Abstract
Background
The current study aimed to assess prevalence of mental disorders during Covid-19 pandemic- and respective lockdown in Germany, and potential behaviors/states that can have protective functions on preventing severe mental problems. Assessing prevalence of mental disorders, as well as to find potential protective variables is very important in order to determine people’s psychological suffering. It provides the basis for teaching possible coping styles in order to prevent a major breakdown on mental health. Prevalence on mental disorders was expected to increase during the pandemic, especially depression, (general-/and health-) anxiety, panic attacks- and disorder, as well as obsessive-compulsive disorder. Additionally, potentially protective variables, such as resilience and coping, were included.
Methods
N = 949 subjects completed an online-survey that asked for symptoms regarding depression, (health) anxiety, panic disorder, obsessive-compulsive disorder, and lock-down related behavior—starting 14 days after lockdown in Germany.
Results
Prevalence of mental disorders in the current sample was much higher than usual prevalence of mental disorders, with 50.6% expressing at least one mental disorder. Resilience was associated with lower risks for any mental disorder (OR = 4.23, p < .0001, 95%CI = 3.21–5.57), as well as with any other measured mental illness (all ORs between = 2.82 for obsessive-compulsive disorder and OR = 41.44 for panic disorder, all p < .001). Similar results were obtained regarding coping (focus on positive).
Conclusion
Results are highly relevant in order to provide a glance on what substantial influence the current pandemic- and lockdown situation has on mental health across the country, and possibly across the world. Possible ways in order to prevent deterioration and help coping with the current situation are being elaborated and discussed.
Introduction
For what is known so far, severe acute respiratory syndrome corona virus 2 (SARS-CoV-2) has begun to spread in Germany since beginning of March 2020. It was first reported of in December 2019 in Wuhan, China [1] and has since then begun to expand across the globe. Whereas most infected people show mild symptoms (≈ 80%), some develop pneumonia (≈ 14%) and/or acute respiratory distress syndrome (ARDS; ≈ 6%, Robert-Koch-Institute, Germany). Eventually many of those severe cases need intensive care [2, 3]. As the virus spreads very fast, many people are being infected in a short time [4].
Because of a possible health-system breakdown after a sudden and substantial increase of patients needing intensive care/intubation, severe restrictions have been put up in most countries facing SARS-CoV-2. In Germany, schools/kindergartens/universities, restaurants, etc. have been closed, and many people are working from home: Public social life has basically stopped existing.
Therefore, providing a first overview of the most prevalent mental health problems at this emergency situation’s early stage will help establishing a targeted support-and treatment-system, and will further allow a prognosis regarding the expected disease-burden for affected societies.
One of the first studies concerning the corona-outbreak and mental health is from Gao et al. [5], reporting high prevalence of mental health problems in China in February 2020: 21.3% of the sample expressed psychological problems/anxiety. Since then, there is a growing body of literature regarding mental health during the COVID-19 outbreak, reporting psychological problems like depressive symptoms, anxiety and decreased quality of sleep in different populations [6–9].
However, most of the available literature only reflects results of mostly Asian countries [9], thus, leaving a need for representative studies also from European- and other areas across the globe–all of which are currently dealing with coronavirus-outbreaks. To our knowledge, no study presenting results of mental health problems with a larger sample in Germany during the Sars-Cov-2 outbreak- and lockdown has been published so far.
In order to assess the current situation's impact on mental health and to be able to respond as quickly as possible, we conducted an online survey on N = 949 participants. We assessed health anxiety/somatoform disorder (HA), general anxiety disorder (GAD), panic disorder (PAD), obsessive-compulsive-disorder (OCD), and depression (DEP). Furthermore, questions regarding life circumstances during the nation’s “lockdown” were measured, as we expected substantial influence of it. Generally, we expected current prevalence of assessed mental disorders to be higher than the usual one in Germany [10]. We considered coping and resilience as behaviors being protective against adverse effects on mental health. Furthermore, in order to reveal emotional and psychological changes throughout the development of the disease, the sample will be longitudinally followed. For what is known so far, severe acute respiratory syndrome corona virus 2 (SARS-CoV-2) has begun to spread in Germany since beginning of March 2020. It was first reported of in December 2019 in Wuhan, China [1] and has since then begun to expand across the globe. Whereas most infected people show mild symptoms (≈ 80%), some develop pneumonia (≈ 14%) and/or acute respiratory distress syndrome (ARDS; ≈ 6%, Robert-Koch-Institute, Germany). Eventually many of those severe cases need intensive care [2, 3]. As the virus spreads very fast, many people are being infected in a short time [4].
