Abstract
Objective
To assess the National Institute of Child Health and Human Development’s (NICHD) Pediatric Critical Care Trauma Scientist Development (PCCTSDP) national K12 program.
Design
Mixed-methods study.
Setting
PCCTSDP participants from 2005 to 2018.
Subjects
Past participants in the PCCTSDP, including those who received funding (scholars), those who did not receive funding (applicants), and those who participated as diversity fellows.
Interventions
None
Measurements and Main Results
34 past scholars, participants and fellows in the PCCTSDP were interviewed, including 19 (56%) women and 15 (44%) men via Skype. Interviews were audio recorded and transcribed, with permission. Codes were developed, using qualitative methods, that included: Community Building and Mentorship; Career and Research Development; and Tensions and Growth Opportunities. Quantitative data about physician-scholar grant success was retrieved from the National Institutes of Health (NIH) RePORTER system, physician-scholar curriculum vitae, and university websites. Since inception of the program, 46 scholars have been appointed. Scholars are equally split between women and men. Four (9%) members of the total cohort are from under-represented minority groups in medicine. Among the total past 46 past participants, 72% of those who completed the K12 achieved an NIH K-award and 36% of those not on K-level funding achieved at least one Research Program Grant-level award. All scholars, except one, remain academically active, as noted by recent publications in the peer reviewed literature; scholars from 2005–2013 are progressing in their careers, with 60% promoted to associate or full professor.
Conclusions
The PCCTSDP is reaching its programmatic goals of building a community of scientists in pediatric critical care and trauma surgery as shown by the qualitative analysis. Key challenges include increasing the diversity of applicants, encouraging applicants who are not funded, increasing the rate of K- to R- conversion, and preserving NICHD priorities for national K12 programs and individual K-awards.
Keywords: physician-scientist, career development, mentorship, junior faculty
Introduction
Challenges facing physicians and surgeons to initiate and sustain a research career are well-documented.(1, 2) Barriers include economic pressures on academic medical centers for higher clinical productivity; an increasingly competitive funding environment; and generational changes in career goals and expectations.(3, 4) Physicians in clinically intensive fields such as pediatric critical care and trauma surgery face additional barriers including remaining procedurally competent, in-house call requirements, and limited numbers of senior and peer role models.(5–7)
Program Description
The Pediatric Critical Care and Trauma Scientist Development (PCCTSDP) national K12 program was established by the Eunice Kennedy Shriver National Institute of Health and Human Development (NICHD) to provide early support to pediatric critical care physicians pursuing a career in basic, translational, or clinical research. In 2013, pediatric trauma surgeons were added because the two groups face similar barriers to research success. Recognizing that physicians bring important insights to the research needs of critically ill and injured children, the PCCTSDP develops a cadre of pediatric critical care and trauma surgeon scientists capable of sustaining careers in research.
The PCCTSDP is a national K12 program that draws applicants from across the country. PCCTSDP scholars participate in the program for five years: Phase I provides two years of funding, requiring 75% protected time for research and career development. For the three-year Phase II, scholars’ departments commit to at least 50% protected research time if the scholar has not achieved additional funding. The programs’ goals are to enhance the K12 scholars’ chance of success through the development of a community of physician-scientists, mentoring and didactics, and to create a cadre of physician-scientists who will exert a sustained influence on the field. These activities occur at an annual three-day retreat attended by current K12 scholars and applicants. Another goal is to increase the racial and ethnic diversity of those entering research by inviting diverse trainees to attend the retreat as Diversity Fellows.
Mentoring for scholar, applicant, and fellow participants is provided by the National Advisory Committee (NAC) that is composed of nationally recognized pediatric critical care physicians and trauma surgeons. NAC members are chosen among professors of pediatric critical care or trauma surgery, with a history of funded research, and/or as liaisons to societies important to the fields. NAC members have expertise across the research spectrum from laboratory-based mechanistic and translational research, to clinical and outcomes research. The NAC provides mentoring through formal feedback of PCCTSDP scholars’ scientific presentations at the retreat; annual site visits to the scholars’ home institution to assure that scholars’ research is on-track and that scholars’ departments are providing the committed support; and, career advice. The NAC serves as the study section for the K12 applications, following standard study section procedures, but additionally meets with each applicant to discuss their research and career progress. Senior program faculty provide mentoring prior to the retreat for potential applicants including discussing readiness to apply for a K12, reviewing specific aims, and helping to find scientific mentors when needed. At the retreat, didactics from senior program faculty include a full day session on scientific presentation skills, sessions promoting leadership and grant skills, and meetings with NIH project officers.
