Abstract
Damage to the annulus fibrosus (AF), the outer region of the intervertebral disc (IVD), results in an undesirable condition that may accelerate IVD degeneration causing low back pain. Despite intense research interest, attempts to regenerate the IVD have failed so far and no effective strategy has translated into a successful clinical outcome. Of particular significance, the failure of strategies to repair the AF has been a major drawback in the regeneration of IVD and nucleus replacement. It is unlikely to secure regenerative mediators (cells, genes, and biomolecules) and artificial nucleus materials after injection with an unsealed AF, as IVD is exposed to significant load and large deformation during daily activities. The AF defects strongly change the mechanical properties of the IVD and activate catabolic routes that are responsible for accelerating IVD degeneration. Therefore, there is a strong need to develop effective therapeutic strategies to prevent or reconstruct AF damage to support operational IVD regenerative strategies and nucleus replacement. By the way of this review, repair and regenerative strategies for AF reconstruction, their current status, challenges ahead, and future outlooks were discussed.
Keywords: intervertebral disc, annulus fibrosus, repair, regeneration, herniation, cell-therapy, gene-therapy, biomolecule-therapy
1. Introduction
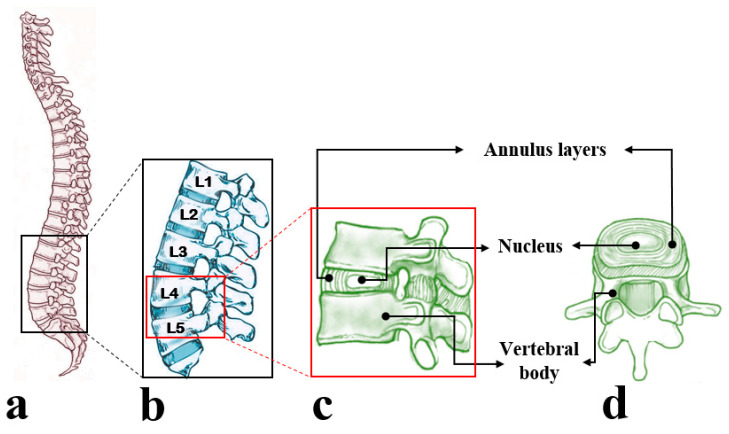
The intervertebral disc (IVD), located between adjacent vertebral bodies in the spine, undergoes large deformations and bears significant loads during daily activities. By occupying approximately one-third of the spinal column’s height, IVDs play a significant role in spinal motion and provide flexibility to the spinal column [1]. The IVD consists of thick outer fibrocartilaginous rings called the annulus fibrosus (AF) that surrounds an inner gelatinous core known as the nucleus pulposus (NP) (Figure 1).
Figure 1.
Schematic presentation of (a) the human spine and (b) lumbar region of the human spine consisting of five intervertebral discs (IVDs). (c,d) Represent a functional spinal unit including IVD and adjacent vertebral bodies from the lumbar spine displayed from the side and top views, respectively. The vertebral body, nucleus, and annulus layers in an isolated IVD were identified using black arrows. The lumbar spine and a functional spinal unit (side view) under two magnifications were denoted by black and red rectangles, respectively.
Degeneration of IVD is a complex process and its association with low back pain (LBP) is not very well known; however, studies have shown aging, genetic, occupation, and IVD disruption may lead to IVD degeneration causing LBP [2,3,4,5]. LBP is a prevalent and debilitating condition with extensive socio-economic impacts affecting the quality of life, reflected by the years lived with disability (YLD). YLD is a measure of the burden of diseases indicating the prevalence of a disorder by loss of health associated with that disability. LBP is the foremost reason for YLD and the second most common cause of hospital visits with the associated direct expenditure of $1.2 billion in Australia, exceeding $100 billion in the US annually [6,7,8].
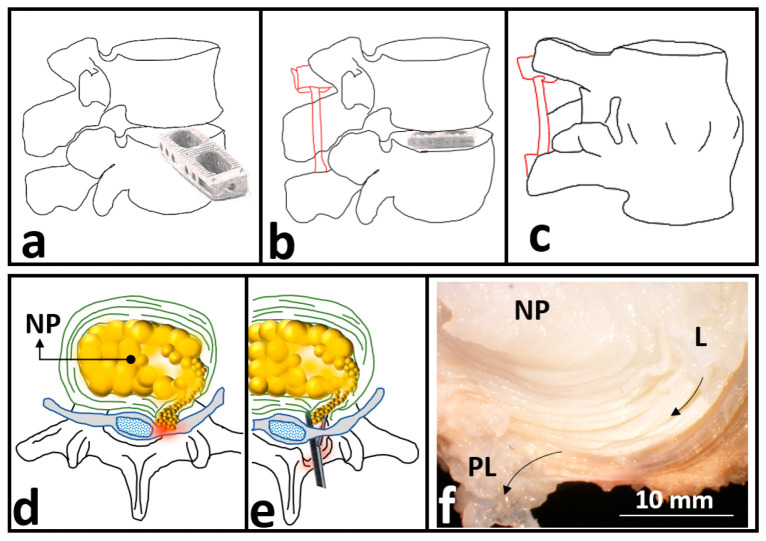
Degenerative changes in spinal IVDs are frequently detected in patients suffering LBP. Current treatments for degeneration-induced-LBP include conservative methods (i.e., rehabilitation) and surgical interventions depending on the severity of IVD degeneration [9,10]. To reduce LBP in highly degenerative IVDs, the current gold standard surgical treatment is spinal fusion aiming to remove the degenerated IVD to finally restrain the adjacent vertebrae (Figure 2a–c). Unfortunately, by fusing the adjacent vertebrae, the method limits the spine mobility and accelerates the degeneration of the adjacent IVDs [11]. Another surgical intervention to replace NP or total IVD, arthroplasty, maintains the spine motion; however, suffers long recovery with notable post-surgery complications. Total IVD implants may induce bone problems in the long term and are not appropriate for patients suffering from osteoporosis or osteopenia [12]. Moreover, the generation of volumetric wear and particulate debris which is likely to occur after total IVD replacement is a concern [13]. While the biological response to the size and volume concentration of generated particles is known to play a key role in osteolysis in other artificial joints, more studies are required to address the concern in IVD implants [14,15,16].
Figure 2.
(a–c) Schematic drawing for spinal fusion to treat degeneration-induced-low back pain (LBP) including (a) remove the degenerated intervertebral disc (IVD) (b) insertion of spin polyetheretherketone (PEEK) cage and (c) restrain the adjacent vertebrae for bone formation. The schematic drawings in red (b,c) denoting an internal fixator used in spinal fusion surgery. (d,e) Schematic drawing of discectomy to treat herniation-induced-LBP including (d) a herniated IVD and (e) the percutaneous endoscopic discectomy process to alleviate LBP by removing the herniated nucleus polposus (NP). (f) A camera photo captured from a herniated IVD to identify herniation pathway initiating from the lateral region (L) moving towards the posterolateral region (PL) of the AF donated by black arrows. (Panel f was reproduced with permission from [18]).
Apart from degeneration, IVD structural defects and damages to the AF are likely to result in herniation causing LBP [17]. Herniation occurs when the NP soft material leaks through the AF of the IVD. Discectomy is the current gold standard surgical intervention to treat herniation-induced-LBP (Figure 2d–f), which aims to remove the herniated NP materials. Consequently, discectomy involves removing a portion of the AF leading to an undesirable condition that may accelerate IVD degeneration causing chronic LBP.
Unfortunately, surgical interventions suffer limitations, and their failure to induce regeneration or stop IVD degeneration is the main drawback. To overcome the inherent restrictions associated with surgical methods to cure LBP, recent investigations have been focused on IVD regenerative medicine with growing interests in cell, biomolecules, and gene therapies [19,20,21,22,23]. Despite intense research interest, attempts to regenerate the IVD have failed so far and no effective strategy has translated into a successful clinical outcome [24,25]. Of particular significance, the failure of strategies to repair the AF has been a major drawback in the regeneration of IVD and nucleus replacement [26]. Since IVD is exposed to significant load and large deformation during daily activities, it is unlikely to secure regenerative mediators (cells, genes, and biomolecules) and artificial nucleus materials after injection into a herniated IVD.
Since AF repair after herniation is still an unsolved challenge, the current review paper aimed to present studies on the repair and regeneration of the AF. This systematic review was undertaken by a search through Science Direct and PubMed (NLM) online databases published in peer-reviewed journals. The search keywords were “annulus fibrosus” AND/OR “repair”, AND/OR “regeneration” covering the period from 2015 to 2020. The bibliographies of these papers were also used to identify additional relevant papers that did not appear in the keyword search.
2. The Anatomy and Physiology of the Annulus Fibrosus
2.1. Structure and Composition of the Annulus Fibrosus
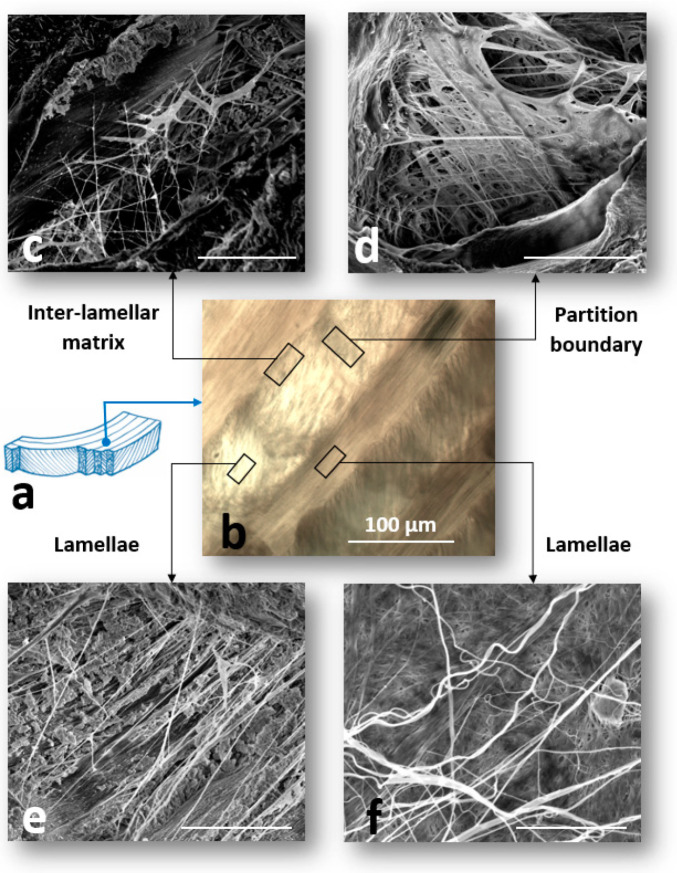
The AF comprises a unique and complex structure of concentric annular lamellae (Figure 3a). Each lamella consists of highly packed collagen fibers (mainly type I) that are oriented at approximately 30° to the transverse plane, varying to −30° relative to the adjacent lamella. The thickness of the lamellae in the AF varies in the radial direction and is approximately 130 µm for the outer AF [27]. The inter-lamellar matrix (ILM), with a thickness of less than 30 µm, located between each adjacent lamellae (Figure 3b). The ILM is composed of elastic fibers, cells, and non-fibrillar matrix consisting of water, lipids, and proteoglycans. A number of glycoproteins including aggrecan, lubricin, GAGs, biglycan, decorine, perlecan, and versican are the main components of the ILM non-fibrillar matrix, which are responsible for lubricating and sustainable hydration of the ILM [28,29]. Additionally, the adjacent ILMs in the AF are connected by partition boundaries (PBs) that provide structural connectivity between the collagen bundles in the AF lamella (Figure 3b) [30].
