Abstract
Objective
To identify factors that contribute to the increased susceptibility and severity of COVID-19 in obese children and adolescents, and its health consequences.
Sources
Studies published between 2000 and 2020 in the PubMed, MEDLINE, Scopus, SciELO, and Cochrane databases.
Summary of findings
Obesity is a highly prevalent comorbidity in severe cases of COVID-19 in children and adolescents; social isolation may lead to increase fat accumulation. Excessive adipose tissue, deficit in lean mass, insulin resistance, dyslipidemia, hypertension, high levels of proinflammatory cytokines, and low intake of essential nutrients are factors that compromise the functioning of organs and systems in obese individuals. These factors are associated with damage to immune, cardiovascular, respiratory, and urinary systems, along with modification of the intestinal microbiota (dysbiosis). In severe acute respiratory syndrome coronavirus 2 infection, these organic changes from obesity may increase the need for ventilatory assistance, risk of thromboembolism, reduced glomerular filtration rate, changes in the innate and adaptive immune response, and perpetuation of the chronic inflammatory response.
Conclusions
The need for social isolation can have the effect of causing or worsening obesity and its comorbidities, and pediatricians need to be aware of this issue. Facing children with suspected or confirmed COVID-19, health professionals should 1) diagnose excess weight; 2) advise on health care in times of isolation; 3) screen for comorbidities, ensuring that treatment is not interrupted; 4) measure levels of immunonutrients; 5) guide the family in understanding the specifics of the situation; and 6) refer to units qualified to care for obese children and adolescents when necessary.
Keywords: Coronavirus, Coronavirus infections, Obesity, Child, Adolescent
Resumo
Objetivo
Identificar fatores que contribuem para o aumento da suscetibilidade e gravidade da COVID-19 em crianças e adolescentes obesos e suas consequências para a saúde.
Fontes de dados
Estudos publicados entre 2000 e 2020 nas bases de dados PubMed, Medline, Scopus, SciELO e Cochrane.
Síntese dos dados
A obesidade é uma comorbidade altamente prevalente em casos graves de COVID-19 em crianças e adolescentes e o isolamento social pode levar ao aumento do acúmulo de gordura. Tecido adiposo excessivo, déficit de massa magra, resistência à insulina, dislipidemia, hipertensão, altos níveis de citocinas pró-inflamatórias e baixa ingestão de nutrientes essenciais são fatores que comprometem o funcionamento dos órgãos e sistemas no indivíduo obeso. Esses fatores estão associados a danos nos sistemas imunológico, cardiovascular, respiratório e urinário, juntamente com a modificação da microbiota intestinal (disbiose). Na infecção por SARS-CoV-2, essas alterações orgânicas causadas pela obesidade podem aumentar a necessidade de assistência ventilatória, risco de tromboembolismo, taxa de filtração glomerular reduzida, alterações na resposta imune inata e adaptativa e perpetuação da resposta inflamatória crônica.
Conclusões
A necessidade de isolamento social pode ter o efeito de causar ou agravar a obesidade e suas comorbidades e pediatras precisam estar cientes desse problema. Diante de crianças com suspeita ou confirmação de COVID-19, os profissionais de saúde devem 1) diagnosticar o excesso de peso; 2) aconselhar sobre cuidados de saúde em tempos de isolamento; 3) fazer a triagem de comorbidades, garantindo que o tratamento não seja interrompido; 4) medir os níveis de imunonutrientes; 5) orientar a família respeitando as especificidades da situação; e 6) encaminhamento a unidades qualificadas para cuidar de crianças e adolescentes obesos, quando necessário.
Palavras-chave: Coronavírus, Infecções por coronavírus, Obesidade, Criança, Adolescente
Introduction
Since December 2019, the world has been surprised by the appearance, in China, of a severe pneumonia caused by a new type of coronavirus, an infection that spread rapidly throughout countries, being considered a pandemic three months later; the disease received the name coronavirus disease 2019 (COVID-19).1, 2 As in adults, but less frequently, children with comorbidities – chronic kidney and lung diseases, malignancies, diabetes, obesity, sickle cell anemia, immune disorders, chromosomal abnormalities, heart disease, and congenital malformations – are more likely to develop severe conditions from COVID-19.3, 4, 5, 6 The present review aims to identify the factors that contribute to the increase in the susceptibility and severity of COVID-19 in obese children and adolescents, and its health consequences, to collaborate for better clinical care of these patients.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and COVID-19
Although less frequently, COVID-19 affects the pediatric age group. Some studies indicate that incidence of COVID-19 among children and adolescents can reach 5% of confirmed cases,7 being slightly higher in males.3, 8 In addition, it presents with less severity when compared to adults. In the United States, in March 2020, hospitalization rates among individuals under the age of 17 ranged between 0.1 and 0.3/100,000 inhabitants.9 Likewise, mortality among children and adolescents has been shown to be low. An epidemiological study in China with 2135 individuals under 18 years of age described only one death; infants presented, proportionally, a greater number of severe and critical cases.8 In a systematic review10 involving 2228 patients under 16 years of age, two deaths were found, one of which was the same reported in the Chinese study.8
Children and adolescents seem to acquire SARS-CoV-2 mainly through contact with infected family members.4, 11, 12, 13 However, the role of children and adolescents in transmission remains unclear;12 the presence of SARS-CoV-2 in the oropharynx and stools of asymptomatic and symptomatic individuals has been described14, 15, 16 and viral load does not differ from that of adults.17 Vertical transmission seems to be rare, with few cases described.18, 19, 20 To date, no viable viral particles have been identified in breast milk, although SARS-CoV-2 RNA has been detected in three samples.21 One study reported the presence of anti-SARS-CoV-2 IgA in breast milk of women who recovered from COVID-19.22 Tests to identify the virus in the umbilical cord, placenta, and amniotic fluid have also been negative.23, 24, 25, 26
The incubation period observed in a series of 11 studies involving individuals under the age of 16 was two to 25 days (mean = 7).13 Most children and adolescents affected by COVID-19 have mild to moderate symptoms, with a significant percentage of asymptomatic patients;13, 27 among those with severe symptoms, a small percentage will require intensive care13 and the highest proportion appears to be concentrated in children under 1 year of age.28 A systematic review found that, in 13 newborns infected with SARS-CoV-2 during perinatal period, most remained asymptomatic or had mild symptoms.29 The most common symptoms of SARS-CoV-2 infection among children and adolescents are cough and fever; sore throat, sneezing, myalgia, wheezing, fatigue, rhinorrhea, nasal obstruction, diarrhea, and vomiting; hypoxia and dyspnea are uncommon findings;10, 11, 13, 27,30 in a Chinese study with people under 16 years of age with SARS-CoV-2 infection, 28.7% presented with tachypnea.4 Discrete changes – such as leukocytosis, leukopenia, lymphopenia, and small elevation of acute phase proteins – were the most common laboratory alterations.4, 13, 30, 31 Radiographic changes are generally less pronounced than in adults, with unilateral or bilateral irregular opacification standing out in some case series.3, 4, 13, 31 In a systematic review that analyzed chest computed tomography of under 18 age patients, ‘ground glass’ opacification was observed in 37.8% of examinations, most commonly unilateral in lower lobes, and was considered mild.32
The reasons for the lower severity of COVID-19 in pediatric age group remain unanswered. Some hypotheses have been raised: less exposure to SARS-CoV-2 due to social isolation and closure of schools; lower frequency of comorbidities and exposure to smoking when compared to adults; and greater capacity for pulmonary regeneration.33, 34 Children have less angiotensin-converting enzyme 2 (ACE-2) expression than adults, making the process of internalizing the virus less efficient35 and may have more effective trained innate immunity, which is an innate memory response of medium duration, due to increased exposure to viruses and vaccines.33, 34, 36 This phenomenon has been used to explain the lower death rates by COVID-19 in countries that carry out universal BCG vaccination, compared to those that do not adopt such strategy.33, 34, 37 Furthermore, children and adolescents do not have the immunosenescence observed in older individuals, a phenomenon characterized by, among other features, a chronic inflammatory state.33, 34, 38 Finally, particularities of the expression of ACE-2 in younger individuals, as observed in animal models,39 could limit consequences of the decreased expression of that enzyme caused by the invasion of pneumocytes by SARS-CoV-2,34 especially those related to the elevation of angiotensin-II.40
Pathophysiology of obesity and its relationship with COVID-19
The relationship between obesity and viral diseases has been studied for several years. During the H1N1 epidemic, this area gained particular interest, as it was observed that obese patients had a higher risk of developing the disease, longer intensive care unit (ICU) stay, and higher mortality.41 This fact was demonstrated even for children, with impairment in immune response, especially cellular, to influenza virus, and also inadequate vaccine response when they were obese.42 Recently, during the COVID-19 epidemic in Canada, obesity was the third most prevalent demographic factor among children admitted to the ICU, behind only those with serious associated diseases, immunosuppression, and cancer.6 In New York, obesity was the most prevalent comorbidity among 50 severe cases of COVID-19 affecting children and adolescents.43
COVID-19 and risks related to obesity among adults
Regarding COVID-19, observations at the beginning of the pandemic demonstrated the existence of risk factors, such as arterial hypertension, cardiovascular diseases, diabetes, chronic respiratory conditions, and cancer;44 however, obesity was later included in this list.45 In March 2020, Wu et al.,46 describing the characteristics of 280 Chinese patients, found a statistically significant difference between the BMI of patients with mild and moderate conditions (23.6 kg/m2) and severe ones (25.8 kg/m2), but this fact did not attract the attention of these researchers, because they were unable to demonstrate the independence of BMI as a risk factor. Simonet et al.,47 in April 2020, showed a high prevalence of obesity among patients with COVID-19 exposed to mechanical ventilation. In addition, the proportion of people who needed this intervention increased according to BMI, reaching 85.7% when BMI was over 35 kg/m2.47 Finally, they found that obesity was a risk factor regardless of age, gender, or presence of diabetes or hypertension, and the risk of requiring invasive mechanical ventilation was 7.36 times higher when patients with a BMI greater than 35 kg/m2 were compared to those with BMI less than 25 kg/m2.47 Other studies confirmed these findings: Bhatraju et al.,44 reporting the first cases in the Seattle region (United States), found a mean BMI of 33.2 among 24 critically ill patients admitted to the ICU. Among Italians hospitalized for COVID-19, Busetto et al.48 found that those with overweight and obesity, even if younger, needed assisted ventilation and intensive care more frequently than patients with normal weight. Data from New York, regarding 770 patients, showed that obese people were more likely to have fever, cough, and dyspnea, in addition to significantly higher rates of ICU admission or death.49 More recently, with accumulated data from three different populations, a systematic review confirmed obesity as an independent risk factor for greater severity of COVID-19, including admission to the ICU. Finally, a very relevant finding was the demonstration, by Yates et al.,50 that the risk of acquiring the disease is greater among obese people.
