Abstract
BACKGROUND
Masked uncontrolled hypertension (MUCH), that is, nonhypertensive clinic but high out-of-office blood pressure (BP) in treated patients is at increased cardiovascular risk than controlled hypertension (CH), that is, nonhypertensive clinic and out-of-office BP. Using ambulatory BP, MUCH can be defined as daytime and/or nighttime and/or 24-hour BP above thresholds. It is unclear whether different definitions of MUCH have similar prognostic information. This study assessed the prognostic value of MUCH defined by different ambulatory BP criteria.
METHODS
Cardiovascular events were evaluated in 738 treated hypertensive patients with nonhypertensive clinic BP. Among them, participants were classified as having CH or daytime MUCH (BP ≥135/85 mm Hg) regardless of nighttime BP (group 1), nighttime MUCH (BP ≥120/70 mm Hg) regardless of daytime BP (group 2), 24-hour MUCH (BP ≥130/80 mm Hg) regardless of daytime or nighttime BP (group 3), daytime MUCH only (group 4), nighttime MUCH only (group 5), and daytime + nighttime MUCH (group 6).
RESULTS
We detected 215 (29%), 357 (48.5%), 275 (37%), 42 (5.5%),184 (25%) and 173 (23.5%) patients with MUCH from group 1 to 6, respectively. During the follow-up (10 ± 5 years), 148 events occurred in patients with CH and MUCH. After adjustment for covariates, compared with patients with CH, the adjusted hazard ratio (95% confidence interval) for cardiovascular events was 2.01 (1.45–2.79), 1.53 (1.09–2.15), 1.69 (1.22–2.34), 1.52 (0.80–2.91), 1.15 (0.74–1.80), and 2.29 (1.53–3.42) from group 1 to 6, respectively.
CONCLUSIONS
The prognostic impact of MUCH defined according to various ambulatory BP definitions may be different.
Keywords: blood pressure, classification, hypertension, masked hypertension, risk
Masked hypertension and masked uncontrolled hypertension (MUCH), that is, nonhypertensive clinic but high out-of-office blood pressure (BP) in untreated subjects and treated patients, respectively, have been extensively studied in the last years.1–27 Various single studies and meta-analyses have globally shown that both masked hypertension and MUCH are at increased cardiovascular risk when compared with normotension and controlled hypertension (CH), respectively.1–19,21–27
These phenomena can be detected by using either home BP recording3–7,21–27 or ambulatory BP monitoring.1,2,8–27 To define masked hypertension and MUCH by ambulatory BP monitoring, previous studies have applied thresholds of ≥135/85 mm Hg for daytime and/or ≥120/70 mm Hg for nighttime and/or ≥130/80 mm Hg for 24-hour BP.1,2,9–12,14–27
Recently, in the International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes (IDACO) study, including more than 8,000 untreated subjects from 12 populations, it has been reported that masked hypertension defined by either daytime or nighttime or 24-hour BP above thresholds was associated with similarly increased risk when compared with normotension.2 At present, it is not yet completely clear whether MUCH defined according to different definitions is associated with a similar prognostic information. Indeed, to the best of our knowledge, there is a single-center study in the literature, including a Black population, that evaluated the prognostic impact of different definitions of MUCH.18
The aim of this study was to evaluate the prognostic value of MUCH defined by different ambulatory BP criteria in a Caucasian population.
METHODS
Patients
We studied 738 treated hypertensive patients with nonhypertensive clinic BP selected from 2,264 sequential treated individuals aged 30–90 years who were prospectively recruited from December 1992 to December 2012. All these patients had been referred to our hospital outpatient clinic for evaluation of BP control. One hundred and three patients were lost during follow-up. Subjects with secondary hypertension were excluded. All the subjects underwent clinical evaluation, electrocardiogram, routine laboratory tests, echocardiographic examination, and noninvasive ambulatory BP monitoring. Study population came from the same geographical area (Chieti and Pescara, Abruzzo, Italy). The study was in accordance with the Second Declaration of Helsinki and was approved by the institutional review committee. Subjects gave informed consent.
BP measurement
Clinic BP was recorded by a physician using a mercury sphygmomanometer and appropriate-sized cuffs. Measurements were performed in triplicate, 2 minutes apart, at least after 5 minutes of rest and the mean value was used as the BP for the visit. Clinic systolic and diastolic BP were defined as nonhypertensive when <140/90 mm Hg. Ambulatory BP monitoring was performed with a noninvasive recorder (SpaceLabs 90207, Redmond, WA) on a typical day, within 1 week from clinic visit. Technical aspects have been previously reported.28 We evaluated the following ambulatory BP parameters: daytime (awake period as reported in the diary), nighttime (asleep period as reported in the diary), and 24-hour systolic and diastolic BP. MUCH was defined as clinic BP <140/90 mm Hg and 6 ambulatory BP definitions: (i) daytime MUCH (BP ≥135 and/or ≥85 mm Hg) regardless of nighttime BP, (ii) nighttime MUCH (BP ≥120 and/or ≥70 mm Hg) regardless of daytime BP, (iii) 24-hour MUCH (BP ≥130 and/or ≥80 mm Hg) regardless of daytime or nighttime BP, (iv) daytime MUCH only (high daytime and nonhypertensive nighttime BP), (v) nighttime MUCH only (high nighttime and nonhypertensive daytime BP), and (vi) daytime + nighttime MUCH (high daytime + high nighttime BP). Supplementary Table S1 online shows ambulatory BP characteristics to define different MUCH groups. Some patients classified according to definitions 1–3 can be present in 2 or more of these groups. All the subjects had recordings of good quality (at least 70% of valid readings during the 24-hour period, at least 20 valid readings while awake with at least 2 valid readings per hour and at least 7 valid readings while asleep with at least 1 valid reading per hour), in line with the European Society of Hypertension requirements.29
Echocardiography
Left atrial and left ventricular (LV) measurements and calculation of LV mass were made according to standardized methods.30 Left atrial diameter (cm) was indexed by body surface area (m2) and left atrial enlargement was defined as left atrial diameter/body surface area ≥2.4 cm/m2.30 LV mass was indexed by height2.7 and LV hypertrophy was defined as LV mass/height2.7 >50 g/m2.7 in men and >47 g/m2.7 in women.31 LV ejection fraction was calculated using the Teichholz formula or the Simpson rule30 and defined as low when it was <50%.
