Abstract
The object of this study is to evaluate the long-term outcome of hind limb weight-bearing function and progression of stifle osteoarthritis (OA) after tibial plateau leveling osteotomy (TPLO). Groups were classified by the degree of cranial cruciate ligament (CrCL) damage and presence or absence of medial meniscus damage as macroscopically evaluated during surgery. Weight-bearing function was assessed via the peak vertical force (PVF), and OA progression was assessed via the radiographic OA score (OAS) preoperatively and 1, 3, 6, 12, 18, 24, and 36 months postoperatively. In all stifles, PVF was significantly higher within 6 months postoperatively than preoperatively, and this high ratio was maintained for 36 months. The OAS was significantly higher 24 months postoperatively than preoperatively in stifles with a partial CrCL tear, and significantly increased at each timepoint after 3 months postoperatively in stifles with complete CrCL rupture. The OAS remained consistently lower in stifles with a partial CrCL tear and no treatment of the medial meniscus than in stifles with complete rupture. Thus, after TPLO, the weight-bearing function improved in the early postoperative period and was maintained for as long as 36 months. Although OA progressed over time after TPLO, the progression was more gradual in stifles with partial tears than in those with complete rupture. Canine patients would benefit from earlier surgical intervention through development of technology that enables early detection of ligament degeneration.
Keywords: cranial cruciate ligament rupture, dog, orthopedic surgery, stifle joint, tibial plateau leveling osteotomy
Cranial cruciate ligament rupture (CrCLR) is a common cause of hind limb lameness in dogs. The cranial cruciate ligament (CrCL) plays a vital role in maintaining the stability of the stifle joint by preventing cranial tibial drawer movement and limiting hyperextension of the joint and excessive internal tibial rotation [3]. In the stance phase, cranial tibial thrust (CrTT) is generated at the femorotibial joint, and the tibia is displaced forward when the CrCL is not functioning [31]. Stifle instability associated with CrCLR probably causes secondary osteoarthritis (OA) and medial meniscus (MM) damage [10, 21, 29].
Tibial plateau leveling osteotomy (TPLO) is a type of functional stabilization that is a useful treatment method for CrCLR, as it enables rapid recovery after surgery. TPLO involves an osteotomy and rotation of the proximal part of the tibia to correct the tibial plateau angle (TPA) [32]. The goal of TPLO is to neutralize CrTT by correcting the slope and preventing forward displacement in the stance phase [32].
Several studies have been performed to assess the optimal postoperative evaluation of TPLO, describing techniques such as functional evaluation using a force plate, radiographic assessment to evaluate the degree of progression of OA, and evaluation of postoperative complications [5, 7, 8, 12, 18, 24, 25, 28]. A systematic review found that the best available evidence most strongly supports a normal return to clinical function following TPLO in dogs with naturally occurring CrCLR [5]. However, several reports observed the progression of OA after TPLO [8, 25, 28]. Furthermore, it is known that the degree of CrCL damage affects the postoperative macroscopic findings of cartilage damage after TPLO [18]. However, it is unclear how the degree of CrCL damage or MM treatment affects the radiographic OA score (OAS), and the influence of OA progression on weight-bearing function remains unknown. In the present study, we retrospectively evaluated the long-term (1- to 3-year) postoperative outcomes with respect to the weight-bearing function and progression of OA in stifles with CrCLR treated by TPLO in uncomplicated cases. We hypothesized that the progressive OA becomes severe as a result of complete CrCLR and MM treatment, and that the OA decreases weight-bearing function.
MATERIALS AND METHODS
Case selection criteria
At the Animal Medical Center of our university from April 2004 to December 2017, TPLO was performed in 189 dogs (249 stifles) with suspected CrCLR. Of these, the present study included the stifle joints that underwent analysis using a force plate and radiographic evaluation from the preoperative period to >1 year postoperatively with the consent of the owners. Dogs that underwent bilateral surgery were judged to have bilateral CrCLR at the time of diagnosis, and the operation of the contralateral limb was performed within 1 month after the operation of the other limb. Dogs that underwent unilateral surgery either had unilateral CrCLR or had bilateral CrCLR for which the contralateral limb had been treated >6 months previously and achieved adequate functional recovery of the contralateral limb as indicated by the PVF. However, as dogs with bilateral CrCLR for which the contralateral limb had been treated by TPLO <6 months previously were at risk of not recovering adequate limb function, these dogs were excluded from the present study. Similarly, dogs were excluded if they had postoperative stifle complications considered to be related to the TPLO, and/or had developed injuries or other orthopedic or neurological diseases after TPLO. The stifles with postoperative TPA >14° were also excluded, as Robinson et al. reported that limb function was not affected by postoperative TPA between 0 and 14° [30]. In addition, dogs weighing less than 15 kg were excluded. CrCLR was diagnosed by the tibial cranial drawer test and tibial compression test, examination of synovial fluid, and tibial compression radiography in the mediolateral direction.
Surgery
TPLO was performed in accordance with the method described by Slocum and Slocum [32]. First, a tibial compression radiograph in the mediolateral direction was taken for preoperative planning. The TPA was measured on this image using the method described by Warzee et al [35]. The surgery was approached from the medial side of the tibia. For intra-articular evaluation, the joint capsule was incised via the medial parapatellar tendon approach. At this time, the CrCL was observed macroscopically, and the extent of damage of the ligament was evaluated. In stifles with a partial CrCLR, the function of the remaining ligament was evaluated by probing and macroscopic examination; tension in the ligament indicated a partial CrCLR with remaining functions, while absence of tension indicated a partial CrCLR without remaining functions. Next, the fibers in the ruptured CrCL or nonfunctional ligament were debrided. After CrCL assessment, the presence or absence of MM damage was evaluated macroscopically and via probing. At this time, we checked only macroscopically for abnormalities of structures such as the caudal cruciate ligament and the lateral meniscus. When the caudal horn of the MM was displaced in front of the medial femoral condyle, only the inverted portion was excised. When the caudal horn of the MM was confirmed to have a bucket handle tear, only the damaged part of the meniscal tissue was partially resected [34]. Meniscal release was not performed in any of the included cases. After evaluation of the intra-articular structures and completion of treatment of the CrCL and MM, we performed an osteotomy at the proximal tibia using a TPLO saw blade, rotated the proximal segment to aim for a postoperative TPA of 5°, and performed fixation. For fixation, a TPLO locking compression plate (Johnson & Johnson, New Brunswick, NJ, USA) was used in 36 stifles, the Slocum plate (Slocum Enterprises, Eugene, OR, USA) was used in 6 stifles, and a dynamic compression plate (Mizuho Ika, Tokyo, Japan) was used in 7 stifles. After surgery, the TPA was reevaluated.