Applicants meet individually with members from the NAC to present their science and research trajectories. Didactics for applicants and diversity fellows include sessions on how the NIH works, a question and answer session with NIH project officers, writing clear specific aims, how to engage with mentors and approaches for time management. Diversity fellows additionally meet individually with the diversity officer.
The PCCTSDP has completed three five-year funding cycles. We therefore performed a mixed-methods program evaluation: a qualitative interview regarding aspects of the program’s value to participants; and a quantitative evaluation of PCCTSDP scholars’ funding records.
Methods
This project was deemed exempt by the University of Utah IRB. Qualitative interviews were conducted with three groups randomly chosen within 5-year funding cycle time periods (2005–2018) of past participants at the national K12 retreats: successful K12 applicants (scholars), unsuccessful applicants (applicants), and diversity fellows (fellows). We first attempted to contact all potential interview participants. Of 177 attempted contacts, we were unable to find working email addresses for 24 (13.5%), and received no response from 72 (40.7%). Of the 81 (45.7%) who responded, 73 (90.1%) agreed to an interview and interviewees were randomly selected from within this group. Interviews were conducted via Skype from questions developed by the investigators. Interviews were transcribed, with permission, and coded in Atlas.ti software. Coding was iterative to assure inter-coder reliability. Interviews and coding were performed by two members of the Qualitative Research Core at the University of Utah to assure no bias. Thematic saturation was reached with the 34 interviews. Themes were developed from the codes.
Quantitative data for PCCTSDP scholars were collected in three ways: First, NIH RePORTER was queried for Research Project Grants (RPG) awards. Second, because only principal investigators are listed in RePORTER, current Curriculum Vitae (CV) were solicited from scholars to identify roles as co-investigator or site principal investigator on National Institutes of Health (NIH) grants, non-NIH federal sources, such as the Centers for Disease Control and Department of Defense, and non-federal sources, such as the American Heart Association. Third, for scholars not sending their CV, institutional websites were searched to ascertain whether the scholars were still participating in research, as defined by publication of original articles or funding as co-investigator. Scholars who achieved independent funding from non-NIH sources were considered to have RPG equivalent funding. Applicant data come solely from NIH RePORTER.
Results
Qualitative findings
Interviewees included 16 scholars, 15 applicants, and 3 diversity fellows: nineteen (56%) women and 15 (44%) men. One interviewed diversity fellow became an applicant and then a PCCTSDP scholar. Broad themes developed in the qualitative analysis included: Community Building and Mentorship; Career and Research Development; and Tensions and Growth Opportunities. Figure 1 illustrates how community building through mentoring and peer mentoring may lead to growth, success with grants, and an improved career trajectory. Quotations associated with each theme are presented below.
Figure 1:
Model of themes noted in the qualitative interviews
Community Building
One major goal of the program was to create a community to help counter the problem of being the only researcher in largely clinical ICU or surgical programs. Interviewees commented that they enjoyed meeting new people at the retreat who were pursuing similar career goals, forming or building peer relationships and potential collaborations with other retreat attendees, and catching up with returning scholars.
“The shared comradery with the fellow participants was really, really helpful in making you feel that, one, this is possible and, two, that you’re not the only one struggling with this“ {Applicant}
[The retreat] was by far the best part of everything. Meeting your peers [who are] doing this work elsewhere. {Scholar}
I really think the value is the interactions you have with other individuals and those personal connections that are made, and how extensive that network actually is and the value of those interactions. {Scholar}
And it’s a nice community as people sort of progress through their careers and research careers, resources-wise. How did you approach submitting your next grant, who did you ask for advice, what program officers did you talk to, etc. So, it’s a nice built-in resource. {Scholar}
Mentorship
Interviewees appreciated the scope of support provided by the NAC and senior program faculty. This included feedback on scientific presentations (scholars), submitted national K12 grants (applicants), career advice, and availability of the faculty at and between retreats. A majority of scholars interviewed asked NAC members and program faculty for letters of support for promotions, new jobs, or as referees for K08/K23 applications.