Follow-up
Subjects were followed-up in our outpatient clinic or by their family doctors. The occurrence of events was recorded during follow-up visits or by telephone interview of the family doctor or the patient or a family member, followed by a visit if the patient was alive. Medical records were obtained to confirm the events. We evaluated a combined endpoint including coronary events (sudden death, fatal and nonfatal myocardial infarction, and coronary revascularization), fatal and nonfatal stroke, heart failure requiring hospitalization, and peripheral revascularization. Outcomes were defined according to standard criteria as previously reported.32–35
Statistical analysis
Data are means ± standard deviation or numbers and percentage. Comparison between CH and MUCH according to various definitions was performed by using unpaired t test for continuous variables and chi-square or Fisher’s exact test for categorical variables. Event rates were expressed as the number of events per 100 patient-years. Univariate and multivariate Cox regression analyses were used to estimate the association of MUCH definitions with outcome. The forced entry model was used in multivariate analysis. Forest plot was also built and hazard ratios were compared. Statistical significance was defined as P < 0.05. Analyses were made with the SPSS 21 software package (SPSS, Chicago, IL) and the Comprehensive Meta-Analysis software version 2 (Biostat, Englewood, NJ).
RESULTS
Prevalence and ambulatory BP features of different MUCH definitions are reported in Table 1.
Table 1.
Prevalence and ambulatory blood pressure features of different MUCH definitions
| Daytime BP ≥135/85 mm Hg only | Nighttime BP ≥120/70 mm Hg only | Daytime BP ≥135/85 mm Hg + nighttime BP ≥120/70 mm Hg | Total | |
|---|---|---|---|---|
| n | n | n | n (%) | |
| Daytime MUCH (regardless of nighttime BP) | 42 | — | 173 | 215 (29) |
| Nighttime MUCH (regardless of daytime BP) | — | 184 | 173 | 357 (48.5) |
| 24-hour MUCH (regardless of daytime or nighttime BP) | 33 | 69 | 173 | 275 (37) |
| Daytime MUCH only | 42 | — | — | 42 (5.5) |
| Nighttime MUCH only | — | 184 | — | 184 (25) |
| Daytime + nighttime MUCH | — | — | 173 | 173 (23.5) |
Abbreviations: BP, blood pressure; MUCH, masked uncontrolled hypertension.
Characteristics, laboratory findings, echocardiographic data, BP values and antihypertensive therapy of patients with CH, daytime MUCH regardless of nighttime BP, nighttime MUCH regardless of daytime BP, and 24-hour MUCH regardless of daytime or nighttime BP are presented in Table 2. Use of aspirin and statin was not different between patients with CH and MUCH for each definition (14–16% vs. 13–16% and 7–9% vs. 6–8%, respectively).
Table 2.
