Abstract
Objectives
This study aims to evaluate the effects of physical therapy modalities five days a week versus twice a week with a three-day interval on pain, depression, and functional disability in patients with chronic mechanical low back pain.
Patients and methods
Between June 2018 and November 2018, a total of 60 patients (39 females, 21 males; mean age 41.0±6.8 years; range, 25 to 55 years) with chronic mechanical low back pain were included. The patients were divided into two groups: Group 1 (n=30) received physical therapy five days a week for a total of 15 sessions, while Group 2 (n=30) received physical therapy twice a week with a three-day interval for a total of six sessions. Per protocol, all patients were applied hot pack for 20 min, followed by conventional transcutaneous electrical nerve stimulation (TENS) for 20 min and therapeutic ultrasound (US) for 10 min in each session. All patients were given exercise training and were instructed to do twice a day up to four weeks after the completion of physical therapy sessions. The severity of low back pain was evaluated using the visual analog scale (VAS), the severity of depression using the Beck Depression Inventory (BDI), and functional disability using the Oswestry Disability Index (ODI). All patients were evaluated before and after physical therapy and at four weeks. The results were compared between the groups.
Results
There was no statistically significant difference in the age, gender, body mass index, occupation, VAS, BDI, and ODI scores at the time of randomization (p>0.05). Intra-group analysis showed a significant improvement in all parameters after physical therapy compared to pre-treatment values and at four weeks compared to the post-treatment values (p<0.001). The differences of changes were used for the inter- group analysis which revealed a difference of change in favor of improvement was significantly higher in Group 2 than Group 1 (p<0.001). There was no significant difference between the post-treatment values and values at four weeks (p>0.05).
Conclusion
Our study results suggest that both physical therapy modalities applied five days week and twice a week are effective in pain, depression, and functional disability. However, physical therapy protocol applied twice a week yields more improvement, indicating that it is more advantageous with less cost and lost workdays.
Keywords: Chronic mechanical low back pain, physical therapy, treatment duration
Introduction
Low back pain (LBP) is a common health problem worldwide. Nearly 80% of the global population experience LBP at least once during lifetime.[1,2] Chronic pain adversely affects the psychological state of patients and limits daily living activities, which predisposes the patient to depression. Low back pain is also associated with high direct and indirect healthcare expenditures.[1,3] In a study carried out in Sweden, the mean duration of a LBP episode was days with a cost of €2,753.[4]
Physical therapy modalities are the most common conservative methods used in the treatment of LBP. In general, these modalities are combined with exercise and hot and cold pack, and electrotherapy.[5-10] Several physical therapy modalities have been investigated in LBP studies; however, there is no consensus regarding the number of sessions and optimal intervals. Study designs in these studies often include the evaluation of treatment responses and outcomes, available modalities, and accessibility to treatment.[11,12] In two studies previously, a positive correlation was found between the number of sessions and duration of symptoms and age of the patient.[13,14] In another study, the mean number of sessions was 9.9 in patients with LBP.[15] A study also compared two physical therapy modalities (10 sessions versus 15 sessions) in a heterogeneous patients with low back, neck, and knee pain and reported a significant improvement in the pain, quality of life, and patient global assessment scores, but not in the depression and anxiety scores, between the two modalities.[16]
In addition to limited number of data regarding the optimal number of sessions of physical therapy, there is no consensus on the time intervals between the sessions. Based on our experiences, physical therapy protocols are applied for five days a week or two or three times a week. However, it is well-known that superficial or deep hot and cold applications are physiological stressors for the human body and adaptive mechanisms are activated by the chemical and physiological imbalance. Time is needed to make these mechanisms function properly.[17,18]
Selye[19] first described General Adaptation Syndrome (GAS) in 1950 which is a three-stage process that the body goes through when it is exposed to stress to preserve the integrity and vitality of the organism:
1. Alarm reaction stage: The alarm reaction stage refers to the initial symptoms the body experiences when under stress (i.e., fight-or- flight response). In an animal model, Selye[19] found a decrease in the size of thymus, spleen, lymph nodes, and liver within six to 48 hours after stimuli in rats. Depending on the strength of the stressor, improvement or deterioration may be seen.
