Abstract
Introduction
Recently, interest in the problem of proper prevention and monitoring of pain, especially acute, has been increasing in relation to various age groups. Greater awareness of the problem prompts discussion about the purpose of analgesia in newborns treated with mechanical ventilation.
Aim
The purpose of the systematic review was to analyze current research on the use of pain scales in newborns treated with mechanical ventilation in the Neonatal Intensive Care Unit.
Methods
Medline databases: PubMed, OVID, EBSCO, Web of Science and Cochrane Library were traced using the appropriate keywords. The search was limited to studies in English. The review took into account the years 2006–2019. Considering the criteria, 12 articles were included in further analysis, to which full access was obtained.
Results
The analyzed scientific research showed differences in beliefs about the validity and credibility of the scales used. Researchers indicated that staff with practical experience in using scales in their daily practice was very skeptical of the results obtained on their basis.
Conclusion
Based on this review, no explicit evidence can be obtained to support the use of one proper scale in pain assessment. It can be inferred that the COMFORT and N-PASS scales are effective for pain assessment and for determining the need for analgesics in mechanically ventilated neonates. These scales may be equally effective in assessing chronic pain, especially in mechanically ventilated children. On the other hand, the PIPP and CRIES scales are most commonly recommended for assessing acute and postoperative pain.
Keywords: pain, scales, newborn, NICUs
Introduction
The issue of adequate prophylaxis and therapy of pain has become a matter of growing concern in recent years.1,2 The increased recognition of this problem has led to a discussion about the usefulness of analgesia in neonates receiving mechanical ventilation.3,4 It is well known that the lower the gestational age of the child, the lower the threshold and higher the sensitivity for pain. Available studies clearly indicate that pain signals reach the brain as early as in the 22nd week of gestation, whereas corticothalamic tracts, which are responsible for the conscious perception of pain, develop in the 29th week of gestation.5 Due to the fact that the nervous system is still very undeveloped, most prematures present a lower pain threshold, which is associated with the high density of receptors in supraspinal centres. Despite these scientific reports, researchers are still unable to determine how much pain neonates feel consciously. On the other hand, however, the analysis of available literature reveals the negative impact that pain and distress have on the further psychomotor development of the affected child. It has been proven that neonates are equipped with all systems required for pain perception from the moment of their birth, yet they are not capable of defending themselves against excessive pain, due to the increased excitability of metabolic and endocrine systems.1,2,6
Specification and Classification of Pain in Neonates
Diagnosing and assessing pain in neonates is a challenge for medical personnel, due to the inhibited identification of whether this is an expression of pain experience or perhaps the effect of a situation that is unpleasant for the child, for example, hunger. Clinical observations indicate that patients of intense therapy wards are subject on average to 7.5–17.3 procedures per day, which are a source of stress, anxiety and pain.7,8
Progress in clinical research, including in the area of medical disciplines such as neonatology, shows that prevention and control as well as the soothing of pain bring both short- and long-term benefits, both to full-term and pre-term newborns. A nociceptive stimulus that is repeated systematically for a longer period will cause disorders in the central nervous system, leading finally to irreversible changes, including: the transformation of acute pain into chronic pain, hyperalgesia, a deficit in pain expression and psychophysiological effects in adult life.9–12
The knowledge of medical personnel regarding the mechanism and indicators of pain in neonates helps in the prophylactics, monitoring and alleviation of pain. The mode of reacting to pain as well as its intensity is an individual characteristic of every neonate and undoubtedly depends, to a large degree, on the level of neonate maturity. The reactions of a neonate to pain stimuli can be divided into physiological, behavioural, hormonal, metabolic and mental. A detailed list of pain indicators is presented in Table 1.2,13,14
Table 1.
| Physiological | Behavioural | Hormonal Metabolic | Psychological |
|---|---|---|---|
|
|
|
|
An essential element in monitoring a pain experience is the identification and knowledge of its source. Based on the relevant literature, the following types of pain have been distinguished in neonatal intensive care units:
1. pain due to procedures, so-called procedural pain;
2. pain related to an illness:
a) acute pain that persists,
In the case of the frequently described procedural pain, its source should be sought in the diagnostic-therapeutic procedures conducted every day on neonates. When analysing pain due to the level of experienced pain, the procedures are distinguished into those with:
mild pain intensity, eg, venepuncture or artery puncture, subcutaneous and intramuscular injections, and urinary bladder catheterization;
moderate pain intensity, eg, bronchial toilet, lumbar puncture, intubation, heel puncture, and physiotherapy of the respiratory system; and
acute pain intensity, eg, applying a drain into a pleural cavity, and surgical interventions.
One source of acute pain experiences is conditions after surgical procedures, when the continuity of skin and of deeper structures, for example, muscles, is interrupted. Chronic pain in neonates, although it is not a new subject, continues to be difficult to define. Numerous researchers agree that causes of chronic pain in neonates include perinatal necrotizing enterocolitis, meningitis, and systematically repeated nociceptive stimuli, such as persistent ailments after surgical operations as well as mechanical ventilation.17–20
The introduction in every healthcare centre of the duty to monitor and soothe pain symptoms in children is reflected in the recommendations of domestic and international Scientific Societies. This is also an indisputable right of every human being. Actions taken to prevent pain in healthcare centres that treat the youngest patients also meet the expectations of the parents of children who experience pain and suffering.6,21
The interpretation of pain sensations in such a different population as neonates can be realistic through the careful and comprehensive observation of the child and the application of an adequate assessment tool (scale) which will be suitable for the age group and the clinical condition of the patient. According to the recommendations of Scientific Societies, a neonate intensive therapy unit should prepare an individual programme of therapy and the prevention of pain based on state-of-the-art standards. The success of actions taken is possible only if all personnel respect the recommendations, which include: systematic monitoring of potential and actual pain symptoms, minimising the number of painful procedures, prophylactics and soothing of acute pain due to invasive procedures and postoperative pain, counteracting stress symptoms and acute pain.6,22 The repeatability and long-term character of invasive breathing support cause excitation and stress in a neonate. This leads to changes regarding psychophysiological, endocrinal and behavioural fields, resulting in chronic stress.23 The assessment of pain in invasively ventilated neonates is difficult, in particular in pre-term newborns, which have a limited behavioural repertoire and a higher sensitivity to pain threshold.24,25 Validated and implemented tools used to measure pain have been developed mostly within research into acute procedural pain, which is directly related to the number of performed invasive procedures at intensive therapy wards.26,27
Aim
The aim of this systematic review was to analyse current studies on the use of pain scales in neonates receiving mechanical ventilation in neonatal intensive care units (NICUs).