Characteristics of patients by specific thresholds regardless of the other time intervals
| Parameter | Daytime BP threshold (regardless of nighttime BP) | Nighttime BP threshold (regardless of daytime BP) | 24-hour BP threshold (regardless of daytime or nighttime BP) | |||
|---|---|---|---|---|---|---|
| CH | MUCH | CH | MUCH | CH | MUCH | |
| n | 523 | 215 | 381 | 357 | 463 | 275 |
| Age, years | 61 ± 10 | 60 ± 11 | 60 ± 11 | 61 ± 11 | 61 ± 10 | 60 ± 11 |
| Men, n (%) | 202 (39) | 126 (59)† | 127 (33) | 201 (56)† | 166 (36) | 162 (59)† |
| Body mass index, kg/m2 | 28 ± 5 | 28 ± 4.0 | 28 ± 5 | 28 ± 4 | 28 ± 5 | 28 ± 4 |
| Smokers, n (%) | 84 (16) | 54 (25)† | 74 (19) | 64 (18) | 76 (16) | 62 (22)* |
| FHCVD, n (%) | 64 (12) | 19 (9) | 41 (11) | 42 (12) | 59 (13) | 24 (9) |
| Previous events, n (%) | 29 (6) | 8 (4) | 15 (4) | 22 (6) | 24 (5) | 13 (5) |
| Diabetes, n (%) | 27 (5) | 14 (7) | 23 (6) | 18 (5) | 24 (5) | 17 (6) |
| eGFR, ml/min/1.73 m2 | 75 ± 19 | 77 ± 21 | 75 ± 40 | 76 ± 19 | 74 ± 19 | 77 ± 20* |
| LDL cholesterol, mg/dl | 129 ± 30 | 127 ± 28 | 130 ± 29 | 126 ± 30* | 130 ± 29 | 126 ± 30 |
| LV hypertrophy, n (%) | 79 (15) | 57 (27)† | 55 (14) | 81 (23)† | 69 (15) | 67 (24)† |
| LA enlargement, n (%) | 74 (14) | 32 (15) | 39 (10) | 67 (19)† | 62 (13) | 44 (16) |
| ALVSD, n (%) | 12 (2) | 6 (3) | 9 (2) | 9 (2) | 11 (2) | 7 (2) |
| Clinic SBP, mm Hg | 130 ± 7 | 134 ± 5† | 129 ± 7 | 133 ± 6† | 129 ± 7 | 133 ± 6† |
| Clinic DBP, mm Hg | 80 ± 6 | 83 ± 5† | 79 ± 6 | 83 ± 5† | 79 ± 6 | 83 ± 5† |
| Daytime SBP, mm Hg | 121 ± 8 | 137 ± 7† | 122 ± 9 | 131 ± 9† | 121 ± 8 | 134 ± 8† |
| Daytime DBP, mm Hg | 75 ± 6 | 84 ± 7† | 74 ± 7 | 81 ± 7† | 74 ± 6 | 83 ± 7† |
| Nighttime SBP, mm Hg | 110 ± 11 | 122 ± 12† | 106 ± 8 | 122 ± 11† | 109 ± 9 | 123 ± 12† |
| Nighttime DBP, mm Hg | 65 ± 7 | 72 ± 8† | 61 ± 5 | 73 ± 7† | 63 ± 6 | 73 ± 7† |
| 24-hour SBP, mm Hg | 118 ± 8 | 133 ± 8† | 117 ± 8 | 128 ± 9† | 117 ± 7 | 131 ± 8† |
| 24-hour DBP, mm Hg | 72 ± 6 | 80 ± 7† | 71 ± 8 | 78 ± 7† | 71 ± 6 | 80 ± 7† |
| Diuretic, n (%) | 207 (40) | 84 (39) | 159 (42) | 132 (37) | 185 (40) | 106 (39) |
| Beta-blocker, n (%) | 177 (34) | 67 (31) | 128 (34) | 116 (33) | 163 (35) | 81 (30) |
| Calcium antagonist, n (%) | 145 (28) | 78 (36)* | 91 (24) | 132 (37)† | 119 (26) | 104 (38)† |
| ACE-I, n (%) | 226 (43) | 84 (39) | 170 (45) | 140 (39) | 202 (44) | 108 (39) |
| ARB, n (%) | 105 (20) | 36 (17) | 83 (22) | 58 (16) | 98 (21) | 43 (16) |
| Alpha-blocker, n (%) | 51 (10) | 26 (12) | 29 (8) | 48 (13)* | 40 (9) | 37 (14)* |
| Single therapy, n (%) | 246 (47) | 99 (46) | 182 (48) | 163 (46) | 220 (48) | 125 (46) |
| Double therapy, n (%) | 194 (37) | 79 (37) | 139 (36) | 134 (37) | 167 (36) | 106 (38) |
| Triple therapy, n (%) | 83 (16) | 37 (17) | 60 (16) | 60 (17) | 76 (16) | 44 (16) |
| A-H medications, n | 1.69 ± 0.7 | 1.71 ± 0.7 | 1.68 ± 0.7 | 1.71 ± 0.7 | 1.69 ± 0.7 | 1.71 ± 0.7 |
Abbreviations: ACE-I, angiotensin-converting enzyme inhibitor; A-H, anti-hypertensive; ALVSD, asymptomatic left ventricular systolic dysfunction (ejection fraction <50%); ARB, angiotensin receptor blocker; BP, blood pressure; CH, controlled hypertension (below threshold value for each classification); DBP, diastolic blood pressure; eGFR, estimated glomerular filtration rate; FHCVD, family history of cardiovascular disease; LA, left atrial; LDL, low-density lipoprotein; LV, left ventricular; MUCH, masked uncontrolled hypertension (above threshold value for each classification, that is, >135/85 mm Hg for daytime, >120/70 for nighttime, and >130/80 for 24-hour BP); SBP, systolic blood pressure.
*P < 0.05, †P < 0.01 vs. CH for each classification.
Characteristics, laboratory findings, echocardiographic data, BP values and antihypertensive therapy of patients with CH, daytime MUCH only, nighttime MUCH only, and daytime + nighttime MUCH are available in Table 3. Use of aspirin and statin was not different between patients with CH and MUCH for each definition (14% vs. 13–18% and 8% vs. 6–10%, respectively).
Table 3.
