Abstract
The SARS-CoV-2 is a novel coronavirus identified as the cause of COVID-19 and, as the pandemic evolves, many have made parallels to previous epidemics such as SARS-CoV (the cause of an outbreak of severe acute respiratory syndrome [SARS]) in 2003. Many have speculated that, like SARS, the activity of SARS-CoV-2 will subside when the climate becomes warmer. We sought to determine the relationship between ambient temperature and COVID-19 incidence in Canada. We analyzed over 77,700 COVID-19 cases from four Canadian provinces (Alberta, British Columbia, Ontario, and Quebec) from January to May 2020. After adjusting for precipitation, wind gust speed, and province in multiple linear regression models, we found a positive, but not statistically significant, association between cumulative incidence and ambient temperature (14.2 per 100,000 people; 95%CI: −0.60–29.0). We also did not find a statistically significant association between total cases or effective reproductive number of COVID-19 and ambient temperature. Our findings do not support the hypothesis that higher temperatures will reduce transmission of COVID-19 and warns the public not to lose vigilance and to continue practicing safety measures such as hand washing, social distancing, and use of facial masks despite the warming climates.
Keywords: SARS-CoV-2, COVID-19, Temperature, Reproductive number, Canada
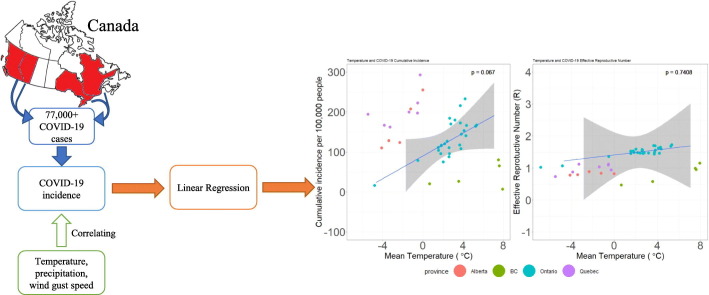
Graphical abstract
1. Background
The novel coronavirus disease (COVID-19) is caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) (World Health Organization, 2020a). Coronaviruses are enveloped RNA viruses that cause respiratory illnesses of varying severity from the common cold to fatal pneumonia. The COVID-19 outbreak was declared a Public Health Emergency of International Concern by the World Health Organization (WHO) on 30 January 2020. Over a month later, with a 13-fold increase in the number of cases outside China and 3-fold increase in the number of countries with reported cases, the WHO declared the COVID-19 outbreak a global pandemic on March 11, 2020. Countries across the world began to launch various aggressive, but common, actions to contain the virus (e.g. national lockdown, closure of school and non-essential services, social/physical distancing, hand sanitizing, use of face mask coverings, self-isolation, etc.). While these actions have had strong disease control and some environmental benefits, it is coupled with rapidly increasing unemployment rates (Juni et al., 2020; Collivignarelli et al., 2020; Zambrano-Monserrate et al., 2020). As a result, the world population faces a significant health and economic burden from COVID-19. As of June 15, 2020, over 7.9 million individuals have been infected with COVID-19 and over 443,000 have died of it globally (Dong et al., 2020).
As the COVID-19 pandemic evolves globally over several seasons, the role of the climate and environment are important factors to consider in transmission. For example, previous studies in California and Italy have shown that air pollutants are associated with increased COVID-19 incidence (Bashir et al., 2020a; Fattorini and Regoli, 2020). In terms of temperature, many have drawn parallels between the COVID-19 pandemic with previous epidemics such as SARS-CoV (the cause of an outbreak of severe acute respiratory syndrome [SARS]) in 2003. Many speculated that, like SARS, the activity of SARS-CoV-2 would subside when the climate becomes warmer. This speculation is drawn from the inverse relationship between warm temperatures and viral infections, including influenza and other coronaviruses like MERS-CoV (Fagbo et al., 2017; Lowen et al., 2007). Likeness of viral activity between SARS-CoV-2 and SARS-CoV is especially emphasized given their similarities in genetics (~79%) (Lu et al., 2020) and their hypothesized primary reservoir of bats (Wang et al., 2006; Lai et al., 2020). However, the widespread cases in warmer climate countries such as India, Iran, and Brazil have contradicted the aforementioned speculation. Nevertheless, this speculation was so widespread that the WHO issued a statement on its web page of COVID-19 myth busters to caution the public that “Exposing yourself to the sun or to temperatures higher than 25 °C degrees DOES NOT prevent the coronavirus disease (COVID-19)” (World Health Organization, 2020b).
