Abstract
Background
Humeral shaft fractures are common but debate still occurs as to whether these are best managed operatively or non-operatively. We sought to undertake a systematic review and meta-analysis of randomised and non-randomised studies to clarify the optimal treatment.
Methods
We performed a search for all randomised and non-randomised comparative studies on humeral shaft fracture. We included only those with an operative and non-operative cohort in adult patients. We undertook a meta-analysis of the following outcome measures: nonunion, malunion, delayed union, iatrogenic nerve injury and infection. Non-operative management was with a functional brace.
Results
Non-operative management resulted in a significantly higher nonunion rate of 17.6% compared to 6.3% with fixation. Operative management had a significantly higher iatrogenic nerve injury rate of 3.4% and infection rate of 3.7%. All nonunions within the included studies went on to union after plate fixation. There was no significant difference in delayed union or patient reported outcome measures. There was a significantly increased risk of malunion with non-operative treatment however this did not correlate with the outcome.
Discussion
Our findings suggest that in the majority of cases, humeral shaft fractures can be managed with non-operative treatment, and any subsequent nonunion should be treated with plate fixation.
Keywords: humerus, surgery, fracture fixation, brace, fractures ununited, treatment outcome
Introduction
Humeral shaft fractures have an incidence of around 13 to 14 per 100,000 and like many injuries there is a bimodal incidence with a peak in early adulthood and later life.1,2 Debate still continues as to the best management of these injuries. Non-operative treatment of these injuries has been described by Sarmiento et al. with good results, however despite this there has been a progressive trend towards operative management of these injuries.3,4 A large variety of techniques are described in the literature including plate fixation through anterior, posterior or minimally invasive approaches, intramedullary (IM) fixation, both anterograde and retrograde, and external fixation. Although there is substantial literature presenting case series, and comparison of various operative techniques, there are few directly comparative studies of operative versus non-operative management. We felt it is this key decision which treating clinicians must take when managing these injuries and therefore sought to further address this.
The outcome of operative versus non-operative management of these fractures has not been investigated in the form of a systematic review, and we sought to address this question looking at both randomised and non-randomised studies. Due to the relative infrequency of these injuries there are no large comparative studies and we therefore sought to systematically examine the evidence available and construct a meta-analysis of results where possible.
Our objective was to assess the outcome and safety of humeral shaft fractures managed operatively, when compared with non-operative methods.
Methods
This systematic review was carried out in accordance with Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidance for systematic reviews of non-randomised trials. A protocol was registered on the international prospective register of systematic reviews (PROSPERO) prior to commencement of the study (CRD42017073161).
Eligibility criteria and study inclusion
We included all randomised prospective, non-randomised prospective and non-randomised retrospective studies directly comparing operative and non-operative management of humeral shaft fractures in adults. There were no limitations of study size, location or follow-up. Non-English language publications without full translation were excluded.
Search strategy and information sources
The following electronic databases were used: Pubmed, OVID medline and the Cochrane Register of Controlled Trials (CENTRAL). The full search terms used in Pubmed were as follows: (“humerus”[MeSH Terms] OR humeral[Title]) AND (Shaft[Title/Abstract] OR diaphysis[Title/Abstract]) AND (surgical[Title/Abstract] OR fixation[Title/Abstract] OR osteosynthesis[Title/Abstract] OR operative[Title/Abstract]) OR plate [Title/Abstract] OR intramedullary [Title/Abstract] AND (conservative[Title/Abstract] OR functional bracing[Title/Abstract] OR non-operative[Title/Abstract)]. In the case of published abstracts of protocols, authors were contacted for preliminary results. Review articles were cross referenced for further relevant references. A further online search using the Google search engine was performed to identify any omitted studies. The electronic search was performed over a period from 01 August 2017 until 01 September 2017.
Patient inclusion and exclusion criteria
Studies were only included if they recruited patients with the following: fractures of the humeral shaft, adult patients (over 16 years), direct comparison of surgical management to non-operative management. Any non-operative and operative techniques were considered and included plate fixation, intramedullary fixation and external fixation.
Any studies including chronic fractures, pathological fractures, those with intra-articular extension or established nonunions were excluded. Direct comparison of surgical techniques without a non-operative cohort was also excluded.
Selection process and data collection
Two authors (HS and LF) carried out the data search independently. Suitable abstracts were screened for eligibility. The remaining papers were then reviewed in full text articles independently for final selection.
A standardised data collection form was used to extract required data from each source. This included study type, population statistics, fixation and non-operative treatments used and outcome measures.
Outcome measures
The primary outcome measure was rate of union. Secondary outcome measures were delayed union, malunion, infection, iatrogenic nerve injury and patient reported outcome measures.
Quality assessment/risk of bias assessment
Individual studies were assessed independently by two assessors (HS and LF) using the Non-Randomised Studies – of Interventions (ROBINS-I) tool.5 Each study was assessed across the following domains: confounding, selection, departure for intended interventions, missing data, outcome measurement and selection of reported result. An overall judgement on risk of bias was then reached for each study. Any discrepancy between reviewers was resolved by discussion or judgement from the supervising authors. Randomised studies were assessed using the Cochrane Collaboration risk of bias tool over seven separate domains.6
Data analysis
Following a risk of bias analysis, the studies without critical risk of bias were deemed appropriate for meta-analysis. When this was undertaken they were assessed for statistical heterogeneity using both I2 and χ2 for inconsistency. In studies with appropriate homogeneity a fixed effects meta-analysis was undertaken. This was when I2 was < 20% and the χ2 statistic produced a p ≥ 0.10. The relative risk (RR) was calculated with a 95% confidence interval (CI). A p value of < 0.05 was deemed statistically significant. All analyses were undertaken using Revman (Review Manager Version 5.3 Edition, Copenhagen, 2014).
