Abstract
This cohort study surveys pediatric patients and their caregivers to elicit reasons for their preferences for nonoperative management vs surgery for uncomplicated appendicitis.
Nonoperative management (NOM) with antibiotics alone has been shown to be safe for uncomplicated appendicitis in pediatric patients.1,2,3 Shared decision-making to choose between 2 treatments may be facilitated by a better understanding of how patients and caregivers value the specific risks and benefits of each treatment and how those are associated with their treatment decisions.4 A recent survey of parents of children who were healthy showed that 42% of caregivers preferred NOM for their child’s appendicitis; however, these families were making only a hypothetical treatment decision, and factors affecting their preferences were not solicited.5 Our objective in this study was to compare values regarding the risks and benefits of each treatment option between patient-caregiver dyads who chose surgery vs NOM for the child’s appendicitis.
Methods
As part of a randomized clinical trial (NCT02110485), patients were evaluated by a research team physician who introduced both treatment options, answered initial questions, and then randomized patient-caregiver dyads to receive a scripted standardized surgical consultation with or without a tablet-based patient activation tool (https://vimeo.com/91207174). This study was approved by the Nationwide Children's Hospital institutional review board and written consent was obtained from all participants, with assent obtained from children 9 years and older. Patients aged 7 to 17 years and their caregivers were enrolled from March 2014 to April 2016. All dyads who used the patient activation tool received the same information about each treatment’s expected course and associated risks and benefits and subsequently completed a values exercise rating the importance of 8 treatment-associated risks and benefits of surgery vs NOM using a 5-point Likert scale.6 Three questions assessed aversion to risks of surgical management, 3 assessed aversion to risks of NOM, and 2 assessed preferences associated with missing school or activities and work. After exercise completion, they chose surgery or NOM for the child’s appendicitis treatment.
Value scores were compared by treatment decision using Cochran-Armitage tests, with a significance threshold set at P < .05. Data analysis for this report was performed from July 2019 to March 2020, and SAS Enterprise Guide 7.1 (SAS Institute) was used for all statistical analyses.
Results
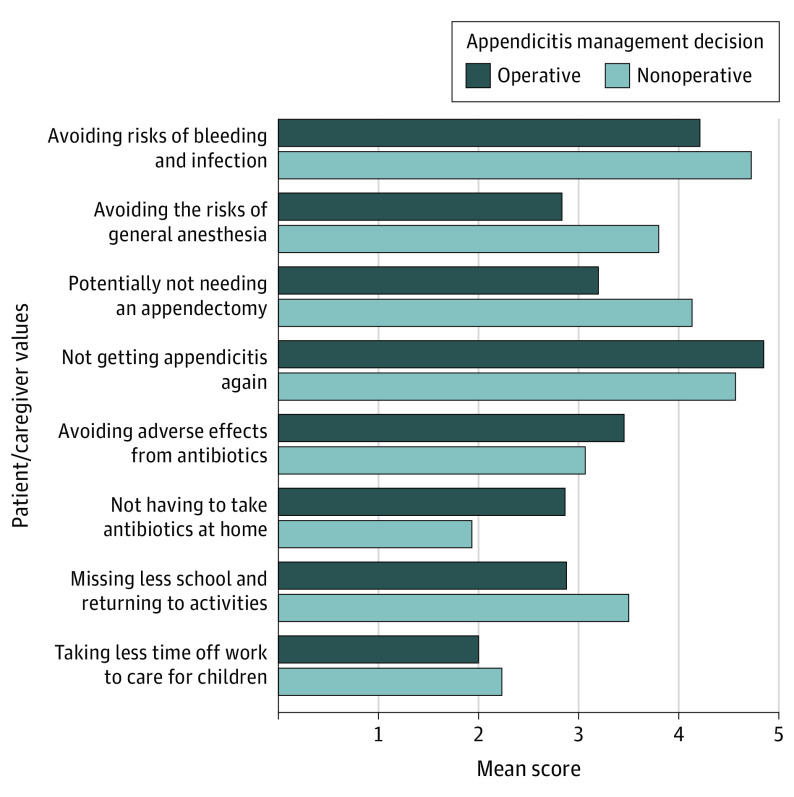
Of 96 individual participants, 66 (69%) chose surgery and 30 (31%) chose NOM. The median age of included children was 12 (interquartile range, 10-14) years, with 58 male participants of 96 total participants (60%). There were no significant differences between participants choosing surgery vs NOM in levels of education, income, employment, or marital status; however, patient-caregiver dyads choosing surgery were more likely to have been transferred from another institution (29 of 66 [43.9%] vs 7 of 30 [23.3%]; P = .03) and speak primarily English at home (59 of 61 [91.8%] vs 23 of 30 [76.7%]; P = .04). Mean scores for each treatment-associated risk or benefit according to treatment choice are shown in the Figure. In the group choosing surgery, the highest 3 priorities were avoiding recurrence of appendicitis, risks of bleeding and infection, and adverse effects from antibiotics (mean [SE] scores, 4.8 [0.07], 4.2 [0.11], and 3.5 [0.16], respectively). In the NOM group, the 2 highest priorities were the same as the surgery group, with the third being avoiding an operation for appendicitis (mean [SE] scores, 4.7 [0.15], 4.7 [0.10], and 4.1 [0.16], respectively). The overall lowest 3 priorities were missing less school and returning to activities and not having to take antibiotics at home (among children) and taking less time off work to care for a child (among caregivers) (mean [SE] scores, 3.1 [0.15], 2.6 [0.14], and 2.1 [0.13], respectively).
