Abstract
As a part of an abnormal healing process of dermal injuries and irritation, keloid scars arise on the skin as benign fibroproliferative tumors. Although the etiology of keloid scarring remains unsettled, considerable recent evidence suggested that keloidogenesis may be driven by epigenetic changes, particularly, DNA methylation. Therefore, genome-wide scanning of methylated cytosine-phosphoguanine (CpG) sites in extracted DNA from 12 keloid scar fibroblasts (KF) and 12 control skin fibroblasts (CF) (six normal skin fibroblasts and six normotrophic fibroblasts) was conducted using the Illumina Human Methylation 450K BeadChip in two replicates for each sample. Comparing KF and CF used a Linear Models for Microarray Data (Limma) model revealed 100,000 differentially methylated (DM) CpG sites, 20,695 of which were found to be hypomethylated and 79,305 were hypermethylated. The top DM CpG sites were associated with TNKS2, FAM45B, LOC723972, GAS7, RHBDD2 and CAMKK1. Subsequently, the most functionally enriched genes with the top 100 DM CpG sites were significantly (p ≤ 0.05) associated with SH2 domain binding, regulation of transcription, DNA-templated, nucleus, positive regulation of protein targeting to mitochondrion, nucleoplasm, Swr1 complex, histone exchange, and cellular response to organic substance. In addition, NLK, CAMKK1, LPAR2, CASP1, and NHS showed to be the most common regulators in the signaling network analysis. Taken together, these findings shed light on the methylation status of keloids that could be implicated in the underlying mechanism of keloid scars formation and remission.
Keywords: keloid scars, DNA methylation, wound healing, epigenetics
1. Introduction
Wound healing in the human body is one of the most complex and progressive processes that require the involvement of several different molecular and cellular events [1,2]. The normal healing process involves multi-dynamic stages in three overlapping phases: the inflammation reaction, cellular elements proliferation and synthesis, and remodeling [2,3]. The latter phase outcomes are clinically predominant where collagen deposition occurs [4]. When the healing process is adequate, inconspicuous harmless scars, the normotrophic, are formed [5].
In response to aberrant healing of skin injuries and irritation, undesirable scars are raised [6,7]. Scars can fall into both hypertrophic and keloids that are not necessarily the same, but can be difficult to differentiate [4,8]. Keloids are often distinguished by their growing to the surrounding healthy skin beyond the margins of the original tissue lesion [8,9]. Keloid scars are benign dermal fibrotic tumors clinically characterized by the excessive production and deposition of the extracellular matrix (ECM) components [4,10,11]. Although the pathogenesis of keloids is poorly elucidated, some genetic and environmental factors, as well as epigenetic mechanisms, have been involved, resulting in dysregulation of the tissue repair and regeneration processes [3,12,13].
Interests have recently progressed toward the field of cutaneous epigenetics as a vital mechanism in regulating gene expression. DNA methylation is one of the most potent epigenetic changes that is common in cytosine-phosphoguanine (CpG) dinucleotides in which cytosine residue is bind to a methyl group (CH3) at position C5 [12,14]. Methylation of the DNA is essential during early normal development and contributes to the natural phenotypic variation in humans [15,16]. The aberrant addition (hypermethylation), or removal (hypomethylation) of the methyl group can either decrease or increase the rate of gene expression [17,18]. Epigenetic modification, including DNA methylation, has been observed in several human disease, including keloid scars [18,19,20,21,22]. These findings strongly suggested that DNA methylation is crucial in maintaining genome stability and plays an important role in disease pathogenesis. Most DNA methylation is known to occur at CpG sites [23].
These studies mainly focused on CpG islands methylation, which are regions with high cluster of CpG sites. Therefore, this study was undertaken to investigate the methylation levels of CpG sites in all genomic regions in keloid fibroblasts compared to the normal skin and normotrophic scar fibroblasts to further understand the role of DNA methylation as an epigenetic modification in keloid pathogenesis.
2. Experimental Section
2.1. Subjects
Keloid tissue samples were obtained from 12 patients (8 males and 4 females with an average age of 34 years) (Table 1) who were enrolled in a clinical trial which included excision of a keloid scar. These subjects had received no previous treatment of the keloid scar within 6 months of surgical excision. A full medical history was taken prior to excision and clinical examination was performed by a surgeon to confirm the diagnosis of keloid scar. The causes of keloid scar include immunization site, surgery, non-burn trauma, acne, and burn injury. Control samples (n = 12) were normotrophic burn scar tissue (Vancouver Scar Scale: height sub-score = 0) and matched normal skin collected from 6 male subjects with an average age of 24.5 years who had sustained a previous unilateral burn injury (Table 1). The clinical criteria used to differentiate a keloid scar from a normotrophic scar include a history of continuous growth outside the boundaries of the original wound and symptoms such as pain and itch.
Table 1.
Patient and keloid scar details.
| Subject ID 1 | Age | Gender 2 | Type of Tissue | Site of Tissue | Ethnicity |
|---|---|---|---|---|---|
| P 1 | 40 | F | keloid scar | shoulder | East Asian |
| P 2 | 38 | F | keloid scar | neck (thyroid) | Southeast European |
| P 3 | 29 | M | keloid scar | forearm | Hispanic |
| P 4 | 30 | M | keloid scar | sternum | Northwest European |
| P 5 | 53 | M | keloid scar | sternum | Northwest European |
| P 6 | 28 | M | keloid scar | upper arm | Northwest European |
| P 7 | 18 | F | keloid scar | shoulder | East Asian |
| P 8 | 42 | M | keloid scar | ear | Northwest European |
| P 9 | 30 | M | keloid scar | sternum | East Asian |
| P 10 | 21 | M | keloid scar | sternum | Northwest European and East Asian |
| P 11 | 47 | F | keloid scar | sternum | Northwest European |
| P 12 | 29 | M | keloid scar | sternum | East Asian |
| C 1 | 29 | M | normotrophic scar | forearm | South East Asian |
| normal skin | contralateral forearm | ||||
| C 2 | 25 | M | normotrophic scar | forearm | Caucasian |
| normal skin | contralateral forearm | ||||
| C 3 | 19 | M | normotrophic scar | forearm | Caucasian |
| normal skin | contralateral forearm | ||||
| C 4 | 25 | M | normotrophic scar | forearm | Caucasian |
| normal skin | contralateral forearm | ||||
| C 5 | 30 | M | normotrophic scar | forearm | Caucasian |
| normal skin | contralateral forearm | ||||
| C 6 | 19 | M | normotrophic scar | forearm | Caucasian |
| normal skin | contralateral forearm |
1 P: Patient; C: Control. 2 M: Male; F: Female.
The study was performed in accordance with the relevant National Health and Medical Research Council (NHMRC) of Australia’s ethical statements and guidelines. Ethical approval for all tissue collection was obtained from the Human Research Ethics Committees of the University of Western Australia (RA/4/1/5604; Date: 03/09/2012) and Royal Perth Hospital (EC2009/114 and EC 2012/067; Date: 03/09/2012). All participants provided written informed consent.
2.2. Isolation and Culture of Fibroblasts from Keloid Scar and Control Samples
Fibroblasts were isolated from fresh tissue by the explant method. This method was slightly modified from previously published methods [24,25]. Cell growth was maintained until the second passage (P2) and then cells were frozen in liquid nitrogen and stored until further experiments.
2.3. DNA Extraction and Bisulfate Conversion
DNA was extracted from the fibroblasts (P2) using a QIAamp DNA Mini kit (Cat. No. 51304, Qiagen, Hulsterweg, The Netherlands) and Promega Wizard SV Genomic DNA system (Cat. No. A2360, Promega, Madison, WI, USA) as per the manufacturers’ instructions. The quality and quantity of extracted DNA were measured using a NanoDrop-2000 spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA). Bisulfite conversion of 800 ng of DNA was carried out on 24 samples using the EZ DNA Methylation kit (Cat. No. D5001, Zymo Research, Irvine, CA, USA) according to the manufacturer’s instructions.