Materials and Methods
This systematic review was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations. The protocol of selecting papers was based on the Cochrane Handbook for Systematic Reviews of Interventions, PICOS model.28 Papers included for further analysis were assessed using the Newcastle–Ottawa Survey (NOS) scale. The above-mentioned tool was developed in order to assess properly the quality of research included in the systematic review or meta-analysis. The maximum number of available points in three different dimensions amounted to 9. The scale assesses three main categories, including the selection of the study group, the comparability of the groups; and the ascertainment of either the exposure or outcome of interest for case-control or cohort studies, respectively. Assessed papers are scored with a star system. The scale was validated and was recognised by a number of authors of systematic reviews.29
Search Strategy
The following databases were searched: PubMed, OVID, EBSCO, Cochrane Library and Web of Science. The following key words were used for verification: pain, neonatal intensive care unit, neonate, scales and mechanical ventilation. Single key words or their combinations using AND, OR or both operators were entered. The search was limited to studies published in English and carried out in the period between 2006 and 2019. The timeframe for preparing the review results from a relatively low number of publications that concern pain in neonatology patients. Moreover, the first recommendations and guidelines concerning pain therapy in neonates were developed in 2006 by the American Academy of Pediatrics and the Canadian Pediatric Society, which were the first to recommend that healthcare systems include programmes of pain assessment and prevention in neonatology wards as routine actions for personnel.30 The number of citations for each search attempt was scanned and reduced according to the inclusion criteria.
The selection of suitable papers was based on the PICOS model framework. The individual criteria of searching for scientific research concerned the following: P – neonates, I – pain experience during mechanical ventilation, C – pain scale used in the assessment of pain in pediatric patients, S – experimental studies, randomized trail study (Table 2).28
Table 2.
Selection Criteria for the Systematic Review (PICOS)28
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| P (participants) | Neonate population. | Studies on adult humans. |
| I (intervention) | Pain experiences during mechanical ventilation. | N/A |
| C (comparison) | Pain scales. | N/A |
| O (outcome) | The assessment of the proper pain scale. | Studies which investigate pain on the basis of different scales. |
| S (study type) | Randomized trial study; Experimental study; Prospective study. |
Review article, conference communication, case studies, editorials, diary studies. |
Study Selection
Only papers describing studies that had been carried out in neonatal intensive care units and which analysed the efficacy of pain assessment using different scales were selected for further analysis. This selection was based on specific inclusion criteria. The search spectrum was limited to neonatal patients who required mechanical ventilation.
Inclusion Criteria
* studies evaluating the efficacy of tools for pain assessment in neonates being treated in NICUs,
* studies which included patients admitted to NICUs, mechanically ventilated,
* studies analysing tools for pain assessment in an NICU setting, which were designed for medical personnel (nurses, physicians).
The eligibility of each paper found was assessed according to the availability of the full-text version and an independent evaluation performed by two reviewers using the above-mentioned inclusion criteria. In cases where the two reviewers did not reach a consensus to qualify the article for further assessment, the paper was consulted by a third reviewer.
Data Extraction
The initially eligible papers were assessed by two independent reviewers, who used a normalised data extraction form. The following criteria were taken into account: author, publication year, type and aim of the study, method of pain assessment and limitations of the study.
The quality of the study was assessed based on the following:
● description of the inclusion and exclusion criteria,
● study method,
● type of study.
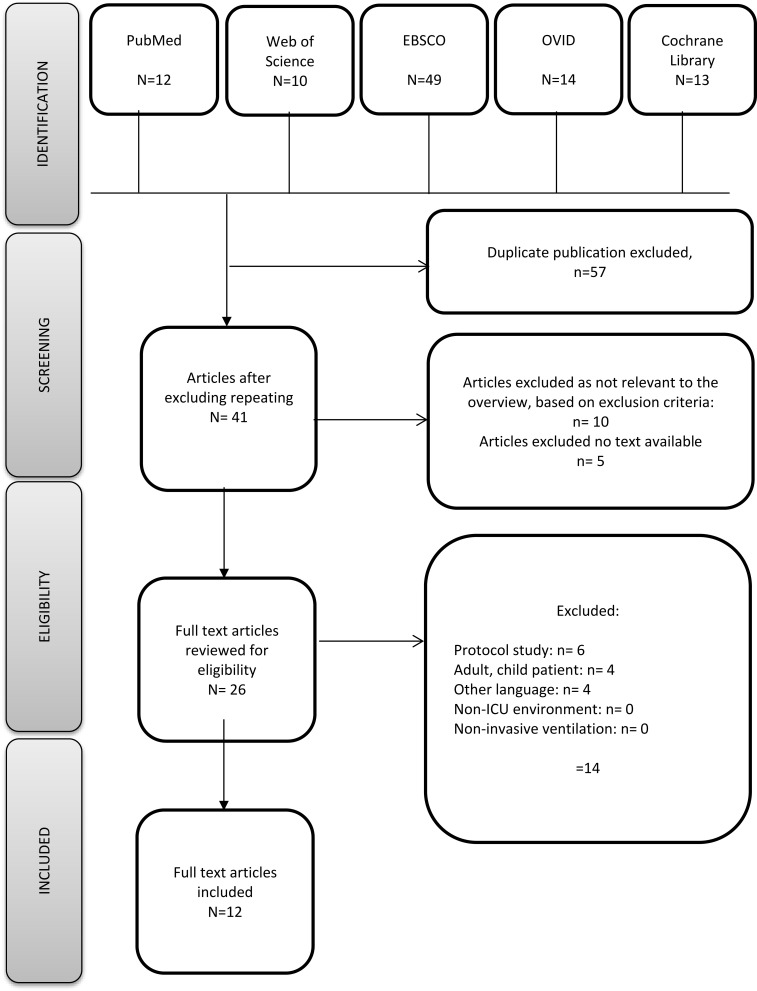
Finally, out of 27 articles, 12 papers were considered eligible for the review (Figure 1). Manuscripts covered by the review were given a minimum of 7 points in the NOS scale. A detailed list of the assessment results is given in Table 3.
Figure 1.
The flowchart of the selection process.
Table 3.