In terms of the NAC, I would say one great benefit of them, again, is that they sort of orient me to what is expected of someone at my level in supporting me and making me feel like I’m doing okay in my progression in my career. And they’ve really been nothing but supportive. They definitely highlight things that I can work on and work towards, but never in a malicious way or negative way. It’s always just suggestions to help me to become better at what I’m doing. {Scholar}
I come from a small critical care training program, where there’s not a lot of academic mentorship and pursuing an academic track, applying for K08s. …. And it was also very helpful to have the mentorship and input of senior clinician scientists in pediatric critical care, of which there aren’t many in my institution {Applicant}
And so the mentorship that you get at the retreat is more sort of global and more focused to how to become a successful physician-scientist within pediatric critical care and less about your content area, which is nice because I think sometimes with your primary research mentor, you miss out on that aspect of mentoring because you’re so deep in the data, the research, that the sort of bigger picture mentorship might go by the wayside. {Scholar}
I mean, I’ve written to people who were on the committee even years after I finished asking them questions or asking them for letters or asking them for ideas, if they thought—to critically review my grant or things like that. {Scholar}
Peer mentorship was noted as another important program strength. Scholars felt a sense of comradeship with others in their cohort. Applicants appreciated meeting others working toward the same goals.
I think the connections I made with other young investigators, really hearing how other people approach their projects I think at that stage of my career was fairly helpful. So I think more, I feel like I gained more from the peer interactions than I did from the reviewers. {Applicant}
The second part that I found most helpful was just the ability to meet with others who are at the same that you are in terms of your training and academic success, because we’re very isolated at our institutions unless you’re a big research centers like Cincinnati or CHOP. You often as a K-awardee are the only person within your division who is federally-funded at the K level. And so, it can feel very isolating. {Scholar}
I’ve had a lot of great mentorship at the junior level with scholars that are one to four years ahead of me in the program. They’ve been really of great benefit in, at least, maybe not even coming up with real problem-solving strategies, but just sort of emotional support in what we do. That’s the thing I value most about that meeting. {Scholar}
Career and Research Development
The program focuses on helping scholars and applicants understand the grant process, typical career trajectories for physician-scientists, skills to navigate their career, and to be resilient to setbacks encountered for most scientists pursuing grant-funded research. Interviewees commented on encouragement, grants, and growth and tensions from the program.
Encouragement
Most interviewees, including all three diversity fellows, felt that the program encouraged them to stay in research.
The program allows fellows to sit in on something that is that intense and give them an exhibition to what their potential future could be and give them the opportunity then to talk to people who are doing something similar to what they want to do or who are following that career path that they want to as well. So, it’s just the mentality behind having diversity fellow involvement, I think—because without it, then I wouldn’t have been able to go or even have known that such a thing existed. {Diversity fellow}
… allowing diversity fellows to go and be part of—more part of the process of listening in and meeting people that are doing things that they would potentially want to do in the future and not being put on the spot necessarily to have to engage in the same way, but understanding that this is a path that they will possibly have to take if they are going to apply for something that’s similar. So, that opportunity for me was the best part, being equal. I don’t know of any other program that would even allow that at all. {Diversity fellow}
… it was also encouraging to see surgeons on the mentoring committee that had been very successful and I have been able to foster relationships with some of them…. I think the whole retreat was very much encouraging. The feedback was very positive, especially the critical feedback. {Applicant}
Grants
A benefit of the K12 program is one-on-one and group meetings with program officers and demystification of the NIH as well as receiving detailed reviews and advice on applications. Applicants are encouraged to discuss reviews with their home institution mentors. Most applicants felt that critiques of their K12 grant were helpful, as was career advice received during and after the annual retreat.
And that may even be something else that I’ve kind of pulled out of the retreat just from having the opportunity to meet program officers and get that inside look to the NIH. Really that even though they were from different institutes that year, it just kind of demystified the process a little bit. {Scholar}
So, the retreat gave me really, really good comments on my grant and how to improve it…..And a lot of it was reworking the grant and reapplying. It changed my mentorship. It changed my approach, It changed the percent effort that came from my senior leadership. It was very useful in keeping me sort of focused on what the next steps were. (Applicant)
So, the critique that I got for my grant, I brought it back home sort of to my mentors and presented it at K-club here. And people here like added on from other things…And then I used that resubmit my grant…to the AHRQ for a K08 award, incorporating all of the comments of the reviewers. (Diversity fellow, applicant)
Career Trajectory
{The program} sort of forced me to a) codify what my short and long term goals would be and—and sort of look at both from a research perspective but also from a career development perspective what I needed to do or what the options were. (Applicant)
… I think as opposed to just submitting a grant and then maybe getting some written feedback, the ability to go there and interact with people who are doing similar things as me, but also then the senior leaders in the field of pediatric critical care, um, to kind of get to know them a little bit and to get their feedback, I think is really, um, helpful for my clinical—well for my research career from a, like, a grant writing standpoint, but also from a just overall career-planning standpoint. (Applicant)
… even though this was many years ago, I’ve maintained contact with many of the scholars that I met through the retreat and meetings, and that has been extremely helpful for career changes, advice, letters for promotions, yeah. {Scholar}
Tensions and Growth Opportunities
Interviewees expressed some tensions in the program that many used as growth opportunities. Tensions included exposure to different types of research than their own and, for applicants, difficulties of not getting funded and thus not having access to the community of K12 scholars.
