Abstract
Background
Data on COVID-19 in Liver Transplant (LT) recipients are scanty, but one can hypothesize that they are more susceptible to infection due to chronic immunosuppression. Telemedicine could be an alternative to the routine clinical care in this difficult period. We aimed to investigate in a cohort of LT recipients the access to remote consultation and the attitude towards Telemedicine using an internet-based survey.
Material and methods
We invited LT recipients from the Liver Transplant Follow-up Center of the University Hospital of Salerno to access remote consultation. A subgroup of them also participated in a self-administered, internet-based survey evaluating demographics; LT data and immunosuppressive therapy; comorbidities; attitudes towards COVID-19 infection; their perceptions of the need for health care, and their approach to telemedicine.
Results
Seventy-four/one hundred and fifty-three (48.3%) LT recipients were unable to access remote consultation. They showed a significantly higher mean age and a higher percentage of low school degree compared to those who accessed it (p = 0.03 and p = 0.001, respectively). Among the remaining LT recipients, 50/79 (63.3%) responded to the survey; mean time from liver transplantation was 12 ± 7 years; 94% of the sample reported at least one comorbidity; 44% of LT recipients declared to be “very much/much” worried because of COVID-19 infection, and 64% considered themselves more vulnerable than the general population. Forty percent of responders refused the routine follow-up visit, and 62% were very interested in using Telemedicine.
Conclusion
LT recipients were anxious because of COVID-19 infection and considered themselves more vulnerable than the general population, refusing the routine clinical visit. For continuing services during the COVID-19 era, new strategies are needed and telemedicine shows promise.
Keywords: Liver transplant, COVID-19; Internet-based survey, telemedicine
Introduction
The outbreak of the novel coronavirus Sars COV2 pandemic (COVID 19), first reported in China in December 2019, has rapidly become a global health emergency [1], [2]. On March 11th, 2020, the World Health Organization (WHO) characterized COVID-19 as a pandemic [1].
Although the lung is the primary organ involved in Sars COV2 infection, several studies have described gastrointestinal symptoms [3] and liver injury in patients with COVID-19 [4], [5].
It has been reported that 2–11% of patients with COVID-19 had liver comorbidities, and 14–53% of cases reported abnormal levels of aminotransferases [4]. High rates of liver dysfunction are present in up to 60% of patients suffering from severe acute respiratory syndrome (SARS). Liver injury could be linked not only to COVID-19 but also drug hepatotoxicity, immune-mediated inflammation [6] or pneumonia-associated hypoxia could contribute to liver damage [4].
Data about COVID-19 infection in liver transplant (LT) recipients are scanty, and COVID-19 is still a matter of concern. A recent report from an Italian group [7] described 3 cases from 111 long-term LT survivors, who died of severe respiratory distress syndrome. Nevertheless, the severity, mortality rate, and incidence of complications in these patients need to be examined in large-cohort clinical studies.
E-health interventions, including via smartphone and other e-health technologies, have seen enormous growth internationally over the past decade, changing the shape of health care and clinical research [8]. In the COVID-19 era, when both the WHO and all the governments recommend robust containment and control activities to reduce the spread of this virus, e-health technologies could gain great importance. Previous studies have described the telemedicine as the use of telecommunications solely to diagnose and treat patients, in different clinical settings to facilitate health care delivery at a distance [9], [10], allocated in the broad field of Telehealth which includes computer-assisted telecommunications to support management, surveillance, literature and access to medical knowledge. While Telehealth is rapidly becoming popular, in Italy there were only a few hospitals providing telemedicine by using appropriate patients’ consent, platforms, and also structured payments forms. However, during the COVID19 emergency, the Italian Governament passed a number of laws regulating the lockdown which included also the cancellation of regular outpatients visits and the passage to telemedicine as first choice.
The present paper aims to report the experience of our Liver Transplant Follow-up Center during the lockdown period in Campania, Italy (5,8 million inhabitants; 4.484 ascertained infections; 364 virus-related deaths as of May 3, 2020) [11], describing the results of the access to telemedicine of a cohort of LT recipients. Furthermore, we report the results of an internet-based survey aimed to investigate the LT patients' perspectives on the COVID-19 infection and their attitude towards telemedicine as an alternative to routine clinical care.
