Abstract
Coronavirus disease 2019 (COVID-19) is a contagious infection disease, which may cause respiratory, physical, psychological, and generalized systemic dysfunction. The severity of disease ranges from an asymptomatic infection or mild illness to mild or severe pneumonia with respiratory failure and/or death. COVID-19 dramatically affects the pulmonary system. There is a lack of knowledge about the long-term outcomes of the disease and the possible sequelae and rehabilitation. This clinical practice guideline includes pulmonary rehabilitation (PR) recommendations for adult COVID-19 patients and has been developed in the light of the guidelines on the diagnosis and treatment of COVID-19 provided by the World Health Organization and Republic of Turkey, Ministry of Health, recently published scientific literature, and PR recommendations for COVID-19 regarding basic principles of PR. In this guideline, the contagiousness of COVID-19, recommendations on limited contact of patient with healthcare providers, and the evidence about possible benefits of PR were taken into consideration.
Keywords: COVID-19, guideline. pulmonary rehabilitation, severe acute respiratory syndrome
The severe acute respiratory syndrome- coronavirus-2 (SARS-CoV-2; COVID-19) is a highly transmissible disease, resulting in the disruption of mainly respiratory, as well as physical, psychological and overall systemic functions. Although the route of spread, diagnosis, clinical features, and treatment and prevention of COVID-19 have not been fully elucidated yet, an increasing number of experiences have been gained and published day by day. Individuals surviving the disease may require pulmonary rehabilitation (PR) either in addition to medical treatment or after the completion of their treatment. In the light of existing information coming from countries such as China, Italy, Spain, the United States, and Iran where the number of patients is high and scientific data are available, there is an apparent unmet need to prepare a guideline for the PR of COVID-19.
COVID-19
Described as novel coronavirus disease 2019 by the World Health Organization (WHO), COVID-19 is a respiratory tract infection caused by SARS-CoV-2, a coronavirus. COVID-19 first appeared in Wuhan province of China in the late December 2019.[1] The first case in Turkey was identified on March 11th, 2020.[2] The WHO declared COVID-19 as a pandemic on March 12th, 2020.[1]
Pathogenesis
SARS-CoV-2 is a betacoronavirus with a genetic sequence highly similar to severe acute respiratory syndrome (SARS) virus.[1] SARS-CoV-2 is an enveloped ribonucleic acid (RNA) virus which can spread from one human to another. Angiotensin-converting enzyme 2 (ACE-2) found in the lower respiratory airways of humans is a cellular receptor for SARS-CoV and has been shown to play a role in the spread from one human to another and in cross-transmission.[3,4] It has also been isolated from the bronchoalveolar lavage fluid of a COVID-19 patient. Zhou et al.[5] confirmed the fact that SARS-CoV-2 used the same cellular entry receptor ACE-2 with SARS-CoV. Biophysical and structural evidence makes us think that SARS-CoV-2 S protein binds to human ACE-2 with a rate possibly 10 to 20 times higher than SARS-CoV.[6] The ACE-2 is mainly associated with cardiovascular diseases and is a type I membrane protein expressed by the lungs, heart, kidneys, and bowel.[7] The virion S-glycoprotein found on the surface of coronavirus binds to ACE-2 on the surface of human cells.[8] Following membrane fusion, the viral genome is secreted into the cytoplasm and the uncoated RNA encodes two polyproteins which encode non-structural proteins and form a replication-transcription complex (RTC) on double- membrane vesicle.[9,10] The RTC continuously replicates and synthesizes a series of subgenomic RNA encoding accessory proteins and structural proteins.[11] Newly formed genomic RNA forms viral particle buds of nucleocapsid proteins and envelope glycoproteins. Finally, virion-containing vesicles join with the plasma membrane to release the virus.[11]
Two patients were operated for pulmonary adenocarcinoma and, during postoperative follow-up, they were identified to have COVID-19 at the time of the operation. In addition, proteinaceous exudate, vascular congestion, multinucleated giant cells, reactive alveolar epithelial hyperplasia and fibroblastic proliferation were identified in the pathological examination of the lung fluid outside the field of adenocarcinoma. As neither of these patients exhibited pneumonia symptoms at the time of the operation, these changes were thought to possibly represent an early stage of the pulmonary pathology of COVID-19 pneumonia.[12]
Based on the existing epidemiological data, the incubation period for the virus is 1 to 14 days, and the transmissibility is high between 3 and 7 days. The COVID-19 is transmissible during the latency period, as well.[13] Elderly individuals and those with underlying health conditions are more prone to infection and more inclined to acute respiratory distress syndrome (ARDS) and severe consequences which may be related to cytokine storms.[14] In the meta-analyses, the most frequent comorbidities were reported as hypertension, cardiovascular disease, and diabetes.[15]
The infection spreads via droplets from individuals who are symptomatic or asymptomatic by sneezing or coughing. Patients can be infectious as long as the symptoms last and also during clinical recovery. The infection spreads by inhaling these particles or by touching the nose, mouth, and eyes after contact with a contaminated surface. Viral nucleocapsid protein has been demonstrated in gastrointestinal epithelial cells and virus particles have been isolated from the stool. Furthermore, the fecal polymerase chain reaction (PCR) test has been found to be positive.[16] Therefore, the virus is assumed to spread via the oral-fecal route.[1] Currently, transplacental transmission from pregnant mothers to their fetuses has not been described, yet. However, newborn disease due to postnatal transmission has been defined.[17]
Clinical Features
