Abstract
Background:
Co-use of tobacco and cannabis has been associated with greater dependence on and lower quit rates for both substances. Tobacco/cannabis co-use among individuals with substance use disorders (SUDs), a population with high rates of cigarette smoking, may hinder the effectiveness of smoking cessation interventions. We examined rates of lifetime (i.e., ever vs. never) cannabis use among current cigarette smokers in SUD treatment, and we identified the subgroup who had used tobacco and cannabis together in the form of blunts and/or spliffs. We then examined variables associated with lifetime use of blunts and/or spliffs.
Methods:
We surveyed 562 clients in 20 residential SUD treatment programs in California, USA, in 2019. Measures included demographics, lifetime use of any cannabis product, lifetime use of blunt/spliffs, patterns of tobacco use, and smoking cessation-related questions. We asked current cigarette smokers who also reported lifetime cannabis use whether they had ever used blunts and/or spliffs. We then assessed relationships of demographic, tobacco use, use of cannabis/tetrahydrocannabinol (THC) in e-cigarettes/vape pens, and smoking cessation-related variables with ever use versus never use of blunts/spliffs.
Results:
Among 340 current cigarette smokers, 93.2% (n=317) reported lifetime use of any cannabis product. Among current cigarette smokers with lifetime cannabis use, 64.4% reported lifetime blunt/spliff use. Compared to those who had never used blunts/spliffs, lifetime blunt/spliff users were more likely to be younger (OR = 0.93, 95% CI 0.90–0.95), more likely to report lifetime use of cigars/cigarillos (OR = 2.95, CI .1.37–6.32), and to have ever used cannabis/THC in e-cigarettes/vape pens (OR = 4.26, CI 1.54–11.80). They were less often ready to quit smoking within 30 days (OR = 0.37, CI 0.23–0.60), but more likely to want help with smoking cessation (OR = 2.39, CI 1.52–3.77).
Conclusion:
Current cigarette smokers in SUD treatment reported a high prevalence of lifetime cannabis use. Smokers with a history of blunt/spliff use were more likely to report lifetime use of e-cigarettes/vape pens for cannabis/THC delivery. They wanted help to quit smoking, but felt less prepared to quit in the next 30 days. Cannabis co-use may warrant clinicians’ attention when providing smoking cessation interventions during SUD treatment.
Keywords: Tobacco, Cannabis, Blunts/spliffs, Substance use, Smoking cessation
1. Introduction
Rates of co-use of cannabis and tobacco are high among smokers in the general population (Schauer, Berg, Kegler, Donovan, & Windle, 2015a) and have been increasing, particularly in states with legalized medical and/or recreational cannabis use (Goodwin et al., 2018; Wang & Cataldo, 2016). Studies have found co-use of tobacco and cannabis to be associated with higher rates of dependence, more difficulty quitting, and higher relapse rates relative to single use of each substance (McClure, Tomko, et al., 2018; Schauer, King, & McAfee, 2017; Voci, Zawertailo, Baliunas, Masood, & Selby, 2020; Weinberger, Platt, Copeland, & Goodwin, 2018). Co-use includes sequential use of cannabis and tobacco as well as co-administration in the form of blunts (i.e., cannabis rolled in cigar wrappers) or spliffs (i.e., cannabis and tobacco rolled together in a joint). Studies of co-administration have reported higher rates of use and poorer psychosocial functioning than use of either substance alone (Tucker et al., 2019), higher rates of dependence for both substances (Fairman, 2015; Ream, Benoit, Johnson, & Dunlap, 2008; Schauer, Rosenberry, & Peters, 2017; Timberlake, 2009) and greater lifetime use of tobacco and illicit drugs (Montgomery & Mantey, 2017).
Individuals with substance use disorders (SUDs) smoke tobacco at rates much higher than the general population. In a national sample of clients enrolled in SUD treatment programs in 2014–2015, 77.9% were current cigarette smokers (Guydish, Tajima, et al., 2016). Efforts to address smoking in SUD treatment over the past thirty years at regulatory, policy, and treatment program levels have achieved modest gains (Apollonio, Philipps, & Bero, 2016; Skelton et al., 2018; Thurgood, McNeill, Clark-Carter, & Brose, 2016). Nevertheless, unlike the dramatic decrease in smoking within the general population, smoking rates among those with SUDs remain high (Weinberger, Gbedemah, et al., 2018). Co-use of tobacco and cannabis, particularly blunt/spliff use, may hinder the effectiveness of smoking cessation interventions delivered in SUD treatment. Yet blunt/spliff use may not be addressed when assessing tobacco use in SUD treatment, missing both the additional tobacco/nicotine exposure that occurs through these methods of administration, and identification of a use pattern that may decrease the probability of successful smoking cessation. We did not identify any studies that examined cannabis/tobacco co-use among smokers in treatment for SUDs other than cannabis use disorder (CUD). Among cannabis treatment studies, findings indicate tobacco co-use is associated with poorer cannabis treatment outcomes (Gray et al., 2017), that moderate/high nicotine dependence is associated with increases in smoking after CUD treatment (McClure, Baker, et al., 2018), and that treatment interventions aimed at both cannabis and tobacco cessation may have some efficacy in reducing cannabis use, but evidence is weaker for tobacco cessation (Walsh, McNeill, Purssell, & Duaso, 2020).
