Abstract
We present the case of a patient with myocardial infarction and COVID-19 disease who developed hemorrhagic pericardial effusion and cardiac tamponade. The differential diagnosis included post-infarction pericarditis and mechanical complications, thrombolysis, Dressler syndrome, and viral pericarditis. The histopathologic examination of the pericardial tissue sample and electron microscopic examination established the diagnosis. (Level of Difficulty: Advanced.)
Key Words: coronavirus, myocardial infarction, tamponade
Abbreviations and Acronyms: COVID-19, coronavirus disease-2019; SARS-CoV-2, severe acute respiratory syndrome-coronavirus-2; TTE, transthoracic echocardiogram
Graphical abstract
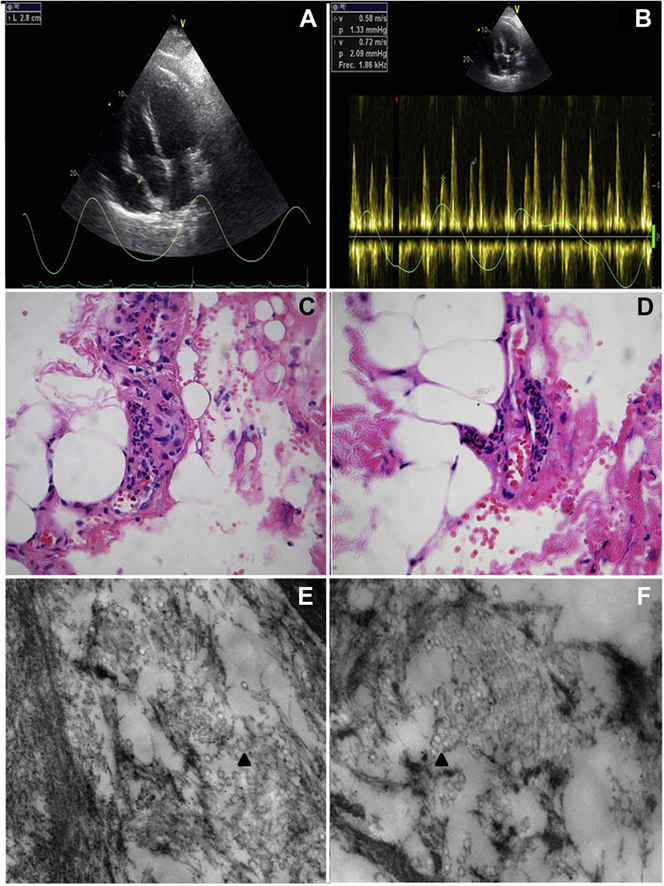
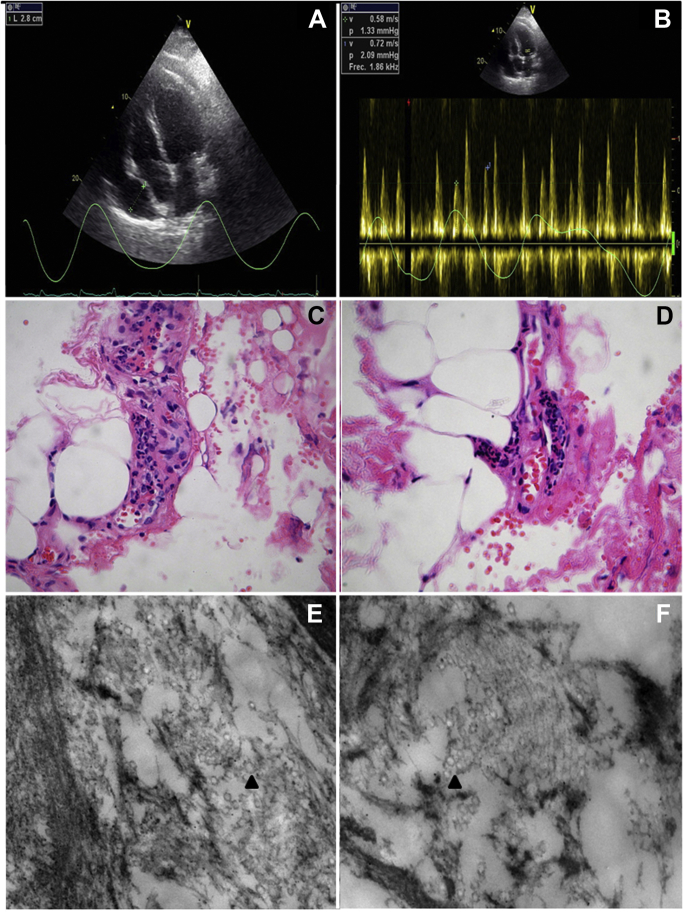
A 64 year-old-man was admitted to the Ignacio Chávez National Institute of Cardiology in Mexico City, Mexico with chest pain, dry cough, and fever (38.3ºC). He was dyspneic, with 85% arterial oxygen saturation, a heart rate of 84 beats/min and blood pressure of 106/87 mm Hg. Diffuse pulmonary rales were found, predominantly at the left lung base. The electrocardiogram showed ST-segment elevation on the inferior and posterior leads. The chest radiograph showed bilateral diffuse interstitial infiltrates, predominantly in the left lung. The result of real-time reverse transcription-polymerase chain reaction for detection of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) RNA was positive, so antiviral therapy was added. A transthoracic echocardiogram (TTE) showed inferolateral and inferior wall akinesia and an ejection fraction of 30% without pericardial effusion. Given the rapid progression (<12 h after chest pain onset), thrombolysis with alteplase was established with reperfusion criteria. On the ninth day of the illness, he had oliguria, sinus tachycardia, and dyspnea. A new TTE showed echogenic pericardial effusion with tamponade physiology (Figures 1A and 1B, Video 1). A pericardial window was performed, with drainage of 750 ml of hemorrhagic fluid. A pericardium sample was sent to the pathology department for evaluation: the hematoxilin and eosin stain findings were compatible with acute pericarditis (Figures 1C and 1D); electron microscopy showed viral particles (Figures 1E and 1F). During the coronavirus-2019 (COVID-19) pandemic, the treatment of ST-segment elevation myocardial infarction has changed to prioritize a safe intrahospital environment with thrombolysis preferred to primary angioplasty (1). In this patient with hemorrhagic pericardial effusion, the differential diagnosis included post-infarction pericarditis, mechanical complications of myocardial infarction, complications associated with thrombolysis, Dressler