Abstract
Background:
The Patient Protection Affordable Care Act has expanded Medicaid eligibility in recent years. However, the provisions of the act have not translated to improved Medicaid payments for specialists such as orthopaedic surgeons. The number of health care practitioners who accept Medicaid is already decreasing, with low reimbursement rates being cited as the primary reason for the trend.
Hypothesis:
Private practice orthopaedic groups will see patients with Medicaid or Medicare at lower rates than academic orthopaedic practices, and business days until appointment availability will be higher for patients with Medicaid and Medicare than those with private insurance.
Study Design:
Cross-sectional study.
Methods:
Researchers made calls to 2 regular-sized orthopaedic practices, 1 small orthopaedic practice, and 1 academic orthopaedic practice in each of the 50 states in the United States. Callers described a scenario of a recent injury resulting in a bucket-handle meniscal tear and an anterior cruciate ligament tear seen on magnetic resonance imaging at an outside emergency department. For a total of 194 practices, 3 separate telephone calls were made, each with a different insurance type. Data regarding insurance acceptance and business days until appointment were tabulated. Student t tests or analysis of variance for continuous data and χ2 or Fisher exact tests for categorical data were utilized.
Results:
After completing 582 telephone calls, it was determined that 31.4% (n = 59) did not accept Medicaid, compared with 2.2% (n = 4) not accepting Medicare and 1% (n = 1) not accepting private insurance (P < .001). There was no significant association between type of practice and Medicaid refusal (P = 0.12). Mean business days until appointment for Medicaid, Medicare, and private insurance were 5.3, 4.1, and 2.9, respectively (P < .001).
Conclusions:
Access to care remains a significant burden for the Medicaid population, given a rate of Medicaid refusal of 32.2% across regular-sized orthopaedic practices. If Medicaid is accepted, time until appointment was significantly longer when compared with private insurance.
Keywords: knee, ACL, meniscus, epidemiology, insurance, Medicaid
Socioeconomic factors have always been an important part of many fields of medicine. Studies1,14,22,32 have repeatedly shown that low socioeconomic status is a risk factor for everything from trauma to chronic kidney disease and diabetes. Patients with lower socioeconomic status face higher mortality rates when compared with those with higher socioeconomic status.12
Patients with Medicaid were found to have high infection and complication rates after spine surgery.15,25 Medicaid patients also have a high 30-day readmission rate in orthopaedics.6
The Patient Protection Affordable Care Act (PPACA) has expanded Medicaid eligibility in recent years.18 However, the provisions of the act that improved Medicaid payments for primary care physicians have not translated to improved Medicaid payments for specialists such as orthopaedic surgeons.18 This is unfortunate in a time when the number of Medicaid-accepting health care practitioners is already decreasing, with low reimbursement rates being cited as the primary reason for the trend.10,16,28 In a study by Kim et al,20 it was shown that Medicaid patients could schedule an appointment only 20% of the time compared with 89% for Medicare and 97% for Blue Cross Blue Shield. Patients with Medicaid had similar difficulties in getting an appointment for knee arthroplasty, and when they did obtain an appointment, they had longer waiting periods compared with those covered by Medicare or private insurance.18 Medicaid patients were found to need more referrals and have longer waiting periods in addition to fewer successful appointments for foot and ankle care when compared with Medicare and private insurance patients.19 Finally, while this study was completed before the PPACA, it was found that children with Medicaid insurance had limited access or no access to orthopaedic care in 38% of offices nationwide.30 They reported a statistically significant relationship between access to care for Medicaid patients and physician reimbursement rates.30
Common sports injuries, including those to the anterior cruciate ligament (ACL), have a better outcome when diagnosed and treated early. Patients with ACL injuries that have been delayed for more than 6 months have an increased medial meniscal tear rate.4 In addition, early ACL reconstruction results in decreased knee instability episodes and better long-term results than delayed reconstruction.11
Bucket-handle meniscal tears are another common injury in sports and can be seen combined with ACL tears. These particular meniscal tears result in significant patient disability because of symptoms such as locking and catching.31 Sood et al31 found that noninsured patients experienced delay to surgery for their bucket-handle meniscal tears. They also found that bucket-handle meniscal tears have a decreased rate of repairability as time from injury increased. Owing to the urgency for immediate treatment of certain sports injuries, access to care is very important for better long-term outcomes. The purpose of this study was to explore Medicaid patients’ access to sports medicine orthopaedic care after the passing of the PPACA.