I think the—one of the downsides to that is, I felt a little bit of a fish out of water … because there were more people with basic science background than I had. And that was as a health services researcher. {Scholar}
…having a better understanding for what a pediatric intensivist has for protected time really opened my eyes and has set a new expectation for me in terms of what I should be getting for protected time…. my only experience was working with surgeons and my understanding of what “protected time” was really only within the frame of reference of seeing my mentors who are surgeons operate within the constraints of their protected time. But, you know, working with scholars of other medical disciplines and see, you know, how much more time they have to dedicate to their own research and writing really opened my eyes a lot. {Applicant}
I think once you’re not in that network, which is absolutely understandable, then, you know, then you’re not a part of that community. And so, if there was a way to improve, I think with recognizing that there can’t be an equal investment in those people, but developing an opportunity for that continued collaboration, I think is valuable. {Applicant}
…And whether it’s not really your area of expertise, cross-over, you’re getting exposed to what people are doing in pediatric critical care and surgical critical care, trauma surgery across the country. And it can really foster new ideas, cross-over ideas. I think it really can help that you think about other aspects that you can bring to your own research. {Scholar}
Quantitative findings
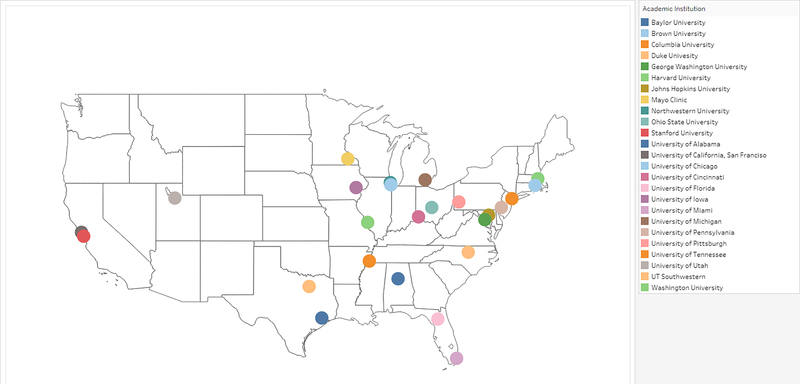
Since inception, 46 PCCTSDP scholars are evenly divided between women and men. Four (8%) are members of groups under-represented in medicine. (8) Two scholars withdrew from the program before completing five years of training, due either to personal circumstances or career plan changes. All scholars hold MDs, and 7 (15%) have MD/PhD training. The program appointed its first surgeon-scholar in 2018. Currently, all scholars (98%), except one, remain in academic medicine. Scholars represent 25 distinct training programs as shown in Figure 2. Two programs had high representation, with six (13%) and four (9%) scholars. There have been 108 unique applicants and 32 diversity fellows who did not become scholars. Two diversity fellows returned as applicants and became scholars. The PCCTSDP has funded research along the T0 through T4 spectrum, including 34 (74%) laboratory-based science and 12 (26%) non-laboratory science projects, including: engineering, epidemiology/outcomes, pharmacology, clinical, ethics, health services and communications. K12 scholars are advancing in their careers, with 60% of those in the first two cohorts (29 scholars who completed the K12) currently promoted to associate (15) or full professor (2); one has an endowed research chair; one is an Institute Director.
