Abstract
a). Purpose of review
The purpose of this systematic review was to characterize the studies published on grief interventions for bereaved older adults in the last 5 years. Grief intervention studies were included that exclusively focused on older adults as well as those that included older adults in their samples, in order to summarize the most up-to-date treatment options available for bereaved older adults.
b). Recent findings
Twenty-four articles that investigated grief interventions in older adults were identified. Generally, findings suggest viable treatment approaches for bereaved older adults are those incorporating behavioral activation and guidance on restoration-oriented coping. However, similar to studies of broader adult populations, grief interventions had small effects on grief-related symptoms in older adults. Few studies examined age as a moderator of treatment effects. Studies varied greatly by study design, sample size, and outcomes measured, which all likely impacted the efficacy of results.
c). Summary
This review suggests that, while there has been a growing focus on older adults, who have unique vulnerabilities in bereavement, the evidence-base of efficacious interventions for this population is limited. Given the need for specialized bereavement support for older adults will increase in the coming years, future research should prioritize rigorous investigations of grief treatment options leveraging technology to increase access and incorporate techniques that enhance engagement in life and connectedness for this vulnerable population.
Keywords: bereavement, grief, geriatric, psychotherapy, interventions, review
Introduction
Older adults (OAs) are likely to experience multiple significant losses as they age [1, 2]. It is often assumed that, because the likelihood of bereavement increases with age, OAs are naturally equipped to adapt to loss. However, a significant subset are at high risk for experiencing debilitating mental health challenges in bereavement [3], such as prolonged grief disorder (PGD) [4, 5], depression [6, 7], anxiety [8, 9], posttraumatic stress disorder (PTSD) [10], existential distress [11, 12], and loneliness [13, 14]. The prevalence of bereavement-related psychological disorders in OAs varies, with approximately 9–25% of bereaved OAs developing PGD [15, 5, 16], 15% experiencing depressive symptoms [6, 17], 20% anxiety symptoms [18], and 9–16% experiencing bereavement-related PTSD [10, 19, 20]. These bereavement-related psychiatric disorders often co-occur and have been linked to numerous negative physical health outcomes [21], including cognitive decline [22–25], vascular disease [26], hospitalizations and over- or under-use of healthcare services [27, 28], suicide [29, 22, 30], and mortality [31, 32].
Numerous factors may contribute to OAs’ heightened risk for negative bereavement outcomes, including changes in social [33, 34], financial [22, 35], and practical support [36]; isolation and loneliness [37, 38, 14]; and potentially simultaneously coping with pre-existing chronic illness [39], reduced mobility [40], and cognitive decline [41]. OA caregivers of OAs with a chronic or life-limiting disease such as Alzheimer’s, dementia, or cancer are at particular risk for bereavement complications [42, 43]. Despite this, few bereavement interventions have demonstrated efficacy in treating grief symptomatology in OAs [44, 45].
To put this in context, prior reviews have suggested that, in general, grief interventions have marginal efficacy in broader adult populations [46, 47], and the majority of grief intervention reviews have not focused on OAs. A recent meta-analysis of grief interventions found that age moderated treatment effects, with mean older age associated with larger effects at follow up time points [46]. A systematic review [47] of grief interventions for adults, including OAs, found that Complicated Grief Treatment (CGT) [48] and Family Focused Grief Therapy [49] were the most efficacious in reducing complicated grief (similar to prolonged grief). Only a single review focused specifically on grief interventions for OAs, identifying three treatment modalities tested in OA bereaved spouses: emotional expression/support, psychoeducation, and a mind-body approach [44], with only the mind-body intervention demonstrating efficacy [44]. Although valuable, this review was completed in 2013 and was limited by solely reviewing interventions for spousal loss [44] and not other types of losses. The purpose of the present systematic review, therefore, was to characterize grief intervention studies published in the last 5 years and to include interventions targeting all types of losses (e.g., spouse, child, sibling) for OAs.
Method
Search Strategy
All procedures were conducted according to guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) criteria [50]. On January 25, 2019, a comprehensive electronic literature search was conducted in the following five databases: Medline (PubMed), Embase.com, CINAHL (EBSCO), PsycInfo (Ovid), and the Cochrane Library (Wiley). Results were restricted to items in English published from January 1, 2009 to the search date. The search was designed in PubMed using MeSH subject headers and keywords, and then translated to other databases.
Three concepts were combined in the search strategy using the AND operator: seniors (e.g., aged, geriatrics, elder, older adult); grief (e.g., attitude to death, bereavement, grief); and interventions (e.g., mental health services, social support, counseling, initiative, program, therapeutic). Results were compiled using the citation management tool EndNote and duplicates were removed following the Bramer method [51]. For a complete strategy, see the accompanying PubMed search displayed in Appendix A.
Selection Strategy
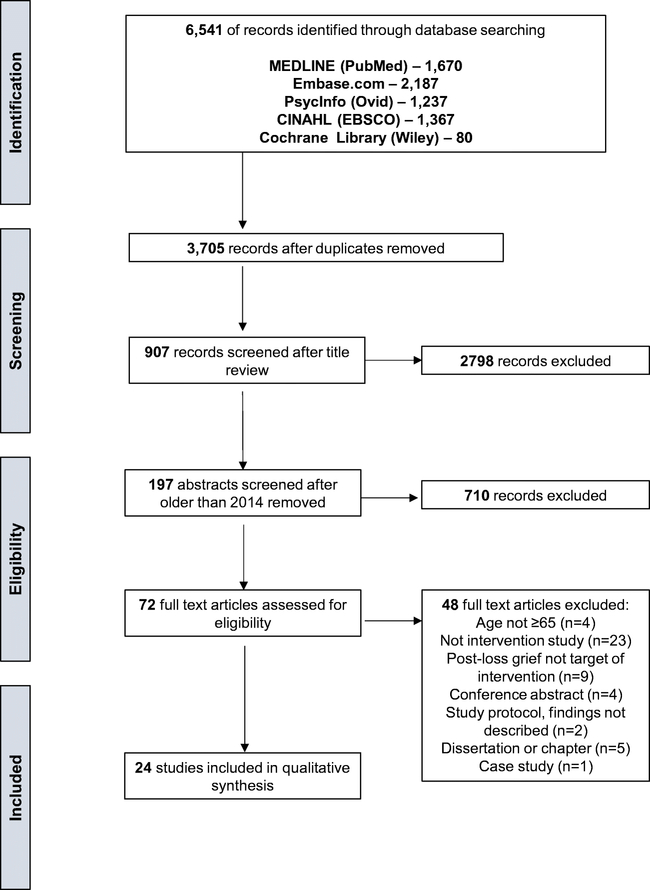
Studies were deemed eligible for inclusion if they described a psychotherapy or psychotropic intervention for bereaved individuals. Preventative interventions for pre-loss caregivers were not included, nor were studies on usual care provided to the bereaved post-loss such as condolence cards. Studies that did not clearly indicate that they included OAs (~65+) in their sample were excluded. Studies which included OAs but did not specifically target OAs were included to fully capture the breadth of which interventions have been tested with OAs. Studies on interventions that did not target bereavement-related outcomes were excluded (See Figure 1 for PRISMA). To present the latest treatment options and to build upon a prior review focusing on grief intervention studies for OA spouses published up to 2013 [44], the qualitative synthesis focused on interventions studies published between 2013 and January 2019 and included all loss types.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram.