Methods
Telemedicine
Telemedicine was not officially in use or regulated in the Campania region, where the University Hospital of San Giovanni di Dio e Ruggi d'Aragona of Salerno is located. From the beginning of the COVID-19 epidemic in Italy (February 2020), the Gastroenterology outpatient Clinic of University Hospital of San Giovanni di Dio e Ruggi d'Aragona of Salerno has been fully operational only for emergencies. The medical staff of the Liver Transplant Follow-up Center have postponed from 12 to 17 routine outpatient follow-up visits per day. In the lack of a hospital Electronic Medical Records (EMR) that patients can have written and virtual visits through, the personnel of the clinic offered free access to remote consultation through phone calls, e-mail, Skype and Whatsapp messages.
Patients who were recently transplanted (<1 year) were excluded from remote consultations and were regularly followed according to the indication of the Liver Transplant Center. Patients with recent episodes of rejection were also excluded.
Survey questionnaire
A subgroup of LT patients completed a self-administered, internet-based questionnaire. The opening page of the survey provided information about the scope and purpose of the study, and the consent.
We invited LT recipients by sending a link to the internet-based questionnaire via Whatsapp or e-mail (Appendix A1). No incentives were provided for participation.
The questionnaire consisted of 25 items evaluating: demographic information; LT data and immunosuppressive therapy; comorbidities (diabetes mellitus, chronic renal disease; dyslipidemia, arterial hypertension, osteoporosis, depression, anxiety); sleep disturbances, fatigue; physical activity; adherence to the flu vaccination.
Attitudes towards COVID-19 infection were investigated using a five-point Likert scale ranging from 1 = not at all; 2 = a little; 3 = enough; 4 = much; 5= very much. In particular, we asked if LT recipients were worried about the COVID-19 infection; if they felt more susceptible to the infection than the general population; if they were worried about going to the hospital, or going in crowded places; if they were interested in vaccination against COVID-19. We also investigated their need for healthcare and their feelings about telemedicine.
Participants were also given the possibility to add comments at the end of the questionnaire. We calculated an average time of 15 min to complete it.
Statistical analysis
Categorical and continuous variables were expressed as frequency and Mean ± Standard Deviation (SD), respectively. Differences in rates were calculated using the χ2 test. The significance level was set below 0.05. The statistical program used was the Statistical Package for Social Sciences (SPSS) for Windows, version 12.0.
Results
Telemedicine
Telemedicine was not in use in our region before the COVID19 pandemic. Neverthless, since the adoption of the strict lockdown measures doctors and nurses organized the at-distance healthcare adapting the mean to the patients’ availability of telecommunication and ability to use the internet. We contacted 153 LT patients through active follow-up by telephone, inviting them to access remote consultation. Furthermore, we provided a simple explanation about the COVID-19 symptoms and two mobile phone numbers that patients could contact in case of suspected symptoms or just to have medical information. None of the contacted LT patients had a recent (<6 months) hospitalization.
From February 25 to April 25 (date of the current analysis) we performed an average of 15 phone calls to LT patients each day, with a mean of 2 remote consultations for each patient per month. We assessed the status of well-being and eventually evaluated the laboratory tests that patients had previously sent via fax, e-mail or Whatsapp. During the telephone consultation, the medical staff could triage the patients who referred clinical conditions that needed a physical examination and further investigations at the hospital clinic from those who could continue remote consultations. Following the remote consultation, we admitted four patients to the hospital. The reasons were: one patient for the onset of anemia that required intravenous iron therapy; one patient for jaundice, pruritus, and fever due to cholangitis; one for the exacerbation of chronic pancreatitis; one patient affected with erythrocytosis for increased haematocrit levels that required phlebotomy.