2. Resistance stage: After the initial shock of a stressful event, the body begins to repair itself. If the stressful situation persists, resistance occurs. In an animal model, Selye[19] reported that organ dysfunctions during the alarm reaction stage resolved over time in rats. However, if the resistance stage continues for extended periods of time without pauses to offset the effects of stress, this can lead to the exhaustion stage.
3. Exhaustion stage: At this stage, the body has depleted its energy resources with continuous efforts, but has failed to recover from the initial alarm reaction stage. If the stressors continue beyond the body’s capacity and the energy for adaptation is fully depleted, the body is susceptible to death or, otherwise, to diseases.[17-21]
It is essential to overcome the alarm reaction stage of the GAS for a patient to comply with physical therapy modalities which induce physiological stress and to repair tissue injury.[19] Therefore, it is reasonable to apply treatment with a few-days interval to improve the compliance of the body with the treatment and to increase the healing effect.
In the present study, we aimed to evaluate the effects of physical therapy modalities five days a week versus twice a week with a three-day interval on pain, depression, and functional disability in patients with chronic mechanical LBP.
Patients and Methods
Between June 2018 and November 2018, a total of 60 patients (39 females, 21 males; mean age 41.0±6.8 years; range, 25 to 55 years) with chronic mechanical low back pain were included. Inclusion criteria were as follows: having complaints for ≥3 months; a diagnosis of LBP based on laboratory test (complete blood count, erythrocyte sedimentation rate, C-reactive protein, routine biochemistry tests) and radiological results (bilateral lumbosacral graphies or lumbar magnetic resonance imaging) with detailed physical examination findings; and being volunteer to participate. Exclusion criteria were as follows: acute LBP (for <3 months), acute disc herniation with neurological symptoms and sciatica, mechanical instability and severe structural deformity, inflammatory LBP, acute vertebral fractures, malignancies, pregnancy, metabolic and endocrine bone disease, and abdominopelvic pain.
A written informed consent was obtained from each patient. The study protocol was approved by the Clinical Researches Ethics Committee of Istanbul Medeniyet University, Goztepe Training and Research Hospital (Decision No. 17.05.2018-2018/0183). The study was conducted in accordance with the principles of the Declaration of Helsinki.
This study was designed as a randomized- controlled trial. All patients were randomly assigned to two groups in accordance with the prespecified criteria per protocol (www.randomizer.org). Group 1 (n=30) received physical therapy five days a week for a total of 15 sessions, while Group 2 (n=30) received physical therapy twice a week with a three-day interval for a total of six sessions. Per protocol, all patients were applied hot pack (25¥40 cm) for 20 min, followed by conventional transcutaneous electrical nerve stimulation (TENS; Compex; 1-150 Hz, 120 mA) for 20 min, and therapeutic ultrasound (US; Sonomed 4, 1 MHz 1.5 w/cm2) for 10 min in each session.
At the initial stage of physical therapy, all patients were given exercise training including mobilization, isometric stretching, pelvic tilt, and abdominal muscle strengthening and were instructed to do twice a day in three sets with 10 repetitions. In each session, the patients were questioned whether they did exercises on a regular basis and about their compliance. In addition, all patients were instructed to do exercises for four weeks after the completion of physical therapy sessions and their compliance to home-based exercises was evaluated by phone calls. No medication was allowed during the study. The patients were re-evaluated in case of severe pain requiring medication.
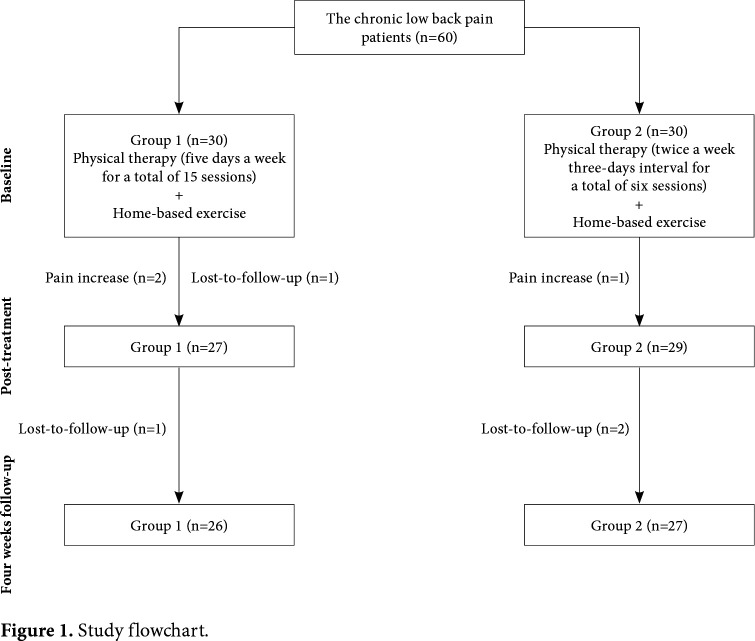
In Group 1, four patients (1 male and 3 females) withdrew from the study (one left in Session 5 and another left in Session 7 due to increased pain; one was lost-to-follow-up at the end of physical therapy; and one was lost-to-follow-up at four weeks). In Group 2, three patients (1 male and 2 females) withdrew from the study (one left in Session 3 due to increased pain; the remaining two patients were lost-to-follow-up at four weeks). Finally, 53 patients completed the study including 26 patients (17 females and 9 males) in Group 1 and 27 patients (17 females and 10 males) in Group 2 (Figure 1). Both groups completed assigned therapies at three weeks. All patients were evaluated before and after physical therapy and at four weeks. The results were compared between the groups.