Quality Assessment of the Included Studies Using the Newcastle–Ottawa Scale
| First Author, Year | Study Design | Selection* | Comparability* | Exposure/Outcome* | Total Scores | |
|---|---|---|---|---|---|---|
| 1 | Cignacco E., et al, 200833 | Randomized controlled trial. | ∗∗∗∗ | ∗ | ∗∗∗ | 8 |
| 2 | Hummel P., et al, 200834 | Prospective study. | ∗∗∗∗ | ∗ | ∗∗∗ | 8 |
| 3 | e Silva YP., et al, 200835 | Randomized double-blind study. | ∗∗∗ | ∗ | ∗∗∗ | 7 |
| 4 | van Dijk M., et al, 200932 | Retrospective cohort study. | ∗∗∗∗ | ∗ | ∗∗∗ | 8 |
| 5 | Williams AL., et al, 200925 | Retrospective cohort study. | ∗∗∗∗ | ∗ | ∗∗∗ | 8 |
| 6 | Chrysostomou C., et al, 201441 | Prospective study. | ∗∗∗ | ∗ | ∗∗∗ | 7 |
| 7 | Acikgoz A., et al, 201536 | Experimental study. | ∗∗∗∗ | ∗ | ∗∗∗∗ | 9 |
| 8 | Cardoso JM., et al, 201737 | Randomized study. | ∗∗∗ | ∗ | ∗∗∗ | 7 |
| 9 | Desai A., et al, 201731 | Prospective study. | ∗∗∗∗ | ∗ | ∗∗∗ | 8 |
| 10 | Abiramalatha T., et al, 201838 | Randomized study. | ∗∗∗ | ∗∗ | ∗∗∗ | 7 |
| 11 | Huang XZ., et al, 201839 | Prospective study. | ∗∗∗∗ | ∗ | ∗∗∗∗ | 9 |
| 12 | Desai A., et al, 201840 | Prospective study. | ∗∗∗∗ | ∗∗ | ∗∗∗ | 9 |
Notes: *A star is awarded for each numbered item within the selection and outcome categories. A maximum of two stars can be given for comparability.
Results
As part of the search of the library-abstract databases, 98 publications were obtained in total (12 from PubMed, 14 from OVID, 49 from EBSCO, 13 from Cochrane Library and 10 from Web of Science). After excluding 57 duplicates, 41 papers were analysed; the full-text analysis was verified as well as the eligibility criteria for the research. Initially, 12 papers that fulfilled the criteria were included in the review. Having assessed the quality of the included papers with the Newcastle–Ottawa Scale, they were then taken into consideration in the review. They focus on mechanically ventilated neonates (except for 3 studies,25,31,32 in which also neonates that were breathing efficiently were covered; however, every group was analysed separately).
In their papers, notwithstanding their purpose, the authors apply suitable tools recommended by the Scientific Societies to measure every type of pain experience. Two studies concern the simultaneous evaluation of procedural pain and chronic pain (N-PASS and NIPS scales were applied), five studies use scales for assessing procedural pain (PIPP was used most often), and five to measure the chronic pain sensation (N-PASS was used most often). In studies by Hummel et al (2008), van Dijk et al (2009), Desai et al (2017) and Huang et al (2018), a primary objective was to assess the efficiency and reliability of tools to measure pain experience. Other papers analysed analgesia, the impact of an open and closed sucking system to assess pain experiences in mechanically ventilated neonates, and behavioural reactions in neonates (Table 4).25,31-41
Table 4.
Systematic Review of Papers Presenting Studies Using Pain Scales in Neonates Treated with Mechanical Ventilation
| Author/Year of Publication | Type of the Study | Aim of the Study | Study Group/Sample Size (N) | Instrument Used to Measure Pain | Character of Pain | Outcomes of Measurement | Conclusion | Limitation of the Study |
|---|---|---|---|---|---|---|---|---|
| Cignacco E., Hamers JP, van Lingen RA. (2008) 33 |
Randomized study. | The aim of the study was to assess the impact of morphine and non-pharmacological methods on pain and stress reduction during endotracheal suctioning of bronchial secretion. | 30 mechanical ventilated neonates | PIPP scale BPSN scale (Bernese Pain Scale for Neonates) |
Procedural pain. | The average pain scores were higher in preterms who received sensorial stimulation as compared to the standard of care, even in the placebo group. | The researcher used the recommended scales. Nurses reported significant problems with pain assessment using the PIPP scale, since it focuses mainly on an infant’s facial expressions. |
A small number of patients included in the study. |
| Hummel P., Puchalski M., Creech SD., Weiss MG. (2008) 34 |
Prospective study. | The aim of the study was to assess the utility and reliability of N-PASS in mechanically ventilated neonates and/or after a postoperative surgery. | 46 mechanical ventilated neonates | N-PASS scale, PIPP scale |
Chronic pain. | N-PASS is a clinically useful, reliable and important tool used to assess persistent pain/excitation and sedation in ventilated children and/or children after a postoperative procedure. | The researcher used the recommended scales in the study. It confirms the reliability of the scale. |
A small number of patients included in the study. |
| e Silva YP., Gomez RS., Marcatto J de O., Maximo TA., Barbosa RF., e Silva CS., (2008) 35 |
Randomized in a prospective double-blinded study. | The aim of the present study was to compare a continuous infusion of remifentanil and morphine during mechanical ventilation of premature neonates with respiratory distress syndrome (RDS). | 20 mechanical ventilated neonates | NIPS scale, COMFORT scale |
Chronic pain. | Both infusions provided adequate analgesia and sedation, as demonstrated by the NIPS (<4) and COMFORT scales (<20). |
The researcher used the recommended scales in the study. No reference to the scale. |
A small number of patients included in the study. |
| van Dijk M., Roofthooft DW., Anand KJ., Guldemond F. et al (2009) 32 |
Prospective cohort study. | The aim of this study was to validate the COMFORTneo scale. | 286 neonates:
|
COMFORTneo scale | Chronic pain. | The COMFORTneo scale showed initial usefulness both in preterms and in term neonates. | Further studies are recommended to establish validity with other instruments of pain control in a patient group with a high probability of ongoing pain. | The measurement of pain intensity by the same person, a nurse, in all the scales, may result in the lower objectivity of the assessment. To compare, the use of a validated scale to assess pain in a neonate might give a better picture of the utility of the COMFORTneo tool. |
| Williams AL., Khattak AZ., Garza CN., Lasky RE. (2009) 25 |
Prospective cohort study. | The aim of the study was to assess the behavioural pain reaction in neonates using the NIPS scale. | 36 neonates:
|
NIPS scale | Procedural pain. | The NIPS scale proved useful in assessing pain in neonates. | The researcher used the recommended scales in the study. It confirms the reliability of the scale. |
A small number of patients included in the study. |
| Chrysostomou C., Schulman SR., Herrera CM., Cofer BE., Mitra S., Rocha MG., et al (2014) 41 |
Prospective study. | The aim of the study was to determine the pharmacokinetic impact of dexmedetomidine on pre-term and full-term newborns. | 42 mechanical ventilated neonates | N-PASS scale | Chronic pain. | The N-PASS scale revealed that dexmedetomidine provided sedation and analgesia. | The researcher used a recommended scale in the study. No reference to the scale. |
N/A |
| Acikgoz A., Yildiz S. (2015) 36 |
Experimental study. | The aim of this project was to compare the impact of open and closed suctioning systems on pain assessment in newborns treated with mechanical ventilation. | 42 neonates mechanical ventilation. | N-PASS scale | Procedural pain. | This study did not reveal any difference in the assessment of pain suffered during the evacuation of the secretion between the open and closed systems (p=0.194). The researchers noticed that the N-PASS score during endotracheal suctioning with the open system was slightly higher as compared to the closed method. | The researcher used a recommended scale in the study. The N-PASS scale is effective in measuring pain in this group of patients. |
A small number of patients included in the study. |
| Cardoso JM., Kusahara, DM., Guinsburg R., Pedreira MLG., (2017) 37 |