Methods
We organized a nationwide survey of orthopaedic sports providers by searching for 4 offices with board-certified orthopaedic sports surgeons from each state. The search criteria “Orthopedic Sports Surgeon (State)” was used in Google Maps. A list of available practices was generated and subsequently randomized in Microsoft Excel. After randomization, the first 2 regular-sized orthopaedic practices, the first small orthopaedic practice, and the first academic orthopaedic practice in each of all 50 states from the United States were chosen to be included in the survey. A small orthopaedic practice was defined as a physician group of ≤3 physicians. A regular-sized practice was defined as a physician group of ≥4 physicians. An academic practice was defined as an orthopaedic practice attached to a medical university. In certain states, such as Alaska and North Dakota, no academic orthopaedic sports program exists, and so an academic practice was not included from these states. If a clinic was unable to be contacted, then the next office in the list that was congruent with the particular type of practice was called.
Researchers made telephone calls to these practices describing a scenario of a recent soccer injury resulting in an “ACL tear with a bucket-handle meniscal tear” seen on magnetic resonance imaging (MRI) at an outside emergency department and were ordered by the outside emergency department to follow-up with an orthopaedic sports surgeon. If asked about their symptoms, callers were to reply that symptoms were progressing. If asked about imaging, callers were to reply that the MRI was obtained and available on a disk. Three separate telephone calls with 3 separate patient scenarios were made, 1 researcher claiming to be a patient having Medicaid, 1 claiming to have Medicare, and 1 claiming to have a form of private insurance. The private insurance was chosen as the largest private insurance provider in that particular state. Each researcher attempted to schedule an appointment, given their chosen form of insurance. If a patient concluded the call with a scheduled appointment, the caller was instructed to cancel the appointment in a later call so as to not interfere with the office scheduling system. If an appointment was refused, this was documented. Moreover, data were separated into Medicaid expansion states and non-Medicaid expansion states.17
The generalized estimating equation approach introduced by Liang and Zeger23 was used to analyze the insurance denial outcome and the business days until appointment outcome. This approach helps model the correlation among the 3 telephone calls made by the same researcher at each orthopaedic practice. Uni- and multivariable analyses were performed.
The analysis for the insurance denial outcome was implemented using the SAS GENMOD procedure (Version 9.4; SAS Institute) with an exchangeable correlation structure for the repeated telephone calls within researcher (binomial-logit model). The statistical model provided estimates of the percentages of practices that denied insurance (plus 95% CIs) for 2 predictors (type of insurance and type of orthopaedic practice). The model-based estimates were unbiased with unbalanced and missing data, as long as the missing data were noninformative (missing completely at random). The multivariable analysis simultaneously included the 2 predictors in the model. The outcome “business days until appointment” was also analyzed with the generalized estimation equation approach with an exchangeable correlation structure for the repeated telephone calls within researcher (normal distribution model). The statistical model provided estimates of mean business days until appointment (plus 95% CIs) for the 2 predictors.
