Abstract
Since the onset of the global pandemic in early 2020, coronavirus disease 2019 (COVID-19) has posed a multitude of challenges to health care systems worldwide. In order to combat these challenges and devise appropriate therapeutic strategies, it becomes of paramount importance to elucidate the pathophysiology of this illness. Coronavirus disease 2019, caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV2), is characterized by a dysregulated immune system and hypercoagulability. COVID-associated coagulopathy (CAC) was recognized based on profound d-dimer elevations and evidence of microthrombi and macrothrombi, both in venous and arterial systems. The underlying mechanisms associated with CAC have been suggested, but not clearly defined. The model of immunothrombosis illustrates the elaborate crosstalk between the innate immune system and coagulation. The rendering of a procoagulant state in COVID-19 involves the interplay of many innate immune pathways. The SARS-CoV2 virus can directly infect immune and endothelial cells, leading to endothelial injury and dysregulation of the immune system. Activated leukocytes potentiate a procoagulant state via release of intravascular tissue factor, platelet activation, NETosis, and inhibition of anticoagulant mechanisms. Additional pathways of specific relevance in CAC include cytokine release and complement activation. All these mechanisms have recently been reported in COVID-19. Immunothrombosis provides a comprehensive perspective of the several synergistic pathways pertinent to the pathogenesis of CAC.
Keywords: COVID-19, immunothrombosis, coagulopathy
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) has led to a global outbreak of coronavirus disease 2019, termed COVID-19.1 Health care workers have been posed with innumerous and unique challenges having to adapt at a rapid pace to prioritize the lives of patients affected by this potentially fatal virus. One of the challenges has been keeping up with the unfolding manifestations of the virus. There have been many published reports detailing these manifestations from China and Italy. Despite the rapid pace at which new information is being published, there remain many questions surrounding the pathogenesis and management of COVID-19. It is now widely recognized that COVID-19 is a systemic disease marked by a dysregulated immune system and a hypercoagulable state. Mortality in COVID-19 has been shown to correlate with both elevated interleukin-6 (IL-6) levels and elevated d-dimer levels.2 Additionally, there have been many case reports detailing the association of both venous thromboembolism (VTE) and arterial events in COVID-19 patients. The model of immunothrombosis puts forth evidence of the elaborate interactions between the innate immune system and the coagulation system.3 These interactions, in a physiological sense, foster the primary role of each system to achieve defense against foreign pathogens and hemostasis, respectively. The model can further be used to demonstrate how the dysregulation of each system can potentiate unchecked activation of the other, leading to pathological and potentially catastrophic consequences for the host.
In this review, we aim to discuss the various components of immunothrombosis, including key mediators such as leukocytes and cytokines, in rendering a procoagulant state and the ultimate result of thrombosis, as it relates to infectious and septic states. We also aim to unravel and illustrate the aspects of COVID-19-associated coagulopathy (CAC). Finally, we conceptualize the pathophysiology of a hypercoagulable state and thrombosis associated with COVID-19 relating to the well-described model of immunothrombosis. Although this is no longer a novel concept, it remains a relevant concept during the current pandemic of COVID-19.
COVID-19-Associated Coagulopathy and Cytokine-Release Syndrome
SARS-CoV2, a novel strain of the single-stranded RNA virus of the coronavirus family, has led to several systemic manifestations, most recognizably acute respiratory failure evidenced by diffuse bilateral infiltrates on chest imaging and progression to acute respiratory distress syndrome (ARDS).4,5 The predominant underlying mechanism in COVID-19-related mortality is hypothesized to be widespread tissue damage and endothelial injury from an overactivated immune system via exaggerated T-cell responses and increased cytokine secretion, leading to a cytokine storm.6 COVID-19 patients demonstrate markedly increased IL-6, IL-2R, IL-10, and tumor necrosis factor α (TNF-α) levels.7,8 These patients are also reported to have strikingly elevated ferritin and C-reactive protein levels, akin to patients presenting with hemophagocytic syndrome or cytokine-release syndrome (CRS).9 These levels appear to be directly associated with increased mortality.9
With increasing numbers of patients with COVID-19, reports of aberrant hematologic parameters became evident, leading to the recognition of CAC. It has been reported that thrombocytopenia happens more often in patients with severe disease and potentially correlates with increased mortality.10,11 Lymphocytopenia is also more prominent among severe cases.10,12
Another prominent finding, which correlates with mortality, is the markedly elevated d-dimer level in patients with severe disease, usually a few folds higher, compared to patients with nonsevere courses.13,14 In COVID-19, patients with complications of ARDS, deep venous thrombosis (DVT), disseminated intravascular coagulopathy (DIC), and cardiac injury, higher d-dimer levels were also observed.10 Some reports suggest that d-dimer higher than 1 μg/mg suggests poor prognosis.14 Other aberrancies in coagulopathy, including elevated prothrombin time (PT), partial thromboplastin time, and fibrin-degradation products level, and fibrinogen levels, are also reported in COVID-19 patients with unclear clinical correlations.10,15,16 Ultimately, the pathophysiology of CAC is yet to be elucidated but, at this time, remains an area of great interest and speculation.
Overview of Hemostasis
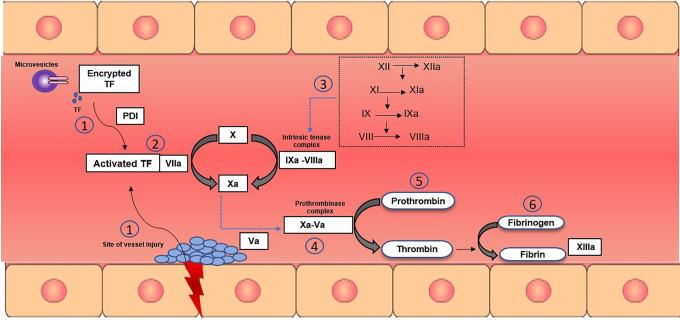
The inciting event for hemostasis occurs with disruption of the integrity of the endothelial lining (Figure 1). When vessel wall injury occurs, collagen and tissue factor (TF) contained in the subendothelium become exposed, triggering the formation of a thrombus. Platelet adhesion at the site of injury occurs via interactions of glycoprotein VI to exposed collagen and glycoprotein Ib-V-IX with collagen-bound von Willebrand factor (vWF).17 Platelet activation is initiated following this interaction. Tissue factor–mediated platelet activation is an alternate pathway, which is independent of endothelial injury.17,18 Platelet activation leads to the release of the contents of α granules and dense granules. Adenosine diphosphate (ADP) and calcium ions are released from dense granules, further stimulating platelet activation through 2 ADP receptors, P2Y1 and P2Y12.19
Figure 1.