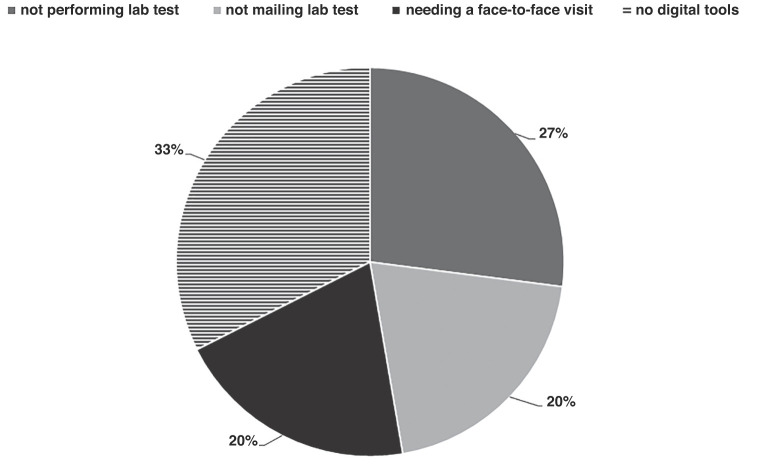
However, we were unable to achieve a good quality visit for 74 of them, due to their limited access to digital tools or because of inability to perform laboratory tests (Fig. 1 ). Table 1 showed the demographic characteristics and a selection of clinical data of patients who were able or not to access remote consultation. LT recipients who were unable to access remote consultation were significantly older and repored a higher percentage of low school degree compared to those who did access it (65.8 ± 8.7 vs 61.9 ± 12.1, p = 0.03 and 71% vs 32.5%, p = 0.001, Table 1).
Figure 1.
Reasons for which LT recipients could not attend remote consultation.
Table 1.
Demographic characteristics, cause and time from LT of LT recipients who were able or not to access remote consultation. In bold the relevant differencies among groups.
| LT recipients able to access remote consultation N = 79 | LT recipients unable to access remote consultation N = 74 | p | |
|---|---|---|---|
| Gender (M/F) | 54/25 | 51/23 | 0.9 |
| Age (years) | 61.9 ± 12.1 | 65.8 ± 8.7 | 0.03 |
| Low school degree (%) | 32.5 | 71 | 0.001 |
| Cause of LT | 0.6 | ||
| -hepatitis C-related cirrhosis | 45% | 41% | |
| -hepatitis B-related cirrhosis | 23% | 31% | |
| -autoimmune liver diseases | 6% | 4% | |
| -other | 26% | 24% | |
| Time from LT (years) | 14.7 ± 8.1 | 14.0 ± 7.8 | 0.7 |
| Rejection episodes from LT | 0.1 ± 0.4 | 0.2 ± 0.4 | 0.6 |
LT liver transplant. Data were expressed as % or M ± SD.
Fifteen of those not attending the remote consultation needed one or more face-to-face visits and laboratory tests for the onset of therapy side effects such as mouth sores and tremors due to increased serum levels of immunosuppressive drugs.
Twenty LT patients did not have the opportunity to access a laboratory outside the hospital for blood testing because of the social distancing that isolated them also from families and caregivers. Fifteen LT patients had laboratory tests but did not have the opportunity to see the results because they did not have the means to do that. However, none of those that could not access remote consultation reported any serious disease during the phone calls. None of the LT recipients were diagnosed with COVID-19 or in contact with a confirmed COVID-19 infection.
Survey questionnaire
We sent the link for the online survey to a subgroup of 79 LT recipients who previously gave their consent to participate in surveys and clinical studies. A total of 50 patients (63.3%) responded.
Table 1 showed the demographic characteristics of patients who participated to the survey compared to those who did not.
Among the responders, the level of compliance to immunosuppressive therapy was excellent for 58%, good in 34%, fair in 6% and poor in 2% of the sample. Fifty-eight percent of the sample did not report any physical activity.
Most of the participants (94%) reported at least one comorbidity: type 2 diabetes mellitus (36%), chronic kidney disease (15%); dyslipidemia (24%), arterial hypertension (28%), osteoporosis (12%), depression (4%), and anxiety (14%) in LT recipients. Sixteen/fifty (32%) LT patients referred sleep disturbances. The presence of sleep disturbances was significantly associated with depression (p = 0.036), anxiety (p = 0.001) and fatigue (p = 0.035).