Because of a possible health-system breakdown after a sudden and substantial increase of patients needing intensive care/intubation, severe restrictions have been put up in most countries facing SARS-CoV-2. In Germany, schools/kindergartens/universities, restaurants, etc. have been closed, and many people are working from home: Public social life has basically stopped existing. Therefore, providing a first overview of the most prevalent mental health problems at this emergency situation’s early stage will help establishing a targeted support-and treatment-system, and will further allow a prognosis regarding the expected disease-burden for affected societies.
Next, we considered coping and resilience as behaviors being protective against adverse effects on mental health. Resilience refers to positive adaptation, or the ability to preserve or regain mental health, in the face of experiencing difficulties in life [11–14]. Coping is viewed as a response to perceived stress and defined as "constantly changing cognitive and behavioral efforts to manage specific external and/or internal demands that are appraised as taxing or exceeding the resources of the person" ([15], p.141). The way of perceiving and interpreting events and differences in dealing with those have been shown to have different impacts on mental health- an effect that can be found across all ages [12, 16–22]. Furthermore, in order to reveal emotional and psychological changes throughout the development of the disease, the sample will be longitudinally followed.
To allow the health care system to respond as quickly as possible, the current study provides an early overview of the most prevalent mental health problems, and of strategies that proofed to be protective regarding mental health problems. We expect
Higher prevalence of all measured mental disorders in comparison to the usual numbers in Germany [10] (namely DEP, GAD, PAD, HA, and OCD), due to the ongoing threatening, unclear situation
Associations of lockdown related behavior (social isolation, hoarding, worrying) with mental disorders
More resilient people being less affected by the lockdown in regard to mental disorders
Mental health outcomes being differentially associated with coping, especially focusing on positive sides of the situation.
Materials and methods
Design and participants
In order to assess the current situation's impact on mental health and to be able to respond as quickly as possible, we conducted an online survey on N = 949 participants. We assessed health anxiety/somatoform disorder (HA), general anxiety disorder (GAD), panic disorder (PAD), obsessive-compulsive-disorder (OCD), and depression (DEP). Furthermore, questions regarding life circumstances during the nation’s “lockdown” were measured, as we expected substantial influence of it. Generally, we expected current prevalence of assessed mental disorders to be higher than the usual one in Germany [10].
This cross-sectional data come from the first wave of a prospective online-survey conducted between March 27th and April 3rd, 2020. A link to the survey was posted on social media, and sent via university e-mail to members of Justus-Liebig University of Giessen, Germany (with the request to answer some questions regarding consequences of the Covid-19 pandemic). In total, 949 participants completed the survey. Subjects were asked if they agreed to participate in a follow-up study, and if agreeing, asked to leave their e-mail-address in order to be contacted again. Data and email-addresses were stored separately from each other in order to guarantee anonymous responding. All participants gave their informed consent prior to the online poll. The study complies with the Declaration of Helsinki and is in accordance with the ethical standards of the institutional-and/or national research commitment.
Measurements
Environmental- and social circumstances regarding SARS-CoV-2
We assessed demographic information regarding subjects’ age and occupation, their living- and family situation, corona-related fears- and worries (current and those about the future). Furthermore, social behavior regarding new rules in times of the pandemic and a new way of thinking- and feeling since the virus’ massive spreading was assessed.
Behavioral items regarding Corona (BCI)
As we came up with the questions regarding the SARS-CoV-2 pandemic ourselves, we calculated reliabilities for those items, in order to proof internal consistency. Furthermore, we calculated a factor analysis in order to be able to cluster items into higher order factors and to be able to associate those higher order factors with SMU as well as with factors that we expected to be protective from mental disorders, such as resilience, and coping strategies.
Therefore, a principal component analysis (PCA) with VARIMAX rotation was calculated (Eigenvalue > 1, maximum iteration: 25, loading > .4), containing 21 items that asked about behavior during the outbreak of SARS-CoV-2 in Germany as well as during the lockdown. Kaiser, Meyer and Olkin (KMO)—value was .785, and, therefore, acceptable in order to calculate the PCA. Four factors were extracted: 1) Social Distancing (not meeting many people, keeping distance, etc.), 2) Hoarding, 3) Global future anxiety (anxiety about the nation’s future and global future), and 4) Hygienic measures (washing hands more often with soap-and disinfectant, rumination about germs).
Mental health
Assuming which psychiatric symptoms might currently be most prevalent, we decided to focus on DEP, HA, GAD, panic attacks and PAD, as well as OCD. Regarding DEP, we used the German Version of the Beck-Depression-Inventory [23, 24]. Cut-off for a clinical depression measured with the BDI-II was divided into “any DEP” (BDI-score starting from 13) and another variable, indicating “severe/major DEP” with a BDI-II-score higher than 28. PAD and GAD were assessed with the German version of the Primary- Health-Questionnaire [25, 26], HA with the German version of the Short Health Anxiety Inventory [27, 28], and obsessive-compulsive symptoms with the German version of the Obsessive-Compulsive Inventory-Revised [29, 30].