Figure 1. Study flowchart.
Assessments
The severity of LBP due to exercise was evaluated using the visual analog scale (VAS). A higher score indicates greater pain intensity.[22,23] The severity of depression was evaluated using the Beck Depression Inventory (BDI). This tool was developed by Beck et al.[24] in 1961 to assess and monitor changes in depressive symptoms. It is a 21-item self-reporting questionnaire which are ranked on a numerical scale of 0-3 with a total summed score range of 0-63. The scores of BDI are classified as minimal (0-13), mild (14-19), moderate (20-28), and severe (29-63). The validity and reliability study of the questionnaire in the Turkish population have been conducted by Hisli.[25] Furthermore, functional disability was evaluated using the Oswestry Disability Index (ODI) which is a patient-reported outcome questionnaire consisting of 10 items. It examines perceived level of disability in everyday activities of daily living including pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, and traveling. Each item has six statements from which patients are requested to select one. It is scored from 0 to 5 for each item.[26-28] The validity and reliability study of the questionnaire in the Turkish population have been shown.[29]
Statistical analysis
Power analysis was performed using the G*Power version 3.1.9 program (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany) to calculate the sample size. Based on the pre- and post-treatment VAS values reported in the study of Yilmaz et al.[30] (Group 1: 2, Group 2: 5), at least 23 patients were needed in each group to obtain 90% study power at an alpha level of 0.05. Considering possible withdrawals, a total of 30 patients were recruited for each group.
Statistical analysis was performed using the Number Cruncher Statistical System (NCSS) version 2007 software (NCSS LLC., Kaysville, Utah, USA). Descriptive data were expressed in mean and standard deviation (SD), median (min-max), number, and frequency. Normality of the data was assessed using the Shapiro-Wilk test and graphical examinations. Normally distributed quantitative data were compared using the Student’s t-test, while non-normally distributed quantitative data were compared using the Mann-Whitney U test between the groups. Qualitative data were compared using the Pearson chi-square test and Fisher-Freeman-Halton exact test. The Friedman test was used to test the within-subject effects of non-normally distributed data, post-hoc comparisons were performed by the Bonferroni-corrected Wilcoxon signed-rank tests. The Cronbach’s alpha was used to assess the internal consistency of the BDI and ODI questionnaires. A p value of <0.05 was considered statistically significant.
Results
Of 60 patients included in the study, 53 completed the study. There was no significant difference in the age, gender, body mass index, occupation, VAS, BDI, and ODI scores at the time of randomization between the groups (p>0.05).
The mean pre-treatment BDI scores were 12.0±6.0 (range, 1 to 29) and the mean post-treatment BDI scores were 8.3±5.3 (range, 0 to 22). In the control group, the mean BDI scores were 5.5±4.4 (range, 0 to 18). The Cronbach’s coefficient alpha values for BDI were 0.850, 0.858, and 0.851, respectively, indicating that the scale was highly reliable (Table 1).