COVID-19 and risks related to obesity among children and adolescents
It is still not possible to explain why the number of children affected and their manifestations vary among different regions.51 The effects of pediatric obesity on COVID-19 are not yet adequately studied and some data are inferences due to the lack of considerable number of studies published on this subject in this age group. The three main risk factors that link obesity to COVID-19 demonstrated for adults52 are also present among children and adolescents: chronic subclinical inflammation, impaired immune response, and underlying cardiorespiratory diseases. Virtually all comorbidities found in adults can be observed during childhood and adolescence,53 and obese children have inadequate immune responses to other infections, such as bacterial pneumonia,54 a common severe complications of COVID-19. Studies in animal models show that rats fed a high-fat diet have increased expression of ACE-2 in lungs, which may help explain the greater severity of the disease among obese individuals.55 Zhang et al. showed that obesity predisposes to high mortality due to COVID-19 even in young patients, aged 14 years and older56 and it is considered that it is precisely the high prevalence of obesity among young people that can shift the age curve of mortality in countries where the prevalence of overweight is higher in this group.57 The mechanisms involved include numerous aspects related to obesity itself and also to its comorbidities,6 and it should be emphasized that the risks may be present even in mildest cases of obesity.58 Below, each will be covered in detail.
Insulin resistance and dyslipidemia
In childhood and adolescence, even in the presence of obesity, type 2 diabetes mellitus is relatively uncommon.59 The high pancreatic capacity of insulin production, characteristic of younger individuals, allows compensation to occur as a result of hyperinsulinism, which has a high prevalence associated with obesity.60 Although glycemia frequently remains at normal levels, the entire pathophysiological process is present, leading to several health repercussions, such as dyslipidemia, arterial hypertension, non-alcoholic steatohepatitis, micronutrients deficiencies, increased oxidative stress, and hyperuricemia. In situations of intense metabolic activity, such as during immune response to coronavirus infection, beta cells are required to produce a high amount of insulin, which may not be achieved when they are already working at their limit;61 SARS-CoV-2 can also lead to rupture of beta cells, through interaction with ACE-2, further aggravating this process.61 In addition, insulin resistance leads to a reduction in phosphoinositidyl 3-kinase, impairing the vasoprotective and anti-inflammatory effects of nitric oxide.62
Dyslipidemias are highly prevalent among obese children and adolescents,60 and low concentrations of HDL-cholesterol and increased LDL-cholesterol are proven risk factors for progression of endothelial dysfunction and atherosclerosis.63
Respiratory system
In New York, obesity was the most important risk factor for necessity of respiratory support among 50 pediatric cases of COVID-19.43 Normal respiratory physiology is usually impaired in obese patients, including children and adolescents.64 As the lung is one of the main targets and leads to greater risks for patients with COVID-19, this aspect must always be considered. In fact, hematosis is impaired in obesity, which becomes even more relevant when the exchange areas are reduced due to coronavirus action.65 The pressure exerted by abdominal adiposity on the lungs, through the diaphragm, also acts to limit the movement of respiratory muscles, with less oxygen saturation66 and worsening clinical presentation due to the lower lung volume of obese patients.67 In addition, some comorbidities linked to obesity may contribute to a higher risk of pulmonary infections, such as the presence of asthma, which is highly prevalent among obese children,68 and obstructive sleep apnea.69 Regarding asthma, the same inflammatory mechanisms linked to leptin and IL-2, which explain the high prevalence and severity of this disease in obese children,70 are also involved in the severity of COVID-19. Finally, in addition to aspects related to impaired lung function, obese children have low exercise tolerance, which closes a vicious circle.71
Cardiovascular system
Cardiac anatomy changes linked to obesity is recognized even in very young children, in whom hypertrophy of left ventricle is observed, related to the degree of obesity and blood pressure, among other structural changes.72 Obese children and adolescents have higher blood pressure, which increases potential endothelial injury, one of the bases of COVID-19 pathophysiology.72 Children, especially obese ones, treated with antihypertensive drugs that inhibit angiotensin-converting enzyme or block angiotensin receptors, have increased expression of ACE-2, increasing their susceptibility to coronavirus.73 Childhood obesity increases risk of cardiovascular disease later in adulthood, and the explanation for this phenomenon lies in the fact that endothelial dysfunctions, in association with insulin resistance, effectively start during childhood.74 The intima layer of arteries is thickened in obese children, foreshadowing the onset of atherosclerosis, which occurs very early.75 Endothelial dysfunction occurs even in the mildest cases of obesity.76 Hardening of the arteries, associated with impaired nitrogen performance and chronic oxidative stress, has been implicated in changes linked to the severity of COVID-19, such as inflammation of endothelium, myocarditis, multiple organ failure, severe acute respiratory syndrome, and venous thromboembolism.62 Recent data from post mortem anatomopathological studies shows inclusion of coronavirus structures in endothelial cells, possibly through the use of ACE-2 receptors in the endothelium by the virus; in these cases, accumulation of inflammatory cells, venous congestion in small pulmonary veins, and inflammation of the endothelium in the intestinal circulation have been found.77 Leptin, which is usually elevated among obese people, damages endothelium leading to less nitric oxide production and increased expression of monocyte chemoattractant protein-1, contributing to the inflammatory infiltrate in vascular cells.62 Perivascular adipose tissue contributes to vasoconstriction and endothelial dysfunction through the production of inflammatory mediators, oxidative stress, and reduction in nitric oxide production.62
Subclinical inflammation
One of the most relevant aspects for understanding the severity of COVID-19 among obese patients is related to inflammatory issues.78 After coronavirus contamination, most patients develop immune defense mechanisms, which include processes related to inflammation, and this happens in a modulated way, so that the host organism is not harmed. However, some patients trigger an uncontrolled process, known as a cytokine storm, which causes tissue damage and intense homeostatic dysregulation, leading to damage of several organic functions, especially regarding the respiratory area.79 Obese patients are known to have chronic subclinical inflammation, characterized by a permanent inflammatory state, albeit of mild intensity.80 High serum concentrations of C-reactive protein and IL-6 prove this process61 which can start early. It is believed that, at least in part, this process is due to cytokines, particularly adipokines with inflammatory properties, produced by adipose tissue61 and also the drop in adiponectin, which has anti-inflammatory properties.81
Coagulation
Obese people, including children and adolescents, with COVID-19 are at increased risk of developing coagulopathy associated with poor clinical outcomes. Chronic inflammation leads to negative regulation of anticoagulant proteins (tissue factor pathway inhibitor, antithrombin, and the protein C anticoagulation system). However, it leads to positive regulation of procoagulant factors (tissue factor pathway inhibitor) and adhesion molecules (P-selectin), in addition to increases in thrombin generation and enhanced platelet activation, increasing the risk of thrombosis.62 In severe SARS-CoV-2 infections, risk of venous thromboembolism is important, as a significant percentage of patients show elevated levels of D-dimers, while others meet clinical criteria for disseminated intravascular coagulation (DIC).62 Severe infections and sepsis are a leading cause of DIC, and pro-inflammatory and immune activation observed in severe COVID-19 is likely sufficient to trigger DIC.82
Renal system
Obesity causes several structural, metabolic, and hemodynamic changes in the kidneys, leading to a lesser functional reserve of this organ.83 Ectopic deposition of fat in renal sinus is responsible for increasing its weight and volume. Hemodynamic changes lead to increased renal plasma flow and glomerular filtration rate, greater absorption of water and sodium by proximal tubules, glomerular stress, tubular hypertrophy, and glomerulomegaly, which in turn cause proteinuria and secondary glomerular sclerosis, culminating in chronic kidney disease.84 The increase in body weight and consequent reduction in urinary pH predispose to urinary lithiasis due to increased excretion of urinary oxalate, sodium, phosphate, and uric acid; obesity can also favor the appearance of some types of neoplasia in renal tissue.85 The dysregulation of lipid metabolism and hormonal responses also play a role in deterioration of renal function. Oxidative stress caused by increased fat deposition promotes inflammation, cellular hypertrophy, increased mesangial matrix, apoptosis, endothelial dysfunction, and renal fibrosis.86 Fatty acids released by adipocytes stimulate secretion of tumor necrosis factor (TNF)-alpha by macrophages, resulting in increased secretion of IL-6 in adipocytes, amplifying inflammation in renal tissue. While TNF-alpha plays a fundamental role in progression of renal fibrosis, the increase in intracellular lipids has a nephrotoxic effect (culminating in glomerulosclerosis), compromising the structure and functioning of mitochondria, which contributes to progression of kidney disease.87 Increased insulin production and insulin resistance contribute to mesangial expansion and renal fibrosis, and the observed activation of the renin-angiotensin-aldosterone system, since the vasoconstrictor effect of angiotensin II on renal arterioles leads to increased production of endothelin-1, stimulating proliferation of mesangial matrix, sodium retention, and vasoconstriction of renal arterioles.88 Coronavirus can cause acute kidney damage in up to 15% of cases, which contributes to mortality. Aggression is due to direct cytotropic effect induced by the virus through ACE-2, which is highly expressed in the kidney,89 and inflammatory response caused by cytokines due to activation of the renin-angiotensin-aldosterone system.90, 91 In addition, acute tubular necrosis and thrombotic effects secondary to endothelial dysfunction are also observed in COVID-19.92