For OCD, the cut-off was set to 21 in accordance with Foa and colleagues [29]. Concerning HA, subjects above one SD of the current samples’ mean, were classified as highly health-anxious, as no clear cut-off is given in scientific literature [28, 31].
Protective factors
As we were, furthermore, interested in which way coping styles, resilience, and well-being might be associated with mental health outcome during stressful circumstances, we assessed those as well using the German version of the brief resilience scale [32, 33], and of the WHO-5 well-being index [34]. Coping styles were recorded with the brief COPE [35, 36]. It assesses four main coping styles, while we focused on “Positive Focus” in the current study. Furthermore, personality dimensions were measured [37], however, results will not be reported here. Instructions of scales (except resilience and personality) were adapted to “during the past two weeks” in order to ensure a focus on the current SARS-CoV-2 situation in Germany.
Statistical analysis
Descriptive statistics were analyzed regarding distribution of age, gender, life situation, occupation, social media use, corona exposition and worries regarding consequences of the Covid-19 pandemic.
Variables for psychiatric disorders were transferred into dichotomous variables in dependence of absence or presence of the respective disease, and frequencies assessed. In order to assess Resilience, and Coping Styles in association, variables were median-splitted and Odd’s Ratios (ORs) were calculated.
In case of multiple testing, Bonferroni correction for multiple comparisons was applied. Significant results are reported only if they survived this correction. For data analysis, SPSS Statistics 26 (IBM Corp., Somer, N.Y., USA) was used.
ANOVAs were calculated in order to detect differences of BCI in people with- and without mental disorders.
Results
Descriptive statistics
N = 949 subjects participated in the study. They were on average 28.9 years old (SD± 10.8), 79.5% (n = 754) female, 19.9% (n = 189) male, and 0.6% (n = 6) non-binary. More detailed descriptive results are presented in Table 1.
Table 1. Total numbers (N) and frequencies (percentage) of various demographic variables in the underlying sample of N = 949 participants.
| No. | % | |
|---|---|---|
| Gender | ||
| Female | 754 | 79.5 |
| Male | 189 | 19.9 |
| Non-binary | 6 | 0.6 |
| Occupational status | ||
| Student | 596 | 62.8 |
| Office worker | 251 | 26.4 |
| Officials | 25 | 2.6 |
| Self-Employed | 12 | 1.3 |
| Other | 46 | 4.8 |
| Unemployed | 9 | 0.9 |
| Relationship status | ||
| Single | 349 | 36.8 |
| Married | 147 | 15.5 |
| Relationship | 428 | 45.1 |
| Other | 25 | 2.7 |
| Living Situation | ||
| Alone | 148 | 15.6 |
| Shared flat | 178 | 18.8 |
| With spouse/partner | 266 | 28.0 |
| With partner and children | 89 | 9.4 |
| With partner, children elsewhere | 8 | 0.8 |
| Without partner, with children | 13 | 1.4 |
| With parents/grandparents | 247 | 26.0 |
| Corona-related variables | ||
| Currently in quarantine | 31 | 3.3 |
| Diagnosed with Covid-19 | 3 | 0.3 |
| With Covid-19 diagnosed family member | 56 | 5.9 |
| Caring for someone with Covid-19 | 269 | 28.3 |
Prevalence of mental disorders
Overall, prevalence of suffering from any of the measured mental disorders was 50.6% (N = 480). Therefore, half of the sample’s subjects were suffering from at least one disease. Regarding specific mental disorders, 35.3% expressed clinically depressive symptoms (BDI-Score > 13), 12.0% met the criteria of GAD, 5.4% those of a PAD. 21.4% experienced clinically obsessive-compulsive symptoms (OCI-Score >21) and 17.4% had above average HA-scores and can, therefore, be classified being highly health-anxious in the direction to somatoform disorder. Data regarding 12-month-prevalence of psychiatric diseases in the German population before this pandemic [10] report the following: 7.7% depression rate, 2.2% for GAD, 2.0% for PAD, 3.6% for OCD, and 3.5% for somatoform disorders. Numbers in our sample are much higher, and might already show trends towards public’s future problems after this emergency situation is over. No significant differences between genders were evident in this sample. Results are depicted in Table 2. More detailed tables of sociodemographic variables and prevalence of mental disorders are provided in the S1 File.