Table 1. Scores of Beck Depression Inventory and Oswestry Disability Index.
| Number of questions | Mean±SD | Median | Min-Max | Cronbach’s alpha | |
| Beck Depression Inventory | |||||
| Pre-treatment | 21 | 12.0±6.0 | 12 | 1-29 | 0.850 |
| Post-treatment | 21 | 8.3±5.3 | 8 | 0-22 | 0.858 |
| Control | 21 | 5.5±4.4 | 4 | 0-18 | 0.851 |
| Oswestry Disability Index | |||||
| Pre-treatment | 10 | 36.0±16.4 | 36 | 4-72 | 0.944 |
| Post-treatment | 10 | 23.8±14.2 | 20 | 2-56 | 0.946 |
| Control | 10 | 14.9±11.8 | 12 | 0-44 | 0.932 |
| SD: Standard deviation; Min: Minimum; Max: Maximum. | |||||
The mean pre-treatment ODI scores were 36.0±16.4 (range, 4 to 72) and the mean post-treatment ODI scores were 23.8±14.2 (range, 2 to 56). In the control group, the mean ODI scores were 14.9±11.8 (range, 0 to 44). The Cronbach’s coefficient alpha values for BDI were 0.944, 0.946, and 0.932, respectively, indicating that the scale was highly reliable (Table 1).
Baseline demographic characteristics of the patients are shown in Table 2. Comparison of both groups in terms of demographic characteristics is presented in Table 3.
Table 2. Baseline demographic characteristics of patients.
| Variable | n | % | Mean±SD | Median | Min-Max |
| Age (year) | 41.0±6.9 | 41 | 29-55 | ||
| Gender | |||||
| Female | 34 | 64.2 | |||
| Male | 19 | 35.8 | |||
| Body mass index (kg/m2) | 30.1±3.9 | 30.4 | 21.1-38.1 | ||
| Occupation | |||||
| Housewife | 25 | 47.2 | |||
| Worker | 7 | 13.2 | |||
| Retired | 4 | 7.5 | |||
| Other | 17 | 32.1 | |||
| Education status | |||||
| Primary school | 23 | 43.4 | |||
| Secondary-high school | 19 | 35.8 | |||
| College | 11 | 20.8 | |||
| SD: Standard deviation; Min: Minimum; Max: Maximum. | |||||
Table 3. Comparison of demographic characteristics of patients.
| Physical therapy | |||||||||||
| Group 1 (n=26) | Group 2 (n=27) | ||||||||||
| n | % | Mean±SD | Median | Min-Max | n | % | Mean±SD | Median | Min-Max | p | |
| Age (year) | 41.2±7.0 | 42 | 30-55 | 40.9±6.9 | 41 | 29-54 | 0.890* | ||||
| Gender | 0.854† | ||||||||||
| Female | 17 | 65.4 | 17 | 63.0 | |||||||
| Male | 9 | 34.6 | 10 | 37.0 | |||||||
| Body mass index (kg/m2) | 30.5±4.4 | 21.1-38.1 | 30.8 | 29.8±3.3 | 30.4 | 22.7-36.3 | 0.520* | ||||
| Occupation | 1.000‡ | ||||||||||
| Housewife | 13 | 50.0 | 12 | 44.4 | |||||||
| Worker | 3 | 11.5 | 4 | 14.8 | |||||||
| Retired | 2 | 7.7 | 2 | 7.4 | |||||||
| Other | 8 | 30.8 | 9 | 33.3 | |||||||
| Education status | 0.919† | ||||||||||
| Primary school | 11 | 42.3 | 12 | 44.4 | |||||||
| Secondary-high school | 10 | 38.5 | 9 | 33.3 | |||||||
| College | 5 | 19.2 | 6 | 22.2 | |||||||
| SD: Standard deviation; * Student t-test; † Pearson chi-square test; ‡ Fisher-Freeman-Halton exact test. | |||||||||||
In addition, there was no significant difference in the VAS, BDI, and ODI scores at baseline between the groups (p>0.05) (Table 4). However, intra- group analysis showed a significant decrease in the VAS scores in both groups after physical therapy, compared to pre-treatment values and at four weeks, compared to the post-treatment values (p<0.001). Although there was a significantly higher decrease in Group 2 than Group 1 after physical therapy and at four weeks, compared to pre-treatment values, the difference was not statistically significant between the post-treatment values and four-week measurements (p=0.529) (Table 3). Inter-group analysis showed significantly lower VAS scores in Group 2 than Group 1 after physical therapy and at four weeks (p<0.002).