Overview of mechanisms of hemostasis. The coagulation cascade during hemostasis is initiated with the release of tissue factor (TF). (1) At the site of endothelial injury, TF that is stored in the adventitial and medial layers of the vessel wall is released. Platelet activation and adhesion occurs at the site of injury. (1) Encrypted TF is also released from monocyte-derived microparticles. Encrypted TF is activated through the secretion of protein disulfide isomerase (PDI), which occurs because of endothelial injury and platelet activation. (2) Activated TF will form a complex with circulating factor VIIa (FVIIa), leading to activation of FX to FXa. A small amount of thrombin generated creates an amplification loop by activating FVIII, FXI, and FV. (3) During the propagation phase, FIXa, which is generated by TF–VIIa complex or FXIa, binds to its cofactor FVIIIa to form the intrinsic tenase complex. FXa is then formed by TF–FVIIa complex or FIXa–FVIIa complex. (4) FXa binds to FVa, forming the prothrombinase complex. (5) FXa–FVa complex converts prothrombin to thrombin. (6) Thrombin further activates fibrinogen to fibrin, which is cross-linked by FXIIIa to form a stable clot.
Concurrently, the coagulation cascade begins with the activation of TF, which is a potent initiator of thrombin generation and fibrin formation. Tissue factor is expressed in 2 major anatomical compartments that are involved in coagulation: the adventitia and the medial layer of the vessel wall, and microparticles circulating in the blood.17 When the endothelial layer of the vessel is structurally damaged, TF is exposed and activated (Figure 1). Additionally, upon platelet and endothelial activation, secretion of protein disulfide isomerase (PDI), dubbed the “damage signal,” activates encrypted TF within the microparticles (Figure 1).17 Activated TF will form a complex with Factor VIIa (FVIIa) to activate FIX, FX, and additional FVII. Generated thrombin will activate FXI, FVIII, and FV. Factor IXa, which is generated by TF–VIIa complex or FXIa, binds to its cofactor FVIIIa to form the intrinsic tenase complex, leading to activation of FX (Figure 1). The resultant FXa and FVa complex converts prothrombin to thrombin, leading to propagation of coagulation cascade (Figure 1).17 Thrombin further activates fibrinogen to fibrin, which will be cross-linked by activated FXIIIa to form stable thrombi (Figure 1). Fibrin formation is counterbalanced by the fibrinolytic system, by tissue-type plasminogen activator (tPA), which cleaves plasminogen to form the serine protease plasmin, which degrades fibrin to limit the extent of thrombus formation.20
Immunothrombosis
The term “immunothrombosis” was conceptualized by Engelmann and Massberg in 20133 to accurately define the intricate network between the coagulation system and the innate immune system. This theory defines the symbiotic relationship between these distinct pathways, specifically in the context of acute infectious states. Immunothrombosis describes the active participation of the innate immune system in forming a thrombus via distinct cellular and molecular interactions, triggered by recognition of pathogens and damaged cells. Under this theory, this response is proposed to be a conserved evolutionary defensive link to inhibit pathogen dissemination.21,22 Although there is overlap, immunothrombosis suggests mechanistically distinct pathways of thrombosis and hemostasis through the influence of the innate immune system.23
Although the extent of the role of microthrombi in the prevention of dissemination of pathogens in septic states has been challenged,24 the concept of immunothrombosis, nevertheless, underscores the crosstalk between the coagulation and the immune system. Furthermore, dysregulation of immunothrombosis sets up a vicious cycle of unchecked immune activation and thrombus formation.3,25 Below, we describe the processes involved in rendering a procoagulant state in infections.
Leukocyte-Mediated Procoagulant State
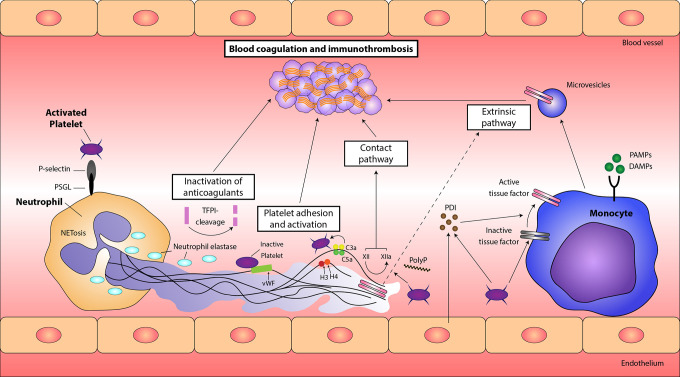
Leukocytes have recently been highlighted in thromboinflammatory diseases as vital components and propagators on thrombosis. Leukocytes, particularly monocytes and neutrophils, activate platelets and the coagulation cascade through various processes (Figures 2 and 3).26 Also, they produce cytokines, which confer a proadhesive and procoagulant effect on endothelial cells (ECs).27 Conversely, leukocyte chemotaxis and phagocytic functions coordinate thrombus resolution.27 Nonetheless, imbalances in the immune system threaten these carefully regulated processes, imposing procoagulant conditions (Figures 2 and 3).
Figure 2.
Principles of immunothrombosis. Monocytes and their microvesicles release activated intravascular tissue factor (TF) in response to pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs), which initiates the extrinsic pathway of coagulation. Activated platelets and endothelium secrete protein disulfide isomerase (PDI), which activates microvesicle-derived TF. Interaction between P-selectin on activated platelets and P-selectin glycoprotein ligand (PSGL) on leukocytes enhance recruitment of leukocytes and increase TF production. Neutrophil extracellular traps (NETs) provide a scaffold consisting of DNA, histones, and neutrophil serine proteases, and they support immunothrombosis through several pathways. (1) NETs bind to von Willebrand factor (VWF) and support the recruitment of platelets. (2) Histones H3 and H4 on NETs can trigger the activation of platelets. (3) NETs bind to TF leading to TF-mediated thrombin generation through the extrinsic pathway (dotted arrow). (4) Neutrophil elastase and other neutrophil serine proteases cleave and inactivate anticoagulants, including TF pathway inhibitor (TFPI) and thrombomodulin. (5) NETs can directly activate factor XII (the contact pathway of coagulation) mediated by platelet-derived polyphosphates (PolyP). The complement system (specifically the activated complement components C3a and C5a) also enhances platelet activation.
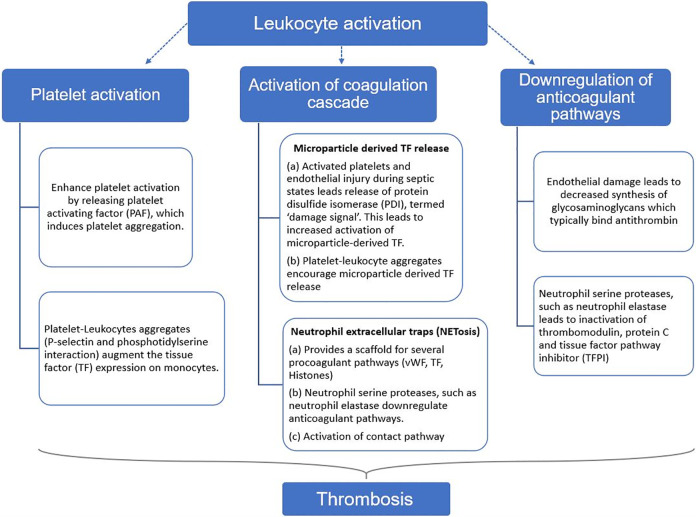
Figure 3.