Table 2. 12-month-prevalence of various mental disorders in Germany before the Covid-19 pandemic, and prevalence assessed during the lockdown in total numbers (No.) and frequencies (%).
| 12-month-prevalence Germany [10], N = 4484 | Observed Prevalence current sample, N = 949 | ||||
|---|---|---|---|---|---|
| % | 95% CI | No. | % | 95% CI | |
| Any Mental Disorder | 27.7 | [26.3–29.2] | 480 | 50.6 | [47.4–53.7] |
| Any Depression | 7.7 | [6.9–8.6] | 335 | 35.3 | [32.1–38.4] |
| General Anxiety Disorder | 2.2 | [1.8–2.8] | 114 | 12.0 | [9.9–14.1] |
| Panic Disorder | 2.0 | [1.6–2.5] | 51 | 5.4 | [4.0–6.8] |
| Obsessive Compulsive Disorder | 3.6 | [3.1–4.4] | 203 | 21.4 | [18.8–24.0] |
| Somatoform Disorder (Health anxiety) | 3.5 | [2.9–4.1] | 165 | 17.4 | [15.0–19.8] |
Annotations: CI = Confidence Interval
Behavior during the lockdown and mental disorders
Analyzes of variance regarding measured mental disorders revealed that subjects with PAD differed significantly in their Social distancing behavior, F(1, 947) = 10.24, p = .001, as did subjects with GAD, F(1, 947) = 14.95, p < .001. Subjects with high HA scored higher on Social Distancing, F(1, 947) = 29.87, p < .001, as well as Hoarding, F(1, 947) = 16.33, p < .001. Differences in subjects with OCD showed a trend toward Social Distancing, which did, however, not withstand correction for multiple comparisons, F(1, 947) = 6.40, p = .012. Depressive subjects did not differ from non-depressive ones regarding lockdown-related behavior (all p > .10). Hygienic measures were not associated with any mental disorder.
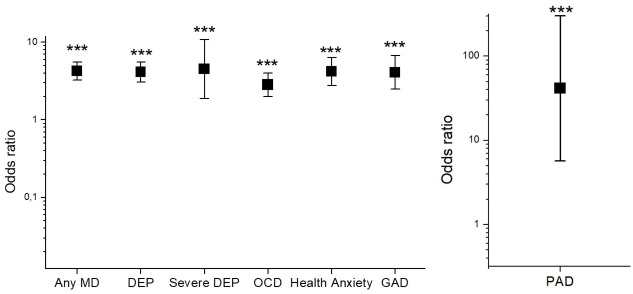
Protective factors
Regarding Resilience, analysis revealed higher Resilience in men compared to women, t = 4.83, p < .001, and a small positive correlation between age and Resilience, r = .09, p = .004. More resilient subjects had lower risks for all tested mental diseases: ORs for depression were lower in resilient subjects (OR = 4.12, p < .0001, 95% CI = 3.49–5.57), also for severe(major) depression (OR = 4.49, p < .0001, 95% CI = 1.86–10.80), PAD (OR = 41.44, p = .0002, 95% CI = 5.7–301.34), OCD (OR = 2.82, p < .0001, 95% CI = 1.98–4.00), HA (OR = 4.18, p < .0001, 95% CI = 2.75–6.73), as well as for GAD (OR = 4.07, p < .0001, 95% CI = 2.47–6.73). OR for any mental disorder in association with Resilience was 4.23, p < .0001, 95% CI = 3.21–5.57). Results are shown in Fig 1 below.
Fig 1. Odds ratios (log-scaled) of different mental disorders in association with resilience during Covid-19 pandemic in Germany.
Any MD = Any mental disorder, HA = Health anxiety, PAD = Panic Disorder, GAD = General Anxiety Disorder, OCD = Obsessive Compulsive Disorder, DEP = Depression, Sev DEP = severe Depression. **p < .01, ***p < .001.
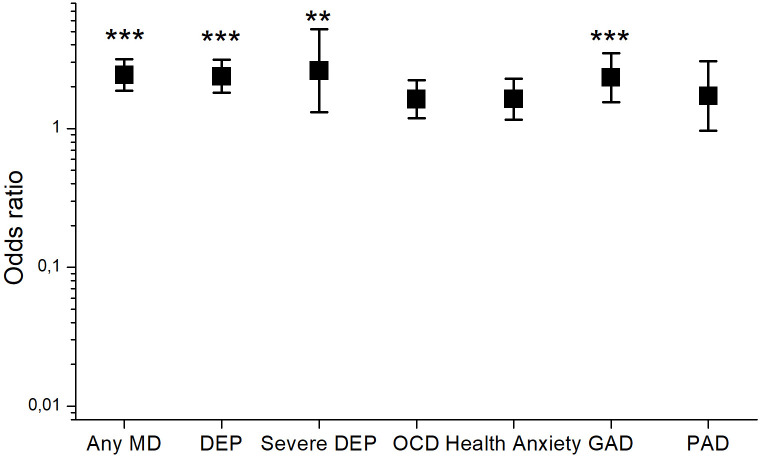
Regarding Coping Styles, Positive Focus was associated with lower risks for depression, (OR = 2.37, p < .0001, 95% CI = 1.80–3.12), severe(major) depression (OR = 2.61, p = .0063, 95% CI = 1.31–5.91), GAD (OR = 2.32, p < .0001, 95% CI = 1.54–3.49), and also with lower risks for any MD (OR = 2.43, p < .0001, 95% CI = 1.87–3.16). ORs were neither significantly different towards PAD (OR = 1.71, p = .066, 95%CI = .96–3.05), nor HA (OR = 1.63, p = .0048, 95% CI = 1.16–2.28), nor OCD (1.62, p = .0024, 95% CI = 1.18–2.22). Results are illustrated in Fig 2 below.