Figure 3.
(a) Schematic drawing of the annulus fibrosus (AF) lamellar structure. (b) A light microscopic image of the AF prepared at a transverse cutting plane. (c–e) Scanning electron microscopy (SEM) images of the structural organization of elastic fibers in different regions of the annulus fibrosus (AF) including (c) inter-lamellar region (ILM), (d) partition boundary (PB), and (e,f) adjacent lamellae. The regions of interest including ILM, PB, and adjacent lamellae in the AF were denoted by black rectangles and the scale bars for the SEM images were 5 μm. (Panels (c,e), panel (d) and panel (f) were reproduced with permission from [34], [30], and [31], respectively).
Recent studies based on the sonication of the AF samples in NaOH solution to remove non-elastin components (collagen, micro-fibrils, and matrix) revealed a loose network of elastic fibers in the AF lamellae [31,32]. The structure of the elastic fiber network in the ILM is considerably more complex compared to the adjacent lamella with a well-organized network of thick and thin elastic fibers forming a network across the ILM [33]. Elastic fibers present a dense network across the ILM orientating at ± 45° and 0° relative to the collagen fibers, creating a highly organized orthotropic network (Figure 3c–f) [34]. PBs consist of a dense structure of elastic fibers, with a lower density compared to the lamella and a higher density compared to those located in the ILM, but similar fiber orientations [30].
2.2. Annulus Fibrosus Cells
The notochords, a rod-like cartilaginous skeletal structure derived from the mesoderm, provide a platform for early development of IVDs in the spine [35]. Multistage mechanisms, including biochemical reactions and biomechanical scenarios, are involved to develop mature cells from notochords. The AF cells in a mature IVD are fibrochondrocytes and chondrocytes, which morphologically are similar to the fibroblasts [36]. These cells, with a higher density in the outer region of the AF ≈ 9 × 106 cm−3, have thin and elongated morphology, as found in meniscus tissue [37].
Within the ILM region, different cell morphologies have been reported. In the inner lamellae of the AF with less organized collagen fibers, ILM cells are flattened into a disc shape, and become elongated in the outer AF [38]. The difference in the ILM cells’ structure and morphology is due to different mechanical loads experienced by the outer compared to the inner AF. Within the ILM region, the morphology of the cells changes from circular to fusiform from the center towards the ILM-lamella interface [39]. The change in the morphology of the ILM cells is likely to be influenced by the elastic fibers’ orientation and density, as well as loading direction and magnitude experienced by the adjacent lamella [28].
3. Repair Strategies for the Annulus Fibrosus
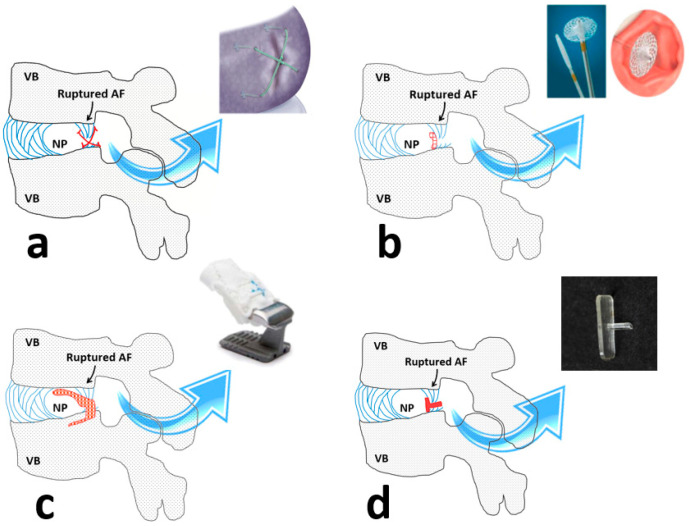
The main challenge associated with the AF repair is the lack of a functional implant integrating host tissue and seal the site of rupture with the mechanical properties similar to the native counterpart. Previous attempts have failed to address the challenge and successfully repair the AF. Early commercial products to close the rupture site in the AF were Xclose® and Inclose® presented by Anulex Technologies Inc (USA). Xclose ® utilized braided polyester bands to make an X-shaped stitch over the AF defect and Inclose® was a surgical mesh to block the AF rupture and prevent re-herniation (Figure 4a,b). Apparently, these products were discontinued since they have failed to neither withstand high mechanical loads experienced by the AF nor improving the healing rate and strength [40].
Figure 4.
(a–c) The schematic drawings and images of three different commercial approaches to repair the annulus fibrosus (AF) including (a) Xclose®, (b) Inclose®, and (c) Barricaid®. (d) A schematic drawing representing a shape memory polymeric implant that was prepared at the laboratory level to repair the AF. The rupture site at the AF and implant images were denoted by black and blue arrows, respectively. The schematic drawings of the implants were denoted in red sketches for each panel. VB, NP, and AF were abbreviations for the vertebral body, nucleus pulposus, and the annulus fibrosus, respectively. (Panels (c,d images) were reproduced with permission from [53] and [55], respectively).
In the absence of an effective closure device, suturing techniques have been recruited; however, inconsistent results to address the efficacy of sutures have been reported. In vitro porcine cadaveric studies showed that modified suturing techniques might provide effective closure to withstand 4000 cycles of flexion/extension with 1500 N of axial loading or resist cyclic compressive loading (≈3000 N) [41,42,43]. However, improvement of healing strength was not observed in ovine sutured IVDs [44]. Further biomechanical assessments revealed that closure of the AF by sutures was not reliable to sustain more than 3400 fatigue cycles [45].
Minimally invasive thermal procedures including “IVD pulse radiofrequency” and “intra-discal electro-thermal” therapies were likely to repair AF with mild rupture. These techniques provided thermal energy to the AF layers in order to denature collagen fibrils locally and seal the rupture site. Severe AF defects are unlikely to be treated by these methods and their contribution to IVD degeneration in the long term is not known [46,47,48,49,50].
Recently, an AF closure device (Barricaid®), with a metallic-base implant and woven polyester component, was introduced (Figure 4c). Barricaid® intended to block the disrupted AF while anchoring to the adjacent vertebral body with a titanium bone anchor [51]. With a successful outcome for reducing pain and decreasing the rate of re-herniation, Barricad® seemed not to maintain or restore native tissue structure and mechanical function [52,53]. This restriction might initiate or accelerate IVD degeneration [54].
Over decades, different polymeric materials for the AF repair have been used in research leading to the creation of several implants and bio-adhesives [56]. The use of fibrin adhesives has improved IVD function and inflammatory response with pain reduction in selected patients suffering from the disco-genic disease [57,58]. A study revealed that the injection of collagen gels crosslinked by riboflavin into the rat IVDs inhibited the progression to the degeneration after needle punctuation [59]. Several studies have shown that the injection of genipin resulted in the integration of AF tissue in degenerated IVD temporarily and improved interfacial shear properties between the AF lamellae [60,61,62,63]. The application of different natural polymers (collagen, alginate, chitosan, silk, and hyaluronan) and synthetic biomaterials (lactic-glycolic composites, poly (1, 8-octanediol malate) and polycaprolactone) for the AF repair have been reported in several studies [64,65,66,67,68,69]. To fabricate collagen-based implants, collagen fibers have been harvested from animal tail tendons and were cross-linked in situ using riboflavin or ammonia [70,71,72,73,74]. A shape memory implant was introduced utilizing macromere of D, L-lactide, and trimethylene carbonate, demonstrating shape recovery at a temperature range of 10 to 40 °C (Figure 4d) [55]. Poly(trimethylene carbonate) combined with an elastic polyurethane membrane was shown to be effective in preventing bovine IVD re-herniation under dynamic loading for 14 days [75]. Amongst studies that suggested polycaprolactone for AF repair, one study introduced a biodegradable construct using poly(caprolactone triol malate) with adjustable degradation and mechanical properties during the pre-polymerization process [76]. Despite successful preliminary laboratory trials to repair AF, the current approaches using polymers lacked appropriate properties (i.e., adhesion) and long-term reliability to resist high stresses during daily activities [77,78,79,80]. Table 1 indicates the current status and the feasibility of the repair strategies that have been used for the AF repair.
Table 1.
The strategies to repair AF and their feasibility.
| Repair Strategies | ||
|---|---|---|
| Strategy | Current Status | Feasibility |
| Early AF closure device (Xclose®, Inclose®) | Not available anymore | Not effective to stop re-herniation and improve the rate or strength of the AF healing. |
| Suturing techniques | Rarely used | Are not reliable to sustain complex cyclic loading and not efficient yet. |
|
Thermal therapies
(pulse radiofrequency and intra-discal electro-thermal therapies) |
In use | Are likely to be effective to seal the structural defects in the mildly ruptured AF. Sever AF defects are unlikely to be treated and their contribution to IVD degeneration in the long term is not known. |
|
Advanced AF closure devices
(Barricaid®) |
Clinical trial | Being effective to reduce the rate of re-herniation and alleviate pain. The key limitation is being different from the native tissue in terms of structure and property, hence it may accelerate the degeneration process. |
| Injectable bio-adhesives | Laboratory trial | The appropriate properties (i.e., adhesion, mechanical strength) and long-term capacity to resist high stresses during daily activities have remained a major concern. |
| Polymeric implants | Laboratory trial | Not sufficient data available to evaluate their feasibility and no further clinical practice was reported. |
4. Regenerative Strategies
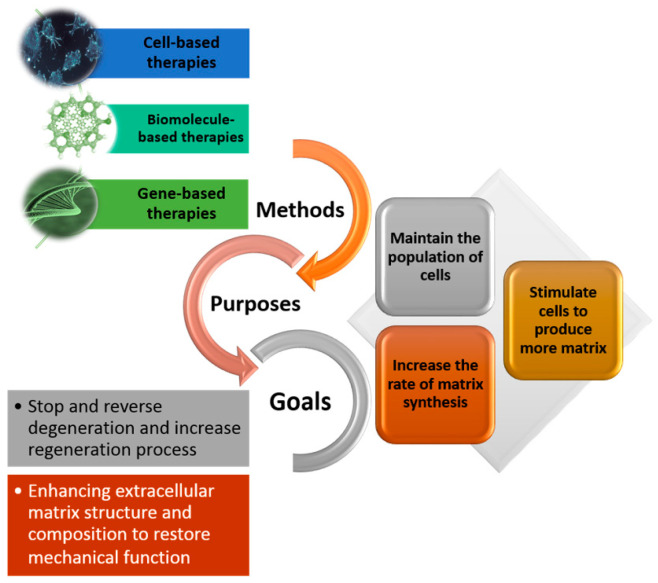
Degeneration of the IVD is a complex condition with multifactorial etiology involving age, genetics, and biology. Additionally, structural defects and damages to the AF manifested by mechanical loads are likely to result in IVD herniation and accelerating degeneration. In a degenerated IVD, the AF is less organized and dehydrated with lower proteoglycans exhibiting different mechanical properties compared to the healthy tissues. A decrease in the AF cell density, as frequently observed in degenerated IVDs, alters the balance of anabolism:catabolism ratio in the extracellular matrix (ECM), changing the AF mechanical, biological, and structural properties [69,70,71]. Therefore, regenerative strategies aim to repopulate a degenerated IVD with healthy cells (cell therapy) or stimulating the existing cells to regulate the ECM reaching an enhanced composition, quantity, and structure (biomolecule and gene therapy) [81,82,83,84,85]. ECM remodeling is crucial to control the action of biochemical mediators such as cytokines (interleukins), growth factors, and enzymes (metalloproteinases and heparanase) to ultimately stop or reverse the IVD degeneration process [86,87,88,89]. In the past few years, cell, biomolecule, and gene therapies have been central to the regenerative strategies (Figure 5).