Summary of the mechanisms of leukocyte induced procoagulant state. Activation of leukocytes during states of sepsis and inflammation leads to a prothrombotic state, primarily through platelet activation, activation of coagulation cascade, and downregulation of anticoagulant pathways.
Leukocytes lead to platelet activation
Platelet activation plays a critical inciting role in thrombosis following vascular injury. Platelets support thrombosis through the release of coagulation factors and exposing negatively charged phospholipids that act as essential cofactors for the proteolytic reactions triggered by coagulation factors.28 Platelets and leukocytes not only engage in bidirectional pathways intended to enhance host defense and pathogen containment but also propagate a procoagulant state as a means of defense.29 First, platelets guide the cells of the immune system to the site of the vascular injury through mediators, including various CXC-chemokine ligands, CD40 ligand, CD154, and TREM1.30,31
Activated cells of the innate immune system and the ensuing cytokine release induce platelet activation by releasing platelet-activating factor (Figure 3).32 Pro-inflammatory stimuli and high shear stress also promote formation of heterotypic platelet–leukocyte aggregates through the interaction of P-selectin on the surface of platelets and leukocyte surface P-selectin glycoprotein ligand (PSGL-1).33 This interaction not only augments the recruitment of leukocytes but also leads to increased expression of TF on monocytes (Figures 2 and 3).27,34 The platelet–leukocyte aggregates are associated with many thromboinflammatory conditions, such as inflammatory bowel disease.27,35 Additional interactions of platelets and vWF with neutrophil extracellular traps (NETs) are pivotal mechanisms in immunothrombosis and will be described below (Figure 2).
Leukocytes enhance the activity of the coagulation system
Leukocytes- and microparticle-derived TF is thought to play a more integral role in thrombosis than in physiologic hemostatic pathways.3 Intravascular TF is functionally inert in its natural state, specifically when expressed on hematopoietic cells.36 Pro-inflammatory states such as infections and sepsis provide the stimulus for activation of monocyte and microparticle-derived intravascular TF release (Figure 3). Protein disulfide isomerase is an oxidoreductase secreted by activated platelets, ECs, or by damaged cells and supports the activation of leukocyte- and microvesicle-derived intravascular TF (Figure 2).37,38 Tissue factor decryption occurs through other various mechanisms, including P-selectin and PSGL interaction,39 and the recognition of pathogen-associated molecular proteins (PAMPs) via toll-like receptors (TLRs) on the surface of monocytes.22 Additionally, damage-associated molecular proteins released from damaged host cells, ECs, and consequent PDI signaling lead to microvesicle-derived TF activation (Figure 2).40 Activated monocytes and the microparticles that they release remain the largest source of intravascular TF,41 with neutrophils and eosinophils contributing to a lesser extent.42–44
Neutrophils mediate a procoagulant environment primarily through the release of NETs (Figure 3).27 Following exposure to pathogens, activated platelets, and cytokines, neutrophils undergo the formation of NETs via a process termed NETosis (Figure 2).3,27 Neutrophil extracellular traps constitute a matrix of DNA, histones, and various neutrophil antimicrobial machinery.29,45 Apart from providing antimicrobial defense, NETs play a fundamental role in providing a scaffold for procoagulant effectors consisting of platelets, vWF, TF, extracellular histones, high mobility group box-1, neutrophil serine proteases, and fibrinogen (Figures 2 and 3).26,46,47
Neutrophil extracellular traps also provide a catalytic platform for proteolytic activity of neutrophil serine proteases, such as neutrophil elastase, which degrades and alters the function of anticoagulants such as thrombomodulin.48 Histone H4 binds to prothrombin and generates thrombin by autoactivation.49 Neutrophil elastase and cathepsin G, which are part of the antimicrobial repertoire, also proteolytically inactivate another anticoagulant, tissue factor pathway inhibitor (TFPI), the primary inhibitor of thrombin (Figures 2 and 3).45,50 Neutrophil extracellular traps have also been shown to bind to factor XII (Hageman factor), leading to its activation to FXIIa, prompting the direct activation of the contact pathway of coagulation (Figures 2 and 3). The contact pathway is thought to have a vital role in immunothrombosis, in contrast to its minor role in physiologic hemostasis.3,50
Thrombosis is regulated by 3 principal anticoagulants, which are antithrombin, thrombomodulin, and TFPI.51 The procoagulant state is further propagated during infections by decreased production of anticoagulants from endothelial injury as well as inhibition of anticoagulant mechanisms via degradation by neutrophil elastase.51 Typically, an intact EC has anticoagulant properties.52 The release of inflammatory cytokines during infection and sepsis significantly alters the antithrombotic nature of the EC. Glycosaminoglycans act as heparin-like cofactors that facilitate binding with antithrombin, leading to the production of a potent inhibitor of thrombin (Figure 3).53,54 Decreased synthesis of glycosaminoglycans on the surface of EC occurs in inflammatory states.54 Endothelial cell also expresses thrombomodulin, which binds to thrombin, leading to decreased protein C activation (Figure 3).55 Activated protein C regulates coagulation activation by proteolytic cleavage of the essential cofactors Va and VIIIa.55 The third, major impaired anticoagulant pathway includes TFPI, the primary inhibitor of the TF–FVIIa complex.56,57 Neutrophil elastase plays a central role in the inactivation of TFPI (Figures 2 and 3).51
Cytokine-Mediated Procoagulant State
Cytokines and interferons play a pivotal role in inflammation. Cytokines are secreted by activated leukocytes and ECs.58 Its relationship with the coagulation system during inflammatory states is complex and dynamic. The cytokines exert a procoagulant effect by means of increased platelet activation, release of TF from monocytes and ECs, downregulation of anticoagulant pathways, and inhibition of fibrinolysis.59–62 Conversely, the production of pro-inflammatory cytokines such as IL-6 and TNF-α by monocytes through protease-activated receptors (PARs) signaling is enhanced by thrombin generation.51
Notably, there is inconclusive evidence suggestive of an association between risk of venous and arterial thrombosis and single-nucleotide polymorphism heterozygosity in inflammatory-related genes of IL-1A, IL-4, IL-6, and IL-13.63,64 Many of the procoagulant effects of cytokines intersect with complement-mediated pathways and have a crucial role through interactions with leukocytes, platelets, and ECs. Therefore, their in-depth mechanisms are detailed in the respective sections in this review.