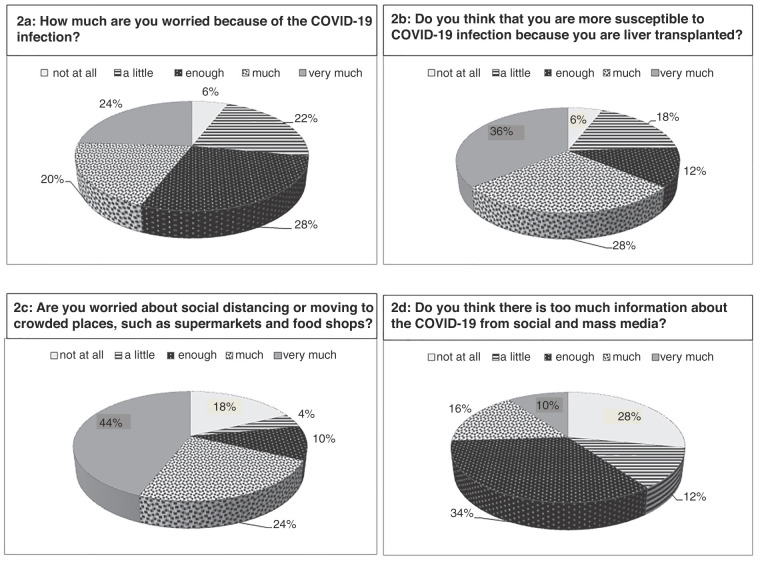
For the question "How much are you worried because of the COVID-19 infection?", the mean score on the 5-point Likert scale was 3.3 ± 1.2. As shown in Fig. 2 a, most of the LT patients were worried because of COVID-19; 36% of the sample answered "very much" and 28% 'much' at the question "Do you think that you are more susceptible to COVID-19 infection because of your liver transplant?" (Fig. 2b). A majority of the participants were worried about going to crowded places (answers much/very much: 68%) (Fig. 2c). On the other hand, 34/50 (68%) of LT patients were not concerned about a lack of food or mask stocks (16/50, 32%). Only a minority of the sample considered the information about COVID-19 to be excessive from social and mass media (Fig. 2d). Although 23/50 LT recipients (46%) had previously refused to adhere to flu vaccination, only 6 of them would refuse the vaccination against COVID 19 if it were available (p = 0.001).
Figure 2.
Attitudes towards COVID-19 infection in LT recipients.
Forty percent of the LT recipients refused the regular, clinic follow-up visit fearing the COVID-19 infection.
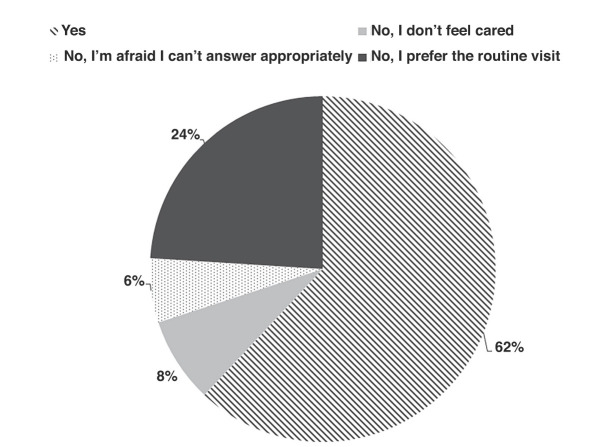
For the question: "Would you use a remote healthcare service (e-health technologies) to interact with your follow-up center, when there are no relevant health problems?" 31/50 (62%) LT recipients declared to be interested in being followed using telemedicine. Fig. 3 shows the percentage of patients who would accept remote healthcare service and the percentage of those who refused for different reasons.
Figure 3.
Percentage of answers to the question: "Would you use a remote healthcare service (e-health technologies) to interact with your follow-up center, when there are no relevant health problems?".
