Abstract
Historically, infectious diseases have been the leading cause of human psychosomatic strain and death tolls. This research investigated the recent threat of COVID-19 contagion, especially its impact among frontline paramedics treating patients with COVID-19, and their perception of self-infection, which ultimately increases their agonistic behaviour. Based on the stressor–strain–outcome paradigm, a research model was proposed and investigated using survey-based data through a structured questionnaire. The results found that the perceived threat of COVID-19 contagion (emotional and cognitive threat) was positively correlated with physiological anxiety, depression, and emotional exhaustion, which led toward agonistic behaviour. Further, perceived social support was a key moderator that negatively affected the relationships between agonistic behaviour and physiological anxiety, depression, and emotional exhaustion. These findings significantly contributed to the current literature concerning COVID-19 and pandemic-related effects on human behaviour. This study also theorized the concept of human agonistic behaviour, which has key implications for future researchers.
Keywords: COVID-19, anxiety, depression, agonistic behaviour, social support
1. Introduction
Since December 2019, the global health system has been fighting with the growing number of cases of COVID-19, a viral respiratory syndrome that first appeared in China and tentatively named 2019-nCoV1 or SARS-CoV-2 [1]. The World Health Organization has assessed that the rate of COVID-19 spread is expected to be very high and long-lasting [2]. As of 4 July 2020, the confirmed number of patients with COVID-19 had reached 11.108 million, causing over 525,790 mortalities worldwide [3]. The rare history and lack of vaccines to control this novel virus may also cause a high level of panic. During a panic, healthcare personnel (in this study, paramedics, defined as “a person who is trained to give emergency medical treatment of sick persons or assist medical professionals”) face not only physical challenges but also mental burdens, including psychological distress and fear [4,5]. The unexpected rise in confirmed cases has brought huge self-infection threats and physical and mental pressure to frontline paramedics [6]. Many health professionals’ worldwide have become infected and died [7]. The threat of contagion is very high due to the novel nature of COVID-19 and its exponential spread rate compared to other diseases that paramedics encounter every day. Meanwhile, the lack of availability of appropriate drugs to treat COVID-19 patients is another potential cause of the high threat from the current pandemic. This risk is bound to alter frontline paramedics’ behaviour and working conditions, and it may influence the treatment of patients. Thus, a study is needed to measure the pervasiveness of several health disorders caused by the threat of self-infection from COVID-19 among frontline paramedics treating patients with COVID-19.
Owing to the increased mortality rate associated with the virus, healthcare professionals and the public have experienced psychological concerns such as anxiety, depression, and emotional exhaustion [8]. Healthcare personnel not only tolerate too much workload but also have an extreme risk of self-infection [9]. This risk and the accompanying work environments with inadequate protection, lack of contact with family members, frustration, prejudice, and fear of getting infected further exacerbate the noted psychological health issues [10]. Furthermore, prolonged fear of illness increases individuals’ health disorders [9], leading to behavioural shifts. Similarly, a prior study posited that perceived threats and the resulting anxiety, discomfort, emotional stress, adaptation difficulties, and depression affect behavioural changes [11]. Concurrently, mass tragedies, especially those involving infectious diseases, often prompt high fear that causes enormous interruptions to individuals’ behaviour and psychological well-being [12]. In contrast with the current literature and editorial reviews, this investigation expects to lure public focus to the agonistic behaviour of frontline paramedics, which is caused by their physiological anxiety, depression, and emotional exhaustion.
Psychosocial interventions have demonstrated that stress-related ailments may affect individual behaviours. The negative consequences of stressors are especially common in humans; perhaps since we have a high degree of symbolic thinking, which may cause a constant strain response to various adverse living and working environments [13]. Based on the assessment of perceived threat, humans and other animals respond accordingly. Therefore, considering the theory of agonistic behaviour [14], this research examined the agonistic behaviour of frontline paramedics treating patients with COVID-19. Agonistic behaviour refers to “the complex of aggression, threat, appeasement, and avoidance behaviours that occur during encounters between members of the same species” [15]. Agonistic behaviour varies among species, which is integrated with a threat, aggression, and submissive interaction. These are also related to aggression in function and physiology; but not in the narrow sense of aggressive behaviour [16]. A prior study [17] extended the theory of agonistic behaviour from the biology and psychology disciplines into the context of marketing and found the impact of perceived scarcity, which increases attractiveness and leads to buying behaviour. However, one piece of knowledge is still unknown about human agonistic behaviour, and a paucity of theoretical development in measuring human agonistic behaviour motivated the authors to develop an in-depth understanding of this vital concept.
Therefore, the authors further extended the theory of agonistic behaviour from the field of animal biological sciences to human behavioural science. The authors integrated the stressor–strain–outcome (SSO) model with the theory of agonistic behaviour to examine the effects of the perceived threat of COVID-19 on human agonistic behaviour. The research contributes by developing and validating the theoretical framework using real-life scenarios—frontline paramedics treating patients with COVID-19. This informs the current transformation of studying animal agonistic behaviour to human agonistic behaviour. Specifically, this study explains that the higher the perceived threat level of COVID-19, the higher the degree of physiological anxiety, depression, and emotional exhaustion leading towards agonistic behaviour among frontline paramedics.
Another factor related to agonistic behaviour is perceived social support (PSS), which refers to individuals’ feelings of being cared for, valued, loved, and having a sense of belonging to those who are relied on [18]. Several studies have shown that, for people with anxiety and depression, a higher sense of social support may be psychologically comforting [17,18,19,20]. Of course, social support can have a salutary effect on health. Concurrently, the potential moderating effect of PSS on human agonistic behaviour has received little interest from scholars. Therefore, our study also examined the moderating role of PSS on the association between selected strain factors (physiological anxiety, depression, and emotional exhaustion) and the agonistic behaviour of frontline paramedics. In this study context, understanding human agonistic behaviour will help to determine specific characteristics and potential mechanisms of human aggression and violence in a variety of contexts.
2. Theoretical Support and Conceptualisation
2.1. Theory of Agonistic Behaviour
Agonistic behaviour is also known as agonism—survivalist animal behaviour, including defence, avoidance, and aggression. The term agonistic behaviour was first used to describe animal fighting behaviour [21]. It is an adaptive behaviour resulting from conflicts within the same species members [14]. While there is no commonly accepted definition of human agonism, it has usually been defined as the act of triggering psychological or physical harm to other persons or in the destruction of property [15]. Moreover, it is further defined as ‘the individual’s aggressive verbal and physical tendencies and aggressive attitudes’ [22]. Agonistic behaviour can serve as a tool for distinct antisocial, constructive activities, and destructive acts. In both human and non-humans, agonistic behaviour is significantly influenced by the general principles of operant and classical conditioning learning and social modelling [17]. The biologist who favoured this concept recognised that behavioural stimuli and underlying feelings and approaches are frequently the same; and actual behaviour is dependent on other factors, especially distance to the stimulus [23]. Moreover, the term ‘agonistic’ introduces that the differences between aggressive and agonistic behaviours have been blurred, and these two labels are often used interchangeably in the literature. In humans, aggression is repeatedly related to living conditions [17].
Behaviour also depends on the level of awareness among group members when stressful events occur in a social environment because individuals are susceptible to behavioural signals [24]. One primary reaction during the pandemic is fear of contagion. Humans react like other animals because they have a similar defence system against ecological threats [25]. Negative emotions brought about by threats can be contagious, and fear makes threats more imminent [26,27]. Behaviour has, in part, a genetic basis, which generally is learned in a social context. Several factors can cause positive and negative behavioural change. Previous literature discussed the change in agonistic behaviour of animals species rather than the human species. This study thus empirically investigated agonistic behaviour in humans and assessed the effect of the perceived threat of COVID-19 on agonistic behaviour by employing the SSO model. This study will make a significant contribution to the existing theory of agonistic behaviour by elucidating how to measure human psychological cognition and behaviour.
2.2. SSO Perspective
Our framework is based on the SSO model because we examined the influence of the perceived threat of COVID-19 (a stressor) on agonistic behaviour [28]. This model divulges how stressors become prominent in individuals’ lives, indicating that the stressor source has a direct influence on the strain, which later contributes to outcome variables. Stressors are environmental stimuli that individuals experience and transmit stress. Strain and outcomes are an individual’s personal emotional, and behavioural responses to stressors [13]. Summing up, the SSO model considers that strain is the result of sensing stressors and the antecedent of the outcome variable. In the past, SSO models have been used to comprehend stress in the workplace and behavioural change as an outcome variable [29,30,31,32]. However, in the context of measuring agonistic behaviour among humans, the implementation of the SSO model has not been sufficiently investigated.
With the rapid rise in COVID-19 cases, the severe threat to medical staff is imminent, which increases their physiological and psychosomatic strain [33]. In addition, the availability of equipment and pandemic control preparedness may have a moral effect on medical personnel [34]. However, the threat of getting sick from COVID-19 persists, which also puts stress on paramedical personnel. This stress further affects the psychosomatic state of frontline paramedics and increases their agonistic behaviour. Recent studies have also confirmed that the perceived fear of COVID-19 contagion affects individuals’ psychological distress [12,34,35].
Since outcome factors interact with psychological responses and perceived stressors, the current research model included three valuable and practical individual strains. The first is physiological anxiety—“a level and nature of anxiety, including physiological worry/oversensitivity, social concerns and concentration” [36]. The second is depression—“a mental illness with physiological and psychological consequences, including sluggishness, diminished interest and pleasure, and disturbances in sleep and appetite” [37]. The third is emotional exhaustion—“the extent to which employees feel drained and overwhelmed by their work” [31].
In this study, agonistic behaviour—“adaptive acts which arise out of conflicts between two members of the same species”—was our dependent variable [15]. In prior literature, it was mostly used interchangeably with aggressive behaviour. Few scholars have discussed human agonistic behaviour, particularly in the field of marketing and customers’ buying behaviour [15,17]. However, there is no empirical evidence concerning the impact of the perceived threat of COVID-19 or any other pandemic-related fears from the perspective of the SSO model. This motivated the authors to investigate the possible consequences of human agonistic behaviour. The SSO model can be an effective way because it emphasises the positive effect of the environmental stimulus on the internal and external behaviour of frontline paramedics treating patients with COVID-19. Moreover, the sequential process of the SSO model has been used to test the theoretical avowals made in this study, which includes how perceived threat of COVID-19 affect the agonistic behaviour of frontline paramedics by creating physiological anxiety, depression, and emotional exhaustion.