We designed the current study to address the research gap regarding cannabis/tobacco co-use among persons with any SUDs. We examined rates of lifetime cannabis use and lifetime use of blunts and/or spliffs among smokers in residential treatment programs in California. We then examined differences between current cigarette smokers reporting lifetime blunt/spliff use and current cigarette smokers reporting never having used blunt/spliffs on variables including demographic characteristics; smoking severity; use of other tobacco products; use of e-cigarettes/vape pens, including e-cigarettes/vape pens for cannabis/THC delivery; and variables associated with smoking cessation.
2. Methods
2.1. Program selection and participants
This study surveyed 562 clients from 20 residential SUD treatment programs located in California, USA, in 2019. We combined data from three ongoing studies for this analysis. There were 7 programs in the first study, 9 in the second, and 4 in the third. Eligible programs in the first study had a minimum 20-bed capacity and had applied to participate in a policy development intervention that the University of California San Francisco (UCSF) Smoking Cessation Leadership Center provided. In study two, eligible programs were those expressing interest in creating tobacco-free grounds policies. The third study sought to improve tobacco intervention in four residential SUD programs in San Francisco, CA. All participating programs were licensed, residential SUD treatment programs and all clients participated in SUD treatment; three programs included beds for prison postrelease clients and all programs included some clients with comorbid SUD and mental health problems. We surveyed clients in all programs during site visits using the same data collection procedures and a core set of tobacco-related measures. All clients present on site visit days were eligible to complete surveys.
2.2. Measures
2.2.1. Demographics and primary reason for treatment entry
Survey items included demographic information (age, gender, race/ethnicity, education) and primary reason for treatment entry. We asked clients, “What are you currently in treatment for?” with response options including SUD, mental health disorder, both SUD and mental health disorder, and other. We asked only clients who responded SUD or both SUD and mental health disorder about their primary drug for treatment entry. Based on these two questions, we developed the variable—primary reason for treatment entry—and coded it as alcohol, stimulants, marijuana/cannabis, opioids, mental health, or other. We coded gender as male, female, or something else. We categorized race/ethnicity as non-Hispanic White, African American, Hispanic/ Latino, or other. We coded education as less than a high school education, high school, or GED equivalent, or greater than a high school education.
2.2.2. Tobacco use
We categorized clients as current cigarette smokers if they responded yes to two survey questions: “Have you smoked at least 100 cigarettes in your entire life?” and “Do you currently smoke cigarettes?” (CDC, 2017). We measured smoking severity using the Heaviness of Smoking Index (HSI) (Heatherton, Kozlowski, Frecker, Rickert, & Robinson, 1989), a 6-point scale based on two self-report items, number of cigarettes smoked per day, and time to first cigarette after awakening. The HSI has demonstrated reliability and validity as a measure of nicotine dependence (Borland, Yong, O’connor, Hyland, & Thompson, 2010). The HSI categorizes level of nicotine dependence as low (0–1), medium (2–4), or high (5–6; Diaz et al., 2005). We asked smokers whether their usual cigarette was menthol or nonmenthol. Participants also reported lifetime use of other tobacco products (i.e., “Have you ever in your lifetime used any of the following products?”) coded as smokeless tobacco, cigarillos and/or cigars, and e-cigarettes.
2.2.3. Cannabis use
Participants reported lifetime cannabis use (“Have you ever in your lifetime used marijuana/cannabis/hash?”). Those responding yes were asked about lifetime use of blunt/spliffs (“Have you ever in your lifetime mixed tobacco and marijuana and smoked them together, as part of the same blunt or spliff?”) Participants who had reported lifetime use of e-cigarettes were asked to report whether they had ever used an e-cigarette with a drug besides nicotine. Those responding yes were asked to select which drugs from a list including the option, marijuana/cannabis/THC/hash.
2.2.4. Smoking cessation-related questions
We asked participants whether they had quit smoking for at least 24 hours within the past year; those responding yes were asked the number of times they had done so. To identify lifetime use of smoking cessation products, we asked participants whether they had ever used any of the following products to try to quit smoking (coded as use of nicotine replacement therapy [NRT], use of non-NRT medication, and/or use of e-cigarette/vape pens), as well as whether they had ever called the California Smokers Helpline (yes/no). We also asked smokers whether they were seriously thinking of quitting within 30 days, six months, but not the next 30 days, or not within the next six months (DiClemente et al., 1991). We used readiness to quit within the next 30 days (yes/no) for this analysis. We asked smokers their primary reason for reducing or quitting smoking (i.e., program requirement, cost of a pack of cigarettes, health concerns, family pressure or encouragement, other, and did not try to quit). Finally, we asked participants whether they wanted help with quitting (yes/no) and whether quitting smoking was a part of their personal treatment plan (yes/no) in their current program.
2.3. Data collection procedures
Two research staff members conducted data collection during 1–2-day site visits at each program. Research staff verbally reviewed study information sheets with clients and distributed iPads with unique participant IDs to each potential participant. Potential participants then used the iPads to review the study information page again, and clicked to agree or decline study participation. Those agreeing to participate then completed the online survey. The self-administered surveys, developed using Qualtrics™ (Provo, Utah) software, took approximately 30 minutes to complete. Clients received a $20.00 gift card for study participation. The institutional review board of the University of California, San Francisco, approved study procedures.