Results
The search criteria identified 372 records after the removal of duplicates (Figure 1). After screening, 22 were selected for full text review. Fourteen of these were removed leaving eight studies that met the eligibility criteria for qualitative and quantitative synthesis. Reasons for exclusion were non-comparative studies, English text unavailable, non-specified surgical treatments and a systematic review. One published protocol was identified which was subsequently published as a completed study during the study period and it was included.7
Figure 1.
PRISMA flow diagram.
Study characteristics and quality assessment
One study was a prospective randomised controlled trial (RCT).7 The remaining seven of the studies were retrospective cohort studies.8–14 The randomised study used computer generated randomisation and allocation concealment in envelopes. Assessors were blinded to the intervention using a concealing gown over the arm. The risk of bias in the non-randomised studies is shown in Table 1; the risk of bias in the RCT is shown in Table 2. Following assessment of risk of bias one study had to be excluded due to critical risk from confounding bias. This was due to a large discrepancy between injury mechanism between operative and non-operative groups. Gunshot wound was 17.5% in the non-operative group and 5.3% in the operative group and motor vehicle accident significantly greater in the operative group.8
Table 1.
ROBINS I risk of bias.
| Paper | Confounding | Selection bias | Classification of intervention | Deviation from intended intervention | Missing data | Outcome measurement bias | Selection of reported result bias | Overall |
|---|---|---|---|---|---|---|---|---|
| Denard et al.8 | Critical risk | Moderate risk | Moderate risk | Moderate risk | Moderate risk | Serious risk | Moderate risk | Critical risk |
| Firat et al.9 | Serious risk | Serious risk | Moderate risk | Serious risk | No information | Moderate risk | Moderate risk | Serious risk |
| Harkin and Large14 | Serious risk | Serious risk | Moderate risk | Serious risk | Serious risk | Moderate risk | Moderate risk | Serious risk |
| Jawa et al.10 | Serious risk | Serious risk | Moderate risk | Moderate risk | Moderate risk | Serious risk | Moderate risk | Serious risk |
| Mahabier et al.13 | Serious risk | Moderate risk | Moderate risk | No Information | No information | Serious risk | Moderate risk | Serious risk |
| Matsunaga et al.7 | Low risk | Low risk | Low risk | Moderate risk | Low risk | Moderate risk | Low risk | Moderate risk |
| Wallny et al.12 | Serious risk | Moderate risk | Moderate risk | Moderate risk | No information | Serious risk | Moderate risk | Serious risk |
| Westrick et al.11 | Serious risk | Serious risk | Moderate risk | Moderate risk | Serious risk | Moderate risk | Moderate risk | Serious risk |
Table 2.
RCT risk of bias assessment.
| Paper | Random sequence generation | Allocation concealment | Blinding of participants /personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Matsunaga et al.7 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk |
Synthesis of results
A total of 943 patients were included from seven studies. Totally 55.6% (n = 524) were managed with fixation, and the remaining with non-operative treatment (n = 419). Mean age for fixation was 41.6 years and 59% of participants were male. Patients with non-operative treatment had a mean age of 50.4 years, and 50% were male. Fixation methods included open reduction internal fixation (ORIF) with plate and screw fixation through anterior and posterior approaches, minimally invasive plate fixation, intramedullary fixation, external fixation and in one case cerclage wires. Non-operative treatment was with a functional brace, with or without a week or two weeks in a coaptation splint or Gilchrist bandage. Characteristics and a summary of included studies are shown in Table 3. A summary of results of outcome measure is shown in Table 4.
Table 3.
Characteristics of included studies.
| Paper | Study | N | Fixation/ Conservative | Surgery Gender (M/F) | Surgery mean age (years) | Fixation method | Conservative gender (M/F) | Conservative mean age (years) | Conservative treatment method | Outcomes |
|---|---|---|---|---|---|---|---|---|---|---|
| Firat et al. | Retrospective cohort study | 128 | 66/62 | 43/23 | N/A (38.5 combined) | Plate fixation or IM nail | 38/24 | N/A (38.5 combined) | Functional brace | Malunion PROMS Radiographic union Infection Nerve palsy |
| Harkin and Large | Retrospective cohort study | 126 (107)a | 27/80 (30/96 but 3/16 lost to follow up)a | 9/21 | No data | IM nail Plate fixation | 32/64 | No data | Hanging cast then functional brace | Radiological union Delayed union Nonunion Neurological injury |
| Jawa et al. | Retrospective cohort study | 40 | 19/21 | 11/8 | 50 (21–97) | Plate fixation | 9/12 | 41 (24–92) | Coaptation splint less than two weeks then functional brace | Malunion Nerve palsy Failure fixation ROM Infection |
| Mahabier et al. | Retrospective cohort study | 186 | 95/91 | 44/51 | 61.1 | IM nail (82.1%) Plate (11.6%) Ex fix (5.3%) Cerclage wire (1.1%) | 36/55 | 60.6 | Not specified | Delayed union Nerve palsy |
| Matsunaga et al. | Randomised controlled trial | 110 | 58/52 | 35/23 | 37.3 | Plate (MIPO) | 38/14 | 40.3 | Coaptation splint then functional brace | DASH score 6 month Shoulder score Pain Nonunion Malunion Complication |
| Wallny et al. | Retrospective cohort study | 89 | 45/44 | 26/19 | 56 | IM nail | 24/20 | 59 | Gilchrist bandage 1 week then functional brace | Mobility Malunion Function Nerve palsy Nonunion infection |
| Westrick et al. | Retrospective cohort study | 296 | 214/69 13 removed as amputationa | 152/75 | 31 | Plate (135) IM nail (77) Ex fix (2) | 34/35 | 42 | Functional bracing | Radiographic union Nerve palsy Infection |
| Total | 956 | 524/419 | 320/220 (59.26% male) | 41.61 | 211/224 (49.66% male) | 50.42 |
aRandomised controlled trial.