Screening Process
After duplicates were removed, titles were randomly assigned to two coders and reviewed independently for initial eligibility. The remaining articles were included in the abstract review stages. In the initial full-text review, two coders reviewed each article to ensure that they met inclusion criteria. When there was disagreement between two coders, discrepancies were discussed; a third coder made the final decision if consensus could not be reached. Finally, the first author completed a standardized template for each article to extract pre-specified information from the included articles.
Treatments: Systematic Review Results
Overview of Treatments
A total of 3,705 records were reviewed after duplicates removed, and a final sample of 24 full-text articles underwent qualitative synthesis (see Figure 1 for PRISMA). Half of the studies (n=12) focused on assessing interventions with exclusively bereaved OAs. Though the remaining studies (n=12) did not exclusively target OAs, they included OAs in the sample and thus were reviewed for relevance. Many of the studies included only (n=7) or mostly (n=4) spousal/partner-bereaved individuals. While several of the studies did not report cause of death (n=10), those that did (n=12) included individuals bereaved by heterogeneous causes (e.g., chronic illness, accident). Inclusion criteria differed among the studies: 11 used a threshold of varying levels of PGD or complicated grief (CG) symptoms1, 1 used a threshold of degree of avoidance and social adjustment [52], and 12 did not screen for clinical symptoms.
Study design and rigor varied, but most studies (n=15) reported using a randomized controlled design. The remaining studies were characterized as non-randomized open-trial [53], quasi-randomized [54], randomized open-case series [55], single condition with no control [56–58], or randomization was not clearly specified [59, 60]. All but three studies [56–58] utilized a control arm; however, the type of control varied, with 11 studies using an active treatment control (e.g., supportive psychotherapy [52], psychoeducation [61]), 6 using waitlist control, and 4 using usual care. While more than half of the studies (n=14) reported utilizing a manualized intervention, only 6 of the studies reported conducting formal treatment fidelity checks. Most studies included a follow-up time point in addition to post-intervention assessments (n=16), but timing of follow-up varied from 6 weeks to up to 15 months.
The most common intervention approaches were variations of cognitive-behavioral therapy (CBT; n=6) [62–65, 60, 66], interventions based on the Dual Process Model of Grief (n=4) [61, 67, 68, 54], and CGT (n=3), which incorporates elements of both CBT and the Dual Process Model [69–71]. Most interventions were delivered individually (n=20) and in person (n=21). In four studies, the intervention included either a telemental health [57, 71] or web-based component [53, 65]. About two-thirds (n=15) of the 21 studies that utilized a control arm demonstrated preliminary efficacy of the experimental intervention on primary outcomes, with complicated or prolonged grief (n=14) and depression (n=13) being the most common intervention targets (see Table 1).
Table 1.
Description of design and outcomes of studies reviewed. Studies differentiated by those that focused on exclusively older adults and those that included older adults in samples of adults broadly.
| Author (Year) | Intervention | Sample | Design/Method | Outcome Measures | Results |
|---|---|---|---|---|---|
| Exclusively Older Adult Samples | |||||
| Chow et al. (2018) | • Dual-Process Model Bereavement Group Intervention – Chinese (DPBGI-C; based on restoration and loss-oriented coping) | • N=125 • Age range: 60 or older • Mage=74.3, SD=7.5 • Type of loss: spousal • Type of death: unspecified |
• Single-blind cluster RCT • Control group: Loss-oriented bereavement group intervention – Chinese (LOBGI-C) • Inclusion criteria: score above 22 on ICG • Use of treatment manual: yes • Treatment fidelity checks: not reported |
• Complicated Grief (CICG) • Depression (HADS-C) • Loneliness (DJGLS-C) • Social support (ISS) |
• Both groups had lower levels of grief and depression post-intervention and follow-up • DPBGI-C more effective than LOBGI-C at post intervention (Cohen’s d=0.35 to 0.56) for primary outcomes (grief, depression, loneliness) • DPBGI-C had significant improvement in anxiety over LOBGI-C (d=0.41) at follow-up • Age not assessed as moderator |
| Hershenberg et al. (2014) | • 5 sessions over 5 weeks of behavioral activation treatment (psychoeducation and adherence to weekly planners) | • N=20 • Age range: not reported • Mage=65.7, SD=11.8 • Type of loss: loved one • Type of death: unspecified |
• Single arm study • No control • Inclusion criteria: 13 or greater on CGA-I and at least 1 risk factor for CB • Use of manual: yes • Treatment fidelity checks: not reported |
• Grief symptoms (CGA-I) • Depression (BDI-II) • Engagement in functional, pleasurable, and social activities on symptoms: weekly planner |
• CGA-I (Cohen’s d=0.72) and BDI (Cohen’s d=0.69) significantly decreased post-intervention • No significant relationship between the total number of or type of activity on outcome measures • Post-hoc power analyses indicate sample size was too small • Age not assessed as moderator |
| Holtslander et al. (2016) | • Finding Balance Intervention (self-administered expressive writing) | • N=19 • Age range: 61–85 • Mage: not provided • Type of loss: spousal • Type of death: advanced cancer |
• RCT • Control group: waitlist • Inclusion criteria: none provided • Treatment manual: yes • Treatment fidelity checks: not reported |
• Hope (HHI) • Grief (HGRS; IDWL) |
• Sole significant result was mean difference in restoration-oriented scale for IWDL for treatment group (Mean increase from 31.0 to 33.9) • No significant mean differences in hope • No significant mean differences for control group • Age not assessed as moderator |
| Knowles et al. (2016) | • Virtual Reality (VR) support group (1-hour twice a week for 8 weeks totaling 16 sessions) | • N=28 • Age range: not reported but only recruited ages 50+ • Mage VR group=67.0, SD=10.73; Mage active control=72.83, SD=11.55 • Type of loss: spouse or romantic partner in past 1–3 years • Type of death: unspecified |
• Non-randomized open trial • Control group: grief website • Inclusion criteria: none reported • Manual: not reported • Fidelity checks: not reported |
• Depression (GDS) • Grief (ICG; GCQ) • Loneliness (UCLA; YSL) • Perceived Stress (PSS) • Sleep (PSQI) • Social support assessed by two face-valid items |
• 94% of VR and 100% of grief website participants would recommend the intervention to a friend. • Both groups showed significant rates of decrease in grief severity, grief cognitions, loneliness, yearning, perceived stress, and improvements in global sleep quality over the three study timepoints (p<.05) • VR group showed significant rates of decreased depressive symptoms (Cohen’s d=1.02) over the three time points compared to grief website group but not on other outcomes • Results remained significant when controlling for age |
| Nam (2016b) | • Complicated Grief Treatment modified for OAs, 8 2-hour weekly sessions • For isolated OAs, therapist telephone calls in lieu of a “supportive person” |