Figure 5.
Strategies for the regeneration of the annulus fibrosus: Methods, purposes, and final goals.
Gene therapies or the addition of specific bone morphogenetic proteins were shown to accelerate the regeneration process, stimulate ECM production, or prevent the progression of annular injuries [90,91,92,93,94]. However, the delivery of genes into the AF cells has been technically challenging due to the low population of cells. Moreover, the selection of appropriate therapeutic genes, while important, is difficult and requires extensive knowledge of the pathogenesis of degradation, specifically timing and stage of degeneration. Besides, the AF cell apoptosis in degenerated IVDs is a barrier to the successful execution of gene-based therapies [95,96,97].
The effect of growth differentiation factors (GDFs) to enhance the anabolism-catabolism ratio in the ECM has been considered as an effective biomolecule-based regenerative strategy [93,97]. An increasing body of evidence indicated that GDFs were central to the IVD homeostatic processes, upregulation of the healthy cell marker genes in degenerative cells, and differentiation of mesenchymal stem cells to the NP cells [98,99,100]. Of particular significance, the efficacy of recombinant protein GDF6 has been shown to enhance stem cells’ immobilization leading to healing of the AF and regenerating the NP in ovine and lapin models and improved pain in a rat-allograft model [92,93,101,102]. This paracrine function of GDFs’ may off set the short lifetime in vivo which has been considered a limitation restraining their efficacy to regenerate the AF [103]. Quite likely that the secondary chemotactic action, of GDF6, led to the reported repair of the annular defect [98]. However, GDF’s efficacy to enhance the structural integrity of the AF in a short time (weeks) leading to biomechanical stability of the AF needs more investigations.
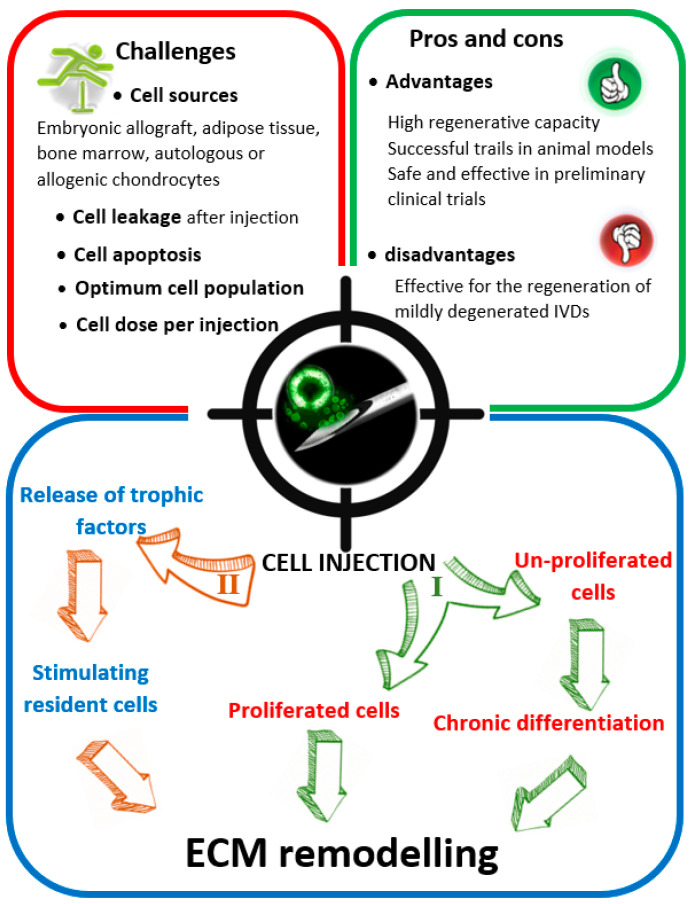
Challenges associated with genetic modification of resident cells through gene transfer or mobilizing endogenous progenitor cells at the degenerated site, making cell therapy more feasible. In addition, the isolation and culture of mesenchymal stem cells have been well documented [102,104,105]. Different external cell sources, including bone marrow stem cells and mesenchymal stromal cells, have been used for AF regeneration [106,107]. Additionally, proliferated mesenchymal stem cells after direct transplantation into the degenerated AF have shown to play a role in the ECM remodeling to enhance the regeneration process (Figure 6).
Figure 6.
Cell-based regenerative strategy seems the most reliable method for annulus fibrosus (AF) regeneration in mildly degeneratedintervertebral discs (IVDs). Two mechanisms are believed to regenerate the AF effectively. The first mechanism (I) is a direct pathway, where the proliferated (or un-proliferated) stem cells contribute to producing extracellular matrix and collagen. The second mechanism (II) involves the injection of the stem cells to encourage resident components (mainly cells) to produce extracellular matrix, indirectly.
However, there are some limitations relevant to cell-based therapy to regenerate the AF [108]. The optimal cell source (bone marrow stem, mesenchymal stromal, and IVD cells) for clinical applications is yet to be defined [106,107]. Preclinical studies have revealed that cell therapy was unlikely to regenerate the AF in highly degenerated IVDs, due to the lack of structural integrity to physically maintain the cells after injection and an appropriate biological environment important to prevent cell apoptosis. Therefore, patients suffering moderate IVD degeneration may benefit most from this type of treatment [109,110,111]. Other restrictions relevant to the cell-based therapy is how to maintain cells at the injection site, preserve their ideal population, and determine the cell dose per injection.
The prevention of cell apoptosis in the AF with avascular structure and poor nutrition is a notable challenge. Indeed, the IVD cellular metabolism is responsible for ECM homeostasis occurring via anaerobic glycolysis pathway with the conversion of glucose to lactic acid. To maintain cell activity and balance the catabolism-to-anabolism ratio, the supply of adequate glucose and appropriate removal of the lactic acid is crucial. Degenerated IVDs or ruptured AF suffer low swelling capacity, due to changes in the quantity and composition of the ECM, with weak nutrition–waste exchange leading to the accumulation of lactic acid. This results in a remarkable drop in pH across the AF that impairs cellular metabolism and increases the risk of cell apoptosis [112,113,114]. Low healing capacity is another restriction towards AF regeneration using cell-based therapies. During the healing process, annular lesions in the posterior AF have been observed to be filled initially with fibrin, blood, and cartilage debris and replaced with a thin layer of fibrous tissue over six months [115]. Studies have shown that almost more than one year is required for the production of collagen fibers with sufficient concentration to improve AF structural integrity [116,117]. Recent attempts to regenerate the AF have been more focused on the stimulation of the resident cells rather than increasing their population. One study suggested that increasing the rate of ECM synthesis was achievable by the transplantation of autologous stem cells to inhibit cell apoptosis [118].
Studies have shown that direct injection of cells has failed to regenerate the AF due to the cell leakage from the defect, making the preservation of the ideal cell population, important to remodel the ECM, almost impossible. Injectable cell delivery systems including biodegradable hydrogels, commercially available collagen II gels (Atelocollagen®), and hyaluronan gels have been employed to promote cell-based strategies via increasing cell retention time at the injection site to prevent leakage-induced-osteophyte formation [88,119,120,121,122,123,124,125]. Studies have revealed that cell-seeded hydrogels based on collagen type II significantly enhanced the rate of ECM synthesis, compared to those employed collagen type I [126,127]. Additionally, collagen gels seeded with ovine AF cells were used for the fabrication of heterogeneous constructs resembling the circumferential alignment of the AF [128]. The rate of degradation in biodegradable hydrogels was found to affect the rate of ECM biosynthesis, with the slower rates of degradation hindering ECM remodeling [129]. Employment of injectable cell-seeded hyaluronan gels was shown to promote ECM production, support the AF cells’ proliferation, and generate a highly conducive environment for chondrogenesis [130,131]. While the challenges of delivering high quality and viable cells at the point of care is a commercial and regulatory challenge, synthetic biomaterials might offer advantages. Despite being minimally invasive, injectable polymers have not been able to entirely address the current problems due to their low mechanical properties. The regenerative strategies to stop or reverse the degeneration process in IVDs are identified in Table 2.
Table 2.
Current regenerative strategies to hinder or reverse the degeneration process in IVDs.
| Regenerative Strategies | ||
|---|---|---|
| Strategy | Current Status | Feasibility |
| Gene therapies | Laboratory trial | Being effective in accelerating the regeneration process, stimulation of ECM remodeling, and prevention of progression to AF injury. The frequent observation of AF cell apoptosis in degenerated IVDs is a barrier. |
|
Biomolecule therapies
(growth factors) |
Laboratory trial | Being effective in cell differentiation, enhancing the healing process, and upregulating of healthy cell marker genes. The short lifetime of biomolecules is a limitation that restrains the efficacy of biomolecules to regenerate AF. |
| Cell therapies | preclinical studies | Being successful in ECM remodeling via direct transplantation of proliferated mesenchymal stem cells into the degenerated AF. Unlikely to regenerate highly degenerated IVDs due to the lack of (1) structural integrity to physically maintain the cells after injection, and (2) an appropriate biological environment important to prevent cell apoptosis. |
| Injectable cell delivery gels | Laboratory trial | Being effective to promote cell-based strategies via increasing cell retention time at the injection site. Injectable polymers have not been able to entirely address the current problems due to their low mechanical properties. |
5. Future Outlook
Understanding the mechanisms of IVD degeneration to stop or reverse this process or re-establishing function through therapies is a challenge at the intersection of biomaterials, biomechanics, clinical practice, and biology [132,133,134]. Despite intense research interest in this area, lack of suitable collaborations has been a severe limitation towards the creation of effective therapeutic devices to regenerate the AF. Yet those who are presently working at this multidisciplinary crossing point indicate the current challenge is to get these scientific cultures to work together. Already formed joint meetings to bridge these disparate disciplines is motivating; however, not adequate, evidenced by the unproductive outcome. Noticeably, it is important to develop a new standard for training the next generation of biomechanical and biomaterials engineers with a strong background in biochemistry, molecular, and cell biology. This new generation of engineers will be specifically able to offer a way of thinking that may contribute practically to unravel the inherent complexity of IVD and propose effective biologically-grounded engineering solutions to cure low back pain, regenerate IVDs, and design future medical devices.