Randomized study. | The aim of this project was to compare the impact of open and closed suctioning systems on pain assessment in newborns treated with mechanical ventilation. | 13 neonates mechanical ventilation. | PIPP | Procedural pain. | The PIPP scale did not reveal any major differences in both studied suction techniques of an endotracheal tube. | The researcher used a recommended scale in the study. No reference to the scale. |
A small number of patients included in the study. |
| Desai SA, Nanavati RN, Jasani BB et al (2017) 31 |
Prospective study. | The aim of this study included: - the assessment of the incidence of chronic pain in neonates receiving assisted ventilation, - a comparison of the usefulness of N-PASS with PIPP in pain monitoring in mechanically ventilated neonates. |
I stage: 15 neonates receiving assisted ventilation for more than 48 hours were included in the study. The mean gestational age was 34.3 ± 4.56 weeks. II stage: 42 neonates with the mean gestational age of 33.5 ± 4.23 were included in the study. |
PIPP scale, N-PASS scale |
Chronic pain. | This study proved that neonates receiving assisted ventilation experience prolonged acute pain . the reliability of the N-PASS scale was comparable to the PIPP scale in term neonates receiving invasive ventilation. N-PASS scale is reliable and useful for the assessment of chronic pain. |
The researcher used a recommended scale in the study. It confirms that the N-PASS scale is reliable and useful in assessing chronic pain. |
The study was limited to one NICU only. |
| Abiramalatha T., Mathew SK., Mathew BS. et al (2018) 38 |
Randomized study. | The aim of this study was to assess the impact of fentanyl analgesia on the clinical status of the child depending on the method of its administration. | 100 mechanically ventilated neonates | N-PASS scale, NIPS scale |
Chronic pain. Procedural pain. |
Pain intensity was similar in both groups, regardless of the scale used. The NIPS score of 1–3 and N-PASS score (0–3) were similar, which indicates adequate pain relief with low serum fentanyl concentrations 0.4–0.6 ng/mL. |
The researcher used a recommended scale in the study. No reference to the scale. |
N/A |
| Huang XZ., Li L., Zhou J. et al (2018) 39 |
Prospective study. | The aim of this study was to assess the reliability and clinical usefulness of three pain scales: N-PASS, NIAPAS, PIPP-R. | 90 neonates invasively ventilated. | N-PASS scale, NIAPAS scale, PIPP-R scale. | Procedural pain. |
the sensitivity and specificity of the N-PASS scale for term and preterm neonates receiving invasive ventilation is comparable to the NIAPAS and PIPP-R scales. the N-PASS scale is reliable and useful to measure acute pain. Nurses consider the N-PASS scale as more functional when being performed and more clinically useful. |
The researcher used a recommended scale in the study. The primary result of this project shows that all three scales are reliable, yet the N-PASS scale is more clinically sensitive and efficient in measuring acute pain in neonates receiving invasive ventilation, as compared to the NIAPAS and PIPP-R scales. |
A small number of mechanically ventilated patients included in the study. The study was limited to one hospital only. The sequence of using pain scales was not randomised |
| Desai A., Aucott S., Frank K., Silbert-Flagg J. (2018) 40 |
Prospective study. | The aim of this project included the assessment of: - the usefulness and reliability of the NIPS and N-PASS scales, - the quality of pain intensity measurement carried out by the personnel, - education of the personnel on the issues of pain and the tools used to assess it. |
44 mechanical ventilated neonates | N-PASS scale, NIPS scale |
Procedural pain. Chronic pain. |
The N-PASS scale is more clinically sensitive and efficient in measuring acute and chronic pain in neonates as compared to the NIPS scale. Effective education had a significant clinical impact on the improvement of the knowledge of personnel. |
The researcher used a recommended scale in the study. The researcher recommends the continuation of research, which should focus on the utility of the N-PASS scale in sedated neonates. |
The study was limited to one hospital only. |
Abbreviation: N/A, not applicable.
Many of the available papers compare both the efficacy of the scales and attempts to validate tools for acute and chronic pain assessment. The analysed material indicates that tools developed to measure acute pain in neonates have to be multidimensional and take into account the combination of physiological and behavioural symptoms. Most tools have been developed to assess pain in neonates who are not treated with mechanical ventilation. Only a few of the available scales were validated for pain assessment in mechanically ventilated children; therefore, skilful use of the adequate instrument for acute, postoperative or chronic pain assessment by NICU personnel is of crucial importance. The tool should be selected with regard to both the age of the child and the diagnostic and therapeutic methods they receive.6,42,43
Discussion
A multicentre study by Carbajal et al concerning the prophylaxis, therapy and monitoring of pain indicates that actions aimed at reducing and preventing pain should have priority in neonatal care, once neonates are admitted to NICUs.44 The analysis of data obtained from 370 neonatal intensive care units in various European countries reveals that pain was monitored with standardised scales in only 32 units, and the spectrum of scales used for pain assessment was quite wide.44,45 Results of studies carried out in other European countries, including Spain, confirm that there no uniform guidelines are available. On the other hand, following the recommendations and guidelines in pain therapy and prophylactics, including the application of scales may significantly reduce the quantities of applied opioid and sedative drugs.46
Observations revealed that pain suffered by patients receiving mechanical ventilation was principally assessed after they received analgesics or sedatives. The following scales are mostly recommended for acute pain assessment: Neonatal Infant Pain Scale (NIPS) and Premature Infant Pain Profile (PIPP). On the other hand, CRIES (crying, oxygenation, vital signs, facial expression, and sleeplessness) is recommended to assess postoperative pain, while the COMFORT and N-PASS (Neonatal-Pain, Agitation and Sedation Scale) scales are suggested for chronic pain assessment in invasively ventilated children.47 Studies by Elella et al confirmed that the COMFORT scale may be applied in children who require mechanical ventilation, including in post-surgery periods. What is more, the application of this assessment explicitly reduces the time of respirotherapy.48 Other authors suggest that no uniform guidelines for pain assessment in neonatal patients are available, despite the fact that they receive both analgesics and sedatives.44,47 A study performed in Sweden and Norway by Andersen et al compared the practice of pain assessment in NICUs.49 It revealed that in Swedish hospitals pain was assessed and documented more frequently than in Norway. The tools for pain assessment were used more often by the former as well. The most commonly used tools for measuring nociception intensity in Sweden included Astrid Lindgren’s Pain Scale (ALPS), as well as COMFORT, Échelle Douleur Inconfort Nouveau-Né (EDIN), Face, Legs, Activity, Cray, Consolability (FLACC), N-PASS and NIPS, while the Norwegians used the Echelle EDIN, ALPS, PIPP and CRIES scales. The analysis revealed that Norwegian nurses not only had more confidence in the tools used for pain assessment in children, but also recognised their validity to a greater extent than nurses working in Sweden.49 Studies analysing the usefulness and reliability of scales for pain assessment tend to evaluate acute pain. Although possible, the assessment of long-lasting or chronic pain is performed very rarely. This has