Results
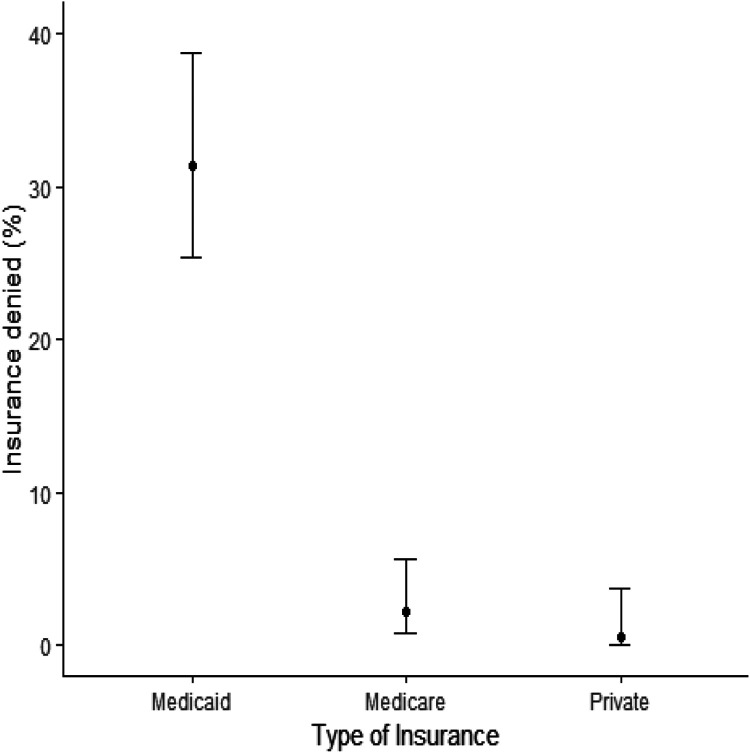
A total of 194 practices were called, and each practice was assessed regarding whether they accepted Medicaid, Medicare, and private insurance, for a total of 582 calls. Private insurance had the highest acceptance rate of 99.5%, followed by 97.8% acceptance by Medicare and 68.6% acceptance by Medicaid (Table 1, Figure 1). There was a significant difference in rejection for Medicaid patients compared with Medicare and private insurance patients (P < .001; Table 1). In addition, private insurance had the quickest turnaround regarding business days until the appointment at 2.9 days, followed by 4.1 days for Medicare and 5.3 days for Medicaid (Table 1) (P < .001). Academic practices accepted a significantly higher overall percentage of patients regardless of insurance (92.1%; P < .001), but also had the longest wait until the appointment (5.8 business days; P = .001) (Table 2). Last, in Medicaid expansion states, there was a similar percentage of Medicaid-accepted patients (65.5% in no expansion, 69.2% in expanded states; P = .61), along with a similar wait time to the appointment (5.2 days vs 5.4 days; P = .88) (Table 3).
Table 1.
Statistics by Type of Insurance
| Type of Insurance | |||||
|---|---|---|---|---|---|
| Overall (n = 582) | Medicaid (n = 194) | Medicare (n = 194) | Private (n = 194) | P | |
| Business days until appointmenta | 4.0 ± 5.7 | 5.3 ± 8.9 | 4.1 ± 4.3 | 2.9 ± 2.3 | <.001 |
| Accept insurance, n (%)b | |||||
| No | 64/562 (11.4) | 59/188 (31.4) | 4/186 (2.2) | 1/188 (0.5) | <.001 |
| Yes | 498/562 (88.6) | 129/188 (68.6) | 182/186 (97.8) | 187/188 (99.5) | |
aData are reported as mean ± SD business days until appointment.
bSeveral practices (n = 20) could not be reached despite repeat telephone calls and were therefore not included in the analysis.
Figure 1.
Percentage of insurance denial by type of insurance (N = 194 orthopaedic sports medicine practices). Error bars indicate CIs.
Table 2.
Statistics by Type of Practice
| Type of Practice | |||||
|---|---|---|---|---|---|
| Overall (n = 582) | Small (n = 150) | Regular (n = 300) | Academic (n = 132) | P | |
| Business days until appointmenta | 4.0 ± 5.7 | 4.1 ± 6.5 | 3.3 ± 3.9 | 5.8 ± 7.6 | .001 |
| Accept insurance, n (%)b | |||||
| No | 64/562 (11.4) | 13/143 (9.1) | 41/293 (14) | 10/126 (7.9) | .12 |
| Yes | 498/562 (88.6) | 130/143 (90.9) | 252/293 (86) | 116/126 (92.1) | |
aData are reported as mean ± SD business days until appointment.
bSeveral practices could not be reached despite repeat telephone calls and were therefore not included in the analysis.