Over decades, separate and independent approaches to find relative solutions for the NP replacement, AF repair, and IVD replacement have resulted in partial achievements. Attempts to replace the NP and keep the implant in place have failed in the absence of appropriate strategies for AF repair. However, there are newer designs of nucleus replacement undergoing clinical trials that are minimally invasive and use sophisticated delivery technology that may come to clinical use in the future [135]. Development of injectable biomaterials to simultaneously replace the NP and repair the AF is one step forward to resolving the problems associated with herniation [136]. Since the clinical translation of in vitro cell studies is yet challenging, the first but not the best approach will be the preparation of cell-free injectable biomaterials to effectively repair the AF defect in the short term [137]. The AF defects strongly change the mechanical properties of the IVD and activate catabolic routes that are responsible for accelerating IVD degeneration [138]. Indeed, the development of mechanically-reinforced injectable biomaterials that resemble tissue properties, although cell-free, provide opportunities to stop or decelerate the degeneration process. This approach may be an effective treatment for both young patients suffering herniation or those who are at the early stage of IVD degeneration. To achieve this, the development of new biomaterials and the employment of novel crosslinking agents is critical. One suggestion is the use of hyperbranched molecules in self-healing hydrogels to simultaneously increase the mechanical and swelling properties [139].
From a structural point of view, another key approach is a thorough understanding of the herniation pathway [18,140]. While a small number of microstructural and one biomechanical–microstructural studies have revealed the herniation pathway in the outer AF, more scientific explorations are required to address the herniation mechanism [124]. Since recent studies revealed that elastic fibers in the AF form an organized network across the AF, understanding of their role in the structural integrity of the healthy and degenerated IVDs is an important step towards developing new strategies to repair the AF. The design of new biomaterials mimicking the biochemical, mechanical, and morphological properties of elastic fibers may provoke the functionality of future repair strategies. One approach would be the formation of chemical bonding between injectable elastic-based biomaterials and the AF elastic network. This may result in more secure treatments reducing the risk of biomaterial leakage which is a common problem with existing injectable systems.
From a clinical point of view, more studies are required to address the impact of total discectomy on the structural integrity of AF tissue adjacent to the rapture site. Likely, one major reason for unsuccessful attempts to repair the AF after discectomy is harsh tissue removal during surgery. The understanding of the impact of discectomy after herniation on the structural integrity of AF remains an important mid- to long-term goal in spine research.
Future challenges toward effective AF repair strategies and IVD replacement include fabrication techniques that replicate the structural complexity of the tissue. Recent studies on presenting electrospun angle-ply structures and collagen gel composites were able to partially replicate the tissue structure [59,141,142,143]. However, the mechanical and morphological properties of the elastic fibers are missing pieces and their primary stability is an unsolved problem. Taking inspiration from the structural organization of elastic fibers and collagen bundles, 3D bioprinting may play an important role in the fabrication of IVD implants to restore the AF function and properties. The addition of calcified biomaterials during 3D bioprinting, an option to captivate the endplate structures and properties, is an approach to resolve the primary stability issue via bone growth. While 3D bioprinting provides unique opportunities for the fabrication of complex constructs by combining cells, fibers, and biomaterials, it has been unexplored for IVD repair strategies [144,145,146]. The challenge ahead is the lack of suitable structural models recapitulating the multiscale hierarchy of the IVD structure [147]. The major drawback is the absence of fibril form in the current 3D IVD approaches [147,148], since the fibril topography was shown to have an impact on cell adhesion and phenotype [149,150]. Technical difficulties in the formulation of bioinks to retain appropriate shape fidelity and adjust their shear-thinning behavior remain challenging. The development of novel hydrogels with optimal mechanical and biochemical properties and modulation of viscosity (blending with thickeners) to enhance shape fidelity will be essential for successful 3D bioprinting of IVD constructs. To the best of our knowledge, there is a lack of bioink specifically designed for IVD construction and it is not clear whether available bioinks for regeneration of cartilage [151], cardiovascular tissues [152], heart valves [153], or other tissues [154,155,156] are appropriate for IVD bioprinting. Another challenge is optimizing printing parameters including the rate of printing, characteristics of bioinks (temperature, concentration, surface charge, and water content), the geometry of the nozzle, post-extrusion shape and size stability of the 3D bioprinted constructs, and crosslinking intervals [148,157]. These parameters critically influence the quality of the final constructs as well as directly affect the viability of cells, if included to the bioink, by being exposed to relatively high pressure during fabrication. Of particular interest is the lack of evidence demonstrating interactions amongst the optimized structural parameters of IVD and cells survival within IVD.
6. Conclusions
Damage to the AF and disintegration of the IVD structure are likely to result in IVD herniation causing low back pain. The main challenge to repair the AF is sealing the site of rupture to achieve a functional implant that integrates the host with match mechanical properties compared to the natural tissue. Unfortunately, despite intense research, attempts to repair the AF have failed so far and no effective strategy has translated into a successful clinical outcome. Although knowledge around IVD regeneration has significantly increased and new methods have developed, numerous attempts to regenerate the AF have not concluded to satisfactory results due to the lack of a method to secure the cells at the defect site. It seems that therapeutic strategies should strongly focus on the prevention of AF damage or techniques for AF reconstruction to preserve the structural integrity of the AF in IVDs. This will result in the restoration of the mechanical properties of IVD and the control of catabolic routes that are responsible for accelerating IVD degeneration. To develop effective repair and regenerative strategies, including mechanically stable cell-seeded hydrogel, challenges ahead are likely to be a thorough understanding of herniation pathway, role, and structural organization of fibrous component of the IVD, as well as incorporating advanced additive manufacturing approach. It is also important to mention that surgical procedures to treat herniation should avoid further damage to the AF as much as possible.
Acknowledgments
Javad Tavakoli is grateful for the support of the University of Technology Sydney (UTS) with a Chancellor’s Postdoctoral Research Fellowship (CPDRF) for the research work.
Abbreviations
| LBP | Low back pain |
| IVD | Intervertebral disc |
| AF | Annulus Fibrosus |
| NP | Nucleus Pulposus |
| ECM | Extracellular Matrix |
| ILM | Inter-lamellar matrix |
| GDF | Growth differentiation factors |
| YLD | Years lived with disability |
Author Contributions
J.T., A.D.D., and J.L.T. have contributed equally and All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Chan S.C.W., Ferguson S.J., Gantenbein-Ritter B. The effects of dynamic loading on the intervertebral disc. Eur. Spine J. 2011;20:1796–1812. doi: 10.1007/s00586-011-1827-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Urban J.P., Fairbank J.C. Current perspectives on the role of biomechanical loading and genetics in development of disc degeneration and low back pain; a narrative review. J. Biomech. 2019:109573. doi: 10.1016/j.jbiomech.2019.109573. [DOI] [PubMed] [Google Scholar]
- 3.Kupka J., Kohler A., El Bagdadi K., Bostelmann R., Brenneis M., Fleege C., Chan D., Zaucke F., Meurer A., Rickert M. Adrenoceptor Expression during Intervertebral Disc Degeneration. Int. J. Mol. Sci. 2020;21:2085. doi: 10.3390/ijms21062085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruiz-Fernández C., Francisco V., Pino J., Mera A., González-Gay M.A., Gómez R., Lago F., Gualillo O. Molecular Relationships among Obesity, Inflammation and Intervertebral Disc Degeneration: Are Adipokines the Common Link? Int. J. Mol. Sci. 2019;20:2030. doi: 10.3390/ijms20082030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahmed A.S., Berg S., Alkass K., Druid H., Hart D.A., Svensson C.I., Kosek E. NF-κB-Associated pain-related neuropeptide expression in patients with degenerative disc disease. Int. J. Mol. Sci. 2019;20:658. doi: 10.3390/ijms20030658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu A., Dong W., Liu S., Cheung J.P.Y., Kwan K.Y.H., Zeng X., Zhang K., Sun Z., Wang X., Cheung K.M.C. The prevalence and years lived with disability caused by low back pain in China, 1990 to 2016: Findings from the global burden of disease study 2016. Pain. 2019;160:237. doi: 10.1097/j.pain.0000000000001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luo X., Pietrobon R., Sun S.X., Liu G.G., Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine. 2004;29:79–86. doi: 10.1097/01.BRS.0000105527.13866.0F. [DOI] [PubMed] [Google Scholar]
- 8.Walker B., Muller R., Grant W. Low back pain in Australian adults: The economic burden. Asia Pac. J. Public Health. 2003;15:79–87. doi: 10.1177/101053950301500202. [DOI] [PubMed] [Google Scholar]