Table 4. Pain, depression, and functional disability according to study groups.
| Physical therapy | †p | ‡p | |||||||
| Group 1 (n=26) | †p | Group 2 (n=27) | |||||||
| Mean±SD | Median | Min-Max | Mean±SD | Median Min-Max | |||||
| Visual analog scale | |||||||||
| Pre-treatment | 7.2±1.7 | 7,5 | 3-9 | 7.0±1.4 | 7 | 4-9 | 0,377 | ||
| Post-treatment | 5.0±1.5 | 5 | 2-7 | 3.7±1.5 | 4 | 1-6 | 0.002** | ||
| Week 4 (EOT) | 3.3±1.4 | 3 | 1-6 | 2.0±1.3 | 2 | 0-5 | 0.002** | ||
| §p | 0.001** | 0.001** | |||||||
| Difference | |||||||||
| Pre-/post-treatment | -2.2±0.6 | -2 | 0.001** | -3.3±0.9 | -3 | 0.001** | 0.001** | ||
| Pre-treatment/week 4 (EOT) | -3.9±1.1 | -4 | 0.001** | -5.0±1.0 | -5 | 0.001** | 0.001** | ||
| Post-treatment/week 4 (EOT) | -1.7±0.7 | -2 | 0.001** | -1.6±0.6 | -2 | 0.001** | 0,529 | ||
| Beck Depression Inventory | |||||||||
| Pre-treatment | 12.0±7.4 | 12 | 1-29 | 12.0±4.4 | 12 | 2-20 | 0,506 | ||
| Post-treatment | 9.4±6.4 | 8 | 0-22 | 7.3±3.9 | 7 | 1-16 | 0,304 | ||
| Week 4 (EOT) | 6.5±5.0 | 6 | 0-18 | 4.6±3.6 | 4 | 0-13 | 0,139 | ||
| §p | 0.001** | 0.001** | |||||||
| Difference | |||||||||
| Pre-/post-treatment | -2.6±2.1 | -2 | 0.001** | -4.7±2.5 | -4 | 0.001** | 0.001** | ||
| Pre-treatment/week 4 (EOT) | -5.5±3.1 | -5 | 0.001** | -7.4±3.1 | -8 | 0.001** | 0.014* | ||
| Post-treatment/week 4 (EOT) | -2.9±1.8 | -2,5 | 0.001** | -2.7±2.9 | -3 | 0.001** | 0,612 | ||
| Oswestry Disability Index | |||||||||
| Pre-treatment | 36.2±18.6 | 33 | 4-72 | 35.9±14.3 | 36 | 8-56 | 0,950 | ||
| Post-treatment | 27.1±16.1 | 23 | 2-56 | 20.7±11. 6 | 16 | 2-44 | 0,104 | ||
| Week 4 (EOT) | 17.8±12.4 | 16 | 0-44 | 12.2±10.7 | 8 | 0-40 | 0.032* | ||
| §p | 0.001** | 0.001** | |||||||
| Difference | |||||||||
| Pre-/post-treatment | -9.2±4.7 | -8 | 0.001** | -15.2±6.6 | -14 | 0.001** | 0.001** | ||
| Pre-treatment/week 4 (EOT) | -18.5±9.1 | -19 | 0.001** | -23.7±9.7 | -24 | 0.001** | 0.041* | ||
| Post-treatment/week 4 (EOT) | -9.3±5.5 | -8 | 0.001** | -8.5±4.5 | -8 | 0.001** | 0,690 | ||
| SD: Standard deviation; EOT: End of treatment; * p<0.05; ** p<0.01; † Wilcoxon signed-rank test; ‡ Mann-Whitney U test; § Friedman test. | |||||||||
Intra-group analysis showed a significant decrease in the BDI scores in both groups after physical therapy, compared to pre-treatment values and at four weeks, compared to the post-treatment values (p<0.001). Inter-group analysis revealed no statistically significant difference in the BDI scores post-treatment values and four-week measurements (p>0.05). The differences of changes were significantly higher in Group 2 than Group 1 after physical therapy and at four weeks, compared to pre-treatment values (p<0.001). There was no significant difference between the post-treatment values and values at four weeks (p=0.612).