Fig 2. Odds ratios (log-scaled) of different mental disorders in association with coping style “Positive Focus” (PF) during Covid-19 pandemic in Germany.
Any MD = Any mental disorder, HA = Health anxiety, PAD = Panic Disorder, GAD = General Anxiety Disorder, OCD = Obsessive Compulsive Disorder, DEP = Depression, Sev DEP = severe Depression. **p < .01, ***p < .001.
Discussion
This study assessed the latest prevalence of various mental disorders during Covid-19 outbreak in Germany, and examined possible variables that could serve as protection against severe mental health problems, such as resilience and coping in N = 949 people:
Prevalence of depression, obsessive-compulsive disorder, panic- and general anxiety disorder were significantly higher than general national data reported on prevalence before the Covid-19 pandemic [10], indicating that the ongoing situation puts people under severe psychological stress: This needs to be monitored and demands immediate support to be established. Results are in line with data on prevalence regarding other major life threatening events, such as the Ebola outbreak, the Tsunami, or 9/11 [38–41] as well as with most recent data on mental health problems in China during the Covid-19 outbreak [5]. Especially prevalence of depression, with more than a third (35.3%) of the sample suffering from it, as well as GAD, PAD and OCD are alarming and already portrait a picture of which problems are going to occur after the lockdown is over, or if it is continuing for a longer time. This study presents a very early picture of general mental health during the first weeks of the pandemic situation in Europe–at least of those who completed our survey. Therefore, these data are also very important for future prognoses and could be relevant for considerations regarding how long the lockdown should go on or at what time maybe other options/solutions should be taken under consideration. As all the considerations are matters of “pros and cons”, mental health and well-being of a whole state should also be monitored and not to be left aside. If this situation should go on for a longer time, for example App-based therapeutic interventions could be helpful, as well as monitoring of mental health, in order to be able to intervene if symptoms deteriorate.
Our study was conducted at a relatively early phase of the lock-down in Germany (starting one week after the measurements were being effective, on March 27th 2020). Specific government policies, e.g. compulsory mask wearing in public areas and stores, were introduced and obligatory around six weeks after the survey ended. Therefore, effects of mandatory mask wearing on studied mental problems cannot be reported here.
Therefore, future work should evaluate long-term mental health consequences of different government policies by comparing results from different countries and assessing associations with e.g. timing of specific legal requirements, risk communication, duration of lock-down and possible mental health interventions. We did, however, observe associations between mental health and corona-related behaviors such as social-distancing and hoarding. As Garbe and colleagues [42] reported associations of personality and stockpiling as well, these factors should be considered by policy makers—as they could be crucial for controlling the pandemic [43]. For example, Rieger [44] determined judgement anxiety as a factor that is related to compliance to wear masks in Germany and gave important recommendations how to address specific target groups in order to increase mask wearing and compliance. Also, in times of protective equipment shortage, thoughtful risk communication is required to ensure supply for healthcare workers and prevent people from hoarding [45]. Furthermore, psychological aspects like mental health problems, as well as discrimination and stigma which might arise due to infection or quarantine, should directly be addressed by politicians via broadcasts, social media and other online services in order to prevent more social isolation and increase of mental health problems [46, 43].
Furthermore, it is crucial to study factors, which are possibly protective against mental disorders, in order to be able to inform the population about possible ways to cope with the situation and to suffer less. We found out that 1) resilient subjects were less likely to suffer from any mental disorder, and 2) that focusing on positive situational aspects as coping style was associated with lower risks for depression, GAD, and HA. Especially the risk for panic disorder was substantially higher in low resilient subjects. Training of resilience in subjects prone to panic attacks could potentially prevent those from developing a PAD. This could be a very powerful starting point in dealing with impact of Covid-19 on mental health:
There are several online interventions that focus on improving resilience and coping styles [47, 48], also designed at times of facing traumatic events [49]. Such interventions could be very helpful for the current situation, as they can be done online-, and, therefore, made available to a great audience. These could prevent further deterioration or development of mental disorders [47]. Interventions could also be adapted to groups being particularly affected by the pandemic such as healthcare workers [50], or chronically ill, as it was done e.g. during/after SARS [51].
