Abstract
Background and aims
Concerns have arisen regarding patient access and delivery of acute stroke care during the COVID-19 pandemic. We investigated key population level events on activity of the three hyperacute stroke units (HASUs) within Greater Manchester and East Cheshire (GM & EC), whilst adjusting for environmental factors.
Methods
Weekly stroke admission & discharge counts in the three HASUs were collected locally from Emergency Department (ED) data and Sentinel Stroke National Audit Programme core dataset prior to, and during the emergence of the COVID-19 pandemic (Jan 2020 to May 2020). Whilst adjusting for local traffic-related air pollution and ambient measurement, an interrupted time-series analysis using a segmented generalised linear model investigated key population level events on the rate of stroke team ED assessments, admissions for stroke, referrals for transient ischaemic attack (TIA), and stroke discharges.
Results
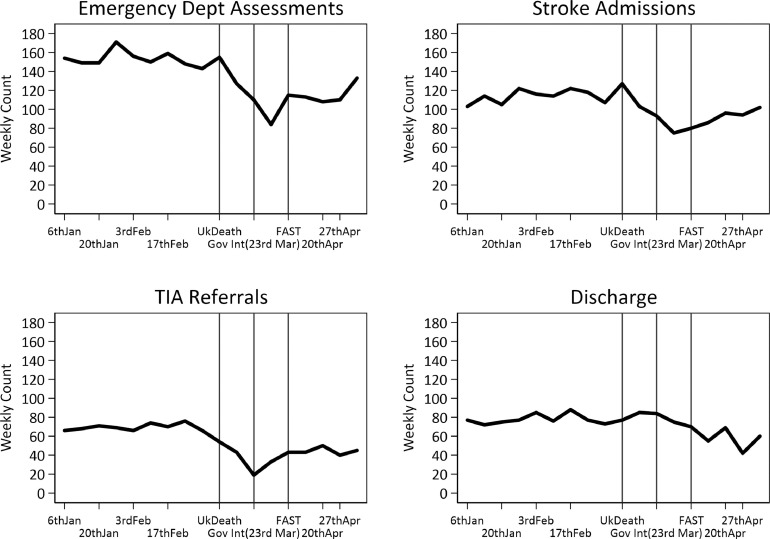
The median total number of ED stroke assessments, admissions, TIA referrals, and discharges across the three HASU sites prior to the first UK COVID-19 death were 150, 114, 69, and 76 per week. The stable weekly trend in ED assessments and stroke admissions decreased by approximately 16% (and 21% for TIAs) between first UK hospital COVID-19 death (5th March) and the implementation of the Act-FAST campaign (6th April) where a modest 4% and 5% increase per week was observed. TIA referrals increased post Government intervention (23rd March), without fully returning to the numbers observed in January and February. Trends in discharges from stroke units appeared unaffected within the study period reported here.
Conclusion
Despite adjustment for environmental factors stroke activity was temporarily modified by the COVID-19 pandemic. Underlying motivations within the population are still not clear. This raises concerns that patients may have avoided urgent health care risking poorer short and long-term health outcomes.
Key Words: COVID-19, Stroke activity, TIA, Interrupted time-series
What this study adds
-
-
This study provides a unique insight into how population level events during the COVID-19 pandemic potentially influenced stroke activity in three specialist Hyperacute Stroke Units serving approximately 3.3 million people across Greater Manchester and Eastern Cheshire.
-
-
We investigated three key population level events; the first recorded UK hospital death from COVID-19, a government proposed intervention (often referred to as lockdown) restricting the spread of the pandemic, and the UK media campaign highlighting the Face Arm Speech Time (FAST) test and stroke awareness.
-
-
During the month between the first UK hospital death from COVID-19 (5th March) and the UK Act-FAST media coverage, we found a reduction in acute stroke activity before a gradual return towards trends observed prior. This included assessments for suspected stroke, stroke service admissions and transient ischaemic attack referrals.
-
-
Although the motivations behind this change are not fully clear, our findings indicate that environmental factors such as traffic related air pollution appeared to have a limited association with the reduction in stroke activity. This raises concerns patients may have avoided health care and in turn the short and longer-term impact on patients' health outcomes.
Introduction
The emergence of the global COVID-19 pandemic, caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), has led to an international public health crisis prompting numerous countries to initiate government intervention (“lockdown”) aimed at containing further spread.1 , 2 Many healthcare systems have been under pressure to meet the demands placed on them by increased hospitalisation and resource utilisation resulting from patients presenting acutely with SARS-CoV-2 infection, and the impact of the pandemic on provision and accessibility of emergency care for other potentially life-threatening conditions is unclear.
Stroke is a leading cause of morbidity and mortality3 where early recognition of symptoms and timely transfer to specialist hospital services are key components of international management guidelines.4 , 5 This is to optimise rapid clinical assessment, brain imaging and time-limited evidence-based interventions such as stroke unit care, intravenous thrombolysis and intra-arterial thrombectomy; and to facilitate investigations, secondary prevention and multi-disciplinary care.