Table 4.
Summary of results.
| Paper | Operative nonunion | Operative delayed union | Non- operative nonunion | Non- operative delayed union | Operative infection | Non- operative Infection | Operative nerve palsy | Operative iatrogenic nerve palsy | Non- operative nerve palsy | Non- operative iatrogenic nerve palsy | Operative PROMS | Non-operative PROMS | Operative Malunion | Non- operative Malunion |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Firat et al. | – | 4/66 | – | 0/66 | 3/66 | 0/62 | − 11 explored and fixeda | – | – | – | Constant Shoulder 85.6 plate, 74 nail Mayo elbow 95.7 plate, 89.2 elbow | Constant Shoulder 92.4 Mayo elbow 96.9 | 0/66 | 19/62 |
| Harkin and Large | 1/27 | 9/27 | 4/80 18/80 converted to surgery | 10/80 | No data | No data | 5/43 | 4/43 | 7/80 | 0/80 | No data | No data | No data | No data |
| Jawa et al. | 0/19 | – | 0/21 | – | 1/19 | 0/21 | 7/19 | 3/19 | 2/21 | 0/21 | – | – | 0/19 | 3/21 |
| Mahabier et al. | – | 18/95 | – | 18/91 | – | 5/95 | 4/95 | 8/91 | 0/91 | |||||
| Matsunaga et al. | 0/58 | – | 7/52 | – | 1/58 | 0/52 | 0/58 | 2/58 | 0/52 | 0/52 | 6 m DASH 10.9 | 6 m DASH 16.9 | 0/58 | 1/52 symptomatic |
| Wallny et al. | 0/45 | – | 2/44 | – | 2/45 | 0/44 | 6/45 | 1/45 | 6/44 | 0/44 | 85.4 ‘Wulker’ et al. score | 90.8 ‘Wulker’ et al. score | – measure only axial shortening | – no time frames specified |
| Westrick et al. | 22/214 | – | 16/69 | – | 8/214 | 0/69 | 2/214 | 2/214 | 14/69 | 0/69 | – | – | – | – |
| Total | 23/363 | 31/188 | 47/266 | 28/237 | 15/402 | 0/248 | 25/474 | 16/474 | 0/357 | 0/143 | 23/135 |
aRandomised controlled trial.
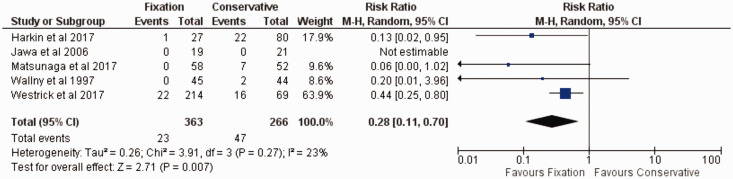
Primary outcome: Nonunion
Five studies measured nonunion rates and were included for meta-analysis (four non-randomised and one RCT). The GRADE quality of evidence was low for the RCT and very low for the non-randomised studies. Jawa et al., Westrick et al. and Harkin et al. defined nonunion as no bridging callus on two radiographs at six months. Matsunaga defined nonunion as absence of clinical or radiological healing at six months. Wallny et al. did not define nonunion. There was a significantly decreased risk of nonunion with operative treatment, RR 0.28 (0.11, 0.70) 95% CI. χ2 for heterogeneity was 3.91, I2 23%, test for overall effect Z = 2.71 (p < 0.007). A forest plot is shown in Figure 2. There was a total of 629 patients. Twenty-three nonunions in 363 patients (6.3%) with fixation were identified, compared to 47 nonunions in 266 patients (17.6%) with non-operative management.
Figure 2.
Nonunion forest plot.