A meta-analysis on COVID-19 was published in China including 54,498 patients of which 53,991 were confirmed cases. According to reported epidemiological data, most of the patients were at 20 to 60 years of age with a higher incidence of infection among men and with a mean time of five days from the onset of the disease until the diagnosis. Most of the cases were mild (81.4%), 13.9% were severe, and 4.7% were critical.[18] In Turkey, based on the statements made by the Republic of Turkey, Ministry of Health (April 24th, 2020), there are 104,912 confirmed cases, 1,790 of these are admitted to intensive care units (ICUs), and 929 of ICU patients are on invasive/non-invasive mechanical ventilators. The ICU admission rate of our patients is 1.7%, and 51.9% of these patients are intubated.[19]
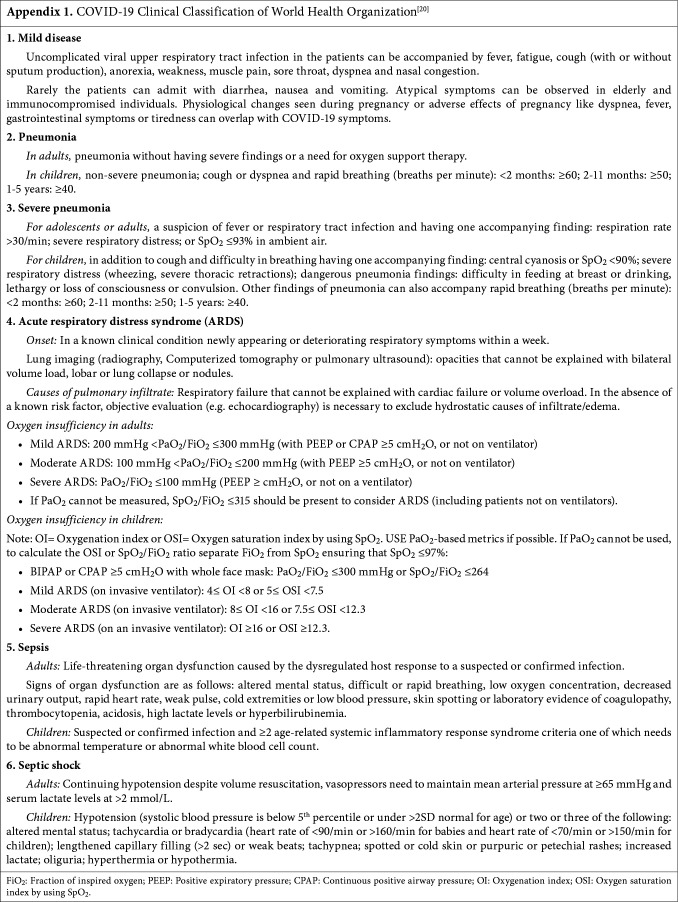
According to the clinical classification by the WHO, COVID-19 disease can manifest as a wide spectrum from mild disease to pneumonia, severe pneumonia, ARDS, sepsis, and septic shock (see Appendix 1).[20] Common clinical findings are fever, frequent dry cough, sore throat, headache, fatigue, muscle pain, and dyspnea.[21] Gastrointestinal symptoms such as nausea, vomiting, stomachache, and gastrointestinal bleeding may be also observed. In a review evaluating 2,023 patients, anorexia (40 to 50%) was reported as the most frequent digestive symptom for adults, diarrhea (2 to 50%) for adults and children and vomiting for children.[16] Anosmia and ageusia may present as the initial symptoms.[22] Although being less frequent, conjunctivitis may be seen in certain patients. [23] In a meta-analysis, most frequent symptoms were reported as fever, cough, and dyspnea.[15] In elderly and individuals with comorbidities such as hypertension, chronic obstructive pulmonary disease (COPD), diabetes, and cardiovascular disease, COVID-19 can rapidly progress into ARDS, septic shock, and a difficulty in correcting metabolic acidosis and coagulation disorders.[24] Symptoms of children with COVID-19 are less severe than those of adults, the disease mainly appears with cough, and fever and co-infections have been reported.[1]
For most COVID-19 patients, the disease course is mild and without any complications, and nearly 14% of patients are admitted to the hospital and develop severe conditions requiring oxygen support, while 5% of patients are admitted to ICU.[1] In severe cases, COVID-19 can be complicated with ARDS, sepsis, septic shock, acute renal failure, and multiorgan failure including heart failure.[1] Of note, ARDS is a life-threatening organ failure which can develop due to pulmonary or extrapulmonary causes. The incidence of ARDS has been reported as 5 to 60 per 100,000 individuals.[25] The mortality rates for ARDS have decreased compared to previous years; however, increased mortality and morbidity rates can be seen in individuals who survive.[26] Advanced age and comorbidities are the most important factors influencing the disease process. Long-term results of ARDS are mostly evaluated with spirometry, diffusion capacity, and cardiopulmonary functional capacity. Herridge et al.[27] reported lung volumes returning to normal within three to six months. However, in the overall evaluation of the spirometry performed within the first year after ARDS, obstructive and restrictive impairments were seen at a rate of 6 to 43% and restrictive impairments at a rate of 15 to 58%.[25] Restrictive problems may develop due to pulmonary fibrosis and the weakness of the respiratory muscles. In general, diffusion capacity is the most affected functional parameter. Throughout the first year, after showing an increase from 62 to 63% of the expected value up to 72 to 77%, the diffusion capacity plateaus at the lower limit of the normal range or even at a somewhat lower value.[27,28] In a 6-minute walk test performed to assess cardiopulmonary functional capacity, the walking distance for the age group concerned increased from 49% of the expected value up to 66 to 75%, remaining lower than the normal level even later during the first year after discharge from the hospital.[25,27,28] As in cases of ARDS, due to other causes, advanced age and comorbidities are reported as risk factors for COVID-19, as well. In a multivariate analysis, advanced age, high Sequential Organ Failure Assessment (SOFA) scores, and a D-dimer level of >1 μg/mL at the time of admission were found to be associated with higher mortality.[1] In COVID-19-associated ARDS cases, long- term mortality and morbidity data are not available currently; however, for certain individuals, there will be definitely a restriction of pulmonary function. However, in a Cochrane review on ARDS, there is no sufficiently high-level evidence demonstrating that the initiation of rehabilitation activities during the intensive care process will improve the functional status.[29]
Diagnosis
The clinical diagnostic method for COVID-19 is the identification of the nucleic acid with real-time PCR on nasal and throat swab samples or other respiratory tract samples.[14] Laboratory findings are usually non-specific. The white cell count is mostly normal or low. There can be lymphopenia, and a lymphocyte count of less than 1,000 has been associated with severe disease. Platelet counts are usually normal or mildly decreased. C-reactive protein (CRP) serum levels and erythrocyte sedimentation rate (ESR) are frequently elevated, but procalcitonin levels are normal. A high procalcitonin level can show a bacterial co-infection. Alanine aminotransferase (ALT), aspartate aminotransferase (AST), prothrombin time, creatinine, D-dimer, creatine phosphokinase (CPK), and lactate dehydrogenase (LDH) can be elevated and high levels associated with severe disease can be observed. Chest X-rays often demonstrate bilateral infiltration; however, they can be normal during early disease. Computerized tomography (CT) is more sensitive and specific than plain radiograph. Infiltrates, ground-glass opacities, and lower segment consolidation can be observed on CT imaging.[30]
Meanwhile, the guidelines by the Republic of Turkey, Ministry of Health define the patients complying with the diagnoses of pneumonia and severe pneumonia and the indications for admission to ICU for our country in detail (Table 1).[31,32]
Table 1. COVID-19 outpatient and emergency room, clinic and intensive care admission indications according to the Republic of Turkey Ministry of Health clinical guidelines[32].