2.4. DNA Methylation Assay
A minimum of 500 ng genomic DNA was amplified, fragmented, and hybridized onto the Illumina Human Methylation 450K BeadChip (Cat. No. WG-314-1003, Illumina, San Diego, CA, USA) according to the manufacturer’s protocol (Illumina 2013). This BeadChip processes 12 samples per array. Two replicates of the methylation assay were performed per sample. The first BeadChip included bisulfite-converted DNA from 6 normal skin fibroblasts and 6 normotrophic fibroblasts. The second BeadChip included bisulfite-converted DNA from 12 keloid scar fibroblasts.
2.5. Data Processing for the 450k Methylation Array
A computational R package (RnBeads) was adapted to process and analyze the raw intensity data from methylation chip (IDAT files) [26]. The dataset was subjected to filtering procedures, background subtraction, and normalization. The filtering stages included the removal of sites overlapped with SNPs, greedycut algorithm, the removal of probes with specific contexts and missing values, and the removal of probes with beta values exhibiting standard deviation lower than 0.005. The methylumi package (method “noob”) was used for background subtraction and the Beta-Mixture Quantile Normalization (BMIQ) method was used to normalize the methylation beta values. As keloid fibroblasts and control fibroblasts were run on separate BeadChips, a batch effect may occur. RnBeads uses the Surrogate Variable Analysis (SVA) package to visualize and adjust for batch effects during differential methylation analysis. As a final outcome, a summary of the changes at CpG sites was generated.
2.6. Differential Methylation Statistical Analysis
Differential methylation (DM) analysis comparing keloid fibroblast (KF) DNA with control fibroblasts (CF) DNA was carried out at the CpG site. The comparison was computed using a Linear Models for Microarray Data (Limma) method [27], which has been adapted by the RnBeads package for use in methylation arrays. The linear models were employed and fitted using an empirical Bayes approach on derived M-values. The Benjamini and Hochberg (B-H) 5% false discovery rate (FDR) was used to correct for multiple testing. The DM for each CpG sites was computed based on three measures: the beta difference in methylation means between KF and CF, the log2 of the quotient in methylation, and the differential methylation p-value using Limma. Using these three measures, each CpG site was given a rank. The combined rank was computed as the maximum (=worst) rank among the three ranks. A smaller combined rank indicates that the CpG sites exhibit more DM [26]. The top-ranking 100,000 sites with the smallest combined rank score were selected for further analysis.
2.7. Enrichment and Pathway Analysis
The Database for Annotation, Visualization, and Integrated Discovery (DAVID) v.6.8 [28,29], was utilized to conduct GO term enrichment analysis of the genes corresponding to the top 100 CpG sites. The GO terms included three criteria: biological process (BP), cellular component (CC), and molecular function (MF). A p-value ≤ 0.05 was used as a cut-off threshold.
2.8. Interaction Network Analysis
The interaction network analysis of genes associated with the top 100 DM CpG sites was explored using the Signaling Network Open Resource 2.0 (SIGNOR) [30]. The type of relation was selected to include only “all” interactions with a relaxed layout and score of “0.0”.
3. Results
3.1. Samples Clustering
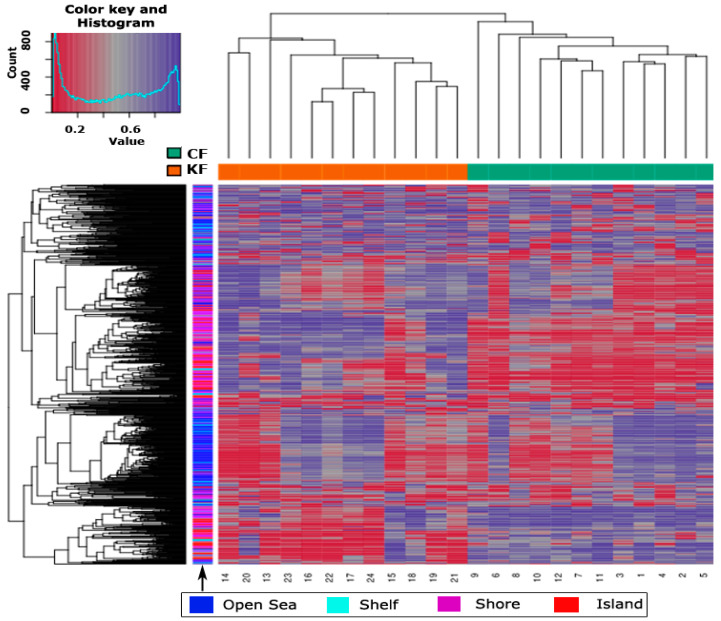
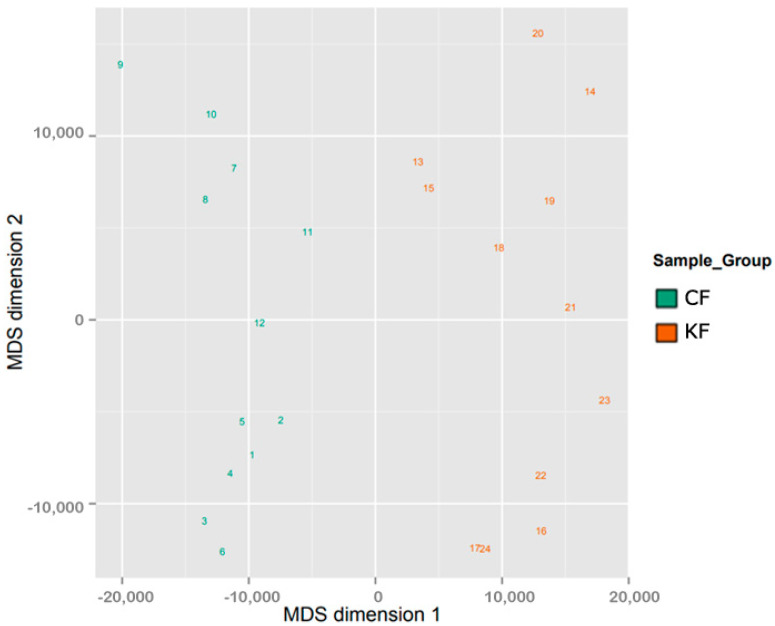
The samples sharing similar methylation patterns showed an expected hierarchal clustering based on all the methylation values of the top 1000 most variable loci (Figure 1). In a study conducted by our research group, we have found no statistical significance in methylation level between normotrophic burn scar fibroblasts and matched normal skin fibroblasts (data not published). Hence, fibroblasts from both tissue types (normotrophic burn scar and normal skin) were used in this study as CF to increase statistical power. Figure 1 shows one hierarchal clustering of CF isolated from normotrophic burn scar and normal skin explaining the similarity in methylation patterns and another clustering of KF isolated from keloid scar. The dataset was inspected for a strong signal in the methylation values using a dimension reduction test by implementing multidimensional scaling (MDS) method (Figure 2). MDS confirmed that the difference in methylation level between KF and CF dominates the analysis.
Figure 1.
Hierarchal clustering of the top 1000 most variable loci across the 24 samples. Clustering used average linkage and Manhattan distance. The top x-axis shows the study groups, where KF and CF stand for keloid fibroblasts and control fibroblasts, respectively. The bottom x-axis shows the samples identification numbers, 13–24 represent KF and 1–12 represent CF. The color key and histogram of the heatmap defines the pattern of methylation, values of 0 (red color) and 1 (purple color) indicate decreased and increased methylation, respectively. The distribution of the 1000 most variable loci across the different cytosine-phosphoguanine (CpG) regions (open sea, shelf, shore and island) is shown with color coding on the bottom x-axis.
Figure 2.
Two Multidimensional scaling (MDS) of the sample groups. The scatter plots show the coordinates of the control fibroblasts (CF) and keloid fibroblasts (KF) samples after performing Kruskal’s multi-dimensional scaling based on the matrix of the average methylation levels and Manhattan distance. The plot of 24 samples (1–12 CF and 13–24 KF) shows that samples cluster according to methylation level, as expected.