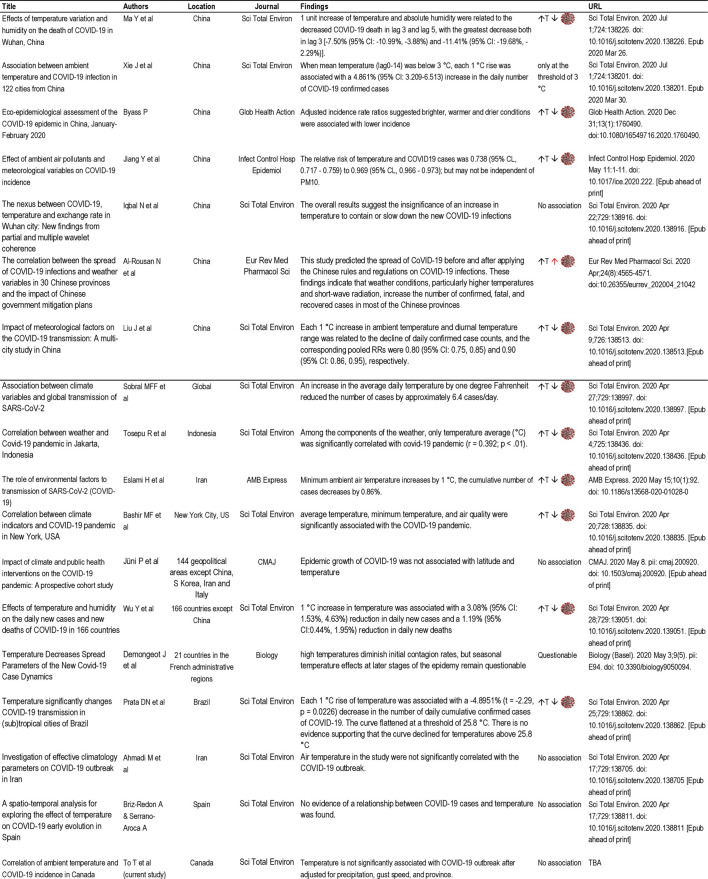
Given its novelty, there is a limited but rapidly growing body of literature on SARS-CoV-2 and meteorological conditions. To date, there have been a limited number of peer-reviewed publications with a major focus on studying the effect of ambient temperature on the transmission of COVID-19. Table 1 provides a literature review of the findings of these studies. Seven of these studies used data from China and the rest were from various parts of the world. All but one of the studies with data from China showed a negative correlation between temperature and COVID-19 incidence (i.e. every unit increase in temperature was associated with decreasing COVID-19 cases). Similarly, among the 10 studies that excluded China, six reported negative correlations, three showed no significant association, and another suggested a questionable association. The mixed and contrasting evidence among observational studies still warrant the need for further investigation. Thus, in the face of inconsistent findings in the literature and an increased urgency to understand this new disease, this study aims to examine the association between temperature and COVID-19 incidence in Canada.
Table 1.
Literature review of 17 peer-reviewed papers on temperature and COVID-19 (Juni et al., 2020; Demongeot et al., 2020; Ahmadi et al., 2020; Briz-Redon and Serrano-Aroca, 2020; Ma et al., 2020; Xie and Zhu, 2020; Byass, 2020; Jiang et al., 2020; Iqbal et al., 2020; Al-Rousan and Al-Najjar, 2020; Liu et al., 2020; Sobral et al., 2020; Tosepu et al., 2020; Eslami and Jalili, 2020; Bashir et al., 2020b; Wu et al., 2020; Prata et al., 2020).