Limitations of the study
This study assessed 949 subjects in Germany within one week (March 27th-April 3rd 2020). Although this is a comparatively high number, several limitations have to be addressed: Mean age of our sample was 28.97 years, with 62.8% students, and in total a sample with higher education (43.1% with university degree), hence, also with a higher socio-economic status (SES). Whereas this reduces the representativeness of the sample, it can also be assumed that prevalence in the broader population is even higher, as SES is a mediator for physiological and mental health [52] with lower prevalence alongside higher SES [10]. Whereas Jacobi and colleagues [10] used a structured clinical interview to assess prevalence, online-questionnaires were used here. Therefore, our prevalence-estimations might not be as accurate as those [10], although applied questionnaires are validated and clinically broadly used. As the purpose of the study was to catch a glance of what is happening to the population during this pandemic on a mental health level, online questionnaires where the only realizable solution. Nonetheless, our data are congruent with latest prevalence rates during the Covid-19 outbreak in China [5]. While the use of questionnaires specifically designed for COVID-19 would have been preferable, such measurements had not been published by the time our study was conducted (March 27th and April 3rd, 2020). Fortunately, new measurements have been developed and validated [7, 53–55].
Moreover, observed effects do not reveal causal relationships, as this is a cross-sectional study and we do not directly have a baseline of mental health issues before the survey. Nevertheless, participants are going to be observed longitudinally, and, therefore, it will be possible to make more clear inferences on causal relationships later on.
Conclusion
To our knowledge, this is the first study in Germany portraying and revealing the severe impact of Covid-19 on the society—not only as a direct physiological, but also as a psychological burden. It is, therefore, crucial to monitor the development of reported prevalence and to find possible treatment solutions for a country (or a world) after the pandemic is “under control”. Furthermore, economic consequences of the pandemic might deteriorate the psychiatric states even further. It is not only substantial to have enough ICU-equipment, it is also crucial to care for the traumatized people after the outbreak, and to provide the necessary infrastructure. In order to observe the development of addressed mental health issues, longitudinal observation/assessment of the participants will show if symptoms deteriorated or improved.
Supporting information
(DOCX)
(SAV)
Acknowledgments
We would like to thank the subjects for participating in this study.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Tang X, Wu C, Li X, Song Y, Yao X, Wu X et al. On the origin and continuing evolution of SARS-CoV-2. Natl Sci Rev 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sun J, He W-T, Wang L, Lai A, Ji X, Zhai X et al. COVID-19: Epidemiology, Evolution, and Cross-Disciplinary Perspectives. Trends Mol Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med 2020; 8(4):420–2. 10.1016/S2213-2600(20)30076-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19).; 2020 [cited 2020 Apr 3]. URL: https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
- 5.Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S et al. Mental Health Problems and Social Media Exposure During COVID-19 Outbreak. SSRN Journal 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen C-Y, Chen I-H, O’Brien K, Latner JD, Lin C-Y. Psychological distress and internet-related behaviors between schoolchildren with and without overweight during the COVID-19 outbreak 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahorsu DK, Imani V, Lin C-Y, Timpka T, Broström A, Updegraff JA et al. Associations Between Fear of COVID-19, Mental Health, and Preventive Behaviours Across Pregnant Women and Husbands: An Actor-Partner Interdependence Modelling. International Journal of Mental Health and Addiction 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res 2020; 288:112954 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr 2020; 52:102066 10.1016/j.ajp.2020.102066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jacobi F, Höfler M, Strehle J, Mack S, Gerschler A, Scholl L et al. Psychische Störungen in der Allgemeinbevölkerung: Studie zur Gesundheit Erwachsener in Deutschland und ihr Zusatzmodul Psychische Gesundheit (DEGS1-MH). Nervenarzt 2014; 85(1):77–87. 10.1007/s00115-013-3961-y [DOI] [PubMed] [Google Scholar]
- 11.Davydov DM, Stewart R, Ritchie K, Chaudieu I. Resilience and mental health. Clin Psychol Rev 2010; 30(5):479–95. 10.1016/j.cpr.2010.03.003 [DOI] [PubMed] [Google Scholar]
- 12.Fletcher D, Sarkar M. Psychological Resilience. European Psychologist 2013; 18(1):12–23. [Google Scholar]
- 13.Herrman H, Stewart DE, Diaz-Granados N, Berger EL, Jackson B, Yuen T. What is resilience? Can J Psychiatry 2011; 56(5):258–65. 10.1177/070674371105600504 [DOI] [PubMed] [Google Scholar]
- 14.Wald J, Taylor S, Asmundson GJ, Jang KL, Stapleton J. Literature review of concepts: Psychological resiliency. BRITISH COLUMBIA UNIV VANCOUVER; 2006.