Started in 2014, Act-FAST (Face, Arms, Speech, and Time) is a public health England awareness campaign focused on identifying the early symptoms of stroke and highlighting it as an emergency medical condition that requires urgent medical care. In the early stages of the COVID-19 pandemic, anecdotal and brief published reports suggested an indirect effect on stroke services based on reduction in stroke presentations to hospital services in some studies,6 – 9 but not others.10 In response the National Clinical Director for Stroke increased the media Act-FAST campaign (6th April) in an effort to remind those experiencing stroke or observing it in others that stroke services remained open and to seek out urgent care immediately. However, there are very limited data in UK healthcare systems relating to activity of acute stroke services during the trajectory of the pandemic, with very little understanding of why stroke activity might be changing. One such reason may relate to environmental factors such as traffic related air pollution and ambient temperature. Air pollution that has previously been shown to be associated with stroke, was observed to reduce during the pandemic11 , 12 making it a key confounding factor to any change in stroke activity. We aimed to evaluate the impact of the COVID-19 pandemic on activity of acute stroke services in Greater Manchester & East Cheshire (GM & EC), a large UK regional centralised stroke care system, whilst adjusting for traffic-related air pollution (Nitrogen Dioxide, NO2) and ambient temperature. Our primary objective was to compare measures of emergency department (ED) stroke assessments, stroke service admissions, referrals for transient ischaemic attack (TIA) and stroke discharges in the weeks before, and during the early phase of the pandemic.
Methods
Data source
Local activity data were collected from EDs at each hospital Trust and collated weekly within the Greater Manchester Stroke Operational Delivery Network (GMSODN). Discharge data were extracted from the national Sentinel Stroke National Audit Programme (SSNAP) registry core-dataset, a mandatory resource auditing stroke services against evidence-based standards (https://www.strokeaudit.org/). All confirmed stroke episodes are entered into the core SSNAP dataset internally at each participating hospital site in England, Wales and Northern Ireland.
Setting
GM & EC have operated a centralised hub and spoke stroke care pathway since 2015.5 The pathway model comprises three Hyperacute Stroke Units (HASUs): Salford Royal (regional neurosciences centre), Fairfield General and Stepping Hill serving approximately 3.0 million people. A central component involves the North West Ambulance Service transporting all patients with suspected stroke (FAST positive) within 48 hours of symptom onset (or time last seen well) directly to one of the three HASU EDs. This is based on geographical proximity between 6:45am-10:45pm, 7 days/week for assessment and admission for hyper-acute care (if stroke is confirmed or requires exclusion). Outside of these hours, all stroke pathway patients are transported directly to the HASU at Salford Royal which operates 24 hours/ day, serving the whole region for neurosurgery, thrombectomy, and thrombolysis overnight. The Salford Royal HASU admits approximately 2100 patients with confirmed stroke/year, whilst Fairfield General and Stepping Hill admit approximately 1000 and 1100/year respectively. The three HASUs directly admit approximately 90% of all strokes in GM & EC, with the remainder admitted to a District Stroke Centre (DSC) (e.g. suspected stroke presenting beyond 48h since onset).
Data collection
Weekly data submitted to the GMSODN includes numbers of stroke pathway arrivals, stroke service admissions, TIA referrals received for urgent out-patient clinical assessment and discharge numbers within the SSNAP database. At Salford Royal, patients may occasionally be assessed and confirmed as stroke within ED and discharged as a virtual admission for review. These virtually admitted patients are included in the admission numbers for the Salford Royal HASU. At Fairfield General, numbers admitted to the stroke unit may occasionally exceed numbers assessed as the trust includes three other units (North Manchester, Oldham and Rochdale) and admit from these other sites via telephone assessment, without assessing these within their ED at Fairfield. This process has been consistent since 2015.
Change in air pollution and temperature are important factors when considering stroke activity.12 , 13 Given their association with stroke, the restrictions placed on motorised travel, and the change in season occurring in parallel with the emergence of the pandemic, ambient air temperature and traffic-related air pollution in the form of NO2 was included in our modelling. Hourly temperature and air pollution measurements were obtained and matched for the three HASU sites (Salford Royal = Salford Eccles, Fairfield General = Shaw Crompton Way Oldham, and Stepping Hill = Manchester Sharston (i.e. Manchester Airport), for the corresponding time-period from the Department for Environment Food and Rural Affairs (DEFRA: https://uk-air.defra.gov.uk/). The weekly (lagged previous week) average air pollution level and temperature during active daytime hours (6am to 11pm) were calculated. Missing hourly values were replaced with the average of the remaining monitors if present, before averaging across the day and then week to give average daily value per week. Temperature is recognised to have a U or reverse J shape relationship with health outcomes. Previous work under a similar temperate climate indicated a double linear relationship with a cut-off of 11°C, i.e. two continuous terms one representing weeks with an average temperature range ≤11°C, and one >11°C.14 , 15 Given the limited data in a cooler climate, the cut off was explored and appropriate covariates included to account for confounding by temperature. The Akaike Information Criterion was compared when covariates representing a potential non-linear temperature relationship (double linear splines split at increasing 2°C intervals). These were found to be no better than a single linear relationship.