- 9.Sabnis A.B., Diwan A.D. The timing of surgery in lumbar disc prolapse: A systematic review. Indian J. Orthop. 2014;48:127. doi: 10.4103/0019-5413.128740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu P.H., Kim H.S., Jang I.-T. Intervertebral Disc Diseases PART 2: A Review of the Current Diagnostic and Treatment Strategies for Intervertebral Disc Disease. Int. J. Mol. Sci. 2020;21:2135. doi: 10.3390/ijms21062135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kishen T.J., Diwan A.D. Fusion versus disk replacement for degenerative conditions of the lumbar and cervical spine: Quid est testimonium? Orthop. Clin. 2010;41:167–181. doi: 10.1016/j.ocl.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 12.Diwan A.D., Parvataneni H.K., Khan S.N., Sandhu H.S., Girardi F.P., Cammisa F.P. Current concepts in intervertebral disk restoration. Orthop. Clin. 2000;31:453–464. doi: 10.1016/S0030-5898(05)70163-2. [DOI] [PubMed] [Google Scholar]
- 13.Vicars R., Hyde P., Brown T., Tipper J., Ingham E., Fisher J., Hall R. The effect of anterior–posterior shear load on the wear of ProDisc-L TDR. Eur. Spine J. 2010;19:1356–1362. doi: 10.1007/s00586-010-1396-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tipper J.L., Ingham E., Hailey J.L., Besong A.A., Fisher J., Wroblewski B.M., Stone M.H. Quantitative analysis of polyethylene wear debris, wear rate and head damage in retrieved Charnley hip prostheses. J. Mater. Sci. Mater. Med. 2000;11:117–124. doi: 10.1023/A:1008901302646. [DOI] [PubMed] [Google Scholar]
- 15.Endo M., Tipper J.L., Barton D.C., Stone M.H., Ingham E., Fisher J. Comparison of wear, wear debris and functional biological activity of moderately crosslinked and non-crosslinked polyethylenes in hip prostheses. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2002;216:111–122. doi: 10.1243/0954411021536333. [DOI] [PubMed] [Google Scholar]
- 16.Suñer S., Gowland N., Craven R., Joffe R., Emami N., Tipper J.L. Ultrahigh molecular weight polyethylene/graphene oxide nanocomposites: Wear characterization and biological response to wear particles. J. Biomed. Mater. Res. Part B Appl. Biomater. 2018;106:183–190. doi: 10.1002/jbm.b.33821. [DOI] [PubMed] [Google Scholar]
- 17.Long R.G., Torre O.M., Hom W.W., Assael D.J., Iatridis J.C. Design requirements for annulus fibrosus repair: Review of forces, displacements, and material properties of the intervertebral disk and a summary of candidate hydrogels for repair. J. Biomech. Eng. 2016;138 doi: 10.1115/1.4032353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Veres S.P., Robertson P.A., Broom N.D. ISSLS Prize Winner: Microstructure and Mechanical Disruption of the Lumbar Disc Annulus Part II: How the Annulus Fails Under Hydrostatic Pressure. Spine. 2008;33:2711–2720. doi: 10.1097/BRS.0b013e31817bb906. [DOI] [PubMed] [Google Scholar]
- 19.Ishiguro H., Kaito T., Yarimitsu S., Hashimoto K., Okada R., Kushioka J., Chijimatsu R., Takenaka S., Makino T., Sakai Y. Intervertebral disc regeneration with an adipose mesenchymal stem cell-derived tissue-engineered construct in a rat nucleotomy model. Acta Biomater. 2019;87:118–129. doi: 10.1016/j.actbio.2019.01.050. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez-Leon E.A., Bielajew B.J., Hu J.C., Athanasiou K.A. Engineering self-assembled neomenisci through combination of matrix augmentation and directional remodeling. Acta Biomater. 2020 doi: 10.1016/j.actbio.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Takeoka Y., Yurube T., Nishida K. Gene therapy approach for intervertebral disc degeneration: An update. Neurospine. 2020;17:3. doi: 10.14245/ns.2040042.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krouwels A., Iljas J.D., Kragten A.H., Dhert W.J., Öner F.C., Tryfonidou M.A., Creemers L.B. Bone Morphogenetic Proteins for Nucleus Pulposus Regeneration. Int. J. Mol. Sci. 2020;21:2720. doi: 10.3390/ijms21082720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tendulkar G., Ehnert S., Sreekumar V., Chen T., Kaps H.-P., Golombek S., Wendel H.-P., Nüssler A.K., Avci-Adali M. Exogenous Delivery of Link N mRNA into Chondrocytes and MSCs—The Potential Role in Increasing Anabolic Response. Int. J. Mol. Sci. 2019;20:1716. doi: 10.3390/ijms20071716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jiang E.Y., Sloan S.R., Jr., Wipplinger C., Kirnaz S., Härtl R., Bonassar L.J. Proteoglycan removal by chondroitinase ABC improves injectable collagen gel adhesion to annulus fibrosus. Acta Biomater. 2019;97:428–436. doi: 10.1016/j.actbio.2019.08.024. [DOI] [PubMed] [Google Scholar]
- 25.Chuah Y.J., Tan J.R., Wu Y., Lim C.S., Hee H.T., Kang Y., Wang D.-A. Scaffold-Free Tissue Engineering with Aligned Bone Marrow Stromal Cell Sheets to Recapitulate the Microstructural and Biochemical Composition of Annulus Fibrosus. Acta Biomater. 2020;107:129–137. doi: 10.1016/j.actbio.2020.02.031. [DOI] [PubMed] [Google Scholar]
- 26.Long R.G., Ferguson S.J., Benneker L.M., Sakai D., Li Z., Pandit A., Grijpma D.W., Eglin D., Zeiter S., Schmid T. Morphological and biomechanical effects of annulus fibrosus injury and repair in an ovine cervical model. JOR Spine. 2019:e1074. doi: 10.1002/jsp2.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cassidy J., Hiltner A., Baer E. Hierarchical structure of the intervertebral disc. Connect. Tissue Res. 1989;23:75–88. doi: 10.3109/03008208909103905. [DOI] [PubMed] [Google Scholar]
- 28.Tavakoli J., Elliott D.M., Costi J.J. Structure and mechanical function of the inter-lamellar matrix of the annulus fibrosus in the disc. J. Orthop. Res. 2016;34:1307–1315. doi: 10.1002/jor.23306. [DOI] [PubMed] [Google Scholar]
- 29.Tavakoli J., Costi J.J. New findings confirm the viscoelastic behaviour of the inter-lamellar matrix of the disc annulus fibrosus in radial and circumferential directions of loading. Acta Biomater. 2018;71:411–419. doi: 10.1016/j.actbio.2018.03.015. [DOI] [PubMed] [Google Scholar]
- 30.Tavakoli J., Costi J.J. Ultrastructural organization of elastic fibres in the partition boundaries of the annulus fibrosus within the intervertebral disc. Acta Biomater. 2018;68:67–77. doi: 10.1016/j.actbio.2017.12.017. [DOI] [PubMed] [Google Scholar]
- 31.Tavakoli J., Costi J.J. Development of a rapid matrix digestion technique for ultrastructural analysis of elastic fibers in the intervertebral disc. J. Mech. Behav. Biomed. Mater. 2017;71:175–183. doi: 10.1016/j.jmbbm.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 32.Tavakoli J., Costi J.J. A method for visualization and isolation of elastic fibres in annulus fibrosus of the disc. Mater. Sci. Eng. C. 2018;93:299–304. doi: 10.1016/j.msec.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 33.Tavakoli J., Costi J.J. New insights into the viscoelastic and failure mechanical properties of the elastic fiber network of the inter-lamellar matrix in the annulus fibrosus of the disc. Acta Biomater. 2018;77:292–300. doi: 10.1016/j.actbio.2018.07.023. [DOI] [PubMed] [Google Scholar]
- 34.Tavakoli J., Elliott D., Costi J. The ultra-structural organization of the elastic network in the intra-and inter-lamellar matrix of the intervertebral disc. Acta Biomater. 2017;58:269–277. doi: 10.1016/j.actbio.2017.05.036. [DOI] [PubMed] [Google Scholar]
- 35.Colombier P., Camus A., Lescaudron L., Clouet J., Guicheux J. Intervertebral disc regeneration: A great challenge for tissue engineers. Trends Biotechnol. 2014;32:433–435. doi: 10.1016/j.tibtech.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 36.Sakai D., Andersson G.B. Stem cell therapy for intervertebral disc regeneration: Obstacles and solutions. Nature Rev. Rheumatol. 2015;11:243–256. doi: 10.1038/nrrheum.2015.13. [DOI] [PubMed] [Google Scholar]
- 37.Vonk L.A., Kroeze R.J., Doulabi B.Z., Hoogendoorn R.J., Huang C., Helder M.N., Everts V., Bank R.A. Caprine articular, meniscus and intervertebral disc cartilage: An integral analysis of collagen network and chondrocytes. Matrix Biol. 2010;29:209–218. doi: 10.1016/j.matbio.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 38.Bruehlmann S.B., Rattner J.B., Matyas J.R., Duncan N.A. Regional variations in the cellular matrix of the annulus fibrosus of the intervertebral disc. J. Anat. 2002;201:159–171. doi: 10.1046/j.1469-7580.2002.00080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hayes A.J., Smith S.M., Gibson M.A., Melrose J. Comparative Immunolocalization of the Elastin Fiber–Associated Proteins Fibrillin-1, LTBP-2, and MAGP-1 With Components of the Collagenous and Proteoglycan Matrix of the Fetal Human Intervertebral Disc. Spine. 2011;36:E1365–E1372. doi: 10.1097/BRS.0b013e31821fd23e. [DOI] [PubMed] [Google Scholar]
- 40.Bowles R.D., Setton L.A. Biomaterials for intervertebral disc regeneration and repair. Biomaterials. 2017;129:54–67. doi: 10.1016/j.biomaterials.2017.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bailey A., Araghi A., Blumenthal S., Huffmon G.V. Prospective, multicenter, randomized, controlled study of anular repair in lumbar discectomy: Two-year follow-up. Spine. 2013;38:1161–1169. doi: 10.1097/BRS.0b013e31828b2e2f. [DOI] [PubMed] [Google Scholar]
- 42.Bateman A.H., Balkovec C., Akens M.K., Chan A.H.W., Harrison R.D., Oakden W., Yee A.J.M., McGill S.M. Closure of the annulus fibrosus of the intervertebral disc using a novel suture application device—in vivo porcine and ex vivo biomechanical evaluation. Spine J. 2016;7:889–895. doi: 10.1016/j.spinee.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 43.Chiang C.J., Cheng C.K., Sun J.S., Liao C.J., Wang Y.H., Tsuang Y.H. The effect of a new anular repair after discectomy in intervertebral disc degeneration: An experimental study using a porcine spine model. Spine. 2011;36:761–769. doi: 10.1097/BRS.0b013e3181e08f01. [DOI] [PubMed] [Google Scholar]
- 44.Ahlgren B.D., Lui W., Herkowitz H.N., Panjabi M.M., Guiboux J.P. Effect of anular repair on the healing strength of the intervertebral disc: A sheep model. Spine. 2000;25:2165–2170. doi: 10.1097/00007632-200009010-00004. [DOI] [PubMed] [Google Scholar]
- 45.Heuer F., Ulrich S., Claes L., Wilke H.J. Biomechanical evaluation of conventional anulus fibrosus closure methods required for nucleus replacement. Laboratory investigation. J. Neurosurg. Spine. 2008;9:307–313. doi: 10.3171/SPI/2008/9/9/307. [DOI] [PubMed] [Google Scholar]