3. Research Model and Hypotheses Development
3.1. Perceived Threat of COVID-19
In this section, we will discuss how threats and risks may be perceived and responded to by people during a pandemic and its aftermath; specifically, fear causes individuals to change their behaviour. Intense fear produces the greatest behavioural changes when people experience physical and psychosomatic disorders such as anxiety, depression, and emotional exhaustion [38,39,40]; whereas intense fear can lead to aggressive and defensive responses [26]. Therefore, we adapted the previous Brief Illness Perception Questionnaire (BIPQ) [41] to determine the level of perceived threat among frontline paramedics treating patients with COVID-19. The concept of illness perception is related to how a person perceives the illness as well as the cognitive structuring of the status of being ill. The model recommends that situational stimuli can produce cognitive and emotional representations of health threats or illness [41]. In other terms, illness perception is the cognitive and emotional representations of patients’ viewpoints about the disease [42].
This cognitive and emotional model also includes beliefs about the treatment and control of the situation. The emotional and cognitive interpretation and evaluation about the perception of illness are the determinants of their behavioural reactions, which is shaped by individuals’ experiences, knowledge levels, and mental strain [43]. Therefore, per prior directions [43], we divided and validated the scale into two parts based on the emotional and cognitive perception of the threat of illness from COVID-19.
First, emotional threat is a psychological disorder characterised by uncontrollable and irrational fears, extreme hostility, or persistent anxiety. It identifies the illness consequences and concern that affect individuals’ emotions and create anxiety and depression, making them angry, scared, and exhausted [41,44,45]. However, it is not the amount of emotions but rather the interpretation of emotional states that is essential for determining an individual’s degree of psychological disorder [46]. They confirmed a relationship between the level of distress intolerance, anxiety, and bulimic behaviour in a non-clinical setting [46]. Second, cognitive threat refers to the identification of an illness threat from a particular disease, understanding its expected effects, and lacking personal control over the situation [44]. It may also contribute to the creation of anxiety disorders and psychological distress, which ultimately leads to behavioural change [41,43,47].
Fear of illness is inextricably linked with depression and anxiety [48]. Per Chinese scholars, a parallel epidemic of depression, anxiety, and emotional exhaustion is triggered by the COVID-19 pandemic [4,49]. In addition, recent studies posited that the pandemic had provoked widespread psychological issues, such as fear, anxiety, and depression, among countries with a high prevalence of viral infections [50,51]. Similarly, we assumed that perceived emotional and cognitive threat concerning COVID-19 would create anxiety, depression, and emotional exhaustion among the paramedics treating patients with COVID-19, which would ultimately lead to their agonistic behaviour (i.e., outcome). Thus, we hypothesised the following:
H1a:
Perceived emotional threat will be positively related to physiological anxiety.
H1b:
Perceived emotional threat will be positively related to depression.
H1c:
Perceived emotional threat will be positively related to emotional exhaustion.
H2a:
Perceived cognitive threat will be positively related to physiological anxiety.
H2b:
Perceived cognitive threat will be positively related to depression.
H2c:
Perceived cognitive threat will be positively related to emotional exhaustion.
3.2. Physiological Anxiety
Anxiety disorders are often caused by stressful life events [13]. Anxiety is defined as “an emotion characterized by feelings of tension, worried thoughts and physical changes like increased blood pressure” [52]. Anxiety is also the cause and effect of many psychosomatic diseases and plays a role in the development of emotional psychosis [16]. Prior literature described the possible role of stress and fear of sickness in the causation of submissive behaviour owing to anxiety [11,53,54]. How long the novel coronavirus will persist and how it will continue to influence the psychological well-being of healthcare staff is unknown. This psychological influence may lead to adverse behavioural change [55]. Thus, we posited that physiological anxiety will increase extensively if the pandemic persists, which ultimately will increase frontline paramedics’ agonistic behaviour. Thus, we also proposed the following hypothesis:
H3:
Physiological anxiety will be positively related to agonistic behaviour.
3.3. Depression
Depression refers to a ‘psychological state of low mood and aversion to activity that can affect a person’s thoughts, behaviour, motivation, feelings, and sense of well-being’ [56]. The maladaptive actions in behavioural theories have underlined the occurrence of depression. Cognitive behavioural therapy assumes that the root cause of depression is negative thinking patterns, which then lead to negative behavioural patterns [57]. People with depression have extremely negative views about themselves and the world. It is believed that long-lasting emotional stress is the pathogenic factor leading to the development of individual depression that leads to behavioural disorders [16,58]. Generally, during the early stages of a pandemic, people have little information about treatment and mortality, which exacerbates people’s fear of infection, leading toward behavioural consequences [59]. Consistently, depression rates are higher during the COVID-19 pandemic as compared to before [6]. Like anxiety, we posited that depression would increase the agonistic behaviours of frontline paramedics:
H4:
Depression will be positively related to agonistic behaviour.
3.4. Emotional Exhaustion
Emotional exhaustion is a stress-related social issue that may affect individuals’ working behaviour [60]. It describes ‘feelings of being emotionally overextended’ [61]. Consequences of emotional exhaustion can lead to behavioural disorders, a preference for remaining at home, and poor work performance [61,62]. Some studies have investigated the causes or consequences of employees’ emotional exhaustion in work-related environments [31,62,63,64,65]. Moreover, one study [63] concluded that greater levels of perceived pandemic threat could be used to anticipate increased levels of emotional exhaustion, leading to increased agonistic behaviour. Given that the increased threat of the COVID-19 pandemic predicts increased emotional exhaustion, it is reasonable to suggest that increased emotional exhaustion will contribute to exacerbated agonistic behaviour among frontline paramedics treating patients with COVID-19. Like anxiety and depression, we hypothesised the following:
H5:
Emotional exhaustion will be positively related to agonistic behaviour.
3.5. The Moderating Role of Perceived Social Support
Social support is defined as “social interactions or relationships that provide practical assistance to individuals or embedding individuals into a social system that is considered to provide love, care, or attachment to a valuable social group” [24]. Simply, social support refers to all kinds of support that individuals obtain from others. Social support is divided into actually received support and perceived support. Although the received social support includes the assistance already provided, PSS is a faith that these assisting behaviours will occur when needed in the future [66]. Increased social support is coupled with better psychological outcomes, and PSS (rather than actual social support) seems to indicate healthier psychological behaviours during times of stress [26]. Moreover, PSS was identified in the SARS outbreak and organisational behaviour literature as adversely associated with burnout [67]. Therefore, PSS was selected as the focus of this research.
Various aspects of sociocultural background influence the degree and speed of behavioural change. Social norms influence employees’ behaviours, what they think about others’ actions, and what they agree or disagree with at the workplace [68]. In addition, many studies have confirmed the relationship between decreased adolescent social support and increased aggression [69,70,71,72,73]. Moreover, greater levels of perceived pandemic threat predict resulted in increased levels of psychological strain, whereas greater social support predicts a decreased effect of psychological strain on behaviour disorders [63]. Increased PSS also protects individuals with high levels of victimisation from increased health disorders such as depression, anxiety, emotional exhaustion [19,69]. The moderating role of PSS using the stress-buffering model was also a significant contributor to depressive symptoms among Chinese nurses [20]. Nonetheless, few studies have explored the impact of PSS on the relationship between COVID-19-related stress and psychological well-being [74,75].
Consequently, we posited that PSS would buffer or moderate the relationship between strain (physiological anxiety, depression, emotional exhaustion) and outcome (agonistic behaviour). Specifically, we hypothesised the following:
H6a:
PSS will moderate the positive association between physiological anxiety and agonistic behaviour; i.e., a rise in PSS will decrease the relationship strength between physiological anxiety and agonistic behaviour.
H6b:
PSS will moderate the positive association between depression and agonistic behaviour; i.e., a rise in PSS will decrease the relationship strength between depression and agonistic behaviour.
H6c:
PSS will moderate the positive association between emotional exhaustion and agonistic behaviour; i.e., a rise in PSS will decrease the relationship strength between emotional exhaustion and agonistic behaviour.
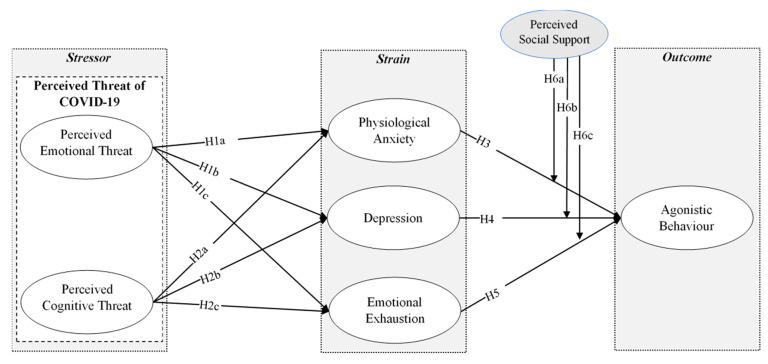
The proposed model of this study is shown in Figure 1.
Figure 1.
Proposed research model.
4. Material and Method
4.1. Context Selection
The threat of COVID-19 initially started after the first case was reported in China. Regardless of common health issues, developing countries are still in the initial phases of tackling this uncertain situation. The COVID-19 pandemic was first verified to have arrived in Pakistan in February 2020 [76] and grew to 69,496 confirmed cases by 31 May 2020 [77]. Paramedics, working in isolation wards, fever clinics, intensive care units and other related departments with an increased workload and risk of infection. In this study, the targeted population encompassed paramedics treating patients with COVID-19 in Pakistan who completed a survey.