Characteristics of patients by specific thresholds only
| Parameter | CH | Daytime MUCH only | Nighttime MUCH only | Daytime + nighttime MUCH |
|---|---|---|---|---|
| N | 339 | 42 | 184 | 173 |
| Age, years | 60 ± 11 | 59 ± 9 | 62 ± 10 | 59 ± 11 |
| Men, n (%) | 103 (30) | 24 (57)† | 99 (54)† | 102 (59)† |
| Body mass index, kg/m2 | 28 ± 5 | 28 ± 4 | 28 ± 4 | 28 ± 4 |
| Smokers, n (%) | 59 (17) | 15 (36)† | 25 (14) | 39 (23) |
| FHCVD, n (%) | 40 (12) | 1 (2) | 24 (13) | 18 (10) |
| Previous events, n (%) | 14 (4) | 1 (2) | 15 (8) | 7 (4) |
| Diabetes, n (%) | 19 (6) | 4 (10) | 8 (4) | 10 (6) |
| eGFR, ml/min/1.73 m2 | 74 ± 19 | 80 ± 26 | 75 ± 19 | 76 ± 20 |
| LDL cholesterol, mg/dl | 131 ± 29 | 126 ± 31 | 126 ± 32* | 127 ± 28 |
| LV hypertrophy, n (%) | 45 (13) | 10 (24) | 34 (19) | 47 (27)† |
| LA enlargement, n (%) | 36 (11) | 3 (7) | 38 (21)† | 29 (17)* |
| ALVSD, n (%) | 8 (2) | 1 (2) | 4 (2) | 5 (3) |
| Clinic SBP, mm Hg | 129 ± 7 | 134 ± 4† | 131 ± 7† | 134 ± 5† |
| Clinic DBP, mm Hg | 79 ± 6 | 83 ± 5† | 82 ± 6† | 83 ± 6† |
| Daytime SBP, mm Hg | 120 ± 8 | 137 ± 6† | 125 ± 6† | 137 ± 7† |
| Daytime DBP, mm Hg | 73 ± 6 | 83 ± 7† | 78 ± 5† | 84 ± 6† |
| Nighttime SBP, mm Hg | 106 ± 8 | 110 ± 9† | 119 ± 10† | 125 ± 11† |
| Nighttime DBP, mm Hg | 61 ± 5 | 63 ± 5* | 72 ± 6† | 74 ± 8† |
| 24-hour SBP, mm Hg | 116 ± 7 | 130 ± 6† | 123 ± 7† | 134 ± 8† |
| 24-hour DBP, mm Hg | 70 ± 6 | 78 ± 6† | 76 ± 5† | 81 ± 7† |
| Diuretic, n (%) | 144 (43) | 15 (36) | 63 (34) | 69 (40) |
| Beta-blocker, n (%) | 113 (33) | 15 (36) | 64 (35) | 52 (30) |
| Calcium antagonist, n (%) | 76 (22) | 15 (36) | 69 (38)† | 63 (36)† |
| ACE-I, n (%) | 155 (46) | 15 (36) | 71 (39) | 69 (40) |
| ARB, n (%) | 76 (22) | 7 (17) | 29 (16) | 29 (17) |
| Alpha-blocker, n (%) | 25 (7) | 4 (10) | 26 (14)* | 22 (13)* |
| Single therapy, n (%) | 163 (48) | 19 (45) | 83 (45) | 80 (46) |
| Double therapy, n (%) | 120 (35) | 19 (45) | 74 (40) | 60 (35) |
| Triple therapy, n (%) | 56 (17) | 4 (10) | 27 (15) | 33 (19) |
| A-H medications, n | 1.68 ± 0.7 | 1.64 ± 0.7 | 1.70 ± 0.7 | 1.73 ± 0.8 |
Abbreviations: ACE-I, angiotensin-converting enzyme inhibitor; A-H, anti-hypertensive; ALVSD, asymptomatic left ventricular systolic dysfunction (ejection fraction <50%); ARB, angiotensin receptor blocker; CH, controlled hypertension (below daytime, nighttime, and 24-hour threshold values); DBP, diastolic blood pressure; eGFR, estimated glomerular filtration rate; FHCVD, family history of cardiovascular disease; LA, left atrial; LDL, low-density lipoprotein; LV, left ventricular; MUCH, masked uncontrolled hypertension (above threshold value for each classification, that is, ≥135/85 mm Hg for daytime and ≥120/70 for nighttime BP); SBP, systolic blood pressure.
*P < 0.05, †P < 0.01 vs. CH.
As reported in Tables 2 and 3, 24-hour BP was progressively lower from daytime + nighttime MUCH to daytime MUCH regardless of nighttime BP to 24-hour MUCH regardless of daytime or nighttime BP to daytime MUCH only to nighttime MUCH regardless of daytime BP and to nighttime MUCH only.
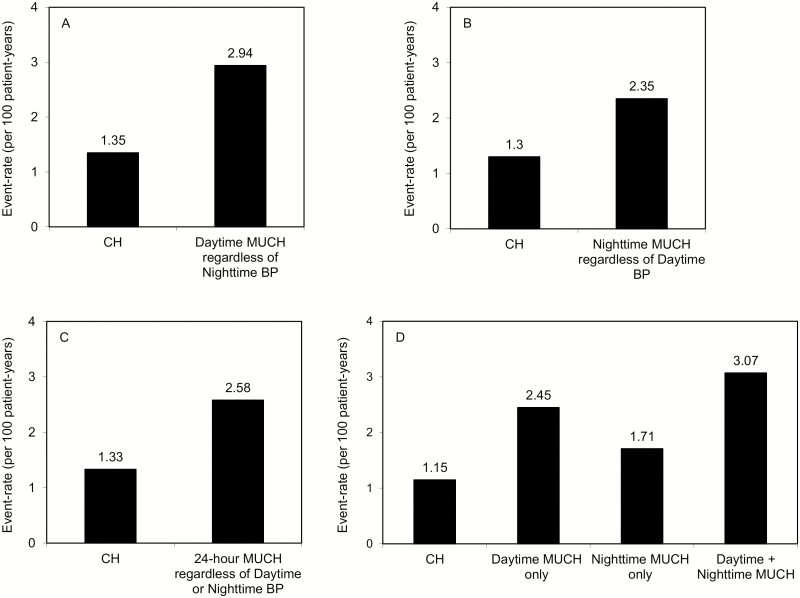
During the follow-up (10 ± 5 years, range 0.4–21 years), 148 events occurred in patients with CH and MUCH. Event rates according to different definitions are reported in Figure 1.