Groups
Based on the macroscopic findings of the stifles during surgery, the stifles were classified into six groups in accordance with the degree of CrCL damage and presence or absence of MM treatment. Group 1 comprised stifles with a partial CrCLR with remaining functions without MM treatment, Group 2 comprised stifles with a partial CrCLR with remaining functions and MM treatment, Group 3 comprised stifles with an partial CrCLR without remaining functions without MM treatment, Group 4 comprised stifles with a partial CrCLR without remaining functions with MM treatment, Group 5 comprised stifles with complete CrCLR without MM treatment, and Group 6 comprised stifles with complete CrCLR and MM treatment.
Force plate analysis
Using force plate equipment (Advanced Mechanical Technology, Inc., Watertown, MA, USA), the weight-bearing function of stifles with CrCLR was objectively evaluated preoperatively and 1, 3, 6, 12, 18, 24, and 36 months postoperatively. The average trotting speed was 1.5 to 2.0 m/sec, and the data of each limb obtained from 10 trials were used to obtain average peak vertical force (PVF) values. All PVF data were expressed as a percentage of body weight (%BW); this ratio was used as an indicator of weight-bearing function.
Radiographic OAS
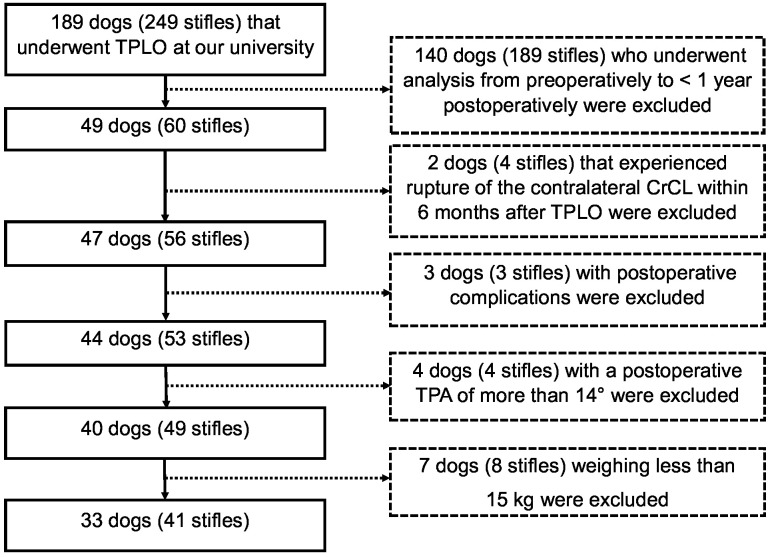
The OAS was calculated as a measure of radiological evaluation. Radiographic images in the mediolateral and craniocaudal directions of the stifle were used for evaluation preoperatively and 1, 3, 6, 12, 18, 24, and 36 months postoperatively. The evaluation was performed in accordance with the method described by Wessely et al [36]. The evaluation sites are shown in Fig. 1, and each site was assigned a grade from 1 to 4. The scoring system for each grade is shown in Table 1. In the present study, the total number of assigned points was considered to be the OAS, which ranged from 15 to 60 points using this evaluation method. All evaluations were performed by a single veterinarian (graduate student) who was not the surgeon. The observer was blinded to the patient data while the radiographic evaluation was performed.
Fig. 1.
Assessment sites for the osteoarthritis score evaluation. 1, patellar apex; 2, patellar base; 3, proximal trochlear ridge; 4, distal trochlear ridge; 5, femoral condyle; 6, tibial tuberosity; 7, cranial aspect of the tibial plateau; 8, caudal aspect of the tibial plateau; 9, central aspect of the tibial plateau; 10, popliteal surface of the femur; 11, sesamoid bones; 12, lateral tibial and femoral condyles; 13, medial tibial and femoral condyles; 14, patella; 15, intercondylar notch.
Table 1. Osteoarthritis grading system and corresponding radiographic changes [36].
| Grade | Severity | Changes |
|---|---|---|
| 1 | None | Radiographically normal/no evidence of sclerosis or osteophytes |
| 2 | Mild | Mild osteophytes and/or mild sclerosis (mild arthrosis) |
| 3 | Moderate | Moderate osteophytes and sclerosis (moderate arthrosis) |
| 4 | Severe | Marked osteophytes and severe sclerosis (severe arthrosis) |
Statistical analysis
SAS software version 9.3 (SAS Institute, Cary, NC, USA) was used for the statistical analysis. Groups 2, 3, and 4 were omitted from the analysis, as these groups contained no stifles or only two stifles. Comparisons of age, BW, and pre- and postoperative TPA among the groups were conducted using the Kruskal-Wallis test. Statistical analyses of the PVF and OAS were carried out by repeated-measures analysis of variance using the Proc Mixed procedure of the SAS software. The linear model included the fixed effects of treatment groups, time, and their interaction. The effects of treatment groups within an individual dog were included as random repeated effects. Multiple comparisons of least square means were adjusted using the Tukey-Kramer test. Statistical analysis of the grade for each site was carried out by repeated-measures analysis of variance using the Proc Mixed procedure of the SAS software. The linear model included the fixed effect of time. The effects at each site within an individual dog were included as random repeated effects. Multiple comparisons of least square means were adjusted using the Tukey-Kramer test. Data were considered statistically significant at a P value of <0.05.