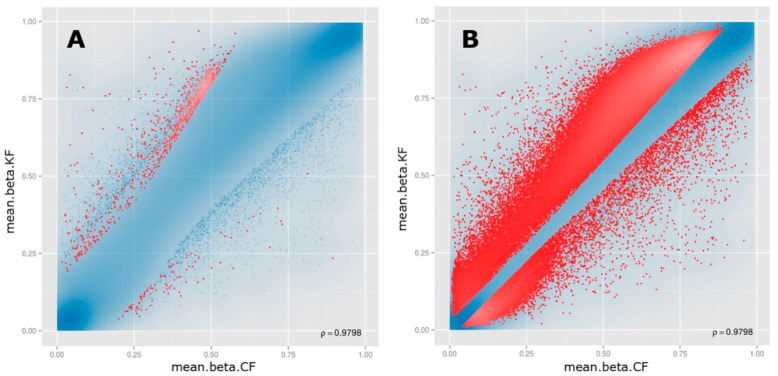
3.2. Differential Methylation of CpG Sites
The top 100,000 sites ranked according to the combined rank score were selected to identify DM CpG sites in KF. Of the 100,000 CpG sites, 20,695 CpG sites were found to be hypomethylated (beta difference range = −0.030 to −0.67) and 79,305 CpG sites were hypermethylated (beta difference range = 0.030 to 0.79) in KF compared to CF with an adjusted p-value (FDR) ≤0.11 (Figure 3). The log2 of the quotient in methylation between KF and CF had a minimum value of −3.34 and a maximum value of 4.42. The top 100 DM CpG sites with the lowest combined rank score are shown in Table S1. The beta difference of the list of 100 DM sites ranged from −0.22 to −0.42 for hypomethylated genes and ranged from 0.23 to 0.60 for hypermethylated genes with an adjusted p-value (FDR) ≤1.72 × 10−6.
Figure 3.
Scatter plots for the (A) top-ranking 1000 and (B) top-ranking 100,000 differentially methylated CpG sites. For each plot, the mean β values of control fibroblasts (mean.beta.CF) are on the x-axis, while the mean β values of keloid fibroblasts (mean.beta.KF) are on the y-axis. Methylation levels (β) varied between 0 (unmethylated) and 1 (fully methylated). Blue points represent variable differentially methylated sites.
3.3. Functional Enrichment Analysis
The genes associated with the top 100 DM CpG sites were subject to functional enrichment analyses using the DAVID webtool. The most significant gene ontology (GO) terms (p-value ≤ 0.05) are shown in Table 2. On the MF level, the associated genes were mainly enriched for “SH2 domain binding”, on the CC level, genes were enriched for “nucleus”, “nucleoplasm”, and “Swr1 complex”. On the BP level, the associated genes were enriched for four terms including “regulation of transcription, DNA-templated”, “positive regulation of protein targeting to mitochondrion”, “histone exchange”, and “cellular response to organic substance”.
Table 2.
Gene ontology enrichment analyses of the genes associated with the top 100 CpG sites.
| Category 1 | Term | p-Value 2 | Genes |
|---|---|---|---|
| MF | GO:0042169~SH2 domain binding | 0.002 | SYP, NLK, DAG1 |
| BP | GO:0006355~regulation of transcription, DNA-templated | 0.005 | ASXL2, PKNOX2, ZNF718, BPTF, TFEC, NLK, SCML1, GAS7, BRD8, KLF3 |
| CC | GO:0005634~nucleus | 0.011 | ANP32C, NLK, ANP32E, SCML1, TKT, CAMKK1, TNKS2, PKNOX2, PSMA1, SERPINB9, ZNF718, FAM64A, SENP1, TAF15, BPTF, C19ORF66, USP36, FANCC, BRD8, MYH10, KLF3 |
| BP | GO:1903955~positive regulation of protein targeting to mitochondrion | 0.016 | HSPA1L, NBPF3, USP36 |
| CC | GO:0005654~nucleoplasm | 0.020 | ASXL2, NLK, FANK1, DAG1, TKT, HSPA1L, PSMA1, SENP1, BPTF, TAF15, TFEC, BRD8, FANCC |
| CC | GO:0000812~Swr1 complex | 0.021 | ANP32E, BRD8 |
| BP | GO:0043486~histone exchange | 0.025 | ANP32C, ANP32E |
| BP | GO:0071310~cellular response to organic substance | 0.038 | SYP, CASP1 |
1 BP: biological process; CC: cellular component; MF: molecular function; 2 Terms with a p-value ≤ 0.05 are shown.
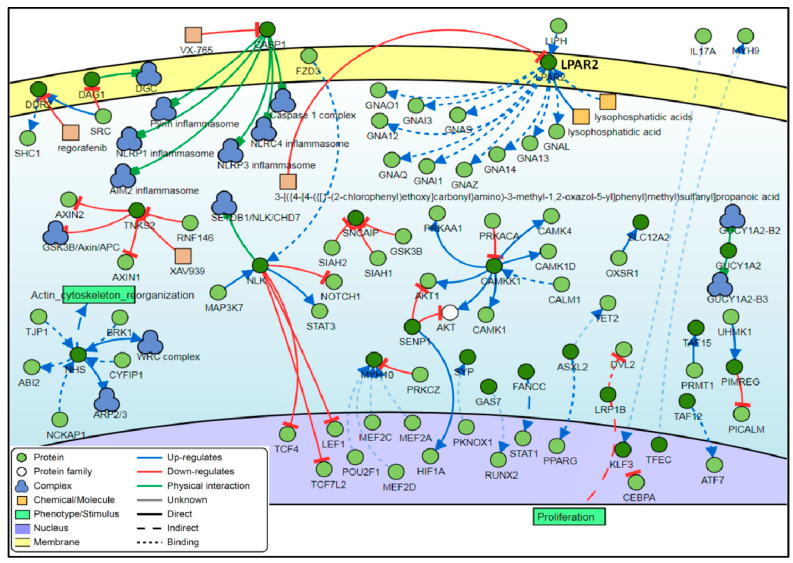
3.4. Interaction Network
Analysis of the interaction between the genes associated with the top 100 DM CpG sites showed that five genes were found to be common regulators with a minimum of 7 connectivities each. These genes are the NLK, CAMKK1, LPAR2, CASP1 and NHS genes (Figure 4).
Figure 4.
Interaction network of the genes associated with the top-ranking 100 CpG sites. Among these genes, five genes (NLK, CAMKK1, LPAR2, CASP1 and NHS) have the most relationships and interactions with proteins and molecules. The type of interactions, proteins and molecules are shown in the color, coded legend at the right corner of the figure.
4. Discussion
Keloid scarring is an aggressive skin disease with unclear pathogenesis. It is characterized by excessive fibroblast proliferation and collagen accumulation in the ECM that does not regress over time [31]. Keloid scars are an ongoing clinical challenge with no single effective treatment regimen. Nevertheless, clinicians use several modalities for scar prevention and management, including massage therapy, pressure garments, adhesive tape support/silicone gel sheeting, intralesional corticosteroid injections, laser and light-based therapy, cryotherapy, radiotherapy, 5-fluorouracil, interferon injections, bleomycin injections, and surgery [32]. Among these wide treatment strategies, intralesional steroid injections remain the first-line treatment for many clinicians alone or in combination with other treatment modalities [33]. A widely used intralesional corticosteroid is triamcinolone acetonide [33]. Treatment with triamcinolone alone proved to be more effective than verapamil for the prevention of keloid scar recurrence after surgical excision [34]. Compared to 5-fluorouracil and bleomycin, triamcinolone is more effective in preventing recurrence and reducing scar size and symptoms [33]. However, a combined treatment of triamcinolone with other treatment modalities such as verapamil, 5-fluorouracil, and laser therapy showed better outcomes and patient satisfaction [33]. Depending on the size and location of scars, the recommended concentration of triamcinolone ranges from 10 to 40 mg/mL [35].
Unlike genetic alterations, epigenetic changes are potentially reversable [36]. Therefore, the identification of epigenetic targets could lead to therapeutic interventions. DNA methylation is an epigenetic gene regulatory mechanism that has been found to play a fundamental role in cancer [37], fibrotic disorders [15,38,39], cutaneous diseases [18,22,40,41,42], and wound healing [20,43]. DNA methylation is known to occur commonly at CpG islands and was traditionally linked to transcriptional silencing. These CpG islands are found in high densities in the promoter regions of genes, where transcription of DNA begins, and thus regulate gene transcription [44,45]. This study has explored whether altered collagen deposition by keloid fibroblasts could at least in part be explained by epigenetic changes sustainably and heritably altering the gene expression profile in these cells. Our findings showed significant DNA methylation changes at the CpG sites across multiple genes in KF DNA compared to CF DNA.