Gut microbiota
Intestinal microbiota is a complex ecosystem with thousands of bacterial phyla and several species distributed throughout digestive tract. It is mostly composed of anaerobic microorganisms and about 90% of fecal bacteria belong to two phylogenetic lineages: Firmicutes and Bacteroidetes.93 Colonization occurs from birth and is individually different, changes over time, and can be influenced by eating habits or diseases, such as obesity and metabolic syndrome. Several studies have demonstrated a correlation between Firmicutes/Bacteroidetes ratio in both obese children and adults, suggesting intestinal dysbiosis.94 Regarding patients with COVID-19, there are reports of intestinal dysbiosis and a decrease in intestinal Lactobacillus and Bifidobacterium populations, and some hospitalized patients were treated with probiotics in order to regulate microbiota balance and reduce risk of infection secondary to bacterial translocation.95
Immune system
Obesity in childhood and adolescence alters entire immune system, changing concentrations of cytokines and proteins and the number and function of immune cells. This imbalance leads to a pro-inflammatory state, resulting in the onset or exacerbation of several diseases such as asthma, allergy, atopic dermatitis, and sleep apnea.96 In relation to COVID-19, whose severe conditions evolve with an intense and severe systemic inflammatory reaction (cytokine storms), the imbalance of immune system observed in obesity may contribute to a worse clinical outcome.79 Adipocytokines, especially leptin, play an important role in this process, as they influence number and function of immune cells through directly effects on cell metabolism. In this context, there may be an increase in cytotoxic and effector T-cells (Th1 and Th7) and M1 macrophages and, in parallel, a reduction in Treg cells and M2 macrophages. However, other molecules that are influenced by nutritional status also act on immunity, which may be increased (IL-1β, IL-6, IL-8, IL-10, IL-1RA, resistin, visfatin, TNF-α, MCP-1, MIF, MIP1 alpha and beta) or reduced (adiponectin, IL-33) in obese patients.62 In addition, imbalance between actions of lymphocytes Treg and CD17+ also contributes to the pro-inflammatory state observed in obesity.97 Furthermore, in obesity, macrophages cells constitute about 40% to 60% of cells of immune system derived from visceral adipose tissue; these macrophages are mostly activated (M1) and secrete high amounts of TNF-alpha, IL-6, IL-12, Il-1b, MCP-1, and nitric oxide.97
Nutrition and immunonutrients
Nutrition plays an important role in immune and inflammatory response, since some nutrients modulate cellular and humoral defense systems, either by modifying formation of inflammatory mediators or interfering with cellular signal transduction pathways. Nutrients have an immunomodulatory action by stimulating the cell-mediated response, modifying the balance between pro-inflammatory and anti-inflammatory cytokines, and attenuating depletion of tissue nutrients.98 Immune response depends on the sufficient supply of nutrients and adequate nutritional status has been considered an important element for coronavirus capacity response. Zhang & Liu,99 in a systematic review, showed that some nutrients are fundamental for adequate response to coronavirus: vitamins A, C, D, and E; omega 3 fatty acids; and the minerals zinc and iron. A suitable qualitative and quantitative supply allows to maintain and repair defense systems, which require adequate energy and structural support.100 Obesity has peculiarities that may impair immune response, because diet often has characteristics that can lead to “hidden hunger.” This is because, despite eating above energy needs, quality is not adequate; numerous studies point to vitamin and mineral deficiencies in those with excess weight.101
Among the most common nutritional deficiencies, hypovitaminosis D stands out, not only linked to insufficient intake, but also, and mainly, to the displacement of part of the organic pool to adipose tissue due to the lipid affinity of this vitamin.102 Additionally, it is known that a sedentary lifestyle is characteristic of obese children, causing the practice of physical activities outdoors – which would increase exposure to sun and skin formation of vitamin D – to be reduced in this group.102 Several studies have linked hypovitaminosis D to an increased risk of severe COVID-19,78 which makes this issue particularly relevant in the pediatric obese population, where the prevalence of this deficiency is high.103 Vitamin D (VD) has immunomodulatory effects, and activated T-lymphocytes and antigen presenting cells, such as macrophages and dendritic cells, express VD receptor in their membranes, leading to anti-proliferative and immunosuppressive effects on immune system cells. It inhibits secretion of IL-12 by macrophages, a fundamental cytokine in differentiation of CD4+ T-lymphocytes in Th1 cells.104 By decreasing activation of Th1 response and production of pro-inflammatory cytokines (IL-2, interferon-γ, TNF-α), VD contributes to the targeting and activation of Th2 response, favoring greater secretion of anti-inflammatory cytokines, such as IL-4.104 This immunosuppression mechanism is important to minimize deleterious effects in transplants, and in autoimmune and inflammatory diseases. Although VD induces Th2 response, it also induces expression of antimicrobial peptides in neutrophils and monocytes, as well as promotes an increase in phagocytic capacity and rapid release of reactive oxygen species.104 Induction of cathelicidins and defensins, caused by VD, reduces viral replication and concentration of proinflammatory cytokines that have potential for lung injury in cases of COVID-19.105 Additionally, hypovitaminosis D has repercussions for disorders with potential impact on COVID-19, such as arterial hypertension, hepatic steatosis, and hyperuricemia.106
Omega-3 fatty acids are considered essential lipids for humans. Eicosapentaenoic (EPA) and docosahexaenoic (DHA) fatty acids are biologically more potent immunomodulators than alpha-linolenic acid. EPA and DHA decrease activity of nuclear transcription factors that promote transcription of genes that encode proteins with pro-inflammatory action, such as TNF-α and IL-1β.107 In addition, EPA and DHA compete with arachidonic acid (omega-6) in the constitution of plasma membrane phospholipids and, consequently, for the metabolism of cyclooxygenase in cell membrane, modulating the production of prostaglandins and leukotrienes.108 Higher concentrations of EPA and DHA favor synthesis of series-3 prostaglandins and series-5 leukotrienes, which attenuate inflammatory response; and inhibit production of series-2 prostaglandins and series-4 leukotrienes, which depress thecytotoxic activity of macrophages, lymphocytes, and natural killer cells,109 with a consequent reduction in synthesis of pro-inflammatory cytokines such as IL-1, IL-6, and TNF-α.107 Immunomodulation exerted is dependent on omega-3/omega-6 ratio: a 1:5 ratio does not impair immune response; however, Western diets provide a ratio of 1:15 to 1:50, with pro-inflammatory effects.110 Consumption of omega-3 fatty acids, especially DHA, is low in most countries in the world, including Brazil.111 Although omega-3 precursors are present in vegetable oils, their conversion into DHA is low and the very excess of omega-6 intake diverts the converting enzymes, further impairing the formation of DHA and contributing to a high deficiency prevalence. Inadequate proportion of omega-3/omega-6, common in obese children,112 leads to loss of modulation of immune response, which may contribute to exacerbation of inflammatory reactions, in addition to aggravating cardiometabolic risks.113
Vitamins A, E, and C are fundamentally found in fruits and vegetables, usually little consumed by children and adolescents, including obese ones.114 Impaired nutritional status of these vitamins may impact immune response.115 Immune cells are at constant risk of oxidative damage by free radicals, which can permanently impair their ability to respond to pathogens. Increased amounts of free radicals in activated macrophages are part of normal response. Vitamin E (VE) acts as an antioxidant and protects the cell membrane against reactive oxygen species.114 Animal studies have shown that VE supplementation increases resistance to infections, including influenza viruses.116 Vitamin A (VA) guarantees the regeneration of the mucosal barriers damaged by infection and supports protective function of macrophages, neutrophils, and natural killer cells.117 It is also necessary for adaptive immunity and plays a role in development of T- and B-cells. Like VD, VA can prevent production of IL-12 cytokines by macrophages, decreasing activation of the Th1 response and increasing Th2.117 VA deficiency impairs Th2 response, which culminates in a lack of IL-4 and fails to induce IgA, impairing salivary IgA response to influenza virus infection, and intestinal response to cholera toxin.117 Vitamin C (VC) contributes to the integrity of the epithelial barrier and accumulates in phagocytic cells, such as neutrophils, which improves chemotaxis; phagocytosis; production of reactive oxygen species; and induces microbial death.118 It also contributes to apoptosis and removal of neutrophils, which have suffered cell death, from infection sites, reducing necrosis and possible tissue damage.118 VC seems to promote differentiation and proliferation of B- and T-cells, probably due to its genetic regulatory effect.118, 119 Deficiency also impairs cytotoxic capacity of neutrophils and T-lymphocytes.114 VC supplementation appears to be able to prevent and treat respiratory and systemic infections,118, 119 and a recent review highlights VC, as well as zinc and VD, as micronutrients with stronger evidence regarding their role in immunity.120