been proved by Desai et al,31,40 whose primary aim was to evaluate the usefulness of the N-PASS scale for pain assessment in invasively ventilated children. The first study consisted of two phases. The initial stage was to answer the question of whether neonates receiving assisted ventilation suffer from prolonged acute pain, which was done using the PIPP scale. The second stage was to compare the N-PASS and PIPP scales in the context of prolonged acute pain assessment in neonates receiving assisted ventilation. The results confirmed that invasively ventilated neonates suffer from prolonged acute pain, as the PIPP score was over 6, which is equivalent to moderate pain. This project confirmed the reliability and usefulness of the N-PASS scale for pain assessment.31 Another project by the same authors confirmed the usefulness of the N-PASS scale for measuring chronic pain in invasively ventilated children. The primary aim of this second study was to improve the quality of pain prophylaxis and therapy in NICU patients. The authors compared the NIPS and N-PASS scales to find the most efficient tool for measuring acute and chronic pain. These analyses revealed that it is the N-PASS scale that is more adequate and more reliable for chronic and acute pain assessment in neonates. The additional advantage of this project was the fact that the nursing personnel of the neonatal units had been trained, which in turn improved their knowledge and recognition of the available tools, as well as the need for adequate pain assessment in neonates receiving assisted ventilation.40 The reliability of the N-PASS scale for pain monitoring in invasively ventilated children was also confirmed by the results of another prospective study carried out by Huang et al.39 The priority in this study was to define the reliability, feasibility and clinical usefulness of three scales, namely the N-PASS, NIAPAS (Neonatal Infant Acute Pain Assessment Scale) and PIPP-R (Premature Infant Pain Profile-Revised). This project revealed that all three scales are reliable and clinically useful. However, the N-PASS scale was more clinically sensitive and functional for acute pain assessment in mechanically ventilated neonates when compared to the NIAPAS and the PIPP-R. The evaluation of the usefulness of these scales by the personnel revealed clearly that the N-PASS scale presented greater clinical usefulness and was evaluated as better.39 Experimental studies carried out by Acikgoz and Yildiz36 seem to confirm the results presented by the above-mentioned authors. The aim of this project was to compare the intensity of pain in mechanically ventilated neonates during the evacuation of secretion from the bronchial tree with closed and open systems. These results clearly showed that the procedure itself is associated with moderate pain, whereas its intensity was assessed as slightly higher during the procedure in which the open system was used for endotracheal suctioning. The above-mentioned studies seem to confirm that the N-PASS scale is effective and useful for procedural pain measurement in mechanically ventilated neonates.36
Abiramalatha et al and Chrysostomou et al in their studies confirmed the efficiency of applying the NIPS and N-PASS scales to evaluate chronic pain experiences in neonates subject to invasive ventilation and receiving opioids.38,41
Another recommended tool to evaluate procedural pain in mechanically ventilated neonates is the PIPP scale, which was used in a randomized study by Cardoso et al. The purpose of the study was to analyse the impact of open and closed suction systems on pain assessment in neonates treated with mechanical ventilation. The study confirmed that the procedure is painful for a neonate to a mild or moderate degree.37
The selection of a reliable, feasible and practical measurement tool for pain intensity is the primary step in adequate procedural pain management for ventilated neonates. Such a tool would aid the precise identification of pain, and improve the quality of nursing care of the neonate.
The assessment of pain intensity, and its measurement and documentation in this patient group pose a challenge for the personnel of many NICUs, because differentiating between suffering and pain or stress is not an easy task. Such experiences may appear concomitantly and stimulate each other. The literature reveals that pain causes suffering, anxiety, stress and agitation. The adequate differentiation between them is clinically important, as each of these negative experiences requires a totally different method of management. An analysis of the obtained material showed that there is currently no tool (either physiological or behavioural) available which would allow a differentiation between suffering and pain. This issue is emphasised by Maaskant et al in their meta-analysis.50 They suggest that the interpretation of all information concerning the situation of the affected child is necessary in everyday practice. Data on the clinical entity, and its management or previous experience may, for example, be very valuable for the adequate assessment of suffering and pain. One of the available tools, which includes more important criteria and was originally developed to measure stress in children up to 18 years of age receiving mechanical ventilation is the COMFORT scale. A research study by Dijk et al32 confirmed the reliability of the COMFORT scale for measuring pain intensity and the level of sedation in such a population. It is currently one of the well-known and recommended methods for monitoring analgesia in invasively ventilated neonates.32,50
Apart from emphasising the problems of differentiating pain-dependent suffering, Bellieni pays special attention to other difficulties in evaluating pain. The author states that due to the complexity of multidimensional tools for pain control, each measurement should be carried out by at least two nurses. As the person who carries out the given procedure is focused on its correct realisation, this often hinders the calm and error-free observation of a child’s behaviour during measurement. Moreover, the author emphasises that none of the scales for chronic pain measurement adequately represents the true pain assessment, as the measurement is most commonly performed every 3–4 hours. Therefore, the results apply only to the time of the examination and observation.51,52
Pain monitoring is an undeniable right of every human being and patient, regardless of age. The literature reveals that neonates admitted to NICUs experience pain, which comes from multiple diagnostic, therapeutic and medical procedures. Clinical observations of children receiving mechanical ventilation indicate that such patients not only experience acute pain, but also repeatedly suffer from chronic pain. Therefore, an individual approach to each patient associated with their clinical situation is not only essential, but above all, they require the modulation of sedatives and an adequate assessment of pain. The authors of the above-mentioned studies emphasise the differences in attitudes and opinions of nursing personnel who assess the usefulness of the scales based on their practical use in everyday practice. This was especially noticed in a study carried out by Cignacco,33 where nurses reported problems with the analysis of pain intensity using the PIPP method, both for neonates with extreme prematurity and term neonates.33 The results of many studies reveal that the primary obstacle in using adequate scales is the lack of knowledge presented by nursing personnel or the lack of adequate training. This issue undoubtedly requires further analysis and research. All the authors of the presented papers emphasised that extensive education is an effective method of improving awareness among the medical personnel of the utility, and the adequate scale selection with regard to the clinical situation of the individual patient.