2.4. Data analysis
We summarized categorical variables using frequencies and percentages. We identified lifetime blunt/spliff users and nonusers among current cigarette smokers based on the lifetime cannabis question and the lifetime blunt/spliff question (see Fig. 1). Among current cigarette smokers, we compared lifetime blunt/spliff users vs. nonusers on: demographics; drug use (primary drug for treatment entry, cannabis as a primary or secondary drug for treatment entry, lifetime use of cannabis in e-cigarettes/vape pens); tobacco use (HSI, menthol use, lifetime use of smokeless, cigar/cigarillo, and/or e-cigarette/vape pens); and smoking cessation-related variables (lifetime use of smoking cessation products, lifetime use of the California Helpline, readiness to quit within 30 days, desire for help with quitting and quitting as part of their treatment plan). We used descriptive statistics (mean, standard deviation) to summarize continuous variables. We computed statistical comparisons using t-test for continuous variables and chi-square test for categorical variables. Last, we used multivariable logistic regression to assess differences between ever/never blunt spliff users, while controlling for covariates. We entered all demographic variables into the regression model. We included all other variables in the model if they were significant at a p ≤ 0.10 in the univariate comparisons. The model accounted for nesting clients within treatment program. We applied generalized estimating equation (GEE) method for correlated data. We conducted the GEE method in the SAS GENMOD procedure with a logit link function and repeated statement. As the rate of missing data was low (3.6%), the multivariable model used complete case analysis. We used the variance inflation factor (VIF) and tolerance coefficient to assess multi-collinearity. We used SAS version 9.4. to conduct the analyses.
Fig. 1.
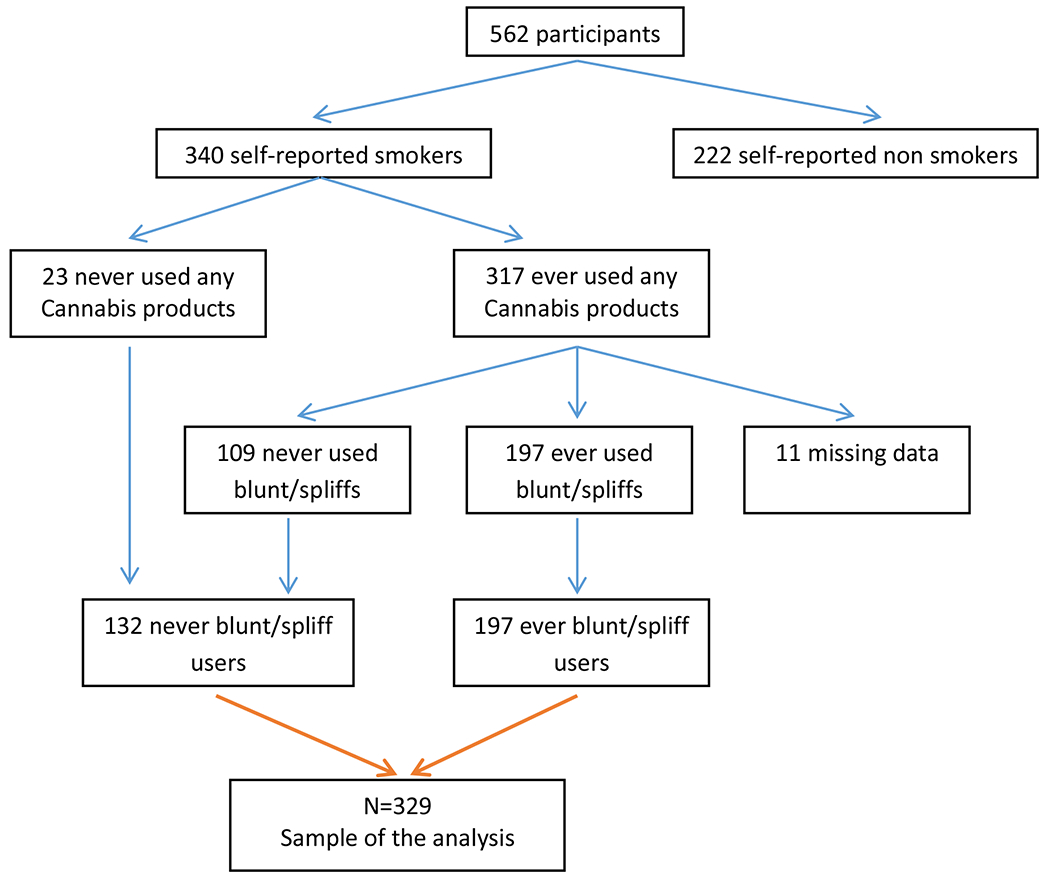
Selection of participants among current cigarette smokers in residential SUD treatment in California who report ever vs. never blunt/spliff use.