• N=89 • Age range: not reported • Mage = 67.45, SD=2.79 • Type of loss: unspecified • Type of death: unspecified |
• RCT • Control group: Supportive psychotherapy (8 two-hour sessions weekly) • Inclusion criteria: score 5 or higher on BDCGA • Manual: yes • Fidelity checks: not reported |
• Complicated Grief (ICG) • Depression (GDS) • Functional Impairment (WSAS) |
• CGT with support provider showed large and significant effects on grief (Cohen’s d=1.02) and depression (Cohen’s d=0.91) but small effect on functional impairment (Cohen’s d=0.28). • CGT with therapist telephone call showed less efficacy than CGT with support provider; results on CGT with telephone call only versus control were not reported • Results remained significant when age controlled |
| Nam (2016a) | • Self-Care in Bereavement (SCB; 4-session therapy on restoration-oriented coping based on the dual process model) | • N=168 • Age range: not reported • Mage=72.07, SD=6.11 • Type of loss: spousal • Type of death: unspecified |
• RCT • Control group: Psychoeducation on CG • Inclusion criteria: 25 or higher on ICG • Manual: not reported • Fidelity checks: not reported |
• Complicated Grief (ICG) • Post-Traumatic Growth (PGI) • Self-Efficacy (BSES) |
• SCB had significant main effects of reducing ICG scores (Cohen’s d=0.66) and increasing PGI (Cohen’s d=−1.06) and BSES scores (Cohen’s d=−1.28) • Results remained significant when controlling for age |
| Pfoff et al. (2014) | • Functional Therapy (20-session intervention focused on sleep hygiene and lifestyle regularity) | • N=38 • Age range: 60–84 • Mage=72, SD=6.9 • Type of loss: spousal • Type of death: unspecified |
• RCT • Control group: 20-session intervention focused on emotional issues • Inclusion criteria: none reported • Manual: main body of experimental and control sessions followed a treatment manual • Fidelity checks: not reported |
• Grief (TRIG) • Depression (HRSD) • Sleep (PghSD, PSQI) |
• Both treatment groups experienced significant improvement in outcomes over time • FT group showed better improvement in HRSD, PghSD (specifically time spent asleep and sleep efficiency) over time (ps<.05) • Age was found to be insignificant as covariate |
| Pishvaei et al. (2015) | • Group-based life review with integrative reminiscence | • N=34 • Age range:60–80 • Mage=69.41, SD=5.72 • Type of loss: Spousal • Type of death: unspecified |
• RCT • Control group: assessment only • Inclusion criteria: none reported • Manual: not reported • Fidelity checks: not reported |
• Self-esteem (RSES) • Anxiety (AGAS) |
• Experimental group showed significant improvement in self-esteem and decrease in anxiety compared to control (ps<.05) • Findings remained significant when controlling for age |
| Shear et al. (2014) | • CGT (manualized 16-session therapy based on dual process model) | • N=151 • Age range: 50–91 • Mage=66.1, SD=8.9 • Type of loss: mostly spousal, also parent, child, other • Type of death: unspecified |
• RCT • Control group: Interpersonal Psychotherapy • Inclusion criteria: 30 or higher on ICG and confirmed CG through clinical interview • Manual: yes (unpublished) • Fidelity checks: yes |
• Complicated grief (SCID-IV-CG; Complicated Grief-focused-CGI-I; CSSSR; ICG) • Grief-Related Avoidance (GRAQ) • Functional impairment (WSAS) • Depression (BDI) |
• Intention to treat analysis found significantly greater response for CGT than IPT • CGT group significant decrease in CGI (p=.01), IPT group still moderately ill post-treatment. • Greater improvement on WSAS, GRAQ, and BDI for CGT group • At 6-month follow-up, response maintained for 100% of CGT responders and 86% of IPT • Findings were not moderated by age |
| Solaimani-Khashab et al. (2017) | • 8-session group CBT treatment tailored to grief | • N=30 • Age range: 60–75 • Mage: not reported • Type of loss: not specified • Type of death: unspecified |
• Randomization unclear • Control group: assessments only • Inclusion criteria: none reported • Manual: not reported • Fidelity checks: not reported |
• Spiritual well-being (SWBS) • Emotional Intelligence (EIQ) |
• Significant difference between pre- and post for control group on EI and experimental group on both SWBS and EIQ (ps<.05) • Greater improvement in SWBS and EIQ in CBT group than control • Age not assessed as moderator |
| Stahl et al. (2017) | • Behavioral self-monitoring (BSM; sleep, diet, exercise) using goal-setting, monitoring of attention, and diary. • Participants provided with tablets for diary • BSM was paired with motivational interviewing (MI) |
• N phase 1=10 • N phase 2 =13 (not completed) • Age range phase 1: 70–87 • Age range phase 2: not reported • Median age phase I=78 • Median age phase II: not reported • Type of loss: spousal loss within last 8 months • Type of death: unspecified |
• Randomized open-case series testing BSM alone against BSM+MI • Randomization for proposed Phase II • Inclusion criteria: at-risk for mental illness based on: high medical morbidity, functional disability, or subthreshold depression (HRSD of 9–14), anxiety (GAD-7=10) and/or complicated grief (ICG=20) • Manual: yes • Fidelity checks: yes |
• Depression (HRSD; PHQ-9) • Anxiety (GAD-7) • Complicated Grief (ICG) • Symptom Burden (measure not reported) |
• Phase I compliance with recording sessions was 61%, increased to 88% in Phase II after technology improvement • Depression and anxiety scores, but not CG, decreased post-intervention for both BSM and BMS+MI (significance not reported) • Phase II not completed at time of publication • Age not assessed as moderator |
| Utz et al. (2014) | • Life After Loss (LAL; 14-week group intervention based on dual-process model of bereavement with skills-building for loss and restoration-oriented coping) | • N=328 • Age range: 50 or older • Mage = not reported • Type of loss: spouses and domestic partners • Type of death: unspecified |
• RCT • Control group: traditional support group focused on only loss-oriented coping • Inclusion criteria: none reported • Manual: no • Fidelity checks: not reported |
• Depression (GDS) • Grief (TRIG) • Loneliness (UCLA) • Stress Related Growth (SRG) • Self-care and daily living scale (developed for study) |
• Both arms showed statistically significant improvement in depression, grief, loneliness and stress-related growth (ps<.05) • LAL group did not perform better than control on outcomes • Confidence in managing healthcare significantly more improved in LAL group than control. • Age not assessed as moderator |
| Included Older Adults In Sample | |||||
| Ando et al. (2014) | • 2-session Bereavement-focused Life Review | • N=20 • Age range: 20 and older • Mage=68.8, SD=11.7 • Type of loss: spousal (n=18) or child (n=2) • Type of death: unspecified |
• Single arm study • Control group: none • Inclusion criteria: none specified • Use of manual: not reported • Treatment fidelity checks: not reported |
• Spirituality (FACIT-Sp) • Depression (BDI-II) |
• BDI-II scores significantly decreased pre-to-post intervention (t=2.1, p=.045) • FACIT-Sp scores did not significantly change pre- to postintervention (p<.05 • Age not assessed as moderator |
| Bryant et al. (2014) | • 10 weekly 2-hour group sessions of CBT and 4 weekly 1-hour individual sessions with exposure | • N=80 • Age range: 17–70 • Mage CBT+exposure group=51.0, SD=4.4 • Mage CBT group=54.8, SD=9 • Type of loss: Partner (n=11), child (n=11), parent (n=14), other (n=5) • Type of deaths: sudden illness (n=9), chronic illness (n=22), accident (n=6), or suicide (n=4) |