4.2. Construct Operationalisation
We adapted the survey items (See Appendix A) for all constructs from prior literature and refined them to fit the context of this research before final data collection. However, in the preliminary analysis, an item from PSS (item number 6) was excluded owing to low factor loadings and to authenticate the results [78]. Moreover, to confirm the content validity of the proposed survey, a team composed of one professor and four scholars were requested to verify the wording and face validity of the survey questionnaire. The approved questionnaire was then distributed for data collection.
4.2.1. Perceived Threat of COVID-19
In this study, the Brief Illness Perception Questionnaire (BIPQ) was adapted [41] to measure the perceived threat of COVID-19 (0 to 10 scale) among frontline paramedics treating patients during the current pandemic. The initial eight-item questionnaire was divided into two categories as per prior directions [43]: perceived emotional threat and perceived cognitive threat. A sample item for the perceived emotional threat was, “How much does your threat of illness from COVID-19 affect you emotionally”? A sample item for the perceived cognitive threat was, “How well do you feel you understand COVID-19”?
4.2.2. Physiological Anxiety (PA)
Physiological anxiety was measured using 11 items (7-point Likert scale) [36], which were obtained from an earlier measure [53]. A sample item was “I cannot concentrate on a task or job without irrelevant thoughts intruding”.
4.2.3. Depression (DP)
Depression was measured using 19 items (7-point Likert scale) adapted from an earlier study [79]. A sample item was, “How often was this happen during the past 10 days; you were bothered by things that usually do not bother you?
4.2.4. Emotional Exhaustion (EE)
Emotional exhaustion was measured using 12 items (7-point Likert scale) adapted from an earlier study [31], which were obtained from an earlier measure [80]. A sample item was, “It is hard for me to relax after dealing with COVID-19 patients”.
4.2.5. Perceived Social Support (PSS)
Perceived social support was assessed using 8-items (7-point Likert scale) adapted from an earlier study [81]. A sample item was, “How much do you feel that your family pays extra attention to you during a current pandemic”?
4.2.6. Agonistic Behaviour (AB)
An aggression scale was adapted from an earlier study [22] as an objective gauge to assess individuals’ agonistic behaviour. We critically analysed several aggression scales; however, we found Regoeczi’s aggression scale to be the most relevant to our definition of agonistic behaviour. A 5-items scale (7-point Likert) was administered to participants. A sample item was, “How often did you feel you were too aggressive toward other people during the past 10 days”?
4.3. Data Collection, Sampling, and Analysis Procedure
Consistent with the focus of this study, data were gathered through a structured questionnaire only from paramedical personnel treating patients with COVID-19 in Pakistan. In the Punjab province of Pakistan, there are two separate layers of professionals that support core medical personnel in their healthcare services, namely “paramedics” and “allied health professionals”. Paramedics are registered with Punjab Medical Faculty (PMF), and Allied Health Professionals are registered with the Higher Education Commission (HEC) [82]. In this study, we have collected the data only from the frontline paramedics working in Punjab, Pakistan particularly dealing with COVID-19 patients. For this, we contacted the head of several quarantine centres and hospitals treating patients with COVID-19 around Punjab province, Pakistan. They were informed of the study purpose. All possible questions were answered to their satisfaction, but no official data were collected to assure the privacy of the respondents and the organisations. After getting verbal permission from the concerned authority, we started our data collection process.
Data collection followed the computer-assisted web interview method—a data-gathering technique in which participants complete questionnaires through an online survey link without the guidance of the interviewer [83]. The expected circulation of the survey was around 1500 using snowball sampling. A total of 372 responses were recorded between 3 March 2020 and 17 May 2020. Twenty-seven responses were omitted from final analyses because they were deemed unreliable [84]. Moreover, the same size exceeding 200 meant it was reasonable to employ structural equation modelling (SEM) [85]. Considering the length of the survey (66 questions), utilising SEM analyses was rational. Moreover, we evaluated the sample adequacy on the advice of [86], based on Cohen’s power theory. A post-hoc was applied for all exogenous indicators (significance level was set at 0.05, the effect size was 0.15, and the sample size was 345) to verify the statistical intensity of the study sample using G*power 3.1.9 (Heinrich-Heine-Universität, Düsseldorf, Germany) [87]. The results of the post-hoc test revealed that the statistical power was 0.9, much higher than the 0.8 thresholds [88]. Therefore, the final sample of 345 respondents was analysed by implementing the partial least square SEM technique in Smart-PLS v3.2.9 (Smart-PLS GmbH, Bönningstedt, Germany). For our purposes, this was more suitable than covariance-based SEM [89,90].
5. Results
5.1. Participants’ Demographics
Table 1 outlines participants’ characteristics (e.g., sex, age, and work experience): 38.6% were men, and 61.4% were women; 18.3% were aged ≤ 29 years old, 39.4% were aged 30 to 39 years, 40.6% were aged 40 to 49 years, and 1.7% were aged ≥ 50 years; and 20.9% had one to three years of work experience, 25.2% had four to six years of work experience, 26.1% had seven to nine years of work experience, and 27.8% had ≥ 10 years of work experience.
Table 1.
Participants profile.
| Category | Frequency | % Age | |
|---|---|---|---|
| Sex | Men | 133 | 38.6 |
| Women | 212 | 61.4 | |
| Total | 345 | 100.0 | |
| Age | 20 to 29 years | 63 | 18.3 |
| 30 to 39 years | 136 | 39.4 | |
| 40 to 49 years | 140 | 40.6 | |
| Over 50 years | 06 | 1.7 | |
| Total | 345 | 100.0 | |
| Work experience | 1 to 3 years | 72 | 20.9 |
| 4 to 6 years | 87 | 25.2 | |
| 7 to 9 years | 90 | 26.1 | |
| Above 10 years | 96 | 27.8 | |
| Total | 345 | 100.0 | |
5.2. The Empirical Results of the Measurement Model
5.2.1. Reliability and Convergent Validity
Convergence validity indicates the correlation level of several indexes in a parallel structure [78]. To verify the convergent validity of each item, Smart-PLS v3.2.9 software was used to conduct a confirmatory factor analysis. Table 2 shows the reliability and convergent validity of this study. In addition, Cronbach’s alpha of all factors ranged from 0.934 to 0.974, which was higher than the threshold value. Concerning convergent validity, this study examined the similarity between operationalisation and theory. The composite reliability (CR) was 0.947 to 0.976, and the average variance extracted (AVE) was 0.684 to 0.861.
Table 2.
Reliability and convergent validity.
| Constructs | Cronbach’s Alpha | rho_A | CR | AVE |
|---|---|---|---|---|
| AB | 0.945 | 0.946 | 0.958 | 0.819 |
| DP | 0.974 | 0.975 | 0.976 | 0.684 |
| EE | 0.961 | 0.962 | 0.966 | 0.703 |
| PA | 0.967 | 0.968 | 0.970 | 0.749 |
| PCT | 0.946 | 0.947 | 0.961 | 0.861 |
| PET | 0.936 | 0.939 | 0.955 | 0.840 |
| PSS | 0.934 | 0.935 | 0.947 | 0.718 |
AB = agonistic behaviour; DP = depression; EE = emotional exhaustion; PA = physiological anxiety; PCT = perceived cognitive threat; PET = perceived emotional threat; PSS = perceived social support. CR = composite reliability; AVE = average variance extracted.
The suggested values for Cronbach’s alpha and CR should be greater than 0.7, and AVE should be greater than 0.5; thus, the instrument was efficient and reliable [78,91] and the data could be used for further structural analysis.
5.2.2. Discriminant Validity
To distinguish the extent of empirical variance among the constructs, discriminant validity evaluation has become a widely accepted assumption to analyse the relationship between potential factors [89]. In this study, we used three methods to evaluate discriminant validity. First, by associating the correlation of the factors with the square root of the AVE. Second, the survey items were checked through the cross-loading criterion to recognise the relevance. Third, discriminant validity was measured by the application of Heterotrait-Monotrait Ration (HTMT) [89,92,93].
As described in Table 3, the correlation between constructs and the square root of AVE was linked to quantify the discriminant validity of the instrument. The diagonal values in Table 3 suggest that the square root of AVE is higher than the correlation coefficients between all variables, a good indication of discriminant validity [93].
Table 3.
Fornell-Larcker criterion.
| Constructs | AB | DP | EE | PA | PCT | PET | PSS |
|---|---|---|---|---|---|---|---|
| AB | 0.905 | ||||||
| DP | 0.531 | 0.827 | |||||
| EE | 0.539 | 0.639 | 0.838 | ||||
| PA | 0.513 | 0.611 | 0.560 | 0.866 | |||
| PCT | 0.333 | 0.364 | 0.384 | 0.382 | 0.928 | ||
| PET | 0.364 | 0.368 | 0.393 | 0.404 | 0.705 | 0.917 | |
| PSS | −0.254 | −0.178 | −0.275 | −0.104 | 0.014 | −0.032 | 0.847 |
Note: Pearson correlations are shown below the diagonals. p < 0.05. AB = agonistic behaviour; DP = depression; EE = emotional exhaustion; PA = physiological anxiety; PCT = perceived cognitive threat; PET = perceived emotional threat; PSS = perceived social support.
Prior studies suggested cross-loadings criteria to assess discriminant validity [91,94]. Accordingly, the loading of each item should be higher than its subsequent construct, and the item loadings are also regarded as a threshold. The calculation results of item loadings and cross-loadings (see Table 4) show that the loadings of each item are higher than the cross-loadings of other subsequent construct items. This shows that it has sufficient discriminant validity by satisfying the cross-loading criteria.
Table 4.