| Disease stage | Hospitalization department | The clinical picture seen with COVID-19 (+) positivity |
| Patients with uncomplicated disease presentation | General Ward | a. There are findings like fever, muscle/joint pain, cough, sore throat and nasal congestion, there is no respiratory distress or tachypnea, SpO2 level in room air is not below 93% |
| b. Patients have no underlying comorbidities (primarily cardiovascular diseases, DM, HT, cancer, chronic pulmonary diseases and other immunocompromised states) and are below 50 years of age | ||
| c. There are no adverse prognostic criteria in blood samples obtained at the time of admission (blood lymphocyte count <800/μL or CRP>40 mg/L or ferritin >500 ng/mL or D-Dimer >1000 ng/mL, etc.), | ||
| d. Patients with normal lung X-ray and tomography | ||
| Patients complying with mild pneumonia/severe pneumonia definitions | General Ward | a. There are findings like fever, muscle/joint pain, cough, sore throat and nasal congestion, respiratory rate is <30/min), SpO2 level is above 90% in room air |
| b. Patients have no underlying comorbidities (primarily cardiovascular diseases, DM, HT, cancer, chronic pulmonary diseases and other immunocompromised states) and are below 50 years of age, | ||
| c. There are no adverse prognostic criteria in blood samples obtained at the time of admission (blood lymphocyte count <800/μL or CRP >40 mg/L or ferritin >500 ng/mL or D-Dimer >1000 ng/mL, etc.), | ||
| d. Patients with findings of mild pneumonia on lung X-ray or tomography | ||
| Hospital admission indications for patients complying with mild pneumonia/severe pneumonia definitions | Intensive care | a. There are findings like fever, muscle/joint pain, cough, sore throat and nasal congestion, tachypnea (≥30/min) is present, SpO2 level is below 90% in room air |
| b. Blood samples obtained at the time of admission have adverse prognostic criteria (blood lymphocyte count <800/μL or CRP >40 mg/L or ferritin >500 ng/mL or D-Dimer >1000 ng/mL, etc), | ||
| c. Patients with findings of bilateral pneumonia on lung X-rays or tomography | ||
| Severe pneumonia | Intensive care (advanced level) | a. Presence of dyspnea and respiratory distress |
| b. Respiratory rate >30/min | ||
| c. PaO2/FiO2 100/min | ||
| d. Development of acute organ dysfunctions like acute renal failure, acute abnormality of liver function tests, confusion, acute hemorrhagic diathesis and immunocompromised patients | ||
| e. Troponin elevations and arrhythmia | ||
| f. Lactate >2 mmoL | ||
| g. Capillary return abnormality and presence of skin disorders like cutis marmorata | ||
| DM: Diabetes mellitus; HT: Hypertension; CRP: C-reactive protein; SpO2: Oxygen saturation; PaO2: Partial pressure of arterial oxygen; FiO2: Fraction of inspired oxygen. | ||
Treatment
Currently, there is no specific antiviral drug or vaccine for COVID-19. In general, symptomatic treatment is recommended for patients with mild symptoms and oxygen therapy is recommended for severe cases. In case of respiratory failure resistant to oxygen therapy, mechanical ventilation may be required, while hemodynamic support is crucial for the management of septic shock. Although there is no approved antiviral regimen yet, the use of drugs such as lopinavir/ritonavir, remdesivir, favipiravir, emtricitabine, chloroquine and hydroxychloroquine, and azithromycin has been recommended. Remdesivir is an RNA polymerase inhibitor which has an in vitro activity on multiple RNA viruses including Ebola virus; however, there are contradictory results in studies. It may be considered as an alternative treatment.[2,33,34]
Pulmonary Rehabilitation[35-38]
In a patient-specific manner, PR is planned based on a detailed patient assessment including but not limited to training, exercise, and behavioral changes, since it aims at improving the physical and psychological status of individuals with chronic respiratory disease and focuses on comprehensive interventions for long-term commitment to health improvement attitudes.[35] Although PR has classically been defined for the treatment of chronic diseases, it is also needed and implemented during the course of different pulmonary diseases and during immobility, surgery, and systemic, neurological, and musculoskeletal diseases which impair breathing.
According to the clinical classification of COVID-19 by the WHO, the respiratory system is significantly affected during the stages of mild pneumonia to severe pneumonia and severe pneumonia to ARDS of the disease.[20] As there are no sufficient data regarding the long-term results, the extent of damage or sequelae after the active stage of the disease is not known. The PR procedures will be definitely necessary for the right patient at the right time. The main goals of PR are:
to maintain the respiratory flow through the tract; to decrease the resistance by positioning, mobilization, effective cough, and other bronchial hygiene techniques; and to improve ventilation,
to decrease dyspnea and achieve relaxation,
to maintain optimal position and functioning of the diaphragm and other respiratory muscles,
to slow down the respiratory rate with a proper respiratory pattern that reduces respiratory work/load and decreases air trapping,
to improve the chest mobility and to prevent and/or correct secondary postural deformities with appropriate exercises,
to improve endurance and general exercise tolerance,
to diminish/eliminate anxiety and depression,
to recover functional loss and to improve quality of life.
The scope of PR includes the following components:
Patient education and smoking cessation
Family and caregiver education
Exercise training; respiratory and peripheral muscle training, and breathing strategies
Bronchial hygiene techniques
Breathing strategies
Occupational therapies
Nutritional evaluation and support
Psychosocial evaluation and support
Long-term oxygen therapy
Utilization of non-invasive and invasive mechanical ventilation
Among the elements of PR, exercise training is the most effective and compulsory method in achieving the goals of PR. Exercise and other rehabilitation approaches are demonstrated in Appendix 2.
In patients with COVID-19 pneumonia or ARDS, a multidisciplinary and holistic approach in COVID-19 management encompasses the PR with the selection of appropriate components listed above according to the individual needs of each patient. Although indications of PR specific to COVID-19 still remain unclear, general indications can be listed as follows, when the effects of the disease on the respiratory system and its consequences are taken into consideration:
During the acute disease stage, dyspnea, cough, difficulty in expectoration, respiratory failure, gas exchange abnormalities, and immobility
Difficulty in daily living activities due to decreased functional status
Nutritional deficiency
Impaired quality of life
Psychosocial problems
Fatigue and chronic respiratory symptoms (in the long-term)
Decreased work performance/productivity
Increased utilization of medical resources associated with hospital and emergency room admissions due to chronic respiratory problems secondary to COVID-19.
Protection
The most important routes of transmission for COVID-19 between humans are close contact and droplet spread. Therefore, healthcare workers who provide service to these patients are regarded as having a high risk for transmission. The protection of healthcare workers is one of the most important priorities. There are guidelines developed by both the WHO.[1,39] and the Republic of Turkey, Ministry of Health.[2] concerning the use of personal protective equipment (PPE). According to these guidelines, healthcare workers having contact with possible/ confirmed COVID-19 patients have to use appropriate PPE, while assigning contact, droplet, and airborne precautions. The risks for healthcare workers having contact with COVID-19 patients should be categorized based on the procedures they perform and the preventive measures they implement at the time of contact. After identifying the contact risks as low, moderate or high, healthcare workers should be followed with prespecified algorithms. For all the patients diagnosed with COVID-19, healthcare workers must use surgical masks, gowns, gloves, and goggles/shields during the patient care/treatment. During procedures with the potential of aerosol transmission of the virus (i.e., respiratory tract sampling, close distance examinations, all types of invasive procedures, and respiratory secretion aspirations), healthcare workers must definitely use particle-blocking masks (N95). According to the guideline published by the Republic of Turkey, Ministry of Health, the risk stratification has not been made for PR bronchial drainage techniques, such as assisted coughing techniques, respiratory exercises, postural drainage, and percussion. However, some of the published guidelines state that all these procedures would lead to aerosol production and that the healthcare workers must definitely use an N95 mask.[40,41] Healthcare workers must also respect the sequencing rules, while putting on and taking off PPE.
Objective of the Guideline
This national guideline was prepared to inform primarily the physical medicine and rehabilitation (PMR) specialists and other physicians who are involved in the management of COVID-19 patients. This guideline provides recommendations regarding the PR methods during the clinical stages of COVID-19 with its possible benefits, contraindications, and disadvantages.
Scope of the Guideline
This guideline is prepared in the light of COVID-19 diagnosis and treatment guidelines of the WHO and the Republic of Turkey, Ministry of Health, Public Health General Directorate,[1,2] of published articles on COVID-19 treatment, and published expert opinion recommendations on PR for COVID-19. It contains recommendations for adult patients. The guideline includes PR recommendations for different clinical presentations of COVID-19 to help patients recover the disease. While these recommendations were developed, the transmissibility of COVID-19, the principle of a limited number of healthcare workers having contact with the patient, and the level of benefits to be provided by PR were taken into account.