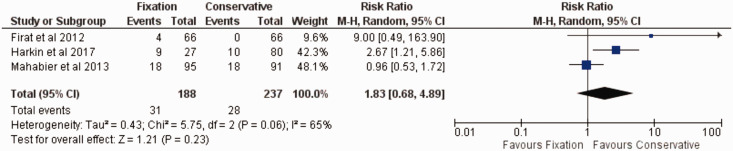
Secondary outcome: Delayed union
Three retrospective studies measured delayed union and were included. The GRADE quality of evidence was very low. Harkin et al. and Mahabier et al. defined delayed union as no radiological union within 24 weeks (bridging callus on three of four cortices on two radiographs). Firat et al. did not define delayed union. There was a trend towards increase in delayed union with operative treatment, however this was not significant. Risk ratio 1.83 (0.68, 4.89) 95% CI. χ2 for heterogeneity was 5.75, I2 65%, test for overall effect Z = 1.21 (p < 0.23). A forest plot is shown in Figure 3. There were a total of 329 patients included. There were 31 delayed unions in 188 in patients with fixation (16.5%) and 28 delayed union in 237 patients with conservative treatment (11.8%). As Firat et al. did not provide a definition for delayed union we performed a separate meta-analysis with this paper removed. The lack of definition was part of the justification for the GRADE quality of evidence as very low. This did not alter the overall findings for delayed union. There was still a trend towards delayed union which was not significant (22.1% with fixation and 16.3% with conservative treatment).
Figure 3.
Delayed union forest plot.
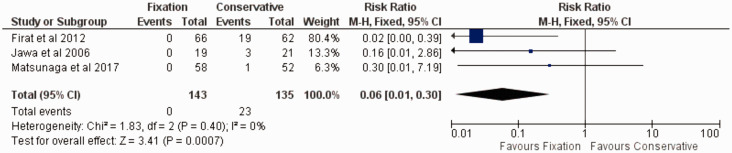
Secondary outcome: Malunion
Three studies, one RCT and two retrospective studies measured malunion and were included. The GRADE quality of evidence was low for non-randomised studies and high for the RCT. Malunion was defined as over 20° mal-alignment on any radiograph by Jawa et al. and as ‘symptomatic malunion’ by Matsunaga et al. Firat et al. measured both coronal and sagittal plane alignment radiographically, and we took the group with over 20° as those with ‘malunion’. There was a significantly decreased risk of malunion with operative treatment. RR 0.06 (0.01, 0.30) 95% CI. χ2 for heterogeneity was 1.83, I2 0%, test for overall effect Z = 3.41 (p < 0.0007). A forest plot is shown in Figure 4. There were a total of 278 patients included, with no malunion in the fixation group and 23 malunions in 135 patients with non-operative treatment (17%).
Figure 4.
Malunion forest plot.
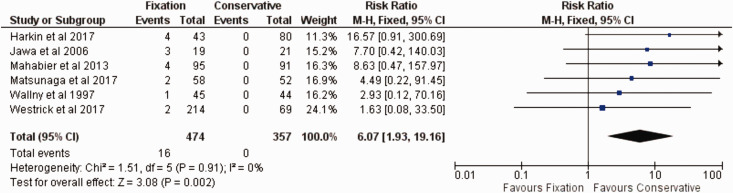
Secondary outcome: Iatrogenic nerve injury
Six studies, one RCT and five retrospective studies measured nerve injury and were included. The GRADE quality of evidence was moderate for non-randomised studies and high for the RCT. Nerve injuries in all studies were diagnosed on a clinical basis. There was a significantly increased risk of iatrogenic nerve injury with operative treatment. RR 6.07 (1.93, 19.16) 95% CI. χ2 for heterogeneity was 1.51, I2 0%, test for overall effect Z = 3.08 (p < 0.002). A forest plot is shown in Figure 5. There were a total of 831 patients with 16 nerve injuries in 474 patients with fixation (3.4%). There were no iatrogenic injuries in the conservatively managed group.
Figure 5.
Iatrogenic nerve injury forest plot.
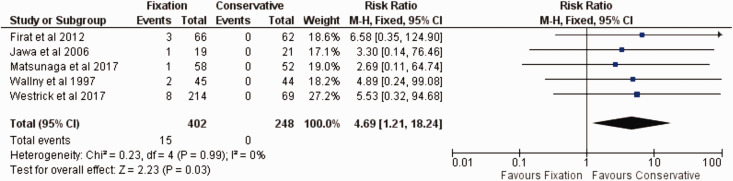
Secondary outcome: Infection
Five studies, one RCT and five retrospective studies measured infection rate and were included. The GRADE quality of evidence was low for non-randomised studies and moderate for the RCT. Infection was diagnosed on a clinical basis in all studies. There was a significantly increased risk of infection with operative treatment. RR 4.69 (1.21, 18.24) 95% CI. χ2 for heterogeneity was 0.23, I2 0%, test for overall effect Z = 2.23 (p < 0.03). A forest plot is shown in Figure 6. There were a total of 650 patients included with 15 infections in 402 patients with fixation (3.7%) and no infections in the conservatively managed group.
Figure 6.
Infection forest plot.
Secondary outcome: Patient reported outcome measures
Three studies included various patient reported outcomes but a meta-analysis was not undertaken as all reported different outcome measures.7,9,12 Matsunaga et al. reported disabilities of the arm shoulder and hand (DASH), Short Form-36, Constant-Murley shoulder score and pain on a visual analogue scale (VAS) at two weeks, one, two and six months and one year. There was no significant difference in any score at any time point aside from the DASH score at six months (p = 0.046); however, this was a six-point difference which is less than what is deemed to be the clinically relevant difference of 10 points.15 Firat et al. reported the Constant Shoulder Score, Mayo Elbow Scores at the time of final review. This time period was not defined. This demonstrated a significantly better score with non-operative treatment and also a significantly greater score with plate fixation over IM fixation. There was no significant difference between Mayo elbow score. Both these studies treated all nonunions with fixation and it is assumed they have been excluded from the non-operative results. Wallny et al. reported a subjective analysis described by Wulker et al., with the results of 85.4 for fixation and 90.8 for non-operative management.16 No statistical analysis was performed.