Cross-loadings criterion.
| Items | AB | DP | EE | PA | PCT | PET | PSS |
|---|---|---|---|---|---|---|---|
| AB1 | 0.899 | 0.480 | 0.458 | 0.464 | 0.293 | 0.312 | −0.215 |
| AB2 | 0.921 | 0.491 | 0.561 | 0.473 | 0.329 | 0.331 | −0.245 |
| AB3 | 0.926 | 0.476 | 0.532 | 0.474 | 0.297 | 0.321 | −0.233 |
| AB4 | 0.914 | 0.476 | 0.453 | 0.459 | 0.307 | 0.355 | −0.230 |
| AB5 | 0.863 | 0.480 | 0.424 | 0.450 | 0.276 | 0.330 | −0.222 |
| DP1 | 0.409 | 0.775 | 0.453 | 0.544 | 0.260 | 0.268 | −0.090 |
| DP2 | 0.444 | 0.857 | 0.508 | 0.556 | 0.268 | 0.293 | −0.110 |
| DP3 | 0.435 | 0.843 | 0.535 | 0.514 | 0.266 | 0.252 | −0.149 |
| DP4 | 0.464 | 0.862 | 0.503 | 0.543 | 0.326 | 0.328 | −0.114 |
| DP5 | 0.486 | 0.843 | 0.551 | 0.552 | 0.338 | 0.326 | −0.180 |
| DP6 | 0.454 | 0.858 | 0.506 | 0.544 | 0.337 | 0.350 | −0.143 |
| DP7 | 0.438 | 0.825 | 0.506 | 0.527 | 0.261 | 0.275 | −0.147 |
| DP8 | 0.460 | 0.816 | 0.498 | 0.523 | 0.322 | 0.316 | −0.140 |
| DP9 | 0.473 | 0.845 | 0.557 | 0.504 | 0.352 | 0.360 | −0.184 |
| DP10 | 0.482 | 0.776 | 0.540 | 0.459 | 0.317 | 0.305 | −0.211 |
| DP11 | 0.469 | 0.804 | 0.579 | 0.467 | 0.294 | 0.328 | −0.137 |
| DP12 | 0.416 | 0.837 | 0.559 | 0.478 | 0.332 | 0.315 | −0.137 |
| DP13 | 0.410 | 0.855 | 0.536 | 0.511 | 0.290 | 0.256 | −0.115 |
| DP14 | 0.369 | 0.786 | 0.499 | 0.426 | 0.239 | 0.233 | −0.071 |
| DP15 | 0.434 | 0.814 | 0.548 | 0.465 | 0.263 | 0.287 | −0.172 |
| DP16 | 0.410 | 0.846 | 0.549 | 0.483 | 0.336 | 0.334 | −0.178 |
| DP17 | 0.415 | 0.857 | 0.526 | 0.510 | 0.293 | 0.315 | −0.170 |
| DP18 | 0.436 | 0.818 | 0.562 | 0.476 | 0.335 | 0.342 | −0.165 |
| DP19 | 0.408 | 0.790 | 0.519 | 0.504 | 0.259 | 0.256 | −0.154 |
| EE1 | 0.432 | 0.615 | 0.786 | 0.469 | 0.281 | 0.310 | −0.269 |
| EE2 | 0.447 | 0.572 | 0.791 | 0.486 | 0.258 | 0.305 | −0.287 |
| EE3 | 0.422 | 0.555 | 0.842 | 0.468 | 0.306 | 0.309 | −0.250 |
| EE4 | 0.450 | 0.521 | 0.861 | 0.484 | 0.307 | 0.306 | −0.254 |
| EE5 | 0.429 | 0.557 | 0.854 | 0.477 | 0.354 | 0.319 | −0.213 |
| EE6 | 0.498 | 0.583 | 0.870 | 0.474 | 0.356 | 0.362 | −0.275 |
| EE7 | 0.451 | 0.566 | 0.882 | 0.464 | 0.348 | 0.353 | −0.243 |
| EE8 | 0.420 | 0.498 | 0.831 | 0.405 | 0.334 | 0.334 | −0.182 |
| EE9 | 0.471 | 0.558 | 0.902 | 0.452 | 0.338 | 0.362 | −0.273 |
| EE10 | 0.461 | 0.511 | 0.833 | 0.500 | 0.346 | 0.385 | −0.218 |
| EE11 | 0.484 | 0.456 | 0.816 | 0.508 | 0.310 | 0.307 | −0.148 |
| EE12 | 0.450 | 0.444 | 0.785 | 0.442 | 0.309 | 0.286 | −0.158 |
| PA1 | 0.425 | 0.510 | 0.507 | 0.836 | 0.362 | 0.348 | −0.126 |
| PA2 | 0.413 | 0.537 | 0.500 | 0.847 | 0.343 | 0.332 | −0.082 |
| PA3 | 0.423 | 0.497 | 0.448 | 0.862 | 0.322 | 0.366 | −0.079 |
| PA4 | 0.487 | 0.571 | 0.493 | 0.881 | 0.347 | 0.369 | −0.111 |
| PA5 | 0.497 | 0.544 | 0.484 | 0.886 | 0.367 | 0.379 | −0.122 |
| PA6 | 0.420 | 0.503 | 0.497 | 0.880 | 0.356 | 0.387 | −0.064 |
| PA7 | 0.443 | 0.575 | 0.485 | 0.887 | 0.362 | 0.361 | −0.030 |
| PA8 | 0.456 | 0.510 | 0.483 | 0.885 | 0.326 | 0.350 | −0.048 |
| PA9 | 0.436 | 0.534 | 0.496 | 0.842 | 0.296 | 0.336 | −0.111 |
| PA10 | 0.456 | 0.518 | 0.479 | 0.866 | 0.278 | 0.318 | −0.070 |
| PA11 | 0.418 | 0.513 | 0.458 | 0.850 | 0.271 | 0.290 | −0.147 |
| PCT1 | 0.320 | 0.361 | 0.334 | 0.359 | 0.935 | 0.664 | 0.025 |
| PCT2 | 0.306 | 0.314 | 0.355 | 0.327 | 0.928 | 0.690 | −0.005 |
| PCT3 | 0.322 | 0.320 | 0.368 | 0.357 | 0.923 | 0.601 | −0.013 |
| PCT4 | 0.287 | 0.356 | 0.366 | 0.374 | 0.927 | 0.663 | 0.043 |
| PET1 | 0.337 | 0.324 | 0.356 | 0.350 | 0.632 | 0.931 | −0.043 |
| PET2 | 0.365 | 0.361 | 0.361 | 0.373 | 0.644 | 0.939 | −0.062 |
| PET3 | 0.313 | 0.348 | 0.388 | 0.391 | 0.631 | 0.932 | −0.057 |
| PET4 | 0.320 | 0.314 | 0.333 | 0.365 | 0.681 | 0.861 | 0.051 |
| PSS1 | −0.206 | −0.130 | −0.245 | −0.097 | −0.003 | −0.026 | 0.909 |
| PSS2 | −0.222 | −0.109 | −0.237 | −0.086 | −0.032 | −0.083 | 0.755 |
| PSS3 | −0.207 | −0.191 | −0.255 | −0.090 | 0.015 | −0.009 | 0.860 |
| PSS4 | −0.211 | −0.176 | −0.244 | −0.082 | 0.006 | −0.041 | 0.853 |
| PSS5 | −0.194 | −0.128 | −0.197 | −0.081 | 0.039 | −0.019 | 0.839 |
| PSS7 | −0.219 | −0.157 | −0.232 | −0.103 | 0.064 | 0.005 | 0.856 |
| PSS8 | −0.237 | −0.161 | −0.220 | −0.073 | −0.003 | −0.016 | 0.852 |
AB = agonistic behaviour; DP = depression; EE = emotional exhaustion; PA = physiological anxiety; PCT = perceived cognitive threat; PET = perceived emotional threat; PSS = perceived social support.
Finally, the HTMT ratio criterion was established to illustrate the insensitivity of Fornell and Larcker’s criterion and cross-loading criterion. The ratio of HTMT was close to 1, indicating the lack of discriminant validity [91]. HTMT is an estimate of factor correlation (or instead, the upper bound). To make a clear distinction between the two factors, HTMT should be less than 1 [92,95]. Therefore, we employed the HTMT ratio; the value in Table 5 shows that the highest value is 0.75, which is lower than the above threshold, indicating sufficient discriminant validity.
Table 5.
HTMT ratio criterion.
| Constructs | AB | DP | EE | PA | PCT | PET | PSS |
|---|---|---|---|---|---|---|---|
| AB | |||||||
| DP | 0.552 | ||||||
| EE | 0.563 | 0.661 | |||||
| PA | 0.536 | 0.628 | 0.581 | ||||
| PCT | 0.351 | 0.376 | 0.401 | 0.398 | |||
| PET | 0.388 | 0.382 | 0.413 | 0.423 | 0.751 | ||
| PSS | 0.269 | 0.184 | 0.290 | 0.109 | 0.041 | 0.065 |
AB = agonistic behaviour; DP = depression; EE = emotional exhaustion; PA = physiological anxiety; PCT = perceived cognitive threat; PET = perceived emotional threat; PSS = perceived social support.
5.3. The Empirical Results of the Structural Model
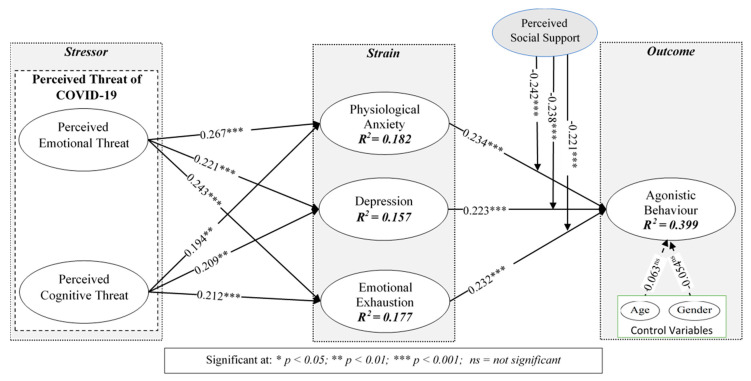
After examining reliability and validity, we measured the causal relationship between the factors with Smart-PLS v3.2.9 software [89,95]. Figure 2 shows the value of the path coefficient. The bootstrap technique was used to measure the significance of the structural model (2000 iterations of resampling). The expressive power of the research model is represented by the illustrative variation of its results (i.e., R2). The R2 (R-Square) value of AB was 0.399, indicating that these selected variables represented 39.9% of the variation. Moreover, the R2 of physiological anxiety was 0.182, indicating that the mutation rate owing to perceived emotional threat (PET) and perceived cognitive threat (PCT) was 18.2%. In addition, the R2 of depression was 0.157 and the R2 of emotional exhaustion was 0.177, indicating the active participation of perceived threat.