Method for Guideline Development
For the purpose of developing a PR guideline to be used in the treatment of COVID-19 patients, PMR specialists who are experienced in the field of cardiopulmonary rehabilitation were invited to work together under the coordination of the Cardiopulmonary Rehabilitation Study Group of the Turkish Society of Physical Medicine and Rehabilitation Specialists. The same group published the Pulmonary Rehabilitation after COVID-19 short guideline on March 25th, 2020, as an expert opinion.[42] Following this fast and brief guideline, preparation of a more detailed PR clinical practice guideline was decided on March 30th, 2020. The Turkish Society of Physical Medicine and Rehabilitation and the Turkish Society of Physical Medicine and Rehabilitation Specialists moved forward together to develop the guideline and Cardiopulmonary Rehabilitation Study Group of the Turkish Society of Physical Medicine and Rehabilitation Specialists drafted the guideline on behalf of these two associations. The steps listed below were followed in the preparation of the guideline:
The AGREE II framework was followed in the development of the guideline.[43]
The literature search was conducted on PubMed, CINAHL, Google Scholar, Cochrane and related online databases. In the literature review, guidelines and recommendations during the last decade, meta-analyses, systematic reviews, randomized studies, and websites of relevant agencies such as the WHO and Republic of Turkey, Ministry of Health were analyzed. The language of the literature search was English. Furthermore, references translated into Turkish were also used. Keywords were identified as “Coronavirus pneumonia”, “Rehabilitation AND Coronavirus infection”, “COVID-19”, “SARS- CoV-2”, “ARDS”, “SARS”, “MERS”, “Influenza pneumonia”, “Pulmonary rehabilitation AND Pneumonia”, “Respiratory rehabilitation AND respiratory failure”, and “Rehabilitation AND Critically ill patient”.
After all the participants reviewed the data obtained by this search, key research questions were prepared in accordance with the PICO framework.[44] The prepared questions were individually reviewed by five of the authors (FK, NKOG, SÜD, TT, YKA), similar questions were combined, and the questions were arranged for a common language and for the sake of clarity. The questions were tailored according to the Delphi technique and the final version was approved unanimously by the five- member group.
One hundred and ninety questions were prepared and sent to all the participants with the Qualtrics Program to be reviewed by the Delphi technique. In the light of scientific publications and personal experience, the participants were asked to mark each question as “Yes”, “No” or “Do not know/Neutral”. The questions receiving more than 70% of the common view were approved as the research questions and those receiving less than 70% of consensus were re-evaluated by the participants. In the second round, the questions approved with a rate of 65% were accepted as the research questions.
Based on the results obtained from the research questions, five authors (FK, NKOG, SÜD, TT, YKA) prepared the recommendations, and these recommendations and the final version of the guideline were presented for the approval of all the participants.
RECOMMENDATIONS
Most of the literature on the definition of PR and the effectiveness of different methods on mortality and morbidity is based on experience about chronic pulmonary disease and mainly COPD. There is no literature with high evidence data about the use of PR for acute respiratory failure/ARDS, COVID-19 and similar acute infectious conditions. Therefore, while preparing a PR guideline for COVID-19, there was a need to consider the characteristics of this disease and its transmissibility together with the results of other methods whose efficacy were investigated for chronic diseases in order to prioritize condition appropriate and individualized recommendations. In the preparation of the recommendations for PR applications the following topics were emphasized:
Recommendations for acute and early post- acute COVID-19 are presented. According to the problems that will arise in the chronic period, when there is no risk of contagiousness, an individualized rehabilitation approach will be implemented within the framework of standard PR and basic rehabilitation principles.
Each patient should be evaluated individually before PR.
Assessments which require any equipment such as pulmonary function tests or cardiopulmonary exercise test is not recommended, when there is a risk of contagiousness.
Psychosocial and nutritional assessments are recommended, before PR and management of any problems should be provided.
Given the fact that all types of rehabilitation practices entail a high level of transmission risk, rehabilitation services should be planned based on the isolation and protection principles, the source of PPE, the staff and infrastructure characteristics of the COVID-19 center. Due to similar reasons, rehabilitation can be provided at home following a single training session through visual materials or tele-rehabilitation.
Bronchial hygiene techniques such as assisted cough, postural drainage and percussion, breathing exercises and mobilization which can trigger cough carry the risk of aerosolization and, therefore, healthcare workers should wear appropriate PPE.
Certain PR and general rehabilitation applications may lead to clinical deterioration by increasing the respiratory workload in acute COVID-19 infection. Rehabilitation programs should be individualized and closely monitored. Close communication with the primary physician of the patient about the clinical course is recommended.
Cardiac and neurological involvements secondary to COVID-19 should be taken into consideration, while planning the PR program.
Patients and their families and/or caregivers should be educated regarding the PR program.
COVID-19 patients with severe lung involvement are expected to develop physical, functional, cognitive, and psychosocial sequelae. It is important to organize rehabilitation programs to address these impairments.
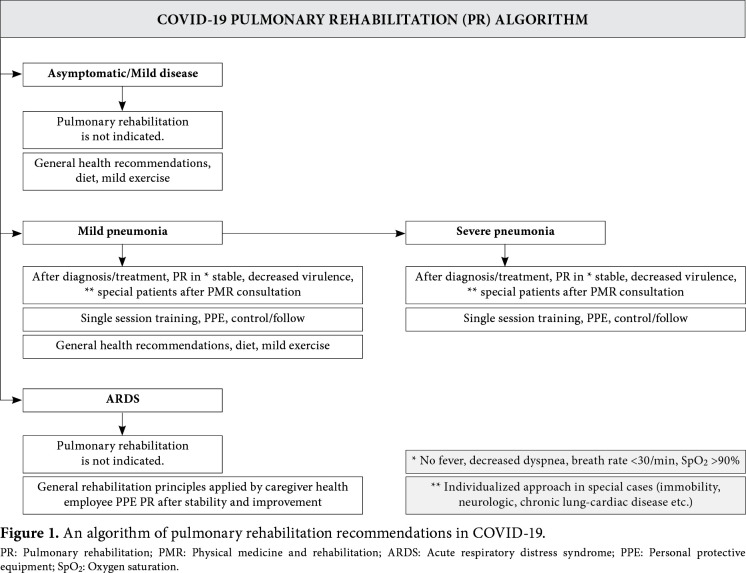
A summary of recommendations is presented in Table 2 and an algorithm is presented in Figure 1.
Table 2. A summary of pulmonary rehabilitation recommendations in COVID-19.
| Pulmonary rehabilitation | Conditions and methods | |
| Mild disease | Pulmonary rehabilitation is not indicated | a. Individualized approach in special cases (immobility, neurologic, chronic lung-cardiac disease etc.) |
| b. General health recommendations | ||
| - Diet | ||
| - Home exercise program | ||
| Pneumonia | a. PR in patients; | a. Individualized approach in special cases (immobility, neurologic, chronic lung-cardiac disease etc.) |
| - With good general condition, | b. General health recommendations | |
| - No fever/dyspnea/tachipnea, | - Diet | |
| - Normal oxygen saturation level, - Decreased viral load | - Home exercise program c. PPE | |
| - Special cases | d. Single session training, home program | |
| b. Pulmonary rehabilitation is not indicated in non-productive cough. | ||
| Severe pneumonia | PR indication decided by PMR physician in patients; | a. Medical stability is a must |
| - After the diagnosis of Covid-19 pneumonia and start of drug treatment by the physician, | b. Stop if patient gets worse during PR | |
| - General condition stabilized (such as fever, decreased dyspnea, respiratory rate <30 breaths/min, SpO2 >90%) | c. Individualized approach in special cases (immobility, neurologic, chronic lung-cardiac disease etc.) | |
| - decreased viral load (mean 10 days later) | d. PPE | |
| e. Single session training if possible | ||
| f. Follow the patient | ||
| Acute respiratory distress syndrome (ARDS) | Pulmonary rehabilitation is not indicated. | a. General rehabilitation measurement handled by the caregiver health employee |
| b. PPE | ||
| c. PR after medical stability | ||
| PR: Pulmonary rehabilitation; PMR: Physical medicine and rehabilitation; PPE: Personal protective equipment. | ||
1. MILD DISEASE STAGE
RECOMMENDATION 1.1
There is no need to perform pulmonary rehabilitation in COVID-19(+) asymptomatic individuals and during the mild disease stage.