2. Methods
2.1. Data sources
Our study used Canadian data to study the potential correlation between ambient temperature and the incidence of COVID-19. Four Canadian provinces (Alberta, British Columbia, Ontario, and Quebec) were included in this study, where the cumulative number of COVID-19 cases was above 77,700. Individual-level epidemiologic data of positive COVID-19 cases from January to May 2020 were obtained from open access datasets. Ontario case data were obtained from a dataset compiled by the Ontario Ministry of Health and Long-Term Care based on information reported by local public health agencies (Ontario Ministry of Health, 2020). Case data for the other three provinces were obtained from a dataset with individual-level data which were collected and updated from publicly available sources including government reports, government websites, and news media by the COVID-19 Canada Open Data Working Group, a team at the University of Toronto (Berry et al., 2020).
2.2. Statistical analysis
We aggregated the COVID-19 incidence data by report date and Canadian health regions. Canadian health regions are administrative geographical units defined by provincial health ministries to facilitate the delivery of health care to communities within the regions. Daily data on mean, minimum, and maximum ambient temperature (°C), total precipitation (mm), and maximum wind gust speed (km/h) were obtained from January to May 2020 from Environment and Climate Change Canada (Environment Canada, 2019); they were averaged across Canadian health regions. Time-varying effective reproductive number (Rt) was calculated from daily case data (Thompson et al., 2019). Cumulative incidence rate per 100,000 was calculated from the total case count divided by the regional population count in 2016 from Statistics Canada (Statistics Canada, 2019). Regions with less than 50 COVID-19 incident cases were excluded from the study.
All province data provided a report date for each case. To estimate the climate around time of infection, climate data was averaged 2 weeks prior to the report date. Linear regression models were used to generate point estimates and 95% confidence intervals (CIs) for associations between temperature and the Rt, total cumulative incident cases, and cumulative incidence rate. Models were made using the latest data available, up to 18 May 2020. Covariates for models were selected a priori. All models were adjusted for wind gust speed, precipitation, and province. Regression models were adjusted for the province where the health region was located to control for different social distancing and public health policies that may have been in place. Statistical significance was defined where p-values were < 0.05. All analyses were performed in R software (version 4.0.0) with the rms (v6.0.0) and tidyverse (v1.3.0) packages (R Foundation, 2020; Harrell Jr, 2020; Wickham et al., 2019).
3. Results
We observed 49 health regions across four Canadian provinces that collectively made up 99.6% (77,773) of Canada's COVID-19 cases from January 25 to May 18, 2020. The mean ± standard deviation and range (min-max) for temperature was (1.48 ± 3.46, −6.83-7.94), wind gust speed was (43.5 ± 2.45, 29.9–49.5), and precipitation was (2.03 ± 0.78, 0.44–3.72). Mean temperature and total precipitation tended to decrease at higher latitudes. The mean ± standard deviation and range for Rt and cumulative incidence were (1.27 ± 1.25, 0.27–8.85) and (133.7 ± 100.4, 15.8–415.7), respectively. Total cumulative cases and cumulative incidence rates tended to be highest in and around urban centres.
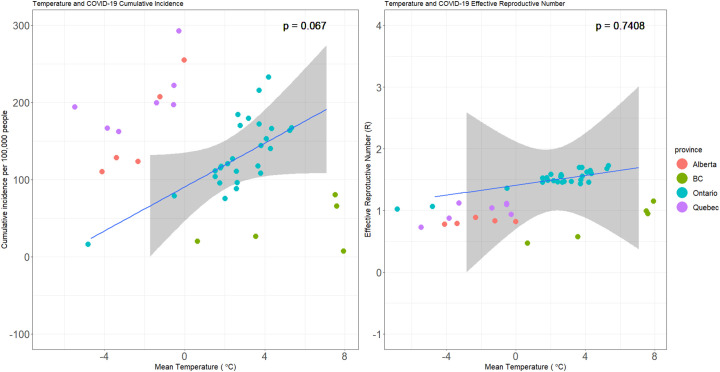
After adjusting for wind gust speed, precipitation, and province, our results did not find a statistically significant association between temperature and Rt (p=0.74) (see Table 2 ). The multiple regression model, adjusted for wind gust speed, precipitation, and province, showed that per unit increase in temperature, there was an associated increase in COVID-19 incidence cases of 14.3 per 100,000 people (95%CI: −0.20–29.0; p=0.07), as shown in Table 2 and Fig. 1 . However, this association was statistically nonsignificant. The association between temperature and cumulative incidence rate was further analyzed by province while adjusting for wind gust speed and precipitation. None of the province-specific regression coefficients for temperature reached statistical significance.