In relation to iron, obese children are at risk for iron deficiency anemia121 due to the low nutritional quality and low iron bioavailability of the diet122 and anemia has been widely demonstrated in this group.123 In addition to inadequate intake, hepcidin, the main controller of iron absorption, has increased expression in obese individuals, contributing to the condition by reducing absorption of iron by enterocytes and their export by macrophages and hepatocytes, increasing splenic and hepatic sequestrations.124
Due to the fact that they have similar nutritional sources, zinc deficiency is also believed to be present among obese children in the same way as iron deficiency, and this has been demonstrated in studies in pediatric age group.125 It should be noted that, in addition to its immunological role, zinc also participates in insulin and leptin metabolism, which can aggravate metabolic dysregulations in obese children, contributing to inadequate inflammatory response.126 Zinc acts as a cofactor for the enzyme superoxide dismutase, which reduces cellular oxidative stress and decreases activation of signaling pathways that promote inflammatory response.127 It induces monocytes to produce IL-1 and IL-6, and to inhibit the production of TNF-α, and is also involved in regulation of peroxisome proliferator-activated receptors (PPARs), whose activation is positively correlated with decrease in inflammatory response. The direct influence of zinc on immune system is due to its ability to stimulate activity of enzymes involved in mitosis.128 Zinc deficiency is related to decreased production of cytokines and interferon-α by leukocytes, atrophy of the thymus and other lymphoid organs, and changes in the proportion of lymphocytes.128
Psychosocial repercussions of COVID-19 on obesity
If, on the one hand, obese patients exhibit COVID-19 with particular characteristics, on the other hand, the pandemic has also led to socioeconomic changes that may impact childhood obesity,129 especially among the poorest.130 In this sense, an important study projected the impact of COVID-19 pandemic on the prevalence of childhood obesity in United States, according to different scenarios:131 closing schools for two months; school closures for two months associated with a 10% drop in physical activity in two subsequent months of summer; adding two more subsequent months of closed schools; adding two more subsequent months of school closures. The increase in prevalence of obesity would be 0.640, 0.972, 1.676, and 2.373 percentage points, respectively. In Italy, Pietrobelli et al.132 followed 41 obese children and adolescents during three weeks of lockdown in Verona and found no changes in vegetables consumption, but observed increased consumption of fruits, chips, red meat, and sugary drinks; the time spent in sports activities was reduced by two and a half hours per week and, in contrast, sleep period increased by 0.65 h/day; and the most impactful data refers to screen time, which increased by 4.85 h/day. An interesting aspect is the idea often disseminated in lay texts that physical activity should be avoided to protect immunity and supposedly that exercise could reduce body’s defenses, a fact that has not been scientifically demonstrated, even among athletes.133 On the contrary, physical activity is important for the proper formation of VD when performed outdoors.102 In fact, with regard to situations related to sedentary lifestyle, such as watching TV or playing video games, changes occur that are related to higher risk of obesity, such as high consumption of fast food and sugar-sweetened beverages,134 in addition to sleep disorders.135 In relation to this last aspect, the COVID-19 pandemic brings high risks for health, as several factors can contribute to quality and duration of sleep being unsatisfactory, such as stress in face of illness, interruption of activities in the morning, time available for screen use, etc.132 In this sense, in addition to predisposing to weight gain and abdominal adiposity, sleep disorders have other health repercussions, such as insulin resistance, deterioration in food quality, poor school performance, and sedentary lifestyle.136
Living with stress during COVID-19 pandemic, in addition to bringing risks of deterioration of immunity,137 may have consequences for pediatric health, in particular for nutritional and emotional areas.138 One such consequence refers to the worsening of sleep quality, discussed above. Additionally, stress increases food consumption, activates brain reward centers that raise interest in highly palatable foods (sugar, salt, and lipids), increases emotional instability, and worsens quality of life.138 Due to the prolonged time of social isolation, another aspect demonstrated in the United States was a drop in adherence to immunization programs, due to the fear of taking children to vaccinate.139 Finally, a Brazilian study showed a high incidence of peri-obstetric mortality due to COVID-19140 and this fact, in cases where delivery is feasible, may lead to a large number of infants being deprived of breastfeeding, known as a protective factor against obesity.141
Final considerations and complications for treatment
The present review has two important limitations. The first is that it is not possible, currently, to carry out a systematic review of the literature with the expected rigor in study classification, since most of published data is based on observations made less than a year ago and, generally, refer to observational and cross-sectional studies. The second is that there are few publications referring to the pediatric age group, which means that some information is, in fact, inferences about the approach to the disease in children and adolescents, based on what is observed in adults.
When the patient presents with mild COVID-19 symptoms, the treatment is only symptomatic and recovery is usually complete,142 ranging from supportive measures for mild cases (isolation, hygiene, rest, hydration, and attention to food intake) to invasive hospital procedures, such as mechanical ventilation. The convalescence period may range from one to three weeks in mild case, or up to six weeks for the most severe.143
Non-obese children are usually asymptomatic and even less susceptible to the infection.144 In these cases, telemedicine alternatives have been proposed in order to help families receive adequate guidance without the need to travel.129 However, for those who develop the most severe forms, the coexistence of obesity can hinder therapy and worsen prognosis, since the inflammatory condition is as severe as in adults.145 Also, extensive involvement of the cardiopulmonary system is frequent146 and respiratory disorders such as Pickwick syndrome, obstructive apnea, and surfactant dysfunctions may be present.147 There are also technical issues, such as the fact that many pieces of equipment may not adequately adapt to the obese patient148 and the greater difficulty of intubation of obese patients, which may lead to the occurrence of lesions and longer periods of hypoxia while the procedure is being completed.148 Nursing care is always more difficult: the possibility of more precarious hygiene and secondary contamination, as well as harder venipuncture and more likelihood to cause injury; control procedures such as blood pressure measurement and cardiac auscultation are more difficult and more error-prone; and the risk of bedsores during intensive care unit stay is always higher the higher the patient’s weight.149
For families, supportive measures that provide high quality information and guidance to help them make decisions on medications, the need to go to the emergency room, and how to conduct emergency care are essential.129 For adolescents, adequate information can often aid to minimize extreme behaviors, both in the aspect of excessive fear, for some, and in the sense of invulnerability, for others.150
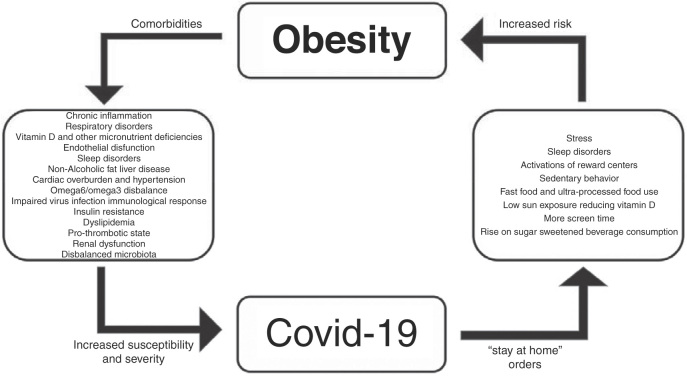
Fig. 1 shows a brief synopsis regarding the relationships between obesity and COVID-19.
Figure 1.
Interrelationships between obesity and COVID-19.
In conclusion, obesity in childhood and adolescence can be considered a risk factor for greater susceptibility and severity of COVID-19 and is associated with nutritional, cardiac, respiratory, renal, and immunological alterations, which may potentiate the complications of SARS-CoV-2 infection. The need for social isolation can have the effect of causing or worsening obesity and its comorbidities, and pediatricians need to be aware of this issue. It is necessary that health professionals, when faced with the care of children with suspected or confirmation of COVID-19, carry out the assessment of nutritional status in order to diagnose overweight; be concerned with guidance on care, in periods of isolation, with the general state of health, including the areas of nutrition, immunization, and psychosocial aspects; trace comorbidities associated with obesity, ensuring that their treatment is not interrupted; screen immunonutrients levels to assess the need for supplementation; provide information to the family respecting the specificities of the condition; and determine, when necessary, referral to hospital units suitable for the care of obese children and adolescents.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Nogueira-de-Almeida CA, Ciampo LA, Ferraz IS, Ciampo IR, Contini AA, Ued FV. COVID-19 and obesity in childhood and adolescence: a clinical review. J Pediatr (Rio J). 2020;96:546–58.