- 15.Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer publishing company; 1984. [Google Scholar]
- 16.Campbell-Sills L, Cohan SL, Stein MB. Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behav Res Ther 2006; 44(4):585–99. 10.1016/j.brat.2005.05.001 [DOI] [PubMed] [Google Scholar]
- 17.Steptoe A, Dockray S, Wardle J. Positive affect and psychobiological processes relevant to health. J Pers 2009; 77(6):1747–76. 10.1111/j.1467-6494.2009.00599.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu G, Feder A, Cohen H, Kim JJ, Calderon S, Charney DS et al. Understanding resilience. Front Behav Neurosci 2013; 7:10 10.3389/fnbeh.2013.00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zimmer-Gembeck MJ, Skinner EA. The Development of Coping: Implications for Psychopathology and Resilience In: Cicchetti D, editor. Developmental psychopathology. Third edition Hoboken, New Jersey: John Wiley & Sons, Inc; 2016-. p. 1–61. [Google Scholar]
- 20.Aspinwall LG, Taylor SE. A stitch in time: self-regulation and proactive coping. Psychol Bull 1997; 121(3):417–36. 10.1037/0033-2909.121.3.417 [DOI] [PubMed] [Google Scholar]
- 21.Austenfeld JL, Stanton AL. Coping through emotional approach: a new look at emotion, coping, and health-related outcomes. J Pers 2004; 72(6):1335–63. 10.1111/j.1467-6494.2004.00299.x [DOI] [PubMed] [Google Scholar]
- 22.Boxer P, Sloan-Power E, Schappell IMAA. Coping with stress, coping with violence: Links to mental health outcomes among at-risk youth. J Psychopathol Behav Assess 2012; 34(3):405–14. 10.1007/s10862-012-9285-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess 1996; 67(3):588–97. 10.1207/s15327752jpa6703_13 [DOI] [PubMed] [Google Scholar]
- 24.Hautzinger M, Keller F, Kühner C. BDI-II. Beck-Depressions-Inventar. [Revision.]. 2nd ed Frankfurt: Pearson Assessment; 2009. [Google Scholar]
- 25.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999; 282(18):1737–44. 10.1001/jama.282.18.1737 [DOI] [PubMed] [Google Scholar]
- 26.Löwe B, Spitzer RL, Herzog W. Gesundheitsfragebogen für Patienten (PHQ D). Komplettversion und Kurzform. [Testmappe mit Manual, Fragebögen, Schablonen.]. 2nd ed. Karlsruhe: Phizer; 2002.
- 27.Salkovskis PM, Rimes KA, Warwick HMC, Clark DM. The Health Anxiety Inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol Med 2002; 32(5):843–53. 10.1017/s0033291702005822 [DOI] [PubMed] [Google Scholar]
- 28.Bailer J, Witthöft M. Deutsches modifiziertes Health Anxiety Inventory (MK-HAI); 2006.
- 29.Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G et al. The Obsessive-Complusive Inventory: Development and validation of a short version. Psychol Assess 2002; 14(4):485–95. [PubMed] [Google Scholar]
- 30.Gönner S, Leonhart R, Ecker W. Das Zwangsinventar OCI-R—die deutsche Version des Obsessive-Compulsive Inventory-Revised—Ein kurzes Selbstbeurteilungsinstrument zur mehrdimensionalen Messung von Zwangssymptomen. Psychother Psychosom Med Psychol 2007; 57(9–10):395–404. 10.1055/s-2007-970894 [DOI] [PubMed] [Google Scholar]
- 31.Alberts NM, Hadjistavropoulos HD, Jones SL, Sharpe D. The Short Health Anxiety Inventory: a systematic review and meta-analysis. J Anxiety Disord 2013; 27(1):68–78. 10.1016/j.janxdis.2012.10.009 [DOI] [PubMed] [Google Scholar]
- 32.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med 2008; 15(3):194–200. 10.1080/10705500802222972 [DOI] [PubMed] [Google Scholar]
- 33.Chmitorz A, Wenzel M, Stieglitz R-D, Kunzler A, Bagusat C, Helmreich I et al. Population-based validation of a German version of the Brief Resilience Scale. PLoS ONE 2018; 13(2):e0192761 10.1371/journal.pone.0192761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WHO. Wellbeing Measures in Primary Health Care/The Depcare Project. Copenhagen: WHO Regional Office for Europe; 1998.