RESULTS
Dogs
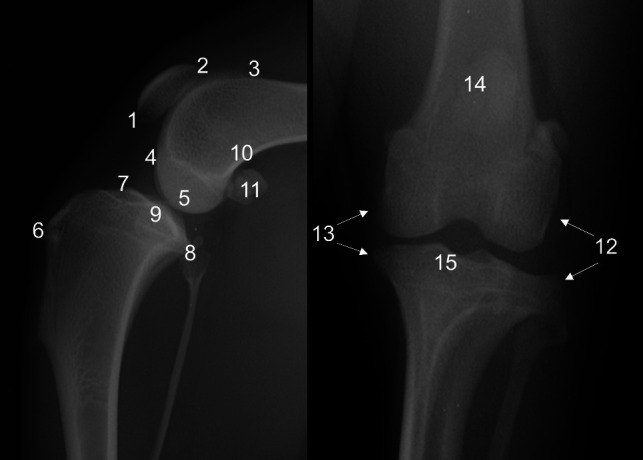
In accordance with case selection criteria, 35 dogs (41 stifles) were included in the present study. Details are presented in the flowchart (Fig. 2). Among all 35 dogs with CrCLR, the median age was 72.0 months (range, 11.0–128.0 months) and the median BW was 30.5 kg (range, 15.9–60.0 kg) at the time of surgery. The dogs comprised 6 males, 13 neutered males, 2 females, and 14 spayed females. The breeds included in the present study are shown in Table 2. Among all 41 stifles, 12 were bilateral surgical stifles, while 29 were unilateral stifles. There were 11 stifles observed for 3 years, and 18 stifles observed for more than 2 years. Based on the intraoperative macroscopic findings, Groups 1, 2, 3, 4, 5 and 6 comprised 5, 2, 0, 2, 14, and 18 stifles, respectively. Age, BW, and TPA before and after TPLO in each group on the day of surgery are shown in Table 3. Although the postoperative TPA in many of the included dogs was much greater than 5°, all cases were confirmed to have no CrTT during the tibial compression test performed postoperatively. There were no significant differences between the groups in age, BW, or TPA before and after TPLO.
Fig. 2.
The flowchart of case selection.
Table 2. Dog breeds included in the present study.
| Number of dogs | Breed |
|---|---|
| n=9 | Labrador retriever |
| n=5 | Golden retriever |
| n=4 | Bernese mountain dog |
| n=3 | Siberian husky, English bulldog |
| n=2 | Border collie, Beagle, Newfoundland, Mixed breed |
| n=1 | Flat-coated retriever, Dalmatian, American pit bull terrier |
Table 3. Data for each group on the day of the tibial plateau leveling osteotomy.
| n | Age (months) |
Bodyweight (kg) |
Preoperative TPA (°) |
Postoperative TPA (°) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median | Min | Max | Median | Min | Max | Median | Min | Max | Median | Min | Max | ||
| All stifles | 41 | 72.0 | 11.0 | 128.0 | 30.5 | 15.9 | 60.0 | 27.5 | 19.5 | 35.0 | 7.5 | 0.0 | 13.5 |
| Group 1 | 5 | 26.0 | 11.0 | 89.0 | 38.0 | 15.9 | 44.7 | 27.5 | 20.5 | 29.5 | 8.5 | 3.0 | 13.0 |
| Group 2 | 2 | 100.0 | 99.0 | 101.0 | 29.4 | 25.8 | 33.0 | 25.3 | 21.5 | 29.0 | 10.0 | 7.5 | 12.5 |
| Group 3 | 0 | - | - | - | - | - | - | - | - | - | - | - | - |
| Group 4 | 2 | 94.0 | 89.0 | 99.0 | 24.5 | 15.9 | 33.0 | 30.0 | 25.0 | 35.0 | 8.3 | 3.5 | 13.0 |
| Group 5 | 14 | 68.0 | 26.0 | 128.0 | 37.8 | 20.5 | 60.0 | 28.3 | 19.5 | 34.0 | 5.5 | 1.5 | 13.0 |
| Group 6 | 18 | 68.5 | 11.0 | 118.0 | 28.9 | 16.2 | 40.3 | 27.5 | 19.5 | 34.0 | 8.3 | 0.0 | 13.5 |
TPA, tibial plateau angle; Min, minimum; Max, maximum.
Force plate analysis
The PVF values in each group are shown in Table 4. In Group 1, the PVF was significantly lower preoperatively than 18 months postoperatively, and did not significantly change after 1 month postoperatively. In Group 5, the PVF was significantly lower preoperatively than at each observation timepoint after 1 months postoperatively. In Group 6, PVF was significantly lower preoperatively than 1 month postoperatively, and did not significantly change after 3 months postoperatively. There were no significant differences between the groups at any observation timepoint.
Table 4. Changes in the least mean square value of the peak vertical force (%body wight) over time.
| Pre | 1 m post | 3 m post | 6 m post | 12 m post | 18 m post | 24 m post | 36 m post | |
|---|---|---|---|---|---|---|---|---|
| Group 1 | 34.1 ± 4.5 | 48.2 ± 5.6 | 52.2 ± 4.9 | 54.0 ± 5.6 | 53.3 ± 4.5 | 60.8 ± 5.6a) | 64.1 ± 9.1 | 54.0 ± 6.6 |
| Group 5 | 28.4 ± 2.7 | 45.2 ± 2.9b) | 51.6 ± 2.7b) | 58.8 ± 3.0b) | 62.4 ± 2.8b) | 62.7 ± 3.8b) | 63.4 ± 3.6b) | 65.6 ± 4.6b) |
| Group 6 | 24.9 ± 2.4 | 37.6 ± 2.5c) | 54.2 ± 2.1c,d) | 61.5 ± 2.4c) | 60.7 ± 2.4c) | 62.7 ± 2.9c) | 62.5 ± 3.3c) | 61.2 ± 4.1c) |
Pre, prior to tibial plateau leveling osteotomy; post, postoperatively; m, months. a) P<0.05 vs. preoperative period within Group 1; b) P<0.05 vs. preoperative period within Group 5; c) P<0.05 vs. preoperative period within Group 6; d) P<0.05 vs. the previous evaluation within Group 6.