Study conducted at Universidade Federal de São Carlos, Departamento de Medicina, São Carlos, SP, Brazil.
References
- 1.Cespedes M.D., Souza J. Coronavirus: a clinical update of COVID-19. Rev Assoc Med Bras (1992). 2020;66:116–123. doi: 10.1590/1806-9282.66.2.116. [DOI] [PubMed] [Google Scholar]
- 2.González J.J.E. SARS-CoV-2 and COVID-19. A pandemic review. Medicina Crítica. 2020;33:53–67. [Google Scholar]
- 3.Gotzinger F., Santiago-Garcia B., Noguera-Julian A., Lanaspa M., Lancella L., Calo Carducci F.I., et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child Adolesc Health. 2020;4:653–661. doi: 10.1016/S2352-4642(20)30177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta N., Kalra A., Nowacki A.S., Anjewierden S., Han Z., Bhat P., et al. Association of use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with testing positive for coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1855. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oualha M., Bendavid M., Berteloot L., Corsia A., Lesage F., Vedrenne M., et al. Severe and fatal forms of COVID-19 in children. Arch Pediatr. 2020;27:235–238. doi: 10.1016/j.arcped.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shekerdemian L.S., Mahmood N.R., Wolfe K.K., Riggs B.J., Ross C.E., McKiernan C.A., et al. Characteristics and outcomes of children with coronavirus disease 2019 (COVID-19) infection admitted to US and Canadian pediatric intensive care units. JAMA Pediatr. 2020;174:868–873. doi: 10.1001/jamapediatrics.2020.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hon K.L., Leung K.K., Leung A.K., Sridhar S., Qian S., Lee S.L., et al. Overview: the history and pediatric perspectives of severe acute respiratory syndromes: novel or just like SARS. Pediatr Pulmonol. 2020;55:1584–1591. doi: 10.1002/ppul.24810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z., et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. J Emerg Med. 2020;58:712–713. [Google Scholar]
- 9.Garg S. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 -COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Panahi L., Amiri M., Pouy S. Clinical characteristics of COVID-19 infection in newborns and pediatrics: a systematic review. Arch Acad Emerg Med. 2020;8:e50. [PMC free article] [PubMed] [Google Scholar]
- 11.Cai J., Xu J., Lin D., Yang Z., Xu L., Qu Z., et al. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa198. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rajmil L. Role of children in the transmission of the COVID-19 pandemic: a rapid scoping review. BMJ Paediatr Open. 2020;4:e000722. doi: 10.1136/bmjpo-2020-000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zimmermann P., Curtis N. COVID-19 in children, pregnancy and neonates: a review of epidemiologic and clinical features. Pediatr Infect Dis J. 2020;39:469–477. doi: 10.1097/INF.0000000000002700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.L’Huillier A.G., Torriani G., Pigny F., Kaiser L., Eckerle I. Culture-competent SARS-CoV-2 in nasopharynx of symptomatic neonates, children, and adolescents. Emerg Infect Dis. 2020;26 doi: 10.3201/eid2610.202403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu Y., Li X., Zhu B., Liang H., Fang C., Gong Y., et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020;26:502–505. doi: 10.1038/s41591-020-0817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yuan C., Zhu H., Yang Y., Cai X., Xiang F., Wu H., et al. Viral loads in throat and anal swabs in children infected with SARS-CoV-2. Emerg Microbes Infect. 2020;9:1233–1237. doi: 10.1080/22221751.2020.1771219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jones Tc, Mühlemann B., Veith T., Biele G., Zuchowski M., Hoffmann J., et al. An analysis of SARS-CoV-2 viral load by patient age. medRxiv. 2020 doi: 10.1101/2020.06.08.20125484. [Epub ahead of print] [DOI] [Google Scholar]
- 18.Alzamora M.C., Paredes T., Caceres D., Webb C.M., Valdez L.M., La Rosa M. Severe COVID-19 during pregnancy and possible vertical transmission. Am J Perinatol. 2020;37:861–865. doi: 10.1055/s-0040-1710050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dong L., Tian J., He S., Zhu C., Wang J., Liu C., et al. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020;323:1846–1848. doi: 10.1001/jama.2020.4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gordon M., Kagalwala T., Rezk K., Rawlingson C., Ahmed M.I., Guleri A. Rapid systematic review of neonatal COVID-19 including a case of presumed vertical transmission. BMJ Paediatr Open. 2020;4 doi: 10.1136/bmjpo-2020-000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WHO . World Health Organization; Geneva: 2020. Breastfeeding and COVID-19: scientific brief.https://apps.who.int/iris/bitstream/handle/10665/332639/WHO-2019-nCoV-Sci_Brief-Breastfeeding-2020.1-eng.pdf Contract No.: WHO/2019-nCoV/Sci_Brief/Breastfeeding/2020.1. [cited 15 Jul 2020]. Available from: [Google Scholar]
- 22.Fox A., Marino J., Amanat F., Krammer F., Hahn-Holbrook J., Zolla-Pazner S., et al. Evidence of a significant secretory-IgA-dominant SARS-CoV-2 immune response in human milk following recovery from COVID-19. medRxiv. 2020 doi: 10.1101/2020.05.04.20089995. [Epub ahead of print] [DOI] [Google Scholar]
- 23.Li Y., Zhao R., Zheng S., Chen X., Wang J., Sheng X., et al. Lack of vertical transmission of severe acute respiratory syndrome coronavirus 2, China. Emerg Infect Dis. 2020;26:1335–1336. doi: 10.3201/eid2606.200287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu W., Wang J., Li W., Zhou Z., Liu S., Rong Z. Clinical characteristics of 19 neonates born to mothers with COVID-19. Front Med. 2020;14:193–198. doi: 10.1007/s11684-020-0772-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Far S., Agora S.A. SARS-CoV-2 infection in neonate: what do we know. Lancet. 2020;395:809–815. [Google Scholar]
- 26.Yang P., Wang X., Liu P., Wei C., He B., Zheng J., et al. Clinical characteristics and risk assessment of newborns born to mothers with COVID-19. J Clin Virol. 2020;127 doi: 10.1016/j.jcv.2020.104356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mantovani A., Rinaldi E., Zusi C., Beatrice G., Saccomani M.D., Dalbeni A. Coronavirus disease 2019 (COVID-19) in children and/or adolescents: a meta-analysis. Pediatr Res. 2020:1–6. doi: 10.1038/s41390-020-1015-2. [DOI] [PubMed] [Google Scholar]
- 28.Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z., et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145 doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 29.Duran P., Berman S., Niermeyer S., Jaenisch T., Forster T., Gomez Ponce de Leon R., et al. COVID-19 and newborn health: systematic review. Rev Panam Salud Publica. 2020;44:e54. doi: 10.26633/RPSP.2020.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ludvigsson J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109:1088–1095. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li B., Yang J., Zhao F., Zhi L., Wang X., Liu L., et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109:531–538. doi: 10.1007/s00392-020-01626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shelmerdine S.C., Lovrenski J., Caro-Dominguez P., Toso S., Collaborators of the European Society of Paediatric Radiology Cardiothoracic Imaging Taskforce Coronavirus disease 2019 (COVID-19) in children: a systematic review of imaging findings. Pediatr Radiol. 2020;50:1217–1230. doi: 10.1007/s00247-020-04726-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Balasubramanian S., Rao N.M., Goenka A., Roderick M., Ramanan A.V. Coronavirus disease 2019 (COVID-19) in children-what we know so far and what we do not. Indian Pediatr. 2020;57:435–442. doi: 10.1007/s13312-020-1819-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dhochak N., Singhal T., Kabra S., Lodha R. Pathophysiology of COVID-19: why children fare better than adults? Indian J Pediatr. 2020;87:537–546. doi: 10.1007/s12098-020-03322-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patel A.B., Verma A. Nasal ACE2 levels and COVID-19 in children. JAMA. 2020;323:2386–2387. doi: 10.1001/jama.2020.8946. [DOI] [PubMed] [Google Scholar]
- 36.Netea M.G., Dominguez-Andres J., Barreiro L.B., Chavakis T., Divangahi M., Fuchs E., et al. Defining trained immunity and its role in health and disease. Nat Rev Immunol. 2020;20:375–388. doi: 10.1038/s41577-020-0285-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miller A., Reandelar M.J., Fasciglione K., Roumenova V., Li Y., Otazu G.H. Correlation between universal BCG vaccination policy and reduced morbidity and mortality for COVID-19: an epidemiological study. MedRxiv. 2020 [Google Scholar]