Viral-Mediated Procoagulant State
The procoagulant effects of bacterial endotoxins via augmentation of TF and plasminogen activator inhibitor expression are well described.65 Nevertheless, many viral infections can cause hemorrhagic or thrombotic complications.66 In one such model, using mice injected with lethal doses of influenza virus developed ARDS and hyperinflammatory cytokine responses, evidence of platelet activation, microvascular thrombi, and NETosis. This model demonstrated similar findings to endotoxemic models of sepsis.67 Viral-mediated coagulation is postulated to occur in 4 main ways: endothelial disruption, leukocyte–platelet interaction, cytokine release, and release of intravascular TF.
Endothelial dysfunction and apoptosis can occur via direct viral infection or through cytokine release. Activation of TF and vWF, as well as exposure of collagen from denuded EC and cytokine release, leads to thrombus formation through platelet activation and extrinsic coagulation cascade.68 Furthermore, viruses can directly infect the cells of the innate immune system, which can lead to immune dysregulation and potential consequential effects on the coagulation system.67–69 Although TLRs, especially TLR7 and platelet interaction, are described in viral infections, the role of this association in the propagation of a thrombus is unclear.70
In conclusion, a viral-mediated coagulant state culminates in the presence of endothelial injury and dysfunction and cytokine-driven inflammatory conditions, leading to activation of TF-mediated thrombosis.
Complement-Mediated Procoagulant State
It has been reported that complement activation enhances thrombosis at different points of the coagulation process.71 Complements can modify phospholipid membranes of cells, which is essential for TF-initiated coagulation.71 Studies have shown that complement pathways can trigger the activation of platelets and fibrin formation (Figure 2).72 Besides, activated complement factors can increase TF expression in various cells and modify mast cells and basophils to a prothrombotic phenotype.72–74 Clinically, complement-related prothrombotic state is observed in diseases such as paroxysmal nocturnal hemoglobinuria, glomerulonephritis, and vasculitis.75
Fibrinolysis During an Infectious State
Under physiological conditions, the innate immune system also modulates fibrinolytic pathways. Leukocytes express urokinase-type plasminogen activator (uPA) and uPA receptor (uPAR), in addition to receptors for plasminogen. Plasminogen is localized to the leukocyte surface increasing the activation of tPA or uPA.29 Although leukocytes possess the endogenous capability to enhance fibrinolysis, excessive coagulation during a state of dysregulated immune system can overwhelm the balance to favor persistent thrombus formation.76
Microthrombosis, VTE, and Arterial Thrombosis in Infection
Microthrombosis during infections and sepsis has been extensively described in the literature, demonstrating the crosstalk between the immune system and the coagulation pathway. Microvascular thrombosis is characterized by the formation of fibrin and platelet-rich thrombus, resulting in occlusion of microvessels (arterioles, venules, capillaries).77 The consequences can range from transient disruptions in the coagulation system to ischemia and organ dysfunction. Microvascular thrombosis likely occurs at a more frequent rate than reported due to difficulty in establishing this diagnosis. As of yet, there is not a specific laboratory surrogate for this entity.
Venous and arterial thrombosis in sepsis with resultant organ ischemia is the telltale sign of dysregulated immunothrombosis. Recent evidence suggests that aberrant immunothrombosis also contributes to thrombus formation in large vessel disease, including atherothrombosis and DVT.51 Structural analysis of venous clots demonstrates activated leukocytes and NETs within the architecture of the thrombus, supporting the involvement of leukocyte-mediated platelet activation and NET-driven VTE.27,29 Arterial thrombosis occurs following plaque rupture and thrombus formation.
Leukocytes can partake in atherothrombosis in inflammatory states by generating microparticle-associated TF at the site of vessel injury.29,78 Plasma levels of TF-expressing monocytes and microparticles, leukocyte–platelet aggregates, and NET markers are elevated in conditions that predispose to cardiovascular disease.3,29 Additionally, pro-inflammatory cytokines destabilize the atherosclerotic plaques by promoting cell apoptosis and matrix degradation.78 Other contributing factors that lead to arterial thrombosis in inflammatory states are demand ischemia, impaired fibrinolysis, endothelial dysfunction, and cytokine-induced vasospasm.79,80
An aberrant immunothrombosis leads to CAC.
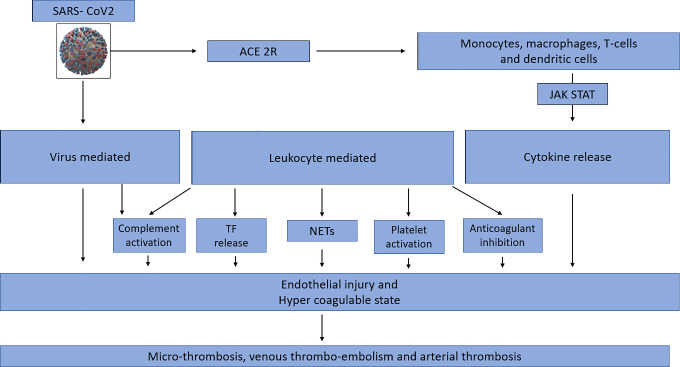
The current COVID-19 pandemic has resurrected the concept of immunothrombosis as it is a relevant model to demonstrate the potentiating effects of the immune system and the coagulation system and the detrimental effects associated with their unrestrained activation, as evidenced by microthrombi and overt venous and arterial thrombi (Figure 4). The impact of aberrant immunothrombosis on mortality in COVID-19 is a matter of ongoing interest and debate as identifying the most significant therapeutic target or synergistic pathways may have enormous implications on outcomes.
Figure 4.
Model of COVID-associated coagulopathy. A, First, SARS-CoV2 gains entry into cells via the angiotensin-converting enzyme 2 receptor (ACE-2R), leading to activation of the innate immune system. Direct viral infection of the immune cells leads to dysregulation and cytokine release. B, Activated monocytes, macrophages stimulate Janus Kinas (JAK)- Signal transducer and activator of transcription (STAT) (JAK STAT) pathways via cis/trans signaling, leading to an amplification of cytokine release. C, SARS-CoV2 infects endothelial cells directly, resulting in endothelial injury and therefore propagating a hypercoagulable state. D, Leukocyte activation and ensuing cytokine storm in SARS-CoV2 leads to a hypercoagulable state though 5 main ways: increased tissue factor release, neutrophil extracellular traps, platelet activation, inactivation of anticoagulant pathways, and complement activation. E, Dysregulation of the immune system in SARS-CoV2 infection and the resultant endothelial injury and hypercoagulable state culminates into widespread microthrombosis, venous thromboembolism, and arterial thrombosis.
We propose the following pathways as contributing to the coagulation abnormalities and thrombosis seen in COVID-19, using supporting evidence from prior published reports.