Statistical analyses
We evaluated key UK COVID-19 events (first UK hospital death from COVID-19, government intervention, and the UK Act-FAST media campaign16) on acute stroke pathway activity defined by the following outcome measures: weekly (Monday to Sunday) counts of stroke assessments in the ED, subsequent stroke service admissions, number of TIA referrals, and number of discharges from inpatient stroke care. An interrupted time-series analysis in the form of a segmented Generalised Linear Regression model was fitted to the weekly Poisson counts. The model was adjusted for site location and available time-dependent confounders such as 6am-11pm weekly average ambient temperature and traffic-related air pollution (lagged previous week) in the form of NO2. The interrupted time-series model includes three variables representing time since start of study (weeks since Jan 2020) that was centred at the first interruption point included in the model, a binary period pre or post interruption, and an interaction variable between weekly trend and binary interruption that represented the change in trend post interruption.17 , 18 Two interruption points were explored: the first announced death from COVID-19 in the UK on Thursday 5th March and thus designated in this analysis of weekly events as the following Monday (9th March); and the Government imposed intervention measures announced on 23rd March.19 , 20 A second interruption point, the Act-FAST media campaign (week beginning 6th April), was included in each model using a three-factor categorical variable to represent the three study periods.13No evidence was found for the presence of autocorrelation (over 5 week lag) in Pearson residuals produced by the baseline models not including the interrupted time-series parameters. However, robust standard errors were applied in order to compensate where possible for potential departures from key assumptions i.e. autocorrelation, over-dispersion, or short-term (day to day) unmeasured time-dependent confounding effects not included in model. Analysis was performed in STATA v15, results are reported as a percentage change in the Incidence Rate Ratio (IRR) along with their 95% Confidence Intervals (C.I.s), where percentage change in IRR is 100*(IRR-1).
Results
During the 18 weeks from 6th January 2020, a total of 2434 ED assessments, 1877 stroke admissions, 996 TIA referrals, and 1327 stroke discharges were reported across the three HASU sites. Table 1 reports the average number (median and IQR) of events occurring per week for the three HASU sites and split by the interrupted study periods. Figure 1 illustrates the change in observed number of events occurring across the study period with the key study time-periods highlighted. The key confounding factors traffic related air pollution (NO2 µgm−3) and ambient temperature (°C) averaged daily (activity 6am-11pm) across the week are described in full in Supplementary Table 1 and Supplementary Figures 1 and 2 In the period post first UK COVID-19 death, NO2 decreased by approximately 10 µgm−3 (down by 45%), and temperature increased by4°C on average across sites. Comparing to the average over the previous five years (2015-19) the weekly average per day was lower overall in the first 5 months of 2020, and indicated a slightly larger seasonal decrease occurred compared to the previous years.
Table 1.
Descriptive statistics for counts within population wide event dates, average across the three HASU combined sites.
| Event | Corresponding Dates | Combined HASU Total |
Combined HASU Total |
||||
|---|---|---|---|---|---|---|---|
| N | Med(IQR) | Min;Max | N | Med(IQR) | Min;Max | ||
| Emergency Assessments | Stroke Admissions | ||||||
| Pre-First death | 6th Jan - 9th Mar | 9 | 150(148;156) | 127,171 | 9 | 114(105;122) | 103,127 |
| First Death - Intervention | 9th Mar - 23rd Mar | 2 | 141(127;155) | 127,155 | 2 | 115(103;127) | 103,127 |
| Intervention to Act-FAST | 23rd Mar - 6th Apr | 2 | 97(84;110) | 84,110 | 2 | 84(75;93) | 75,93 |
| Post Act-FAST | 6th Apr - 11th May | 5 | 113(110;115) | 108,133 | 5 | 94(86;96) | 80,102 |
| Total | 1st Jan - 11th May | 18 | 146(113;154) | 84,171 | 18 | 104(94;116) | 75,127 |
| TIA Referrals | Stroke Unit Discharges | ||||||
| Pre-First death | 6th Jan - 9th Mar | 9 | 68(66;71) | 43,76 | 9 | 77(75;77) | 72,88 |
| First Death - Intervention | 9th Mar - 23rd Mar | 2 | 48.5(43;54) | 43,54 | 2 | 81(77;85) | 77,85 |
| Intervention to Act-FAST | 23rd Mar - 6th Apr | 2 | 26(19;33) | 19,33 | 2 | 79.5(75;84) | 75,84 |
| Post Act-FAST | 6th Apr - 11th May | 5 | 43(43;45) | 40,50 | 5 | 60(55;69) | 42,70 |
| Total | 1st Jan - 11th May | 18 | 60(43;69) | 19,76 | 18 | 75.5(70;77) | 42,88 |
First death = Week post UK COVID-19 death reported on Thursday 5th March, HASU=hyperacute stroke unit, TIA=transient ischaemic attack, Act-FAST = Public Heath England campaign to increase early identification of suspected stroke, N = Number of Weeks.
Fig. 1.
Observed weekly stroke activity counts occurring at the three HASUs.