Figure 2:
Map displaying the diversity of PCCTSDP scholars’ institutions
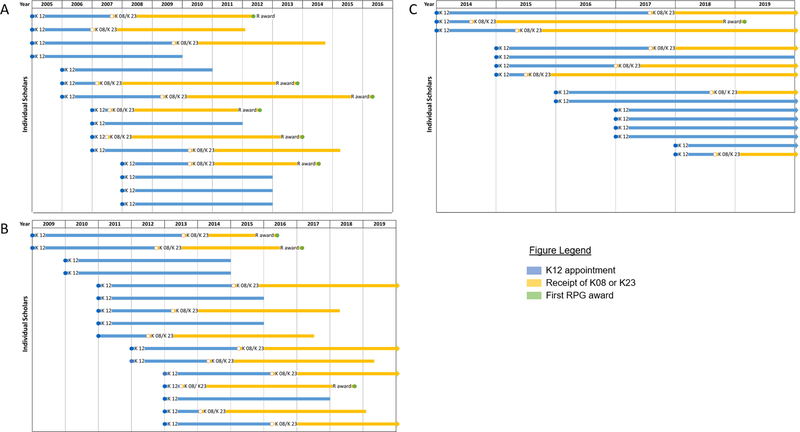
Funding success
Since program inception through January 2019, >60% (29/46) of scholars received a K08/K23, divided evenly between women and men. See Figure 3. This percentage increases to 72% when those still in the national K12 program are removed from the denominator. Approximately 22% (10/46) of all scholars have received at least one RPG level award as principal investigator. This percentage increases to (10/28) 36% when excluding scholars currently funded on K-awards or those still in the K12 program. Ten of the 16 scholars (62.5%) who completed a K08 or K23 received RPG-level funding. Figure 3. Applicants also have had success. Over the same time period, 25/108 (23%) applicants received a K08/K23 and 9/108 (8%) have received at least one RPG level award from the NIH, as reported in NIH RePORTER.
Figure 3:
Time from appointment as a PCCTSDP K12 scholar to future funding for three cohorts of scholars: (A) 2004–2008 (B) 2009–2013 (C) 2014–2018
Discussion
The PCCTSDP is fulfilling its major programmatic goal of creating a community of pediatric critical care and trauma surgeon physician-scientists who will have sustained influence in their fields. Community building accompanied by mentorship are key components of the PCCTSDP. Results of a survey to pediatric critical care and neonatology trainees and faculty identified limitations of mentorship, number of role models, and protected time, and current NIH funding lines, as major challenges to initiating and sustaining a research career.(5) Creating a community of researchers in pediatric critical care and trauma surgery helps to overcome these challenges by giving participants a network beyond their home institutions. PCCTSDP program success in creating a community and is reflected in our qualitative themes. This is especially important for scholars and applicants from smaller institutions that may have few funded investigators on the faculty in pediatric critical care or trauma surgery.(9) Unfortunately, we frequently cannot fund all meritorious applications. Unsuccessful applicants are encouraged to discuss their written grant reviews with their mentors and to reapply to the PCCTSDP or to apply directly to the NIH for a K08/K23. Our inability to fund all meritorious applications diminishes our ability to broaden the PCCTSDP community. The desire to remain within the community is noted in the qualitative comments; however, additional resources would be required to sustain outreach efforts to this larger group.
Mentoring is an important component of the PCCTSDP and this strength was noted in the qualitative themes. Both the NAC and senior program faculty provide mentoring and role models of successful senior physician- and surgeon-scientists who enjoy engaging with K12 scholars, applicants, and fellows, and investing in those individuals’ success. Over the past 15 year, the scientific expertise of our NAC has evolved reflecting trends in pediatric critical care and trauma research. Newer NAC members, added as original members have stepped down, continue our strengths in laboratory-based science expertise and have added strengths in non-laboratory-based research and methods such as clinical trials, clinical research, qualitative research and outcomes research reflective of the types of applications received by the program. This breadth of research expertise enables both career and scientific mentoring of our scholars.
The PCCTSDP provides protected time for scholars through the two-year provision of funding and by commitment from departments to continue scholars’ protected time, if they are not immediately successful with their next award. K12 scholars are positioned to exert a sustained influence on research in their fields with the earliest cohorts gaining promotions at their academic institutions and with a 36% R-level funding success rate, similar to that reported recently for all K-awardees.(10) Additionally, PCCTSDP scholars who have completed K08 or K23 awards have similar levels of funding to other junior faculty who have both K12 and K08/K23 support reported nationally (62.5% to 61.5%). (11)
National K12 programs face challenges. One challenge is shifting priority at the NICHD to de-emphasize national K12 programs to instead emphasize and increase the funding for individual K08s/K23s.(11) An important point to make, shown in the supplemental material for that report and our study, is that scholars who participate in both national K12s and individual K08s/K23s receive more grant awards than recipients of either mechanism alone. (11) Other challenges are increasing the conversion of K- to R- level awards; how to encourage excellent applicants who do not receive K12 funding; and how to increase the pool of diverse applicants to such programs. In spite of these challenges, the PCCTSDP is achieving its programmatic goals of building a community of pediatric critical care and trauma surgery scholars that fosters the careers of young physician scientists. Our former scholars are progressing in their careers and are poised to have a sustained influence on the field.