SARS-CoV-2, a β-coronavirus, infects host cells through angiotensin-converting enzyme 2 (ACE2) receptor facilitated by the host’s TMPRSS2 membrane protease.81 Angiotensin-converting enzyme 2 receptors are found on cardiopulmonary cells, ECs, as well as hematopoietic cells such as monocytes and macrophages.80 The mechanisms of SARS-CoV-2-mediated procoagulant effects are described below.
Angiotensin-converting enzyme 2 has inherent anti-inflammatory properties through direct communication with macrophages and attenuation of angiotensin II levels. Under normal physiological condition, angiotensin II is pro-inflammatory.82 Downregulation of ACE2 occurs following viral engagement, leading to elevated angiotensin II levels, further adding to a hyperinflammatory state.83,84
Varga et al85 recently published a case series of 3 patients with SARS-CoV2 and found to have EC infection and endothelitis. Histological examination of vascular structures of varying organs in all 3 of the patients demonstrated viral inclusion bodies, mononuclear and neutrophilic infiltration, and apoptosis of endothelial and inflammatory cells.85 Apart from direct infection of the ECs, secondary endothelial injury also occurs as a result of widespread immune activation and cytokine release (Figure 4).86
Interleukin-6 is suggested to be a significant contributor to the immune dysregulation and ensuing CRS that occurs in COVID-19. Interleukin-6 binds to the membrane-bound IL-6 receptor (mIL-6R) on immune cells or soluble IL-6R typically on ECs (sIL-6R), resulting in a complex with gp130, leading to downstream signal transduction via JAK-STAT pathway (Figure 4).87
Additionally, SARS-CoV2 infection is associated with decreased circulating lymphocytes and T-cell subsets (CD4+, CD8+ T lymphocytes, and regulatory T cells) either due to selective destruction, functional exhaustion, or potentially direct viral infection.84,88 A decreased T-cell response has injurious effects due to attenuated viral clearance and antibody production; this leads to macrophage activation syndrome and cytokine storm.84 The end result is an amplified production of cytokines leading to microthrombosis and organ dysfunction, as evidenced by high mortality in COVID-19 patients with elevated IL levels (Figure 4).
Postmortem analysis of COVID-19 patients verifies the presence of widespread microthrombi and suggests a possible cause for mortality. Fox et al89 described 4 cases with thrombus formation within capillaries and small vessels, surrounded by aggregates of CD4+ cells. Furthermore, the demonstration of NETs on histologic analysis supports the relevance of immunothrombosis (Figure 4).90 Zuo et al91 also demonstrated increased levels of cell-free DNA, myeloperoxidase-DNA, and citrullinated histone H3, which are the specific markers of NETs, in the sera of COVID-19 patients. The addition of the sera of COVID-19 patients to healthy controls further promoted NETosis.91
Disseminated intravascular coagulopathy is the most common coagulopathy that is associated with sepsis states. COVID-associated coagulopathy differs from DIC in specific manifestations; decreased fibrinogen, significant prolongation of PT/international normalized ratio, or schistocytes are not frequently seen. A recent report by Panigada et al92 supports the discrepancy of these claims through thromboelastography (TEG). The analysis included 24 patients who collectively demonstrated a hypercoagulable state by TEG parameters. Factor VIII and vWF levels are markedly elevated in COVID-19, reflective of endothelial dysfunction and hypercoagulability.86,92 Elevated d-dimer in COVID-19 levels also reflects hyperfibrinolysis. A retrospective trial by Tang et al93 showed that antithrombin and fibrinogen levels were significantly lower in nonsurvivors.
Excessive complement activation likely contributes to the thrombogenic state in COVID-19 (Figure 4). Mannose-binding lectin (MBL) complement pathway binds to SARS-CoV spike glycoprotein, leading to initiation of the lectin pathways through MBL-associated serine protease-2 (MASP-2) activation.94
Murine models have demonstrated that C3-deficient mice and C5a inhibition led to decreased localized inflammation and lung damage in SARS-CoV infection.95 A recently published case series aimed to evaluate the contribution of the complement system in 2 subsets of COVID-19 patients with lung and skin manifestations.96 The primary histologic findings in examined lung tissues were septal capillary injury, microthrombosis associated with extensive deposits of the terminal complement complex C5b-9, as well as C4d and MASP2.96 In the 3 patients with retiform and purpuric skin lesions, a similar pattern of the microvascular-associated complement of deposition was noted.96
To date, there have also been several case reports, case series, and retrospective analyses published in the literature of the thrombotic manifestations in COVID-19, including microthrombi, DVT, pulmonary embolism, myocardial infarction, and strokes. Klok et al97 reported a 27% (95% CI: 17-37) VTE incidence and 3.7% arterial vascular events in critically ill patients with COVID-19. Tang et al93 also reported a similar incidence of VTE.
The procoagulant pathways highlighted in immunothrombosis (Figure 4) in concert appear to overwhelm the balance of hemostasis and result in microthrombi and overt thrombus formation. Microthrombosis appears to be the more frequent finding in COVID-19, compared to VTE or arterial thrombosis. The factors that dictate the occurrence of macrothrombosis in individual patients are unclear and likely multifactorial. Factors such as genetics, underlying comorbidities, immobility, cytokine storm, and viral load are inclined to play a role in that determination.