Figure 1.
Event rates in patients with different definitions of controlled hypertension (CH) and masked uncontrolled hypertension (MUCH). There were 79 events in patients with CH and 69 in those with daytime MUCH regardless of nighttime BP (Panel A), 55 in patients with CH and 93 in those with nighttime MUCH regardless of daytime BP (Panel B), 67 in patients with CH and 81 in those with 24-hour MUCH regardless of daytime or nighttime BP (Panel C), and 43, 12, 36, and 57 in patients with CH (nonhypertensive daytime, nighttime, and 24-hour BP) and daytime MUCH only, nighttime MUCH only, and daytime + nighttime MUCH, respectively (Panel D). Abbreviation: BP, blood pressure.
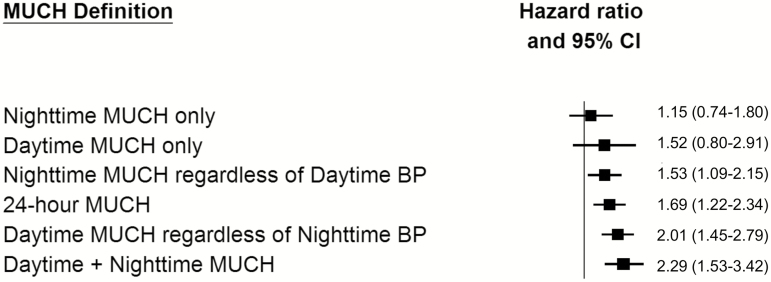
Results of univariate and multivariate Cox regression analyses are reported in Table 4. In univariate analysis, daytime MUCH regardless of nighttime BP, nighttime MUCH regardless of daytime BP, 24-hour BP MUCH regardless of daytime or nighttime BP, daytime MUCH only, and daytime + nighttime MUCH were associated with increased risk, whereas nighttime MUCH only did not attain statistical significance. After adjustment for covariates, risk remained higher in all MUCH definitions that were associated with outcome in univariate analysis, except for daytime MUCH only (probably because of the small sample size).
Table 4.
Risk of cardiovascular events according to masked uncontrolled hypertension definition when compared with controlled hypertension
| Unadjusted | Adjusteda | |
|---|---|---|
| HR (95% CI) | HR (95% CI) | |
| Daytime MUCH (regardless of nighttime BP) | 2.21 (1.60–3.06) | 2.01 (1.45–2.79) |
| Nighttime MUCH (regardless of daytime BP) | 1.83 (1.31–2.55) | 1.53 (1.09–2.15) |
| 24-hour MUCH (regardless of daytime or nighttime BP) | 1.90 (1.37–2.63) | 1.69 (1.22–2.34) |
| Daytime MUCH only | 2.04 (1.07–3.86) | 1.52 (0.80–2.91) |
| Nighttime MUCH only | 1.47 (0.94–2.29) | 1.15 (0.74–1.80) |
| Daytime + nighttime MUCH | 2.75 (1.85–4.08) | 2.29 (1.53–3.42) |
Abbreviations: BP, blood pressure; CI, confidence interval; HR, hazard ratio; MUCH, masked uncontrolled hypertension.
aAdjusted for age, sex, body mass index, smoking habit, family history of cardiovascular disease, diabetes, previous events, estimated glomerular filtration rate, low-density lipoprotein cholesterol, left ventricular hypertrophy, left atrial enlargement, and asymptomatic left ventricular systolic dysfunction (ejection fraction <50%).
Figure 2 shows in increasing order adjusted hazard ratios described in Table 4. From visual inspection it is evident that there is a numerical difference, sometimes even substantial, between various hazard ratios. However, when the hazard ratios were compared, there was no statistically significant difference (P = 0.75), probably because of the limited number of patients and events.
Figure 2.
Risk of cardiovascular events of different masked uncontrolled hypertension (MUCH) definitions vs. controlled hypertension (CH) in increasing order. Vertical line is for hazard ratio = 1. Abbreviations: BP, blood pressure; CI, confidence interval.
DISCUSSION
The present study shows that different definitions of MUCH may be associated with a different prognostic impact. Compared with CH, the increased cardiovascular risk was lowest in nighttime MUCH only, intermediate in daytime MUCH only, nighttime MUCH regardless of daytime BP, and 24-hour MUCH regardless of daytime or nighttime BP and highest in daytime MUCH regardless of nighttime BP and daytime + nighttime MUCH.