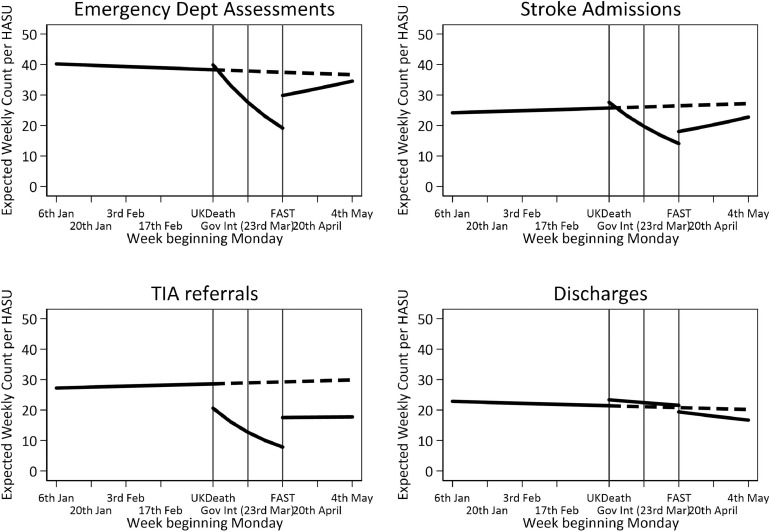
Table 2 and Figs. 2 and 3 , illustrate the results of the interrupted segmented time-series analysis; the full model with direct covariate effect estimates can be found in Supplementary Table 2. Table 2 reports the percentage change in rate (95% C.I.) per week leading up to the first interruption (first UK hospital COVID-19 death or Government Intervention), the difference at both the first interruption time-point and the second interruption (Act-FAST), and the change (i.e. interaction effect) in weekly trend for the period between interruption and Act-FAST, and post Act-FAST. In each case these have been adjusted for environmental confounding factors (traffic-related air pollution and ambient temperature). Table 2 indicates, for example, that prior to the interrupted time point first UK COVID-19 death, the trend in stroke admissions was a -0.5% decrease per week; on the 9th March there was a 4.2% decrease in average admissions, and the interaction effect indicated that compared to pre-first COVID-19 death there was an -16.3% decrease in the weekly trend between first UK COVID-19 death and Act-FAST.
Table 2.
Interrupted segmented time-series, percentage change in Emergency Department assessments, stroke admissions, TIA referrals, and stroke discharges, as associated with segmented periods.
| % Change in Stroke Event Rate (95% C.I.) |
ED Assess | Stroke Admission | TIA referrals | Discharges | |
|---|---|---|---|---|---|
| Characteristic | Period | First Week Post UK Death (9th Mar) | |||
| First Week Post UK Death (9th Mar) to UK Act-FAST (6th Apr ) | |||||
| Trend (per wk trend Pre-First death) | 6th Jan-9th Mar | -0.5(-3.3,2.3) | 0.7(-1.8,3.3) | 0.5(-4.6,6) | -0.7(-2.7,1.2) |
| Post vs Pre First Death | 9th Mar | 4.2(-9.1,19.3) | 7.2(-9.6,27.1) | -28(-51.6,7) | 9.2(-8.4,30.3) |
| Post- Act-Fast v Pre First Death | 6th April | -32.7(-50.8,-8) | -44.6(-63.6,-15.6) | -39.4(-70.5,24.3) | 5.4(-37,76.3) |
| Interaction (per wk trend*Post vs Pre First Death) | 9th Mar-6th Apr | -16.3(-20.3,-12.2) | -16.1(-27.2,-3.2) | -21.8(-40,1.8) | -1.3(-11.5,10) |
| Interaction (per wk trend*Post Act-Fast vs Pre First Death) | 6th Apr-11th May | 4.3(-1.4,10.3) | 5.3(-1.5,12.5) | -0.3(-13,14.4) | -3(-10.1,4.7) |
| Intercept (No. Events)* | 42.4(31,58) | 27(18.5,39.4) | 29.8(14.4,61.8) | 37.1(24.9,55.4) | |
| Government Intervention (23rd Mar) to UK Act-FAST (6th Apr) | |||||
| Trend (per wk trend Pre-Gov Intervention) | 6th Jan-23rd Mar | -0.8(-2.5,1) | 0.6(-1.1,2.3) | -2.4(-6.1,1.4) | 0.1(-1.1,1.3) |
| Post vs Pre Gov Intervention | 23rd Mar | -21.4(-30.4,-11.3) | -19.8(-41,8.8) | -66.7(-75.3,-55.2) | 1.5(-18,25.6) |
| Post-Act Fast vs Pre Gov Intervention | 6th April | -22.1(-37.5,-2.9) | -35.1(-52.3,-11.8) | -17.5(-52.8,44.3) | -6.8(-35.6,34.9) |
| Interaction (per wk trend*Post vs Pre Gov Intervention) | 23rd Mar-6th Apr | -21.7(-31.5,-10.4) | -19(-53.2,40.3) | 85.9(5.3,228.1) | -5.8(-34.1,34.6) |
| Interaction (per wk trend*Post Act-Fast vs Pre Gov Int) | 6th April-11th May | 5.2(0.2,10.5) | 6.1(-0.4,12.9) | 4.8(-8.1,19.5) | -4(-11,3.6) |
| Intercept (No. Events)* | 42(30.7,57.5) | 27.6(19,40.1) | 31.8(14.6,69.1) | 36.9(24.5,55.6) | |
ED = Emergency Department, Act-FAST = Public Heath England campaign to increase early identification of stroke event, TIA-transient ischaemic attack. All models adjusted for site (Stepping Hill, Salford Royal, and Fairfield General), one week lagged Nitrogen Dioxide µgm−3, one week lagged Temp = Temperature °C, (full models can be found in supplementary tables). *Weekly trend was centred at the first intervention time point (i.e. UK COVID-19 death (9th March), or government intervention (23rd March).