Table 3.
Descriptive Statistics by Medicaid Expansion
| Medicaid Expansiona | ||||
|---|---|---|---|---|
| Overall (N = 194) | No (n = 55) | Yes (n = 136) | P | |
| Business days until appointmentb | 5.3 ± 8.9 | 5.2 ± 9.5 | 5.4 ± 8.9 | .88 |
| Accept insurance, n (%)c | ||||
| No | 59/188 (31.4) | 19/55 (34.5) | 40/130 (30.8) | .61 |
| Yes | 129/188 (68.6) | 36/55 (65.5) | 90/130 (69.2) | |
aStatus unknown for n = 3.
bData are reported as mean ± SD business days until appointment.
cSeveral practices could not be reached despite repeat telephone calls and were therefore not included in the analysis.
Further analysis shows that academic practices and small practices accepted a similar percentage of Medicaid patients (79% vs 72.9%, respectively) (Table 4). Regular-sized practices accepted a significantly lower amount of Medicaid patients compared with academic practices (61.2% vs 72.9%, respectively; P = .02) (Table 4). When looking at patients with Medicaid or private insurance, there was no statistically significant difference in the percentage of practices from each practice type that accepted these patients (Tables 5 and 6).
Table 4.
Descriptive Statistics by Type of Practice for Medicaid Insurance
| Type of Practice | ||||
|---|---|---|---|---|
| Accept Medicaid, n (%)a | Overall (N = 194) | Small (n = 50) | Regular (n = 100) | Academic (n = 44) |
| No | 59/188 (31.4) | 13/48 (27.1) | 38/98 (38.8) | 8/42 (19) |
| Yes | 129/188 (68.6) | 35/48 (72.9) | 60/98 (61.2) | 34/42 (81) |
aP (χ2 test) = .05.
Table 5.
Descriptive Statistics by Type of Practice for Medicare Insurance
| Type of Practice | ||||
|---|---|---|---|---|
| Accept Medicare, n (%)a | Overall (N = 194) | Small (n = 50) | Regular (n = 100) | Academic (n = 44) |
| No | 4/186 (2.2) | 0/47 (0) | 3/97 (3.1) | 1/42 (2.4) |
| Yes | 182/186 (97.8) | 47/47 (100) | 94/97 (96.9) | 41/42 (97.6) |
aP (χ2 test) = .48.
Table 6.
Descriptive Statistics by Type of Practice for Private Insurance
| Type of Practice | ||||
|---|---|---|---|---|
| Accept private insurance, n (%)a | Overall (N = 194) | Small (n = 50) | Regular (n = 100) | Academic (n = 44) |
| No | 1/188 (0.5) | 0/48 (0) | 0/98 (0) | 1/42 (2.4) |
| Yes | 187/188 (99.5) | 48/48 (100) | 98/98 (100) | 41/42 (97.6) |
aP (χ2 test) = .17.