Most of previous studies evaluating the prognostic value of MUCH have used daytime and/or nighttime and/or 24-hour BP thresholds for its definition but did not compare various definitions within the same study.8–19 At present, to the best of our knowledge, there is a single report in the literature assessing the prognostic value of different definitions of MUCH.18 The Jackson Heart Study,18 including 738 Black adults, evaluated the prognostic impact of daytime, nighttime, and 24-hour MUCH. Compared with CH, the hazard ratios for cardiovascular disease according to various models were 2.33–3.18, 2.00–2.43, and 2.23–3.14 in daytime, nighttime, and 24-hour MUCH, respectively.18 All definitions were associated with risk but a decreasing gradient of risk from daytime to 24-hour to nighttime MUCH was observed.18 The Jackson Heart Study definitions of daytime, nighttime, and 24-hour MUCH18 resemble our definitions of daytime MUCH regardless of nighttime BP, nighttime MUCH regardless of daytime BP, and 24-hour MUCH regardless of daytime or nighttime BP. All these MUCH types in our study were independently associated with increased risk, when compared with CH, with a decreasing risk gradient from daytime to 24-hour to nighttime MUCH regardless of the other time intervals. Thus, our data are similar to those reported in the Jackson Heart Study. However, the Jackson Heart Study’s groups with daytime, nighttime, and 24-hour MUCH and our groups with daytime MUCH regardless of nighttime BP, nighttime MUCH regardless of daytime BP, and 24-hour MUCH regardless of daytime or nighttime BP do not disentangle patients with daytime MUCH only, nighttime MUCH only, and daytime + nighttime MUCH. We also classified our patients according to these criteria observing a decreasing risk gradient from daytime + nighttime MUCH to daytime MUCH only and to nightime MUCH only. Our data add further knowledge on the ways in which MUCH can be classified and their potential prognostic implications.
We observed that daytime + nighttime MUCH and daytime MUCH regardless of nighttime BP (likewise to daytime MUCH definition in the Jackson Heart Study) were associated with the highest hazard ratios when compared with CH. These definitions were also associated with the highest 24-hour BP in our study. If this finding appears obvious in patients with daytime + nighttime MUCH, it is also true in those with daytime MUCH regardless of nighttime BP probably because daytime BP is generally higher and longer lasting than nighttime BP and this definition captured very frequently high nighttime BP. It has recently been reported that the higher the 24-hour BP the higher the cardiovascular risk,36 and this aspect could help explain our findings.
At present, there are not yet data showing the superiority of out-of-office BP control over clinic BP control in reducing risk and a multicenter study37 is ongoing to evaluate whether out-of-office BP control improves cardiovascular outcome in patients with MUCH. However, given that different types of MUCH are associated with different prognostic impact, our data suggest that therapeutic strategies should be targeted on MUCH type for a better out-of-office BP control and risk reduction.
Some meta-analyses have assessed the prognostic significance of MUCH.21–27 The present data remark that comparisons across studies should be based on the same classification of MUCH.
The present study has some limitations. First, we studied only Caucasian subjects and our results cannot be applied to other ethnic groups. It cannot be excluded that the impact of daytime, nighttime, and 24-hour BP could be different in patients with MUCH in different ethnic groups. Second, though we observed an evident numerical difference between various hazard ratios, we could not find a statistically significant difference because of the limited sample size; future larger studies are needed to confirm our findings. Third, our data can only be applied to patients with MUCH and not to all untreated or treated hypertensive patients in whom the impact of daytime, nighttime, and 24-hour BP might be different.36,38–40
In conclusion, our study shows that the prognostic impact of MUCH defined according to various ambulatory BP criteria may be different. This finding might suggest that (i) therapeutic strategies should be targeted on MUCH type for a better ambulatory BP control and risk reduction, and (ii) comparison across studies evaluating the prognostic value of MUCH should be performed by using the same definition.
DISCLOSURE
The authors declared no conflict of interest.
Supplementary Material
REFERENCES
- 1. Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta analysis. Am J Hypertens 2011; 24:52–58. [DOI] [PubMed] [Google Scholar]
- 2. Asayama K, Thijs L, Li Y, Gu YM, Hara A, Liu YP, Zhang Z, Wei FF, Lujambio I, Mena LJ, Boggia J, Hansen TW, Björklund-Bodegård K, Nomura K, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Stolarz-Skrzypek K, Malyutina S, Casiglia E, Nikitin Y, Lind L, Luzardo L, Kawecka-Jaszcz K, Sandoya E, Filipovský J, Maestre GE, Wang J, Imai Y, Franklin SS, O’Brien E, Staessen JA; International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes (IDACO) Investigators Setting thresholds to varying blood pressure monitoring intervals differentially affects risk estimates associated with white-coat and masked hypertension in the population. Hypertension 2014; 64:935–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, Menard J, Mallion JM. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA 2004; 291:1342–1349. [DOI] [PubMed] [Google Scholar]