OAS
Radiographic images of typical cases in each group preoperatively and 36 months postoperatively are shown in Fig. 3. It can be seen that Groups 5 and 6 had more severe progressive OA at 36 months postoperatively compared with Group 1 in these images. The OAS values in each group are shown in Table 5. In Group 1, the OAS did not significantly change over time. In Groups 5 and 6, the OAS was significantly lower preoperatively than at each observation timepoint after 3 months postoperatively. There were still no significant changes over time within each group at 24 months postoperatively; at 36 months postoperatively, the OAS in Group 1 was significantly lower than the OAS in Group 5. Although there was no significant difference between the groups in the OAS until 24 months postoperatively, the OAS remained consistently lower in Group 1 than in Groups 5 and 6 at each observation timepoint.
Fig. 3.
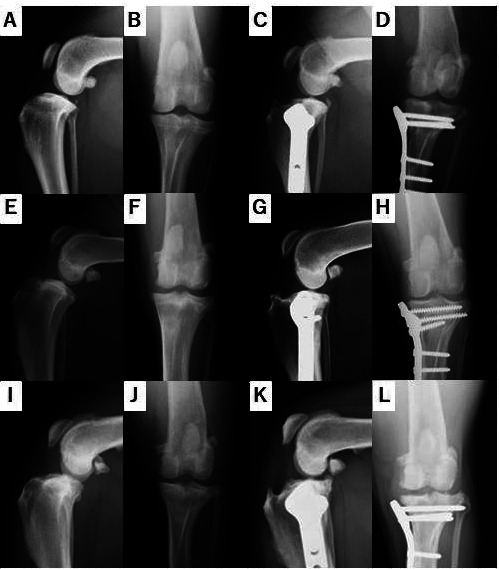
Radiographic images of typical cases from each group. Radiographic images in the (A) mediolateral direction and (B) craniocaudal direction of Group 1 before surgery. Radiographic images in the (C) mediolateral direction and (D) craniocaudal direction of Group 1 at 36 months after surgery. Radiographic images in the (E) mediolateral direction and (F) craniocaudal direction of Group 5 before surgery. Radiographic images in the (G) mediolateral direction and (H) craniocaudal direction of Group 5 at 36 months after surgery. Radiographic images in the (I) mediolateral dimension and (J) craniocaudal dimension of Group 6 before surgery. Radiographic images in the (K) mediolateral dimension and (L) craniocaudal dimension of Group 6 at 36 months after surgery.
Table 5. Changes in the least mean square value of the radiographic osteoarthritis score over time.
| Pre | 1 m post | 3 m post | 6 m post | 12 m post | 18 m post | 24 m post | 36 m post | |
|---|---|---|---|---|---|---|---|---|
| Group 1 | 15.8 ± 2.5 | 16.4 ± 2.5 | 16.6 ± 2.5 | 17.3 ± 2.5 | 17.6 ± 2.5 | 20.1 ± 3.1 | 21.1 ± 3.1 | 16.4 ± 3.1c) |
| Group 5 | 20.6 ± 1.5 | 22.4 ± 1.5 | 24.5 ± 1.5a) | 26.2 ± 1.5a) | 27.4 ± 1.5a) | 28.4 ± 1.7a) | 29.8 ± 1.7a) | 31.5 ± 2.0a,c) |
| Group 6 | 18.7 ± 1.3 | 20.5 ± 1.3 | 22.2 ± 1.3b) | 24.0 ± 1.3b) | 25.6 ± 1.3b) | 26.5 ± 1.4b) | 27.3 ± 1.4b) | 28.5 ± 1.6b) |
Pre, prior to tibial plateau leveling osteotomy; post, postoperatively; m, months. a) P<0.05 vs. preoperative period within Group 5; b) P<0.05 vs. preoperative period within Group 6; c) P<0.05 Group 1 at 36 m post vs. Group 5 at 36 m post.
Changes in the 15 sites of the OAS evaluation over time are shown in Table 6. At 5 of the 15 sites (patellar apex, proximal trochlear ridge, distal trochlear ridge, caudal aspect of the tibial plateau, and medial tibial and femoral condyles), the OAS was significantly lower preoperatively than at each observation timepoint after 3 months postoperatively. In particular, the patellar apex consistently showed the highest postoperative OAS value among the 15 sites.
Table 6. Changes in the least mean square value of the radiographic osteoarthritis score at each evaluation site over time.
| Pre | 1 m post | 3 m post | 6 m post | 12 m post | 18 m post | 24 m post | 36 m post | |
|---|---|---|---|---|---|---|---|---|
| Patellar apex | 1.7 ± 0.1 | 2.0 ± 0.1 | 2.4 ± 0.1a,b) | 3.6 ± 0.1a) | 2.8 ± 0.1a) | 3.0 ± 0.1a) | 2.9 ± 0.1a) | 2.9 ± 0.1a) |
| Patellar base | 1.4 ± 0.1 | 1.5 ± 0.1 | 1.6 ± 0.1 | 1.7 ± 0.1 | 1.8 ± 0.1a) | 1.9 ± 0.1a) | 1.9 ± 0.1a) | 1.9 ± 0.1 |
| Proximal trochlear ridge | 1.4 ± 0.1 | 1.6 ± 0.1 | 1.7 ± 0.1a) | 1.9 ± 0.1a) | 2.0 ± 0.1a) | 2.1 ± 0.1a) | 2.0 ± 0.1a) | 2.0 ± 0.1a) |
| Distal trochlear ridge | 1.2 ± 0.1 | 1.3 ± 0.1 | 1.4 ± 0.1a) | 1.5 ± 0.1a) | 1.6 ± 0.1a) | 1.8 ± 0.1a) | 1.7 ± 0.1a) | 1.7 ± 0.1 |
| Femoral condyle | 1.1 ± 0.1 | 1.1 ± 0.1 | 1.1 ± 0.1 | 1.1 ± 0.1 | 1.1 ± 0.1 | 1.2 ± 0.1 | 1.4 ± 0.1 | 1.6 ± 0.1a) |
| Tibial tuberosity | 1.0 ± 0.1 | 1.1 ± 0.1 | 1.1 ± 0.1 | 1.2 ± 0.1 | 1.2 ± 0.1 | 1.2 ± 0.1 | 1.4 ± 0.1 | 1.5 ± 0.1 |
| Cranial aspect of the tibial plateau | 1.0 ± 0.1 | 1.1 ± 0.1 | 1.2 ± 0.1 | 1.2 ± 0.1 | 1.3 ± 0.1 | 1.3 ± 0.1 | 1.4 ± 0.1 | 1.6 ± 0.1a) |
| Caudal aspect of the tibial plateau | 1.4 ± 0.1 | 1.6 ± 0.1 | 1.8 ± 0.1a,b) | 1.9 ± 0.1a) | 2.1 ± 0.1a) | 2.1 ± 0.1a) | 2.3 ± 0.1a) | 2.5 ± 0.1a) |
| Central aspect of the tibial plateau | 1.1 ± 0.1 | 1.3 ± 0.1 | 1.4 ± 0.1 | 1.6 ± 0.1a) | 1.7 ± 0.1a) | 1.9 ± 0.1a) | 2.0 ± 0.1a) | 2.2 ± 0.1 |
| Popliteal surface of the femur | 1.2 ± 0.1 | 1.2 ± 0.1 | 1.2 ± 0.1 | 1.3 ± 0.1 | 1.3 ± 0.1 | 1.4 ± 0.1 | 1.4 ± 0.1 | 1.5 ± 0.1 |
| Sesamoid bone | 1.2 ± 0.1 | 1.3 ± 0.1 | 1.3 ± 0.1 | 1.3 ± 0.1 | 1.4 ± 0.1 | 1.4 ± 0.1 | 1.5 ± 0.1 | 1.7 ± 0.1a) |
| Lateral tibial and femoral condyles | 1.6 ± 0.1 | 1.8 ± 0.1 | 1.9 ± 0.1 | 1.9 ± 0.1a) | 2.1 ± 0.1a) | 2.3 ± 0.1a) | 2.3 ± 0.1a) | 2.2 ± 0.1a) |
| Medial tibial and femoral condyles | 1.4 ± 0.1 | 1.5 ± 0.1 | 1.7 ± 0.1a) | 1.8 ± 0.1a) | 1.9 ± 0.1a) | 1.9 ± 0.1a) | 2.0 ± 0.1a) | 2.0 ± 0.1a) |
| Patella | 1.0 ± 0.1 | 1.1 ± 0.1 | 1.0 ± 0.1 | 1.1 ± 0.1 | 1.2 ± 0.1 | 1.1 ± 0.1 | 1.2 ± 0.1 | 1.3 ± 0.1 |
| Intercondylar notch | 1.1 ± 0.1 | 1.2 ± 0.1 | 1.4 ± 0.1 | 1.5 ± 0.1a) | 1.7 ± 0.1a) | 1.7 ± 0.1a) | 1.8 ± 0.1a) | 1.6 ± 0.1a) |
Pre, prior to tibial plateau leveling osteotomy; post, postoperatively; m, months. a) P<0.05 vs. preoperative period; b) P<0.05 vs. the previous evaluation.
