Introduction
Good sleep in sportspersons is an important factor that contributes to performance in events and to the prevention of and early recovery from injury.1 The International Olympic Committee consensus lays emphasis on adequate sleep for athletic development in the young.2 Sleep restriction is commonly found in adolescents. In a study conducted by Dinges et al., sleep restriction was associated with increase in lapses in the psychomotor vigilance task.3 Sleep restriction was found to affect the serving accuracy in tennis players.4 Chronic effects of sleep loss are found to be associated with increased sports injuries. Sleep in terms of both good quality and quantity aids in better athletic performance not only directly by enhancing vigilance and cognitive task but also indirectly by increased training participation due to better physical and mental recovery.5 There is limited available literature on efforts to improve sleep in elite sportspeople with sleep problems and studying its impact on performance. This case highlights the effect of non-pharmacological sleep intervention on sports performance in an elite archer with sleep maintenance insomnia.
Case report
A 14-year-old patient, an elite male archer with experience practicing archery professionally since 2012 presented after a sleep awareness campaign conducted by the principal author in an elite sports institute. He complained of “Neend se Khush Nahin” (not happy with sleep, unrestful sleep) since 2 years. The patient had history of increased sleep breaks at night and not being able to sleep after getting up at night, almost four to five times in a week. The total amount of time he lay awake in bed ranged from half an hour to sometimes an hour. He had history of excessive daytime sleepiness and was not able to focus and concentrate during the day. He slept almost 2 h during the afternoon and often felt irresistible sleep during classes from 11 am to 1 pm. The patient's archery performance was an average of 575.86 (standard deviation [SD] = 3.57) out of 720 at that time. This average is calculated from a set of score of 72 arrows which the archer shoots in two slots of 36 each. A maximum score of 720 can be attained.
A 2-week baseline sleep diary was filled by the patient. He underwent a baseline actigraphy with electroencephalogram (EEG) module (Somnomedics, Germany) which recorded EEG, Electromyogram (EMG), and Electrooculogram (EOG) for sleep–wake analysis.
The patient's baseline sleep diary showed increased wake duration after lying on the bed to sleep. Wake after sleep onset (WASO) was more than sleep onset latency (SOL). SOL was found to be within normal limits. A diagnosis of chronic insomnia with a predominant difficulty in sleep maintenance was made as per the International Classification of Sleep Disorders (ICSD)-3 classification.
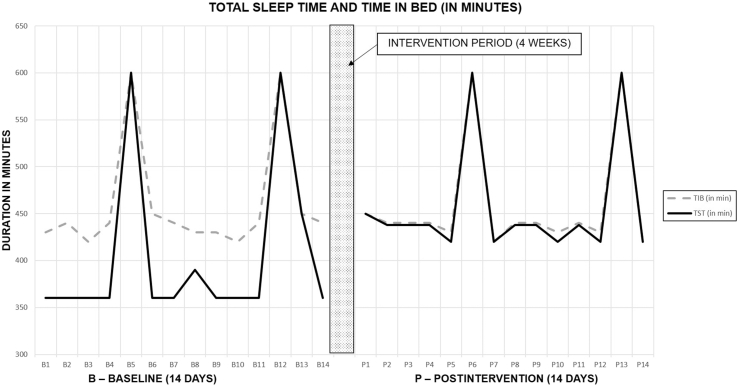
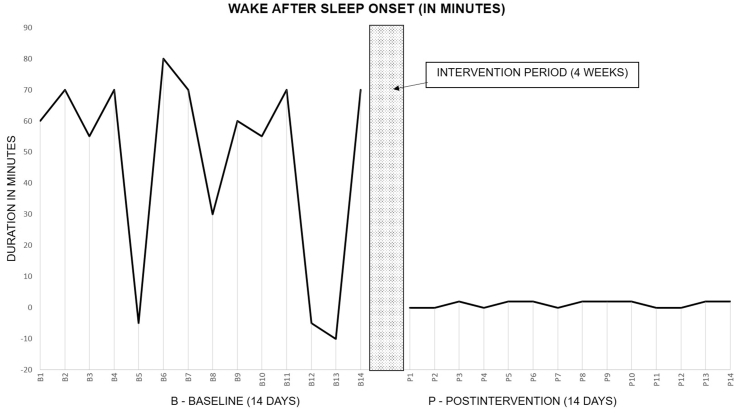
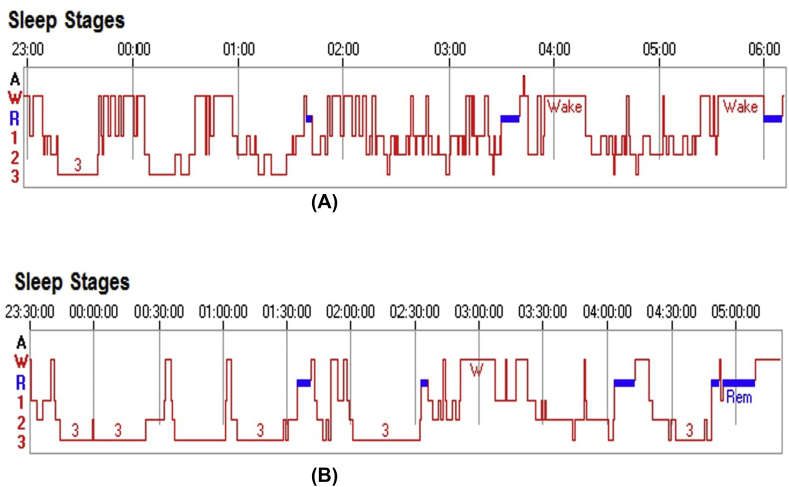