Conclusion
COVID-associated coagulopathy exemplifies the potentiating interactions between the immune system and the coagulation pathway. A procoagulant state in COVID-19 is the result of a direct viral-related endothelial injury, leukocyte- and cytokine-mediated platelet activation, TF release, and NETosis augmented by an unchecked activation of the complement system. Aberrant activation of the immune system during SARS-CoV viral infection leads to unregulated thrombosis, presenting with widespread microthrombi, as well as manifestations of VTE and arterial events.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Apoorva Jayarangaiah  https://orcid.org/0000-0002-9692-7841
https://orcid.org/0000-0002-9692-7841
Abhishek Kumar  https://orcid.org/0000-0001-9617-3579
https://orcid.org/0000-0001-9617-3579
References
- 1. Munster VJ, Koopmans M, Doremalen NV, Riel DV, Wit ED. A novel coronavirus emerging in China—key questions for impact assessment. N Eng J Med. 2020;382(8):692–694. doi:10.1056/nejmp2000929 [DOI] [PubMed] [Google Scholar]
- 2. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi:10.1016/s0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Engelmann B, Massberg S. Thrombosis as an intravascular effector of innate immunity. Nat Rev Immunol. 2012;13(1):34–45. doi:10.1038/nri3345 [DOI] [PubMed] [Google Scholar]
- 4. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061 doi:10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi:10.1016/s0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cao Y-C, Deng Q-X, Dai S-X. Remdesivir for severe acute respiratory syndrome coronavirus 2 causing COVID-19: an evaluation of the evidence. Travel Med Infect Dis. 2020;35:101647 doi:10.1016/j.tmaid.2020.101647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chen G, Wu D, Guo W, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130(5):2620-2629. doi:10.1172/JCI137244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Xu X, Gao X. Immunological responses against SARS-coronavirus infection in humans. Cell Mol Immunol. 2004;1(2):119-122. [PubMed] [Google Scholar]
- 9. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China [published online ahead of print, Mar 3, 2020] [published correction appears in Intensive Care Med. Apr 6, 2020]. Intensive Care Med. 2020;1-3. doi:10.1007/s00134-020-05991-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Terpos E, Ntanasis-Stathopoulos I, Elalamy I, et al. Hematological findings and complications of COVID-19 [published online ahead of print, Apr 13, 2020]. Am J Hematol. 2020. doi:10.1002/ajh.25829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145-148. doi:10.1016/j.cca.2020.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tan L, Wang Q, Zhang D, et al. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct Target Ther. 2020;5(1):33 doi:10.1038/s41392-020-0148-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lippi G, Favaloro EJ. d-Dimer is associated with severity of coronavirus disease 2019: a pooled analysis [published online ahead of print, Apr 3, 2020]. Thromb Haemost. 2020. doi:10.1055/s-0040-1709650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study [published correction appears in Lancet. 2020;395(10229):1038]. Lancet. 2020;395(10229):1054-1062. doi:10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Han H, Yang L, Liu R, et al. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin Chem Lab Med. 2020;58(7):1116–1120. doi:10.1515/cclm-2020-0188 [DOI] [PubMed] [Google Scholar]
- 16. Lillicrap D. Disseminated intravascular coagulation in patients with 2019-nCoV pneumonia. J Thromb Haemost. 2020;18(4):786-787. doi:10.1111/jth.14781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Furie B, Furie BC. Mechanisms of thrombus formation. N Engl J Med. 2008;359(9):938-949. doi:10.1056/NEJMra0801082 [DOI] [PubMed] [Google Scholar]
- 18. Dubois C, Panicot-Dubois L, Merrill-Skoloff G, Furie B, Furie BC. Glycoprotein VI-dependent and -independent pathways of thrombus formation in vivo. Blood. 2006;107(10):3902-3906. doi:10.1182/blood-2005-09-3687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Davì G, Patrono C. Platelet activation and atherothrombosis. N Engl J Med. 2007;357(24):2482-2494. doi:10.1056/NEJMra071014 [DOI] [PubMed] [Google Scholar]
- 20. Weisel JW. Fibrinogen and fibrin. Adv Protein Chem. 2005;70:247-299. doi:10.1016/S0065-3233(05)70008-5 [DOI] [PubMed] [Google Scholar]
- 21. Loof TG, Mörgelin M, Johansson L, et al. Coagulation, an ancestral serine protease cascade, exerts a novel function in early immune defense. Blood. 2011;118(9):2589-2598. doi:10.1182/blood-2011-02-337568 [DOI] [PubMed] [Google Scholar]
- 22. Ito T. PAMPs and DAMPs as triggers for DIC. J Intensive Care. 2014;2(1):67 doi:10.1186/s40560-014-0065-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Esmon CT. The interactions between inflammation and coagulation. Br J Haematol. 2005;131(4):417-430. doi:10.1111/j.1365-2141.2005.05753.x [DOI] [PubMed] [Google Scholar]
- 24. Palankar R, Greinacher A. Challenging the concept of immunothrombosis. Blood. 2019;133(6):508-509. doi:10.1182/blood-2018-11-886267 [DOI] [PubMed] [Google Scholar]
- 25. Budnik I, Brill A. Immune factors in deep vein thrombosis initiation. Trends Immunol. 2018;39(8):610-623. doi:10.1016/j.it.2018.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. von Brühl ML, Stark K, Steinhart A, et al. Monocytes, neutrophils, and platelets cooperate to initiate and propagate venous thrombosis in mice in vivo. J Exp Med. 2012;209(4):819-835. doi:10.1084/jem.20112322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Swystun LL, Liaw PC. The role of leukocytes in thrombosis. Blood. 2016;128(6):753-762. doi:10.1182/blood-2016-05-718114 [DOI] [PubMed] [Google Scholar]
- 28. Lentz BR. Exposure of platelet membrane phosphatidylserine regulates blood coagulation. Prog Lipid Res. 2003;42(5):423-438. doi:10.1016/s0163-7827(03)00025-0 [DOI] [PubMed] [Google Scholar]
- 29. Gaertner F, Massberg S. Blood coagulation in immunothrombosis—at the frontline of intravascular immunity. Semin Immunol. 2016;28(6):561-569. doi:10.1016/j.smim.2016.10.010 [DOI] [PubMed] [Google Scholar]
- 30. Yeaman MR. Platelets in defense against bacterial pathogens. Cell Mol Life Sci. 2010;67(4):525-544. doi:10.1007/s00018-009-0210-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Semple JW, Italiano JE, Jr, Freedman J. Platelets and the immune continuum. Nat Rev Immunol. 2011;11(4):264-274. doi:10.1038/nri2956 [DOI] [PubMed] [Google Scholar]
- 32. Zimmerman GA, McIntyre TM, Prescott SM, Stafforini DM. The platelet-activating factor signaling system and its regulators in syndromes of inflammation and thrombosis. Crit Care Med. 2002;30(5 suppl):S294-S301. doi:10.1097/00003246-200205001-00020 [DOI] [PubMed] [Google Scholar]