- 46.Kloth D., Fenton D., Andersson G., Block J. Intradiscal electrothermal therapy (IDET) for the treatment of discogenic low back pain: Patient selection and indications for use. Pain Physician. 2008;11:659–668. [PubMed] [Google Scholar]
- 47.Maurer P., Block J.E., Squillante D. Intradiscal electrothermal therapy (IDET) provides effective symptom relief in patients with discogenic low back pain. Clin. Spine Surg. 2008;21:55–62. doi: 10.1097/BSD.0b013e31812f4f29. [DOI] [PubMed] [Google Scholar]
- 48.Fukui S., Nitta K., Iwashita N., Tomie H., Nosaka S., Rohof O. Results of intradiscal pulsed radiofrequency for lumbar discogenic pain: Comparison with intradiscal electrothermal therapy. Korean J. Pain. 2012;25:155–160. doi: 10.3344/kjp.2012.25.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fukui S., Nitta K., Iwashita N., Tomie H., Nosaka S., Rohof O. Intradiscal pulsed radiofrequency for chronic lumbar discogenic low back pain: A one year prospective outcome study using discoblock for diagnosis. Pain Physician. 2013;16:435–442. [PubMed] [Google Scholar]
- 50.Kim H.S., Wu P.H., Jang I.-T. Lumbar degenerative disease part 1: Anatomy and pathophysiology of intervertebral discogenic pain and radiofrequency ablation of basivertebral and sinuvertebral nerve treatment for chronic discogenic back pain: A prospective case series and review of literature. Int. J. Mol. Sci. 2020;21:1483. doi: 10.3390/ijms21041483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hahn B.S., Ji G.Y., Moon B., Shin D.A., Ha Y., Kim K.N., Yoon D.H. Use of annular closure device (Barricaid®) for preventing lumbar disc Reherniation: One-year results of three cases. Korean J. Neurotrauma. 2014;10:119–122. doi: 10.13004/kjnt.2014.10.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Choy W.J., Phan K., Diwan A.D., Ong C.S., Mobbs R.J. Annular closure device for disc herniation: Meta-analysis of clinical outcome and complications. BMC Musculoskelet. Disord. 2018;19:290. doi: 10.1186/s12891-018-2213-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Parker S.L., Grahovac G., Vukas D., Vilendecic M., Ledic D., McGirt M.J., Carragee E.J. Effect of an Annular Closure Device (Barricaid) on Same-Level Recurrent Disk Herniation and Disk Height Loss After Primary Lumbar Discectomy: Two-year Results of a Multicenter Prospective Cohort Study. Clin. Spine Surg. 2016;29:454–460. doi: 10.1097/BSD.0b013e3182956ec5. [DOI] [PubMed] [Google Scholar]
- 54.Trummer M., Eustacchio S., Barth M., Klassen P.D., Stein S. Protecting facet joints post-lumbar discectomy: Barricaid annular closure device reduces risk of facet degeneration. Clin. Neurol. Neurosurg. 2013;115:1440–1445. doi: 10.1016/j.clineuro.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 55.Sharifi S., van Kooten T.G., Kranenburg H.-J.C., Meij B.P., Behl M., Lendlein A., Grijpma D.W. An annulus fibrosus closure device based on a biodegradable shape-memory polymer network. Biomaterials. 2013;34:8105–8113. doi: 10.1016/j.biomaterials.2013.07.061. [DOI] [PubMed] [Google Scholar]
- 56.Stephen R.S., Jr., Marianne L., Ibrahim H., Roger H., Lawrence J.B. Biologic Annulus Fibrosus Repair: A Review of Preclinical In Vivo Investigations. Tissue Eng. Part B Rev. 2018;24:179–190. doi: 10.1089/ten.TEB.2017.0351. [DOI] [PubMed] [Google Scholar]
- 57.Yin W., Pauza K., Olan W.J., Doerzbacher J.F., Thorne K.J. Intradiscal injection of fibrin sealant for the treatment of symptomatic lumbar internal disc disruption: Results of a prospective multicenter pilot study with 24-month follow-Up. Pain Med. 2014;15:16–31. doi: 10.1111/pme.12249. [DOI] [PubMed] [Google Scholar]
- 58.Buser Z., Liu J., Thorne K.J., Coughlin D., Lotz J.C. Inflammatory response of intervertebral disc cells is reduced by fibrin sealant scaffold in vitro. J. Tissue Eng. Regen. Med. 2014;8:77–84. doi: 10.1002/term.1503. [DOI] [PubMed] [Google Scholar]
- 59.Grunert P., Borde B.H., Towne S.B., Moriguchi Y., Hudson K.D., Bonassar L.J., Härtl R. Riboflavin crosslinked high-density collagen gel for the repair of annular defects in intervertebral discs: An in vivo study. Acta Biomater. 2015;26:215–224. doi: 10.1016/j.actbio.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 60.Slusarewicz P., Zhu K., Kirking B., Toungate J., Hedman T. Optimization of protein crosslinking formulations for the treatment of degenerative disc disease. Spine. 2011;36:E7. doi: 10.1097/BRS.0b013e3181cc3de9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hsu Y.-C., Kuo Y.-W., Chang Y.-C., Nikkhoo M., Wang J.-L. Rheological and dynamic integrity of simulated degenerated disc and consequences after cross-linker augmentation. Spine. 2013;38:E1446–E1453. doi: 10.1097/BRS.0b013e3182a3d09d. [DOI] [PubMed] [Google Scholar]
- 62.Kirking B., Hedman T., Criscione J. Changes in the interfacial shear resistance of disc annulus fibrosus from genipin crosslinking. J. Biomech. 2014;47:293–296. doi: 10.1016/j.jbiomech.2013.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schek R., Michalek A., Iatridis J. Genipin-crosslinked fibrin hydrogels as a potential adhesive to augment intervertebral disc annulus repair. Eur. Cells Mater. 2011;21:373. doi: 10.22203/eCM.v021a28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mizuno H., Roy A.K., Vacanti C.A., Kojima K., Ueda M., Bonassar L.J. Tissue-Engineered Composites of Anulus Fibrosus and Nucleus Pulposus for Intervertebral Disc Replacement. Spine. 2004;29:1290–1297. doi: 10.1097/01.BRS.0000128264.46510.27. [DOI] [PubMed] [Google Scholar]
- 65.Saad L., Spector M. Effects of collagen type on the behavior of adult canine annulus fibrosus cells in collagen-glycosaminoglycan scaffolds. J. Biomed. Mater. Res. Part A. 2004;71:233–241. doi: 10.1002/jbm.a.30150. [DOI] [PubMed] [Google Scholar]
- 66.Wilda H., Gough J.E. In vitro studies of annulus fibrosus disc cell attachment, differentiation and matrix production on PDLLA/45S5 Bioglass composite films. Biomaterials. 2006;27:5220–5229. doi: 10.1016/j.biomaterials.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 67.Shen B., Wei A., Bhargav D., Kishen T., Diwan A.D. Hyaluronan: Its potential application in intervertebral disc regeneration. Orthop. Res. Rev. 2010 doi: 10.2147/ORR.S7741. [DOI] [Google Scholar]
- 68.Tavakoli J. Tissue engineering of the intervertebral disc’s annulus fibrosus: A scaffold-based review study. Tissue Eng. Regenrattive Med. 2016 doi: 10.1007/s13770-017-0024-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Growney Kalaf E.A., Flores R., Bledsoe J.G., Sell S.A. Characterization of slow-gelling alginate hydrogels for intervertebral disc tissue-engineering applications. Mater. Sci. Eng. C. 2016;63:198–210. doi: 10.1016/j.msec.2016.02.067. [DOI] [PubMed] [Google Scholar]
- 70.Bowles R.D., Williams R.M., Zipfel W.R., Bonassar L.J. Self-assembly of aligned tissue-engineered annulus fibrosus and intervertebral disc composite via collagen gel contraction. Tissue Eng. Part A. 2010;16:1339–1348. doi: 10.1089/ten.tea.2009.0442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Elsdale T., Bard J. Collagen Substrata for Studies on Cell Behavior. J. Cell Biol. 1972;54:626–637. doi: 10.1083/jcb.54.3.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Borde B., Grunert P., Hartl R., Bonassar L.J. Injectable, high-density collagen gels for annulus fibrosus repair: An in vitro rat tail model. J. Biomed. Mater. Res. A. 2014 doi: 10.1002/jbm.a.35388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bowles R.D., Gebhard H.H., Hartl R., Bonassar L.J. Tissue-engineered intervertebral discs produce new matrix, maintain disc height, and restore biomechanical function to the rodent spine. Proc. Natl. Acad. Sci. USA. 2011;108:13106–13111. doi: 10.1073/pnas.1107094108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chik T.K., Ma X.Y., Choy T.H., Li Y.Y., Diao H.J., Teng W.K., Han S.J., Cheung K.M., Chan B.P. Photochemically crosslinked collagen annulus plug: A potential solution solving the leakage problem of cell-based therapies for disc degeneration. Acta Biomater. 2013;9:8128–8139. doi: 10.1016/j.actbio.2013.05.034. [DOI] [PubMed] [Google Scholar]
- 75.Pirvu T., Blanquer S.B.G., Benneker L.M., Grijpma D.W., Richards R.G., Alini M., Eglin D., Grad S., Li Z. A combined biomaterial and cellular approach for annulus fibrosus rupture repair. Biomaterials. 2015;42:11–19. doi: 10.1016/j.biomaterials.2014.11.049. [DOI] [PubMed] [Google Scholar]
- 76.Wan Y., Feng G., Shen F.H., Laurencin C.T., Li X. Biphasic scaffold for annulus fibrosus tissue regeneration. Biomaterials. 2008;29:643–652. doi: 10.1016/j.biomaterials.2007.10.031. [DOI] [PubMed] [Google Scholar]
- 77.Vadalà G., Mozetic P., Rainer A., Centola M., Loppini M., Trombetta M., Denaro V. Bioactive electrospun scaffold for annulus fibrosus repair and regeneration. Eur. Spine J. 2012;21:20–26. doi: 10.1007/s00586-012-2235-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Guillaume O., Daly A., Lennon K., Gansau J., Buckley S.F., Buckley C.T. Shape-memory porous alginate scaffolds for regeneration of the annulus fibrosus: Effect of TGF-β3 supplementation and oxygen culture conditions. Acta Biomater. 2014;10:1985–1995. doi: 10.1016/j.actbio.2013.12.037. [DOI] [PubMed] [Google Scholar]