• RCT • Control group: CBT alone • Inclusion criteria: Meet diagnostic criteria for PGD; cutoff not provided • Use of manual: yes • Treatment fidelity checks: yes (20% of audiotapes of each condition were randomly selected and rated |
• Complicated Grief (ICG) • Depression (BDI-II) • PTSD (CAPS-1, PTCI) • Quality of Life (WHO QOL-BREF) |
• Follow up: CBT+exposure led to greater reductions in complicated grief (Hedge’s g = 1.77), depression (Hedge’s g = 1.31), negative appraisals of self (Hedge’s g = 1.06), and functional impairment (Hedge’s g: 1.31–1.77) than CBT alone • Fewer treatment completers in CBT+exposure condition (14.8%) met criteria for PGD than those in the CBT condition (37.9%) at follow-up • Age not assessed as moderator |
| Cotter et al. (2017) | • 7 weekly sessions CBT or Eye Movement Desensitization and Reprocessing (EMDR) | • N=19 • Age range: 22–75 • Mage=45.6, SD=15.52 • Type of loss: spousal (n=8), parent (n=6), child (n=2), girlfriend/boyfriend (n=1), other family member (n=2) • Type of death: unspecified |
• RCT • Control group: Wait-list • Inclusion criteria: none; participants self-identified as experiencing difficulty in coping with the death of a loved one • Use of manual: protocol used for both EMDR and CBT • Treatment fidelity checks: yes |
• Thematic analysis | • Participant feedback similar and positive for both therapies • Reported developments in insight, a positive shift in emotions, increased activity, improved self-confidence and a healthier mental relationship to the deceased. • CBT group described the acquisition of emotion regulation tools and improvements in grief • EMDR group reported more distance from distressing memories • Age not assessed as moderator |
| Kealy et al. (2017) | • Short-term interpretive psychotherapy. 90-minute sessions once a week for 12 weeks (insight-oriented intervention focusing on conflicts and trauma associated with loss and developing tolerance for ambivalence) | • N=110 • Age range: 22–74 • Mage=45.2, SD=11.7 • Type of loss: parent (n=61), sibling (n=12), partner (n=13, child (n=11), friend (n=4), grandparent (n=2), other (n=7) • Type of death: unspecified |
• RCT • Control group: Short-term Supportive psychotherapy. 90-minute sessions 1x/ week for 12 weeks • Inclusion criteria: score 10 or higher on: ICG, intrusion or avoidance subscales of IES; and a 2 or higher on one of six subscales of the SAS-SR • Manual: yes • Fidelity checks: not reported |
• Complicated grief (IBACS; ICG-R) • Post-traumatic stress (IES-R) • General psychological distress (SCL-90-R) |
• Experimental group associated with improvements post-intervention and in 6-month follow up general symptoms, grief symptoms and life satisfaction (p<.05) • No significant association between age and treatment outcome found |
| Litz et al. (2014) | • HEAL (CBT assisted internet-delivered intervention involving grief psychoeducation and behavioral activation) • Designed to increase accessibility, including for older adults • No formal exposure or cognitive reappraisal |
• N=84 • Age range: not reported • Mage=55.37, SD=10.3 • Type of loss: spousal (n=29), partner (n=3), parent (n=4), sibling (n=2), relative (n=2), friend (n=1) with cancer |
• RCT, stratified block design • Control group: 6-week waitlist control • Inclusion criteria: 23 or higher on PG-13 and functional impairment in social, occupational, or household responsibilities as indicated on PG-13 • Manual: not reported • Fidelity checks: not reported |
• Prolonged Grief (PG-13) • Depression (BDI-II) • Anxiety (BAI) • PTSD (PCL-C) • Drug Abuse (DAST; AUDIT) |
• HEAL (across all conditions) resulted in significant reduction of PG-13 (Cohen’s d=1.10), BDI (Cohen’s d=.85), and PCL (Cohen’s d=.92) scores at each follow-up assessment (ps<.02) • Significant difference between conditions at post treatment • Post-intervention 6% of HEAL participants met criteria for PGD, compared to 24% in control • Age not assessed as moderator |
| Meysner et al. (2016) | • 7 weekly sessions CBT or eye movement desensitization and reprocessing (EMDR) | • N=19 • Age range: 22–75 • Mage=45.6, SD=15.52 • Type of loss: spouse (n=8), parent (n=6), child (n=2), girlfriend or boyfriend (n=1), other family member (n=2); 5 participants suffered multiple losses • Type of death: unspecified |
• RCT • Control group: Wait-list before randomization to an active treatment • Inclusion criteria: none reported • Manual: yes • Fidelity checks: not reported |
• PTSD (IES) • Dissociation (DES-II) • Complicated Grief (ICG) • Depression and Anxiety (DASS-21) • Quality of Life (QOLS) |
• Participants with higher levels of grief at baseline showed more substantial improvement in outcomes • Both conditions saw decrease in IES, DASS, ICG (all p’s <.05) • No significant difference between efficacy of control and experimental condition on outcome measures • Age not assessed as moderator |
| Miller et al. (2018) | • Two-tiered peer support and interpersonal psychotherapy model • Peer support: telephone contact every 1–2 weeks for supportive "check-in” • IPT: weekly sessions via telephone or face-to-face |
N=14 • Age range: not reported • Mage=70.4, SD=12.22 • Type of loss: spouse (n=6), parent (n=6), child (n=1), nephew (n=6) • Type of death: unspecified |
• Feasibility and acceptability pilot study • Inclusion criteria: Participants that met criteria for PCBD (ICG>20) or MDD within first 9 months of loss given IPT. Remaining participants given peer support and IPT if symptoms worsened • Control group: none • Inclusion criteria: none reported • Manual: yes • Fidelity checks: not reported |
• Grief (ICG) • Depression (PHQ-9; DSM-V criteria for MDD) |
• 14 out of 16 recruited and eligible participants completed all time points • Participants in either group did not develop syndromal PCBD • Age not assessed as moderator |
| Nam (2016c) | • Psychoeducation on grief and social support both arms • Experimental group: participants interviewed twice about their interpersonal relationships; support providers also offered psychoeducation coaching on bereavement support |
• N=42 • Age range: 21–73 • Mage=45.57, SD=13.04 • Type of loss: unspecified • Type of death: unspecified |
RCT • Control group: psychoeducation only • Inclusion criteria: score 5 or higher on BDCGA • Manual: not reported • Fidelity checks: not reported |
• Complicated Grief (ICG) • Depression (CES-D) |
• Experimental group greater improvement on grief (η2 = 0.64) and depression (η2 = 0.38) than control at post-intervention • Experimental group had significant indirect effect on follow-up grief (95% CI: [-3.17, -1.35]) and depression (95% CI: [-1.96, -0.65]) scores dependent on whether the support received was perceived as helpful • No significant differences by age in treatment outcome |
| Nappa et al. (2016) | • Bereavement groups (focused on positive verbalization, re-exposure of grief experience in a safe group context) | • N=124 • Age range: 39–86 • Mage: not provided • Median age=64.5 • 63% of sample 61+ • Type of loss: mostly spousal • Type of death: unspecified |
• Controlled, prospective intervention study • Control group: those who declined/unable to participate in group completed questionnaires • Inclusion criteria: none reported • Manual: not reported • Fidelity checks: not reported |