DISCUSSION
The clinical usefulness of TPLO for the treatment of CrCLR in dogs is widely recognized [5, 23]. Reports of the usefulness of TPLO are based on clinical cases evaluated with respect to various factors such as postoperative complications, function, and OA [5, 7, 8, 12, 18, 23, 25, 28]. However, the postoperative observation periods in many of these past reports were short (only about 1 year), while few have described the findings of long-term postoperative evaluation. Thus, we assessed long-term outcomes during a 36-month postoperative period in the present study.
The PVF obtained using a force plate is an effective and objective index for comparing normal and abnormal limbs [26]. In the present study, the postoperative PVF was increased compared with preoperatively, and there was sufficient function recovery from 6 months postoperatively in each group. In other words, the dogs quickly recovered their weight-bearing ability, and this was maintained for 36 months postoperatively. Krotscheck et al. compared the PVF between normal dogs versus dogs with CrCLR treated by TPLO, and found that the PVF in the TPLO group had recovered to the level of the normal dogs during both walking and trotting by 6 months postoperatively [23]. The PVF in normal dogs during trotting (1.7–2.1 m/sec) is reportedly about 70% [24]. In the present study, considering the possibility that the PVF may have been low due to the slightly slow walking speed, we consider that sufficient weight-bearing function was recovered after 6 months postoperatively in each group, similarly to previous reports [23]. However, the observation period in these past reports was relatively short (about 1 year postoperatively), and so the long-term weight-bearing function after TPLO has not been confirmed. Moreover, OA progresses after TPLO, and even if the unstable femorotibial joint is stabilized by TPLO, weight-bearing function may still be affected in the long-term by secondary OA. Therefore, we observed both the weight-bearing function and the OA progression in the present study. A previous study that used force plates to evaluate the weight-bearing function of dogs with stifle OA found no relationship between the OAS and the weight-bearing function [4]. Furthermore, in the present study in which the evaluation period was extended to 36 months postoperatively, despite progression of OA, weight-bearing function was maintained for a long time after TPLO. This suggests that there is only a small association between the degree of OA and the weight-bearing function. In particular, we confirmed that the PVF after TPLO was recovered as early as 6 months after surgery, and was maintained for up to 36 months postoperatively. Furthermore, the PVF did not significantly differ between the groups, and our data confirmed that TPLO enables the maintenance of long-term weight-bearing function, even in stifles with complete CrCLR and MM injury.
In the present study, the OAS was evaluated in accordance with a previously described method that has been shown to result in small intra- and interobserver errors [36]. In the present study, OA progression was confirmed in the complete CrCLR group (comprising Groups 5 and 6) from as early as 3 months after TPLO. In the partial CrCLR with remaining functions group (Group 1), OA progression was slow and was maintained at a lower score than in the other groups. At 5 of the 15 evaluated sites, an increase in the OAS was observed from the early stage. In particular, the patellar apex consistently showed the highest OAS value among the 15 sites from the preoperative period to 36 months postoperatively. Kahn et al. reported that dogs euthanized 3 weeks after CrCL resection had developed damage of the femur and tibial cartilage that contacted the caudal horn of the MM, and osteophytosis at the patellar apex [21]. Additionally, osteophytosis at the cranial aspect of the stifle joint, such as osteophytosis at the patella and femoral trochlea, reportedly limits the extension of the stifle after TPLO [28]. That is, osteophytosis at the cranial aspect of the stifle after TPLO may be associated with postoperative function, and one reason for this may be preservation of the instability of the patellofemoral joint by CrCLR. Rayward et al. reported a significant increase in the OAS from preoperatively to 6 months postoperatively, but progression of OA was not confirmed in 60% of the stifles [28]. Additionally, the OAS was significantly higher in stifles with than without MM damage preoperatively, but the presence or absence of MM damage did not affect the progression of postoperative OA [28]. However, the authors used an OAS with a scoring classification of 0 to 5 points for the entire stifle [28], which may have made it difficult to detect minor changes. As the evaluation criteria for OA differs between past studies, it is difficult to simply compare the results obtained in the present study with the results of each past report. However, as the OAS reportedly does not change [28],it seems that the progression of OA after TPLO has a complicated association with various factors such as the TPA of the affected stifle joint, the degree of pathological abnormality of the stifle joints before surgery, the method of surgical treatment of the inter-articular structures, the postoperative exercise frequency, and weight change [13, 18, 22].