3. Results
3.1. Demographics and drug use
Among all 562 clients surveyed, 340 reported current cigarette smoking. Among 340 current cigarette smokers, 317 (93.2 %) reported lifetime use of any cannabis product, and 23 (6.8%) reported never having used a cannabis product. Among current cigarette smokers who reported lifetime use of cannabis, 197 (64.4%) reported lifetime blunt/spliff use, and 109 reported never having used blunt/spliffs. In addition, 11 cases did not respond to the blunt/spliff use survey question and we removed them from the analyses, as shown in Figure 1. Among current smokers composing our blunt/spliff analyses (N=329), average age was 37.8, (s.d.=11.4) with the majority identifying as male, 33.7% identifying as Hispanic/Latino, and 38.6% as non-Hispanic white (see Table 1). There were 117 (35.6%) reporting high school or GED diplomas and 119 (36.2%) reporting more than a high school education. Stimulants were reported as primary drug for treatment entry by 47.7%, followed by 21.7% reporting opioids. Cannabis was reported as either a primary or secondary drug for treatment entry by 12.7% of participants, while 23.4% reported using cannabis/THC in e-cigarettes/vape pens.
Table 1.
Demographics and drug use among current cigarette smokers in residential SUD treatment in California who report ever vs. never blunt/spliff use (N = 329).
| Mean (SD) or n (%) |
||||
|---|---|---|---|---|
| Total (N=329) | Smokers reporting ever blunt spliff use (n=197) | Smokers reporting never blunt spliff use (n=132) | p-value | |
| Demographics | ||||
| Age | 37.8 (11.4) | 34.0 (9.0) | 43.5 (12.1) | <0.0001 |
| Gender1 | 0.404 | |||
| Male | 242 (73.8%) | 150 (76.1%) | 92 (70.2%) | |
| Female | 81 (24.7%) | 44 (22.3%) | 37 (28.2%) | |
| Something else | 5 (1.5%) | 3 (1.5%) | 2 (1.5%) | 0.018 |
| Race/ethnicity | 0.018 | |||
| Hispanic/Latino | 111 (33.7%) | 67 (34.0%) | 44 (33.3%) | |
| African American | 58 (17.6%) | 25 (12.7%) | 33 (25.0%) | |
| Non- Hispanic White | 127 (38.6%) | 86 (43.7%) | 41 (31.1%) | |
| Other Education | 33 (10.0%) | 19 (9.6%) | 14 (10.6%) | 0.355 |
| <HS | 93 (28.3%) | 50 (25.4%) | 43 (32.6%) | |
| HS/GED | 117 (35.6%) | 72 (36.6%) | 45 (34.1%) | |
| >HS | 119 (36.2%) | 75 (38.1%) | 44 (33.3%) | 0.156 |
| Primary reason for treatment entry1 | ||||
| Alcohol | 51 (15.8%) | 28 (14.6%) | 23 (17.6%) | |
| Stimulant | 154 (47.7%) | 89 (46.4%) | 65 (49.6%) | |
| Marijuana/Cannabis | 11 (3.4%) | 7 (3.7%) | 4 (3.1%) | |
| Opioids | 70 (21.7%) | 50 (26.0%) | 20 (15.3%) | |
| Mental health or other | 37 (11.5%) | 18 (9.4%) | 19 (14.5%) | |
| Marijuana/cannabis as primary or secondary drug for treatment entry1,2 | 37 (12.7%) | 25 (14.0%) | 12 (10.6%) | 0.402 |
| Use of cannabis/THC in e-cigarettes/vape pens1 | 76 (23.4%) | 69 (35.2%) | 7 (5.4%) | <0.0001 |
Missing data: Gender (2), Primary drug for treatment entry (6), Marijuana/cannabis as primary or secondary drug for treatment entry (1), Use of cannabis/THC in e-cigarettes/vape pens (4).
Excluded 37 smokers whose reason for treatment entry was mental health or other.
3.2. Variables associated with blunt/spliff use
Table 1 shows results of univariate analyses of demographic and drug use variables for ever vs. never blunt/spliff users. Blunt/spliff users were younger (p. < 0.0001), were more often non-Hispanic white, and were less often African American (p < 0.018). Blunt/spliff users were significantly more likely to report use of cannabis/THC in e-cigarettes/vape pens (p < 0.0001). Results of univariate comparisons for tobacco use and smoking cessation-related variables are shown in Table 2. Variables significant at the p ≤ 0.10 level and included in the multivariate model were lifetime use of cigars/cigarillos, lifetime use of smokeless tobacco, and lifetime use of e-cigarettes/vape pens, all of which were reported in higher numbers by blunt/spliff users. Smoking cessation-related variables significant at p ≤ 0.10 were lifetime use of NRT, lifetime use of e-cigarettes for cutting down or quitting smoking, thinking of quitting in the next 30 days, and wanting help with quitting.
Table 2.