Figure 2.
SEM results for hypotheses testing.
The SEM results in Figure 2 show that all exogenous factors are positively associated with endogenous factors. The p-value confirms the level of significance of the relationship between the proposed relations per the criterion [96,97]. Meanwhile, the value of Standardized Root Mean Square Residual (SRMR) is 0.042, and the value of Normed Fit Index (NFI) is 0.891, showing the good fitness of the model. In Figure 2, the SEM analysis results verify the path analysis coefficient between PET and physiological anxiety is (β = 0.267, p < 0.001). PET had a significant positive effect on physiological anxiety, and the beta correlation coefficient between PET and depression was significant (β = 0.221, p < 0.001). The findings further indicated that PET and emotional exhaustion were significantly positively correlated (β = 0.243, p < 0.001). Based on these statistical findings, H1a, H1b, and H1c were supported.
The beta coefficient of PCT was significant (β = 0.194, p < 0.01), implying that it positively impacted physiological anxiety; therefore, H2a was supported. PCT was positively correlated with depression and emotional exhaustion. PCT and depression were also significantly positively correlated (β = 0.209, p < 0.01), as were PCT and emotional exhaustion (β = 0.212, p < 0.001). Therefore, H2b and H2c were supported.
Physiological anxiety also had a considerable effect on AB (Figure 2; β = 0.234, p < 0.001). The coefficient values of depression and AB (β = 0.223, p < 0.001) and emotional exhaustion and AB (β = 0.232, p < 0.001) indicated that the selected strain factors (physiological anxiety, depression, and emotional exhaustion) had a substantial positive effect on the AB. Therefore, H3, H4, and H5 are were supported.
5.4. The Moderating Role of Perceived Social Support
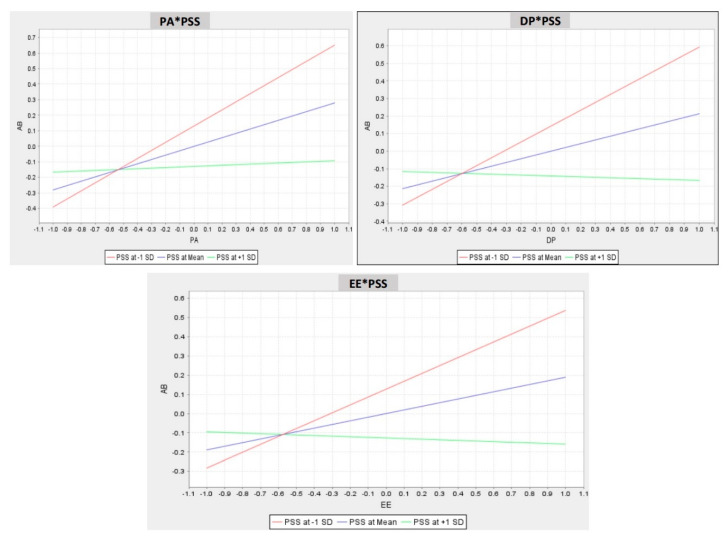
Figure 2 shows the interaction value of the beta coefficient of PSS on the association between physiological anxiety and AB (β = −0.242, p < 0.001), the coefficient value of PSS on the association between depression and AB is (β = −0.238, p < 0.001), and the coefficient value of PSS on the relationship between emotional exhaustion and AB (β = −0.221, p < 0.001). PSS significantly and negatively influenced the relationships between physiological anxiety, depression, and emotional exhaustion with AB (Figure 3). Consequently, H6a, H6b, and H6c were supported. Figure 3 also illustrates the moderating effect of PSS on the relationship between physiological anxiety, depression, and emotional exhaustion with AB. In sum, per the present analyses, the proposed theoretical model was acceptable.
Figure 3.
Moderating effect of PSS on the relationship of PA, DP, and EE with AB. DP = depression; EE = emotional exhaustion; PA = physiological anxiety; PSS = perceived social support.
5.5. Common Method Bias and Multicollinearity
The common method bias (CMB) possibly exposes the efficacy of this study. The survey notes informed participants that there were no right or wrong answers and that their replies would remain anonymous and confidential. Moreover, Harman’s single factor test is usually used to test for the existence of CMB [98,99]. We used SPSS v26 (IBM SPSS Inc., Chicago, IL, USA) software to perform Harman’s single factor test.
The first factor accounted for 40.9% of the variation. In social science literature, a value below 50% is the threshold of the CMB [98,100,101]. Concurrently, the inner variance inflation factor (VIF) was also used to evaluate the CMB problem. According to Kock (2015), inner-VIF should be less than 3.3. We discovered that the value varied between 1.09 to 2.01; thus, CMB was not a problem in this study.
The values of outer-VIF were used for multicollinearity assessment of the survey items. The literature shows that if the VIF value of a study is lower than 10, multicollinearity may not be a problem [102,103,104]. The highest value of VIF was 5.93; thus, there was no severe multicollinearity problem. In sum, the proposed model did not have CMB or multicollinearity problems, indicating that the structural model measured significant differences between the constructs.
6. Discussion
The global understanding of disease transmission and management has improved during the several pandemics in history. However, COVID-19 has limited global health authorities’ abilities. As previous studies disclosed, working directly with patients will increase individuals’ fear of getting sick and uncertainty about pandemic contagion [63,105], which we called perceived threat of COVID-19 in this study. Therefore, we investigated the impact of perceived COVID-19 threat in forecasting greater levels of physiological anxiety, depression, and emotional exhaustion among frontline paramedics, which may boost their agonistic behaviour. Another objective was to examine the moderating influence of PSS in reducing the adverse consequences of physiological anxiety, depression, and emotional exhaustion on agonistic behaviour owing to the perceived threat of COVID-19. The BIPQ [41] was used to measure the perceived threat of COVID-19, which was divided into two constructs: perceived emotional threat and perceived cognitive threat. SEM was applied to the data to test the research model under the podium of the SSO framework.
The results revealed that frontline paramedics in the isolation wards did not think that they were exempt from the peril, which was associated with increased psychological distress. Moreover, paramedics worried about the inadequacy of protective measures and vigilance taken by the health department. Paramedics’ perception of risk contributed to their psychological morbidity and irregular behaviour. Based on the empirical results, we postulated that an increased perceived threat of COVID-19 would increase the level of paramedics’ physiological anxiety and depression, which would ultimately increase their agonistic behaviour. A causal link between the perceived threat of COVID-19 and psychological distress was found. After working in isolation for a considerable period, paramedics reported emotional exhaustion. Treating patients with COVID-19 had become routine, and they were inured to being around death almost every day. However, they also experienced substantial stress owing to the fear of getting ill during the pandemic. The cognitive and emotional threat from COVID-19 was positively associated with increased emotional exhaustion at work, which was associated with paramedics’ behavioural change.
Moreover, the results showed that PSS reduced the effect of anxiety, depression, and emotional exhaustion on agonistic behaviour. PSS is helpful as friends or family members provide social support and express empathy. With the increase in the number of cases of COVID-19 infection around the globe, frontline paramedics are required to wear protective masks, protective clothing, and treat many patients with COVID-19, which may cause added stress. However, PSS can help reduce this stress by reducing the perception of the threat of stressful events and the physiological response and inappropriate behaviour that can result from stress. These results are also supported by prior studies [75,106]. Positive social feedback should thus be provided to frontline paramedics in times of uncertainty to offset potential agonistic behaviour.
7. Implications, Limitations, and Research Directions
7.1. Theoretical Implications
First, this research offers a more account of the theory of agonistic behaviour from the field of animal biological sciences to human behavioural science. The authors integrated the SSO model with the theory of agonistic behaviour to examine the effects of the perceived threat of COVID-19 on human agonistic behaviour. This empirical investigation elucidated human behaviour research. Second, by using the SSO model, this study tested several theoretical-based relationships between the perceived threat of COVID-19 and human agonistic behaviour. Most of the recent studies concerning COVID-19 discussed the consequences and adverse effect on patients’ health, daily life, economy, and education [4,55,107,108,109,110]; however, this study mainly concentrated on the perceived threat of COVID-19 among frontline paramedics, and how it influenced their psychological strain and increased their agonistic behaviour. Therefore, the authors hope that this model can be further extended and used as an ideal platform for future work in a similar context. Third, this study further divided the BIPQ into two major parts—emotional and cognitive threats—and empirically tested it during the current pandemic situation. This significantly contributes to validating the existing scales and can be used in future research.
7.2. Practical Implications
This study also provides some useful insights for practice. First, the findings significantly highlighted the risk of infection that frontline paramedics face, which may cause several mental health problems such as anxiety and depression. Health organisations should implement full security measures to protect this at-risk population to mitigate the threat of COVID-19. Second, the results emphasised the need for healthcare managers to understand the magnitude and sources of psychosocial stress faced by frontline paramedics. Providing adequate protection and facilities, communicating effectively, creating transparent guidelines, and implementing appropriate feedback mechanisms for healthcare personnel are essential to reduce the strain in the current pandemic situation. Third, this study highlights the significant role of PSS in reducing the effect of psychological strain on agonistic behaviour. Concerning stress management, it is also essential to strengthen social support in the workplace. For frontline paramedics with severe psychological strain, it is necessary to identify high-risk groups early, and provide counselling, social support, and stress management to mitigate negative behavioural change.
7.3. Limitations and Research Directions
Some limitations need to be addressed while discussing the outcomes of the current study. First, a cross-sectional design was employed, and the agonistic behaviour of paramedics was measured during the current pandemic. Future scholars should employ a multimethod or longitudinal design by comparing the results obtained during and after the COVID-19 pandemic. Second, this study did not examine sex and age differences. The level of threat may not be the same between female and male paramedics. Similarly, those in different age groups will respond to strain differently and may display agonistic behaviour in diverse ways. Therefore, multigroup analyses should examine any possible sex or age differences. Third, the strain factors discussed in this study are not limited to these particular factors; future researchers could extend the model using several other factors such as scepticism, sadism, and poor sleep quality, which may impact human agonistic behaviour. Organisational and government support can also be used as a moderating factor in addition to PSS. Finally, future researcher should continuously validate the scale used in the current study.