The overgrowth and hyperproliferative nature of keloids are common features with tumorigenesis, in addition to epigenetic and genetic aberration. Of the differentially methylated 100,000 CpG sites in our analysis, more than two-thirds were hypermethylated. Consistent with several cancers-linked DNA hypermethylation, such as in prostate cancer (PCa) [46], and breast cancer [47]. In contrast, more hypomethylation profiles found in keloids genome, frequently in the non-promoter regions [17].
Among the 100 top-ranking DM CpG sites in KF compared to CF, the top seven genes were tankyrase 2 (TNKS2), hepatopoietin PCn127 (LOC723972), family with sequence similarity 45 member B (FAM45B), growth arrest specific 7 (GAS7), neuroblastoma breakpoint member 3 (NBPF3), rhomboid domain containing 2 (RHBDD2), and family with sequence similarity 64 member A (FAM64A). TNKS2 (cg11963436) and LOC723972 (cg21581312) were reported to be among the 50 DM CpG sites associated with lung function in cystic fibrosis patients [48]. From a methylation-based Epigenome-Wide Association Study (EWAS) in Parkinson’s disease (PD) identifying 9983 DM genes, FAM45B, LOC723972, and TNKS2 were among 20 unique DM genes in the patients. In further evaluation, TNKS2 (cg11963436) was one of two significantly confirmed DM genes that hypermethylated in PD patients [49]. Using the Illumina Human Methylation 450K BeadChip, LOC723972 (cg21581312) CpG site was hypomethylated in cervical squamous cell carcinoma (SCC) as well as in cervical intraepithelial neoplasia grade 3 (CIN3) compared with the normal tissues [50]. Methylation profiles in colorectal cancer (CRC) showed 50 significantly hypermethylated CpG sites located within six genes in African American patients, including GAS7 gene [51]. Moreover, among 355 methylated CpG sites in CRC, GAS7 was one of 59 significantly methylated sites in CRC tissues compared to normal tissues [52]. Furthermore, several epigenomic analyses revealed the hypermethylation pattern of GAS7 in lung cancer [53,54], prostate cancer [55], CRC [56], and pancreatic endocrine tumors (PETs) [57]. In order to investigate the strong association of the obesity-associated (FTO) gene variants and obesity with epigenetic changes, a genome-wide methylation scan in obese and normal weight females identified 20 DM sites in obese females, of which one was hypomethylated site in NBPF3 gene [58]. There are little or no reports on the methylation status of RHBDD2, but it was found to be overexpressed in CRC [59], breast cancer [60,61], and as a pathogenic gene in familial non-medullary thyroid cancer (FNMTC) [62]. The FAM64A gene correlated in differentially methylated regions (DMRs) containing multiple CpG sites associated with nevus count (n-DMRs), which is a strong risk factor, contributed to melanoma pathogenesis [63].
An interaction network analysis of the top 100 DM CpG sites showed five common regulator genes: nemo-like kinase (NLK), calcium/calmodulin-dependent protein kinase 1 (CAMKK1), lysophosphatidic acid receptor 2 (LPAR2), caspase 1 (CASP1), and Nance-Horan syndrome (NHS). The mitogen-activated protein kinase (MAPK) member, NLK is involved in a variety of signaling pathways as well as in several types of cancer. NLK was found to positively regulate the activation of CCAAT/enhancer binding proteins (C/EBPs) signaling cascade triggered by the proinflammatory cytokine, interleukin-1 (IL-1) [64]. In contrast, it was found to negatively regulate the ternary transcriptional complex in the Notch signaling pathway that is crucial in cell fates of metazoan tissues [65]. Aberrant expression of NLK has been associated with the initiation or progression of oral squamous cell carcinoma [66], laryngeal cancer [67], non-small-cell lung cancer (NSCLC) [68,69], and CRC [70]. The CAMKK1 gene mediated the upstream activation of AMP-activated protein kinase (AMPK) by phosphorylation of the α-subunit threonine 172 (Thr172) residue. AMPK is a key regulator in various cellular events and targets, such as in the treatment of type 2 diabetes (T2D) and maintaining homeostasis of the cellular energy [71,72]. The expression levels of LPAR2 have a critical role in carcinogenesis and during tumor progression [73,74,75,76,77]. In a mouse model, overexpression of LPAR2 induces intestinal dysplasia, which therefore alters the proliferation and differentiation of the intestinal epithelial cells (IEC) [78]. The pivotal inflammasome component, Caspase-1, is an emerging player in various diseases progressions, as well as a biomarker for early diagnosis and a therapeutic target [79,80,81,82]. The encoded protein of the NHS gene regulates the development of brain, craniofacial, eye, and tooth, in addition to actin remodeling and thus maintaining cell morphology. Mutations in the NHS gene were found to cause Nance–Horan syndrome (NHS), an X-linked disorder [83,84,85,86,87,88].
Ontology enrichment analysis of the genes provides insight into the role of the significantly methylated genes, showed that hypo- and hypermethylated CpG sites have occurred at various categories of biological processes, cellular components, and molecular functions. The most relevant genes class was associated with the Src-homology 2 (SH2) domain binding (GO:0042169). Interestingly, the genes in SH2 domain binding were hypermethylated (Table S1). Among them is the synaptophysin (SYP) gene, where SH2 domains bind to its multiple carboxyterminal tyrosine-phosphorylated residues [89]. SH2 domains are involved in various signaling transduction and found to regulate cellular behavior and functions upon interactions with other domains and cellular components [90]. However, the SYP gene is a pivotal regulator in the release of neurotransmitters and synaptic plasticity. It was found to be associated with some psychiatric disorders such as attention-deficit/hyperactivity disorder (ADHD) [91], schizophrenia [92], and depression [93]. Other prevailing ontological terms are the regulation of transcription, DNA-templated (GO:0006355) and histone exchange (GO:0043486). The latter of which process genes, acidic nuclear phosphoprotein 32 family member C and member E (ANP32C and ANP32E, respectively) and were also hypermethylated (Table S1). They were frequently found to regulate gene expression by acting on the substitution of histones or histone subunits within the chromatin, especially the ANP32E gene [94,95,96]. The ANP32E gene was enriched in two other cellular component terms, nucleus (GO:0005634) and Swr1 complex (GO:0000812). Although some ANP 32 family members function as tumor suppresser, ANP32C is an oncogene that has been overexpressed in prostate and breast cancer [97,98]. In a similar context, ANP32E is found to induce oncogenesis of triple-negative breast cancer (TNBC) by upregulation of the transcription factor, E2F1 [99]. Furthermore, those genes belong to the regulation of transcription, DNA-templated ontology, were represented by hypo- and hypermethylation patterns (Table S1). Among them is the ASXL transcriptional regulator 2 (ASXL2) gene, in which de novo germline truncation in ASXL2 variants have been associated with various clinical features of intellectual disabilities, macrocephaly, and dysmorphism [100]. Similarly, ASXL2 deficiency in mice model (ASXL2−/−) was directed towards insulin resistance, osteopetrosis, and lipodystrophy [101]. Moreover, it promotes breast carcinogenesis through epigenetic regulation of the estrogen receptor alpha (ERα) [102].
5. Conclusions
In addition to the preliminary known genetic predisposition of keloids, methylation sequencing of CpG sites in keloids revealed significant hyper- and hypomethylated genes in fibroblasts from keloid scars compared to control fibroblasts demonstrated the vital role of DNA methylation as an epigenetic regulation mechanism in keloids formation and progression, as well as a putative therapeutic target, by reversing the methylation status to halt the overgrowth in scars. The DM genes and their products are known to elaborate several biological pathways, signaling, and functions that could be implicated further to understand keloid etiology and targeted treatment development in future exploration.