Tobacco use characteristics among current cigarette smokers in residential SUD treatment in California who report ever vs. never blunt/spliff use.
| Mean (SD) or n (%) |
|||
|---|---|---|---|
| Smokers reporting ever blunt spliff use (N=197) | Smokers reporting never blunt spliff use (N=132) | p-value | |
| Tobacco/Nicotine Use | |||
| Heaviness of Smoking Index (HSI) | 2.1 (1.3) | 2.0 (1.5) | 0.563 |
| Menthol as usual cigarette | 64 (32.5%) | 42 (31.8%) | 0.899 |
| Lifetime cigars/cigarillos1 | 168 (85.7%) | 68 (53.1%) | <0.0001 |
| Lifetime smokeless | 106 (53.8%) | 32 (24.2%) | <0.0001 |
| Lifetime e-cigarettes/vape pens1 | 150 (76.5%) | 58 (45.0%) | <0.0001 |
| Smoking cessation-related variables | |||
| Past year number of quit attempts | 4.5 (10.1) | 5.8 (13.2) | 0.343 |
| Main reason for quitting/cutting down1 | 0.373 | ||
| Treatment program requirement | 33 (16.8%) | 14 (10.7%) | |
| Cost of a pack of cigarettes | 33 (16.8%) | 19 (14.5%) | |
| Health concerns | 63 (32.1%) | 51 (38.9%) | |
| Family (pressure, encouragement, being a good model) | 15 (7.7%) | 16 (12.2%) | |
| Other reason | 26 (13.3%) | 15 (11.5%) | |
| I have not tried to reduce my smoking/quitting | 26 (13.3%) | 16 (12.2%) | |
| Methods Used for Quitting | |||
| Lifetime NRT use1 | 101 (51.3%) | 48 (36.6%) | 0.009 |
| Lifetime non-NRT medication1 | 16 (8.5%) | 11 (8.7%) | 0.935 |
| Lifetime e-cigarettes/vape pens use1 | 107 (55.7%) | 40 (31.0%) | <0.0001 |
| Lifetime California Smokers Helpline use1 | 15 (7.7%) | 12 (9.1%) | 0.642 |
| Readiness- Thinking of quitting next 30 days | 53 (26.9%) | 52 (39.4%) | 0.017 |
| Want help with quitting1 | 83 (42.1%) | 41 (31.3%) | 0.048 |
| Quitting part of personal treatment plan1 | 60 (30.6%) | 40 (30.3%) | 0.952 |
Missing data: Lifetime cigars/cigarillos (5), Lifetime e-cigarettes/vape pens (4), Main reason for quitting/cutting down (2), Lifetime NRT use (1), Lifetime non-NRT medication (14), Lifetime e-cigarettes/vape pens use (8), Lifetime California Smokers Helpline use (1), Want help with quitting (1), Quitting part of personal treatment plan (1).
Results for the multivariate analysis are shown in Table 3. Participants reporting lifetime use of cannabis/THC in e-cigarettes/vape pens were 4.26 times more likely to report lifetime blunt/spliff use (95% CI: 1.54–11.80). Participants reporting lifetime use of cigars/cigarillos were 2.95 times more likely to report blunt/spliff use (CI: 1.37–6.32). Participants thinking of quitting smoking within the next 30 days were significantly less likely to report blunt/spliff use (OR= 0.37, CI: 0.23–0.60). However, those reporting that they wanted help with quitting smoking were significantly more likely to report lifetime blunt/spliff use (OR=2.39, CI: 1.52–3.77). Multi-collinearity was evaluated using VIF and tolerance coefficient. For the variables in the model, the VIF are small (< 2) and the tolerance coefficients are greater than 0.5. These indicators suggest that multicollinearity did not threaten the model.
Table 3.
Factors associated with blunt/spliff use among current cigarette smokers in residential SUD treatment in California.
| Adjusted OR (95%CI) | p1 | |
|---|---|---|
| Use of cannabis/THC in e-cigarettes/vape pens | ||
| No (Ref) | 1 | |
| Yes | 4.26 (1.54- 11.80) | 0.005 |
| Tobacco/Nicotine Use | ||
| Lifetime cigars/cigarillos | ||
| No (Ref) | 1 | |
| Yes | 2.95 (1.37- 6.32) | 0.006 |
| Lifetime Smokeless | ||
| No (Ref) | 1 | |
| Yes | 1.71 (0.75- 3.87) | 0.201 |
| Lifetime e-cigarettes/vape pens | ||
| No (Ref) | 1 | |
| Yes | 1.01 (0.55- 1.84) | 0.982 |
| Smoking cessation-related variables | ||
| Lifetime NRT use | ||
| No (Ref) | 1 | |
| Yes | 1.24 (0.65- 2.36) | 0.513 |
| Lifetime e-cigarette/vape pen use for quitting | ||
| No (Ref) | 1 | |
| Yes | 0.97 (0.53- 1.80) | 0.929 |
| Readiness- Thinking of quitting next 30 days | ||
| No (Ref) | 1 | |
| Yes | 0.37 (0.23- 0.60) | <0.0001 |
| Want help with quitting | ||
| No (Ref) | 1 | |
| Yes | 2.39 (1.52- 3.77) | <0.001 |
| Demographics | ||
| Age | 0.93 (0.90- 0.95) | <0.0001 |
| Gender | ||
| Male | 1 | |
| Female | 0.72 (0.38- 1.34) | 0.298 |
| Other | 0.74 (0.49- 1.12) | 0.156 |
| Race/Ethnicity | ||
| Hispanic (Ref) | 1 | |
| Non-Hispanic White | 1.55 (0.78- 3.07) | 0.208 |
| Non-Hispanic Black | 1.06 (0.39- 2.84) | 0.913 |
| Non-Hispanic Other | 0.96 (0.42- 2.21) | 0.924 |
| Education | ||
| <HS | 1 | |
| HS/GED | 1.62 (0.91- 2.87) | 0.102 |
| >HS | 1.44 (0.71- 2.92) | 0.316 |
Logistic regression with clients nested within clinic.