The patient was started on a 4-week non-pharmacological regimen comprising application of sleep hygiene principles, sleep education, stimulus control, and the practice of a therapeutic model of yoga nidra. Yoga nidra therapeutic model for insomnia consists of initial supervised sessions of yoga nidra practice followed by self-administered sessions. The details of yoga nidra model and analysis of sleep diary in this model have been described earlier in detail. The individual was kept under constant supervision of the sleep specialist with continuous monitoring of sleep diary as is mentioned in the model to keep an eye on untoward side effects.6 No side effects were seen. Fig. 1 shows the sleep diary parameters of total sleep time and time in bed. Fig. 2 depicts WASO during baseline and after 4 weeks of intervention. 14 days' baseline and postintervention sleep diary parameters were analyzed using paired t test. There was a significant improvement in the sleep diary sleep efficiency (total sleep time/time in bed as percentage) (p < 0.0001), WASO (p < 0.0001), and total wake duration (p < 0.0001). Averaged sleep diary parameters at baseline and after intervention are tabulated in Table 1. Actigraphy with EEG module was repeated after the intervention. Both actigraphy with EEG records, i.e. baseline and after intervention, were given to the principle author for analysis in a lot of ten along with records of other patients from the outpatient department (OPD). All the files in the lot were coded to ensure anonymity of the records, such that there was no bias at the time of analysis. The sleep–wake analysis was carried out using American Academy of Sleep Medicine (AASM) analysis.7 Baseline and postintervention actigraphy sleep–wake hypnograms are shown in Fig. 3. Slow wave sleep in actigraphy showed an increase from 65 min to 135 min, and slow wave sleep/time in bed as a percentage (N3/TIB %) was 14.98% at baseline and 38.4% after intervention. In our study, there were no objective parameters used to assess daytime sleepiness. In sleep OPD, the patient was followed up fortnightly for up to 6 months where he reported that he felt much more alert than before. Postintervention afternoon sleep reduced and was only 2–3 times/week (never >20 min). He showed improvement in sleep and was sustained, although sleep diary was not recorded.
Fig. 1.
Baseline and postintervention sleep diary total sleep time (TST) and time in bed (TIB) in minutes (averaged 14 days).
Fig. 2.
Baseline and postintervention sleep diary wake after sleep onset (WASO) in minutes (averaged 14 days).
Table 1.
Sleep diary parameters of a chronic insomnia patient before (baseline) and after 4 weeks of non-pharmacological intervention for insomnia (after intervention).
| Sr No | Parameters | Baseline (mean ± SD) | After intervention (mean ± SD) | Result of statistical analysis (paired t test) |
|---|---|---|---|---|
| 1 | Time in bed (TIB) in min | 460.77 ± 60.32 | 458.57 ± 60.49 | Not significant |
| 2 | Total sleep time (TST) in min | 406.15 ± 87.04 | 455.57 ± 61.97 | Not significant |
| 3 | Total wake duration in min | 54.62 ± 32.96 | 1 ± 1.04 | p < 0.0001 |
| 4 | Sleep efficiency (in percentage) | 87.45 ± 7.49 | 99.31 ± 0.91 | p < 0.0001 |
| 5 | Sleep onset latency (SOL) in minutes | 8.46 ± 2.34 | 7.14 ± 2.56 | Not significant |
SD, standard deviation.