Acknowledgements
We are grateful for the support of the Program Officials of the Pediatric Trauma and Critical Illness Branch of the NICHD for their support of the PCCTSDP, Robert Tamburro, MD and Tammara Jenkins, RN. We also would like to acknowledge the University of Utah qualitative research Core including its Director, Dr. Susan Zickmund, and Ms. Stacey Slager, Ms. Bom Choi, and Ms. Alex Bellinger who performed the interviews and qualitative coding.
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development national K12 HD047349
Footnotes
Copyright form disclosure: Drs. Keenan and Dean’s institution received funding from National Institutes of Health (NIH), Eunice Kennedy Shriver National Institute of Child Health and Human Development. Drs. Keenan and Albertine’s institution received funding from the NIH. Dr. Keenan’s institution received funding from the Centers for Disease Control and Prevention, and she received funding from University of Utah. Drs. Keenan, Albertine, and Dean received support for article research from the NIH. Dr. Albertine’s institution received funding from Shire Pharmaceuticals and United Therapeutics/Boston Children’s Hospital, and he received funding from the American Association for Anatomy (Editor-in-Chief of the Anatomical Record). Dr. Upperman disclosed that he does not have any potential conflicts of interest.
This work was performed at the University of Utah School of Medicine
No reprints requested
References
- 1.Garrison HH, Deschamps AM. NIH research funding and early career physician scientists: continuing challenges in the 21st century. FASEB Journal 2014;28(3):1049–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salata RA, Geraci MW, Rockey DC, Blanchard M, Brown NJ, Cardinal LJ, Garcia M, Madaio MP, Marsh JD, Todd RF, 3rd. U.S. Physician-Scientist Workforce in the 21st Century: Recommendations to Attract and Sustain the Pipeline. Acad Med 2018;93(4):565–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alvira CM, Steinhorn RH, Balistreri WF, Fineman JR, Oishi PE, Padbury JF, Kinsella JP, Abman SH. Enhancing the Development and Retention of Physician-Scientists in Academic Pediatrics: Strategies for Success. J Pediatr 2018;200:277–284. [DOI] [PubMed] [Google Scholar]
- 4.Schafer AI. The vanishing physician-scientist? Transl Res. 2010;155(1):1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christou H, Dizon ML, Farrow KN, Jadcherla SR, Leeman KT, Maheshwari A, Rubin LP, Stansfield BK, Rowitch DH. Sustaining careers of physician-scientists in neonatology and pediatric critical care medicine: formulating supportive departmental policies. Pediatr Res 2016;80(5):635–640. [DOI] [PubMed] [Google Scholar]
- 6.Goldstein AM, Blair AB, Keswani SG, Gosain A, Morowitz M, Kuo JS, Levine M, Ahuja N, Hackam DJ, Basic Science Committee of the Society of University S. A Roadmap for Aspiring Surgeon-Scientists in Today’s Healthcare Environment. Ann Surg 2019;269(1):66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Markel TA, Valsangkar NP, Bell TM, Kiel BA, Zimmers TA, Koniaris LG. Endangered academia: preserving the pediatric surgeon scientist. J Pediatr Surg 2017;52(7):1079–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Association of American Medical Colleges. The status of the new AAMC definition of “underrepresented in medicine” following the Supreme Court’s decision in Grutter. 2004. [Available from: https://www.aamc.org/download/54278/data/urm.pdf.
- 9.Oishi PE, Klein OD, Keller RL, University of California San Francisco N, Pediatric Critical Care Early Faculty Development C. Developing physician-scientists in the fields of neonatology and pediatric critical care medicine: an effort to formulate a departmental policy. J Pediatr 2013;163(3):616–617 e1. [DOI] [PubMed] [Google Scholar]
- 10.Nikaj S, Lund PK. The Impact of Individual Mentored Career Development (K) Awards on the Research Trajectories of Early-Career Scientists. Acad Med 2019;94(5):708–714. [DOI] [PubMed] [Google Scholar]
- 11.Twombly DA, Glavin SL, Guimond J, Taymans S, Spong CY, Bianchi DW. Association of National Institute of Child Health and Human Development Career Development Awards With Subsequent Research Project Grant Funding. JAMA Pediatr 2018;172(3):226–231. [DOI] [PMC free article] [PubMed] [Google Scholar]