Figure. Mean Scores for Treatment-Associated Benefits and Risks According to Treatment Choice.
The mean value for each survey question is displayed based on treatment decision (light blue: nonoperative management with antibiotics alone; dark blue: operative management with urgent laparoscopic appendectomy).
Patient-caregiver dyads differed in their answers to the following questions assessing aversion to surgical risks, on a scale from 1 (least valued) to 5 (most valued): avoiding risks of bleeding and infection (surgery: 1 [least valued], 1 participant [2%]; 2, 1 participant [2%]; 3, 12 participants [18%]; 4, 21 participants [32%]; 5 [most valued], 31 participants [47%] vs NOM: 1 [least valued], 0 participants; 2, 0 participants; 3, 1 participant [3%]; 4, 6 participants [21%]; 5 [most valued], 23 participants [76%]; P = .007), avoiding the risks of general anesthesia (surgery: 10 [15%]; 15 [23%]; 22 [33%]; 14 [21%]; 13 [20%] vs NOM: 0; 4 [13%]; 7 [23%]; 10 [33%]; 9 [30%]; P < .001), and potentially not needing an appendectomy (surgery: 9 [14%]; 9 [14%]; 21 [32%]; 14 [21%]; 13 [20%]; vs NOM: 1 [3%]; 0; 3 [10%]; 16 [53%]; 10 [33%]; P < .001). In each case, the responses favored NOM. In assessing aversion to risks of NOM, the groups differed in their answer to the question on not having to take antibiotics at home, favoring surgery (surgery: 18 [27%]; 9 [14%]; 14 [21%]; 14 [21%]; 11 [17%] vs NOM: 1 [3%]; 0; 3 [10%]; 16 [53%]; 10 [33%]; P = .003). Compared with the surgical group, participants who chose NOM had a nonsignificant difference in valuing missing less school (surgery: 14 [21%]; 14 [21%]; 12 [18%]; 18 [27%]; 8 [12%] vs NOM: 5 [17%]; 4 [13%]; 3 [10%]; 7 [23%]; 11 [37%]; P = .05).
Discussion
The relative importance of treatment-associated risks and benefits differed between patients and caregivers choosing surgery vs NOM. However, the 2 most highly prioritized treatment-associated risks and benefits were the same in both groups. This suggests that the associated risks and benefits of each treatment were interpreted and valued differently by individual patients and caregivers. These results support the need for shared decision-making with patients and their caregivers when deciding on treatment for uncomplicated appendicitis.
References
- 1.Georgiou R, Eaton S, Stanton MP, Pierro A, Hall NJ. Efficacy and safety of nonoperative treatment for acute appendicitis: a meta-analysis. Pediatrics. 2017;139(3):e20163003. doi: 10.1542/peds.2016-3003 [DOI] [PubMed] [Google Scholar]
- 2.Huang L, Yin Y, Yang L, Wang C, Li Y, Zhou Z. Comparison of antibiotic therapy and appendectomy for acute uncomplicated appendicitis in children: a meta-analysis. JAMA Pediatr. 2017;171(5):426-434. doi: 10.1001/jamapediatrics.2017.0057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Minneci PC, Mahida JB, Lodwick DL, et al. Effectiveness of patient choice in nonoperative vs surgical management of pediatric uncomplicated acute appendicitis. JAMA Surg. 2016;151(5):408-415. doi: 10.1001/jamasurg.2015.4534 [DOI] [PubMed] [Google Scholar]
- 4.Barry MJ, Edgman-Levitan S. Shared decision making—pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780-781. doi: 10.1056/NEJMp1109283 [DOI] [PubMed] [Google Scholar]
- 5.Brahmamdam P, Carveth SL, Smyth M, Gendelman BS, Maisels MJ. Factors influencing choice of medical vs. surgical treatment of pediatric appendicitis. J Pediatr Surg. 2019;54(9):1800-1803. doi: 10.1016/j.jpedsurg.2019.02.053 [DOI] [PubMed] [Google Scholar]
- 6.Minneci PC, Cooper JN, Leonhart K, et al. Effects of a patient activation tool on decision making between surgery and nonoperative management for pediatric appendicitis: a randomized clinical trial. JAMA Netw Open. 2019;2(6):e195009. doi: 10.1001/jamanetworkopen.2019.5009 [DOI] [PMC free article] [PubMed] [Google Scholar]