- 38.Caruso C., Buffa S., Candore G., Colonna-Romano G., Dunn-Walters D., Kipling D., et al. Mechanisms of immunosenescence. Immun Ageing. 2009;6:10. doi: 10.1186/1742-4933-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xie X., Chen J., Wang X., Zhang F., Liu Y. Age- and gender-related difference of ACE2 expression in rat lung. Life Sci. 2006;78:2166–2171. doi: 10.1016/j.lfs.2005.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Imai Y., Kuba K., Rao S., Huan Y., Guo F., Guan B., et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436:112–116. doi: 10.1038/nature03712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Diaz E., Rodriguez A., Martin-Loeches I., Lorente L., Del Mar Martin M., Pozo J.C., et al. Impact of obesity in patients infected with 2009 influenza A(H1N1) Chest. 2011;139:382–386. doi: 10.1378/chest.10-1160. [DOI] [PubMed] [Google Scholar]
- 42.Green W.D., Beck M.A. Obesity impairs the adaptive immune response to Influenza virus. Ann Am Thorac Soc. 2017;14:S406–S409. doi: 10.1513/AnnalsATS.201706-447AW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zachariah P., Johnson C.L., Halabi K.C., Ahn D., Sen A.I., Fischer A., et al. Epidemiology, clinical features, and disease severity in patients with coronavirus disease 2019 (COVID-19) in a children’s hospital in New York City, New York. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.2430. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bhatraju P.K., Ghassemieh B.J., Nichols M., Kim R., Jerome K.R., Nalla A.K., et al. COVID-19 in critically Ill patients in the Seattle region—case series. N Engl J Med. 2020;382:2012–2022. doi: 10.1056/NEJMoa2004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Caussy C., Wallet F., Laville M., Disse E. Obesity is associated with severe forms of COVID-19. Obesity (Silver Spring). 2020;28:1175. doi: 10.1002/oby.22842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu J., Li W., Shi X., Chen Z., Jiang B., Liu J., et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19) J Intern Med. 2020;288:128–138. doi: 10.1111/joim.13063. [DOI] [PubMed] [Google Scholar]
- 47.Simonnet A., Chetboun M., Poissy J., Raverdy V., Noulette J., Duhamel A., et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring). 2020;28:1195–1199. doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Busetto L., Bettini S., Fabris R., Serra R., Dal Pra C., Maffei P., et al. Obesity and COVID-19: an Italian snapshot. Obesity (Silver Spring). 2020 doi: 10.1002/oby.22918. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hajifathalian K., Kumar S., Newberry C., Shah S., Fortune B., Krisko T., et al. Obesity is associated with worse outcomes in COVID-19: analysis of early data from New York City. Obesity (Silver Spring). 2020 doi: 10.1002/oby.22923. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yates T., Razieh C., Zaccardi F., Davies M.J., Khunti K. Obesity and risk of COVID-19: analysis of UK biobank. Prim Care Diabetes. 2020 doi: 10.1016/j.pcd.2020.05.011. S1751-9918(20)30196-0. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Newland J.G., Bryant K.A. Children in the eye of the pandemic storm-lessons from New York City. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.2438. [DOI] [PubMed] [Google Scholar]
- 52.Fruhbeck G., Baker J.L., Busetto L., Dicker D., Goossens G.H., Halford J.C.G., et al. European Association for the study of obesity position statement on the Global COVID-19 pandemic. Obes Facts. 2020;13:292–296. doi: 10.1159/000508082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nogueira-de-Almeida C.A. We need to look at the comorbidities of obesity during childhood and adolescence. Biomed J Sci Tech Res. 2017;1:1931–1932. [Google Scholar]
- 54.Alwarawrah Y., Kiernan K., MacIver N.J. Changes in nutritional status impact immune cell metabolism and function. Front Immunol. 2018;9:1055. doi: 10.3389/fimmu.2018.01055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Heialy S.A., Hachim M., Senok A., Tayoun A.A., Hamoudi R., Alsheikh-Ali A., et al. Regulation of angiotensin converting enzyme 2 (ACE2) in obesity: implications for COVID-19. bioRxiv. 2020 doi: 10.1101/2020.04.17.046938. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang F., Xiong Y., Wei Y., Hu Y., Wang F., Li G., et al. Obesity predisposes to the risk of higher mortality in young COVID-19 patients. J Med Virol. 2020 doi: 10.1002/jmv.26039. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kass D.A., Duggal P., Cingolani O. Obesity could shift severe COVID-19 disease to younger ages. Lancet. 2020;395:1544–1545. doi: 10.1016/S0140-6736(20)31024-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zabarsky G., Beek C., Hagman E., Pierpont B., Caprio S., Weiss R. Impact of severe obesity on cardiovascular risk factors in youth. J Pediatr. 2018;192:105–114. doi: 10.1016/j.jpeds.2017.09.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nogueira-de-Almeida C.A., Pires L.A., dos Santos R.G. Comparação de indicadores de perfis glicêmico e lipídico entre crianças e adolescentes obesos egressos de serviço público ou privado da cidade de Ribeirão Preto (SP) Medicina (Ribeirao Preto Online). 2016;49:504–510. [Google Scholar]
- 60.Nogueira-de-Almeida C.A., de Mello E.D. Different criteria for the definition of insulin resistance and its relation with dyslipidemia in overweight and obese children and adolescents. Pediatr Gastroenterol Hepatol Nutr. 2018;21:59–67. doi: 10.5223/pghn.2018.21.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sattar N., McInnes I.B., McMurray J.J. Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation. 2020;142:4–6. doi: 10.1161/CIRCULATIONAHA.120.047659. [DOI] [PubMed] [Google Scholar]
- 62.Korakas E., Ikonomidis I., Kousathana F., Balampanis K., Kountouri A., Raptis A., et al. Obesity and COVID-19: immune and metabolic derangement as a possible link to adverse clinical outcomes. Am J Physiol Endocrinol Metab. 2020;319:E105–9. doi: 10.1152/ajpendo.00198.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bendor C.D., Bardugo A., Pinhas-Hamiel O., Afek A., Twig G. Cardiovascular morbidity, diabetes and cancer risk among children and adolescents with severe obesity. Cardiovasc Diabetol. 2020;19:79. doi: 10.1186/s12933-020-01052-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kochli S., Endes K., Bartenstein T., Usemann J., Schmidt-Trucksass A., Frey U., et al. Lung function, obesity and physical fitness in young children: the examin youth study. Respir Med. 2019;159 doi: 10.1016/j.rmed.2019.105813. [DOI] [PubMed] [Google Scholar]
- 65.Umbrello M., Fumagalli J., Pesenti A., Chiumello D. Pathophysiology and management of acute respiratory distress syndrome in obese patients. Semin Respir Crit Care Med. 2019;40:40–56. doi: 10.1055/s-0039-1685179. [DOI] [PubMed] [Google Scholar]
- 66.Fearnbach S.N., Johannsen N.M., Martin C.K., Katzmarzyk P.T., Beyl R.A., Hsia D.S., et al. A pilot study of cardiorespiratory fitness, adiposity, and cardiometabolic health in youth with overweight and obesity. Pediatr Exerc Sci. 2020;1:1–8. doi: 10.1123/pes.2019-0192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rychter A.M., Zawada A., Ratajczak A.E., Dobrowolska A., Krela-Kazmierczak I. Should patients with obesity be more afraid of COVID-19? Obes Rev. 2020;21:e13083. doi: 10.1111/obr.13083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.De A., Rastogi D. Association of pediatric obesity and asthma, pulmonary physiology, metabolic dysregulation, and atopy; and the role of weight management. Expert Rev Endocrinol Metab. 2019;14:335–349. doi: 10.1080/17446651.2019.1635007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Samuels J.D. Obesity phenotype is a predictor of COVID-19 disease susceptibility. Obesity (Silver Spring). 2020;28:1368. doi: 10.1002/oby.22866. [DOI] [PubMed] [Google Scholar]
- 70.Al-Ayed M., Alshaybari K., Alshehri D., Jamaan A., Nasser I., Alaamri H., et al. Obesity and childhood asthma in male schoolchildren in Saudi Arabia: is there a role for leptin, interleukin-4, interleukin-5, and interleukin-21? Ann Saudi Med. 2019;39:295–301. doi: 10.5144/0256-4947.2019.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Durbin C., Egan R., Gervasi K., Nadeau N., Neal E., Reich S., et al. The effects of obesity on pulmonary function in children. JAAPA. 2017;30:30–33. doi: 10.1097/01.JAA.0000522135.76069.ce. [DOI] [PubMed] [Google Scholar]
- 72.Mauad Filho F., Caixe S.H., Benedetia A.C., Garcia J., WdP Martins, Del Ciampo L.A., et al. Evaluation of echocardiography as a marker of cardiovascular risk in obese children and adolescents. Int J Clin Pediatr. 2014;3:72–78. [Google Scholar]
- 73.Kassir R. Risk of COVID-19 for patients with obesity. Obes Rev. 2020;21 doi: 10.1111/obr.13034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sommer A., Twig G. The impact of childhood and adolescent obesity on cardiovascular risk in adulthood: a systematic review. Curr Diab Rep. 2018;18:91. doi: 10.1007/s11892-018-1062-9. [DOI] [PubMed] [Google Scholar]
- 75.Garcia J., Benedeti A., Caixe S.H., Mauad F., Nogueira-de-Almeida C.A. Ultrasonographic evaluation of the common carotid intima-media complex in healthy and overweight/obese children. J Vasc Bras. 2019;18:e20190003. doi: 10.1590/1677-5449.190003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Al-Shorman A., Al-Domi H., Faqih A. Markers of subclinical atherosclerosis in schoolchildren with obesity and metabolic syndrome. Swiss Med Wkly. 2017;147 doi: 10.4414/smw.2017.14446. [DOI] [PubMed] [Google Scholar]