8. Conclusions
Our study concludes that the effect of perceived COVID-19 threat on predicting greater levels of physiological anxiety, depression, and emotional exhaustion among frontline healthcare paramedics may contribute to their agonistic behaviour. Moreover, we have concluded the moderating role of PSS in decreasing the adverse effect of physiological anxiety, depression, and emotional exhaustion on agonistic behaviour due to the perceived threat of COVID-19. Our study provides understanding about human agonistic behaviour will help to identify precise characteristics and probable mechanisms of human aggression and violence in several contexts, which will contribute to the implementation of conflict management practices in the workplace.
Acknowledgments
We acknowledge the anonymous reviewers and editor for their feedback and all paramedics who participated in this study.
Appendix A: Survey Items
Perceived Emotional Threat
“How much does COVID-19 affect your life?”
“How much do you feel symptoms COVID-19 contagion?”
“How concerned are you about COVID-19 contagion?”
“How much does your threat of illness from COVID-19 affect you emotionally? (e.g., does it make you angry, scared, upset or depressed)”
Perceived Cognitive Threat
“How long do you think COVID-19 will continue?”
“How much control do you feel over COVID-19 contagion?”
“How much do you think that current treatment is helpful from the recovery of COVID-19 contagion?”
“How well do you feel you understand COVID-19?”
Physiological Anxiety
“I picture some future misfortune.”
“I cannot get some thoughts out of my mind.”
“I abide on mistakes that I have made.”
“I think about possible misfortunes to my loved ones.”
“I cannot concentrate on a task or job without irrelevant thoughts intruding.”
“I keep trying to avoid uncomfortable thoughts.”
“I cannot get some pictures or images out of my mind.”
“I imagine myself appearing foolish with a person whose opinion of me is important.”
“I am concerned that others might not think well of me.”
“I have to be careful not to let my real feelings show.”
“I have an uneasy feeling.”
Depression
How often was this happen during the past 10 days:
“you were bothered by things that usually do not bother you?”
“you did not feel like eating, and your passion was poor?”
“you felt that you could not shake the blues, even with help from family and friends?”
“you felt that you were just as good as other people?”
“you had trouble keeping your mind on what you were doing?”
“you felt depressed?”
“you felt that you were too tired to do things?”
“you felt hopeful about the future?”
“you thought your life had been a failure?”
“you felt fearful?”
“you were happy?”
“you talked less than usual?”
“you felt lonely?”
“people were unfriendly to you?”
“you enjoyed life?”
“you felt sad?”
“you felt that people disliked you?”
“it was hard to get started doing things?”
“you felt life was not worth living?”
Emotional Exhaustion
“It is hard for me to relax after dealing with COVID-19 patients.”
“If others speak to me, I will sometimes give an errant reply.”
“I mostly feel annoyed while dealing with COVID-19 patients.”
“I sometimes act aggressively, although I do not want to do so. “
“I feel irritable after dealing with COVID-19 patients for hours.”
“I feel emotionally drained sometimes.”
“I feel used up at the end of my work.”
“I feel fatigued when I get up in the morning and being confronted with news of COVID-19 patients.”
“I feel burned out from dealing with COVID-19 patients. “
“I feel frustrated after work.”
“I fell, I am working with COVID-19 patients for too long.”
“Dealing with COVID-19 patients puts too much stress on me.”
Perceived Social Support
“How much do you feel that adults care about you?”
“How much do you feel that your employer care about you?”
“How much do you feel that your parents care about you?”
“How much do you feel that your friends care about you?”
“How much do you feel that people in your family understand you?”
“How much do you feel that you want to leave home?” (deleted)
“How much do you feel that you and your family have fun together during a current pandemic?”
“How much do you feel that your family pays extra attention to you during a current pandemic?”
Agonistic Behaviour
“How often did you feel, you were too aggressive toward other people during the past 10 days?”
“How often did you feel, you influence other people too much to get what you want during the past 10 days?”
“How often did you feel, not at all aggressive-aggressive during the past 10 days?”
“How often did you feel, you like people to be afraid of you during the past 10 days?”
“How often did you feel, you try to get into a position of authority during the past 10 days?”
Author Contributions
Conceptualization, F.S. and J.D.; methodology, I.K. and A.F.; software, F.S. and I.K.; formal analysis, F.S. and A.A; data curation, I.K., M.S., and M.U.W.; writing—original draft preparation, F.S.; writing—review and editing, A.F., M.S, A.A., and M.U.W.; supervision, J.D.; funding acquisition, J.D. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Special Funds of the National Social Science Fund of China [18VSJ038] and supported in part by the National Science Foundation of China under grant 71974081, 71704066, and 71971100.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Jiao W.Y., Wang L.N., Liu J., Fang S.F., Jiao F.Y., Pettoello-Mantovani M., Somekh E. Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J. Pediatr. 2020:8–11. doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adhanom Ghebreyesus T. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. [(accessed on 18 May 2020)]; Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 3.University J.H. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) [(accessed on 4 July 2020)]; Available online: https://coronavirus.jhu.edu/map.html.
- 4.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., et al. Factors Associated with Mental Health Outcomes among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li S., Wang Y., Xue J., Zhao N., Zhu T. The impact of covid-19 epidemic declaration on psychological consequences: A study on active weibo users. Int. J. Environ. Res. Public Health. 2020;17:1–9. doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu J., Xu Q.-H., Wang C.-M., Wang J. Psychological status of surgical staff during the COVID-19 outbreak. Psychiatry Res. 2020;288:1–3. doi: 10.1016/j.psychres.2020.112955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Remuzzi A., Remuzzi G. COVID-19 and Italy: What next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kang L., Li Y., Hu S., Chen M., Yang C., Yang B.X., Wang Y., Hu J., Lai J., Ma X., et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7:e14. doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liao Y.T., Hsieh M.H., Yang Y.H., Wang Y.C., Tsai C.S., Chen V.C.H., Gossop M. Association between depression and enterovirus infection. Medicine (United States) 2017;96:e5983. doi: 10.1097/MD.0000000000005983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fink G. Stress, Definitions, Mechanisms, and Effects Outlined: Lessons from Anxiety. Elsevier Inc.; Amsterdam, The Netherlands: 2016. [Google Scholar]
- 12.Satici B., Gocet-Tekin E., Deniz M.E., Satici S.A. Adaptation of the fear of COVID-19 scale: Its association with psychological distress and life satisfaction in Turkey. Int. J. Ment. Health Addict. 2020:1–9. doi: 10.1007/s11469-020-00294-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schneiderman N., Ironson G., Siegel S.D. Stress and health: Psychological, behavioral, and biological determinants. Annu. Rev. Clin. Psychol. 2005;1:607–628. doi: 10.1146/annurev.clinpsy.1.102803.144141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clark A.M. Koyukuk River Culture. Prentice-Hall; Englewood Cliffs, NJ, USA: 2018. Hostility and Aggression; pp. 181–204. [Google Scholar]
- 15.Tranel D., Damasio A.R. International Encyclopedia of the Social & Behavioral Sciences. Pergamon Press; Oxford, UK: 1999. Agonistic Behavior; pp. 1–4. [Google Scholar]
- 16.Kudryavtseva N.N. Agonistic behavior: A model, experimental studies, and perspectives. Neurosci. Behav. Physiol. 2000;30:293–305. doi: 10.1007/BF02471782. [DOI] [PubMed] [Google Scholar]
- 17.Sutrisna E., Teah M., Phau I. Agonistic Behaviour in Marketing: An Extended Abstract. In: Rossi P., editor. Academy of Marketing Science. Springer; Berlin, Germany: 2017. pp. 563–568. [Google Scholar]
- 18.Mukhtar S., Mahmood Z. Moderating Role of Perceived Social Support between Perceived Parenting Styles and Relational Aggression in Adolescents. J. Aggress. Maltreatment Trauma. 2018;27:831–845. doi: 10.1080/10926771.2018.1468842. [DOI] [Google Scholar]
- 19.Stanton S.C.E., Campbell L. Perceived Social Support Moderates the Link between Attachment Anxiety and Health Outcomes. PLoS ONE. 2014;9:e95358. doi: 10.1371/journal.pone.0095358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kwok S.Y.C.L., Yeung D.Y.L., Chung A. The moderating role of perceived social support on the relationship between physical functional impairment and depressive symptoms among Chinese nursing home elderly in Hong Kong. Sci. World J. 2011;11:1017–1026. doi: 10.1100/tsw.2011.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scott J.P., Fredericson E. The Causes of Fighting in Mice and Rats. Physiol. Zool. 1951;24:273–309. doi: 10.1086/physzool.24.4.30152137. [DOI] [Google Scholar]
- 22.Regoeczi W.C. The Impact of Density: The Importance of Nonlinearity and Selection on Flight and Fight Responses. Soc. Forces. 2002;81:505–530. doi: 10.1353/sof.2003.0018. [DOI] [Google Scholar]
- 23.Velarde A., Geers R. On Farm Monitoring of Pig Welfare. [(accessed on 12 March 2020)]; Available online: https://www.britannica.com/topic/agonism.