Intra-group analysis showed a significant decrease in the ODI scores in both groups after physical therapy, compared to pre-treatment values and at four weeks, compared to the post-treatment values (p<0.001). Inter-group analysis revealed no significant difference in the ODI scores after physical therapy (p=0.104); however, Group 2 had significantly lower scores at four weeks. The differences of changes were significantly higher in Group 2 than Group 1 after physical therapy and at four weeks, compared to pre-treatment values (p<0.05). There was no significant difference between the post-treatment values and values at four weeks (p=0.690).
Throughout the study, all patients were questioned in each visit and by phone call after the completion of physical therapy whether they were compliant to home-based exercises. All patients showed compliance. During follow-up, none of the patients required analgesics.
Discussion
In this study, we evaluated the effects of two physical therapy modalities on pain, depression, and functional disability using VAS, BDI, and ODI, respectively in patients with chronic mechanical LBP. We showed a significant improvement in all scores after physical therapy and at four weeks. However, physical therapy protocol applied twice a week with a three-day interval yielded more improved scores in VAS after treatment and in both VAS and ODI at four weeks. In addition, the difference of changes was significantly higher in this protocol, except for the difference between the post-treatment values and four-week measurements.
Physical therapy modalities are used widespread in the treatment of LBP. The literature is rich in articles using a broad range of physical therapy modalities and protocols.[7,8,30-33] In these studies, protocols five days a week have been particularly used. These studies have also demonstrated that combination of different modalities can yield satisfactory results.[7] In their study, Narin et al.[7] showed that hot pack + TENS for five days a week for three weeks decreased LBP-related pain and improved functional disability and quality of life for daily living activities. In another study combining hot pack + TENS + US with a functional back school program, physical therapy for five days a week for two weeks statistically significantly decreased the subjective pain scores and functional disability in the early stage.[31] Some other authors also suggested that physical therapy protocols for five days a week for two weeks combined with exercise training decreased pain and functional disability in patients with LBP.[8,30] In our study, similar to the aforementioned studies, we also obtained favorable results for pain, depression, and functional disability with a physical therapy protocol for five days a week for three weeks combined with exercise training in patients with LBP.
Despite satisfactory results of protocols on a five- day-a-week basis, we also attempted to investigate the effectiveness of another protocol with intervals waiting for the adaptation timing, according to the GAS described by Selye.[19] In our literature search, we found three studies using protocols two or three times a week. Two of these studies compared therapeutic US and placebo US, while the other used a combination therapy with exercise.[32,33] In both studies, therapeutic US was found to be effective.
In a study, Koldas Dogan et al.[10] applied physical therapy three times a week for a total of six weeks in patients with LBP. The patients were divided into three groups: one received physical therapy (hot pack + TENS + US) combined with home-based exercise; one received aerobic exercises with a home-based exercise program; and one received home-based exercises alone. In all groups, all therapy protocols decreased pain and increased exercise capacity, although there was a significant improvement in the functional disability and psychological state in patients receiving physical therapy. Consistent with these findings, we also showed that physical therapy twice a week with a three-day interval was effective in decreasing pain intensity and depression severity.
Review of the literature reveals that both physical therapy protocols (five days a week and two or three times a week) are effective in patients with LBP. However, to the best of our knowledge, the present study is the first to compare both protocols and to show the superiority of the protocol applied twice a week. Of note, we achieved favorable results with both protocols, although we found a significant improvement and decrease in Group 2 than Group 1 after physical therapy and at four weeks.
These results are thought to be due to creating an acute, and controllable stress achieved with intermittent treatment of physical therapy, which allows for recovery.[18] Physical or mental stress induces a counter-response in the body. Exogenously applied physical therapy, which can be considered a stressor, increases heat in tissue with both physical and chemical changes by altered electrical activity of the cell membrane. As a result of adaptation to each stressor, the organism attempts to regain its stability. Autonomic nervous system, hypothalamic-pituitary- adrenal axis, cardiovascular, metabolic, and immune systems contribute to this adaptation ability, defined as allostasis. Once the stressor disappears, inactivation of these systems begins and cortisol and catecholamine levels return to their baseline values. However, if the stressor frequently appears, inactivation of these systems becomes insufficient and the exposure to stress hormones may be prolonged. This may lead to an allostatic load, resulting in a delay in stabilization (i.e., delayed recovery).[34]
We believe that the results of our study suggest that daily physical therapy methods may slow down the healing process, as indicated by Selye’s GAS.[20] Therefore, the implementation of the physical therapy modalities applied within a few-day intervals may be useful for the adaptation of the body with the treatments applied during the resistance stage and to improve the healing effect.