Acute rupture caused by trauma is the most common mechanism of CrCLR in humans, whereas CrCLR in dogs more often occurs due to chronic ligament degeneration that occurs over time [11]. The chronic progression toward CrCLR in dogs is also called “cruciate disease”. Cruciate disease is characterized by cartilage metaplasia in the CrCL [19], microfracture by weakening, and eventual partial tearing followed by complete CrCLR [14, 15]. Hulse et al. reported that the extent of injury of the articular cartilage after TPLO depends on the degree of CrCL damage [18]. They evaluated the articular cartilage by arthroscopy after TPLO and found that when the CrCL function was preserved, the articular cartilage was normal or nearly normal, and the degeneration of the CrCL was suppressed, whereas when the CrCL function was not preserved, the degree of damage of the articular cartilage worsened [18]. These findings indicate a possible protective effect of the CrCL. A recent ex vivo study showed that the smaller the TPA created by TPLO, the lesser the CrCL strain during compression in the stifle [16]. CrCLR treatment that aims to achieve small corrections in the TPA, such as TPLO, has a residual protective effect on the CrCL that slows the progression of ligament degeneration, prevents complete ligament rupture, and minimizes joint instability. In addition, a partial rupture remaining in the CrCL prompts biological effects such as changes to the blood supply of the ligament and mechanoreceptors in the CrCL [1, 2, 6]. These factors may explain why Group 1 showed a consistently lower OAS than Groups 5 and 6 in the present study. However, the progression of OA in Groups 5 and 6 was slower after than before 6 months postoperatively. Increased instability in stifles with CrCLR is thought to increase the progression of OA and periarticular fibrosis. TPLO dynamically stabilizes the CrTT that occurs in the stance phase, while it is thought that stabilization in the swing phase and stabilization of rotation in the stance phase are insufficient. Furthermore, Tashman et al. reported that although there is a large amount of displacement in the craniocaudal direction (10 mm), this decreases to about 5 mm by 2 years after CrCL excision; this is thought to be due to OA progression and periarticular fibrosis [33]. Considering the degenerative changes of the CrCL and the potential progression of OA in dogs undergoing CrCLR, we speculate that periarticular fibrosis was accompanied by OA in the affected stifle joint at the time of the TPLO operation in many cases in the present study. In other words, because of the instability in internal and external rotation of the femorotibial joint and the surgical invention associated with arthrotomy, the periarticular fibrosis further progressed after TPLO, resulting in the possibility of stabilization of the stifles.
In the present study, we found no significant difference between the groups in the OAS at each timepoint. However, Group 1 comprised only five cases, which may have led to a lack of statistical significance compared with the other groups. In addition, a past ex vivo study of MM damage revealed that the detection power is better when using arthroscopy rather than arthrotomy [27]. The present study used arthrotomy, and so there may have been false-negative cases. Previous reports suggest that TPLO induces progression of stifle OA after surgery, but the correlation between the OA findings and the function of the affected limb remains unclear [4]. The development of OA after TPLO is reportedly associated with a decrease in the range of motion of the stifle joint [20]. Focusing on weight-bearing function, it is also known that PVF increases with a limited range of motion of the knee joint in humans [9]. Therefore, the PVF might have been increased as a result of the limited range of motion of the stifle joint with OA, and increased PVF may be attributed to functional stabilization or the onset of OA case-by-case. Thus, it was shown that TPLO could achieve the recovery of weight-bearing function in CrCLR cases with various conditions. However, it is known that lameness scoring increases with OA [20] and that OA causes chronic joint pain [17]. Therefore, the progression of OA may be a risk factor for a lower quality of life even if the weight-bearing function recovers after TPLO.
The present study had several limitations. First, the number of cases was small especially in Group 1, which raises the risk of type two error. Second, the included dogs ranged in weight from 15.9 kg to 60 kg. Although the BW did not significantly differ between groups, differences in BW may also affect OA progression. Third, it was not possible to clearly distinguish whether the effect of postoperative OAS progression was related to OA after CrCLR or to postoperative changes after TPLO. We consider that this may be determined by evaluating the range of motion of the stifle joint over time. However, as the present study was retrospective study, a unified measurement of range of motion has not been performed. In addition, it has not been clarified whether postoperative recovery of PVF is same as functional recovery. Consideration this issue would also require assessment of the range of motion of the joints and motion analysis during walking.
In conclusion, in the present study in which TPLO was performed to treat stifles with CrCLR, we confirmed that the weight-bearing function improved from the pre-operative period, and this improvement could be maintained for up to 36 months. Furthermore, although it was confirmed that OA progressed over time after TPLO, the increase in the OAS after surgery was considered to have only a minor effect on the weight-bearing function. Thus, CrCLR cases with various conditions could achieve the recovery of weight-bearing function after TPLO. OA progression after TPLO was confirmed from an early stage, especially in stifles with complete CrCLR. In contrast, progression of OA was gradual in the stifles with partial CrCLR, and progression was not confirmed in every case. The progression of OA may be a risk factor for a lower quality of life even if the weight-bearing function recovers after TPLO. Therefore, these data suggest that TPLO may be the preferred treatment in the early stages of cruciate disease in dogs.