Fig. 2.
Trend lines for expected change in events associated with the interrupted segmented periods split at first UK death and UK Act-FAST campaign, dash represents projected pre-UK Death trend.
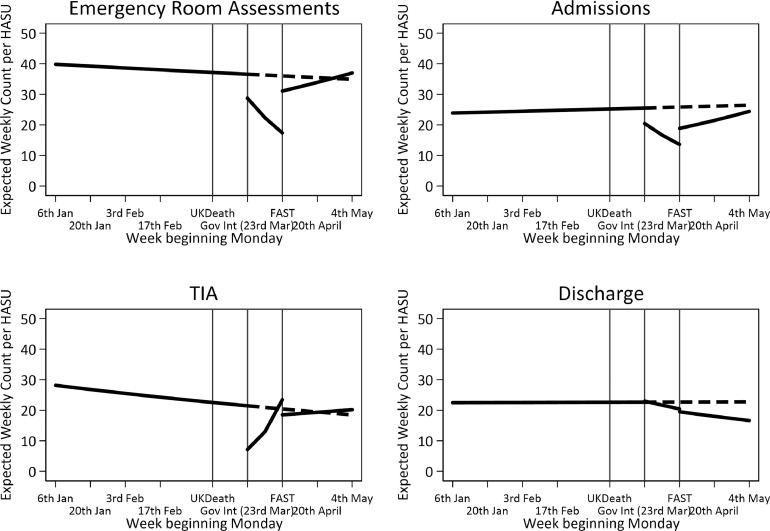
Fig. 3.
Trend lines for expected change in events associated with the interrupted segmented periods split at Government Intervention and UK Act-FAST campaign, dash represents projected Government Intervention trend.
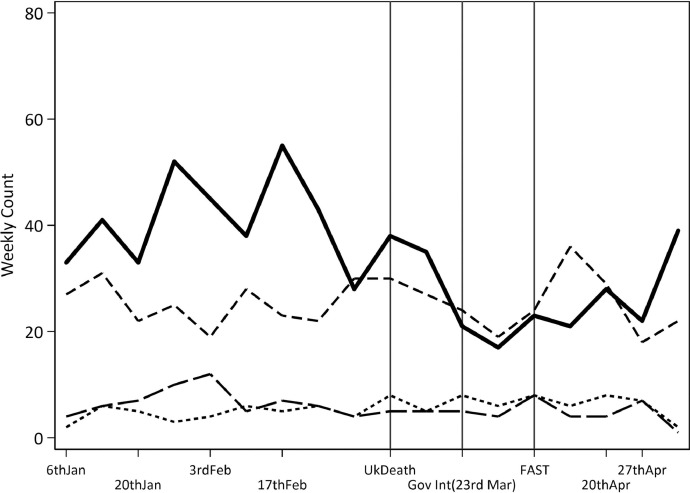
For ED assessments, stroke admissions, and TIA referrals respectively, the per week rate of events presenting were consistent (-0.5%, 0.7%, 0.5% change per week) up until the first reported UK death from COVID-19. The average weekly number of ED assessments and stroke admissions at first week post UK COVID-19 death had a modest increase of 4.2% and 7.2% respectively, however TIA referrals dropped by -28%. The per week trend in all three events presenting between UK COVID-19 death and Act-FAST decreased by -16.7, -15.5, and -21.4%. Post Act-FAST on 6th April the per week trend for ED assessments and stroke admissions indicated a gradual increase in activity per week of 3.7% and 6%, whereas TIA referrals appeared to have no per week trend at 0.2%. Note, when first interruption point was UK Government intervention (23rd March) weekly trends in TIA indicated stronger differences between government intervention and Act-FAST, with an 84% increase in TIA referrals observed per week for the two weeks between government intervention and Act-FAST. However, the number of TIA referrals at week of 23rd March was low (median 8 per site) indicating an 84% increase per week relates to a small increase in events presenting per week. Stroke severity in the form of National Institute of Health Stroke Scale (NIHSS) on entry were available for stroke admissions only. Fig. 4 plots the total count of patients admitted at four severity levels defined as Mild (NIHSS<5), Moderate5, 6, 7, 8, 9, 10, 11, 12, 13, 14, Severe15, 16, 17, 18, 19, 20, and Very Severe (>20).
Fig. 4.
Number Stroke admissions per week split by NIHSS severity level <5 = mild (solid black), 5-14 = moderate (dash), 15-20 = severe (long dash), >20 = very severe (short-dash).
The rate of stroke related discharges across the three sites appeared to be consistent during the study period. A small decrease in rate of discharge post first UK COVID-19 death (≈1%) was followed by slightly larger decrease post Act-FAST (≈3%). Some evidence was observed for a short-term increase in discharges during the week of the first UK COVID-19 death as indicated by 9.2% increase at the interruption point.