Acknowledgments
The authors are grateful to all the participants of this study for their invaluable contribution. The authors also would like to express their gratitude to King Khalid University, Saudi Arabia, for providing administrative and technical support.
Supplementary Materials
The following are available online at https://www.mdpi.com/2227-9059/8/7/181/s1, Table S1: The top 100 CpG sites and the associated genes.
Author Contributions
Conceptualization, M.W.F., F.M.W., P.L.D., H.J.W. and E.K.M.; methodology, M.A.A., A.S., S.R. and P.E.M.; software, M.A.A., A.S. and P.E.M.; validation, M.W.F., H.J.W. and P.E.M.; formal analysis, M.A.A., A.S. and P.E.M.; investigation, M.A.A., P.E.M. and A.S.; resources, M.W.F., E.K.M., C.M.P., S.R. and F.M.W.; data curation, M.A.A. and P.E.M.; writing—original draft preparation, M.W.F., J.M.D., M.A.A. and L.N.A.-E.; writing—review and editing, M.A.A., M.W.F., L.N.A.-E., E.K.M., H.J.W., J.M.D., C.M.P., P.L.D. and F.M.W.; visualization, M.A.A., J.M.D., C.M.P., H.J.W. and M.W.F.; supervision, M.W.F., P.L.D., P.E.M. and H.J.W.; project administration, M.W.F.; funding acquisition, M.W.F., F.M.W., and H.J.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Rodrigues M., Kosaric N., Bonham C.A., Gurtner G.C. Wound healing: A cellular perspective. Physiol. Rev. 2019;99:665–706. doi: 10.1152/physrev.00067.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gonzalez A.C.D.O., Andrade Z.D.A., Costa T.F., Medrado A.R.A.P. Wound healing—A literature review. An. Bras. Dermatol. 2016;91:614–620. doi: 10.1590/abd1806-4841.20164741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Potter D.A., Veitch D., Johnston G.A. Scarring and wound healing. Br. J. Hosp. Med. 2019;80:C166–C171. doi: 10.12968/hmed.2019.80.11.C166. [DOI] [PubMed] [Google Scholar]
- 4.Trace A.P., Enos C.W., Mantel A., Harvey V.M. Keloids and hypertrophic scars: A Spectrum of clinical challenges. Am. J. Clin. Dermatol. 2016;17:201–223. doi: 10.1007/s40257-016-0175-7. [DOI] [PubMed] [Google Scholar]
- 5.Safonov I. Normotrophic scars. In: Safonov I., editor. Atlas of Scar Treatment and Correction. Springer; Berlin/Heidelberg, Germany: 2012. pp. 161–188. [DOI] [Google Scholar]
- 6.Shih B., Garside E., McGrouther D.A., Bayat A. Molecular dissection of abnormal wound healing processes resulting in keloid disease. Wound Repair Regen. 2010;18:139–153. doi: 10.1111/j.1524-475X.2009.00553.x. [DOI] [PubMed] [Google Scholar]
- 7.Ogawa R. Keloid and hypertrophic scars are the result of chronic inflammation in the reticular dermis. Int. J. Mol. Sci. 2017;18:606. doi: 10.3390/ijms18030606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Limandjaja G.C., van den Broek L.J., Waaijman T., van Veen H.A., Everts V., Monstrey S., Scheper R.J., Niessen F.B., Gibbs S. Increased epidermal thickness and abnormal epidermal differentiation in keloid scars. Br. J. Dermatol. 2017;176:116–126. doi: 10.1111/bjd.14844. [DOI] [PubMed] [Google Scholar]
- 9.Lemonas P., Ahmad I. Keloid scars: The hidden burden of disease. J. Pigment. Disord. 2015;2:1–5. doi: 10.4172/2376-0427.1000231. [DOI] [Google Scholar]
- 10.Zhang G., Guan Q.Y., Chen G., Qian F., Liang J. DNA methylation of the CDC2L1 gene promoter region decreases the expression of the CDK11p58 protein and reduces apoptosis in keloid fibroblasts. Arch. Dermatol. Res. 2018;310:107–115. doi: 10.1007/s00403-017-1801-9. [DOI] [PubMed] [Google Scholar]
- 11.Halim A.S., Emami A., Salahshourifar I., Kannan T.P. Keloid scarring: Understanding the genetic basis, advances, and prospects. Arch. Plast. Surg. 2012;39:184–189. doi: 10.5999/aps.2012.39.3.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.He Y., Deng Z., Alghamdi M., Lu L., Fear M.W., He L. From genetics to epigenetics: New insights into keloid scarring. Cell Prolif. 2017;50:1–8. doi: 10.1111/cpr.12326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berman B., Maderal A., Raphael B. Keloids and hypertrophic scars: Pathophysiology, classification, and treatment. Dermatol. Surg. 2017;43:S3–S18. doi: 10.1097/DSS.0000000000000819. [DOI] [PubMed] [Google Scholar]
- 14.Mann J., Mann D.A. Epigenetic regulation of wound healing and fibrosis. Curr. Opin. Rheumatol. 2013;25:101–107. doi: 10.1097/BOR.0b013e32835b13e1. [DOI] [PubMed] [Google Scholar]
- 15.Neary R., Watson C.J., Baugh J.A. Epigenetics and the overhealing wound: The role of DNA methylation in fibrosis. Fibrogenes Tissue Repair. 2015;8:1–13. doi: 10.1186/s13069-015-0035-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kader F., Ghai M. DNA methylation-based variation between human populations. Mol. Genet. Genom. 2017;292:5–35. doi: 10.1007/s00438-016-1264-2. [DOI] [PubMed] [Google Scholar]
- 17.Jones L.R., Young W., Divine G., Datta I., Chen K.M., Ozog D., Worsham M.J. Genome-wide scan for methylation profiles in keloids. Dis. Markers. 2015;2015 doi: 10.1155/2015/943176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones L.R., Greene J., Chen K.M., Divine G., Chitale D., Shah V., Datta I., Worsham M.J. Biological significance of genome-wide DNA methylation profiles in keloids. Laryngoscope. 2017;127:70–78. doi: 10.1002/lary.26063. [DOI] [PubMed] [Google Scholar]
- 19.Jones P.A., Takai D. The role of DNA methylation in mammalian epigenetics. Science. 2001;293:1068–1070. doi: 10.1126/science.1063852. [DOI] [PubMed] [Google Scholar]
- 20.Mardaryev A.N. Epigenetic regulation of skin wound healing. In: Botchkarev V., Millar S., editors. Epigenetic Regulation of Skin Development and Regeneration. Humana Press; Cham, Switzerland: 2018. pp. 293–314. Stem Cell Biology and Regenerative Medicine. [DOI] [Google Scholar]
- 21.Robertson K.D. DNA methylation and human disease. Nat. Rev. Genet. 2005;6:597–610. doi: 10.1038/nrg1655. [DOI] [PubMed] [Google Scholar]
- 22.Russell S.B., Russell J.D., Trupin K.M., Gayden A.E., Opalenik S.R., Nanney L.B., Broquist A.H., Raju L., Williams S.M. Epigenetically altered wound healing in keloid fibroblasts. J. Investig. Dermatol. 2010;130:2489–2496. doi: 10.1038/jid.2010.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jin B., Li Y., Robertson K.D. DNA methylation: Superior or subordinate in the epigenetic hierarchy? Genes Cancer. 2011;2:607–617. doi: 10.1177/1947601910393957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Keira S.M., Ferreira L.M., Gragnani A., Duarte I.d.S., Santos I.A.N. Experimental model for fibroblast culture. Acta Cir. Bras. 2004;19:11–16. doi: 10.1590/S0102-86502004000700004. [DOI] [Google Scholar]