Discussion
The COVID-19 outbreak has been radically changing our routine healthcare. Because of the recent pandemic, the usual face-to-face interaction scheme was not possible [12], [13], [14]. In any case, an attempt was made to reach chronic patients, including LT patients, in follow-up by establishing a rudimentary but effective form of telemedicine which, with all its limitations, was certainly a support for them [15], [16]. However, only those accustomed to new digital technologies could take advantage of previous experience and stay in touch with their healthcare professionals. A significant part of our patients, mostly with a low education and over the age of 60, not born or raised in the digital age, did not have access to the network, to e-mails. Our report shows that 74/153 (48.3%) were not able to perform telemedicine visits. The percentage is not surprising as the Salerno province, South Italy, where the University Hospital is located, is a rural community. Almost half of LT recipients attending our Center were then unable to access the offered full remote consultation. However, from the beginning of the COVID-19 outbreak, each LT patient has received a mean of 2 phone consultations per month by our medical staff, which allowed us to select those who needed to access the outpatient clinic for further investigations or therapies.
As reported by our survey, LT patients were anxious because of COVID-19 infection, although the prevalence of COVID-19 infection in Campania was about 10 times lower than in the North of Italy [17]. They considered themselves more vulnerable than the general population, due to their condition of chronic immunosuppression and the presence of multiple comorbidities. Furthermore, they expressed concern about the routine follow-up visit at the hospital clinic for outpatients due to possible infection. Considering that WHO, scientific societies, and governments suggest social distancing and a containment strategy, especially in the presence of "frailty", it is of paramount importance to assess new plans for the follow-up of LT patients to ensure they receive the care services they require.
According to the WHO definition, "Telemedicine" is "the delivery of health care services at a distance using electronic means for "the diagnosis of treatment, and prevention of disease and injuries, research and evaluation, education of health care providers" [10], [18]. Previous studies have evaluated the application of telemedicine in the management of HCV infection in particular settings such as imprisoned patients or the rural population [10] or those with liver cirrhosis [9], [19] or patients referred for LT [20] to facilitate health care delivery at a distance. Other authors have also demonstrated that telemedicine could be a time and cost-saving alternative to clinic follow-up of LT patients [21].
Our attempt to turn the current COVID-19 crisis into an opportunity to introduce in our clinical practice telemedicine had a limited application. Notably, 48.3% of our LT patients were not able to access the remote consultation. We can speculate that the reason may be the older age and the lower school degree of some of our LT recipients. The consequences of the delay or missing healthcare are, at the moment, unknown.
As shown by the survey results, the remaining LT patients were very interested in this new clinical approach since they felt "in contact" with their follow-up LT Center even in the present challenging period. Although this on-line survey cannot be considered a Telemedicine instrument [10], it has revealed the healthcare needs and expectations of our LT population, allowing us to improve the quality of our clinical care during this challenging period.
However, despite the undoubted advantage of telemedicine in enhancing access to care and reducing costs, there are some barriers. Firstly, the lack of reimbursement for healthcare providers for healthcare provided by telemedicine in Italy, that could be solved by the creation of an "ad hoc" reimbursement. Secondly, the limited use of e-technologies in the older population but also to the inadequate number of e-technologies in many hospitals of our Region. In fact, only a widespread distribution of e-technologies could promote the diffusion of new digital tools such as the EMR, that could help healthcare providers in their work.
Conclusion
Telemedicine in LT patients is promising, especially during this COVID-19 pandemic, as in our experience it can reassure the patients and improve the quality of healthcare. Moreover, we can safely select patients needing further investigation. The COVID-19 experience has teached us that temedicine needs to be supported by a broad intervention of telehealth, that is teleducation, teleinformation and also proper attention to the privacy issues. We report, moreover, in older LT patients, high frequency of a lack of digital instruments and some diffidence towards remote consultation. Our results show, in young and middle-aged LT patients, that the combination of standard medical assistance and a more innovative approach could achieve optimization in healthcare in the LT population.
Funding sources
None declared.