• Grief (TRIG) • Depressions (HADS) |
• Grief and depression scores did not change significantly over time for participants • Participants who were unable to participate experienced greater anxiety and depression than group members at 1-year follow up • Age not assessed as moderator |
| Newsom et al. (2017) | • Community Based Bereavement Counseling (CBBC; unstructured, individual counseling informed by dual-process model) | • N=344 • Age range 20–85 • Mage=49.3, SD=14.20 • Type of loss: partner (n=75), parent (n=75), sibling (n=11), child (n=18), other friend/relative (n=7) • Type of death: unspecified |
• Quasi-randomized longitudinal controlled investigation • Control group: 18-month no intervention observation period • Inclusion criteria: none; individuals actively sought help (no routine referrals) • Manual: not reported • Fidelity checks: not reported |
• Complicated Grief (IBACS, ICG-R) • Post-traumatic stress (IES-R) • General psychological distress (SCL-90-R) |
• Decrease in CG symptoms from baseline to post-intervention in both groups, but CBBC not significantly more efficacious than control • Intervention group had greater decrease in CG between post-intervention and follow-up than control • Age not assessed as moderator but study completers older on average |
| Shear et al. (2016) | • Complicated Grief Treatment (CGT; manualized 16-session therapy) with placebo or Citalopram (CIT) • CIT alone or with CGT |
• N=395 • Age range: not reported, 18–95 eligible • Mage=53, SD=14.5 • Type of loss: spouse/partner (n=70), parent (n=41), child, (n=28) other (n=12); most causes of death due to illness • Type of death: unspecified |
• RCT • Control group: CBT + placebo • Inclusion criteria: 30 or higher on ICG and confirmed CG through clinical interview • Manual: yes • Fidelity checks: yes |
• Complicated Grief (SCID-IV-CG); Complicated Grief -focused CGI; ICG) • Functional impairment (WSAS) • Grief-Related Avoidance (GRAQ) • Depression (QIDS-SR16) • Suicidal ideation (Columbia Suicide Scale modified for bereavement) |
• Greater response to CGT with placebo than placebo alone or to CGT with CIT. • Greater response to citalopram with addition of CGT (versus CIT alone). • CIT response not different from placebo alone. • No significantly different improvements in MDD for CIT group, even with CGT and CIT combined. • Age not assessed as moderator |
| Wenn et al. (2019) | • Metacognitive Grief Therapy (MCGT is a 6-session intervention based on grief psychoeducation and a metacognitive model) | • N=22 • Age range: 38–78 • Mage=62, SD=11.2 • Type of loss: partner (n=8), parent (n=3), child (n=1) • Type of death: sudden (n=3), chronic illness (n=7), accident (n=2) |
• Pilot RCT • Control group: waitlist • Inclusion criteria: Score of at least 26 on PG-13 • Manual: yes • Fidelity checks: yes |
• Prolonged Grief (PG-13) • Depression (DASS-21) • Rumination (UGRS) • Metacognition (MCQ-30) • Quality of Life (Q-LES-Q-18) • Global Improvement (CGI) |
Significant reduction in PGD in MCGT group (Cohen’s d=1.68) and increase in PGD severity in waitlist control • Age not assessed as moderator • Significant differences in depression (Cohen’s d=1.28), anxiety (Cohen’s d=0.77), stress, (Cohen’s d=1.03), rumination (Cohen’s d=0.91),, and QoL (Cohen’s d=0.56) in MCGT compared to control • No significant differences for metacognition. • Improvements were maintained for MCGT group 3- and 6-months post-intervention |
Abbreviations: Ahvaz General Anxiety Scale (AGAS); Alcohol Use Disorders Identification Test (AUDIT); Beck Anxiety Inventory (BAI); Beck Depression Inventory – Revised (BDI-II); Brief Dimensional Complicated Grief Assessment (BDCGA); Brief Self-Efficacy Scale (BSES); Center for Epidemiologic Studies – Depression Scale (CES-D); Chinese Inventory of Complicated Grief (CICG); Clinical Global Impressions Scale (CGI); Clinician-Administered PTSD Scale-1(CAPS-1); Columbia Suicide Severity Rating Scale (CSRS); Complicated Grief Assessment Interview (CGA-I); De Jong Gierveld Loneliness Scale – Chinese Version (DJGLS-C); Depression Anxiety Stress Scales – 21 (DASS-21); Dissociative Experiences Scale – II (DES-II); Drug Abuse Screening Test (DAST); Emotional Intelligence Questionnaire (EIQ); Functional Assessment of Chronic Illness Therapy – Spiritual Well-Being Scale (FACIT-Sp); Generalized Anxiety Scale (GAD-7); Geriatric Depression Scale (GDS); Grief Cognitions Questionnaire (GCQ); Grief Related Avoidance Questionnaire (GRAQ); Hamilton Rating Scale for Depression (HRSD); Herth Hope Index (HHI); Hospital Anxiety and Depression Scale (HADS); Hospital Anxiety and Depression Scale – Chinese Version (HADS-C); Hogan Grief Reaction Checklist (HGRS); Impact of Events Scale (IES); Impact of Events Scale – Revised (IES-R); Inventory of Complicated Grief (ICG); Inventory of Complicated Grief, Revised (ICG-R); Inventory of Daily Widowed Life (IDWL); Inventory of Social Support (ISS); Metacognition Questionnaire – 30 (MCQ-30); Patient Health Questionnaire-9 (PHQ-9); Perceived Stress Scale (PSS); Pittsburgh Sleep Diary (PghSD); Pittsburgh Sleep Quality Index (PSQI); Post Traumatic Growth Inventory (PGI); Posttraumatic Cognitions Inventory (PTCI); Prolonged Grief Inventory (PG-13); PTSD Checklist (PCL-C); Texas Revised Inventory of Grief (TRIG); Quality of Life Enjoyment and Satisfaction Questionnaire – 18 (Q-LES-Q-18); Quality of Life Scale (QOLS); Quick Inventory of Depressive Symptoms – Self Report (QIDS-SR16); Rosenberg Self-Esteem Scale (RSES); Spiritual Well Being Scale (SWBS); Stress Related Growth Scale (SRG); Structured Clinical Interview for Complicated Grief (SCID-IV-CG); Symptom Checklist – 90 – Revised (SCL-90-R); Texas Revised Inventory of Grief (TRIG); The Inventory of Bereavement Adaptation – Cruse Scotland (IBACS); UCLA Loneliness Scale (UCLA); Utrecht Grief Rumination Scale (UGRS); Work and Social Adjustment Scale (WSAS); World Health Organization Quality of Life Scale – Brief (WHO QOL - BREF); Yearning in Situations of Loss Scale (YSL)
Cognitive-Behavioral Therapies
A quarter of the studies reviewed (n=6) investigated CBT-based interventions, which included grief psychoeducation, modification of maladaptive loss-related thoughts, fostering of adaptive thoughts (e.g., positive memories of the deceased), and behavioral activation, which may be particularly relevant for OAs because it can address isolation and be helpful even in the context of cognitive decline [72] (see Table 1). Only one CBT study specifically targeted OAs [60], which found preliminary evidence for a group-delivered CBT intervention in improving spiritual well-being and emotional intelligence in widowed OAs in a nursing home. No other bereavement outcomes were described in this report [60]. Five additional studies examined the efficacy of CBT interventions with samples that included OAs. These included studies of CBT paired with exposure [62], Metacognitive Grief Therapy [66], and CBT versus eye movement desensitization and reprocessing [63, 64]. Litz et al. [65] found that their CBT Internet-based self-management intervention, Healthy Experiences After Loss (HEAL), showed preliminary, large effects on reducing PGD symptoms and noted how it could address access and mobility issues in bereaved OAs.