- 25.Tucci-Viegas V.M., Hochman B., Frana J.P., Ferreira L.M. Keloid explant culture: A model for keloid fibroblasts isolation and cultivation based on the biological differences of its specific regions. Int. Wound J. 2010;7:339–348. doi: 10.1111/j.1742-481X.2010.00698.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Assenov Y., Müller F., Lutsik P., Walter J., Lengauer T., Bock C. Comprehensive analysis of DNA methylation data with RnBeads. Nat. Methods. 2014;11:1138–1140. doi: 10.1038/nmeth.3115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ritchie M.E., Phipson B., Wu D., Hu Y., Law C.W., Shi W., Smyth G.K. Limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47. doi: 10.1093/nar/gkv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang D., Sherman B.T., Lempicki R.A. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat. Protoc. 2009;4:44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- 29.Huang D., Sherman B.T., Lempicki R.A. Bioinformatics enrichment tools: Paths toward the comprehensive functional analysis of large gene lists. Nucleic Acids Res. 2009;37:1–13. doi: 10.1093/nar/gkn923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Licata L., Lo Surdo P., Iannuccelli M., Palma A., Micarelli E., Perfetto L., Peluso D., Calderone A., Castagnoli L., Cesareni G. SIGNOR 2.0, the SIGnaling network open resource 2.0: 2019 Update. Nucleic Acids Res. 2020;48:D504–D510. doi: 10.1093/nar/gkz949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Deng C.C., Zhu D.H., Chen Y.J., Huang T.Y., Peng Y., Liu S.Y., Lu P., Xue Y.H., Xu Y.P., Yang B., et al. TRAF4 promotes fibroblast proliferation in keloids by destabilizing p53 via interacting with the deubiquitinase USP10. J. Investig. Dermatol. 2019;139:1925–1935.e5. doi: 10.1016/j.jid.2019.03.1136. [DOI] [PubMed] [Google Scholar]
- 32.Arno A.I., Gauglitz G.G., Barret J.P., Jeschke M.G. Up-to-date approach to manage keloids and hypertrophic scars: A useful guide. Burns. 2014;40:1255–1266. doi: 10.1016/j.burns.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coppola M.M., Salzillo R., Segreto F., Persichetti P. Triamcinolone acetonide intralesional injection for the treatment of keloid scars: Patient selection and perspectives. Clin. Cosmet. Investig. Dermatol. 2018;11:387–396. doi: 10.2147/CCID.S133672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Danielsen P.L., Rea S.M., Wood F.M., Fear M.W., Viola H.M., Hool L.C., Gankande T.U., Alghamdi M., Stevenson A.W., Manzur M., et al. Verapamil is less effective than triamcinolone for prevention of keloid scar recurrence after excision in a randomized controlled trial. Acta Derm. Venereol. 2016;96:774–779. doi: 10.2340/00015555-2384. [DOI] [PubMed] [Google Scholar]
- 35.Robles D.T., Moore E., Draznin M., Berg D. Keloids: Pathophysiology and management. Dermatol. Online J. 2007;13:9. [PubMed] [Google Scholar]
- 36.Jin Z., Liu Y. DNA methylation in human diseases. Genes Dis. 2018;5:1–8. doi: 10.1016/j.gendis.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burns S.N. Gene expression, epigenetic regulation, and cancer. In: Mishra M., Bishnupuri K., editors. Epigenetic Advancements in Cancer. Springer; Cham, Switzerland: 2016. pp. 79–96. [DOI] [Google Scholar]
- 38.Robinson C.M., Watson C.J., Baugh J.A. Epigenetics within the matrix, a neo-regulator of fibrotic disease. Epigenetics. 2012;7:987–993. doi: 10.4161/epi.21567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dowson C., O’Reilly S. DNA methylation in fibrosis. Eur. J. Cell Biol. 2016;95:323–330. doi: 10.1016/j.ejcb.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 40.Al-Eitan L.N., Alghamdi M.A., Tarkhan A.H., Al-Qarqaz F.A. Genome-wide tiling array analysis of HPV-induced warts reveals aberrant methylation of protein-coding and non-coding regions. Genes. 2020;11:34. doi: 10.3390/genes11010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Al-Eitan L.N., Alghamdi M.A., Tarkhan A.H., Al-Qarqaz F.A. Epigenome-wide analysis of common warts reveals aberrant promoter methylation. Int. J. Med. Sci. 2020;17:191–206. doi: 10.7150/ijms.39261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Al-Eitan L.N., Alghamdi M.A., Tarkhan A.H., Al-Qarqaz F.A. Genome-wide CpG island methylation profiles of cutaneous skin with and without HPV infection. Int. J. Mol. Sci. 2019;20:4822. doi: 10.3390/ijms20194822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ti D., Li M., Fu X., Han W. Causes and consequences of epigenetic regulation in wound healing. Wound Repair Regen. 2014;22:305–312. doi: 10.1111/wrr.12160. [DOI] [PubMed] [Google Scholar]
- 44.Antequera F., Bird A. CpG islands: A historical perspective. In: Vavouri T., Peinado M., editors. CpG Islands. Methods in Molecular Biology. Volume 1766. Humana Press; New York, NY, USA: 2018. pp. 3–13. [DOI] [PubMed] [Google Scholar]
- 45.Lea A.J., Vockley C.M., Johnston R.A., Del Carpio C.A., Barreiro L.B., Reddy T.E., Tung J. Genome-wide quantification of the effects of DNA methylation on human gene regulation. Elife. 2018;7:1–27. doi: 10.7554/eLife.37513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rauluseviciute I., Drabløs F., Rye M.B. DNA hypermethylation associated with upregulated gene expression in prostate cancer demonstrates the diversity of epigenetic regulation. BMC Med. Genom. 2020;13:1–15. doi: 10.1186/s12920-020-0657-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dedeurwaerder S., Fumagalli D., Fuks F. Unravelling the epigenomic dimension of breast cancers. Curr. Opin. Oncol. 2011;23:559–565. doi: 10.1097/CCO.0b013e32834bd481. [DOI] [PubMed] [Google Scholar]
- 48.Magalhães M., Tost J., Pineau F., Rivals I., Busato F., Alary N., Mely L., Leroy S., Murris M., Caimmi D., et al. Dynamic changes of DNA methylation and lung disease in cystic fibrosis: Lessons from a monogenic disease. Epigenomics. 2018;10:1131–1145. doi: 10.2217/epi-2018-0005. [DOI] [PubMed] [Google Scholar]
- 49.Moore K., McKnight A.J., Craig D., O’Neill F. Epigenome-wide association study for Parkinson’s disease. NeuroMolecular Med. 2014;16:845–855. doi: 10.1007/s12017-014-8332-8. [DOI] [PubMed] [Google Scholar]
- 50.Farkas S.A., Milutin-Gašperov N., Grce M., Nilsson T.K. Genome-wide DNA methylation assay reveals novel candidate biomarker genes in cervical cancer. Epigenetics. 2013;8:1213–1225. doi: 10.4161/epi.26346. [DOI] [PubMed] [Google Scholar]
- 51.Ashktorab H., Daremipouran M., Goel A., Varma S., Leavitt R., Sun X., Brim H. DNA methylome profiling identifies novel methylated genes in African American patients with colorectal neoplasia. Epigenetics. 2014;9:503–512. doi: 10.4161/epi.27644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ashktorab H., Rahi H., Daremiporan M., Lee E.L., Frederick W.A., Laiyemo A.O., Nouraie M., Brim H. Sa1989 novel genes mutation and methylation targets in colon cancer using whole exome sequencing. Gastroenterology. 2013;144:S-353. doi: 10.1016/S0016-5085(13)61298-6. [DOI] [Google Scholar]
- 53.Morán A., Fernández-Marcelo T., Carro J., De Juan C., Pascua I., Head J., Gómez A., Hernando F., Torres A.J., Benito M., et al. Methylation profiling in non-small cell lung cancer: Clinical implications. Int. J. Oncol. 2012;40:739–746. doi: 10.3892/ijo.2011.1253. [DOI] [PubMed] [Google Scholar]
- 54.Pradhan M.P., Desai A., Palakal M.J. Systems biology approach to stage-wise characterization of epigenetic genes in lung adenocarcinoma. BMC Syst. Biol. 2013;7:141. doi: 10.1186/1752-0509-7-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Angulo J.C., Andrés G., Ashour N., Sánchez-Chapado M., López J.I., Ropero S. Development of castration resistant prostate cancer can be predicted by a DNA hypermethylation profile. J. Urol. 2016;195:619–626. doi: 10.1016/j.juro.2015.10.172. [DOI] [PubMed] [Google Scholar]