The guidelines of the American Academy of Paediatrics, the Canadian Paediatric Society and the Polish Neonatal Society indicate that NICU personnel should measure and document pain intensity and accompanying symptoms. The analysis of pain in such a diverse patient group as neonates is possible only by profound observation of the child and the use of methods adequate for the age group and their clinical situation. The authors of the above-mentioned guidelines emphasise that each NICU should develop its own program for the prevention and therapy of pain, which would be based on the most recent standards. The success of such actions is possible only when each member of the team complies with and follows the recommendations, including: the assessment of pain and its symptoms on an everyday basis, the reduction of painful procedures, the prophylaxis and reduction of acute pain associated with invasive procedures and postoperative pain, the prevention of stress and chronic pain. Each intervention in an NICU should include prophylactic actions with documented efficacy, ie using analgesia before every potentially painful procedure, the exclusion of unnecessary stimuli and painful procedures, support during procedures given to a neonate by the personnel or a parent, a combination of procedures and their performance at the same time, the delay of nursing activities by at least an hour from nociceptive stimulus and a combination of non-pharmacological and pharmacological methods.6,22,30
Every action aimed at the monitoring and therapy of pain in neonates has a positive impact on the child in every aspect of their functioning, ie, psychomotor, physiological and hormonal.24 Moreover, as indicated by clinical observations, the application of a pain guideline protocol increases the level of satisfaction among nursing personnel. Furthermore, it very often results in reduced doses of applied opioids.53 The lack of a single, universal scale for the assessment of pain intensity, as well as the lack of recommendations concerning pain therapy depending on age, leads to a situation where the adequate assessment of pain intensity is remarkably difficult. Some of the authors suggest that biological markers, such as stress hormones in saliva (adrenalin, cortisol), as well as examinations, such as electroencephalography, positron emission tomography, magnetic resonance imaging, near-infrared spectroscopy and NIPE, may be used to assess pain in NICU patients. The above-mentioned methods are extraordinarily objective, yet due to the relative unavailability of highly sophisticated equipment, it is impossible to use them in clinical practice.54–57
Conclusions
Despite the available guidelines and recommendations, the assessment and monitoring of pain in neonates is not a standard procedure. Moreover, the availability of many scales leads to a situation where every institution may freely choose an assessment tool.
Based on this review, no explicit evidence can be obtained to support the use of one proper scale in pain assessment. It can be inferred that the COMFORT and N-PASS scales are effective for pain assessment and for determining the need for analgesics in mechanically ventilated neonates. These scales may be equally effective in assessing chronic pain, especially in mechanically ventilated children. On the other hand, the PIPP and CRIES scales are most commonly recommended for assessing acute and postoperative pain.15,22,34,58
Strength and Limitations of the Systematic Review
The conducted analysis did not show in full which of the tools used for pain assessment should be essential in assessing pain among mechanically ventilated patients in NICUs. What is more, pain cannot be assessed explicitly if the analysed scale used to assess pain refers only and exclusively to acute or chronic pain, because, as the relevant literature indicates, pain can have different dimensions. A child that requires mechanical ventilation usually experiences both acute and chronic pain. Therefore, it is hard to determine a clear boundary. Another limitation of the analysed papers was the low number of observations, restricted, as a rule, to a single research centre and ward. Observations very often concerned a low number of patients. Moreover, the analysed material did not always include answers to the question regarding the effectiveness of the applied scales of pain assessment. There is no doubt that the strength of the conducted analysis is the number of databases that were searched through. The strict criteria for the inclusion of papers in the further research analysis using the PICOS model as well as their assessment using the Newcastle–Ottawa Scale warrant that the qualified papers meet the criteria of eligibility for the analysis. The review included only and exclusively research, prospective, randomized or experimental papers, which also affects the benefits of the conducted analysis. One potential limitation of the paper may be the fact that the selected papers are only and exclusively in English, which may naturally exclude papers dedicated to pain issues published in other languages. On the other hand, the scope of matters discussed limits the number of research papers dedicated to this problem to a low number.
Implications for Nursing Practice
Although there are no universal guidelines with respect to the applied pain assessment scales in neonatal patients, the research explicitly shows that the application of tools recommended by the International Scientific Societies significantly reduces the quantity of administered anaesthetic drugs. There is no doubt that the application of scales means not only the comfort of a patient, but also greater satisfaction from work among nursing personnel. The efficiency of each scale used in daily nursing practice has to be based on training and education. Therefore, every healthcare centre should implement a training system on a regular basis, similarly to the practices of cardiopulmonary resuscitation and blood donation.
Disclosure
None of the authors discloses potential conflict of interest in this work.
References
- 1.Simons SH, van Dijk M, Anand KS, Roofthooft D, van Lingen RA, Tibboel D. Do we still hurt newborn babies? A prospective study of procedural pain and analgesia in neonates. Arch Pediatr Adolesc Med. 2003;157(11):1058–1064. doi: 10.1001/archpedi.157.11.1058 [DOI] [PubMed] [Google Scholar]
- 2.Zielińska M. Czy noworodek odczuwa ból? Adv Clin Exp Med. 2006;15(2):339–344. [Google Scholar]