Quality of evidence for outcome
The Grades of Recommendation, Assessment, Development and Evaluation (GRADE) approach was used to analyse the quality of evidence for each outcome measure17. A summary of this is shown in Table 5.
Table 5.
GRADE summary.
| Outcome | Studies | Number participants (studies) | Risk ratio (95% CI) | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Other | GRADE quality of evidence |
|---|---|---|---|---|---|---|---|---|---|---|
| Nonunion | Jawa et al. Westrick et al. Wallny et al. Matsunaga et al.a Harkin and Large | 679 (5) | 0.25 (0.14, 0.44) | Seriousb | Not serious | Not serious | Not serious | Undetected | Large magnitude of effect | Very low (non- randomised) Low (RCT) |
| Delayed union | Firat et al. Mahabier et al. Harkin and Large | 425 (3) | 1.83 (0.68, 4.89) | Seriousb | Seriousc | Not serious | Seriousd | Undetected | None | Very low |
| Infection | Firat et al. Jawa et al. Westrick et al. Wallny et al. Matsunaga et al.a | 700 (5) | 4.14 (1.14, 17.08) | Seriousb | Not serious | Not serious | Not serious | Undetected | Large magnitude of effect | Low (non- randomised) Moderate (RCT) |
| Iatrogenic nerve injury | Jawa et al. Westrick et al. Wallny et al. Mahabier et al. Matsunaga et al.a Harkin and Large | 881 (6) | 5.94 (1.90, 18.61) | Seriousb | Not serious | Not serious | Not serious | Undetected | Very large magnitude of effect | Moderate (non- randomised) High (RCT) |
| Malunion | Firat et al. Jawa et al. Matsunaga et al.a | 278 (3) | 0.06 (0.01, 0.30) | Seriousb | Not serious | Not serious | Not serious | Undetected | Large magnitude of effect | Low (non- randomised) High (RCT) |
aRandomised controlled trial.
bStudies included moderate and serious risk of bias through multiple categories including confounding, selection bias and outcome assessment.
cIndication of moderate heterogeneity.
dLow number of events and wide confidence interval conferring effect and no effect at each limit.
Discussion
Primary outcome: Nonunion
This study has demonstrated a significantly increased risk of nonunion with non-operative treatment with 5.6% in the operative and 17.6% in the non-operative group. This results in a number needed to treat 8.26 patients. Sarmiento first described a series of 51 patients managed non-operatively with a functional brace with only one nonunion in a patient with a pathological fracture.18 A further larger study from the same centre showed a 3% nonunion rate in 620 patients treated in this fashion.3 This low rate has been repeated in other observational studies of non-operative treatment using a functional brace with nonunion rates of 2% and 3%.19,20 Comparative studies have not replicated this low number, with rates of 27.5% 23.2,% 13.5% and 4.5% in those in this study. Selection bias in these non-comparative studies may account for this difference. More difficult and severe injuries may be selected away from conservative treatment into operative treatment, therefore lowering the nonunion rate. Publication or selection bias may be another cause for the discrepancy in nonunion rate. Small comparative studies with neutral or negative findings are less likely to be published in the literature.21
Open fracture rates were higher with fixation in some included studies, one of the justifications for serious risk of bias. Two studies excluded open fracture, two papers had no data on this and all others excluded grade III open fractures. Given this, the rate of union with surgery may be higher if the rates of open fracture and mechanism of injury were comparable between groups.
Westrick et al. had a high energy mechanism in 76% of patients and a 33% open fracture rate. This study accounted for the most variation in rates of open fracture, and had higher rates of polytrauma in the operative group. A simple fall was the mechanism of injury in only 11%. Again this was a justification for serious confounding and selection bias. Nonunion in both groups were relatively high as expected with such a highly traumatised patient cohort. Polytrauma and open fracture are often considered indications for surgery. However, in the series from Sarmiento et al. there is a high rate of high energy trauma with 34% motor vehicle accident, 19% gunshot wound and 31% low energy fall.3 Furthermore 25% were open fractures and managed without fixation.
There may have been a selection bias with younger, fitter patients treated with fixation who would be less likely to have surgical complications and be keen to avoid long periods of immobilisation to return to work. The average age of the two cohorts in our meta-analysis was 41.6 and 50.4 in the operative and non-operative groups, respectively. There was no data on ASA grade. Some studies had attempted to minimise selection bias, Wallny et al. excluded all multiply injured patients and had comparable demographics between groups. Harkin et al. had similar proportions of patients who smoked, had Diabetes Mellitus or were obese. There were more patients with a psychiatric history in the non-operative group.
Large centres who have specialised in non-operative treatment of humeral shaft fractures seem to achieve lower rates of nonunion, however in these comparative studies this low rate has not been replicated and we see a significantly increased risk with non-operative management. Further prospective randomised trials can only confirm this, however it appears from this study that nonunion rate with non-operative treatment is significantly higher in comparative studies.