- 56.Kim Y.H., Lee H.C., Kim S.Y., Yeom Y.I., Ryu K.J., Min B.H., Kim D.H., Son H.J., Rhee P.L., Kim J.J., et al. Epigenomic analysis of aberrantly methylated genes in colorectal cancer identifies genes commonly affected by epigenetic alterations. Ann. Surg. Oncol. 2011;18:2338–2347. doi: 10.1245/s10434-011-1573-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.How-Kit A., Dejeux E., Dousset B., Renault V., Baudry M., Terris B., Tost J. DNA methylation profiles distinguish different subtypes of gastroenteropancreatic neuroendocrine tumors. Epigenomics. 2015;7:1245–1258. doi: 10.2217/epi.15.85. [DOI] [PubMed] [Google Scholar]
- 58.Almén M.S., Jacobsson J.A., Moschonis G., Benedict C., Chrousos G.P., Fredriksson R., Schiöth H.B. Genome wide analysis reveals association of a FTO gene variant with epigenetic changes. Genomics. 2012;99:132–137. doi: 10.1016/j.ygeno.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 59.Lacunza E., Canzoneri R., Rabassa M.E., Zwenger A., Segal-Eiras A., Croce M.V., Abba M.C. RHBDD2: A 5-fluorouracil responsive gene overexpressed in the advanced stages of colorectal cancer. Tumor Biol. 2012;33:2393–2399. doi: 10.1007/s13277-012-0503-3. [DOI] [PubMed] [Google Scholar]
- 60.Abba M.C., Lacunza E., Nunez M.I., Colussi A., Isla-Larrain M., Segal-Eiras A., Croce M.V., Aldaz C.M. Rhomboid domain containing 2 (RHBDD2): A novel cancer-related gene over-expressed in breast cancer. Biochim. Biophys. Acta Mol. Basis Dis. 2009;1792:988–997. doi: 10.1016/j.bbadis.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Canzoneri R., Lacunza E., Isla Larrain M., Croce M.V., Abba M.C. Rhomboid family gene expression profiling in breast normal tissue and tumor samples. Tumor Biol. 2014;35:1451–1458. doi: 10.1007/s13277-013-1199-8. [DOI] [PubMed] [Google Scholar]
- 62.Zhu J., Wu K., Lin Z., Bai S., Wu J., Li P., Xue H., Du J., Shen B., Wang H., et al. Identification of susceptibility gene mutations associated with the pathogenesis of familial nonmedullary thyroid cancer. Mol. Genet. Genom. Med. 2019;7:1–7. doi: 10.1002/mgg3.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Roos L., Sandling J.K., Bell C.G., Glass D., Mangino M., Spector T.D., Deloukas P., Bataille V., Bell J.T. Higher nevus count exhibits a distinct DNA methylation signature in healthy human skin: Implications for melanoma. J. Investig. Dermatol. 2017;137:910–920. doi: 10.1016/j.jid.2016.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang Z.-Y., Li S.-Z., Zhang H.-H., Wu Q.-R., Gong J., Liang T., Gao L., Xing N.-N., Liu W.-B., Du R.-L., et al. Stabilization of ATF5 by TAK1–nemo-like kinase critically regulates the interleukin-1β-stimulated C/EBP signaling pathway. Mol. Cell. Biol. 2015;35:778–788. doi: 10.1128/MCB.01228-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ishitani T., Hirao T., Suzuki M., Isoda M., Ishitani S., Harigaya K., Kitagawa M., Matsumoto K., Itoh M. Nemo-like kinase suppresses Notch signalling by interfering with formation of the Notch active transcriptional complex. Nat. Cell Biol. 2010;12:278–285. doi: 10.1038/ncb2028. [DOI] [PubMed] [Google Scholar]
- 66.Zhang B., Li K.Y., Chen H.Y., Pan S.D., Chen S.F., Zhang W.F., Xia C.P., Jiang L.C., Liu X.B., Zhao F.J., et al. Lentivirus-based RNA silencing of nemo-like kinase (NLK) inhibits the CAL 27 human adenosquamos carcinoma cells proliferation and blocks G0/G1 phase to S phase. Int. J. Med. Sci. 2013;10:1301–1306. doi: 10.7150/ijms.6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dong J.R., Guo N., Zhao J.P., Liu P.D., Feng H.H., Li Y. Inhibition of nemo-like kinase increases taxol sensitivity in laryngeal cancer. Asian Pac. J. Cancer Prev. 2013;14:7137–7141. doi: 10.7314/APJCP.2013.14.12.7137. [DOI] [PubMed] [Google Scholar]
- 68.Shi C., Xu L., Tang Z., Zhang W., Wei Y., Ni J., Zhang S., Feng J. Knockdown of Nemo-like kinase promotes metastasis in non-small-cell lung cancer. Oncol. Rep. 2019;42:1090–1100. doi: 10.3892/or.2019.7226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Suwei D., Liang Z., Zhimin L., Ruilei L., Yingying Z., Zhen L., Chunlei G., Zhangchao L., Yuanbo X., Jinyan Y., et al. NLK functions to maintain proliferation and stemness of NSCLC and is a target of metformin. J. Hematol. Oncol. 2015;8:1–14. doi: 10.1186/s13045-015-0203-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhang W., He J., Du Y., Gao X.H., Liu Y., Liu Q.Z., Chang W.J., Cao G.W., Fu C.G. Upregulation of nemo-like kinase is an independent prognostic factor in colorectal cancer. World J. Gastroenterol. 2015;21:8935–8942. doi: 10.3748/wjg.v21.i29.8836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kodiha M., Ho-Wo-Cheong D., Stochaj U. Pharmacological AMP-kinase activators have compartment-specific effects on cell physiology. Am. J. Physiol. Cell Physiol. 2011;301:1307–1315. doi: 10.1152/ajpcell.00309.2011. [DOI] [PubMed] [Google Scholar]
- 72.Viollet B., Foretz M., Schlattner U. Bypassing AMPK phosphorylation. Chem. Biol. 2014;21:567–569. doi: 10.1016/j.chembiol.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 73.Kitayama J., Shida D., Sako A., Ishikawa M., Hama K., Aoki J., Arai H., Nagawa H. Over-expression of lysophosphatidic acid receptor-2 in human invasive ductal carcinoma. Breast Cancer Res. 2004;6:640–646. doi: 10.1186/bcr935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Radhika V., Ha J.H., Jayaraman M., Tsim S.T., Dhanasekaran N. Mitogenic signaling by lysophosphatidic acid (LPA) involves Gα12. Oncogene. 2005;24:4597–4603. doi: 10.1038/sj.onc.1208665. [DOI] [PubMed] [Google Scholar]
- 75.Takahashi K., Fukushima K., Tanaka K., Minami K., Ishimoto K., Otagaki S., Fukushima N., Honoki K., Tsujiuchi T. Involvement of LPA signaling via LPA receptor-2 in the promotion of malignant properties in osteosarcoma cells. Exp. Cell Res. 2018;369:316–324. doi: 10.1016/j.yexcr.2018.05.037. [DOI] [PubMed] [Google Scholar]