- 3.Ambalavanan N, Carlo WA. Analgesia for ventilated neonates: where do we stand? J Pediatr. 1999;135(4):403–405. doi: 10.1016/s0022-3476(99)70156-3 [DOI] [PubMed] [Google Scholar]
- 4.Kennedy KA, Tyson JE. Narcotic analgesia for ventilated newborns: are placebo-controlled trials ethical and necessary? J Pediatr. 1999;134(2):127–129. doi: 10.1016/s0022-3476(99)70399-9 [DOI] [PubMed] [Google Scholar]
- 5.Fitzgerald M. The development of nociceptive circuits. Nat Rev Neurosci. 2005;6:507–520. doi: 10.1038/nrn1701 [DOI] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics. AAP committee on fetus and newborn and section on anesthesiology and pain medicine. Prevention and management of procedural pain in the neonate: an update. Pediatrics. 2016;137(2):e20154271. doi: 10.1542/peds.2015-4271 [DOI] [PubMed] [Google Scholar]
- 7.Cruz MD, Fernandes AM, Oliveira CR. Epidemiology of painful procedures performed in neonates a systematic review of observational studies. Eur J Pain. 2016;20(4):489–498. doi: 10.1002/ejp.757 [DOI] [PubMed] [Google Scholar]
- 8.Carbajal R, Rousset A, Danan C, et al. Epidemiology and treatment of painful procedures in neonates in intensive care units. JAMA. 2008;300:60–70. doi: 10.1001/jama.300.1.60 [DOI] [PubMed] [Google Scholar]
- 9.Anand KJ, Aranda JV, Berde CB, et al. Summary proceedings from the neonatal pain-control group. Pediatrics. 2006;117(3 Pt 2):S9–S22. doi: 10.1542/peds.2005-0620C [DOI] [PubMed] [Google Scholar]
- 10.Schwaller F, Fitzgerald M. The consequences of pain in early life: injury-induced plasticity in developing pain pathways. Eur J Neurosci. 2014;39:344–352. doi: 10.1111/ejn.12414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vinall J, Grunau RE. Impact of repeated procedural pain-related stress in infants born very preterm. Pediatr Res. 2014;75:584–587. doi: 10.1038/pr.2014.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grunau RE. Neonatal pain in very preterm infants: long-term effects on brain, neurodevelopment and pain reactivity. Rambam Maimonides Med J. 2013;4(4):e0025. doi: 10.5041/RMMJ.10132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stevens BJ, Johnston CC. Physiological responses of premature infants to a painful stimulus. Nurs Res. 1994;43:226–231. doi: 10.1097/00006199-199407000-00007 [DOI] [PubMed] [Google Scholar]
- 14.Anand KJS, Hickey PR. Halothane - morphine compared with high dose- sufentanil for anesthesia and postoperative analgesia in neonatal cardiac surgery. N Engl J Med. 1992;326(1):1–9. doi: 10.1056/NEJM199201023260101 [DOI] [PubMed] [Google Scholar]
- 15.Panek M, Kwinta P. Ocena bólu oraz niefarmakologiczne metody jego łagodzenia u noworodków. Standardy Medyczne/Pediatria. 2014;11:249–256. [Google Scholar]
- 16.Stevens B, Yamada J, Lee GY, Ohlsson A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database Systematic Rev. 2013;1:CD001069. [DOI] [PubMed] [Google Scholar]
- 17.Stevens BJ, Pillai Riddell RR, Oberlander TE, et al. Assessment of pain in neonates and infants In W: Anand KJS, Stevens BJ, McGrath PJ, editors. Pain in Neonates and Infants. Elsevier; 2007. 67–90. [Google Scholar]
- 18.Anand KJS. Defining pain in newborns: need for a uniform taxonomy? Acta Paediatr. 2017;106:1438–1444. doi: 10.1111/apa.13936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Ganzewinkel CJ, Anand KJS, Kramer BW, Andriessen P. Chronic pain in the newborn: toward a definition. Clin J Pain. 2014;30:970–977. doi: 10.1097/AJP.0000000000000056 [DOI] [PubMed] [Google Scholar]
- 20.Pillai Riddell RR, Stevens BJ, McKeever P, et al. Chronic pain in hospitalized infants: health professionals’ perspectives. J Pain. 2009;10:1217–1225. doi: 10.1016/j.jpain.2009.04.013 [DOI] [PubMed] [Google Scholar]
- 21.Franck LS, Allen A, Cox S, Winter I. Parents’ views about infant pain in neonatal intensive care. Clin J Pain. 2005;21:133–139. doi: 10.1097/00002508-200503000-00004 [DOI] [PubMed] [Google Scholar]
- 22.Gulczyńska E, Piotrowski A. Profilaktyka I Leczenie Bólu u Noworodka. Standardy Opieki Medycznej Nad Noworodkiem w Polsce. 2019 Zalecenia Polskiego Towarzystwa Neonatologicznego. Wyd: Media-Press Sp. z o.o Warszawa; 2019:118–128. [Google Scholar]
- 23.Hall RW, Boyle E, Young T. Do ventilated neonates require pain management? Semin Perinatol. 2007;31(5):289–297. doi: 10.1053/j.semperi.2007.07.002 [DOI] [PubMed] [Google Scholar]
- 24.Grunau RE, Holsti L, Haley DW, et al. Neonatal procedural pain exposure predicts lower cortisol and behavioral reactivity in preterm infants in the NICU. Pain. 2005;113:293–300. doi: 10.1016/j.pain.2004.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams AL, Khattak AZ, Garza CN, Lasky RE. The behavioral pain response to heelstick in preterm neonates studied longitudinally: description, development, determinants, and components. Early Hum Dev. 2009;85(6):369–374. doi: 10.1016/j.earlhumdev.2009.01.001 [DOI] [PubMed] [Google Scholar]
- 26.Hatfield LA, Ely EA. Measurement of acute pain in infants: a review of behavioral and physiological variables. Biol Res Nurs. 2015;17:100–111. doi: 10.1177/1099800414531448 [DOI] [PubMed] [Google Scholar]
- 27.Stevens B, Gibbins S. Clinical utility and clinical significance in the assessment and management of pain in vulnerable infants. Clin Perinatol. 2002;29:459–468. doi: 10.1016/S0095-5108(02)00016-7 [DOI] [PubMed] [Google Scholar]
- 28.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0. The Cochrane Collaboration; 2008. [Google Scholar]
- 29.Wells. GA. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed July14, 2020.
- 30.American Academy of Pediatrics Committee on Fetus and Newborn, American Academy of Pediatrics Section on Surgery, Canadian Pediatric Society Fetus and Newborn Committe i wsp. Prevention and management of pain in the neonate: an update. Pediatrics. 2007;119(2):425. doi: 10.1542/peds.2006-2277 [DOI] [Google Scholar]
- 31.Desai A, Nanavati RN, Jasani BB, Kabra N. Comparison of neonatal pain, agitation, and sedation scale with premature infant pain profile for the assessment of acute prolonged pain in neonates on assisted ventilation: a prospective observational study. Indian J Palliat Care. 2017;23(3):287–292. doi: 10.4103/IJPC.IJPC_42_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Dijk M, Roofthooft DW, Anand KJ, et al. Taking up the challenge of measuring prolonged pain in (premature) neonates: the COMFORTneo scale seems promising. Clinical J Pain. 2009;25(7):607–616. doi: 10.1097/AJP.0b013e3181a5b52 [DOI] [PubMed] [Google Scholar]