Two studies commented on the subsequent management of nonunions. Denard et al. treated all with ORIF and bone grafting; resulting in all 26 patients achieving union. Matsunaga et al. treated all with ORIF without grafting and all 10 patients achieved union. The high success rate of this technique has been replicated in other literature.22–24
Secondary outcome: Delayed union
There was a trend towards favouring non-operative treatment with reduced rate of delayed union, however the quality of evidence was very low. Absolute fixation with primary bone healing does not routinely produce callus and therefore it is logical that this may not always produce bridging callus after 24 weeks; which was the definition used by two of the studies. Some studies used techniques that produce relative stability which should produce callus. Surgical insult to periosteal or intramedullary blood supply during fixation may also account for this increase in time to union. One might argue that this is not relevant in operatively treated patients as they should be using their limb without restriction prior to radiological union, therefore as long as healing does eventually occur before hardware failure this is irrelevant.
Secondary outcome: Malunion
We showed a significantly increased risk of malunion with non-operative treatment. This was difficult to define consistently across groups, and the quality of evidence was low. Matusnaga et al. were the only study to consider whether this malunion was symptomatic. Twenty degrees was the limit defined by the other studies. Sarmiento et al. considered less than 25° to be clinically and functionally acceptable. This is supported by Firat et al. despite a large number of malunions (>20°) in the non-operative group (30%), these patients had the best shoulder and elbow functional scores.
Secondary outcome: Infection and nerve injury
There was a significantly increased risk of infection and iatrogenic nerve injury with operative management. Rates were 3% and 3.3% respectively. These rates would be consistent with those in other non-comparative studies in the literature.25,26
Secondary outcome: Patient reported outcome measures
Due to a variation in outcome measures used across the studies, we were unable to undertake a meta-analysis. Those that did provide outcome measures do not demonstrate any significant difference at final review. Those in favour of fixation may argue that earlier mobilisation after fixation could increase function and outcome in the shorter term, and Matsunaga et al. did show a significant difference in DASH at six months although this was not greater than the minimum clinically relevant difference. Furthermore non-operatively managed patients who undergo surgery for nonunion are removed from some studies and their outcome measures are not included. If included these would likely have an adverse effect on patient reported outcomes within the non-operative cohort. If successful however, these studies demonstrate no difference or a trend towards better function with non-operative management.
Anterograde intramedullary nails have been shown to have high complication rates in some studies.27,28 Although small numbers in each cohort Firat et al. demonstrated a significantly better shoulder score with both non-operative and plate fixation when compared to anterograde nail fixation. Wallny et al. noted that 86.4% of patients had free range of movement with bracing and 48.9% with anterograde nail fixation. These findings indicate that fixation using anterograde nails, as in other studies, can cause shoulder pain and limit function at this joint.
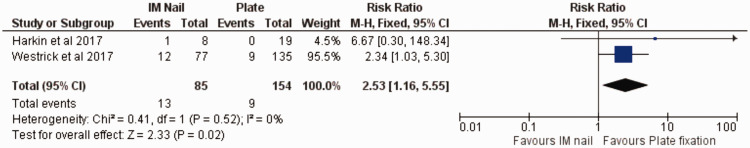
Comparison of fixation
It was not our aim to compare fixation methods in this study. This was mainly due to the large variation in technique within one type of fixation method. Plates were used through various approaches, and in both bridging and compression modes. When grouped together as one technique as ‘plate fixation’ it was possible to perform a subgroup meta-analysis of two papers which demonstrated a trend towards plate fixation with the outcome of nonunion. RR 2.53 (1.16, 5.55) 95% CI, p < 0.02. A forest plot is shown in Figure 7. There were 13 nonunions in 85 nail fixations (15.3%) and nine in 154 plate fixation (5.8%) This was only from the two studies which had both nail and plates within their operative cohort. Across all studies there were 13 nonunions in 130 treated with nail fixation (10%) and nine in 231 with plate fixation (3.9%).
Figure 7.
Treatment algorithm.
Fracture subtypes
Proximal and distal third shaft subtypes were specifically looked at by a number of the studies included. Matsunaga et al. had seven proximal and six distal third fractures managed non-operatively. There were no nonunions within these fracture subtypes. Wallny did not undertake subgroup analysis with regard to location; however they had a large proportion of proximal third fractures. They classified 47.7% and 48.9% of fractures in the non-operative and operative treatment groups respectively as proximal third fractures. Nonunion rate was 4.5% and 0% respectively in these groups. Firat et al. also did not undertake subgroup analysis but did include 26 proximal and 21 distal fractures spread evenly across the three treatment groups. Jawa et al. focused only on distal third fractures and achieved union in all cases. There was a relatively high rate of iatrogenic nerve injury (3/19) with fixation. Harkin et al. performed subgroup analysis between location, but found that when compared to other fracture locations treated with the same method, there was no significant difference in nonunion. Westrick et al. only studied AO classification subgroup not location, but found no statistically significant difference between fracture types and nonunion. Mahabier et al. also only studied AO classification and found no significant difference between nonunion. Denard et al. did not classify the fracture type. In one large cohort of 620 patients, which included 92 proximal third shaft fractures managed non-operatively, there was no nonunion within this subtype.3 There is however contrasting evidence that there can be an increased risk of nonunion with proximal third fractures.29,30 From these comparative studies it does not appear that proximal or distal fractures differ in rates of nonunion from middle third fractures and should be treated similarly.