Discussion
Access to care in orthopaedics, especially after the PPACA, has been a popular topic of discussion in orthopaedic research.13,18,29 This study sought to examine access to orthopaedic care for urgent sports medicine patients based on the insurance they possessed. In the literature, there was a similar study published in 2017 looking at access to care based on insurance.34 They found a similar result in that Medicaid patients had a harder time getting an appointment along with long wait times until an appointment.34 In addition, they found that the Medicaid expansion versus nonexpanded states did not have any significant difference in access to care.34
Multiple other studies2,21,26 have looked at access to care for orthopaedics among other subspecialties. A previous study35 showed that Medicaid patients with operative ankle fractures had similar difficulty scheduling an appointment. In addition, there was also no difference between Medicaid expansion and nonexpanded states.35 In a similar study conducted with regard to access to orthopaedic spine surgeons, patients with Medicare were unable to book appointments.29
Studies have shown that patients with low socioeconomic status have a negative disparity in their health.7,27 The purpose of Medicaid is to provide low-income patients with insurance,33 and while expanding Medicaid may provide some patients with insurance that they would otherwise lack, it fails to grant them equal access to care when compared to patients with other insurance types. Our study showed that fewer orthopaedic practices will schedule an appointment for a patient with Medicaid insurance and meniscal and ACL tears in comparison with the same patient with Medicare or private insurance, which suggests that patients with Medicaid may have to go through more trouble to get an appointment. While academic institutes accepted Medicaid patients more frequently, they also had the longest wait before the appointment. This study adds further data to the current literature that the Medicaid expansion certainly improved access to care for the previously uninsured but may not have equalized that access among different insurance types, showing that socioeconomically disadvantaged populations still have a ways to go.
Given documented delays in the first appointment scheduling date for patients indicating Medicaid payer status, our study raises the question as to whether delays in appointment time have a significant clinical effect. Without doubt, delay in treatment time affects clinical outcomes, particularly with regard to ACL injuries.3,11 Early operative intervention, as defined by Dunn et al11 as surgery within 6 weeks of injury, faired variably with regard to reduction in knee instability and a hastened return to preinjury activity level. Our study demonstrated a mean time of 5.3 days to appointment for patients with Medicaid and a mean time of 2.9 days to appointment for patients with private practice insurance options, representing a mean difference of 2.4 days. Although unlikely that a time difference of 2-3 days will have clinical significance, additional research is needed to ascertain whether this difference of several days in time to evaluation would ultimately negatively affect clinical outcome. While this time difference may represent only a minor clinically relevant statistic, our study did not evaluate downstream delays to operative intervention in patients reporting Medicaid payer status. It is reasonable to assume that delays would not be limited to only time of initial appointment, but also to time of reconstructive procedure as well as time to access postoperative adjuncts such as physical therapy. This would require additional research, as our study did not focus on any future delays in care.
The results of this study necessitate discussion regarding why private orthopaedic sports medicine practices generally prefer patients with private insurance payer status rather than patients with Medicaid payer status. Without doubt, Medicaid reimbursement rates for common orthopaedic surgical procedures are not consistent across state lines.8 Rates can be as low as 20.6% of Medicare reimbursement rates.8 In an economic environment where maintaining a privately functioning orthopaedic surgical practice is becoming increasingly difficult,24 perhaps surgeons are reticent to take a financial risk, given the inconsistency in Medicaid payments. Our study demonstrates higher acceptance rates of Medicaid payer status in smaller orthopaedic surgical practices, with 72.9% of these practices accepting patients with Medicaid versus 61.2% of regular-sized orthopaedic groups. These data may indicate that smaller practices may be struggling for a market share, lacking the ability for widespread marketing and a larger network of referrals; thus, there may be more willingness to accept any insurance type. If this trend negatively affects their reimbursements, then they may be forced out of the market. On the other hand, increasing malpractice litigation9 against orthopaedic surgeons over the past 3 decades has caused rising malpractice insurance costs, which may be burdensome to smaller-sized practices. A general perception that patients with Medicaid status will be more likely to pursue malpractice lawsuits exists.5 However, this idea is not borne out in the available literature, with documented rates of litigation being identical across insurance payer statuses.5
There are some limitations to this study. First, an academic center was not able to be reached in all states. Second, there is a similar study on access to orthopaedic sports medicine surgeons.34 However, the current study expands on some very important categories. This study compares different types of practices. In addition, we also have surveyed the entire country comparing Medicaid expansion and nonexpansion states. These subcategories help to counsel patients with Medicaid about which type of practice is most likely to accept their insurance.