Interventions Informed by the Dual Process Model of Grief
Three studies (see Table 1) examined interventions designed specifically for OAs based on the Dual Process Model of Grief [73, 74], which asserts that adaptive grieving involves a natural oscillation between loss-oriented coping (e.g., emotional processing of grief) and restoration-oriented coping (e.g., [re]engaging in activities, developing new relationships/roles, distraction from grief). Interventions based on this model focused on facilitating these coping processes. These included a Chinese group-based intervention, Dual-Process Bereavement Group Intervention-Chinese (DPBGI-C), which targeted widowed OAs [67]; a 4-week Self-Care in Bereavement (SCB) intervention targeting the needs of bereaved OAs [61]; and Life After Loss (LAL), a 14-week group-based intervention involving psychoeducation and skills-building for both loss- and restoration-oriented coping in OAs [68]. These interventions aimed to address the unique restoration-oriented needs of bereaved OAs (e.g., psychoeducation about obtaining support for meal preparation, finances, independent living). DPBGI-C resulted in moderate effects on reduced CG depression [67] and SCB demonstrated large effects on reducing CG [61] when compared to loss-oriented coping control conditions. In contrast, LAL was not superior to a loss-oriented control group in improving grief, depression, and loneliness [68]. Finally, though not focused exclusively on OAs, a study of community-based grief counseling and Dual Process Model training demonstrated preliminary efficacy in improving CG in a sample of bereaved individuals up to age 85 when compared to a no-intervention control group [54].
Complicated Grief Treatment
Two included studies investigated the efficacy of Complicated Grief Treatment (CGT), which draws on the Dual Process Model of Grief and utilizes CBT-based exposure techniques, in bereaved OAs (see Table 1). Shear et al. [69] found that OAs reported significantly greater reductions in CG symptoms after receiving CGT when compared to Interpersonal Therapy (IPT). The authors noted that they expanded their sample from ages 65+ to 50+ years in the last 8 months of recruitment, and they did not find a statistically significant moderating effect of age [69]. In a separate study that did not focus only on OAs, Shear et al. [70] found that bereaved adults who received CGT alone and those who received CGT with citalopram demonstrated greater treatment responses than those who received citalopram alone. Of note, traditional CGT involves a support provider (e.g., trusted family member or friend) in sessions, which may be a challenge for isolated OAs. To address this, Nam [71] investigated whether, in cases in which a participant did not have a support provider, a weekly telephone call from the CGT therapist would be helpful. CGT (support provider and telephone call formats combined) demonstrated efficacy over supportive counseling with moderate effect on CG and CGT with a support provider was more effective than CGT with therapist telephone contact. This suggests alternatives for a support provider for isolated OAs need further investigation.
Behavioral Interventions
Three studies investigated the efficacy of behavioral interventions for bereaved OAs. Behavioral interventions broadly focus on reducing experiential avoidance, increasing positive reinforcement for engaging in pleasurable activities, and skills building (see Table 1). One study [75] found that Functional Therapy, a behavioral intervention focusing on sleep hygiene, demonstrated greater improvements in depression and sleep quality and efficiency than emotion-focused therapy in a small sample of spousal/partner-bereaved OAs. Stahl et al. [55] found that a behavioral self-monitoring intervention focusing on sleep, diet, and exercise with and without motivational interviewing showed preliminary efficacy for reducing symptoms of depression and anxiety but not CG in a small sample of widowed OAs. Finally, Hershenberg et al. [58] found a moderate effect of a psychoeducational and behavioral activation intervention on CG and depression symptoms in a small sample of bereaved OAs; however, this trial lacked a control arm, limiting interpretation of their findings.
Life Review Interventions
Two studies investigated the efficacy of life review interventions on bereaved adults, with one specifically focusing on OAs (see Table 1). Life review interventions involve a therapist facilitating reminiscence on significant memories and events using interview prompts. Pishvaei et al. [76] investigated the effect of a group-based life review intervention that included reframing past conflicts and challenges, a process referred to as integrative reminiscence, to foster greater self-knowledge in a small sample of OA widowers. Compared to a time-only control group, the intervention group experienced improvements in the primary outcomes, self-esteem and anxiety. Ando et al. [56] investigated the efficacy of a two-session bereavement-oriented life review that involved reflection and construction of photo album with significant words/phrases in a mostly OA sample, though the study recruited adults broadly. While participants in the intervention experienced significantly reduced depression and increased sense of spirituality, the study did not use a control arm and did not examine age as a treatment moderator, limiting conclusions that can be drawn about its effects among OAs [56].
Interpersonal Psychotherapies
Two studies examining interventions that focused on interpersonal challenges and social support included OAs in their broad sample of adults (see Table 1). Nam et al. [77] assessed the impact of psychoeducation about grief and social support alone or psychoeducation paired with an interview about interpersonal conflicts and found the addition of the interview resulted in moderate effects on CG and depression compared to psychoeducation alone; participant age did not moderate intervention effects. Miller et al. [57] utilized a two-tiered intervention in which recently-bereaved adults were first offered peer support and then IPT if their symptoms did not improve. This early intervention model demonstrated promise as participants in neither intervention arm developed syndromal persistent-complex bereavement disorder (similar to prolonged grief); however, given this was a feasibility and acceptability study, significance of this finding was not assessed. Although most participants were OAs, the influence of age on treatment effects was not assessed.
Expressive Therapies
Two studies investigated the efficacy of interventions promoting emotional expression, with one [78] assessing an expressive writing intervention for bereaved OAs, and another [59] evaluating the impact of emotional expression bereavement groups comprised mostly of OAs (see Table 1). Neither study found promising efficacy of the interventions in improving primary outcomes (e.g., hope and grief-related coping [78]; depression and CG [59]). Furthermore, it is possible that the primary outcomes measured did not capture how emotional expression in group interventions is beneficial, such as addressing the loneliness and isolation bereaved OAs commonly face.
Insight-oriented Psychotherapy
Only one study [52] investigated the efficacy of an insight-oriented, group psychodynamic therapy (see Table 1). The psychodynamic intervention demonstrated superior preliminary efficacy in reducing CG symptoms over supportive psychotherapy. Though this study did not target exclusively OAs, they assessed for age-related differences in outcomes and found no association, suggesting the intervention was just as effective for OAs.