Discussion
Whilst accounting for key environmental factors, we investigated aggregated weekly stroke activities occurring in three specialist HASUs serving approximately 3.0 million people across GM & EC during the emergence of the COVID-19 pandemic. The GM & EC conurbation admits approximately 4-4.5% of all confirmed strokes in England, Wales and Northern Ireland (https://www.strokeaudit.org/). Our results suggested that despite the adjustment for environmental factors traffic related air pollution and ambient air temperature, stroke activity was still associated with key population level events during the pandemic. Our results also suggest a reduction in TIA referrals and stroke events presenting to HASUs following the first UK COVID-19 death, with some evidence of a return towards the normal after Act-FAST, although particularly with respect to TIA referrals the stroke activity levels had not returned to previously normal levels as reported in January and February. The rate of ED assessments and subsequent admissions to a HASU indicated a ≈16% decrease per week that was statistically significantly different from the weeks leading up to the first UK COVID-19 death. Post Act-FAST, the per week trend appears to indicate stroke activities were beginning to return towards the levels observed in January and February 2020, but were still being reported at lower levels. The severity level of stroke admissions were considered, and indicated that the number of patients considered to have a mild stroke (NIHSS<5) on admission were lower during the pandemic. In addition to the caution that should be applied when interpreting a segmented analysis with short disjointed time periods, the context should be accounted for when interpreting the rate of TIA referrals. After an initial decrease similar to that observed in ED assessments and stroke admissions, an increase of approximately 85% per week for the two weeks between government intervention (23rd March) and the Act-FAST intervention (6th April) was observed. During this period, the rate of TIA referrals across HASUs was very low, with median (IQR) average across the three HASUs at 84 , 8 which could correspond to an addition of approximately 6 patients per week at each site.
The potential mechanisms underlying our observations remain uncertain and speculative. First, the reduction in strokes and TIAs presenting to hospital could be due to fewer strokes and TIAs occurring at population level, although currently evidence for this is lacking. However, it is also possible that stroke incidence could increase during the pandemic, based on known associations between preceding viral respiratory infections and stroke.21 Secondly, urgent care pathways, including those facilitating rapid-transfer stroke pathways, might be disrupted by conflicting demands on ambulance utilisation and emergency care due to acutely unwell patients with SARS-CoV-2. Likewise, availability of specialist HASU beds and staff might be impacted by redeployment of staff (or sickness) and beds for acute COVID-19 admissions. Finally, societal and individual behaviours are likely to be important, for example a reluctance in the population to seek medical care for fear of increased risk of infection or diverting resources away from what might be perceived as more urgent and pressing need. This may be the case particularly for milder or transient stroke symptoms, where urgency to seek medical attention might be attenuated by the pandemic, and for which the Act-FAST has previously been less effective than for more severe stroke symptoms.22 , 23 Recent studies in China and Spain have reported a reduction in various measures of stroke activity during the pandemic, including reduced stroke admissions, inpatient stroke care capacity and thrombolysis/ thrombectomy.24 , 25 In addition, delays in patients presenting to hospital with stroke symptoms during the pandemic have been reported, resulting in fewer patients arriving within the thrombolysis window.26 Whilst the clinical significance of our findings, and those of these other recent studies, are currently uncertain, they raise concerns that short and longer-term outcomes after stroke and TIA could be compromised by the pandemic.
We selected interventions with strong fixed time points within the series relating to the pandemic. Other factors such as air pollution and traffic have been associated with stroke onset. During the period of study these appear to be reduced and could be associated with the number of strokes presenting to hospital. We have made attempts to account for changes in traffic related air pollution, and ambient temperature during the time period. We were limited to a single pollutant model and given the broader nature of weekly counts, a more sophisticated day to day change and exploration of a multi-pollutant relationships would improve our understanding. Even so, there may be the possibility that further time-varying confounding factors are still present in the characteristics of the population that correlate to the timing of the COVID-19 pandemic, for example, population lifestyle, diet, and exercise habits that are associated with stroke risk.27 , 28 Anecdotal evidence has suggested both positive (e.g. sales of exercise equipment)29 and negative (e.g. sales of alcohol)30 lifestyle changes. It is unlikely that such changes would have such an immediate influence on stroke risk, however it does illustrate that multiple time-dependent factors were present and further work would need to be done to identify and assess their influence.
Limitations
We are confident the data collection included in this study was consistent throughout and all presenting patients were included. The ED activity, admission and TIA data are essential data collection measures that were recorded as standard and were not limited due to additional staff workload. Discharges were collected via local site SSNAP data collection processes, whereas we are aware that teams nationally reduced their in/out into SSNAP, our three HASUs continued to enter all records as standard into the national SSNAP database. However, as with any observational study where bias and confounding might be present, we acknowledge caution when interpreting our findings. Interrupted time-series designs offer a robust quasi-experimental method for evaluating population level intervention effects so long as suitable data are available at multiple time points prior to and after the intervention. Given the time constraints of reacting to health care changes in a global pandemic, we felt we were unable to collect further data. However, we have made some assumptions that are difficult to test and so the results here should be treated with caution. An interrupted time-series is only appropriate when the trends are considered to be linear (or in this case the appropriate log-linear transformation). This may not be the case under larger time frames, however given the relatively short time period investigated here we believe that log-linear trends can be appropriate and any bias extrapolating over the short time period minimal.