Limitations
The predominant limitation in this study is the retrospectivity of most included studies. We have undertaken this analysis in an attempt to combine the body of evidence available with regard to humeral shaft fracture management. All studies indicated the same trends across nonunion, malunion, delayed union, infection and nerve injury. Risk of bias was serious for all retrospective studies, and moderate for the RCT. The level of evidence has therefore been accordingly judged in Table 5. There was clinical homogeneity across most outcome measures.
Future research
It is clear that more prospective RCTs are required to further clarify the best treatment option for humeral shaft fractures. Modern surgical techniques and fixation methods should be evaluated in direct comparison with non-operative management. The publication of the first RCT on this topic is encouraging. This would help clarify why non-operative management has a higher rate of nonunion in comparative studies when compared with non-comparative studies. The studies evaluated here suggest that anterograde nailing of the humerus can be associated with shoulder pain and dysfunction and we would lean towards plate fixation as a first choice of operative treatment. With new developments in surgical technique and fixation methods these must be continually re-evaluated in direct comparison to non-operative methods.
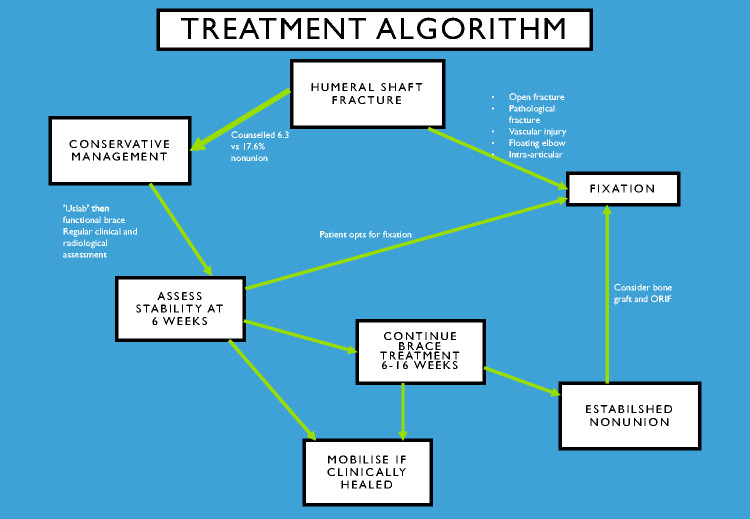
Suggested treatment algorithm
Based on these findings we can suggest the following treatment algorithm shown in Figure 8. All patients should initially be managed conservatively with a coaptation splint then a humeral brace; having been counselled on the slightly higher rate of nonunion, but lower rate of potential complications with this treatment. Indications for surgical treatment and fixation are open injury, vascular injury, pathological fractures, intra-articular extension, ‘floating elbow’, patient preference, polytrauma, bilateral humeral fractures, intolerance of bracing and failure of conservative treatment. A brace should be worn until clinical stability is achieved at the fracture site. There is evidence that excessive fracture site mobility at six weeks is predictive of nonunion and patients at this stage should be counselled accordingly.22 Non-operative treatment at six weeks should be continued after consideration of patient preference, fracture site mobility and radiographic findings. Painful nonunion is an indication for surgery, and we would suggest ORIF with iliac crest bone graft.
Figure 8.
Subgroup analysis: nail vs. plate.
Conclusion
In comparative studies we have shown a significantly higher risk of nonunion with non-operative treatment for humeral shaft fractures. Operative management is however associated with a significantly higher risk of infection and iatrogenic nerve injury. There is a trend towards increased delayed union with operative management. There is a significantly increased risk of malunion with non-operative management, however whether this has any impact on function is unclear. There was no significant difference in functional outcome or range of movement between treatments; although there may be a trend towards decreased shoulder scores with anterograde nail fixation. Subsequent nonunion has a high rate of union when treated with ORIF and bone grafting. Our findings suggest that in the majority of cases, humeral shaft fractures can be managed with non-operative treatment, and any resulting nonunion should be treated with plate fixation achieving high rates of union.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Ekholm R, Adami J, Tidermark J, et al. Fractures of the shaft of the humerus: an epidemiological study of 401 fractures. Bone Joint J 2006; 88: 1469–1473. [DOI] [PubMed] [Google Scholar]
- 2.Bergdahl C, Ekholm C, Wennergren D, et al. Epidemiology and patho-anatomical pattern of 2,011 humeral fractures: data from the Swedish Fracture Register. BMC Musculoskelet Disord 2016; 17: 159–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarmiento A, Zagorski JB, Zych GA, et al. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am 2000; 82: 478–486. [DOI] [PubMed] [Google Scholar]
- 4.Huttunen TT, Kannus P, Lepola V, et al. Surgical treatment of humeral-shaft fractures: a register-based study in Finland between 1987 and 2009. Injury 2012; 43: 1704–1708. [DOI] [PubMed] [Google Scholar]