- 76.Lin S., Lee S.J., Shim H., Chun J., Yun C.C. The absence of LPA receptor 2 reduces the tumorigenesis by Apc Min mutation in the intestine. Am. J. Physiol. Gastrointest. Liver Physiol. 2010;299:1128–1138. doi: 10.1152/ajpgi.00321.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lin S., Wang D., Iyer S., Ghaleb A.M., Shim H., Yang V.W., Chun J., Yun C.C. The absence of LPA2 attenuates tumor formation in an experimental model of colitis-associated cancer. Gastroenterology. 2009;136:1711–1720. doi: 10.1053/j.gastro.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yoshida M., He P., Yun C.C. Transgenic expression of human lysophosphatidic acid receptor LPA2 in mouse intestinal epithelial cells induces intestinal dysplasia. PLoS ONE. 2016;11:1–16. doi: 10.1371/journal.pone.0154527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fu K.Y.J., Zamudio R., Frost J.H., Almuedo A., Steinberg H., Clipman S.J., Duran G., Marcus R., Crawford T., Alyesh D., et al. Association of caspase-1 polymorphisms with chagas cardiomyopathy among individuals in Santa Cruz, Bolivia. Rev. Soc. Bras. Med. Trop. 2017;50:516–523. doi: 10.1590/0037-8682-0015-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bauer R.N., Brighton L.E., Mueller L., Xiang Z., Rager J.E., Fry R.C., Peden D.B., Jaspers I. Influenza enhances caspase-1 in bronchial epithelial cells from asthmatic volunteers and is associated with pathogenesis. J. Allergy Clin. Immunol. 2012;130:958–967. doi: 10.1016/j.jaci.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zheng F., Gong Z., Xing S., Xing Q. Overexpression of caspase-1 in aorta of patients with coronary atherosclerosis. Heart Lung Circ. 2014;23:1070–1074. doi: 10.1016/j.hlc.2014.04.256. [DOI] [PubMed] [Google Scholar]
- 82.McKenzie B.A., Mamik M.K., Saito L.B., Boghozian R., Monaco M.C., Major E.O., Lu J.Q., Branton W.G., Power C. Caspase-1 inhibition prevents glial inflammasome activation and pyroptosis in models of multiple sclerosis. Proc. Natl. Acad. Sci. USA. 2018;115:E6065–E6074. doi: 10.1073/pnas.1722041115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Burdon K.P., McKay J.D., Sale M.M., Russell-Eggitt I.M., Mackey D.A., Wirth M.G., Elder J.E., Nicoll A., Clarke M.P., FitzGerald L.M., et al. Mutations in a novel gene, NHS, cause the pleiotropic effects of Nance-Horan syndrome, including severe congenital cataract, dental anomalies, and mental retardation. Am. J. Hum. Genet. 2003;73:1120–1130. doi: 10.1086/379381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Brooks S.P., Coccia M., Tang H.R., Kanuga N., Machesky L.M., Bailly M., Cheetham M.E., Hardcastle A.J. The Nance-Horan syndrome protein encodes a functional WAVE homology domain (WHD) and is important for co-ordinating actin remodelling and maintaining cell morphology. Hum. Mol. Genet. 2010;19:2421–2432. doi: 10.1093/hmg/ddq125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shoshany N., Avni I., Morad Y., Weiner C., Einan-Lifshitz A., Pras E. NHS gene mutations in Ashkenazi Jewish families with Nance–Horan syndrome. Curr. Eye Res. 2017;42:1240–1244. doi: 10.1080/02713683.2017.1304560. [DOI] [PubMed] [Google Scholar]
- 86.Sun W., Xiao X., Li S., Guo X., Zhang Q. Exome sequencing of 18 Chinese families with congenital cataracts: A new sight of the NHS gene. PLoS ONE. 2014;9:e100455. doi: 10.1371/journal.pone.0100455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Li H., Yang L., Sun Z., Yuan Z., Wu S., Sui R. A novel small deletion in the NHS gene associated with Nance-Horan syndrome. Sci. Rep. 2018;8:1–7. doi: 10.1038/s41598-018-20787-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ling C., Sui R., Yao F., Wu Z., Zhang X., Zhang S. Whole exome sequencing identified a novel truncation mutation in the NHS gene associated with Nance-Horan syndrome. BMC Med. Genet. 2019;20:1–7. doi: 10.1186/s12881-018-0725-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Felkl M., Leube R.E. Interaction assays in yeast and cultured cells confirm known and identify novel partners of the synaptic vesicle protein synaptophysin. Neuroscience. 2008;156:344–352. doi: 10.1016/j.neuroscience.2008.07.033. [DOI] [PubMed] [Google Scholar]
- 90.Pawson T., Gish G.D., Nash P. SH2 domains, interaction modules and cellular wiring. Trends Cell Biol. 2001;11:504–511. doi: 10.1016/S0962-8924(01)02154-7. [DOI] [PubMed] [Google Scholar]
- 91.Liu L., Chen Y., Li H., Qian Q., Yang L., Glatt S.J., Faraone S.V., Wang Y. Association between SYP with attention-deficit/hyperactivity disorder in Chinese Han subjects: Differences among subtypes and genders. Psychiatry Res. 2013;210:308–314. doi: 10.1016/j.psychres.2013.04.029. [DOI] [PubMed] [Google Scholar]
- 92.Shen Y.C., Tsai H.M., Ruan J.W., Liao Y.C., Chen S.F., Chen C.H. Genetic and functional analyses of the gene encoding synaptophysin in schizophrenia. Schizophr. Res. 2012;137:14–19. doi: 10.1016/j.schres.2012.01.028. [DOI] [PubMed] [Google Scholar]
- 93.Kuwano N., Kato T.A., Mitsuhashi M., Sato-Kasai M., Shimokawa N., Hayakawa K., Ohgidani M., Sagata N., Kubo H., Sakurai T., et al. Neuron-related blood inflammatory markers as an objective evaluation tool for major depressive disorder: An exploratory pilot case-control study. J. Affect. Disord. 2018;240:88–98. doi: 10.1016/j.jad.2018.07.040. [DOI] [PubMed] [Google Scholar]
- 94.Reilly P.T., Yu Y., Hamiche A., Wang L. Cracking the ANP32 whips: Important functions, unequal requirement, and hints at disease implications. BioEssays. 2014;36:1062–1071. doi: 10.1002/bies.201400058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gursoy-Yuzugullu O., Ayrapetov M.K., Price B.D. Histone chaperone Anp32e removes H2A.Z from DNA double-strand breaks and promotes nucleosome reorganization and DNA repair. Proc. Natl. Acad. Sci. USA. 2015;112:7507–7512. doi: 10.1073/pnas.1504868112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Obri A., Ouararhni K., Papin C., Diebold M.L., Padmanabhan K., Marek M., Stoll I., Roy L., Reilly P.T., Mak T.W., et al. ANP32E is a histone chaperone that removes H2A.Z from chromatin. Nature. 2014;505:648–653. doi: 10.1038/nature12922. [DOI] [PubMed] [Google Scholar]
- 97.Kadkol S.S., Brody J.R., Pevsner J., Bai J., Pasternack G.R. Modulation of oncogenic potential by alternative gene use in human prostate cancer. Nat. Med. 1999;5:275–279. doi: 10.1038/6488. [DOI] [PubMed] [Google Scholar]
- 98.Kadkol S.S., Naga G.A.E., Brody J.R., Bai J., Gusev Y., Dooley W.C., Pasternack G.R. Expression of pp32 gene family members in breast cancer. Breast Cancer Res. Treat. 2001;68:65–73. doi: 10.1023/A:1017919507109. [DOI] [PubMed] [Google Scholar]
- 99.Xiong Z., Ye L., Zhenyu H., Li F., Xiong Y., Lin C., Wu X., Deng G., Shi W., Song L., et al. ANP32E induces tumorigenesis of triple-negative breast cancer cells by upregulating E2F1. Mol. Oncol. 2018;12:896–912. doi: 10.1002/1878-0261.12202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Shashi V., Pena L.D., Kim K., Burton B., Hempel M., Schoch K., Walkiewicz M., McLaughlin H.M., Cho M., Stong N., et al. De novo truncating variants in ASXL2 are associated with a unique and recognizable clinical phenotype. Am. J. Hum. Genet. 2016;99:991–999. doi: 10.1016/j.ajhg.2016.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Izawa T., Rohatgi N., Fukunaga T., Wang Q.T., Silva M.J., Gardner M.J., McDaniel M.L., Abumrad N.A., Semenkovich C.F., Teitelbaum S.L., et al. ASXL2 regulates glucose, lipid, and skeletal homeostasis. Cell Rep. 2015;11:625–637. doi: 10.1016/j.celrep.2015.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Park U.H., Kang M.R., Kim E.J., Kwon Y.S., Hur W., Yoon S.K., Song B.J., Park J.H., Hwang J.T., Jeong J.C., et al. ASXL2 promotes proliferation of breast cancer cells by linking ERα to histone methylation. Oncogene. 2016;35:3742–3752. doi: 10.1038/onc.2015.443. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.