- 79.Xu X., Hu J., Lu H. Histological observation of a gelatin sponge transplant loaded with bone marrow-derived mesenchymal stem cells combined with platelet-rich plasma in repairing an annulus defect. PLoS ONE. 2017;12:e0171500. doi: 10.1371/journal.pone.0171500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.McGuire R., Borem R., Mercuri J. The fabrication and characterization of a multi-laminate, angle-ply collagen patch for annulus fibrosus repair. J. Tissue Eng. Regen. Med. 2016;11:3488–3493. doi: 10.1002/term.2250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cunha C., Teixeira G.Q., Ribeiro-Machado C., Pereira C.L., Ferreira J.R., Molinos M., Santos S.G., Barbosa M.A., Goncalves R.M. Modulation of the In Vivo Inflammatory Response by Pro-Versus Anti-Inflammatory Intervertebral Disc Treatments. Int. J. Mol. Sci. 2020;21:1730. doi: 10.3390/ijms21051730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kameda T., Zvick J., Vuk M., Sadowska A., Tam W.K., Leung V.Y., Bölcskei K., Helyes Z., Applegate L.A., Hausmann O.N. Expression and Activity of TRPA1 and TRPV1 in the Intervertebral Disc: Association with Inflammation and Matrix Remodeling. Int. J. Mol. Sci. 2019;20:1767. doi: 10.3390/ijms20071767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Huang B.-R., Bau D.-T., Chen T.-S., Chuang I., Tsai C.-F., Chang P.-C., Hsu H.-C., Lu D.-Y. Pro-Inflammatory Stimuli Influence Expression of Intercellular Adhesion Molecule 1 in Human Anulus Fibrosus Cells through FAK/ERK/GSK3 and PKCδ Signaling Pathways. Int. J. Mol. Sci. 2019;20:77. doi: 10.3390/ijms20010077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Stich S., Möller A., Cabraja M., Krüger J.P., Hondke S., Endres M., Ringe J., Sittinger M. Chemokine CCL25 induces migration and extracellular matrix production of anulus fibrosus-derived cells. Int. J. Mol. Sci. 2018;19:2207. doi: 10.3390/ijms19082207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.De Luca P., De Girolamo L., Perucca Orfei C., Viganò M., Cecchinato R., Brayda-Bruno M., Colombini A. Vitamin D’s effect on the proliferation and inflammation of human intervertebral disc cells in relation to the functional vitamin D receptor gene FokI polymorphism. Int. J. Mol. Sci. 2018;19:2002. doi: 10.3390/ijms19072002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chung S.A., Khan S.N., Diwan A.D. The molecular basis of intervertebral disk degeneration. Orthop. Clin. N. Am. 2003;34:209–219. doi: 10.1016/S0030-5898(03)00026-9. [DOI] [PubMed] [Google Scholar]
- 87.de Oliveira C.P., Rodrigues L.M.R., Fregni M.V.V.D., Gotfryd A., Made A.M., da Silva Pinhal M.A. Extracellular matrix remodeling in experimental intervertebral disc degeneration. Acta Ortop. Bras. 2013;21:144. doi: 10.1590/S1413-78522013000300003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fuller E.S., Shu C., Smith M.M., Little C.B., Melrose J. Hyaluronan oligosaccharides stimulate matrix metalloproteinase and anabolic gene expression in vitro by intervertebral disc cells and annular repair in vivo. J. Tissue Eng. Regen. Med. 2018;12:e216–e226. doi: 10.1002/term.2319. [DOI] [PubMed] [Google Scholar]
- 89.Cazzanelli P., Wuertz-Kozak K. MicroRNAs in Intervertebral Disc Degeneration, Apoptosis, Inflammation, and Mechanobiology. Int. J. Mol. Sci. 2020;21:3601. doi: 10.3390/ijms21103601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Masuda K. Biological repair of the degenerated intervertebral disc by the injection of growth factors. Eur. Spine J. 2008;17:441. doi: 10.1007/s00586-008-0749-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wei A., Brisby H., Chung S.A., Diwan A.D. Bone morphogenetic protein-7 protects human intervertebral disc cells in vitro from apoptosis. Spine J. 2008;8:466–474. doi: 10.1016/j.spinee.2007.04.021. [DOI] [PubMed] [Google Scholar]
- 92.Wei A., Williams L.A., Bhargav D., Shen B., Kishen T., Duffy N., Diwan A.D. BMP13 Prevents the Effects of Annular Injury in an Ovine Model. Int. J. Biol. Sci. 2009;5:388–396. doi: 10.7150/ijbs.5.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhou F.Y., Wei A.-Q., Shen B., Williams L., Diwan A.D. Cartilage derived morphogenetic protein-2 induces cell migration and its chondrogenic potential in C28/I2 cells. Int. J. Spine Surg. 2015;9 doi: 10.14444/2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hodgkinson T., Shen B., Diwan A., Hoyland J.A., Richardson S.M. Therapeutic potential of growth differentiation factors in the treatment of degenerative disc diseases. JOR Spine. 2019;2:e1045. doi: 10.1002/jsp2.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bendtsen M., Bunger C., Colombier P., Le Visage C., Roberts S., Sakai D., Urban J.P. Biological challenges for regeneration of the degenerated disc using cellular therapies. Acta Orthop. 2016;87:39–46. doi: 10.1080/17453674.2017.1297916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gruber H.E., Riley F.E., Hoelscher G.L., Ingram J.A., Bullock L., Hanley E.N. Human annulus progenitor cells: Analyses of this viable endogenous cell population. J. Orthop. Res. 2016;34:1351–1360. doi: 10.1002/jor.23319. [DOI] [PubMed] [Google Scholar]
- 97.Stich S., Jagielski M., Fleischmann A., Meier C., Bussmann P., Kohl B., Schmidt J., Krüger J.-P., Endres M., Cabraja M. Degeneration of Lumbar Intervertebral Discs: Characterization of Anulus Fibrosus Tissue and Cells of Different Degeneration Grades. Int. J. Mol. Sci. 2020;21:2165. doi: 10.3390/ijms21062165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Williams L.A., Bhargav D., Diwan A.D. Unveiling the bmp13 enigma: Redundant morphogen or crucial regulator? Int. J. Biolog. Sci. 2008;4:318. doi: 10.7150/ijbs.4.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Razban V., Lotfi A.S., Soleimani M., Ahmadi H., Massumi M., Khajeh S., Ghaedi M., Arjmand S., Najavand S., Khoshdel A. HIF-1α overexpression induces angiogenesis in mesenchymal stem cells. BioRes. Open Access. 2012;1:174–183. doi: 10.1089/biores.2012.9905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Attar M., Arefian E., Nabiuni M., Adegani F.J., Bakhtiari S.H.A., Karimi Z., Barzegar M., Soleimani M. MicroRNA 17–92 expressed by a transposone-based vector changes expression level of cell-cycle-related genes. Cell Biol. Int. 2012;36:1005–1012. doi: 10.1042/CBI20110089. [DOI] [PubMed] [Google Scholar]
- 101.Williams L.A., Wei A., Bhargav D., Diwan A.D. Cartilage derived morphogenetic protein 2 – A potential therapy for intervertebral disc regeneration? Biologicals. 2014;42:65–73. doi: 10.1016/j.biologicals.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 102.Miyazaki S., Diwan A.D., Kato K., Cheng K., Bae W.C., Sun Y., Yamada J., Muehleman C., Lenz M.E., Inoue N., et al. ISSLS PRIZE IN BASIC SCIENCE 2018: Growth differentiation factor-6 attenuated pro-inflammatory molecular changes in the rabbit anular-puncture model and degenerated disc-induced pain generation in the rat xenograft radiculopathy model. Eur. Spine J. 2018;27:739–751. doi: 10.1007/s00586-018-5488-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tendulkar G., Chen T., Ehnert S., Kaps H.P., Nüssler A.K. Intervertebral disc nucleus repair: Hype or hope? Int. J. Mol. Sci. 2019;20:3622. doi: 10.3390/ijms20153622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Soleimani M., Nadri S. A protocol for isolation and culture of mesenchymal stem cells from mouse bone marrow. Nature Protoc. 2009;4:102–106. doi: 10.1038/nprot.2008.221. [DOI] [PubMed] [Google Scholar]
- 105.Brisby H., Tao H., Ma D.D., Diwan A.D. Cell therapy for disc degeneration—potentials and pitfalls. Orthop. Clin. N. Am. 2004;35:85–93. doi: 10.1016/S0030-5898(03)00104-4. [DOI] [PubMed] [Google Scholar]
- 106.Shafiee A., Seyedjafari E., Soleimani M., Ahmadbeigi N., Dinarvand P., Ghaemi N. A comparison between osteogenic differentiation of human unrestricted somatic stem cells and mesenchymal stem cells from bone marrow and adipose tissue. Biotechnol. Lett. 2011;33:1257–1264. doi: 10.1007/s10529-011-0541-8. [DOI] [PubMed] [Google Scholar]
- 107.Nadri S., Soleimani M. Comparative analysis of mesenchymal stromal cells from murine bone marrow and amniotic fluid. Cytotherapy. 2007;9:729–737. doi: 10.1080/14653240701656061. [DOI] [PubMed] [Google Scholar]
- 108.Thorpe A.A., Bach F.C., Tryfonidou M.A., Le Maitre C.L., Mwale F., Diwan A.D., Ito K. Leaping the hurdles in developing regenerative treatments for the intervertebral disc from preclinical to clinical. JOR Spine. 2018;1:e1027. doi: 10.1002/jsp2.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Smith L.J., Silverman L., Sakai D., Le Maitre C.L., Mauck R.L., Malhotra N.R., Lotz J.C., Buckley C.T. Advancing cell therapies for intervertebral disc regeneration from the lab to the clinic: Recommendations of the ORS spine section. JOR Spine. 2018;1:e1036. doi: 10.1002/jsp2.1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sakai D., Schol J. Cell therapy for intervertebral disc repair: Clinical perspective. J. Orthop. Translat. 2017;9:8–18. doi: 10.1016/j.jot.2017.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Werner B.C., Li X., Shen F.H. Stem cells in preclinical spine studies. Spine J. 2014;14:542–551. doi: 10.1016/j.spinee.2013.08.031. [DOI] [PubMed] [Google Scholar]
- 112.Costi J.J., Hearn T.C., Fazzalari N.L. The effect of hydration on the stiffness of intervertebral discs in an ovine model. Clin. Biomech. 2002;17:446–455. doi: 10.1016/S0268-0033(02)00035-9. [DOI] [PubMed] [Google Scholar]
- 113.Wuertz K., Godburn K., Iatridis J.C. MSC response to pH levels found in degenerating intervertebral discs. Biochem. Biophys. Res. Commun. 2009;379:824–829. doi: 10.1016/j.bbrc.2008.12.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Bibby S.R., Jones D.A., Ripley R.M., Urban J.P. Metabolism of the intervertebral disc: Effects of low levels of oxygen, glucose, and pH on rates of energy metabolism of bovine nucleus pulposus cells. Spine. 2005;30:487–496. doi: 10.1097/01.brs.0000154619.38122.47. [DOI] [PubMed] [Google Scholar]
- 115.Hampton D., Laros G., McCarron R., Franks D. Healing potential of the anulus fibrosus. Spine. 1989;14:398–401. doi: 10.1097/00007632-198904000-00009. [DOI] [PubMed] [Google Scholar]
- 116.Key J.A., Ford L.T. Experimental intervertebral-disc lesions. J. Bone Jt. Surg. 1948;30:621–630. doi: 10.2106/00004623-194830030-00009. [DOI] [PubMed] [Google Scholar]
- 117.Smith J., Walmsley R. Experimental incision of the intervertebral disc. J. Bone Jt. Surg. 1951;33:612–625. doi: 10.1302/0301-620X.33B4.612. [DOI] [PubMed] [Google Scholar]
- 118.Benneker L.M., Andersson G., Iatridis J.C., Sakai D., Hartl R., Ito K., Grad S. Cell therapy for intervertebral disc repair: Advancing cell therapy from bench to clinics. Eur. Cell Mater. 2014;27:5–11. doi: 10.22203/eCM.v027sa02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Tan H., Marra K.G. Injectable, biodegradable hydrogels for tissue engineering applications. Materials. 2010;3:1746–1767. doi: 10.3390/ma3031746. [DOI] [Google Scholar]
- 120.Nicodemus G.D., Bryant S.J. Cell encapsulation in biodegradable hydrogels for tissue engineering applications. Tissue Eng. Part B Rev. 2008;14:149–165. doi: 10.1089/ten.teb.2007.0332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Iwasa J., Ochi M., Uchio Y., Katsube K., Adachi N., Kawasaki K. Effects of cell density on proliferation and matrix synthesis of chondrocytes embedded in atelocollagen gel. Artif. Organs. 2003;27:249–255. doi: 10.1046/j.1525-1594.2003.07073.x. [DOI] [PubMed] [Google Scholar]