Conclusion
This study investigated access to an orthopaedic sports medicine surgeon based on the patient’s insurance and type of orthopaedic practice. The results of this study support the investigator’s hypothesis that there is still a significant barrier to orthopaedic care for Medicaid patients with ACL injuries. This manifests most prominently as refusal of care because of insurance type. Though academic institutions more readily accept Medicaid patients, the disparity should alert orthopaedic surgeons to the barriers that still remain after Medicaid expansion.
ACKNOWLEDGMENT
The authors acknowledge Yunyun Chen for his work on the statistical analysis related to this study.
Footnotes
Final revision submitted February 17, 2020; accepted February 27, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: K.E.H. has received research and educational support from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Abedzadeh-Kalahroudi M, Razi E, Sehat M. The relationship between socioeconomic status and trauma outcomes. J Public Health (Oxf). 2018;40(4):e431–e439. [DOI] [PubMed] [Google Scholar]
- 2. Al-Refaie WB, Zheng C, Jindal M, et al. Did pre-Affordable Care Act Medicaid expansion increase access to surgical cancer care? J Am Coll Surg. 2017;224(4):662–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(2):275–281. [DOI] [PubMed] [Google Scholar]
- 4. Arastu MH, Grange S, Twyman R. Prevalence and consequences of delayed diagnosis of anterior cruciate ligament ruptures. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1201–1205. [DOI] [PubMed] [Google Scholar]
- 5. Baldwin LM, Greer T, Wu R, et al. Differences in the obstetric malpractice claims filed by Medicaid and non-Medicaid patients. J Am Board Fam Pract. 1992;5(6):623–627. [PubMed] [Google Scholar]
- 6. Bernatz JT, Tueting JL, Anderson PA. Thirty-day readmission rates in orthopedics: a systematic review and meta-analysis. PLoS One. 2015;10(4):e0123593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Calixto OJ, Anaya JM. Socioeconomic status. The relationship with health and autoimmune diseases. Autoimmun Rev. 2014;13(6):641–654. [DOI] [PubMed] [Google Scholar]
- 8. Casper DS, Schroeder GD, Zmistowski B, et al. Medicaid reimbursement for common orthopedic procedures is not consistent. Orthopedics. 2019;42(2):e193–e196. [DOI] [PubMed] [Google Scholar]
- 9. Cichos KH, Ewing MA, Sheppard ED, et al. Trends and risk factors in orthopedic lawsuits: analysis of a National Legal Database. Orthopedics. 2019;42(2):e260–e267. [DOI] [PubMed] [Google Scholar]
- 10. Decker SL. In 2011 nearly one-third of physicians said they would not accept new Medicaid patients, but rising fees may help. Health Aff (Millwood). 2012;31(8):1673–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dunn KL, Lam KC, Valovich McLeod TC. Early operative versus delayed or nonoperative treatment of anterior cruciate ligament injuries in pediatric patients. J Athl Train. 2016;51(5):425–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Feinstein JS. The relationship between socioeconomic status and health: a review of the literature. Milbank Q. 1993;71(2):279–322. [PubMed] [Google Scholar]
- 13. Froelich JM, Beck R, Novicoff WM, Saleh KJ. Effect of health insurance type on access to care. Orthopedics. 2013;36(10): e1272–1276. [DOI] [PubMed] [Google Scholar]
- 14. Global Burden of Metabolic Risk Factors for Chronic Diseases C. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol. 2014;2(8):634–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hacquebord J, Cizik AM, Malempati SH, et al. Medicaid status is associated with higher complication rates after spine surgery. Spine (Phila Pa 1976). 2013;38(16):1393–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hinman A, Bozic KJ. Impact of payer type on resource utilization, outcomes and access to care in total hip arthroplasty. J Arthroplasty. 2008;23(6)(suppl 1):9–14. [DOI] [PubMed] [Google Scholar]