- 33. Hu H, Varon D, Hjemdahl P, et al. Platelet–leukocyte aggregation under shear stress: differential involvement of selectins and integrins. Thromb Haemost. 2003;90(4):679-687. doi:10.1160/TH03-05-0274 [DOI] [PubMed] [Google Scholar]
- 34. Rinder HM, Bonan JL, Rinder CS, Ault KA, Smith BR. Dynamics of leukocyte–platelet adhesion in whole blood. Blood. 1991;78(7):1730-1737. [PubMed] [Google Scholar]
- 35. Yan SL, Russell J, Granger DN. Platelet activation and platelet–leukocyte aggregation elicited in experimental colitis are mediated by interleukin-6. Inflamm Bowel Dis. 2014;20(2):353-362. doi:10.1097/01.MIB.0000440614.83703.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Niemetz J. Coagulant activity of leukocytes. Tissue factor activity. J Clin Invest. 1972;51(2):307-313. doi:10.1172/JCI106815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Furie B, Flaumenhaft R. Thiol isomerases in thrombus formation. Circ Res. 2014;114(7):1162-1173. doi:10.1161/CIRCRESAHA.114.301808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Carta S, Castellani P, Delfino L, et al. DAMPs and inflammatory processes: the role of redox in the different outcomes. J Leukoc Biol. 2009;86(3):549-555. doi:10.1189/jlb.1008598 [DOI] [PubMed] [Google Scholar]
- 39. Falati S, Liu Q, Gross P, et al. Accumulation of tissue factor into developing thrombi in vivo is dependent upon microparticle P-selectin glycoprotein ligand 1 and platelet P-selectin. J Exp Med. 2003;197(11):1585-1598. doi:10.1084/jem.20021868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wolberg AS, Monroe DM, Roberts HR, Hoffman MR. Tissue factor de-encryption: ionophore treatment induces changes in tissue factor activity by phosphatidylserine-dependent and -independent mechanisms. Blood Coagul Fibrinol. 1999;10(4):201-210. [PubMed] [Google Scholar]
- 41. Shantsila E, Lip GY. The role of monocytes in thrombotic disorders. Insights from tissue factor, monocyte–platelet aggregates and novel mechanisms. Thromb Haemost. 2009;102(5):916-924. doi:10.1160/TH09-01-0023 [DOI] [PubMed] [Google Scholar]
- 42. Zwicker JI, Trenor CC, III, Furie BC, Furie B. Tissue factor-bearing microparticles and thrombus formation. Arterioscler Thromb Vasc Biol. 2011;31(4):728-733. doi:10.1161/ATVBAHA.109.200964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Maugeri N, Brambilla M, Camera M, et al. Human polymorphonuclear leukocytes produce and express functional tissue factor upon stimulation. J Thromb Haemost. 2006;4(6):1323-1330. doi:10.1111/j.1538-7836.2006.01968.x [DOI] [PubMed] [Google Scholar]
- 44. Moosbauer C, Morgenstern E, Cuvelier SL, et al. Eosinophils are a major intravascular location for tissue factor storage and exposure. Blood. 2007;109(3):995-1002. doi:10.1182/blood-2006-02-004945 [DOI] [PubMed] [Google Scholar]
- 45. Massberg S, Grahl L, von Bruehl ML, et al. Reciprocal coupling of coagulation and innate immunity via neutrophil serine proteases. Nat Med. 2010;16(8):887-896. doi:10.1038/nm.2184 [DOI] [PubMed] [Google Scholar]
- 46. Fuchs TA, Brill A, Duerschmied D, et al. Extracellular DNA traps promote thrombosis. Proc Natl Acad Sci U S A. 2010;107(36):15880-15885. doi:10.1073/pnas.1005743107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Martinod K, Wagner DD. Thrombosis: tangled up in NETs. Blood. 2014;123(18):2768-2776. doi:10.1182/blood-2013-10-463646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Takano S, Kimura S, Ohdama S, Aoki N. Plasma thrombomodulin in health and diseases. Blood. 1990;76(10):2024-2029. [PubMed] [Google Scholar]
- 49. Barranco-Medina S, Pozzi N, Vogt AD, Di Cera E. Histone H4 promotes prothrombin autoactivation. J Biol Chem. 2013;288(50):35749-35757. doi:10.1074/jbc.M113.509786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gould TJ, Vu TT, Swystun LL, et al. Neutrophil extracellular traps promote thrombin generation through platelet-dependent and platelet-independent mechanisms. Arterioscler Thromb Vasc Biol. 2014;34(9):1977-1984. doi:10.1161/ATVBAHA.114.304114 [DOI] [PubMed] [Google Scholar]
- 51. Levi M, Schultz M, van der Poll T. Sepsis and thrombosis. Semin Thromb Hemost. 2013;39(5):559-566. doi:10.1055/s-0033-1343894 [DOI] [PubMed] [Google Scholar]
- 52. Nawroth PP, Stern DM. Modulation of endothelial cell hemostatic properties by tumor necrosis factor. J Exp Med. 1986;163(3):740-745. doi:10.1084/jem.163.3.740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Seitz R, Wolf M, Egbring R, Havemann K. The disturbance of hemostasis in septic shock: role of neutrophil elastase and thrombin, effects of antithrombin III and plasma substitution. Eur J Haematol. 1989;43(1):22-28. doi:10.1111/j.1600-0609.1989.tb01246.x [DOI] [PubMed] [Google Scholar]
- 54. Opal SM, Kessler CM, Roemisch J, Knaub S. Antithrombin, heparin, and heparan sulfate. Crit Care Med. 2002;30(5 suppl):S325-S331. doi:10.1097/00003246-200205001-00024 [DOI] [PubMed] [Google Scholar]
- 55. Eckle I, Seitz R, Egbring R, Kolb G, Havemann K. Protein C degradation in vitro by neutrophil elastase. Biol Chem Hoppe Seyler. 1991;372(11):1007-1013. doi:10.1515/bchm3.1991.372.2.1007 [DOI] [PubMed] [Google Scholar]
- 56. Gando S, Kameue T, Morimoto Y, et al. Tissue factor production not balanced by tissue factor pathway inhibitor in sepsis promotes poor prognosis. Crit Care Med. 2002;30(8):1729-1734. doi:10.1097/00003246-200208000-00009 [DOI] [PubMed] [Google Scholar]
- 57. Levi M. The imbalance between tissue factor and tissue factor pathway inhibitor in sepsis. Crit Care Med. 2002;30(8):1914-1915. doi:10.1097/00003246-200208000-00046 [DOI] [PubMed] [Google Scholar]
- 58. Dosquet C, Weill D, Wautier JL. Cytokines and thrombosis. J Cardiovasc Pharmacol. 1995;25(suppl 2):S13-S19. doi:10.1097/00005344-199500252-00004 [DOI] [PubMed] [Google Scholar]
- 59. McIntyre TM. Inflammatory cytokines and thrombosis. Blood. 2012;120(21):SCI–44. doi:10.1182/blood.V120.21.SCI-44.SCI-44 [Google Scholar]
- 60. Nan B, Lin P, Lumsden AB, Yao Q, Chen C. Effects of TNF-alpha and curcumin on the expression of thrombomodulin and endothelial protein C receptor in human endothelial cells. Thromb Res. 2005;115(5):417-426. doi:10.1016/j.thromres.2004.10.010 [DOI] [PubMed] [Google Scholar]
- 61. Bester J, Pretorius E. Effects of IL-1β, IL-6 and IL-8 on erythrocytes, platelets and clot viscoelasticity. Sci Rep. 2016;6:32188 doi:10.1038/srep32188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Joseph L, Fink LM, Hauer-Jensen M. Cytokines in coagulation and thrombosis: a preclinical and clinical review. Blood Coagul Fibrinolysis. 2002;13(2):105-116. doi:10.1097/00001721-200203000-00005 [DOI] [PubMed] [Google Scholar]
- 63. Beckers MM, Ruven HJ, Haas FJ, et al. Single nucleotide polymorphisms in inflammation-related genes are associated with venous thromboembolism. Eur J Intern Med. 2010;21(4):289-292. doi:10.1016/j.ejim.2010.04.001 [DOI] [PubMed] [Google Scholar]