Table 2.
Point estimates, 95% confidence intervals, and p-values of associations for linear regression models. Effective reproductive number and cumulative incidence rate hold no significant associations with mean temperature. Models were adjusted for precipitation, gust speed, and province.
| Estimate | 95% LCI | 95% UCI | p-value | ||
|---|---|---|---|---|---|
| Effective R | Temperature | 0.04 | −0.20 | 0.28 | 0.74 |
| Precipitation | 0.15 | −0.80 | 1.10 | 0.75 | |
| Wind Gust Speed | −0.016 | −0.19 | 0.16 | 0.86 | |
| Province | |||||
| Alberta | Ref | Ref | Ref | Ref | |
| British Columbia | −0.57 | −2.67 | 1.54 | 0.60 | |
| Ontario | 0.26 | −1.37 | 1.89 | 0.75 | |
| Quebec | −0.14 | −2.48 | 2.19 | 0.90 | |
| Cumulative Incidence (per 100,000) | Temperature | 14.2 | −0.6 | 29.0 | 0.067 |
| Precipitation | −27.1 | −86.9 | 32.6 | 0.38 | |
| Wind Gust Speed | 12.6 | 1.40 | 23.8 | 0.034 | |
| Province | |||||
| Alberta | Ref | Ref | Ref | Ref | |
| British Columbia | −182.2 | −314.4 | −50.0 | 0.01 | |
| Ontario | −60.9 | −163.2 | 41.4 | 0.25 | |
| Quebec | 102.1 | −44.4 | 248.6 | 0.18 | |
Fig. 1.
Temperature, COVID-19 Cumulative Incidence, and Effective R. Cumulative incidence rate (left) and effective reproductive number (right) hold no significant association with mean temperature. Models are adjusted for precipitation, gust speed, and province. Solid lines and grey areas refer to the linear trend and 95% confidence interval, respectively, of the correlation between cumulative incidence rate or effective reproductive number and mean temperature.
4. Discussion
This study is the first Canadian study that used daily meteorological data from four major provinces to investigate the association between ambient temperature and COVID-19 from January to May 2020. Our study found no statistically significant associations between Rt, total cumulative cases, or cumulative incidence rates and ambient temperature using multiple regression analyses.
To date, several COVID-19 studies have suggested an inverse relationship between temperature and COVID-19 case incidence. However, our study results are in keeping with those reported by a few recent studies. A study in Wuhan, China and a Canadian study of 144 geopolitical areas found no association (Juni et al., 2020; Yao et al., 2020). Similarly, in a study of 21 countries and French administrative regions, Demongeot et al. found an inverse association at high temperatures but questioned the association at lower, seasonal temperatures (Demongeot et al., 2020). At the time of this study, it is likely that Canada experienced these lower seasonal temperatures rather than high temperatures sufficiently needed to affect COVID-19, as seen in Demongeot et al.'s study. Moreover, neither the study in Iran that looked at various climate variables nor the spatio-temporal analysis of Spain during its early wave of COVID-19 found an association between temperature and COVID-19 (Ahmadi et al., 2020; Briz-Redon and Serrano-Aroca, 2020). A pre-print study in Nigeria did not find an association either (Taiwo and Adebayo, 2020). While our study reported a statistically nonsignificant association between temperature and COVID-19 cases, its positive regression coefficient indicated that COVID-19 incidence increased as temperature increased. However, our findings should be interpreted with caution. During our study period, spikes in COVID-19 incidence were noted in April and May, when outbreaks occurred in meat processing plants in Alberta and a number of long-term care homes in Ontario and Quebec (Public Health Agency of Canada, 2020). These outbreaks might have skewed the association away from the null independent of increasing temperatures in these provinces.