- 4. Shimada K, Fujita T, Ito S, Naritomi H, Ogihara T, Shimamoto K, Tanaka H, Yoshiike N. The importance of home blood pressure measurement for preventing stroke and cardiovascular disease in hypertensive patients: a sub-analysis of the Japan Hypertension Evaluation with Angiotensin II Antagonist Losartan Therapy (J-HEALTH) study, a prospective nationwide observational study. Hypertens Res 2008; 31:1903–1911. [DOI] [PubMed] [Google Scholar]
- 5. Stergiou GS, Asayama K, Thijs L, Kollias A, Niiranen TJ, Hozawa A, Boggia J, Johansson JK, Ohkubo T, Tsuji I, Jula AM, Imai Y, Staessen JA; International Database on HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO) Investigators Prognosis of white-coat and masked hypertension: International Database of HOme blood pressure in relation to Cardiovascular Outcome. Hypertension 2014; 63:675–682. [DOI] [PubMed] [Google Scholar]
- 6. Tientcheu D, Ayers C, Das SR, McGuire DK, de Lemos JA, Khera A, Kaplan N, Victor R, Vongpatanasin W. Target organ complications and cardiovascular events associated with masked hypertension and white-coat hypertension: analysis from the Dallas Heart Study. J Am Coll Cardiol 2015; 66:2159–2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kushiro T, Kario K, Saito I, Teramukai S, Sato Y, Okuda Y, Shimada K. Increased cardiovascular risk of treated white coat and masked hypertension in patients with diabetes and chronic kidney disease: the HONEST Study. Hypertens Res 2017; 40:87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez DA, Fagard RH, Gheeraert PJ, Missault LH, Braun JJ, Six RO, Van Der Niepen P, O’Brien E; Office versus Ambulatory Pressure Study Investigators Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med 2003; 348:2407–2415. [DOI] [PubMed] [Google Scholar]
- 9. Ohkubo T, Kikuya M, Metoki H, Asayama K, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y. Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol 2005; 46:508–515. [DOI] [PubMed] [Google Scholar]
- 10. Pierdomenico SD, Lapenna D, Bucci A, Di Tommaso R, Di Mascio R, Manente BM, Caldarella MP, Neri M, Cuccurullo F, Mezzetti A. Cardiovascular outcome in treated hypertensive patients with responder, masked, false resistant, and true resistant hypertension. Am J Hypertens 2005; 18:1422–1428. [DOI] [PubMed] [Google Scholar]
- 11. Fagard RH, Van Den Broeke C, De Cort P. Prognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens 2005; 19:801–807. [DOI] [PubMed] [Google Scholar]
- 12. Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp-Pedersen C. Ambulatory blood pressure monitoring and risk of cardiovascular disease: a population based study. Am J Hypertens 2006; 19:243–250. [DOI] [PubMed] [Google Scholar]
- 13. Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension 2006; 47:846–853. [DOI] [PubMed] [Google Scholar]
- 14. Hansen TW, Kikuya M, Thijs L, Björklund-Bodegård K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Jeppesen J, Ibsen H, Imai Y, Staessen JA; IDACO Investigators Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7,030 individuals. J Hypertens 2007; 25:1554–1564. [DOI] [PubMed] [Google Scholar]
- 15. Ben-Dov IZ, Kark JD, Mekler J, Shaked E, Bursztyn M. The white coat phenomenon is benign in referred treated patients: a 14-year ambulatory blood pressure mortality study. J Hypertens 2008; 26:699–705. [DOI] [PubMed] [Google Scholar]
- 16. Franklin SS, Thijs L, Hansen TW, Li Y, Boggia J, Kikuya M, Björklund-Bodegård K, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA; International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes Investigators Significance of white-coat hypertension in older persons with isolated systolic hypertension: a meta-analysis using the International Database on Ambulatory Blood Pressure Monitoring in Relation to Cardiovascular Outcomes population. Hypertension 2012; 59:564–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Franklin SS, Thijs L, Li Y, Hansen TW, Boggia J, Liu Y, Asayama K, Björklund-Bodegård K, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Filipovsky J, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA; International Database on Ambulatory blood pressure in Relation to Cardiovascular Outcomes Investigators Masked hypertension in diabetes mellitus: treatment implications for clinical practice. Hypertension 2013; 61:964–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Booth JN 3rd, Diaz KM, Seals SR, Sims M, Ravenell J, Muntner P, Shimbo D. Masked hypertension and cardiovascular disease events in a prospective cohort of blacks: the Jackson heart study. Hypertension 2016; 68:501–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pierdomenico SD, Pierdomenico AM, Coccina F, Porreca E. Prognosis of masked and white coat uncontrolled hypertension detected by ambulatory blood pressure monitoring in elderly treated hypertensive patients. Am J Hypertens 2017; 30:1106–1111. [DOI] [PubMed] [Google Scholar]
- 20. Banegas JR, Ruilope LM, de la Sierra A, de la Cruz JJ, Gorostidi M, Segura J, Martell N, García-Puig J, Deanfield J, Williams B. High prevalence of masked uncontrolled hypertension in people with treated hypertension. Eur Heart J 2014; 35:3304–3312. [DOI] [PubMed] [Google Scholar]
- 21. Pickering TG, Eguchi K, Kario K. Masked hypertension: a review. Hypertens Res 2007; 30:479–488. [DOI] [PubMed] [Google Scholar]