Non-traditional Intervention
One study investigated a virtual reality-based support group for bereaved OAs in which group members had virtual avatars to simulate being present in a group [53] (see Table 1). Participants could participate from any location by using a software program called Second Life, designed for OA widows who may have difficulty accessing an in-person group. Compared to an online psychoeducational control arm, the virtual reality group demonstrated a significant, large effect on depression. Both groups reported improvements in grief, loneliness, and sleep [53]. Notably, while this study only reported preliminary efficacy, most participants acknowledged they would recommend the intervention to a friend [53], suggesting the acceptability of digital interventions for OAs.
Discussion
Summary of findings
Findings from this systematic review suggest that CGT, Dual Process Model-based, and behavioral interventions may be most relevant and efficacious for reducing symptoms of pathological grief among bereaved OAs. Studies of these interventions exclusively focused on OAs and similarly focused on supporting OAs with re-engaging in life and managing independent living in bereavement. Although these treatments show promise for bereaved OAs, only 12 of the 24 studies reviewed exclusively focused on OAs. Samples of OAs differed widely in age ranges, with some including adults aged 50+. None investigated the efficacy of grief interventions on the “older old” (individuals 85+). Given most interventions reviewed were not tailored specifically for OAs, they may not have addressed unique developmental considerations for bereaved OAs, such as possible dwindling social networks [33, 34], physical frailty [39–41], and existential concerns around one’s own mortality and sense of meaning in life [11, 12]. This was particularly notable for the studies reviewed investigating CBT approaches, which were largely understudied with exclusively OAs, yet have demonstrated efficacy with bereaved adults more broadly [47]. The one trial of CBT that focused on bereaved OAs did not describe how this group intervention was tailored to their needs and did not assess grief or depression symptoms as other CBT interventions have [60]. Consistent with prior reviews, we found that both studies exclusively focused on OAs and those that included OAs in broader adult samples resulted in relatively small effects on bereavement outcomes [46, 79]. Also similar to prior reviews, the studies had wide heterogeneity in rigor, design, inclusion criteria, and outcomes. Thus, the findings of this review must be considered in the context of the methodological limitations of the studies.
Methodological limitations of treatment studies
The primary limitation of the studies reviewed was the limited number focusing on OAs or examining age as a moderator of treatment effects. While there have been increased efforts to employ more rigorous methods in the study of grief interventions (RCT design) [47], few studies utilized both a usual care or wait list control and active treatment control condition (e.g., supportive psychotherapy). Studies on grief interventions often only use an active treatment comparator because of ethical concerns about neglecting the bereaved while they are acutely distressed [80]. Yet, given the intensity of grief symptoms commonly dissipates over time, it is valuable to observe a comparison group. A compromise in some studies has been to provide enhanced usual care or to use a wait list control to ensure distressed bereaved individuals have access to some form of support. Notably, nearly all the studies, including those that demonstrated efficacy of interventions over control, were underpowered; therefore, only preliminary efficacy was shown. With only a few exceptions, most reports did not provide information about treatment fidelity; thus, findings should be interpreted with this in mind [81].
As has been previously recommended to increase the rigor of bereavement research [79, 47, 46], half of the studies targeted bereaved individuals reporting greater challenges by screening for PGD or CG. Grief interventions have been shown to be, at best, ineffective and, at worst, harmful for those experiencing normative grief [79]. Thus, there has been a growing emphasis on targeting those suffering from bereavement-related mental health challenges and having explicit inclusion criteria for both intervention research and clinical practice. This may be especially relevant for bereaved OAs, as age-related assumptions can contribute to under- or misdiagnosis and inappropriate treatment of bereavement-related mental health challenges. While basing inclusion on a symptom threshold is critical, the studies reviewed varied widely in the screening measures and cutoff scores used. This heterogeneity in screening has been previously noted as a limitation of grief intervention studies [46] and is in part due to a lack of consensus in the field as to a) what form(s) of psychopathology to target (e.g., PGD, depression, PTSD) and b) validated cutoff scores for measures of PGD or CG specifically. Notably, these issues common to grief intervention research may soon be resolved as the field is arriving consensus on diagnostic criteria for PGD. It is currently included in the International Classification of Disease, Eleventh Revision and the revised 5th Edition of the Diagnostic and Statistical Manual of Mental Disorders is preparing to add PGD as a new disorder, pending final empirical validation.
Similarly, across the studies reviewed and those described in previous reviews primary outcomes selected were heterogeneous, though most focused on PGD, CG, and/or depression. There was also substantial variability in the outcome measures used, which has been attributed in part to the lack of established criteria or recommended assessment tools in bereavement research [46]. Study samples were diverse with respect to participant age, relationship to the deceased, and cause of death. Such factors can contribute to risk for negative bereavement-related mental health outcomes [83] and therefore may also impact response to intervention. While the age range of participants in the studies reviewed was wide, none included the “older old” (85+ years), who may be particularly isolated as members of their peer support network die.
Half of the studies primarily focused on spousal/partner loss which is consistent with a prior review of interventions for bereaved OAs [44]. While bereaved spouses/partners make up a sizeable portion of bereaved OAs, it is imperative to also consider other types of loss, as many OAs may experience loss of siblings, parents, friends, and, in some cases, children [6]. Finally, many studies did not report cause of death or included a sample with wide variation in cause of death, despite this potentially being a significant factor in predicting grief outcomes [84] and OA caregivers of individuals with dementia being at particular risk for negative bereavement outcomes [43].
Conclusions
The current review suggests there may be viable treatment approaches for bereaved OAs, particularly those incorporating behavioral activation and guidance on restoration-oriented coping. Investigations of applications of other approaches tailored to the needs of OAs have been limited. It is important to note, however, that this review did not include potentially effective interventions published before 2013. Though limited in scope by its focus on bereaved spouses, a previous review of grief interventions for OAs published between 1990 and 2013 suggested a mind-body intervention showed promise for improving bereavement outcomes, potentially by addressing somatic manifestations of emotional distress [44]. While the present review did not identify recent studies on such interventions, future work should examine a mind-body focus as a possibility for reducing distress in bereavement. Additionally, this review was limited to only those interventions delivered to bereaved OAs post-loss. Interventions designed to be delivered pre-loss to prevent negative bereavement outcomes may have potential utility for OAs, most notably Family-Focused Grief Therapy [47, 49].
Future studies should not only test evidence-based treatments for grief with OAs but should also consider their unique needs, most notably significant social isolation, access and mobility issues, potential cognitive decline, and existential distress. Researchers can learn from efforts made to address other mental health concerns in non-bereaved OAs, including depression interventions adapted for those with cognitive impairment [85] and interventions that have leveraged technology (e.g., whether tele-mental health, computer-based [86], or Internet-based [87]), to reduce treatment barriers. Studies have demonstrated OAs are receptive to eHealth technology use [88, 55, 65, 53] and that web-based interventions can be effective in reducing social isolation in OAs [89].