By comparing results between provinces, this study takes advantage of the strongly heterogeneous climate that occurs across Canada. Compared to other countries with large outbreaks, Canada had a greater variation in temperature across the country that allowed for a more robust study and a better identification of the association between temperature and COVID-19 incidence in the findings. Additionally, by using a health region level of analysis, this study was able to accurately represent area-wide climate patterns. Despite this advantage, using health regions as a geographical unit was also a study limitation as the regions could not be further disaggregated at a more granular level like cities. As such, the ecological nature of this study may be confounded by other factors like local public health policies, testing rates, and urbanization. Furthermore, this study could not encompass the summer season and largely occurred in the winter and spring seasons. It is possible that this study did not reach a threshold in which the effects of temperature on viral activity would be more pronounced.
This is an unprecedented situation whereby a new disease is evolving in front of us. Unlike a controlled clinical trial, we are in a natural experiment, observing what is being unfolded as opposed to applying controlled parameters. As we learn how the disease is being transmitted, how it manifests in different patient groups, and how the environment may or may not influence its activity, we must be cautious in making causal inference. Globally, many clinical interventions are being implemented over time, such as new treatment options, novel tests, case finding, contact tracing, together with community-based strategies, that collectively impact the curbing of COVID-19 transmission independent of the climate. The attribution of the observed difference in the pandemic outcome (decrease in cases and deaths) to changing climates may be subject to a potential ecological fallacy because the climate is changing regardless of the pandemic, and the pandemic is slowing down with implementations of collective actions. Nonetheless, it is important to monitor how changes in the environment may contribute to improving or impairing immunity, which may put the population at risk for infection.
In summary, our study did not find any evidence to support the hypothesis that higher temperatures will reduce transmission of COVID-19. While this knowledge may not help curtail the current pandemic, it warns the public not to lose vigilance and to continue practicing safety measures such as hand washing, social distancing, and use of facial masks despite the warming of climates. Our findings may also shed light in preparing for future potential resurgences of COVID-19. Future studies, which will be able to encompass more climate and case data as cases substantially increase globally into the summer months, should continue to look at meteorological factors to further elucidate the relationship between COVID-19 and the climate.
CRediT authorship contribution statement
Teresa To: Conceptualization, Supervision, Writing - original draft. Kimball Zhang: Formal analysis, Writing - original draft, Visualization, Project administration. Bryan Maguire: Formal analysis, Methodology, Writing - review & editing. Emilie Terebessy: Project administration, Data curation, Writing - review & editing. Ivy Fong: Data curation, Writing - review & editing. Supriya Parikh: Data curation, Writing - review & editing. Jingqin Zhu: Writing - review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
This study used data compiled and provided by the Ontario Ministry of Health, COVID-19 Canada Open Data Working Group, Environment and Climate Change Canada, and Statistics Canada. The results, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the data sources.
Editor: Jay Gan
References
- Ahmadi M., Sharifi A., Dorosti S., Jafarzadeh Ghoushchi S., Ghanbari N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Rousan N., Al-Najjar H. The correlation between the spread of COVID-19 infections and weather variables in 30 Chinese provinces and the impact of Chinese government mitigation plans. Eur. Rev. Med. Pharmacol. Sci. 2020;24(8):4565–4571. doi: 10.26355/eurrev_202004_21042. [DOI] [PubMed] [Google Scholar]
- Bashir M.F., Ma B.J., Bilal, et al. Correlation between environmental pollution indicators and COVID-19 pandemic: a brief study in Californian context. Environ. Res. 2020;187 doi: 10.1016/j.envres.2020.109652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Ma B., Bilal, et al. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry I., Soucy J.-P.R., Tuite A., Fisman D. Open access epidemiologic data and an interactive dashboard to monitor the COVID-19 outbreak in Canada. Can. Med. Assoc. J. 2020;192(15):E420. doi: 10.1503/cmaj.75262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briz-Redon A., Serrano-Aroca A. A spatio-temporal analysis for exploring the effect of temperature on COVID-19 early evolution in Spain. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byass P. Eco-epidemiological assessment of the COVID-19 epidemic in China, January-February 2020. Glob. Health Action. 2020;13(1) doi: 10.1080/16549716.2020.1760490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collivignarelli M.C., Abba A., Bertanza G., Pedrazzani R., Ricciardi P., Carnevale Miino M. Lockdown for CoViD-2019 in Milan: what are the effects on air quality? Sci. Total Environ. 2020;732 doi: 10.1016/j.scitotenv.2020.139280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demongeot J., Flet-Berliac Y., Seligmann H. Temperature decreases spread parameters of the new Covid-19 case dynamics. Biology (Basel) 2020;9(5) doi: 10.3390/biology9050094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Environment Canada Historical data. 2019. https://climate.weather.gc.ca/historical_data/search_historic_data_e.html