Authorship
A.S. and C.C. conception and design of the study, the acquisition of data, or the analysis and interpretation, drafted or provided critical revision of the article.
F.Z. performed data analysis and interpretation and provided critical revision of the article.
S.C. and M.S. acquisition of the data and revision of the paper.
All authors provided final approval of the version to publish.
Conflict of interest
The authors declare no conflicts of interest.
Appendix A1
The outbreak of the novel Coronavirus is influencing our lives. We ask you to answer this questionnaire about how the Coronavirus 19 impacts on your life. The questionnaire is not anonymous to allow us to contact you if you need medical assistance
-
1
Name_________________
-
2
Surname________________
-
3
Sex
-
o
Male
-
o
Female
-
4
Year of birth ________________________
-
5
Weight Kg ___
-
6
Why did you undergo liver transplant?
-
o
hepatitis C-related cirrhosis
-
o
hepatitis B-related cirrhosis
-
o
autoimmune liver diseases
-
o
Other ________________________
-
7
Year of the liver transplant ________________________
-
8
Your city________________________________
-
9
How well do you follow the immunosuppressive therapy?
-
o
Bad, I often forget the tablets
-
o
Quite well; I sometimes forget the tablets
-
o
Well
-
o
Very well; I’m meticulous.
-
10
Do you have one of these health problems or symptoms? (multiple answers allowed)
-
o
Kidney problems
-
o
Diabetes
-
o
High cholesterol levels
-
o
Hypertension
-
o
Osteoporosis
-
o
Depression
-
o
Anxiety
-
o
Sleep disturbances
-
o
Gastrointestinal symptoms
-
o
Headache
-
o
Fatigue
-
11
Do you perform physical exercise?
-
o
No; I’m lazy
-
o
Enough; I daily walk at least 40 minutes
-
o
I regularly go to the gym
-
o
I train strongly every day
-
12
Did you have the flu vaccination?
-
o
Yes
-
o
No
-
o
Specify why_____________
-
13
How much are you worried because of the COVID-19 infection?
Not at all ___ ___ ___ very much
1 2 3 4 5
-
14
Do you think that you are more susceptible to COVID-19 infection because you have had a liver transplant?
Not at all ___ ___ ___ very much
1 2 3 4 5
-
15
Are you worried about social distancing or moving in crowded places, such as supermarkets and food shops?
Not at all ___ ___ ___ very much
1 2 3 4 5
-
16
Do you think there is too much information about COVID-19 from social and mass media?
Not at all ___ ___ ___ very much
1 2 3 4 5
-
17
Do you feel disturbed or tense thinking about coronavirus infection?
Not at all ___ ___ ___ very much
1 2 3 4 5
-
18
Are you worried about the food stocks running out?
Not at all ___ ___ ___ very much
1 2 3 4 5
-
19
Are you worried about mask stocks running out?
Not at all ___ ___ ___ very much
1 2 3 4 5
-
20
Are you worried that during the COVID-19 outbreak you will not be followed as required?
-
o
Yes
-
o
No
-
o
I don’t know
-
21
Are you worried about going to the hospital for a routine visit?
-
o
Yes
-
o
No
-
o
I don’t know
-
22
Will you have the vaccination against COVID 19 if it becomes available?
-
o
Yes
-
o
No
-
o
I don’t know
-
23
Would you use a remote healthcare service (e-health technologies) to interact with your follow-up center, when there are no relevant health problems?”
-
o
Yes
-
o
No, I don't feel the need
-
o
No, I'm afraid I can't answer appropriately
-
o
No, I prefer the routine visit
-
24Do you want to be contacted for a clinical visit?
-
oYes, as soon as possible
-
oYes, but without hurry
-
oI’ll contact the Center if I need
-
oNo thanks
-
oOther (specify)____________________
-
o
-
25
Do you have any comments or suggestions?__________________________
References
- 1.WHO. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen.