- 33.Cignacco E, Hamers JP, van Lingen RA, et al. Pain relief in ventilated preterms during endotracheal suctioning: a randomized controlled trial. Wiss Med Wkly. 2008;138(4344):635–645. [DOI] [PubMed] [Google Scholar]
- 34.Hummel P, Puchalski M, Creech SD, Weiss MG. Clinical reliability and validity of the N-PASS: neonatal pain, agitation and sedation scale with prolonged pain. J Perinatol. 2008;28(1):55–60. doi: 10.1038/sj.jp.7211861 [DOI] [PubMed] [Google Scholar]
- 35.e Silva YP, Gomez RS, Marcatto J, de O, Maximo TA, Barbosa RF, e Silva CS. Early awakening and extubation with remifentanil in ventilated premature neonates. Pediatric Anesthesia. 2008;18(2):176–183. doi: 10.1111/j.1460-9592.2007.02378.x [DOI] [PubMed] [Google Scholar]
- 36.Acikgoz A, Yildiz S. Effects of open and closed suctioning systems on pain in newborns treated with mechanical ventilation. Pain Management Nursing. 2015;16(5):653–663. doi: 10.1016/j.pmn.2015.01.002 [DOI] [PubMed] [Google Scholar]
- 37.Cardoso JM, Kusahara DM, Guinsburg R, Pedreira MLG. Randomized crossover trial of endotracheal tube suctioning systems use in newborns. Nurs Crit Care. 2017;22(5):276–283. doi: 10.1111/nicc.12170 [DOI] [PubMed] [Google Scholar]
- 38.Abiramalatha T, Mathew SK, Mathew BS, et al. Continuous infusion versus intermittent bolus doses of fentanyl for analgesia and sedation in neonates: an open-label randomised controlled trial. Arch Dis Child. 2019;104(4):F433F439. doi: 10.1136/archdischild-2018-315345 [DOI] [PubMed] [Google Scholar]
- 39.Huang XZ, Li L, Zhou J, He F, Zhong CX, Wang B. Evaluation of three pain assessment scales used for ventilated neonates. J Clin Nursing. 2018;27(1920):3522–3529. doi: 10.1111/jocn.14585 [DOI] [PubMed] [Google Scholar]
- 40.Desai A, Aucott S, Frank K, Silbert-Flagg J. Comparing N-PASS and NIPS: improving pain measurement in the neonate. Adv Neonatal Care. 2018;18(4):260–266. doi: 10.1097/ANC.0000000000000521 [DOI] [PubMed] [Google Scholar]
- 41.Chrysostomou C, Schulman SR, Herrera Castellanos M, et al. A Phase II/III, multicenter, safety, efficacy, and pharmacokinetic study of dexmedetomidine in preterm and term neonates. J Pediatrics. 2014;164(2):276‐282. doi: 10.1016/j.jpeds.2013.10.002 [DOI] [PubMed] [Google Scholar]
- 42.Milesi C, Cambonie G, Jacquot A. Validation of a neonatal pain scale adapted to the new practices in caring for preterm newborns. Arch Dis Child Fetal Neonatal Ed. 2010;95(4):F263F266. doi: 10.1136/adc.2008.144758 [DOI] [PubMed] [Google Scholar]
- 43.Hünseler C, Merkt V, Gerloff M, Eifinger F, Kribs A, Roth B. Assessing pain in ventilated newborn and infants: validation of the Hartwig score. Eur J Pediatr. 2011;170(7):837–843. doi: 10.1007/s00431-010-1354-9 [DOI] [PubMed] [Google Scholar]
- 44.Carbajal R, Eriksson M, Courtois E, et al. EUROPAIN Survey Working Group. Sedation and analgesia practices in neonatal intensive care units: results from the prospective observational EUROPAIN study. Lancet Respir Med. 2015;3(10):796–8122015. doi: 10.1016/S2213-2600(15)00331-8 [DOI] [PubMed] [Google Scholar]
- 45.Anand KJS, Eriksson M, Boyle EM, et al. Assessment of continuous pain in newborns admitted to NICUs in 18 European countries. Acta Paediatr. 2017;106(8):1248–1259. doi: 10.1111/apa.13810 [DOI] [PubMed] [Google Scholar]
- 46.Rana D, Bellflower B, Sahni J, et al. Reduced narcotic and sedative utilization in a NICU after implementation of pain management guidelines. J Perinatol. 2017;37(9):1038–1042. doi: 10.1038/jp.2017.88 [DOI] [PubMed] [Google Scholar]
- 47.Avila-Alvarez A, Carbajal R, Courtois E, et al. Grupo español del proyecto Europain. Valoración clínica del dolor en unidades de cuidados intensivos neonatales españolas. Annales De Pediatria. 2016;85(4):167–220. doi: 10.1016/j.anpedi.2015.09.019 [DOI] [PubMed] [Google Scholar]
- 48.Elella RA, Adalaty H, Koay YN, et al. The efficacy of the COMFORT score and pain management protocol in ventilated pediatric patients following cardiac surgery. Int J Pediatr Adolesc Med. 2015;2(34):123‐127. doi: 10.1016/j.ijpam.2015.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Andersen RD, Munsters JMA, Vederhus BJ, Gradin M. Pain assessment practices in Swedish and Norwegian neonatal care units. Scand J Caring Sci. 2018;32(3):1074–1082. doi: 10.1111/scs.12553 [DOI] [PubMed] [Google Scholar]
- 50.Maaskant J, Raymakers-Janssen P, Veldhoen E, Ista E, Lucas C, Vermeulen H. The clinimetric properties of the Comfort scale: A systematic review. European j Pain. 2016;20(10):1587–1611. doi: 10.1002/ejp.880 [DOI] [PubMed] [Google Scholar]
- 51.Bellieni C. Reasons to avoid pain scales in newborns, and reasons to use them. J Clin Anesthesia and Pain Manage. 2017;1(1):17–19. doi: 10.36959/377/318 [DOI] [Google Scholar]
- 52.Bellieni CV, Cordelli DM, Caliani C, et al. Inter-observer reliability of two pain scales for newborns. Early Hum Dev. 2007;83:549–552. doi: 10.1016/j.earlhumdev.2006.10.006 [DOI] [PubMed] [Google Scholar]
- 53.Deindl P, Unterasinger L, Kappler G, et al. Successful implementation of a neonatal pain and sedation protocol at 2 NICUs. Pediatrics. 2013;132(1):e211e218. doi: 10.1542/peds.2012-234 [DOI] [PubMed] [Google Scholar]
- 54.Herrington CJ, Olomu IN, Geller SM. Salivary cortisol as indicators of pain in preterm infants: a pilot study. Clin Nurs Res. 2004;13(1):53–68. doi: 10.1177/1054773803259665 [DOI] [PubMed] [Google Scholar]
- 55.Guinsburg R, Kopelman BI, Anand KJ, de Almeida MF, Peres CA, Miyoshi MH. Physiological, hormonal, and behavioral responses to a single fentanyl dose in intubated and ventilated preterm neonates. J Pediatr. 1998;132(6):954–959. doi: 10.1016/S0022-3476(98)70390-7 [DOI] [PubMed] [Google Scholar]
- 56.Bellieni CV. Pain Assessment in human fetus and infants. AAPS J. 2012;14(3):456–461. doi: 10.1208/s12248-012-9354-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Benoit B, Martin-Misener R, New- Man A, Latimer M, Campbell-Yeo M. Neurophysiological assessment of acute pain in infants: a scoping review of research methods. Acta Paediatr. 2017;106:1053–1066. doi: 10.1111/apa.13839 [DOI] [PubMed] [Google Scholar]
- 58.de Melo GM, Lélis AL, de Moura AF, Cardoso MV, da Silva VM. Pain assessment scales in newborns: integrative review. Revista Paulista Pediatria. 2014;32(4):395–402. doi: 10.1016/j.rpped.2014.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Wells. GA. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed July14, 2020.