- 77.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S., et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Belancic A., Kresovic A., Racki V. Potential pathophysiological mechanisms leading to increased COVID-19 susceptibility and severity in obesity. Obes Med. 2020;19 doi: 10.1016/j.obmed.2020.100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kim J., Nam J.H. Insight into the relationship between obesity-induced low-level chronic inflammation and COVID-19 infection. Int J Obes (Lond). 2020;44:1541–1542. doi: 10.1038/s41366-020-0602-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wu H., Ballantyne C.M. Metabolic inflammation and insulin resistance in obesity. Circ Res. 2020;126:1549–1564. doi: 10.1161/CIRCRESAHA.119.315896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Luzi L., Radaelli M.G. Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol. 2020;57:759–764. doi: 10.1007/s00592-020-01522-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Marchandot B., Sattler L., Jesel L., Matsushita K., Schini-Kerth V., Grunebaum L., et al. COVID-19 related coagulopathy: a distinct entity? J Clin Med. 2020;9:1651. doi: 10.3390/jcm9061651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lavie C.J., Sanchis-Gomar F., Henry B.M., Lippi G. COVID-19 and obesity: links and risks. Expert Rev Endocrinol Metab. 2020;15:215–216. doi: 10.1080/17446651.2020.1767589. [DOI] [PubMed] [Google Scholar]
- 84.D’Agati V.D., Chagnac A., de Vries A.P., Levi M., Porrini E., Herman-Edelstein M., et al. Obesity-related glomerulopathy: clinical and pathologic characteristics and pathogenesis. Nat Rev Nephrol. 2016;12:453–471. doi: 10.1038/nrneph.2016.75. [DOI] [PubMed] [Google Scholar]
- 85.Kelly C., Geraghty R.M., Somani B.K. Nephrolithiasis in the obese patient. Curr Urol Rep. 2019;20:36. doi: 10.1007/s11934-019-0898-0. [DOI] [PubMed] [Google Scholar]
- 86.Gai Z., Wang T., Visentin M., Kullak-Ublick G.A., Fu X., Wang Z. Lipid accumulation and chronic kidney disease. Nutrients. 2019;11:722. doi: 10.3390/nu11040722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yang S., Cao C., Deng T., Zhou Z. Obesity-related glomerulopathy: a latent change in obesity requiring more attention. Kidney Blood Press Res. 2020;4:1–13. doi: 10.1159/000507784. [DOI] [PubMed] [Google Scholar]
- 88.Vaneckova I., Hojna S., Kadlecova M., Vernerova Z., Kopkan L., Cervenka L., et al. Renoprotective effects of ET(A) receptor antagonists therapy in experimental non-diabetic chronic kidney disease: is there still hope for the future? Physiol Res. 2018;67:S55–67. doi: 10.33549/physiolres.933898. [DOI] [PubMed] [Google Scholar]
- 89.Gabarre P., Dumas G., Dupont T., Darmon M., Azoulay E., Zafrani L. Acute kidney injury in critically ill patients with COVID-19. Intensive Care Med. 2020;46:1339–1348. doi: 10.1007/s00134-020-06153-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Alexandre J., Cracowski J.L., Richard V., Bouhanick B. Drugs, COVID-19’ working group of the French Society of Pharmacology, Therapeutics. Renin-angiotensin-aldosterone system and COVID-19 infection. Ann Endocrinol (Paris). 2020;81:63–67. doi: 10.1016/j.ando.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Martinez-Rojas M.A., Vega-Vega O., Bobadilla N.A. Is the kidney a target of SARS-CoV-2? Am J Physiol Renal Physiol. 2020;318:F1454–62. doi: 10.1152/ajprenal.00160.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Adapa S., Chenna A., Balla M., Merugu G.P., Koduri N.M., Daggubati S.R., et al. COVID-19 pandemic causing acute kidney injury and impact on patients with chronic kidney disease and renal transplantation. J Clin Med Res. 2020;12:352–361. doi: 10.14740/jocmr4200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Abenavoli L., Scarpellini E., Colica C., Boccuto L., Salehi B., Sharifi-Rad J., et al. Gut microbiota and obesity: a role for probiotics. Nutrients. 2019;11:2690. doi: 10.3390/nu11112690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Indiani C., Rizzardi K.F., Castelo P.M., Ferraz L.F.C., Darrieux M., Parisotto T.M. Childhood obesity and firmicutes/bacteroidetes ratio in the gut microbiota: a systematic review. Child Obes. 2018;14:501–509. doi: 10.1089/chi.2018.0040. [DOI] [PubMed] [Google Scholar]
- 95.Xu K., Cai H., Shen Y., Ni Q., Chen Y., Hu S., et al. Management of COVID-19: the Zhejiang experience. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2020;49:147–157. doi: 10.3785/j.issn.1008-9292.2020.02.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kelishadi R., Roufarshbaf M., Soheili S., Payghambarzadeh F., Masjedi M. Association of childhood obesity and the immune system: a systematic review of reviews. Child Obes. 2017;13:332–346. doi: 10.1089/chi.2016.0176. [DOI] [PubMed] [Google Scholar]
- 97.Magrone T., Jirillo E. Childhood obesity: immune response and nutritional approaches. Front Immunol. 2015;6:76. doi: 10.3389/fimmu.2015.00076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rogero M.M. In: Biodisponibilidade de nutrientes. Cozzolino S.M.F., editor. Manole; Barueri, SP: 2016. Nutrição e sistema imune; pp. 991–1021. [Google Scholar]
- 99.Zhang L., Liu Y. Potential interventions for novel coronavirus in China: a systematic review. J Med Virol. 2020;92:479–490. doi: 10.1002/jmv.25707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.López Plaza B., Bermejo López L.M. Nutrición y trastornos del sistema inmune. Nutrición hospitalaria. 2017;34:68–71. doi: 10.20960/nh.1575. [DOI] [PubMed] [Google Scholar]
- 101.Cigerli O., Parildar H., Dogruk Unal A., Tarcin O., Kut A., Eroglu H., et al. Vitamin deficiency and insulin resistance in nondiabetic obese patients. Acta Endocrinol (Buchar). 2016;12:319–327. doi: 10.4183/aeb.2016.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dura-Trave T., Gallinas-Victoriano F., Chueca-Guindulain M.J., Berrade-Zubiri S. Prevalence of hypovitaminosis D and associated factors in obese Spanish children. Nutr Diabetes. 2017;7:e248. doi: 10.1038/nutd.2016.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Carter S.J., Baranauskas M.N., Fly A.D. Considerations for obesity, vitamin D, and physical activity amid the COVID-19 pandemic. Obesity (Silver Spring). 2020;28:1176–1177. doi: 10.1002/oby.22838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sadeghi K., Wessner B., Laggner U., Ploder M., Tamandl D., Friedl J., et al. Vitamin D3 down-regulates monocyte TLR expression and triggers hyporesponsiveness to pathogen-associated molecular patterns. Eur J Immunol. 2006;36:361–370. doi: 10.1002/eji.200425995. [DOI] [PubMed] [Google Scholar]
- 105.Grant W.B., Lahore H., McDonnell S.L., Baggerly C.A., French C.B., Aliano J.L., et al. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020;12:988. doi: 10.3390/nu12040988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wojcik M., Janus D., Kalicka-Kasperczyk A., Sztefko K., Starzyk J.B. The potential impact of the hypovitaminosis D on metabolic complications in obese adolescents– preliminary results. Ann Agric Environ Med. 2017;24:636–639. doi: 10.5604/12321966.1230676. [DOI] [PubMed] [Google Scholar]
- 107.Calder P.C. Dietary modification of inflammation with lipids. Proc Nutr Soc. 2002;61:345–358. doi: 10.1079/pns2002166. [DOI] [PubMed] [Google Scholar]
- 108.Simopoulos A.P. The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomed Pharmacother. 2002;56:365–379. doi: 10.1016/s0753-3322(02)00253-6. [DOI] [PubMed] [Google Scholar]
- 109.Takeuchi H., Ikeuchi S., Kawaguchi Y., Kitagawa Y., Isobe Y., Kubochi K., et al. Clinical significance of perioperative immunonutrition for patients with esophageal cancer. World J Surg. 2007;31:2160–2167. doi: 10.1007/s00268-007-9219-8. [DOI] [PubMed] [Google Scholar]
- 110.Simopoulos A. An increase in the omega-6/omega-3 fatty acid ratio increases the risk for obesity. Nutrients. 2016;8:128. doi: 10.3390/nu8030128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Silva Figueiredo P., Carla Inada A., Marcelino G., Maiara Lopes Cardozo C., de Cassia Freitas K., de Cassia Avellaneda Guimaraes R., et al. Fatty acids consumption: the role metabolic aspects involved in obesity and its associated disorders. Nutrients. 2017;9 doi: 10.3390/nu9101158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Czerwonogrodzka-Senczyna A., Janusz M., Jeznach-Steinhagen A., Demkow U., Pyrzak B. Advances in Clinical Science. Springer; 2015. Nutrition and immune system in children with simple obesity; pp. 49–56. [DOI] [PubMed] [Google Scholar]
- 113.Vuholm S., Rantanen J.M., Teisen M.N., Stark K.D., Molgaard C., Christensen J.H., et al. Effects of oily fish intake on cardiometabolic markers in healthy 8- to 9-y-old children: the FiSK Junior randomized trial. Am J Clin Nutr. 2019;110:1296–1305. doi: 10.1093/ajcn/nqz233. [DOI] [PubMed] [Google Scholar]