- Eslami H., Jalili M. The role of environmental factors to transmission of SARS-CoV-2 (COVID-19) AMB Express. 2020;10(1):92. doi: 10.1186/s13568-020-01028-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagbo S.F., Garbati M.A., Hasan R., et al. Acute viral respiratory infections among children in MERS-endemic Riyadh, Saudi Arabia, 2012–2013. J. Med. Virol. 2017;89(2):195–201. doi: 10.1002/jmv.24632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fattorini D., Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ. Pollut. 2020;264 doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell F.E., Jr. R package version 6.0-0; 2020. rms: Regression Modeling Strategies.https://CRAN.R-project.org/package=rms [Google Scholar]
- Iqbal N., Fareed Z., Shahzad F., He X., Shahzad U., Lina M. The nexus between COVID-19, temperature and exchange rate in Wuhan city: new findings from partial and multiple wavelet coherence. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Y., Wu X.J., Guan Y.J. Effect of ambient air pollutants and meteorological variables on COVID-19 incidence. Infect. Control Hosp. Epidemiol. 2020:1–11. doi: 10.1017/ice.2020.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juni P., Rothenbuhler M., Bobos P., et al. Impact of climate and public health interventions on the COVID-19 pandemic: a prospective cohort study. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne. 2020;192(21):E566–E573. doi: 10.1503/cmaj.200920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Ag. 2020;55(3) doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Zhou J., Yao J., et al. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowen A.C., Mubareka S., Steel J., Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog. 2007;3(10):1470–1476. doi: 10.1371/journal.ppat.0030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu R.J., Zhao X., Li J., et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y., Zhao Y., Liu J., et al. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ontario Ministry of Health Confirmed positive cases of COVID-19 in Ontario. 2020. https://data.ontario.ca/dataset/confirmed-positive-cases-of-covid-19-in-ontario
- Prata D.N., Rodrigues W., Bermejo P.H. Temperature significantly changes COVID-19 transmission in (sub)tropical cities of Brazil. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health Agency of Canada . Canada PHAo; 2020. Update on COVID-19 in Canada: Epidemiology and Modelling. ed. [Google Scholar]
- R Foundation The R project for statistical computing. 2020. https://www.r-project.org/
- Sobral M.F.F., Duarte G.B., da Penha Sobral A.I.G., Marinho M.L.M., de Souza Melo A. Association between climate variables and global transmission oF SARS-CoV-2. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada . 2019. Census Profile, 2016 Census. In: 98-316-X2016001, ed. [Google Scholar]
- Taiwo I.F., Adebayo . 2020. COVID-19 Spread and Average Temperature Distribution in Nigeria. [Google Scholar]
- Thompson R.N., Stockwin J.E., van Gaalen R.D., et al. Improved inference of time-varying reproduction numbers during infectious disease outbreaks. Epidemics. 2019;29 doi: 10.1016/j.epidem.2019.100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosepu R., Gunawan J., Effendy D.S., et al. Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia. Sci. Total Environ. 2020;725 doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L.F., Shi Z.L., Zhang S.Y., Field H., Daszak P., Eaton B.T. Review of bats and SARS. Emerg. Infect. Dis. 2006;12(12):1834–1840. doi: 10.3201/eid1212.060401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickham H., Averick M., Bryan J., et al. Welcome to the Tidyverse. Journal of Open Source Software. 2019;4(43):1686. [Google Scholar]
- World Health Organization WHO Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020
- World Health Organization Coronavirus disease (COVID-19) advice for the public: myth busters. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters
- Wu Y., Jing W., Liu J., et al. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.139051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y., Pan J., Liu Z., et al. No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur. Respir. J. 2020;55:2000517. doi: 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambrano-Monserrate M.A., Ruano M.A., Sanchez-Alcalde L. Indirect effects of COVID-19 on the environment. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138813. [DOI] [PMC free article] [PubMed] [Google Scholar]