454-457. doi:10.1097/IOP.0b013e31829f3a73. [DOI] [PMC free article] [PubMed]
- 4.Siriwanasan R., Puranajoti S., Ittipunkul N., Martin T. Squamous cell carcinoma of the lacrimal sac: a case report. J Med Assoc Thail. 2004;87(1):106–110. [PubMed] [Google Scholar]
- 5.Rahmi D., Ceyda B., Mehmet B., Sibel Ö., Ismail A. Squamous cell carcinoma of the lacrimal sac: a case and literature review. Ophthalmol Res An Int J. 2014;2(6):431–439. doi: 10.9734/or/2014/9904. [DOI] [Google Scholar]
- 6.Kim H., Shields C., Langer P. Lacrimal sac tumors: diagnosis and treatment. In: Nesi F., Calvano C.J., Gladstone G.J., Black E.H., editors. Smith and Nesi's Ophthalmic and Reconstructive Surgery. third ed. Springer; New York, NY: 2011. pp. 609–614. [Google Scholar]
- 7.Krishna Y., Coupland S.E. Lacrimal sac tumors - a review. Asia-Pacific J Ophthalmol. 2017;6(2):173–178. doi: 10.22608/APO.201713. [DOI] [PubMed] [Google Scholar]
- 8.Wang M.-J., Noel J.E. Etiology of sinonasal inverted papilloma: a narrative review. World J Otorhinolaryngol - head neck Surg. 2016;3(1):54–58. doi: 10.1016/j.wjorl.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuo C.-Y., Tsai C.-C., Kao S.-C., Hsu W.-M., Jui-Ling Liu C. Comparison of clinical features and treatment outcome in benign and malignant lacrimal sac tumors. Kim KG. BioMed Res Int. 2020;2020:3545839. doi: 10.1155/2020/3545839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shields J.A., Shields C.L. Conjunctival, and Orbital Tumors : Atlas and Textbook. second ed. Lippincott Wiliams & Wilkins; Philadelphia: 2008. Shields JAA of eyelid, conjunctival tumors, Shields JAA of orbital tumors, Ovid Technologies I. Eyelid. [Google Scholar]
- 11.Parsons J.T., Fitzgerald C.R., Ian Hood C., Ellingwood K.E., Bova F.J., Million R.R. The effects of irradiation on the eye and optic nerve. Int J Radiat Oncol Biol Phys. 1983;9(5):609–622. doi: 10.1016/0360-3016(83)90225-0. [DOI] [PubMed] [Google Scholar]
- 12.Takeda A., Shigematsu N., Suzuki S. Late retinal complications of radiation therapy for nasal and paranasal malignancies: relationship between irradiated-dose area and severity. Int J Radiat Oncol Biol Phys. 1999;44(3):599–605. doi: 10.1016/S0360-3016(99)00057-7. [DOI] [PubMed] [Google Scholar]
- 13.Miller N.R., Walsh F.B., Hoyt W.F. Walsh and Hoyt's Clinical Neuro-Ophthalmology. sixth ed. Lippincott Williams and Wilkins; Philadelphia: 2005. Complications of cancer therapy. [Google Scholar]
- 14.DeSantis C.E., Miller K.D., Goding Sauer A., Jemal A., Siegel R.L. Cancer statistics for african Americans. CA A Cancer J Clin. 2019;69(3):211–233. doi: 10.3322/caac.21555. 2019. [DOI] [PubMed] [Google Scholar]
- 15.George P., Chandwani S., Gabel M. Diagnosis and surgical delays in African American and white women with early-stage breast cancer. J Womens Health (Larchmt) 2015;24(3):209–217. doi: 10.1089/jwh.2014.4773. [DOI] [PMC free article] [PubMed] [Google Scholar]