Acknowledgments
We thank Dr. Tatsuyuki Yoshida for performing the statistical analysis. No third-party funding or support was received in connection with this study or the writing or publication of the manuscript.
REFERENCES
- 1.Adachi N., Ochi M., Uchio Y., Iwasa J., Ryoke K., Kuriwaka M.2002. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop. Scand. 73: 330–334. doi: 10.1080/000164702320155356 [DOI] [PubMed] [Google Scholar]
- 2.Arcand M. A., Rhalmi S., Rivard C. H.2000. Quantification of mechanoreceptors in the canine anterior cruciate ligament. Int. Orthop. 24: 272–275. doi: 10.1007/s002640000153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arnoczky S. P., Marshall J. L.1977. The cruciate ligaments of the canine stifle: an anatomical and functional analysis. Am. J. Vet. Res. 38: 1807–1814. [PubMed] [Google Scholar]
- 4.Au K. K., Gordon-Evans W. J., Dunning D., O’Dell-Anderson K. J., Knap K. E., Griffon D., Johnson A. L.2010. Comparison of short- and long-term function and radiographic osteoarthrosis in dogs after postoperative physical rehabilitation and tibial plateau leveling osteotomy or lateral fabellar suture stabilization. Vet. Surg. 39: 173–180. doi: 10.1111/j.1532-950X.2009.00628.x [DOI] [PubMed] [Google Scholar]
- 5.Bergh M. S., Sullivan C., Ferrell C. L., Troy J., Budsberg S. C.2014. Systematic review of surgical treatments for cranial cruciate ligament disease in dogs. J. Am. Anim. Hosp. Assoc. 50: 315–321. doi: 10.5326/JAAHA-MS-6356 [DOI] [PubMed] [Google Scholar]
- 6.Bray R. C., Leonard C. A., Salo P. T.2002. Vascular physiology and long-term healing of partial ligament tears. J. Orthop. Res. 20: 984–989. doi: 10.1016/S0736-0266(02)00012-8 [DOI] [PubMed] [Google Scholar]
- 7.Coletti T. J., Anderson M., Gorse M. J., Madsen R.2014. Complications associated with tibial plateau leveling osteotomy: a retrospective of 1519 procedures. Can. Vet. J. 55: 249–254. [PMC free article] [PubMed] [Google Scholar]
- 8.Cook J. L., Luther J. K., Beetem J., Karnes J., Cook C. R.2010. Clinical comparison of a novel extracapsular stabilization procedure and tibial plateau leveling osteotomy for treatment of cranial cruciate ligament deficiency in dogs. Vet. Surg. 39: 315–323. doi: 10.1111/j.1532-950X.2010.00658.x [DOI] [PubMed] [Google Scholar]
- 9.Cook T. M., Farrell K. P., Carey I. A., Gibbs J. M., Wiger G. E.1997. Effects of restricted knee flexion and walking speed on the vertical ground reaction force during gait. J. Orthop. Sports Phys. Ther. 25: 236–244. doi: 10.2519/jospt.1997.25.4.236 [DOI] [PubMed] [Google Scholar]
- 10.de Bruin T., de Rooster H., Bosmans T., Duchateau L., van Bree H., Gielen I.2007. Radiographic assessment of the progression of osteoarthrosis in the contralateral stifle joint of dogs with a ruptured cranial cruciate ligament. Vet. Rec. 161: 745–750. doi: 10.1136/vr.161.22.745 [DOI] [PubMed] [Google Scholar]
- 11.Duval J. M., Budsberg S. C., Flo G. L., Sammarco J. L.1999. Breed, sex, and body weight as risk factors for rupture of the cranial cruciate ligament in young dogs. J. Am. Vet. Med. Assoc. 215: 811–814. [PubMed] [Google Scholar]
- 12.Fitzpatrick N., Solano M. A.2010. Predictive variables for complications after TPLO with stifle inspection by arthrotomy in 1000 consecutive dogs. Vet. Surg. 39: 460–474. doi: 10.1111/j.1532-950X.2010.00663.x [DOI] [PubMed] [Google Scholar]
- 13.Fujita Y., Hara Y., Ochi H., Nezu Y., Harada Y., Yogo T., Orima H., Tagawa M.2006. The possible role of the tibial plateau angle for the severity of osteoarthritis in dogs with cranial cruciate ligament rupture. J. Vet. Med. Sci. 68: 675–679. doi: 10.1292/jvms.68.675 [DOI] [PubMed] [Google Scholar]
- 14.Hayashi K., Frank J. D., Dubinsky C., Zhengling H., Markel M. D., Manley P. A., Muir P.2003. Histologic changes in ruptured canine cranial cruciate ligament. Vet. Surg. 32: 269–277. doi: 10.1053/jvet.2003.50023 [DOI] [PubMed] [Google Scholar]
- 15.Hayashi K., Frank J. D., Hao Z., Schamberger G. M., Markel M. D., Manley P. A., Muir P.2003. Evaluation of ligament fibroblast viability in ruptured cranial cruciate ligament of dogs. Am. J. Vet. Res. 64: 1010–1016. doi: 10.2460/ajvr.2003.64.1010 [DOI] [PubMed] [Google Scholar]
- 16.Haynes K. H., Biskup J., Freeman A., Conzemius M. G.2015. Effect of tibial plateau angle on cranial cruciate ligament strain: an ex vivo study in the dog. Vet. Surg. 44: 46–49. [DOI] [PubMed] [Google Scholar]
- 17.Hielm-Björkman A. K., Kapatkin A. S., Rita H. J.2011. Reliability and validity of a visual analogue scale used by owners to measure chronic pain attributable to osteoarthritis in their dogs. Am. J. Vet. Res. 72: 601–607. doi: 10.2460/ajvr.72.5.601 [DOI] [PubMed] [Google Scholar]
- 18.Hulse D., Beale B., Kerwin S.2010. Second look arthroscopic findings after tibial plateau leveling osteotomy. Vet. Surg. 39: 350–354. doi: 10.1111/j.1532-950X.2010.00676.x [DOI] [PubMed] [Google Scholar]