- 64. Liu H, Yang Y, Jiang J, et al. Coexistence of a huge venous thromboembolism and bleeding tendency in cytokine release syndrome during CAR-T therapy. Onco Targets Ther. 2019;12:8955-8960. doi:10.2147/OTT.S223697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Cox D, Kerrigan SW, Watson SP. Platelets and the innate immune system: mechanisms of bacterial-induced platelet activation. J Thromb Haemost. 2011;9(6):1097-1107. doi:10.1111/j.1538-7836.2011.04264.x [DOI] [PubMed] [Google Scholar]
- 66. Beristain-Covarrubias N, Perez-Toledo M, Thomas MR, et al. Understanding infection-induced thrombosis: lessons learned from animal models. Front Immunol. 2019;10:2569 doi:10.3389/fimmu.2019.02569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Yang Y, Tang H. Aberrant coagulation causes a hyper-inflammatory response in severe influenza pneumonia. Cell Mol Immunol. 2016;13(4):432-442. doi:10.1038/cmi.2016.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Visseren FL, Bouwman JJ, Bouter KP, et al. Procoagulant activity of endothelial cells after infection with respiratory viruses. Thromb Haemost. 2000;84(2):319-324. [PubMed] [Google Scholar]
- 69. Goeijenbier M, van Wissen M, van de Weg C, et al. Review: viral infections and mechanisms of thrombosis and bleeding. J Med Virol. 2012;84(10):1680-1696. doi:10.1002/jmv.23354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Koupenova M, Vitseva O, MacKay CR, et al. Platelet-TLR7 mediates host survival and platelet count during viral infection in the absence of platelet-dependent thrombosis. Blood. 2014;124(5):791-802. doi:10.1182/blood-2013-11-536003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Markiewski MM, Nilsson B, Ekdahl KN, Mollnes TE, Lambris JD. Complement and coagulation: strangers or partners in crime? Trends Immunol. 2007;28(4):184-192. doi:10.1016/j.it.2007.02.006 [DOI] [PubMed] [Google Scholar]
- 72. Esmon CT. The impact of the inflammatory response on coagulation. Thromb Res. 2004;114(5-6):321-327. doi:10.1016/j.thromres.2004.06.028 [DOI] [PubMed] [Google Scholar]
- 73. Wojta J, Kaun C, Zorn G, et al. C5a stimulates production of plasminogen activator inhibitor-1 in human mast cells and basophils. Blood. 2002;100(2):517-523. doi:10.1182/blood.v100.2.517 [DOI] [PubMed] [Google Scholar]
- 74. Wong EKS, Kavanagh D. Diseases of complement dysregulation—an overview. Semin Immunopathol. 2018;40(1):49-64. doi:10.1007/s00281-017-0663-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Davalos D, Akassoglou K. Fibrinogen as a key regulator of inflammation in disease. Semin Immunopathol. 2012;34(1):43-62. doi:10.1007/s00281-011-0290-8 [DOI] [PubMed] [Google Scholar]
- 76. Frantzeskaki F, Armaganidis A, Orfanos SE. Immunothrombosis in acute respiratory distress syndrome: cross talks between inflammation and coagulation. Respiration. 2017;93(3):212-225. doi:10.1159/000453002 [DOI] [PubMed] [Google Scholar]
- 77. Pfeiler S, Massberg S, Engelmann B. Biological basis and pathological relevance of microvascular thrombosis. Thromb Res. 2014;133(suppl 1):S35-S37. doi:10.1016/j.thromres.2014.03.016 [DOI] [PubMed] [Google Scholar]
- 78. Ait-Oufella H, Taleb S, Mallat Z, Tedgui A. Recent advances on the role of cytokines in atherosclerosis. Arterioscler Thromb Vasc Biol. 2011;31(5):969-979. doi:10.1161/ATVBAHA.110.207415 [DOI] [PubMed] [Google Scholar]
- 79. Kariyanna PT, Naseem HA, Jayarangaiah A, et al. Pharmaco-invasive therapy for STEMI in a patient with COVID-19. Am J Case Rep. 2020;8(7):192–196. doi:10.12691/ajmcr-8-7-9 [Google Scholar]
- 80. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-733. doi:10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271-280.e8. doi:10.1016/j.cell.2020.02.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Imai Y, Kuba K, Rao S, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436(7047):112-116. doi:10.1038/nature03712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Oudit GY, Kassiri Z, Jiang C, et al. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009;39(7):618-625. doi:10.1111/j.1365-2362.2009.02153.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Liu PP, Blet A, Smyth D, Li H. The science underlying COVID-19: implications for the cardiovascular system [published online ahead of print, Apr 15, 2020] Circulation. 2020. doi:10.1161/CIRCULATIONAHA.120.047549 [DOI] [PubMed] [Google Scholar]
- 85. Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417-1418. doi:10.1016/S0140-6736(20)30937-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Escher R, Breakey N, Lämmle B. Severe COVID-19 infection associated with endothelial activation. Thromb Res. 2020;190:62 doi:10.1016/j.thromres.2020.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Moore JB, June CH. Cytokine release syndrome in severe COVID-19. Science. 2020;368(6490):473-474. doi:10.1126/science.abb8925 [DOI] [PubMed] [Google Scholar]
- 88. Wong RS, Wu A, To KF, et al. Haematological manifestations in patients with severe acute respiratory syndrome: retrospective analysis. BMJ. 2003;326(7403):1358-1362. doi:10.1136/bmj.326.7403.1358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Fox SE, Akmatbekov A, Harbert JL, et al. Pulmonary and cardiac pathology in Covid-19: the first autopsy series from New Orleans [published online ahead of print, April 10, 2020]. medRxiv. 2020. doi:10.1101/2020.04.06.20050575 [Google Scholar]
- 90. Barnes BJ, Adrover JM, Baxter-Stoltzfus A, et al. Targeting potential drivers of COVID-19: neutrophil extracellular traps. J Exp Med. 2020;217(6):e20200652 doi:10.1084/jem.20200652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Zuo Y, Yalavarthi S, Shi H, et al. Neutrophil extracellular traps in COVID-19 [published online ahead of print, Apr 24, 2020]. JCI Insight. 2020. doi:10.1172/jci.insight.138999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID-19 patients in intensive care unit. A report of thromboelastography findings and other parameters of hemostasis [published online ahead of print, Apr 17, 2020]. J Thromb Haemost. 2020. doi:10.1111/jth.14850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844-847. doi:10.1111/jth.14768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Gao T, Hu M, Zhang X, et al. Highly pathogenic coronavirus N protein aggravates lung injury by MASP-2-mediated complement over-activation. MedRxiv. 2020. doi:10.1101/2020.03.29.20041962 [Google Scholar]
- 95. Wilk CM. Coronaviruses hijack the complement system [published online ahead of print, Apr 14, 2020]. Nat Rev Immunol. 2020 doi:10.1038/s41577-020-0314-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Magro C, Mulvey JJ, Berlin D, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1–13. doi:10.1016/j.trsl.2020.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19 Thromb Res. 2020;191:145–147. doi:10.1016/j.thromres.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]