4. Discussion
Among clients surveyed in residential treatment in California, 60.5% self-reported current cigarette smoking, a finding indicative of continued high smoking prevalence among individuals with other SUDs. Smokers in this sample reported a very high rate of lifetime cannabis use (93.2%), compatible with other reports of high cannabis use rates among smokers in general population samples (Dierker, Braymiller, Rose, Goodwin, & Selya, 2018; Goodwin et al., 2018; Hindocha et al., 2015) and high rates of tobacco smoking among cannabis users (Schauer, Berg, Kegler, Donovan, & Windle, 2015b; Schauer, King, et al., 2017; Weinberger, Platt, et al., 2018). Additionally, a majority of those reporting lifetime cannabis use also reported lifetime blunt/spliff use. Lifetime blunt/spliff users in our sample were more likely to be younger than non-blunt/spliff users, and more likely to report lifetime cigar/cigarillo use and use of cannabis/THC in e-cigarettes/vape pens. The association of cigar/cigarillo use with blunt/spliff use may be expected given that blunts consist of cannabis rolled in cigar wrappers. This is concerning because blunt use may lead to cigar use among adolescents (Audrain-McGovem, Rodriguez, Alexander, Pianin, & Sterling, 2019) and conversely, cigar use may lead to blunt/spliff use (Fairman & Anthony, 2018). Moreover, using multiple tobacco products has been associated with greater nicotine dependence among smokers in SUD treatment (Guydish, Tajima, et al., 2016). Blunt/spliff users in our sample were also more likely to report lifetime use of e-cigarettes/vape pens for cannabis/THC delivery. The emergence of e-cigarette/vaping product use–associated lung injury (EVALI) has raised alarm regarding acute health hazards associated with e-cigarettes/vape pen use, particularly for cannabis or THC-delivery (King, Jones, Baldwin, & Briss, 2020). Our survey did not ask for information regarding co-administration of cannabis and tobacco via e-cigarette/vape pens, which has also been associated with EVALI. This should be addressed in future research.
Current cigarette smokers in our sample who expressed readiness to quit within 30 days were significantly less likely to report lifetime blunt/spliff use. However, those who wanted help with quitting were over two times more likely to report blunt/spliff use. It is possible that smokers with histories of blunt/spliff use in this high smoking population want to quit but feel less confident, thus less ready, to do so and want more help to achieve smoking cessation. Evidence showing that co-users of tobacco and cannabis have more difficulty quitting and sustaining smoking cessation supports this interpretation (Voci et al., 2020; Weinberger, Platt, et al., 2018)
Quit-related findings in our study offer directions for research and may also inform clinical considerations for addressing cigarette smoking in SUD treatment. Research should examine the relationship between co-use and cigarette smoking–cessation outcomes for those in SUD treatment. Researchers could develop and test readiness interventions that address co-use , with the goal of facilitating motivation to address cannabis use as a part of quitting tobacco (Guydish, Gruber, et al., 2016). Additionally, consideration should be given to simultaneous treatment of tobacco and cannabis use in outpatient SUD treatment settings, although this may not be relevant in residential treatment, where, presumably, smokers are not engaged in active cannabis use. Emerging evidence suggests that such interventions are feasible, although the evidence also suggests that simultaneous treatment may be more helpful for cannabis cessation than tobacco cessation (Becker, Haug, Kraemer, & Schaub, 2015; Lee et al., 2019; Walsh et al., 2020). Researchers should carry out clinical trials to examine simultaneous cannabis/tobacco treatment interventions utilizing evidence-based treatments for both among co-users in SUD treatment.
Our findings should be interpreted with several limitations in mind. As a cross-sectional survey, causal interpretations are not possible. Self-reported cigarette smoking, cannabis, and blunt/spliff use may not have been accurate. For example, an additional 47 clients self-reported as nonsmokers but blew expired carbon monoxide above the 9 parts per million (ppm) cutoff. These probable, current tobacco smokers were not surveyed about cigarette smoking behaviors, thus they were not included in our sample. Our measures of lifetime cannabis and blunt/spliff use preclude the ability to assess the relationship of frequency and heaviness of cannabis use with cigarette smoking and nicotine dependence. Additionally, although information regarding recent or current blunt/spliff use was likely to be confounded with length of time in residential treatment, our study’s lack of findings regarding recent/current blunt/spliff use also precludes understanding the impact of that use on smoking cessation-related variables. There are generalizability limitations related to our sample selection, since it was a convenience sample restricted to residential programs within California. However, given the legalization of medical cannabis in California in 1996 and recreational cannabis in 2016, cross-sectional data regarding co-use among smokers in SUD treatment in California provide information on which to build regarding possible increases in co-use rates and consequences of co-use that may occur as recreational cannabis becomes legally available across states. The racial/ethnic composition of our sample may be another limitation. African Americans composed 17.6% of our study sample, higher than the estimated 11.6% of adults in the United States with SUDS who are African American (McCance-Katz, 2019). However, reports indicate a higher prevalence of blunt use among African Americans than other racial/ethnic groups, thus they may be underrepresented in our study sample (Cohn, Johnson, Ehlke, & Villanti, 2016; Montgomery & Mantey, 2017).