Clinical symptoms are mild during the mild disease stage. As in the case of any mild disease, it is important that these individuals stay home and achieve a balance between rest and physical activity by paying attention to their symptoms. At a time when it is compulsory for all asymptomatic individuals to stay at home, indoor exercises such as marching on spot, joint range of motion (ROM) exercises to fatigue limit are advised to refrain from adverse effects of physical activity restriction.
RECOMMENDATION 1.2
During the mild disease stage, preventive measures such as cessation of smoking and management of excess weight that affects the pulmonary system, adequate fluid intake, and supportive measures (daily intake of 2 g/kg protein, vitamin C, zinc, selenium and high fiber content in the diet) should be taken.[45-50]
RECOMMENDATION 1.3
Pulmonary rehabilitation is recommended to individuals with special conditions (elderly, immunocompromised, or limited mobility/ immobility due to stroke, etc.) and with primary pulmonary disease and program should be individualized.
These individuals should be evaluated by a PMR specialist, and the program should be revised accordingly.
2. MILD PNEUMONIA STAGE
RECOMMENDATION 2.1
After the treatment of COVID-19 mild pneumonia is started and when patient’s condition is stabilized (decreased fever, reduced dyspnea, a respiratory rate <30 breaths/min, oxygen saturation [SpO2] >90%) and virulence decreases, it is recommended to apply an individualized PR program in patients deemed appropriate after evaluation.
For patients with mild COVID-19, pneumonia measures for the management of smoking and excess weight and easing the expelling of secretions (by increasing fluid intake, making sure that the air is not dry, or using cold vapor, etc.) for the possible progression of the disease into pneumonia should be taken and sleep hygiene recommendations should be given.
For patients with mild COVID-19 pneumonia who are eligible, the PR program includes active-assisted or active ROM exercises, achieving mobilization, whole body muscle strengthening exercises, incentive spirometry for patients having sputum and productive cough, the utilization of devices for individual use such as Tri-f low, f lutter breathing device, acapella, cornet, and positive expiratory pressure (PEP) and having sputum expelled with controlled cough and huffing maneuvers and finally breathing techniques. As these activities result in aerosol formation, necessary measurements should be taken on relevant measures to prevent spreads to the environment (e.g., collecting the sputum in closed plastic bags).[51]
It is not necessary to use airway clearance techniques for patients who have a dry cough and no sputum.
At this stage, PR to be used is thought to help deal with problems such as dyspnea, cough and sputum, muscle weakness that may develop in respiratory and other body muscles, immobilization, anxiety and depression; however, there are no such data available in the context of evidence-based medicine.
RECOMMENDATION 2.2
Recommendation for patients with special conditions (elderly, immunocompromised, limited mobility or immobility due to causes like stroke, etc.) and individuals with respiratory system diseases having mild pneumonia should be different.
These individuals should be evaluated by a PMR specialist and the program that the patient continues to follow at home should be revised or a new home-based program should be recommended.
RECOMMENDATION 2.3
The use of individual devices, mobilization techniques, and exercises deemed appropriate for the patient by the PMR specialist should be instructed to the patient by one of the rehabilitation team members during a single session. Some or all of these practices can be performed by the PMR physician or existing healthcare personnel (nurse, physiotherapist, occupational therapist, physiotherapy technician) depending on the existing conditions, and availability of human resources and PPE at the center.[52] It is recommended to perform a daily follow-up of the activities instructed to the patient.
During these activities, PPE complying with the standard definitions of the Republic of Turkey, Ministry of Health must be used.
In patients with mild pneumonia whose follow- up and treatment are deemed appropriate at home, a home-based program can be offered using printed and visual materials, videos, social media, or tele- rehabilitation depending on the cognitive status of the patient.
3. SEVERE PNEUMONIA (COVID-19 POSITIVE OR POSSIBLE COVID-19)
RECOMMENDATION 3.1
After evaluation by a PMR specialist, it is recommended to plan an individualized PR program for patients with severe COVID-19 pneumonia, if the patient fulfills the criteria.
After the assessment of the general physical condition, fever, symptoms of respiratory system such as dyspnea, cough, respiration rate, SpO2, blood tests, radiological findings, ROM, respiratory and whole body muscle strength, in-bed activities, functional capacity, exercise capacity and other comorbidities, a rehabilitation program appropriate for the current impairments of the patient should be planned.
Although it is thought that PR to be implemented during this period will help to relieve symptoms such as dyspnea, cough, sputum, weaknesses of respiratory and other body muscles, immobilization, and anxiety and depression, there are no such data available in the context of evidence-based medicine. The evidence obtained from studies evaluating the effectiveness of PR is mostly derived from researches including individuals with chronic pulmonary diseases.[35,37,53,54]
RECOMMENDATION 3.2
It is recommended to start implementing the pulmonary rehabilitation program, after the patient becomes medically stable.
Following the establishment of a diagnosis of COVID-19 pneumonia and the initiation of medical treatment by the primary physician, it is recommended to start PR, when the general condition of the patient becomes stable (decreased fever, reduced dyspnea, respiratory rate <30 breaths/min, SpO2 >90%) and the viral load decreases.
During these activities, PPE complying with standard definitions of the Republic of Turkey, Ministry of Health must be used.
RECOMMENDATION 3.3
It is recommended to discontinue pulmonary rehabilitation, if there is a deterioration of the general health condition of the patient and a worsening of pulmonary findings.
The program should be discontinued, if there is an increase in the respiratory workload of the patient and an increase in dyspnea, if the respiratory rate is >30 breaths/min, SpO2 is <90% under oxygen therapy, or there is a decrease of more than 4% compared to baseline, resulting in hypoxemia and desaturation, a fraction of inspired oxygen (FiO2) of >50% or positive end-expiratory pressure (PEEP)/continuous positive airway pressure (CPAP) of >10 cmH2O is seen during non-invasive ventilation and there are onset and continuation of symptoms such as high fever, chest pain and a feeling of pressure, vertigo, tinnitus, severe headache, visual impairment, palpitation, profuse sweating and imbalance and more than 50% progression of the radiological lesion within 24 to 48 hours.[40,41,51,55-58]
RECOMMENDATION 3.4
Although the pulmonary rehabilitation program is individualized according to the condition of the patient, it should basically include techniques used for acute stage pneumonia.
During this period, the signs and findings listed in Recommendation 3.3 should be closely followed:
Positioning in bed and frequent position changes should be made; in cases with severe pneumonia and/or using non-invasive mechanical ventilators, a semi-sitting or sitting position is recommended to prevent the risk of aspiration. While positioning, aids such as pillows can be used to minimize effort.