syndrome, and viral pericarditis. Viral pericarditis has been recognized as the cause of up to 62% of hemorrhagic pericardial effusions (2). The presence of SARS-CoV-2 in pericardial fluid has been recently reported (also hemorrhagic) (3). For this reason, we sent a pericardium sample to the pathology service, where changes compatible with acute pericarditis were found and where the presence of viral particles was documented by electron microscopy, so the final diagnosis was hemorrhagic pericardial effusion with cardiac tamponade secondary to COVID-19. This is the first case reported with histopathologic evidence of the virus in pericardial tissue.
Figure 1.
Viral Hemorrhagic Pericardial Effusion With Cardiac Tamponade
(A) Transthoracic echocardiographic apical 4-chamber view with separation of pericardial layers of 28 mm. (B) Respiratory variation in transmitral flow of 25%. (C and D) Hematoxylin and eosin–stained sections of the pericardium tissue sample. (C) Capillary congestion and wall infiltration of polymorphonuclear leukocytes (original magnification ×40). (D) Incipient periarteriolar fibrinoid necrosis and leukocyte infiltrate (original magnification ×40). (E and F) Electron microscopy of the pericardium ultrastructure. (E) Viral particles (arrowhead) are shown in a blood vessel (original magnification ×50,000). (F) Viral particles (arrowhead) are shown in the interstitium of a vessel and an epithelial cell (original magnification ×50,000).
Author Relationship With Industry
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Acknowledgments
The authors acknowledge the COVID 19-INC Committee and Marco Antonio Rosas Ortega.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACC: Case Reportsauthor instructions page.
Appendix
For a supplemental video, please see the online version of this paper.
Appendix
Apical 4-Chamber View Showing Diastolic Collapse of the Right Atrium and Ventricle
References
- 1.Jing Z., Zhu H., Yan X., Chai W., Zhang S. Recommendations from the Peking Union Medical College Hospital for the management of acute myocardial infarction during the COVID-19 outbreak. Eur Heart J. 2020;41:1791–1794. doi: 10.1093/eurheartj/ehaa258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meyers D., Meyers R., Prendergast T. The usefulness of diagnostic tests on pericardial fluid. Chest. 1997;111:1213–1221. doi: 10.1378/chest.111.5.1213. [DOI] [PubMed] [Google Scholar]
- 3.Dabbagh M., Aurora L., D’Souza P., Weinmann A., Bhargava P., Basir M. Cardiac tamponade secondary to COVID-19. J Am Coll Cardiol Case Rep. 2020;2:1326–1330. doi: 10.1016/j.jaccas.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Apical 4-Chamber View Showing Diastolic Collapse of the Right Atrium and Ventricle