- 114.Garipagaoglu M., Sahip Y., Budak N., Akdikmen O., Altan T., Baban M. Food types in the diet and the nutrient intake of obese and non-obese children. J Clin Res Pediatr Endocrinol. 2008;1:21–29. doi: 10.4008/jcrpe.v1i1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wu D., Lewis E.D., Pae M., Meydani S.N. Nutritional modulation of immune function: analysis of evidence, mechanisms, and clinical relevance. Front Immunol. 2018;9:3160. doi: 10.3389/fimmu.2018.03160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rizvi S., Raza S.T., Ahmed F., Ahmad A., Abbas S., Mahdi F. The role of vitamin E in human health and some diseases. Sultan Qaboos Univ Med J. 2014;14:e157–65. [PMC free article] [PubMed] [Google Scholar]
- 117.Huang Z., Liu Y., Qi G., Brand D., Zheng S.G. Role of vitamin A in the immune system. J Clin Med. 2018;7 doi: 10.3390/jcm7090258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Carr A.C., Maggini S. Vitamin C and immune function. Nutrients. 2017;9:1211. doi: 10.3390/nu9111211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Huijskens M.J., Walczak M., Koller N., Briede J.J., Senden-Gijsbers B.L., Schnijderberg M.C., et al. Technical advance: ascorbic acid induces development of double-positive T cells from human hematopoietic stem cells in the absence of stromal cells. J Leukoc Biol. 2014;96:1165–1175. doi: 10.1189/jlb.1TA0214-121RR. [DOI] [PubMed] [Google Scholar]
- 120.Gombart A.F., Pierre A., Maggini S. A review of micronutrients and the immune system-working in harmony to reduce the risk of infection. Nutrients. 2020;12:236. doi: 10.3390/nu12010236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Nead K.G., Halterman J.S., Kaczorowski J.M., Auinger P., Weitzman M. Overweight children and adolescents: a risk group for iron deficiency. Pediatrics. 2004;114:104–108. doi: 10.1542/peds.114.1.104. [DOI] [PubMed] [Google Scholar]
- 122.Shubham K., Anukiruthika T., Dutta S., Kashyap A.V., Moses J.A., Anandharamakrishnan C. Iron deficiency anemia: a comprehensive review on iron absorption, bioavailability and emerging food fortification approaches. Trends Food Sci Technol. 2020;99:58–75. [Google Scholar]
- 123.Sypes E.E., Parkin P.C., Birken C.S., Carsley S., MacArthur C., Maguire J.L., et al. Higher body mass index is associated with iron deficiency in children 1 to 3 years of age. J Pediatr. 2019;207:198–204. doi: 10.1016/j.jpeds.2018.11.035. [DOI] [PubMed] [Google Scholar]
- 124.Sal E., Yenicesu I., Celik N., Pasaoglu H., Celik B., Pasaoglu O.T., et al. Relationship between obesity and iron deficiency anemia: is there a role of hepcidin? Hematology. 2018;23:542–548. doi: 10.1080/10245332.2018.1423671. [DOI] [PubMed] [Google Scholar]
- 125.do Nascimento Marreiro D., Fisberg M., Cozzolino S.M. Zinc nutritional status and its relationships with hyperinsulinemia in obese children and adolescents. Biol Trace Elem Res. 2004;100:137–149. doi: 10.1385/bter:100:2:137. [DOI] [PubMed] [Google Scholar]
- 126.Sandoval D.A., Davis S.N. Leptin: metabolic control and regulation. J Diabetes Complications. 2003;17:108–113. doi: 10.1016/s1056-8727(02)00167-8. [DOI] [PubMed] [Google Scholar]
- 127.Powell S.R. The antioxidant properties of zinc. J Nutr. 2000;130:S1447–54. doi: 10.1093/jn/130.5.1447S. [DOI] [PubMed] [Google Scholar]
- 128.Sena K.C.Md, Pedrosa Ld F.C. Efeitos da suplementação com zinco sobre o crescimento, sistema imunológico e diabetes. Rev Nutr. 2005;18:251–259. [Google Scholar]
- 129.Woo Baidal J.A., Chang J., Hulse E., Turetsky R., Parkinson K., Rausch J.C. Zooming towards a telehealth solution for vulnerable children with obesity during COVID-19. Obesity (Silver Spring, Md). 2020;28:1184–1186. doi: 10.1002/oby.22860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Dooley D.G., Bandealy A., Tschudy M.M. Low-income children and coronavirus disease 2019 (COVID-19) in the US. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.2065. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 131.An R. Projecting the impact of the coronavirus disease-19 pandemic on childhood obesity in the United States: a microsimulation model. J Sport Health Sci. 2020;9:302–312. doi: 10.1016/j.jshs.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Pietrobelli A., Pecoraro L., Ferruzzi A., Heo M., Faith M., Zoller T., et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity (Silver Spring). 2020;28:1382–1385. doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Simpson R.J., Campbell J.P., Gleeson M., Krüger K., Nieman D.C., Pyne D.B., et al. Can exercise affect immune function to increase susceptibility to infection? Exerc Immunol Rev. 2020;26:8–22. [PubMed] [Google Scholar]
- 134.Turel O., Romashkin A., Morrison K.M. A model linking video gaming, sleep quality, sweet drinks consumption and obesity among children and youth. Clin Obes. 2017;7:191–198. doi: 10.1111/cob.12191. [DOI] [PubMed] [Google Scholar]
- 135.Kenney E.L., Gortmaker S.L. United States adolescents’ television, computer, videogame, smartphone, and tablet use: associations with sugary drinks, sleep, physical activity, and obesity. J Pediatr. 2017;182:144–149. doi: 10.1016/j.jpeds.2016.11.015. [DOI] [PubMed] [Google Scholar]
- 136.Felső R., Lohner S., Hollódy K., Erhardt É, Molnár D. Relationship between sleep duration and childhood obesity: systematic review including the potential underlying mechanisms. Nutr Metab Cardiovasc Dis. 2017;27:751–761. doi: 10.1016/j.numecd.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 137.Khedri M., Samei A., Fasihi-Ramandi M., Taheri R.A. The immunopathobiology of T cells in stress condition: a review. Cell Stress Chaperones. 2020;25:743–752. doi: 10.1007/s12192-020-01105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Abbas A.M., Fathy S.K., Fawzy A.T., Salem A.S., Shawky M.S. The mutual effects of COVID-19 and obesity. Obes Med. 2020;19 doi: 10.1016/j.obmed.2020.100250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Santoli J.M., Lindley M.C., DeSilva M.B., Kharbanda E.O., Daley M.F., Galloway L., et al. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration – United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:591–593. doi: 10.15585/mmwr.mm6919e2. [DOI] [PubMed] [Google Scholar]
- 140.Takemoto M.L., Menezes M.O., Andreucci C.B., Nakamura-Pereira M., Amorim M.M., Katz L., et al. The tragedy of COVID-19 in Brazil: 124 maternal deaths and counting. Int J Gynaecol Obstet. 2020;151:154–156. doi: 10.1002/ijgo.13300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Anderson C.E., Whaley S.E., Crespi C.M., Wang M.C., Chaparro M.P. Every month matters: longitudinal associations between exclusive breastfeeding duration, child growth and obesity among WIC-participating children. J Epidemiol Community Health. 2020;74:785–791. doi: 10.1136/jech-2019-213574. [DOI] [PubMed] [Google Scholar]
- 142.Rasmussen S.A., Thompson L.A. Coronavirus disease 2019 and children: what pediatric health care clinicians need to know. JAMA Pediatr. 2020;174:743–744. doi: 10.1001/jamapediatrics.2020.1224. [DOI] [PubMed] [Google Scholar]
- 143.Yazdanpanah F., Hamblin M.R., Rezaei N. The immune system and COVID-19: Friend or foe? Life Sci. 2020;256 doi: 10.1016/j.lfs.2020.117900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Das L.T., Abramson E.L., Kaushal R., editors. Reopening US schools in the era of COVID-19: practical guidance from other nations. JAMA Health Forum. American Medical Association; 2020. [DOI] [PubMed] [Google Scholar]
- 145.Riphagen S., Gomez X., Gonzalez-Martinez C., Wilkinson N., Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395:1607–1608. doi: 10.1016/S0140-6736(20)31094-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Whittaker E., Bamford A., Kenny J., Kaforou M., Jones C.E., Shah P., et al. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. JAMA. 2020;324:259–269. doi: 10.1001/jama.2020.10369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Fuenzalida L., Garcia-Diaz D.F. Obesity as a risk factor for complications during acute respiratory infections in children. Rev Med Chil. 2016;144:1177–1184. doi: 10.4067/S0034-98872016000900012. [DOI] [PubMed] [Google Scholar]
- 148.Donoso A., Córdova P., Hevia Juricic Md P., Arriagada D. The obese child in the intensive care unit. Arch Argent Pediatr. 2016;114:258–666. doi: 10.5546/aap.2016.eng.258. [DOI] [PubMed] [Google Scholar]
- 149.Ewens B., Kemp V., Towel-Barnard A., Whitehead L. What evidence informs the nursing care of people with class iii obesity in an acute care setting? A scoping review. 2020. Res Square. 2020 doi: 10.21203/rs.3.rs-31488/v1. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Oosterhoff B., Palmer C.A. Attitudes and psychological factors associated with news monitoring, social distancing, disinfecting, and hoarding behaviors among US adolescents during the coronavirus disease 2019 pandemic. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1876. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]