- 19.Ichinohe T., Kanno N., Harada Y., Yogo T., Tagawa M., Soeta S., Amasaki H., Hara Y.2015. Degenerative changes of the cranial cruciate ligament harvested from dogs with cranial cruciate ligament rupture. J. Vet. Med. Sci. 77: 761–770. doi: 10.1292/jvms.14-0383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jandi A. S., Schulman A. J.2007. Incidence of motion loss of the stifle joint in dogs with naturally occurring cranial cruciate ligament rupture surgically treated with tibial plateau leveling osteotomy: longitudinal clinical study of 412 cases. Vet. Surg. 36: 114–121. doi: 10.1111/j.1532-950X.2006.00226.x [DOI] [PubMed] [Google Scholar]
- 21.Kahn D., Mittelstaedt D., Matyas J., Qu X., Lee J. H., Badar F., Les C., Zhuang Z., Xia Y.2016. Meniscus induced cartilaginous damage and non-linear gross anatomical progression of early-stage osteoarthritis in a canine model. Open Orthop. J. 10: 690–705. doi: 10.2174/1874325001610010690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim S. E., Pozzi A., Banks S. A., Conrad B. P., Lewis D. D.2009. Effect of tibial plateau leveling osteotomy on femorotibial contact mechanics and stifle kinematics. Vet. Surg. 38: 23–32. doi: 10.1111/j.1532-950X.2008.00470.x [DOI] [PubMed] [Google Scholar]
- 23.Krotscheck U., Nelson S. A., Todhunter R. J., Stone M., Zhang Z.2016. Long term functional outcome of tibial tuberosity advancement vs. tibial plateau leveling osteotomy and extracapsular repair in a heterogeneous population of dogs. Vet. Surg. 45: 261–268. doi: 10.1111/vsu.12445 [DOI] [PubMed] [Google Scholar]
- 24.Lascelles B. D., Roe S. C., Smith E., Reynolds L., Markham J., Marcellin-Little D., Bergh M. S., Budsberg S. C.2006. Evaluation of a pressure walkway system for measurement of vertical limb forces in clinically normal dogs. Am. J. Vet. Res. 67: 277–282. doi: 10.2460/ajvr.67.2.277 [DOI] [PubMed] [Google Scholar]
- 25.Lazar T. P., Berry C. R., deHaan J. J., Peck J. N., Correa M.2005. Long-term radiographic comparison of tibial plateau leveling osteotomy versus extracapsular stabilization for cranial cruciate ligament rupture in the dog. Vet. Surg. 34: 133–141. doi: 10.1111/j.1532-950X.2005.00021.x [DOI] [PubMed] [Google Scholar]
- 26.McLaughlin R. M.2001. Kinetic and kinematic gait analysis in dogs. Vet. Clin. North Am. Small Anim. Pract. 31: 193–201. doi: 10.1016/S0195-5616(01)50045-5 [DOI] [PubMed] [Google Scholar]
- 27.Pozzi A., Hildreth B. E., 3rd., Rajala-Schultz P. J.2008. Comparison of arthroscopy and arthrotomy for diagnosis of medial meniscal pathology: an ex vivo study. Vet. Surg. 37: 749–755. doi: 10.1111/j.1532-950X.2008.00442.x [DOI] [PubMed] [Google Scholar]
- 28.Rayward R. M., Thomson D. G., Davies J. V., Innes J. F., Whitelock R. G.2004. Progression of osteoarthritis following TPLO surgery: a prospective radiographic study of 40 dogs. J. Small Anim. Pract. 45: 92–97. doi: 10.1111/j.1748-5827.2004.tb00209.x [DOI] [PubMed] [Google Scholar]
- 29.Ritzo M. E., Ritzo B. A., Siddens A. D., Summerlott S., Cook J. L.2014. Incidence and type of meniscal injury and associated long-term clinical outcomes in dogs treated surgically for cranial cruciate ligament disease. Vet. Surg. 43: 952–958. doi: 10.1111/j.1532-950X.2014.12220.x [DOI] [PubMed] [Google Scholar]
- 30.Robinson D. A., Mason D. R., Evans R., Conzemius M. G.2006. The effect of tibial plateau angle on ground reaction forces 4–17 months after tibial plateau leveling osteotomy in Labrador Retrievers. Vet. Surg. 35: 294–299. doi: 10.1111/j.1532-950X.2006.00147.x [DOI] [PubMed] [Google Scholar]
- 31.Slocum B., Devine T.1983. Cranial tibial thrust: a primary force in the canine stifle. J. Am. Vet. Med. Assoc. 183: 456–459. [PubMed] [Google Scholar]
- 32.Slocum B., Slocum T. D.1993. Tibial plateau leveling osteotomy for repair of cranial cruciate ligament rupture in the canine. Vet. Clin. North Am. Small Anim. Pract. 23: 777–795. doi: 10.1016/S0195-5616(93)50082-7 [DOI] [PubMed] [Google Scholar]
- 33.Tashman S., Anderst W., Kolowich P., Havstad S., Arnoczky S.2004. Kinematics of the ACL-deficient canine knee during gait: serial changes over two years. J. Orthop. Res. 22: 931–941. doi: 10.1016/j.orthres.2004.01.008 [DOI] [PubMed] [Google Scholar]
- 34.Thieman K. M., Pozzi A., Ling H. Y., Lewis D.2010. Comparison of contact mechanics of three meniscal repair techniques and partial meniscectomy in cadaveric dog stifles. Vet. Surg. 39: 355–362. doi: 10.1111/j.1532-950X.2010.00661.x [DOI] [PubMed] [Google Scholar]
- 35.Warzee C. C., Dejardin L. M., Arnoczky S. P., Perry R. L.2001. Effect of tibial plateau leveling on cranial and caudal tibial thrusts in canine cranial cruciate-deficient stifles: an in vitro experimental study. Vet. Surg. 30: 278–286. doi: 10.1053/jvet.2001.21400 [DOI] [PubMed] [Google Scholar]
- 36.Wessely M., Brühschwein A., Schnabl-Feichter E.2017. Evaluation of intra- and inter-observer measurement variability of a radiographic stifle osteoarthritis scoring system in dogs. Vet. Comp. Orthop. Traumatol. 30: 377–384. doi: 10.3415/VCOT-16-09-0134 [DOI] [PubMed] [Google Scholar]