- 24.Dantzer R. Behavior: Overview. Elsevier Inc.; Amsterdam, The Netherlands: 2016. [Google Scholar]
- 25.Mobbs D., Hagan C.C., Dalgleish T., Silston B., Prévost C. The ecology of human fear: Survival optimization and the nervous system. Front. Neurosci. 2015;9:1–22. doi: 10.3389/fnins.2015.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bavel J.J.V., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M., Crockett M.J., Crum A.J., Douglas K.M., Druckman J.N., et al. Using social and behavioural science to support COVID-19 pandemic response. Nat. Hum. Behav. 2020;4:460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- 27.Cole S., Balcetis E., Dunning D. Affective Signals of Threat Increase Perceived Proximity. Psychol. Sci. 2013;24:34–40. doi: 10.1177/0956797612446953. [DOI] [PubMed] [Google Scholar]
- 28.Koeske G.F., Koeske R.D. A preliminary test of a stress-strain-outcome model for reconceptualizing the burnout phenomenon. J. Soc. Serv. Res. 1993;17:107–135. doi: 10.1300/J079v17n03_06. [DOI] [Google Scholar]
- 29.Podsakoff N.P., Lepine J.A., Lepine M.A. Differential challenge stressor-hindrance stressor relationships with job attitudes, turnover intentions, turnover, and withdrawal behavior: A meta-analysis. J. Appl. Psychol. 2007;92:438–454. doi: 10.1037/0021-9010.92.2.438. [DOI] [PubMed] [Google Scholar]
- 30.Ragu-Nathan T.S., Tarafdar M., Ragu-Nathan B.S., Tu Q. The consequences of technostress for end users in organizations: Conceptual development and validation. Inf. Syst. Res. 2008;19:417–433. doi: 10.1287/isre.1070.0165. [DOI] [Google Scholar]
- 31.Maier C., Laumer S., Eckhardt A., Weitzel T. When social networking turns to social overload: Explaining the stress, emotional exhaustion, and quitting behavior from social network sites’ users; Proceedings of the 20th European Conference on Information Systems; Barcelona, Spain. 11–13 June 2012. [Google Scholar]
- 32.Wang J., Okoli C.T.C., He H., Feng F., Li J., Zhuang L., Lin M. Factors associated with compassion satisfaction, burnout, and secondary traumatic stress among Chinese nurses in tertiary hospitals: A cross-sectional study. Int. J. Nurs. Stud. 2020;102:103472. doi: 10.1016/j.ijnurstu.2019.103472. [DOI] [PubMed] [Google Scholar]
- 33.De Vos J. The effect of COVID-19 and subsequent social distancing on travel behavior. Transp. Res. Interdiscip. Perspect. 2020;5:1–8. doi: 10.1016/j.trip.2020.100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Suleiman A., Bsisu I., Guzu H., Santarisi A., Alsatari M., Abbad A., Jaber A., Harb T., Abuhejleh A., Nadi N., et al. Preparedness of frontline doctors in Jordan healthcare facilities to COVID-19 outbreak. Int. J. Environ. Res. Public Health. 2020;17:1–13. doi: 10.3390/ijerph17093181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patnaik N.M. The Effects of COVID-19 and Its Psychological Impact on People, Agricultural Extension in South Asia. Academic Press; Cambridge, MA, USA: 2020. pp. 1–5. [Google Scholar]
- 36.Perrewé P.L., Zellars K.L., Ferris G.R., Rossi A.M., Kacmar C.J., Ralston D.A. Neutralizing job stressors: Political skill as an antidote to the dysfunctional consequences of role conflict. Acad. Manag. J. 2004;47:141–152. doi: 10.2307/20159566. [DOI] [Google Scholar]
- 37.Haddad M., Boyce P. In: Fast Facts: Depression. Abingdon, editor. Karger Medical and Scientific Publishers; Basel, Switzerland: 2017. [Google Scholar]
- 38.Witte K., Allen M. A meta-analysis of fear appeals: Implications for effective public health campaigns. Heal. Educ. Behav. 2000;27:591–615. doi: 10.1177/109019810002700506. [DOI] [PubMed] [Google Scholar]
- 39.Beck A.T., Epstein N., Brown G., Steer R.A. Anxiety Inventory (BAI) Behavioral Health. J. Consult. Clin. Psychol. 1988;56:893–897. doi: 10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- 40.Ahmed M.Z., Ahmed O., Aibao Z., Hanbin S., Siyu L., Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatr. 2020;51:102092. doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Broadbent E., Petrie K.J., Main J., Weinman J. The brief illness perception questionnaire. J. Psychosom. Res. 2006;60:631–637. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 42.Petrie K.J., Jago L.A., Devcich D.A. The role of illness perceptions in patients with medical conditions. Curr. Opin. Psychiatry. 2007;20:163–167. doi: 10.1097/YCO.0b013e328014a871. [DOI] [PubMed] [Google Scholar]
- 43.Karatas T., Şükrü Ö., Kutlutürkan S. Factor structure and psychometric properties of the brief illness perception questionnaire in Turkish cancer patients. Asia-Pacific J. Oncol. Nurs. 2017;4:77. doi: 10.4103/2347-5625.199080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weinman J., Petrie K.J., Moss-Morris R., Horne R. The illness perception questionnaire: A new method for assessing the cognitive representation of illness. Psychol. Health. 1996;11:431–445. doi: 10.1080/08870449608400270. [DOI] [Google Scholar]
- 45.Mandel D.R., Vartanian O. Bush v. Bin laden: Effect of state emotion on perceived threat is mediated by emotion towards the threat agent. Rev. Int. Psychol. Soc. 2010;23:5–23. [Google Scholar]
- 46.Ioannou K., Fox J.R.E. Perception of threat from emotions and its role in poor emotional expression within eating pathology. Clin. Psychol. Psychother. 2009;16:336–347. doi: 10.1002/cpp.632. [DOI] [PubMed] [Google Scholar]
- 47.Rawson H.E., Bloomer K., Kendall A. Stress, anxiety, depression, and physical illness in college students. J. Genet. Psychol. 1994;155:321–330. doi: 10.1080/00221325.1994.9914782. [DOI] [PubMed] [Google Scholar]
- 48.Arthur A.R. When stress is mental illness: A study of anxiety and depression in employees who use occupational stress counselling schemes. Stress Health. 2005;21:273–280. doi: 10.1002/smi.1069. [DOI] [Google Scholar]
- 49.Yao H., Chen J.H., Xu Y.F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7:e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sorokin M.Y., Kasyanov E.D., Rukavishnikov G.V., Makarevich O.V., Neznanov N.G., Lutova N.B., Mazo G.E. Structure of anxiety associated with the COVID-19 pandemic in the russian-speaking sample: Results from on-line survey. medRxiv. 2020 doi: 10.1101/2020.04.28.20074302. [DOI] [Google Scholar]
- 51.Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Corsini R.J. Encyclopedia of Psychology. Am. J. Psychol. 1985;98:312. doi: 10.2307/1422449. [DOI] [Google Scholar]
- 53.Lehrer P.M., Woolfolk R.L. Self-report assessment of anxiety: Somatic, cognitive, and behavioral modalities. Behav. Assess. 1982;4:167–177. [Google Scholar]
- 54.Misra R., McKena M. College Students’ Academic Stress and Its Relation To Their Anxiety, Time Management, and Leisure Satisfaction. Am. J. Health Stud. 2000;16:41–51. [Google Scholar]
- 55.De Oliveira Araújo F.J., de Lima L.S.A., Cidade P.I.M., Nobre C.B., Neto M.L.R. Impact of Sars-Cov-2 and Its Reverberation in Global Higher Education and Mental Health. Psychiatry Res. 2020;288:1–2. doi: 10.1016/j.psychres.2020.112977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.De Zwart P.L., Jeronimus B.F., De Jonge P. Empirical evidence for definitions of episode, remission, recovery, relapse and recurrence in depression: A systematic review. Epidemiol. Psychiatr. Sci. 2019;28:544–562. doi: 10.1017/S2045796018000227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Blatt S.J., Maroudas C. Convergences among psychoanalytic and cognitive-behavioral theories of depression. Psychoanal. Psychol. 1992;9:157–190. doi: 10.1037/h0079351. [DOI] [Google Scholar]
- 58.Horne J.A. Sleep loss and behaviour for the prefrontal cortex and psychiatric disorder. Br. J. Psychiatry. 1993;162:413–419. doi: 10.1192/bjp.162.3.413. [DOI] [PubMed] [Google Scholar]
- 59.Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wright T.A., Cropanzano R. Emotional exhaustion as a predictor of job performance and voluntary turnover. J. Appl. Psychol. 1998;83:486–493. doi: 10.1037/0021-9010.83.3.486. [DOI] [PubMed] [Google Scholar]
- 61.Cropanzano R., Rupp D.E., Byrne Z.S. The relationship of emotional exhaustion to work attitudes, job performance, and organizational citizenship behaviors. J. Appl. Psychol. 2003;88:160–169. doi: 10.1037/0021-9010.88.1.160. [DOI] [PubMed] [Google Scholar]
- 62.Seidler A., Thinschmidt M., Deckert S., Then F., Hegewald J., Nieuwenhuijsen K., Riedel-Heller S.G. The role of psychosocial working conditions on burnout and its core component emotional exhaustion—A systematic review. J. Occup. Med. Toxicol. 2014;9 doi: 10.1186/1745-6673-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fiksenbaum L., Marjanovic Z., Greenglass E.R., Coffey S. Emotional exhaustion and state anger in nurses who worked during the sars outbreak: The role of perceived threat and organizational support. Can. J. Community Ment. Heath. 2006;25:89–103. doi: 10.7870/cjcmh-2006-0015. [DOI] [Google Scholar]
- 64.Gopalan N., Culbertson S.S., Leiva P.I. Explaining emotional labor’s relationships with emotional exhaustion and life satisfaction: Moderating role of perceived autonomy. Univ. Psychol. 2013;12:347–356. doi: 10.11144/Javeriana.UPSY12-2.eelr. [DOI] [Google Scholar]
- 65.Xu S., Ouyang X., Shi X., Li Y., Chen D., Lai Y., Fan F. Emotional exhaustion and sleep-related worry as serial mediators between sleep disturbance and depressive symptoms in student nurses: A longitudinal analysis. J. Psychosom. Res. 2020;129:1–27. doi: 10.1016/j.jpsychores.2019.109870. [DOI] [PubMed] [Google Scholar]
- 66.Norris F.H., Kaniasty K. Received and Perceived Social Support in Times of Stress: A Test of the Social Support Deterioration Deterrence Model. J. Pers. Soc. Psychol. 1996;71:498–511. doi: 10.1037/0022-3514.71.3.498. [DOI] [PubMed] [Google Scholar]
- 67.Tam C.W.C., Pang E.P.F., Lam L.C.W., Chiu H.F.K. Severe acute respiratory syndrome (SARS) in Hongkong in 2003: Stress and psychological impact among frontline healthcare workers. Psychol. Med. 2004;34:1197–1204. doi: 10.1017/S0033291704002247. [DOI] [PubMed] [Google Scholar]
- 68.Cialdini R.B., Goldstein N.J. Social Influence: Compliance and Conformity. Annu. Rev. Psychol. 2004;55:591–621. doi: 10.1146/annurev.psych.55.090902.142015. [DOI] [PubMed] [Google Scholar]
- 69.Wolff J.C., Frazier E.A., Esposito-Smythers C., Becker S.J., Burke T.A., Cataldo A., Spirito A. Negative cognitive style and perceived social support mediate the relationship between aggression and NSSI in hospitalized adolescents. J. Adolesc. 2014;37:483–491. doi: 10.1016/j.adolescence.2014.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kashani J.H., Canfield L.A., Borduin C.M., Soltys S.M., Reid J.C. Perceived Family and Social Support: Impact on Children. J. Am. Acad. Child. Adolesc. Psychiatry. 1994;33:819–823. doi: 10.1097/00004583-199407000-00007. [DOI] [PubMed] [Google Scholar]
- 71.Kerr D.C.R., Preuss L.J., King C.A. Suicidal adolescents’ social support from family and peers: Gender-specific associations with psychopathology. J. Abnorm. Child. Psychol. 2006;34:103–114. doi: 10.1007/s10802-005-9005-8. [DOI] [PubMed] [Google Scholar]
- 72.Scarpa A., Haden S.C. Community Violence Victimization and Aggressive Behavior: The Moderating Effects of Coping and Social Support. Aggress. Behav. 2006;32:502–515. doi: 10.1002/ab.20151. [DOI] [Google Scholar]
- 73.Andrews J.L., Foulkes L., Blakemore S.-J. Peer influence in adolescence: Public-health implications for COVID-19. Trends Cogn. Sci. 2020;24:2–8. doi: 10.1016/j.tics.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jianjun J., Deng D., Tsingan T., Li L., Jiali J., Wang W., Limei L., Teng T. The Effect of COVID-19 Stress on Sexual Compulsivity Symptom: The Mediating Role of Perceived Social Support. Res. Sq. 2020:1–23. doi: 10.21203/rs.3.rs-17956/v1. [DOI] [Google Scholar]
- 75.Xiao H., Zhang Y., Kong D., Li S., Yang N. The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020;26:e923549. doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gul A. Pakistan Detects First Coronavirus Cases, Links to Iran Outbreak. [(accessed on 29 February 2020)]; Available online: https://www.voanews.com/science-health/coronavirus-outbreak/pakistan-detects-first-coronavirus-cases-links-iran-outbreak.