Mobilization as soon as possible (sitting position in bed, sitting on the edge of the bed, transfer to the chair, and standing with the help of a tilt table)
Progressive ambulation of patients who can tolerate mobilization with the help of walking aids
Active-assisted and active joint ROM exercises
Isometric muscle strengthening
Neuromuscular electrical stimulation (NMES) (by selecting 4 to 6 muscles).
If the respiratory muscles are weak, teach the inspiratory muscle training exercises. Measurement of respiratory muscle strength requires the use of portable maximal inspiratory pressure and maximal expiratory pressure (MIP-MEP) devices. The measurement process increases aerosolization and respiratory muscle training can also be a method which increases hypoxemia. Therefore, it should be preferred to apply, only after the patient's clinical status is improved.
For patients having sputum and productive cough, prescriptions of devices for personal use such as incentive spirometry, Tri-flow, f lutter breathing device, acapella, cornet, and PEP should be given and instructed; the patient should be taught how to expel the sputum accumulated and the central airways should be cleared by maneuvers such as controlled cough and huffing with the help of these devices.
Airway clearance techniques should not be used in patients who have a dry cough and no sputum.
The use of controlled breathing techniques such as diaphragmatic breathing, alternate breathing, and pursed-lip breathing can be attempted in patients having respiratory diseases such as COPD. It should be kept in mind that the use of these techniques can increase the respiratory workload during the acute stage of the disease and can lead to deterioration of the patient’s condition.
Nutritional support; a carbohydrate-restricted diet should be introduced to decrease respiratory failure and carbon dioxide accumulation; attention should be paid to conditions including hypophosphatemia, hypomagnesemia, and hypocalcemia that can aggravate respiratory failure.
During these activities, PPE complying with standard definitions of the Republic of Turkey, Ministry of Health must be used.
RECOMMENDATION 3.5
The use of individual devices, mobilization techniques and exercises deemed appropriate for the patient by the PMR specialist should be instructed to the patient by one of the rehabilitation team members during a single session. Some or all of these practices should be performed by a PMR physician and available healthcare personnel (nurse, physiotherapist, occupational therapist, physiotherapy technician) depending on the existing conditions and availability of human resources and PPE at the center.
General rehabilitation practices such as positioning, mobilization, ROM, general muscle strengthening exercises in the aforementioned recommendations can be demonstrated by a physiotherapist, occupational therapist, or nurse with the prescription of a PMR specialist. Tele-rehabilitation, video or other visual materials can be used in the presence of eligible infrastructure and if the patient's cognitive status is appropriate. The PR practices (bronchial hygiene techniques, other respiratory strategies, respiratory muscle strength training and training of devices used for these purposes, etc.) require an active participation of the patient, and one-on-one training should be provided by a team of specialists with the prescription PMR specialist.
During these activities, PPE complying with the standard definitions by the Republic of Turkey, Ministry of Health must be used.
ACUTE ARDS STAGE OF COVID-19 INFECTION
RECOMMENDATION 4.1
Pulmonary rehabilitation is not recommended for patients at the acute stage of COVID-19 ARDS, except for passive ROM exercises and secretion management.
PR is not appropriate or safe for patients who are at the active and acute stage (cases during the first 10 days of the admission to the ICU) who have a fever, a respiratory rate of >30 breaths/min, an SpO2 of <90% despite oxygen support, a FiO2 of >50% on a non-invasive mechanical ventilator and PEEP/CPAP >10 cmH2O, who are in respiratory stress, bradycardia, tachycardia or variable arrhythmias, who are in shock or deep sedation, and whose radiological progression has been continuing for 24 hours.[40,41,51,55-58]
In patients requiring secretion management, these procedures should be done in negative pressure rooms and closed systems, as this may cause aerosol formation. Mechanical insufflator and exufflator (MI-E) and Vest-like devices, which are other airway cleaning techniques used in the intensive care, should be used very carefully considering the benefit/harm due to aerosol formation.
RECOMMENDATION 4.2
General rehabilitation principles should be followed in COVID-19 patients with ARDS.[39]
General rehabilitation principles:
The patients should be followed for difficulty in weaning from the ventilator and spontaneous breathing.
To refrain from ventilator-associated pneumonia, a semi-sitting position is recommended and, when possible, all aspiration processes should be performed within closed systems. In addition, the patients need to be followed for the involvement of posterior lung fields and prone position that increases oxygenation should be tried for 12 to 16 hours, if applicable. In this process, while shifting from a supine position to prone position, the patient safety should be ensured and all the catheters on the patient should be safely monitored.
The patient should be protected from venous thromboembolism, and the use of pressure stockings and anticoagulants should be decided upon by taking into consideration benefit/ harm, particularly in high-risk patients.
Patients should be carefully inspected for bedsores. A particular attention should be paid to the proper positioning.
Joint contractures should be considered. Contractures can develop in major joints, specifically such as shoulder, elbow, hip, knee and ankle during the first 10 days. Therefore, ROM exercises should be performed in specific joints 15 times once a day, when the patient is in the supine position. The patient should do active exercises, if possible or should be encouraged to do.
Electrical stimulation modalities such as NMES can be used in patients with muscle weakness for large muscle groups at an intensity which does not cause any burns.
Nutritional support; a carbohydrate-restricted diet should be given to decrease respiratory failure and carbon dioxide accumulation; attention should be paid to conditions including hypophosphatemia, hypomagnesemia, and hypocalcemia that can aggravate respiratory failure.
The general rehabilitation principles to be implemented during this period should not hinder the clinical stability of the patient; therefore, close monitoring should be made. If the respiratory rate is >30 breaths/min, SpO2 is below 90% despite oxygen support therapy, FiO2 is >50% on a non-invasive ventilator and PEEP/CPAP is >10 cmH2O and bradycardia, tachycardia, and variable arrhythmias appear, the applications need to be discontinued.[51]
After the cytokine storm and excessive viral load disappears and all the signs of infectionare normalized, slow mobilization exercises can be started, if the general condition of the patient allows and if the patient is cooperated.
Besides these exercises, self-care activities can be initiated in patients who are able to start daily living activities.
RECOMMENDATION 4.3
The patient whose clinical findings started improving after the acute and subacute stage, who is stable and who is to be disconnected from the mechanical ventilator needs to be evaluated together with the PMR physician and the attending physicians to decide about the timing and appropriateness of rehabilitation including pulmonary. For the patients who are eligible for general rehabilitation, Recommendation 2 applies. If the patient who is a candidate for PR has a severe cough, he/she can be, then, followed with recommendations for COVID-19 patients with severe pneumonia.
RECOMMENDATION 4.4
The patient who progresses to the post-ARDS period is evaluated by the PMR physician for all rehabilitation recommendations including PR and programs after leaving the ICU. Following this evaluation, a patient-specific rehabilitation program is prepared and other components of rehabilitation can be added.
During the evaluation process, the general physical condition of the patient, blood tests, radiological findings, respiratory parameters, joint ROM, muscle strength, respiratory muscle strength, activities of daily living, functional capacity, and other existing comorbid conditions are considered. At the current stage, respiratory muscle exercises (inspiratory muscle training, expiratory muscle training, respiratory muscle strategies (controlled respiratory techniques, bronchial hygiene techniques)) and aerobic muscle training, progressive resistive exercises and shoulder girdle and upper extremity exercises can be recommended, only if the patient’s status allows.