- 5.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016; 355: i4919–i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011; 343: d5928–d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matsunaga FT, Tamaoki MJ, Matsumoto MH, et al. Minimally invasive osteosynthesis with a bridge plate versus a functional brace for humeral shaft fractures: a randomized controlled trial. J Bone Joint Surg Am 2017; 99: 583–592. [DOI] [PubMed] [Google Scholar]
- 8.Denard A, Richards JE, Obremskey WT, et al. Outcome of nonoperative vs operative treatment of humeral shaft fractures: a retrospective study of 213 patients. Orthopedics 2010; 33: 511–515. [DOI] [PubMed] [Google Scholar]
- 9.Fırat A, Deveci A, Güler F, et al. Evaluation of shoulder and elbow functions after treatment of humeral shaft fractures: a 20–132-month follow-up study. Acta Orthop Traumatol Turc 2012; 46: 229–236. [DOI] [PubMed] [Google Scholar]
- 10.Jawa A, McCarty P, Doornberg J, et al. Extra-articular distal-third diaphyseal fractures of the humerus: a comparison of functional bracing and plate fixation. J Bone Joint Surg Am 2006; 88: 2343–2347. [DOI] [PubMed] [Google Scholar]
- 11.Westrick E, Hamilton B, Toogood P, et al. Humeral shaft fractures: results of operative and non-operative treatment. Int Orthop 2017; 41: 385–395. [DOI] [PubMed] [Google Scholar]
- 12.Wallny T, Sagebiel C, Westerman K, et al. Comparative results of bracing and interlocking nailing in the treatment of humeral shaft fractures. Int Orthop 1998; 21: 374–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mahabier KC, Vogels LM, Punt BJ, et al. Humeral shaft fractures: retrospective results of non-operative and operative treatment of 186 patients. Injury 2013; 44: 427–430. [DOI] [PubMed] [Google Scholar]
- 14.Harkin FE, Large RJ. Humeral shaft fractures: union outcomes in a large cohort. J Shoulder Elbow Surg 2017; 26: 1881–1888. [DOI] [PubMed] [Google Scholar]
- 15.Hudak PL, Amadio PC, Bombardier C, et al. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and hand). Am J Ind Med 1996; 29: 602–608. [DOI] [PubMed] [Google Scholar]
- 16.Wulker N, Kohn D, Grimm C. Evaluation of the shoulder function with various scores. Orthop Praxis 1991; 12: 750–754. [Google Scholar]
- 17.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011; 64: 383–394. [DOI] [PubMed] [Google Scholar]
- 18.Sarmiento A, Kinman PB, Galvin EG, et al. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am 1977; 59: 596–601. [PubMed] [Google Scholar]
- 19.Ostermann PA, Ekkernkamp A, Muhr G. Functional bracing of shaft fractures of the humerus – an analysis of 195 cases. Orthop Trans 1993; 17: 937–937. [Google Scholar]
- 20.Zagorski JB, Latta LL, Zych GA, et al. Diaphyseal fractures of the humerus. Treatment with prefabricated braces. J Bone Joint Surg Am 1988; 70: 607–610. [PubMed] [Google Scholar]
- 21.Harris IA, Mourad M, Kadir A, et al. Publication bias in abstracts presented to the annual meeting of the American Academy of Orthopaedic Surgeons. J Orthop Surg 2007; 15: 62–66. [DOI] [PubMed] [Google Scholar]
- 22.Driesman AS, Fisher N, Karia R, et al. Fracture site mobility at 6 weeks after humeral shaft fracture predicts nonunion without surgery. J Orthop Trauma 2017; 31: 657–662. [DOI] [PubMed] [Google Scholar]
- 23.Fattah HA, Halawa EE, Shafy TH. Non-union of the humeral shaft: a report on 25 cases. Injury 1982; 14: 255–262. [DOI] [PubMed] [Google Scholar]
- 24.Marti RK, Verheyen CC, Besselaar PP. Humeral shaft nonunion: evaluation of uniform surgical repair in fifty-one patients. J Orthop Trauma 2002; 16: 108–115. [DOI] [PubMed] [Google Scholar]
- 25.McCormack RG, Brien D, Buckley RE, et al. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail: a prospective, randomised trial. Bone Joint J 2000; 82: 336–339. [DOI] [PubMed] [Google Scholar]
- 26.Heim D, Herkert F, Hess P, et al. Surgical treatment of humeral shaft fractures – the Basel experience. J Trauma 1993; 35: 226–232. [PubMed] [Google Scholar]
- 27.Robinson CM, Bell KM, Court-Brown CM, et al. Locked nailing of humeral shaft fractures. Experience in Edinburgh over a two-year period. J Bone Joint Surg Br 1992; 74: 558–562. [DOI] [PubMed] [Google Scholar]
- 28.Hems TE, Bhullar TP. Interlocking nailing of humeral shaft fractures: the Oxford experience 1991 to 1994. Injury1996, 27: 485–489. [DOI] [PubMed] [Google Scholar]
- 29.Rutgers M, Ring D. Treatment of diaphyseal fractures of the humerus using a functional brace. J Orthop Trauma 2006; 20: 597–601. [DOI] [PubMed] [Google Scholar]
- 30.Ali E, Griffiths D, Obi N, et al. Nonoperative treatment of humeral shaft fractures revisited. J Shoulder Elbow Surg 2015; 24: 210–214. [DOI] [PubMed] [Google Scholar]