- 17. Kaiser. Kaiser Family Foundation. Status of State Medicaid Expansion. Kaiser Family Foundation; https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/. Updated 2019.2018. [Google Scholar]
- 18. Kim CY, Wiznia DH, Hsiang WR, Pelker RR. The effect of insurance type on patient access to knee arthroplasty and revision under the Affordable Care Act. J Arthroplasty. 2015;30(9):1498–1501. [DOI] [PubMed] [Google Scholar]
- 19. Kim CY, Wiznia DH, Roth AS, Walls RJ, Pelker RR. Survey of patient insurance status on access to specialty foot and ankle care under the Affordable Care Act. Foot Ankle Int. 2016;37(7):776–781. [DOI] [PubMed] [Google Scholar]
- 20. Kim CY, Wiznia DH, Wang Y, et al. The effect of insurance type on patient access to carpal tunnel release under the Affordable Care Act. J Hand Surg Am. 2016;41(4):503–509, e501. [DOI] [PubMed] [Google Scholar]
- 21. Kirchner GE, Rivers NJ, Balogh EF, et al. Does Medicaid expansion improve access to care for the first-time shoulder dislocator? J Shoulder Elbow Surg. 2019;28(11):2079–2083. [DOI] [PubMed] [Google Scholar]
- 22. Leng B, Jin Y, Li G, Chen L, Jin N. Socioeconomic status and hypertension: a meta-analysis. J Hypertens. 2015;33(2):221–229. [DOI] [PubMed] [Google Scholar]
- 23. Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- 24. Lundy DW. A day at the office: is private practice orthopaedic surgery dead? Clin Orthop Relat Res. 2016;474(11):2354–2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Manoso MW, Cizik AM, Bransford RJ, et al. Medicaid status is associated with higher surgical site infection rates after spine surgery. Spine (Phila Pa 1976). 2014;39(20):1707–1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Marrero CE, Igbokwe LI, Leonardi C. Access to orthopedic care post Medicaid expansion through the Affordable Care Act. J Natl Med Assoc. 2019;111(2):148–152. [DOI] [PubMed] [Google Scholar]
- 27. Pickett KE, Wilkinson RG. Income inequality and health: a causal review. Soc Sci Med. 2015;128:316–326. [DOI] [PubMed] [Google Scholar]
- 28. Schwarzkopf R, Phan DL, Hoang M, Ross SD, Mukamel D. Do patients with income-based insurance have access to total joint arthroplasty? J Arthroplasty. 2014;29(6):1083–1086, e1081. [DOI] [PubMed] [Google Scholar]
- 29. Segal DN, Grabel ZJ, Shi WJ, Gottschalk MB, Boden SD. The impact of insurance coverage on access to orthopedic spine care. J Spine Surg. 2018;4(2):260–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Skaggs DL, Lehmann CL, Rice C, et al. Access to orthopaedic care for children with Medicaid versus private insurance: results of a national survey. J Pediatr Orthop. 2006;26(3):400–404. [DOI] [PubMed] [Google Scholar]
- 31. Sood A, Gonzalez-Lomas G, Gehrmann R. Influence of health insurance status on the timing of surgery and treatment of bucket-handle meniscus tears. Orthop J Sports Med. 2015;3(5):2325967115584883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Volaco A, Cavalcanti AM, Filho RP, Precoma DB. Socioeconomic status: the missing link between obesity and diabetes mellitus? Curr Diabetes Rev. 2018;14(4):321–326. [DOI] [PubMed] [Google Scholar]
- 33. Wilensky G. Revisiting Medicaid. JAMA. 2017;318(3):229–230. [DOI] [PubMed] [Google Scholar]
- 34. Wiznia DH, Nwachuku E, Roth A, et al. The influence of medical insurance on patient access to orthopaedic surgery sports medicine appointments under the Affordable Care Act. Orthop J Sports Med. 2017;5(7):2325967117714140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wiznia DH, Wang M, Kim CY, Leslie MP. The effect of insurance type on patient access to ankle fracture care under the Affordable Care Act. Am J Orthop (Belle Mead NJ). 2018;47(9). [DOI] [PubMed] [Google Scholar]