5. REHABILITATION APPROACH AFTER DISCHARGE in COVID-19
RECOMMENDATION 5.1
In the post-discharge period, the rehabilitation program with a holistic approach is organized within the scope of general rehabilitation principles by evaluating the impairments in physical, functional, cognitive, psychosocial, and occupational aspects associated with COVID-19.
Depending on the scope of the rehabilitation program, the place and model of application (i.e., inpatient, outpatient, hospital-centered control, home-based program, or tele-rehabilitation, etc.) should be determined.
The Strengths of the Guideline
As is the case worldwide, the number of COVID-19 cases has been on a rise in our country. This guideline has been prepared considering the local health practices in our country. We believe that it will provide guidance primarily to PMR specialists and to all physicians. The PMR specialists who are involved in the development of this guideline are experienced in PR and they routinely follow COVID-19 patients in Turkey, as well. Hence, this guideline will create an opportunity for sharing patient evaluation experiences in accordance with the existing COVID-19 treatment guidelines.
The Limitations of the Guideline
This guideline has been prepared with the aim of incorporating the principles of PR with scientific data pertaining to the COVID-19 pandemic which has started nearly a month ago. As our knowledge of COVID-19 and post-recovery patients grows, this guide will need to be further developed. Due to time constraints during the preparation of this guideline, we were unable to refer to the opinions of other healthcare staff taking part in the PR process. As COVID-19 is an acute disease and has a wide spectrum of clinical presentations, patient experiences and opinions were not included in this guideline, either.
The Time and Method for Revision
Following the publication of this guideline, we aim at revising it with the participation of a larger group of healthcare personnel after evaluating the results of clinical applications and mid-term results of patients within a period of three to six months.
Figure 1. An algorithm of pulmonary rehabilitation recommendations in COVID-19. PR: Pulmonary rehabilitation; PMR: Physical medicine and rehabilitation; ARDS: Acute respiratory distress syndrome; PPE: Personal protective equipment; SpO2: Oxygen saturation.
Appendix 1. COVID-19 Clinical Classification of World Health Organization[20].
Appendix 2. Exercises and other approaches used in pulmonary rehabilitation.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Coronavirus Disease 2019 (COVID-19) Technical Guidance. Available at: https://www.who.int/health-topics/coronavirus#tab=tab_1 .
- 2.COVID-19 (SARS-CoV-2 Enfeksiyonu) Rehberi (Bilim Kurulu Calışması) 24 Nisan 2020 Erişim linki: https://covid19bilgi.saglik.gov.tr/depo/rehberler/COVID-19_ Rehberi.pdf. [Accessed: April 24, 2020]
- 3.Jia HP, Look DC, Shi L, Hickey M, Pewe L, Netland J, et al. ACE2 receptor expression and severe acute respiratory syndrome coronavirus infection depend on differentiation of human airway epithelia. J Virol. 2005;79:14614–14621. doi: 10.1128/JVI.79.23.14614-14621.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor Recognition by the Novel Coronavirus from Wuhan: an Analysis Based on Decade-Long Structural Studies of SARS Coronavirus. e00127-20J Virol. 2020;94 doi: 10.1128/JVI.00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367:1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Donoghue M, Hsieh F, Baronas E, Godbout K, Gosselin M, Stagliano N, et al. A novel angiotensin-converting enzyme- related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1-9. E1-9Circ Res. 2000;87 doi: 10.1161/01.res.87.5.e1. [DOI] [PubMed] [Google Scholar]
- 8.Tortorici MA, Veesler D. Structural insights into coronavirus entry. Adv Virus Res. 2019;105:93–116. doi: 10.1016/bs.aivir.2019.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Wilde AH, Snijder EJ, Kikkert M, van Hemert MJ. Host Factors in Coronavirus Replication. Curr Top Microbiol Immunol. 2018;419:1–42. doi: 10.1007/82_2017_25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sawicki SG, Sawicki DL. Coronavirus transcription: a perspective. Curr Top Microbiol Immunol. 2005;287:31–55. doi: 10.1007/3-540-26765-4_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hussain S, Pan J, Chen Y, Yang Y, Xu J, Peng Y, et al. Identification of novel subgenomic RNAs and noncanonical transcription initiation signals of severe acute respiratory syndrome coronavirus. J Virol. 2005;79:5288–5295. doi: 10.1128/JVI.79.9.5288-5295.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tian S, Hu W, Niu L, Liu H, Xu H, Xiao SY. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID- 19) pneumonia in two patients with lung cancer. J Thorac Oncol. 2020;15:700–704. doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Mil Med Res. 2020;7:4–4. doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7:11–11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. 101623Travel Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51:843–851. doi: 10.1111/apt.15731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borges do Nascimento IJ, Cacic N, Abdulazeem HM, von Groote TC, Jayarajah U, Weerasekara I, et al. Novel Coronavirus Infection (COVID-19) in Humans: A Scoping Review and Meta-Analysis. E941J Clin Med. 2020;9 doi: 10.3390/jcm9040941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.COVID-19 Türkiye Web Portalı . Erişim linki: https://covid19.tubitak.gov.tr/turkiyede-durum. [Accessed: April 24, 2020]
- 20.Clinical management of severe acute respiratory infection when COVID-19 is suspected Interim guidance. Available at: https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected. [Accessed: April 02, 2020]
- 21.Singhal T. A Review of Coronavirus Disease-2019 (COVID- 19) Indian J Pediatr. 2020;87:281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vaira LA, Salzano G, Deiana G, De Riu G. Anosmia and ageusia: Common findings in COVID-19 patients. Laryngoscope. 2020 doi: 10.1002/lary.28692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. e201291JAMA Ophthalmol. 2020 doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chiumello D, Coppola S, Froio S, Gotti M. What's Next After ARDS: Long-Term Outcomes. Respir Care. 2016;61:689–699. doi: 10.4187/respcare.04644. [DOI] [PubMed] [Google Scholar]
- 26.Sigurdsson MI, Sigvaldason K, Gunnarsson TS, Moller A, Sigurdsson GH. Acute respiratory distress syndrome: nationwide changes in incidence, treatment and mortality over 23 years. Acta Anaesthesiol Scand. 2013;57:37–45. doi: 10.1111/aas.12001. [DOI] [PubMed] [Google Scholar]
- 27.Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348:683–693. doi: 10.1056/NEJMoa022450. [DOI] [PubMed] [Google Scholar]