As with all observational records-based studies, we were limited to the available data recorded. Data for those patients presenting acutely to one of the GM & EC DSCs (approximately 10% of all stroke admissions) rather than directly to a HASU, were not available. Importantly, there were no substantive changes to the stroke pathway during the time period analysed. However, we could not reliably collect certain variables such as availability of HASU beds or changes to numbers of core stroke team staff, reflecting staff redeployment to COVID-19 areas or sickness. Where possible we have made every attempt to account for time varying factors (such as, local air pollution or temperature levels) and adjust autocorrelation between adjacent admission measures. We were unable to account for seasonal changes in stroke incidence or compare to a similar time-period in previous years. However, though mortality from stroke has been shown to be greater in the winter, incidence of stroke itself has not been shown to link independently from air pollution or temperature with season.31 , 32 Finally, it is unclear how generalizable our findings are when considering wider UK stroke services, as few other regions operate centralised stroke models.
Autocorrelation in the residuals (i.e. lack of independence between observations) were investigated and found to be minimum, hence no further adjustment was made. Despite the multiple sites the sample size (time-points) was relatively small and the power of the study to see a true effect may be limited. However, more data points prior to January 2020 may have incurred additional seasonal changes or historical trends that would not represent accurately the immediate underlying trends. In addition, it has been shown previously that power increases if the numbers of data points are equally distributed before and after the intervention.33 Given our limited time-frame between and post intervention, a larger number of data points prior may have not been beneficial. As the analyses were based on routine data collection, it is worth noting that despite our confidence in the data collection there may be potential for unobserved changes to data collection given the strain on resources, that could have affected our results.34
Conclusion
Despite adjustment for environmental factors, specifically traffic-related air pollution a key confounding factor, a reduction in stroke activity occurring in HASUs across GM & EC appears to be associated with key population level COVID-19 pandemic events. ED assessments for stroke, stroke service admissions, and TIA referrals across HASUs in GM & EC were reduced in the immediate period post first UK-COVID death. Trends have subsequently begun to return, though not fully, towards the levels observed earlier in the same year. Reduction in overall activity appears to be associated with fewer mild strokes presenting. Further work will be required to not only understand the underlying motivations and mechanisms within the population, but also the short and long-term consequences this might have on patient health outcomes and quality of life.
Funding
There was no external funding for this project.
Data sharing statement
Data and the statistical analysis code can be made available upon request. Please send an email to Matthew.Gittins@manchester.ac.uk. The ambient air pollution and temperature data is available online at the UK Air Information Resource provided by the Department for Environment Food and Rural Affairs. https://uk-air.defra.gov.uk/data/
Disclaimer
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Patient consent for publication
Not required.
Ethics approval
Ethical approval was not required as the research presented in this manuscript comprises a secondary analysis of routinely collected anonymised and aggregated clinical data.
Declaration of Competing Interest
All authors have completed the Unified Competing Interest form (available on request from the corresponding author) and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work.
Transparency declaration
The lead author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Acknowledgments
Acknowledgements
We thank the people and organisations participating in the Sentinel Stroke National Audit Programme (SSNAP) and Greater Manchester Stroke Operational Delivery Network (GMSODN).
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jstrokecerebrovasdis.2020.105229.
Appendix. Supplementary materials
References
- 1.Lin Q, Zhao S, Gao D, Lou Y, Yang S, Musa SS. A conceptual model for the coronavirus disease 2019 (COVID-19) outbreak in Wuhan, China with individual reaction and governmental action. Int J Infect Dis. 2020;93:211–216. doi: 10.1016/j.ijid.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Signorelli C, Scognamiglio T, Odone A. COVID-19 in Italy: impact of containment measures and prevalence estimates of infection in the general population. Acta Biomed. 2020;91(3-S):175–179. doi: 10.23750/abm.v91i3-S.9511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stroke Association. Stroke Statistics: State of the Nation stroke.org.uk2018 [Available from: https://www.stroke.org.uk/sites/default/files/state_of_the_nation_2018.pdf.
- 4.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. 2019;50(12):e344–e418. doi: 10.1161/STR.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 5.RCP. The Intercollegiate Stroke working party: National Clinical guideline for stroke 5th Edition. 2016.
- 6.Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid-19 on stroke evaluation in the United States. N Engl J Med. 2020 doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fischer MA. World Stroke Organisation: The Global Impact of COVID-19 on Stroke - Survey Report 2020 [Available from: https://www.world-stroke.org/news-and-blog/news/the-global-impact-of-covid-19-on-stroke-survey.
- 8.Spinney L. The Guardian; 2020. Concern as heart attack and stroke patients delay seeking help. [Google Scholar]
- 9.McNamara D. COVID-19: are acute stroke patients avoiding emergency care?2020 [Available from: https://www.mdedge.com/neurology/article/220491/stroke/covid-19-are-acute-stroke-patients-avoiding-emergency-care.
- 10.Holmes JL, Brake S, Docherty M, Lilford R, Watson S. Emergency ambulance services for heart attack and stroke during UK's COVID-19 lockdown. Lancet. 2020;395(10237):e93–ee4. doi: 10.1016/S0140-6736(20)31031-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NASA. Airborne Nitrogen Dioxide Plummets Over China: NASA; 2020 [Available from: https://earthobservatory.nasa.gov/images/146362/airborne-nitrogen-dioxide-plummets-over-china.