- 77.GOP See the Realtime Pakistan and Worldwide COVID-19 situation. [(accessed on 19 May 2020)]; Available online: http://covid.gov.pk/
- 78.Hair J.F., Jr., Sarstedt M., Hopkins L., Kuppelwieser V.G. Partial least squares structural equation modeling (PLS-SEM): An emerging tool in business research. Eur. Bus. Rev. 2014;26:106–121. doi: 10.1108/EBR-10-2013-0128. [DOI] [Google Scholar]
- 79.Meier A.M. Adolescent first sex and subsequent mental health. Am. J. Sociol. 2007;112:1811–1847. doi: 10.1086/512708. [DOI] [Google Scholar]
- 80.Maslach C., Jackson S.E. The measurement of experienced burnout. J. Organ. Behav. 1981;2:99–113. doi: 10.1002/job.4030020205. [DOI] [Google Scholar]
- 81.Harker K. Immigrant Generation, Assimilation, and Adolescent Psychological Well-Being. Soc. Forces. 2001;79:969–1004. doi: 10.1353/sof.2001.0010. [DOI] [Google Scholar]
- 82.PPHA Policy Round Table Series. [(accessed on 4 July 2020)]; Available online: http://www.ppha.punjab.gov.pk/news-and-highlights/allied-health-professionals-and-paramedics.html.
- 83.Ziemba E., Zelazny R., Papaj T., Jadamus-Hacura M. Factors influencing the success of E-government. J. Comput. Inf. Syst. 2016;56:156–167. doi: 10.1080/08874417.2016.1117378. [DOI] [Google Scholar]
- 84.Barger P., Behrend T., Sharek D., Sinar E. I-O and the Crowd: Frequently Asked Questions About Using Mechanical Turk for Research. Ind. Psychol. 2011;49:11–17. [Google Scholar]
- 85.Kline R.B. Principles and Practice of Structural Equation Modeling. Volume 156. The Guilford Press; New York, NY, USA: 2005. ISBN 1572306904, 1593850751, 9781572306905, 9781593850753. [Google Scholar]
- 86.Hair J.F., Thomas G.M.H., Ringle C., Sarstedt M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM) 2nd ed. Sage Publications; Thousand Oaks, CA, USA: 2017. [Google Scholar]
- 87.Faul F., Erdfelder E., Lang A.G., Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods. 2007;39:175–191. doi: 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- 88.Cohen J. Statistical Power Analysis for Behavioural Sciences. Lawrence Erlbaum associates; Mahwah, NJ, USA: 1988. [Google Scholar]
- 89.Hair J.F., Hult G.T.M., Ringle C.M., Sarstedt M. Partial Least Squares Structural Equation Modeling (PLS-SEM) Sage publications; Thousand Oaks, CA, USA: 2014. [Google Scholar]
- 90.Sarstedt M., Hair J.F., Cheah J.H., Becker J.M., Ringle C.M. How to specify, estimate, and validate higher-order constructs in PLS-SEM. Australas. Mark. J. 2019;27:197–211. doi: 10.1016/j.ausmj.2019.05.003. [DOI] [Google Scholar]
- 91.Fornell C., Larcker D.F. Structural equation models with unobservable variables and measurement error: Algebra and statistics. J. Mark. Res. 1981;18:382. doi: 10.1177/002224378101800313. [DOI] [Google Scholar]
- 92.Henseler J., Ringle C.M., Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Mark. Sci. 2014;43:115–135. doi: 10.1007/s11747-014-0403-8. [DOI] [Google Scholar]
- 93.Fornell C., Larcker D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981;18:39. doi: 10.1177/002224378101800104. [DOI] [Google Scholar]
- 94.Liu H., Chu H., Huang Q., Chen X. Enhancing the flow experience of consumers in China through interpersonal interaction in social commerce. Comput. Human Behav. 2016;58:306–314. doi: 10.1016/j.chb.2016.01.012. [DOI] [Google Scholar]
- 95.Henseler J., Hubona G., Ray P.A. Using PLS path modeling in new technology research: Updated guidelines. Ind. Manag. Data Syst. 2016;116:2–20. doi: 10.1108/IMDS-09-2015-0382. [DOI] [Google Scholar]
- 96.Streukens S., Leroi-Werelds S. Bootstrapping and PLS-SEM: A step-by-step guide to get more out of your bootstrap results. Eur. Manag. J. 2016;34:618–632. doi: 10.1016/j.emj.2016.06.003. [DOI] [Google Scholar]
- 97.Hair J.F.J., Sarstedt M., Ringle C.M., Gudergan S.P. Advanced Issues in Partial Least Squares Structural Equation Modeling. Sage publications; Thousand Oaks, CA, USA: 2017. ISBN 1483377385, 9781483377384. [Google Scholar]
- 98.Podsakoff P.M., MacKenzie S.B., Lee J.-Y., Podsakoff N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J. Appl. Psychol. 2003;88:879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- 99.Podsakoff P.M., MacKenzie S.B., Podsakoff N.P. Sources of method bias in social science research and recommendations on how to control it. Annu. Rev. Psychol. 2012;63:539–569. doi: 10.1146/annurev-psych-120710-100452. [DOI] [PubMed] [Google Scholar]
- 100.Gentry L., Calantone R. A Comparison of Three Models to Explain Shop-Bot Use on the Web. Psychol. Mark. 2002;19:945–956. doi: 10.1002/mar.10045. [DOI] [Google Scholar]
- 101.Kock N. Common method bias in PLS-SEM: A full collinearity assessment approach. Int. J. e-Collab. 2015;11:1–10. doi: 10.4018/ijec.2015100101. [DOI] [Google Scholar]
- 102.Mason C.H., Perreault W.D. Collinearity, Power, and Interpretation of Multiple Regression Analysis. J. Mark. Res. 1991;28:268. doi: 10.1177/002224379102800302. [DOI] [Google Scholar]
- 103.Shieh G. On the misconception of multicollinearity in detection of moderating effects: Multicollinearity is not always detrimental. Multivariate Behav. Res. 2010;45:483–507. doi: 10.1080/00273171.2010.483393. [DOI] [PubMed] [Google Scholar]
- 104.Hair J.F., Anderson R.E., Tatham R.L., Black W.C. Multivariate Data Analysis with Readings. 5th ed. Prentice hall; Upper Saddle River, NJ, USA: 1998. [Google Scholar]
- 105.Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004;10:1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yang N., Xiao H., Wang W., Li S., Yan H., Wang Y. Effects of doctors’ empathy abilities on the cellular immunity of patients with advanced prostate cancer treated by orchiectomy: The mediating role of patients’ stigma, self-efficacy, and anxiety. Patient Prefer. Adherence. 2018;12:1305–1314. doi: 10.2147/PPA.S166460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Guan M. A panel analysis on preventing and controlling efficiency of COVID-19 pandemic. Res. Sq. 2020 doi: 10.21203/rs.3.rs-26006/v1. [DOI] [Google Scholar]
- 108.Haleem A., Javaid M., Vaishya R. Effects of COVID-19 pandemic in daily life. Curr. Med. Res. Pract. 2020;10:78–79. doi: 10.1016/j.cmrp.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Erikson S. Pandemics show us what government is for. Nat. Hum. Behav. 2020;4:441–442. doi: 10.1038/s41562-020-0871-4. [DOI] [PubMed] [Google Scholar]
- 110.Laing T. The economic impact of the Coronavirus 2019 (Covid-2019): Implications for the mining industry. Extr. Ind. Soc. 2020:1–5. doi: 10.1016/j.exis.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]