To the best of our knowledge, the present study is the first to primarily evaluate the frequency of physical therapy application. However, the lack of a control group (exercise alone) is the main limitation of this study. Using a control group, we might have evaluated the effects of exercise more accurately. Although our study suggests that intermittent therapy is more effective in patients with LBP, further long-term studies are needed to confirm these findings.
In conclusion, our study results show that both physical therapy modalities applied five days week and twice a week are effective in pain, depression, and functional disability. However, physical therapy protocol applied twice a week yields more improvement, indicating that it is more advantageous with less time, direct and indirect cost, and lost workdays with short hospital stay. Based on these findings, we suggest that intermittent physical therapy protocols may be more useful. However, further evidence-based studies are required to establish a conclusion regarding the frequency of sessions.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Ay S, Evcik D. Kronik bel ağrılı hastalarda depresyon ve yaşam kalitesi. Fiziksel Tıp ve Rehabilitasyon Anabilim Dalı. Ankara Yeni Tıp Dergisi. 2008;25:228–231. [Google Scholar]
- 2.Almeida DC, Kraychete DC. Low back pain-a diagnostic approach. Rev Dor SãoPaulo. 2017;18:173–177. [Google Scholar]
- 3.Ambrose KR, Golightly YM. Physical exercise as non- pharmacological treatment of chronic pain: Why and when. Best Pract Res Clin Rheumatol. 2015;29:120–130. doi: 10.1016/j.berh.2015.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olafsson G, Jonsson E, Fritzell P, Hägg O, Borgström F. Cost of low back pain: results from a national register study in Sweden. Eur Spine J. 2018;27:2875–2881. doi: 10.1007/s00586-018-5742-6. [DOI] [PubMed] [Google Scholar]
- 5.Akarırmak Ü, Erden G. Bel ağrılarında konservatif tedavi. Clinic Medicine. 2007;1:40–46. [Google Scholar]
- 6.Hayashi Y. Classification, diagnosis, and treatment of low back pain. JMAJ. 2004;47:227–223. [Google Scholar]
- 7.Narin S, Bozan Ö, Cankurtaran F, Bakırhan S. Kronik bel ağrılı hastalarda fizyoterapi programının fonksiyonel kapasite ve yaşam kalitesi üzerine etkisi. DEU Tıp Fakültesi Dergisi. 2008;22:137–143. [Google Scholar]
- 8.Şahin N, Albayrak İ, Karahan AY, Uğurlu H. Kronik bel ağrılı hastalarda fizik. tedavinin etkinliği, Genel Tıp Derg. 2011;21:17–20. [Google Scholar]
- 9.Günaydın R. General physical therapy applications for elderly people. Turk J Phys Med Rehab. 2009;55(Suppl 2):85–87. [Google Scholar]
- 10.Koldaş Doğan S, Sonel Tur B, Kurtaiş Y, Atay MB. Comparison of three different approaches in the treatment of chronic low back pain. Clin Rheumatol. 2008;27:873–881. doi: 10.1007/s10067-007-0815-7. [DOI] [PubMed] [Google Scholar]
- 11.Gracey JH, McDonough SM, Baxter GD. Physiotherapy management of low back pain: a survey of current practice in northern Ireland. Spine (Phila Pa 1976) 2002;27:406–411. doi: 10.1097/00007632-200202150-00017. [DOI] [PubMed] [Google Scholar]
- 12.Clair DA, Edmondston SJ, Allison GT. Physical therapy treatment dose for nontraumatic neck pain: a comparison between 2 patient groups. J Orthop Sports Phys Ther. 2006;36:867–875. doi: 10.2519/jospt.2006.2299. [DOI] [PubMed] [Google Scholar]
- 13.Mitchell JM, de Lissovoy G. A comparison of resource use and cost in direct access versus physician referral episodes of physical therapy. Phys Ther. 1997;77:10–18. doi: 10.1093/ptj/77.1.10. [DOI] [PubMed] [Google Scholar]
- 14.Zuijderduin W, Dekker J, Abrahamse H. Determinants of the number of sessions in a physical therapeutic treatment. Tijdschr Soc Gezondheidsz. 1995;73:274–281. [Google Scholar]