Fig. 3.
(A) Baseline hypnogram. (B) Postintervention actigraphy sleep wake hypnogram. A, artefact; W, wake; R, rapid eye movement sleep; Stage 1 sleep (N1 American Academy of Sleep Medicine); Stage 2 sleep (N2 American Academy of Sleep Medicine); Stage 3 and 4 sleep-slow wave sleep (N3 American Academy of Sleep Medicine).
After 4 weeks of intervention, the patient's performance improved from an average score of 575.86 (SD = 3.57) at baseline to a score of 683.71 (SD = 2.70) out of a maximum score of 720 (p < 0.001) after six rounds of six arrows shot in two sessions (6 × 6 × 2 = 72 arrows × 10 maximum score that can be scored by each arrow = 720 maximum score).
Discussion
Sleep is an important factor in sports. Insomnia patients are known to show performance deficits especially involving attention tasks that have high cognitive loads.8 In the present sportsperson with insomnia, improvement of sleep led to enhanced performance. In the subjective sleep diary, a significant improvement in total wake duration and sleep efficiency was seen, and objectively slow wave sleep showed an improvement. Slow wave sleep is the most reliable criterion from a single night sleep–wake analysis9 because of night-to-night variability in insomniacs.
Propagation of sleep hygiene principles and early intervention of sleep using non-pharmacological approach10 are recommended for sportspersons. The exact role of individualized therapy in elite sportspersons needs to be studied with larger sample size. This will benefit sportspersons with sleep problems not only during training but also before and during competitions. This may be helpful in maintaining their optimum performance at that time. The study also highlights the importance of identifying individually susceptible population who might need special attention of sleep in the precompetition phase or international travel when sleep is often disturbed. Targeted educational interventions to improve sleep patterns may be vital to achieve the best of performance in our trained elite sportsperson.
Conflicts of interest
The authors have none to declare.
References
- 1.Kellmann M., Bertollo M., Bosquet L. Recovery and performance in sport: consensus statement. Int J Sports Physiol Perform. 2018 Jan 18:1–19. doi: 10.1123/ijspp.2017-0759. [DOI] [PubMed] [Google Scholar]
- 2.Bergeron M.F., Mountjoy M., Armstrong N. International Olympic Committee consensus statement on youth athletic development. Br J Sports Med. 2015 Jul 1;49(13):843–851. doi: 10.1136/bjsports-2015-094962. [DOI] [PubMed] [Google Scholar]
- 3.Dinges D.F., Pack F., Williams K. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4-5 hours per night. Sleep. 1997 Apr;20(4):267–277. [PubMed] [Google Scholar]
- 4.Reyner L.A., Horne J.A. Sleep restriction and serving accuracy in performance tennis players, and effects of caffeine. Physiol Behav. 2013 Aug 15;120:93–96. doi: 10.1016/j.physbeh.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Watson A.M. Sleep and athletic performance. Curr Sports Med Rep. 2017 Nov 1;16(6):413–418. doi: 10.1249/JSR.0000000000000418. [DOI] [PubMed] [Google Scholar]
- 6.Datta K., Tripathi M., Mallick H.N. Yoga Nidra: an innovative approach for management of chronic insomnia- A case report. Sleep Sci Pract [Internet] 2017 Dec;1(1) http://sleep.biomedcentral.com/articles/10.1186/s41606-017-0009-4 [cited 2018 Feb 9] Available from: [Google Scholar]
- 7.Berry R.B., Brooks R., Gamaldo C. AASM scoring manual updates for 2017 (Version 2.4) J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2017 May 15;13(5):665–666. doi: 10.5664/jcsm.6576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shekleton J.A., Rogers N.L., Rajaratnam S.M.W. Searching for the daytime impairments of primary insomnia. Sleep Med Rev. 2010 Feb;14(1):47–60. doi: 10.1016/j.smrv.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 9.Levendowski D.J., Ferini-Strambi L., Gamaldo C., Cetel M., Rosenberg R., Westbrook P.R. The accuracy, night-to-night variability, and stability of frontopolar sleep electroencephalography biomarkers. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2017 Jun 15;13(6):791–803. doi: 10.5664/jcsm.6618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leger D., Metlaine A., Choudat D. Insomnia and sleep disruption: relevance for athletic performance. Clin Sports Med. 2005 Apr;24(2):269–285. doi: 10.1016/j.csm.2004.12.011. [viii] [DOI] [PubMed] [Google Scholar]