- 122.Sakai D., Mochida J., Iwashina T., Hiyama A., Omi H., Imai M., Nakai T., Ando K., Hotta T. Regenerative effects of transplanting mesenchymal stem cells embedded in atelocollagen to the degenerated intervertebral disc. Biomaterials. 2006;27:335–345. doi: 10.1016/j.biomaterials.2005.06.038. [DOI] [PubMed] [Google Scholar]
- 123.Sakai D., Mochida J., Yamamoto Y., Nomura T., Okuma M., Nishimura K., Nakai T., Ando K., Hotta T. Transplantation of mesenchymal stem cells embedded in Atelocollagen® gel to the intervertebral disc: A potential therapeutic model for disc degeneration. Biomaterials. 2003;24:3531–3541. doi: 10.1016/S0142-9612(03)00222-9. [DOI] [PubMed] [Google Scholar]
- 124.Alini M., Li W., Markovic P., Aebi M., Spiro R.C., Roughley P.J. The potential and limitations of a cell-seeded collagen/hyaluronan scaffold to engineer an intervertebral disc-like matrix. Spine. 2003;28:446–453. doi: 10.1097/01.BRS.0000048672.34459.31. [DOI] [PubMed] [Google Scholar]
- 125.Vadalà G., Sowa G., Hubert M., Gilbertson L.G., Denaro V., Kang J.D. Mesenchymal stem cells injection in degenerated intervertebral disc: Cell leakage may induce osteophyte formation. J. Tissue Eng. Regen. Med. 2012;6:348–355. doi: 10.1002/term.433. [DOI] [PubMed] [Google Scholar]
- 126.Wan Y., Feng G., Shen F.H., Balian G., Laurencin C.T., Li X. Novel Biodegradable Poly(1,8-octanediol malate) for Annulus Fibrosus Regeneration. Macromol. Biosci. 2007;7:1217–1224. doi: 10.1002/mabi.200700053. [DOI] [PubMed] [Google Scholar]
- 127.Schneider T.O., Mueller S.M., Shortkroff S., Spector M. Expression of α-smooth muscle actin in canine intervertebal disc cells in situ and in collagen-glycosaminoglycan matrices in vitro. J Orthop. Res. 1999;17:192–199. doi: 10.1002/jor.1100170207. [DOI] [PubMed] [Google Scholar]
- 128.Nerurkar N.L., Elliott D.M., Mauck R.L. Mechanics of oriented electrospun nanofibrous scaffolds for annulus fibrosus tissue engineering. J. Orthop. Res. 2007;25:1018–1028. doi: 10.1002/jor.20384. [DOI] [PubMed] [Google Scholar]
- 129.Silva-Correia J., Correia S.I., Oliveira J.M., Reis R.L. Tissue engineering strategies applied in the regeneration of the human intervertebral disk. Biotechnol. Adv. 2013;31:1514–1531. doi: 10.1016/j.biotechadv.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 130.Peroglio M., Grad S., Mortisen D., Sprecher C.M., Illien-Jünger S., Alini M., Eglin D. Injectable thermoreversible hyaluronan-based hydrogels for nucleus pulposus cell encapsulation. Eur. Spine J. 2012;21:839–849. doi: 10.1007/s00586-011-1976-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Nesti L.J., Li W.-J., Shanti R.M., Jiang Y.J., Jackson W., Freedman B.A., Kuklo T.R., Giuliani J.R., Tuan R.S. Intervertebral Disc Tissue Engineering Using a Novel Hyaluronic Acid–Nanofibrous Scaffold (HANFS) Amalgam. Tissue Eng. Part A. 2008;14:1527–1537. doi: 10.1089/ten.tea.2008.0215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Dahia C.L., Iatridis J.C., Risbud M.V. New horizons in spine research: Disc biology, tissue engineering, biomechanics, translational, and clinical research. JOR Spine. 2018;1 doi: 10.1002/jsp2.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Buckley C.T., Hoyland J.A., Fujii K., Pandit A., Iatridis J.C., Grad S. Critical aspects and challenges for intervertebral disc repair and regeneration—Harnessing advances in tissue engineering. JOR Spine. 2018;1:e1029. doi: 10.1002/jsp2.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Martin J.T., Gullbrand S.E., Fields A.J., Purmessur D., Diwan A.D., Oxland T.R., Chiba K., Guilak F., Hoyland J.A., Iatridis J.C. Publication trends in spine research from 2007 to 2016: Comparison of the Orthopaedic Research Society Spine Section and the International Society for the Study of the Lumbar Spine. JOR Spine. 2018;1:e1006. doi: 10.1002/jsp2.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ashish A., Diwan U.C. A Multi-centre, Randomised, Single-Blinded, Twelve-Month Follow-Up Trial to Evaluate the Safety and Effectiveness of the Kunovus Disc Device for the Preservation of Lumbar Disc Form and Function in Patients Undergoing Microdiscectomy for Sciatica due to Lumbar Disc Herniation. [(accessed on 1 March 2020)]; Available online: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=375184&showOriginal=true&isReview=true.
- 136.Fearing B.V., Hernandez P.A., Setton L.A., Chahine N.O. Mechanotransduction and cell biomechanics of the intervertebral disc. JOR Spine. 2018;1:e1026. doi: 10.1002/jsp2.1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Loibl M., Wuertz-Kozak K., Vadala G., Lang S., Fairbank J., Urban J.P. Controversies in regenerative medicine: Should intervertebral disc degeneration be treated with mesenchymal stem cells? JOR Spine. 2019;2:e1043. doi: 10.1002/jsp2.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.D’Este M., Eglin D., Alini M. Lessons to be learned and future directions for intervertebral disc biomaterials. Acta Biomater. 2018;78:13–22. doi: 10.1016/j.actbio.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 139.Dehbari N., Tavakoli J., Khatrao S.S., Tang Y. In situ polymerized hyperbranched polymer reinforced poly (acrylic acid) hydrogels. Mater. Chem. Front. 2017;1:1995–2004. doi: 10.1039/C7QM00028F. [DOI] [Google Scholar]
- 140.Tavakoli J., Amin D.B., Freeman B.J.C., Costi J.J. The Biomechanics of the Inter-Lamellar Matrix and the Lamellae During Progression to Lumbar Disc Herniation: Which is the Weakest Structure? Ann. Biomed. Eng. 2018;46:1280–1291. doi: 10.1007/s10439-018-2056-0. [DOI] [PubMed] [Google Scholar]
- 141.Martin J.T., Milby A.H., Chiaro J.A., Kim D.H., Hebela N.M., Smith L.J., Elliott D.M., Mauck R.L. Translation of an engineered nanofibrous disc-like angle-ply structure for intervertebral disc replacement in a small animal model. Acta Biomater. 2014;10:2473–2481. doi: 10.1016/j.actbio.2014.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Nerurkar N.L., Baker B.M., Sen S., Wible E.E., Elliott D.M., Mauck R.L. Nanofibrous biologic laminates replicate the form and function of the annulus fibrosus. Nature Mater. 2009;8:986. doi: 10.1038/nmat2558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Nerurkar N.L., Sen S., Huang A.H., Elliott D.M., Mauck R.L. Engineered disc-like angle-ply structures for intervertebral disc replacement. Spine. 2010;35:867. doi: 10.1097/BRS.0b013e3181d74414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Jammalamadaka U., Tappa K. Recent advances in biomaterials for 3D printing and tissue engineering. J. Funct. Biomater. 2018;9:22. doi: 10.3390/jfb9010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kim B.S., Kwon Y.W., Kong J.-S., Park G.T., Gao G., Han W., Kim M.-B., Lee H., Kim J.H., Cho D.-W. 3D cell printing of in vitro stabilized skin model and in vivo pre-vascularized skin patch using tissue-specific extracellular matrix bioink: A step towards advanced skin tissue engineering. Biomaterials. 2018;168:38–53. doi: 10.1016/j.biomaterials.2018.03.040. [DOI] [PubMed] [Google Scholar]
- 146.Luo Y., Li Y., Qin X., Wa Q. 3D printing of concentrated alginate/gelatin scaffolds with homogeneous nano apatite coating for bone tissue engineering. Mate. Des. 2018;146:12–19. doi: 10.1016/j.matdes.2018.03.002. [DOI] [Google Scholar]
- 147.Costa J.B., Silva-Correia J., Ribeiro V.P., da Silva Morais A., Oliveira J.M., Reis R.L. Engineering patient-specific bioprinted constructs for treatment of degenerated intervertebral disc. Mater. Today Commun. 2019;19:506–512. doi: 10.1016/j.mtcomm.2018.01.011. [DOI] [Google Scholar]
- 148.Oner T., Cengiz I., Pitikakis M., Cesario L., Parascandolo P., Vosilla L., Viano G., Oliveira J., Reis R., Silva-Correia J. 3D segmentation of intervertebral discs: From concept to the fabrication of patient-specific scaffolds. J. 3D Print. Med. 2017;1:91–101. doi: 10.2217/3dp-2016-0011. [DOI] [Google Scholar]
- 149.Doyle A.D., Yamada K.M. Mechanosensing via cell-matrix adhesions in 3D microenvironments. Exp. Cell Res. 2016;343:60–66. doi: 10.1016/j.yexcr.2015.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Jokinen J., Dadu E., Nykvist P., Kapyla J., White D.J., Ivaska J., Vehvilainen P., Reunanen H., Larjava H., Hakkinen L., et al. Integrin-mediated cell adhesion to type I collagen fibrils. J. Biol. Chem. 2004;279:31956–31963. doi: 10.1074/jbc.M401409200. [DOI] [PubMed] [Google Scholar]
- 151.Kesti M., Müller M., Becher J., Schnabelrauch M., D’Este M., Eglin D., Zenobi-Wong M. A versatile bioink for three-dimensional printing of cellular scaffolds based on thermally and photo-triggered tandem gelation. Acta Biomater. 2015;11:162–172. doi: 10.1016/j.actbio.2014.09.033. [DOI] [PubMed] [Google Scholar]
- 152.Kolesky D.B., Truby R.L., Gladman A.S., Busbee T.A., Homan K.A., Lewis J.A. 3D bioprinting of vascularized, heterogeneous cell-laden tissue constructs. Adv. Mater. 2014;26:3124–3130. doi: 10.1002/adma.201305506. [DOI] [PubMed] [Google Scholar]
- 153.Duan B., Hockaday L.A., Kang K.H., Butcher J.T. 3D bioprinting of heterogeneous aortic valve conduits with alginate/gelatin hydrogels. J. Biomed. Mater. Res. Part A. 2013;101:1255–1264. doi: 10.1002/jbm.a.34420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Chimene D., Lennox K.K., Kaunas R.R., Gaharwar A.K. Advanced bioinks for 3D printing: A materials science perspective. Ann. Biomed. Eng. 2016;44:2090–2102. doi: 10.1007/s10439-016-1638-y. [DOI] [PubMed] [Google Scholar]
- 155.Skardal A., Devarasetty M., Kang H.-W., Mead I., Bishop C., Shupe T., Lee S.J., Jackson J., Yoo J., Soker S. A hydrogel bioink toolkit for mimicking native tissue biochemical and mechanical properties in bioprinted tissue constructs. Acta Biomater. 2015;25:24–34. doi: 10.1016/j.actbio.2015.07.030. [DOI] [PubMed] [Google Scholar]
- 156.Do A.V., Khorsand B., Geary S.M., Salem A.K. 3D printing of scaffolds for tissue regeneration applications. Adv. Healthc. Mater. 2015;4:1742–1762. doi: 10.1002/adhm.201500168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Kokkinis D., Bouville F., Studart A.R. 3D Printing of Materials with Tunable Failure via Bioinspired Mechanical Gradients. Adv. Mater. 2018;30:1705808. doi: 10.1002/adma.201705808. [DOI] [PubMed] [Google Scholar]