- 28.Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 29.Doiron KA, Hoffmann TC, Beller EM. Early intervention (mobilization or active exercise) for critically ill adults in the intensive care unit. CD010754Cochrane Database Syst Rev. 2018;3 doi: 10.1002/14651858.CD010754.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kooraki S, Hosseiny M, Myers L, Gholamrezanezhad A. Coronavirus (COVID-19) Outbreak: What the Department of Radiology Should Know. J Am Coll Radiol. 2020;17:447–451. doi: 10.1016/j.jacr.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.COVID-19 Türkiye Web Portalı. Erişim linki: https://covid19.tubitak.gov.tr/korunma-tedavi-yontemleri . [Accessed: April 24, 2020]
- 32.COVID-19 Polikliniğine/Acilde Hasta Kabulü ve Takibi (15 yaş ve üzeri vakalar için) Erişim linki: https://covid19.tubitak.gov.tr/sites/default/files/docs/2020-03/covid19-hasta-yonetimi-ve-tedavisi-15-yas-uzeri-icin-23032020.pdf . [Accessed: April 24, 2020]
- 33.Features, Evaluation and Treatment Coronavirus (COVID-19) Available at: https://www.ncbi.nlm.nih.gov/books/NBK554776/ [Accessed: April 24, 2020]
- 34.Wang Y, Zhang D, Du G, Du R, Zhao J, Jin Y, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. The Lancet. 2020 doi: 10.1016/S0140-6736(20)31022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An official American Thoracic Society/ European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. e13-64Am J Respir Crit Care Med. 2013;188 doi: 10.1164/rccm.201309-1634ST. [DOI] [PubMed] [Google Scholar]
- 36.Güell Rous MR, Díaz Lobato S, Rodríguez Trigo G, Morante Vélez F, San Miguel M, Cejudo P, et al. Pulmonary rehabilitation. Sociedad Española de Neumología y Cirugía Torácica (SEPAR) Arch Bronconeumol. 2014;50:332–344. doi: 10.1016/j.arbres.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 37.Bolton CE, Bevan-Smith EF, Blakey JD, Crowe P, Elkin SL, Garrod R, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. ii1-30Thorax. 2013;68 doi: 10.1136/thoraxjnl-2013-203808. [DOI] [PubMed] [Google Scholar]
- 38.Andrianopoulos V, Klijn P, Franssen FM, Spruit MA. Exercise training in pulmonary rehabilitation. Clin Chest Med. 2014;35:313–322. doi: 10.1016/j.ccm.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19): interim guidance, 19 March 2020. Available at: https://apps.who.int/iris/handle/10665/331498 . [Accessed: April 24, 2020]
- 40.Lazzeri M, Lanza A, Bellini R, Bellofiore A, Cecchetto S, Colombo A, et al. Respiratory physiotherapy in patients with COVID-19 infection in acute setting: a Position Paper of the Italian Association of Respiratory Physiotherapists (ARIR) Monaldi Arch Chest Dis. 2020;90 doi: 10.4081/monaldi.2020.1285. [DOI] [PubMed] [Google Scholar]
- 41.Thomas P, Baldwin C, Bissett B, Boden I, Gosselink R, Granger CL, et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. 2020;66:73–82. doi: 10.1016/j.jphys.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.COVID-19 Sonrası Pulmoner Rehabilitasyon. Erişim linki: http://www.tsprm.org/haber.php?id=118 . [Accessed: April 31, 2020]
- 43.Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. Development of the AGREE II, part 1: performance, usefulness and areas for improvement. CMAJ. 2010;182:1045–1052. doi: 10.1503/cmaj.091714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Richardson WS, Wilson MC, Nishikawa J, Hayward RS. The well-built clinical question: a key to evidence-based decisions. A12-3ACP J Club. 1995;123 [PubMed] [Google Scholar]
- 45.Nathens AB, Neff MJ, Jurkovich GJ, Klotz P, Farver K, Ruzinski JT, et al. Randomized, prospective trial of antioxidant supplementation in critically ill surgical patients. Ann Surg. 2002;236:814–822. doi: 10.1097/00000658-200212000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hanson C, Lyden E, Rennard S, Mannino DM, Rutten EP, Hopkins R, et al. The Relationship between Dietary Fiber Intake and Lung Function in the National Health and Nutrition Examination Surveys. Ann Am Thorac Soc. 2016;13:643–650. doi: 10.1513/AnnalsATS.201509-609OC. [DOI] [PubMed] [Google Scholar]
- 47.Patel V, Dial K, Wu J, Gauthier AG, Wu W, Lin M, et al. Dietary Antioxidants Significantly Attenuate Hyperoxia- Induced Acute Inflammatory Lung Injury by Enhancing Macrophage Function via Reducing the Accumulation of Airway HMGB1. Int J Mol Sci. 2020;21:977–977. doi: 10.3390/ijms21030977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fowler AA 3rd, Truwit JD, Hite RD, Morris PE, DeWilde C, Priday A, et al. Effect of Vitamin C Infusion on Organ Failure and Biomarkers of Inflammation and Vascular Injury in Patients With Sepsis and Severe Acute Respiratory Failure: The CITRIS-ALI Randomized Clinical Trial. JAMA. 2019;322:1261–1270. doi: 10.1001/jama.2019.11825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mahmoodpoor A, Hamishehkar H, Shadvar K, Ostadi Z, Sanaie S, Saghaleini SH, et al. The Effect of Intravenous Selenium on Oxidative Stress in Critically Ill Patients with Acute Respiratory Distress Syndrome. Immunol Invest. 2019;48:147–159. doi: 10.1080/08820139.2018.1496098. [DOI] [PubMed] [Google Scholar]
- 50.Boudreault F, Pinilla-Vera M, Englert JA, Kho AT, Isabelle C, Arciniegas AJ, et al. Zinc deficiency primes the lung for ventilator-induced injury. e86507JCI Insight. 2017;2 doi: 10.1172/jci.insight.86507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Joint statement on the role of respiratory rehabilitation in the COVID-19 crisis: the Italian position paper. Available at: https://ers.app.box.com/s/825awayvkl7hh670yxbmzfvcw5medm1d . [Accessed: April 24, 2020] [DOI] [PMC free article] [PubMed]
- 52.Hemşirelik Yönetmeliğinde Değişiklik Yapılmasına Dair Yönetmelik. In., 19 April 2011 edn. Resmi Gazete; 2011. Erişim linki: https://www.resmigazete.gov.tr/eskiler/2011/04/20110419-5.htm . [Accessed: April 24, 2020] [Google Scholar]
- 53.Chinese Association of Rehabilitation Medicine; Respiratory rehabilitation committee of Chinese Association of Rehabilitation Medicine; Cardiopulmonary rehabilitation Group of Chinese Society of Physicai Medicine and Rehabilitation E029(Recommendations for respiratory rehabilitation of COVID-19 in adult) 2020;43 Zhonghua Jie He He Hu Xi Za Zhi. [Google Scholar]
- 54.Ambrosino N, Clini EM. Response to pulmonary rehabilitation: toward personalised programmes. Eur Respir J. 2015;46:1538–1540. doi: 10.1183/13993003.01125-2015. [DOI] [PubMed] [Google Scholar]
- 55.Zhao HM, Xie YX, Wang C. Recommendations for respiratory rehabilitation in adults with COVID-19. Chin Med J (Engl) 2020 doi: 10.1097/CM9.0000000000000848. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.The First Affiliated Hospital ZUSoM: Handbook of COVID-19 prevention and treatment; 2020. Available at: http://www.zju.edu.cn/english/2020/0323/c19573a1987520/page.htm. [Accessed: April 24, 2020] [Google Scholar]
- 57.Yang F, Liu N, Hu JY, Wu LL, Su GS, Zhong NS, et al. Pulmonary rehabilitation guidelines in the principle of 4S for patients infected with 2019 novel coronavirus (2019-nCoV) Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:180–182. doi: 10.3760/cma.j.issn.1001-0939.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 58.COVID-19 (SARS-CoV-2 Enfeksiyonu) Rehberi (Bilim Kurulu Çalışması) 12 Nisan 2020 . Erişim linki: https://covid19bilgi.saglik.gov.tr/depo/rehberler/COVID-19_Rehberi.pdf . [Accessed: April 24, 2020] [Google Scholar]