4.1. Conclusion
Co-use of tobacco and cannabis has been associated with more severe nicotine dependence and more difficulty quitting cigarette smoking, but has been understudied in the high number of smokers in SUD treatment. We found a high rate of lifetime cannabis use, including blunt/spliff use, among smokers in residential SUD treatment. Cigarette smokers expressing less readiness to quit, but requesting help with quitting, were more likely to have a history of blunt/spliff use, suggesting blunt/spliff use may be a variable that affects the probability of smoking cessation success. Co-use of cannabis and tobacco should be addressed for smokers in SUD treatment.
Highlights.
93.2% of current cigarette smokers in treatment reported lifetime cannabis use
64.4% of cigarette/cannabis co-users reported lifetime blunt/spliff use
Lifetime use of cannabis in e-cigarettes predicted lifetime blunt/spliff use
Lower readiness to quit smoking cigarettes was associated with blunt/spliff use
Smokers wanting help with quitting were more likely to have used blunt/spliffs
Acknowledgments
The authors would like to thank the directors, staff, and patients enrolled in the participating treatment programs.
Funding Sources
This work was supported by the California Tobacco Control Program (18-10025), by the California Tobacco Related Disease Research Program (TRDRP 27IR-0040, 28CP-0038), and by the NCI Cancer Center Support Grant (P30 CA082103). The content is solely the responsibility of the authors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: none
References
- Apollonio D, Philipps R, & Bero L (2016). Interventions for tobacco use cessation in people in treatment for or recovery from substance use disorders. Cochrane Database of Systematic Reviews (11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Alexander E, Pianin S, & Sterling KL (2019). Association Between Adolescent Blunt Use and the Uptake of Cigars. JAMA Network Open, 2(12), e1917001–e1917001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker J, Haug S, Kraemer T, & Schaub MP (2015). Feasibility of a group cessation program for co-smokers of cannabis and tobacco. Drug and Alcohol Review, 27(4), 418–426. [DOI] [PubMed] [Google Scholar]
- Borland R, Yong H-H, O’connor R, Hyland A, & Thompson M (2010). The reliability and predictive validity of the Heaviness of Smoking Index and its two components: findings from the International Tobacco Control Four Country study. Nicotine & Tobacco Research, 72(suppl 1), S45–S50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. (2017). National Center for Health Statistics Adult Tobacco Use Information. National Health Interview Survey; Retrieved from https://www.cdc.gov/nchs/nhis/tobacco/tobacco_glossary.htm. [Google Scholar]
- Cohn A, Johnson A, Ehlke S, & Villanti AC (2016). Characterizing substance use and mental health profiles of cigar, blunt, and non-blunt marijuana users from the National Survey of Drug Use and Health. Drug and Alcohol Dependence, 160, 105–111. [DOI] [PubMed] [Google Scholar]
- Diaz FJ, Jane M, Salto E, Pardell H, Salleras L, Pinet C, & De Leon J (2005). A brief measure of high nicotine dependence for busy clinicians and large epidemiological surveys. Australian & New Zealand Journal of Psychiatry, 39(3), 161–168. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, & Rossi JS (1991). The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. Journal of Consulting and Clinical Psychology, 59(2), 295. [DOI] [PubMed] [Google Scholar]
- Dierker L, Braymiller J, Rose J, Goodwin R, & Selya A (2018). Nicotine dependence predicts cannabis use disorder symptoms among adolescents and young adults. Drug and Alcohol Dependence, 187, 212–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairman BJ (2015). Cannabis problem experiences among users of the tobacco-cannabis combination known as blunts. Drug and Alcohol Dependence, 150, 77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairman BJ, & Anthony JC (2018). Does starting to smoke cigars trigger onset of cannabis blunt smoking? Nicotine and Tobacco Research, 20(3), 355–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin RD, Pacek LR, Copeland J, Moeller SJ, Dierker L, Weinberger A, Hasin DS (2018). Trends in daily cannabis use among cigarette smokers: United States, 2002–2014. American Journal of Public Health, 705(1), 137–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray KM, Sonne SC, McClure EA, Ghitza UE, Matthews AG, McRae-Clark AL, … Mooney LJ. (2017). A randomized placebo-controlled trial of N-acetylcysteine for cannabis use disorder in adults. Drug and Alcohol Dependence, 177, 249–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guydish J, Gruber VA, Le T, Tajima B, Andrews KB, Leo EL, Tsoh JY (2016). A pilot study of a readiness group to increase initiation of smoking cessation services among women in residential addiction treatment. Journal of Substance Abuse Treatment, 63, 39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guydish J, Tajima B, Pramod S, Le T, Gubner NR, Campbell B, & Roman P (2016). Use of multiple tobacco products in a national sample of persons enrolled in addiction treatment. Drag and Alcohol Dependence, 166, 93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, & Robinson J (1989). Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Addiction, 84(1), 791–800. [DOI] [PubMed] [Google Scholar]