- 12.Shah AS, Lee KK, McAllister DA, Hunter A, Nair H, Whiteley W. Short term exposure to air pollution and stroke: systematic review and meta-analysis. BMJ. 2015;350:h1295. doi: 10.1136/bmj.h1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lian H, Ruan Y, Liang R, Liu X, Fan Z. Short-term effect of ambient temperature and the risk of stroke: a systematic review and meta-analysis. Int J Environ Res Public Health. 2015;12(8):9068–9088. doi: 10.3390/ijerph120809068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carder M, McNamee R, Beverland I, Elton R, Cohen GR, Boyd J. The lagged effect of cold temperature and wind chill on cardiorespiratory mortality in Scotland. Occup Environ Med. 2005;62(10):702–710. doi: 10.1136/oem.2004.016394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gittins M, McNamee R, Carder M, Beverland I, Agius RM. Has the short-term effect of black smoke exposure on pneumonia mortality been underestimated because hospitalisation is ignored: findings from a case-crossover study. Environ Health. 2013;12:97. doi: 10.1186/1476-069X-12-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roberts M. BBC: 'Dial 999 for stroke emergencies despite coronavirus' BBC2020 [Available from: https://www.bbc.co.uk/news/health-52173471.
- 17.Kontopantelis E, Doran T, Springate DA, Buchan I, Reeves D. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ. 2015;350:h2750. doi: 10.1136/bmj.h2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O'Keeffe AG, Geneletti S, Baio G, Sharples LD, Nazareth I, Petersen I. Regression discontinuity designs: an approach to the evaluation of treatment efficacy in primary care using observational data. BMJ. 2014;349:g5293. doi: 10.1136/bmj.g5293. [DOI] [PubMed] [Google Scholar]
- 19.Dept of Health and Social Care. CMO for England announces first death of patient with COVID-19 2020 [Available from: https://www.gov.uk/government/news/cmo-for-england-announces-first-death-of-patient-with-covid-19.
- 20.UK Government. PM address to the nation on coronavirus: 23 March 20202020 [Available from: https://www.gov.uk/government/speeches/pm-address-to-the-nation-on-coronavirus-23-march-2020.
- 21.Boehme AK, Luna J, Kulick ER, Kamel H, Elkind MSV. Influenza-like illness as a trigger for ischemic stroke. Ann Clin Transl Neurol. 2018;5(4):456–463. doi: 10.1002/acn3.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wolters FJ, Li L, Gutnikov SA, Mehta Z, Rothwell PM. Medical attention seeking after transient ischemic attack and minor stroke before and after the UK face, arm, speech, time (fast) public education campaign: results from the oxford vascular study. JAMA Neurol. 2018;75(10):1225–1233. doi: 10.1001/jamaneurol.2018.1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wise J. FAST education campaign did not improve response to minor strokes. BMJ. 2018;362:k2898. [Google Scholar]
- 24.Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 Epidemic on Stroke Care and Potential Solutions. Stroke. 2020 doi: 10.1161/STROKEAHA.120.030225. STROKEAHA120030225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rudilosso S, Laredo C, Vera V, Vargas M, Renu A, Llull L. Acute Stroke Care Is at Risk in the Era of COVID-19: Experience at a Comprehensive Stroke Center in Barcelona. Stroke. 2020 doi: 10.1161/STROKEAHA.120.030329. STROKEAHA120030329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Teo KC, Leung WCY, Wong YK, Liu RKC, Chan AHY, Choi OMY. Delays in Stroke Onset to Hospital Arrival Time During COVID-19. Stroke. 2020 doi: 10.1161/STROKEAHA.120.030105. STROKEAHA120030105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tikk K, Sookthai D, Monni S, Gross ML, Lichy C, Kloss M. Primary preventive potential for stroke by avoidance of major lifestyle risk factors: the European Prospective Investigation into Cancer and Nutrition-Heidelberg cohort. Stroke. 2014;45(7):2041–2046. doi: 10.1161/STROKEAHA.114.005025. [DOI] [PubMed] [Google Scholar]
- 28.Stroke Association. Are you at risk of stroke?2020 [Available from: https://www.stroke.org.uk/what-is-stroke/are-you-at-risk-of-stroke.
- 29.Harrabin R. BBC Coronavirus: Boom time for bikes as virus changes lifestyles BBC: BBC; 2020 [Available from:https://www.bbc.co.uk/news/business-52564351.
- 30.Finlay IG, I. Covid-19 and alcohol—a dangerous cocktail BMJ2020 [Available from:https://www.bmj.com/content/369/bmj.m1987. [DOI] [PubMed]
- 31.Gomes J, Damasceno A, Carrilho C, Lobo V, Lopes H, Madede T. The effect of season and temperature variation on hospital admissions for incident stroke events in Maputo, Mozambique. J Stroke Cerebrovasc Dis. 2014;23(2):271–277. doi: 10.1016/j.jstrokecerebrovasdis.2013.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rothwell PM, Wroe SJ, Slattery J, Warlow CP. Is stroke incidence related to season or temperature? The Oxfordshire Community Stroke Project. Lancet. 1996;347(9006):934–936. doi: 10.1016/s0140-6736(96)91415-4. [DOI] [PubMed] [Google Scholar]
- 33.Liu W, Ye S, Barton BA, Fischer MA, Lawrence C, Rahn EJ. Simulation-based power and sample size calculation for designing interrupted time series analyses of count outcomes in evaluation of health policy interventions. Contemp Clin Trials Commun. 2020;17 doi: 10.1016/j.conctc.2019.100474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.