- 15.Swinkels IC, Wimmers RH, Groenewegen PP, van den Bosch WJ, Dekker J, van den Ende CH. What factors explain the number of physical therapy treatment sessions in patients referred with low back pain; a multilevel analysis. BMC Health Serv Res. 2005;5:74–74. doi: 10.1186/1472-6963-5-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Atalay NS, Akkaya N, Konukcu S, Balci CS, Sahin F. Psychic predictors of outcomes of physical therapy. J Back Musculoskelet Rehabil. 2013;26:71–77. doi: 10.3233/BMR-2012-00352. [DOI] [PubMed] [Google Scholar]
- 17.Hatungil R. Stres ve demansta hipotalamus-hipofiz-adrenal ekseninin rolü. Mersin Univ Saglık Bilim Derg. 2008;1:1–7. [Google Scholar]
- 18.Kocaturk PA. Strese cevap. Ankara Üniversitesi Tıp Fakültesi Mecmuası. 2000;53:49–56. [Google Scholar]
- 19.Selye H. Stress and the general adaptation syndrome. Br Med J. 1950;1:1383–1392. doi: 10.1136/bmj.1.4667.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crevecoeur GU. A system approach to the General Adaptation Syndrome. Available from: https://www.researchgate.net/publication/305609884_A_system_approach_to_the_General_Adaptation_Syndrome. [Accessed: February 26, 2019]. [Google Scholar]
- 21.Deliorman D. Adaptojenler ve adaptojenik aktivite taramasında kullanılan farmakolojik testler. Ankara Ecz Fak Derg. 2000;29:33–48. [Google Scholar]
- 22.Shupak NM, McKay JC, Nielson WR, Rollman GB, Prato FS, Thomas AW. Exposure to a specific pulsed low-frequency magnetic field: a double-blind placebo- controlled study of effects on pain ratings in rheumatoid arthritis and fibromyalgia patients. Pain Res Manag. 2006;11:85–90. doi: 10.1155/2006/842162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weber H. Lumbar disc herniation: A controlled prospective study with ten years of observation. SAS Journal. 2009;3:30–40. [PubMed] [Google Scholar]
- 24.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 25.Hisli N. Beck Depresyon Envanterinin üniversite öğrencileri için geçerliği, güvenirliği. Psikoloji Dergisi. 1989;7:3–13. [Google Scholar]
- 26.Delitto A. Are measures of function and disability important in low back care. Phys Ther. 1994;74:452–462. doi: 10.1093/ptj/74.5.452. [DOI] [PubMed] [Google Scholar]
- 27.Frost H, Klaber Moffett JA, Moser JS, Fairbank JC. Randomised controlled trial for evaluation of fitness programme for patients with chronic low back pain. BMJ. 1995;310:151–154. doi: 10.1136/bmj.310.6973.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 29.Yakut E, Düger T, Oksüz C, Yörükan S, Ureten K, Turan D, et al. Validation of the Turkish version of the Oswestry Disability Index for patients with low back pain. Spine (Phila Pa 1976) 2004;29:581–585. doi: 10.1097/01.brs.0000113869.13209.03. [DOI] [PubMed] [Google Scholar]
- 30.Yılmaz Ö, Küçük Eroğlu P, Yurdakul FG, Garip Çimen Y, Eser F, Alhan A, et al. Comparing physical therapy accompanying exercise with only exercise treatments in patients with chronic low back pain. Turk J Osteoporos. 2015;21:73–78. [Google Scholar]
- 31.Tuğcu İ, Önder ME, Yazıcıoğlu K, Möhür H. The effectiveness of functional back school concurrently applied with exercise and physical therapy modalities in patients with chronic mechanical low back pain-short term results. Turk J Phys Med Rehab. 2008;54:63–68. [Google Scholar]
- 32.Ebadi S, Ansari NN, Henschke N, Naghdi S, van Tulder MW. The effect of continuous ultrasound on chronic low back pain: protocol of a randomized controlled trial. BMC Musculoskelet Disord. 2011;12:59–59. doi: 10.1186/1471-2474-12-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ansari NN, Ebadi S, Talebian S, Naghdi S, Mazaheri H, Olyaei G, et al. A randomized, single blind placebo controlled clinical trial on the effect of continuous ultrasound on low back pain. Electromyogr Clin Neurophysiol. 2006;46:329–336. [PubMed] [Google Scholar]
- 34.McEvven BS. Protective and damaging effects of stress mediators. New England J Med. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]