- Hindocha C, Shaban ND, Freeman TP, Das RK, Gale G, Schafer G, Curran ΗV (2015). Associations between cigarette smoking and cannabis dependence: a longitudinal study of young cannabis users in the United Kingdom. Drug and Alcohol Dependence, 148, 165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King BA, Jones CM, Baldwin GT, & Briss PA (2020). The EVALI and Youth Vaping Epidemics—Implications for Public Health. New England Journal of Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee DC, Walker DD, Hughes JR, Brunette MF, Scherer E, Stanger C, … Budney AJ, (2019). Sequential and simultaneous treatment approaches to cannabis use disorder and tobacco use. Journal of Substance Abuse Treatment, 98, 39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCance-Katz EF (2019). The National Survey on Drug Use and Health: 2017. Substance Abuse and Mental Health Services Administration, https://www.samhsa.gov/data/sites/default/files/nsduh-ppt-09-2018.pdf. Accessed May, 7. [Google Scholar]
- McClure EA, Baker NL, Sonne SC, Ghitza UE, Tomko RL, Montgomery L, … Gray KM. (2018). Tobacco use during cannabis cessation: Use patterns and impact on abstinence in a National Drug Abuse Treatment Clinical Trials Network study. Drug and Alcohol Dependence, 192, 59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure EA, Tomko RL, Salazar CA, Akbar SA, Squeglia LM, Herrmann E, Peters EN (2018). Tobacco and cannabis co-use: Drug substitution, quit interest, and cessation preferences. Experimental and Clinical Psychopharmacology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery L, & Mantey DS (2017). Correlates of blunt smoking among African American, Hispanic/Latino, and white adults: results from the 2014 national survey on drug use and health. Substance Use & Misuse, 52(11), 1449–1459. [DOI] [PubMed] [Google Scholar]
- Ream GL, Benoit E, Johnson BD, & Dunlap E (2008). Smoking tobacco along with marijuana increases symptoms of cannabis dependence. Drug and Alcohol Dependence, 95(3), 199–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schauer GL, Berg CJ, Kegler MC, Donovan DM, & Windle M (2015a). Assessing the overlap between tobacco and marijuana: Trends in patterns of co-use of tobacco and marijuana in adults from 2003–2012. Addictive Behaviors, 49, 26–32. [DOI] [PubMed] [Google Scholar]
- Schauer GL, Berg CJ, Kegler MC, Donovan DM, & Windle M (2015b). Differences in tobacco product use among past month adult marijuana users and nonusers: Findings from the 2003–2012 National Survey on Drug Use and Health. Nicotine & Tobacco Research, 73(3), 281–288. [DOI] [PubMed] [Google Scholar]
- Schauer GL, King BA, & McAfee TA (2017). Prevalence, correlates, and trends in tobacco use and cessation among current, former, and never adult marijuana users with a history of tobacco use, 2005–2014. Addictive Behaviors, 73, 165–171. [DOI] [PubMed] [Google Scholar]
- Schauer GL, Rosenberry ZR, & Peters EN (2017). Marijuana and tobacco coadministration in blunts, spliffs, and mulled cigarettes: A systematic literature review. Addictive Behaviors, 64, 200–211. [DOI] [PubMed] [Google Scholar]
- Skelton E, Tzelepis F, Shakeshaft A, Guillaumier A, McCrabb S, & Bonevski B (2018). Integrating smoking cessation care in alcohol and other drug treatment settings using an organizational change intervention: a systematic review. Addiction, 775(12), 2158–2172. [DOI] [PubMed] [Google Scholar]
- Thurgood SL, McNeill A, Clark-Carter D, & Brose LS (2016). A systematic review of smoking cessation interventions for adults in substance abuse treatment or recovery. Nicotine & Tobacco Research, 18(5), 993–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timberlake DS (2009). A comparison of drug use and dependence between blunt smokers and other cannabis users. Substance Use & Misuse, 44(5), 401–415. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Pedersen ER, Seelam R, Dunbar MS, Shih RA, & DAmico EJ (2019). Types of cannabis and tobacco/nicotine co-use and associated outcomes in young adulthood. Psychology of Addictive Behaviors, 55(4), 401–411. doi: 10.1037/adb0000464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voci S, Zawertailo L, Baliunas D, Masood Z, & Selby P (2020). Is cannabis use associated with tobacco cessation outcome? An observational cohort study in primary care. Drug and Alcohol Dependence, 206, 107756. [DOI] [PubMed] [Google Scholar]
- Walsh H, McNeill A, Purssell E, & Duaso M (2020). A systematic review and Bayesian meta-analysis of interventions which target or assess co-use of tobacco and cannabis in single or multi-substance interventions. Addiction [DOI] [PubMed] [Google Scholar]
- Wang JB, & Cataldo JK (2016). Medical marijuana legalization and co-use in adult cigarette smokers. American Journal of Health Behavior, 40(2), 205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger AH, Gbedemah M, Wall MM, Hasin DS, Zvolensky MJ, & Goodwin RD (2018). Cigarette use is increasing among people with illicit substance use disorders in the United States, 2002–14: emerging disparities in vulnerable populations. Addiction, 775(4), 719–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger AH, Platt J, Copeland J, & Goodwin RD (2018). Is Cannabis Use Associated With Increased Risk of Cigarette Smoking Initiation, Persistence, and Relapse? Longitudinal Data From a Representative Sample of US Adults. The Journal of Clinical Psychiatry, 79(2). [DOI] [PMC free article] [PubMed] [Google Scholar]