- 22. Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens 2007; 25:2193–2198. [DOI] [PubMed] [Google Scholar]
- 23. Bobrie G, Clerson P, Ménard J, Postel-Vinay N, Chatellier G, Plouin PF. Masked hypertension: a systematic review. J Hypertens 2008; 26:1715–1725. [DOI] [PubMed] [Google Scholar]
- 24. Peacock J, Diaz KM, Viera AJ, Schwartz JE, Shimbo D. Unmasking masked hypertension: prevalence, clinical implications, diagnosis, correlates and future directions. J Hum Hypertens 2014; 28:521–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pierdomenico SD, Pierdomenico AM, Coccina F, Clement DL, De Buyzere ML, De Bacquer DA, Ben-Dov IZ, Vongpatanasin W, Banegas JR, Ruilope LM, Thijs L, Staessen JA. Prognostic value of masked uncontrolled hypertension. Hypertension 2018; 72:862–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zhang DY, Guo QH, An DW, Li Y, Wang JG. A comparative meta-analysis of prospective observational studies on masked hypertension and masked uncontrolled hypertension defined by ambulatory and home blood pressure. J Hypertens 2019; 37:1775–1785. [DOI] [PubMed] [Google Scholar]
- 27. Thakkar HV, Pope A, Anpalahan M. Masked hypertension: a systematic review. Heart Lung Circ 2020; 29:102–111. [DOI] [PubMed] [Google Scholar]
- 28. Pierdomenico SD, Lapenna D, Guglielmi MD, Antidormi T, Schiavone C, Cuccurullo F, Mezzetti A. Target organ status and serum lipids in patients with white coat hypertension. Hypertension 1995; 26:801–807. [DOI] [PubMed] [Google Scholar]
- 29. O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, vanMontfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y; European Society of Hypertension Working Group on Blood Pressure Monitoring European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens 2013; 31:1731–1768. [DOI] [PubMed] [Google Scholar]
- 30. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ; Chamber Quantification Writing Group ; American Society of Echocardiography’s Guidelines and Standards Committee; European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005; 18:1440–1463. [DOI] [PubMed] [Google Scholar]
- 31. de Simone G, Devereux RB, Daniels SR, Koren MJ, Meyer RA, Laragh JH. Effect of growth on variability of left ventricular mass: assessment of allometric signals in adults and children and their capacity to predict cardiovascular risk. J Am Coll Cardiol 1995; 25:1056–1062. [DOI] [PubMed] [Google Scholar]
- 32. Pierdomenico SD, Pierdomenico AM, Cuccurullo F. Morning blood pressure surge, dipping, and risk of ischemic stroke in elderly patients treated for hypertension. Am J Hypertens 2014; 27:564–570. [DOI] [PubMed] [Google Scholar]
- 33. Pierdomenico SD, Pierdomenico AM, Di Tommaso R, Coccina F, Di Carlo S, Porreca E, Cuccurullo F. Morning blood pressure surge, dipping, and risk of coronary events in elderly treated hypertensive patients. Am J Hypertens 2016; 29:39–45. [DOI] [PubMed] [Google Scholar]
- 34. Pierdomenico SD, Pierdomenico AM, Coccina F, Lapenna D, Porreca E. Ambulatory blood pressure parameters and heart failure with reduced or preserved ejection fraction in elderly treated hypertensive patients. Am J Hypertens 2016; 29:1001–1007. [DOI] [PubMed] [Google Scholar]
- 35. Pierdomenico SD, Pierdomenico AM, Coccina F, Lapenna D, Porreca E. Circadian blood pressure changes and cardiovascular risk in elderly-treated hypertensive patients. Hypertens Res 2016; 39:805–811. [DOI] [PubMed] [Google Scholar]
- 36. Yang WY, Melgarejo JD, Thijs L, Zhang ZY, Boggia J, Wei FF, Hansen TW, Asayama K, Ohkubo T, Jeppesen J, Dolan E, Stolarz-Skrzypek K, Malyutina S, Casiglia E, Lind L, Filipovský J, Maestre GE, Li Y, Wang JG, Imai Y, Kawecka-Jaszcz K, Sandoya E, Narkiewicz K, O’Brien E, Verhamme P, Staessen JA; International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes (IDACO) Investigators Association of office and ambulatory blood pressure with mortality and cardiovascular outcomes. JAMA 2019; 322:409–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Parati G, Agabiti-Rosei E, Bakris GL, Bilo G, Branzi G, Cecchi F, Chrostowska M, De la Sierra A, Domenech M, Dorobantu M, Faria T, Huo Y, Jelaković B, Kahan T, Konradi A, Laurent S, Li N, Madan K, Mancia G, McManus RJ, Modesti PA, Ochoa JE, Octavio JA, Omboni S, Palatini P, Park JB, Pellegrini D, Perl S, Podoleanu C, Pucci G, Redon J, Renna N, Rhee MY, Rodilla Sala E, Sanchez R, Schmieder R, Soranna D, Stergiou G, Stojanovic M, Tsioufis K, Valsecchi MG, Veglio F, Waisman GD, Wang JG, Wijnmaalen P, Zambon A, Zanchetti A, Zhang Y. MASked-unconTrolled hypERtension management based on office BP or on ambulatory blood pressure measurement (MASTER) Study: a randomised controlled trial protocol. BMJ Open 2018; 8:e021038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fagard RH, Celis H, Thijs L, Staessen JA, Clement DL, De Buyzere ML, De Bacquer DA. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension 2008; 51:55–61. [DOI] [PubMed] [Google Scholar]
- 39. Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA. Predictive role of the nighttime blood pressure. Hypertension 2011; 57:3–10. [DOI] [PubMed] [Google Scholar]
- 40. ABC-H Investigators, Roush GC, Fagard RH, Salles GF, Pierdomenico SD, Reboldi G, Verdecchia P, Eguchi K, Kario K, Hoshide S, Polonia J, de la Sierra A, Hermida RC, Dolan E, Zamalloa H. Prognostic impact from clinic, daytime, and night-time systolic blood pressure in nine cohorts of 13,844 patients with hypertension. J Hypertens 2014; 32:2332–2340. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.