- 2.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gu J., Han B., Wang J. COVID-19: gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.02.054]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang C., Shi L., Wang F.S. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020 doi: 10.1016/s2468-1253(20)30057-1]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feng G., Zheng K.I., Yan Q.Q., Rios R.S., Targher G., Byrne C.D., et al. COVID-19 and liver dysfunction: current insights and emergent therapeutic strategies. J Clin Transl Hepatol. 2020;8(1):18–24. doi: 10.14218/jcth.2020.00018]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi: 10.1016/s2213-2600(20)30076-x]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhoori S., Rossi R.E., Citterio D., Mazzaferro V. COVID-19 in long-term liver transplant patients: preliminary experience from an Italian transplant centre in Lombardy. Lancet Gastroenterol Hepatol. 2020 doi: 10.1016/s2468-1253(20)30116-3]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klasnja P., Pratt W. Healthcare in the pocket: mapping the space of mobile-phone health interventions. J Biomed Inform. 2012;45(1):184–198. doi: 10.1016/j.jbi.2011.08.017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Serper M., Cubell A.W., Deleener M.E., Casher T.K., Rosenberg D.J., Whitebloom D., et al. Telemedicine in liver disease and beyond: can the COVID-19 crisis lead to action? Hepatology. 2020 doi: 10.1002/hep.31276]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Serper M., Volk M.L. Current and future applications of telemedicine to optimize the delivery of care in chronic liver disease. Clin Gastroenterol Hepatol. 2018;16(2) doi: 10.1016/j.cgh.2017.10.004]. 157-161 e158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.http://www.regione.campania.it/assets/documents/bollettini-epidemiologico. 2020.
- 12.Bokolo A.J. Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Ir J Med Sci. 2020 doi: 10.1007/s11845-020-02299-z]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nearing K.A., Lum H.D., Dang S., Powers B., McLaren J., Gately M., et al. National Geriatric Network Rapidly Addresses Trainee Telehealth Needs in Response to COVID-19. J Am Geriatr Soc. 2020 doi: 10.1111/jgs.16704]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ganne-Carrié N., Fontaine H., Dumortier J., Boursier J., Bureau C., Leroy V., et al. Suggestions for the care of patients with liver disease during the Coronavirus 2019 pandemic. Clin Res Hepatol Gastroenterol. 2020;44(3):275–281. doi: 10.1016/j.clinre.2020.04.001]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Siniscalchi M., Zingone F., Savarino E.V., D’Odorico A., Ciacci C. COVID-19 pandemic perception in adults with celiac disease: an impulse to implement the use of telemedicine: COVID-19 and CeD. Dig Liver Dis. 2020 doi: 10.1016/j.dld.2020.05.014]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ciacci C., Siniscalchi M. Tips from the battlefront: psychological support of patients with a chronic illness during the COVID-19 lockdown in four steps. United European Gastroenterol J. 2020;8(6):741–742. doi: 10.1177/2050640620927564]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.http://www.protezionecivile.gov.it/home. 2020.
- 18.Weinstein R.S., Krupinski E.A., Doarn C.R. Clinical examination component of telemedicine, telehealth, mhealth, and connected health medical practices. Med Clin North Am. 2018;102(3):533–544. doi: 10.1016/j.mcna.2018.01.002]. [DOI] [PubMed] [Google Scholar]
- 19.Stotts M.J., Grischkan J.A., Khungar V. Improving cirrhosis care: the potential for telemedicine and mobile health technologies. World J Gastroenterol. 2019;25(29):3849–3856. doi: 10.3748/wjg.v25.i29.3849]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.John B.V., Love E., Dahman B., Kurbanova N., Konjeti V.R., Sundaram L.T., et al. Use of telehealth expedites evaluation and listing of patients referred for liver transplantation. Clin Gastroenterol Hepatol. 2020;18(8) doi: 10.1016/j.cgh.2019.12.021]. 1822-1830 e1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Le Lb, Rahal Hk, Viramontes Mr, Meneses Kg, Dong Ts, Saab S. Patient satisfaction and healthcare utilization using telemedicine in liver transplant recipients. Dig Dis Sci. 2019;64(5):1150–1157. doi: 10.1007/s10620-018-5397-5]. [DOI] [PubMed] [Google Scholar]