- 35.Knoll N, Rieckmann N, Schwarzer R. Coping as a mediator between personality and stress outcomes: a longitudinal study with cataract surgery patients. Eur J Pers 2005; 19(3):229–47. [Google Scholar]
- 36.Carver CS. You want to measure coping but your protocol's too long: consider the brief COPE. Int J Behav Med 1997; 4(1):92–100. 10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- 37.Rammstedt B, John OP. Measuring personality in one minute or less: A 10-item short version of the Big Five Inventory in English and German. J Res Pers 2007; 41(1):203–12. [Google Scholar]
- 38.Shultz JM, Baingana F, Neria Y. The 2014 Ebola outbreak and mental health: current status and recommended response. JAMA 2015; 313(6):567–8. 10.1001/jama.2014.17934 [DOI] [PubMed] [Google Scholar]
- 39.van Griensven F, Chakkraband MLS, Thienkrua W, Pengjuntr W, Lopes Cardozo B, Tantipiwatanaskul P et al. Mental health problems among adults in tsunami-affected areas in southern Thailand. JAMA 2006; 296(5):537–48. 10.1001/jama.296.5.537 [DOI] [PubMed] [Google Scholar]
- 40.Chandra V, Pandav R, Bhugra D. Mental health and psychosocial support after the tsunami: observations across affected nations. Int Rev Psychiatry 2006; 18(3):205–11. 10.1080/09540260600655805 [DOI] [PubMed] [Google Scholar]
- 41.Updegraff JA, Silver RC, Holman EA. Searching for and finding meaning in collective trauma: results from a national longitudinal study of the 9/11 terrorist attacks. J Pers Soc Psychol 2008; 95(3):709–22. 10.1037/0022-3514.95.3.709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Garbe L, Rau R, Toppe T. Influence of perceived threat of Covid-19 and HEXACO personality traits on toilet paper stockpiling. PLoS ONE 2020; 15(6):e0234232 10.1371/journal.pone.0234232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lin M-W, Cheng Y. Policy actions to alleviate psychosocial impacts of COVID-19 pandemic: Experiences from Taiwan. Soc Health Behav 2020; 3(2):72. [Google Scholar]
- 44.Rieger M. To wear or not to wear? Factors influencing wearing face masks in Germany during the COVID-19 pandemic. Soc Health Behav 2020; 3(2):50. [Google Scholar]
- 45.Shrivastava S, Shrivastava P. COVID-19 pandemic: Responding to the challenge of global shortage of personal protective equipment. Soc Health Behav 2020; 3(2):70. [Google Scholar]
- 46.Lin C-Y. Social reaction toward the 2019 novel coronavirus (COVID-19). Soc Health Behav 2020; 3(1):1. [Google Scholar]
- 47.Herrero R, Mira A, Cormo G, Etchemendy E, Baños R, García-Palacios A et al. An Internet based intervention for improving resilience and coping strategies in university students: Study protocol for a randomized controlled trial. Internet Interv 2019; 16:43–51. 10.1016/j.invent.2018.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jung Y-H, Ha TM, Oh CY, Lee US, Jang JH, Kim J et al. The Effects of an Online Mind-Body Training Program on Stress, Coping Strategies, Emotional Intelligence, Resilience and Psychological State. PLoS ONE 2016; 11(8):e0159841 10.1371/journal.pone.0159841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hirai M, Clum GA. An Internet-based self-change program for traumatic event related fear, distress, and maladaptive coping. J Trauma Stress 2005; 18(6):631–6. 10.1002/jts.20071 [DOI] [PubMed] [Google Scholar]
- 50.Maunder RG, Lancee WJ, Mae R, Vincent L, Peladeau N, Beduz MA et al. Computer-assisted resilience training to prepare healthcare workers for pandemic influenza: a randomized trial of the optimal dose of training. BMC Health Serv Res 2010; 10:72 10.1186/1472-6963-10-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ng SM, Chan THY, Chan CLW, Lee AM, Yau JKY, Chan CHY et al. Group debriefing for people with chronic diseases during the SARS pandemic: Strength-Focused and Meaning-Oriented Approach for Resilience and Transformation (SMART). Community Ment Health J 2006; 42(1):53–63. 10.1007/s10597-005-9002-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sternthal MJ, Williams DR, Musick MA, Buck AC. Depression, anxiety, and religious life: a search for mediators. J Health Soc Behav 2010; 51(3):343–59. 10.1177/0022146510378237 [DOI] [PubMed] [Google Scholar]
- 53.Lee SA. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Stud 2020; 44(7):393–401. 10.1080/07481187.2020.1748481 [DOI] [PubMed] [Google Scholar]
- 54.Lee SA. How much "Thinking" about COVID-19 is clinically dysfunctional? Brain Behav Immun 2020; 87:97–8. 10.1016/j.bbi.2020.04.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sakib N, Bhuiyan AIM, Hossain S, Al Mamun F, Hosen I, Abdullah AH et al. Psychometric validation of the Bangla Fear of COVID-19 Scale: Confirmatory factor analysis and Rasch analysis. International Journal of Mental Health and Addiction 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(SAV)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.