Future intervention development endeavors should also address an often-neglected clinical topic that has particular relevance for OAs, namely existential challenges. Bereaved OAs, particularly those experiencing PGD and depression, have been found to experience substantial threats to their sense of meaning in life and personal mortality [11, 12, 90, 91]. Furthermore, bereaved OAs often experience social isolation and loneliness as they lose members of their social network [37, 14]. Therefore, OAs who have experienced a significant loss may benefit from a meaning-centered intervention to facilitate meaningful engagement in life and connection to others [92, 93]
In addition to the limitations of existing grief interventions to address certain unique needs of OAs, future research on grief interventions should consider increased methodological rigor, including specificity in sampling and screening for mental health challenges. Particularly relevant to bereaved OAs and consistent with Nseir and Larkey’s [44] review, there is a limited evidence-base of treatment options for the older old (85+). It is imperative not to ignore individuals 85+, as they are a growing population [94] at heightened risk for loneliness and underutilization of health and social services [95]. Given the overrepresentation of spousal/partner loss in bereavement intervention studies with OAs, further evaluation of effective grief interventions in OAs experiencing other types of loss is necessary. Screening for mental health challenges in bereavement is an issue relevant to all age groups [96] but may be particularly relevant to OAs given potential stereotyped assumptions about emotional fragility [97]. Thus, for intervention research, it is critical to utilize a standard in screening methodology and clinically it is important for providers on the frontline of treating OAs, such as primary care providers, to be able to differentiate those who may need intervention and those who are normatively grieving.
The results of this review indicate behavioral activation and promotion of [re]engagement in life are integral to enhance social connections and improve mood in bereaved OAs, as is identifying those most in need of targeting support. Such intervention approaches could be enhanced by focusing on existential distress. Finally, interventions for bereaved OAs should aim to increase access to treatment by leveraging technology such as telehealth or web-based interventions.
Supplementary Material
Acknowledgments
Rebecca M. Saracino, Wendy G. Lichtenthal, Taylor Coats, and Kailey E. Roberts received grants from the National Cancer Institute.
Footnotes
Compliance with Ethics Guidelines
Conflicts of Interest
Leah E. Walsh, Justin Fogarty, Johanna Goldberg, and Holly Prigerson declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Studies varied in their use and measurement of prolonged grief or complicated grief. Results are reported according to how each study labeled and measured these constructs of pathological grief.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Williams BR, Sawyer Baker P, Allman RM, Roseman JMJJoa, health. Bereavement among African American and White older adults. 2007;19(2):313–33. [DOI] [PubMed] [Google Scholar]
- 2.Garrett JE. Multiple losses in older adults. J Gerontol Nurs. 1987;13(8):8–12. [DOI] [PubMed] [Google Scholar]
- 3.Keyes KM, Pratt C, Galea S, McLaughlin KA, Koenen KC, Shear MK. The burden of loss: Unexpected death of a loved one and psychiatric disorders across the life course in a national study. American Journal of Psychiatry. 2014;171(8):864–71. doi: 10.1176/appi.ajp.2014.13081132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prigerson HG, Maciejewski PK. Rebuilding Consensus on Valid Criteria for Disordered Grief. JAMA Psychiatry. 2017;74(5):435–6. doi: 10.1001/jamapsychiatry.2017.0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newson RS, Boelen PA, Hek K, Hofman A, Tiemeier H. The prevalence and characteristics of complicated grief in older adults. J Affect Disord. 2011;132(1–2):231–8. doi: 10.1016/j.jad.2011.02.021. [DOI] [PubMed] [Google Scholar]
- 6.d’Epinay CJ, Cavalli S, Guillet LA. Bereavement in very old age: impact on health and relationships of the loss of a spouse, a child, a sibling, or a close friend. Omega (Westport). 2009;60(4):301–25. [DOI] [PubMed] [Google Scholar]
- 7.Galatzer-Levy IR, Bonanno GA. Beyond normality in the study of bereavement: heterogeneity in depression outcomes following loss in older adults. Social science & medicine. 2012;74(12):1987–94. doi: 10.1016/j.socscimed.2012.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prigerson HG, Shear MK, Newsom JT, Frank E, Reynolds CF 3rd, Maciejewski PK et al. Anxiety among widowed elders: is it distinct from depression and grief? Anxiety. 1996;2(1):1–12. doi:. [DOI] [PubMed] [Google Scholar]
- 9.Valdimarsdottir U, Helgason AR, Furst CJ, Adolfsson J, Steineck G. Awareness of husband’s impending death from cancer and long-term anxiety in widowhood: a nationwide follow-up. Palliat Med. 2004;18(5):432–43. doi: 10.1191/0269216304pm891oa. [DOI] [PubMed] [Google Scholar]
- 10.O’Connor M PTSD in older bereaved people. Aging Ment Health. 2010;14(6):670–8. doi: 10.1080/13607860903311725. [DOI] [PubMed] [Google Scholar]
- 11.Kim SH, Kjervik D, Belyea M, Choi ES. Personal strength and finding meaning in conjugally bereaved older adults: a four-year prospective analysis. Death Stud. 2011;35(3):197–218. [DOI] [PubMed] [Google Scholar]
- 12.Fry PS. The unique contribution of key existential factors to the prediction of psychological well-being of older adults following spousal loss. Gerontologist. 2001;41(1):69–81. doi: 10.1093/geront/41.1.69. [DOI] [PubMed] [Google Scholar]
- 13.Carr D, Jeffreys JS. Spousal bereavement in later life Grief and bereavement in contemporary society: Bridging research and practice. New York, NY: Routledge/Taylor & Francis Group; US; 2011. p. 81–92. [Google Scholar]
- 14.Cohen-Mansfield J, Hazan H, Lerman Y, Shalom V. Correlates and predictors of loneliness in older-adults: a review of quantitative results informed by qualitative insights. Int Psychogeriatr. 2016;28(4):557–76. doi: 10.1017/S1041610215001532. [DOI] [PubMed] [Google Scholar]
- 15.Kersting A, Brahler E, Glaesmer H, Wagner B. Prevalence of complicated grief in a representative population-based sample. J Affect Disord. 2011;131(1–3):339–43. doi: 10.1016/j.jad.2010.11.032. [DOI] [PubMed] [Google Scholar]
- 16.Lundorff M, Holmgren H, Zachariae R, Farver-Vestergaard I, O’Connor MJJoAD. Prevalence of prolonged grief disorder in adult bereavement: A systematic review and meta-analysis. 2017;212:138–49. [DOI] [PubMed] [Google Scholar]
- 17.Jozwiak N, Preville M, Vasiliadis HM. Bereavement-related depression in the older adult population: a distinct disorder? J Affect Disord. 2013;151(3):1083–9. doi: 10.1016/j.jad.2013.08.038. [DOI] [PubMed] [Google Scholar]
- 18.Zisook S, Mulvihill M, Shuchter SR. Widowhood and anxiety. Psychiatr Med. 1990;8(4):99–116. [PubMed] [Google Scholar]
- 19.Cook JM, Simiola V. Trauma and PTSD in older adults: Prevalence, course, concomitants and clinical considerations. Curr Opin Psychol. 2017;14:1–4. doi: 10.1016/j.copsyc.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 20.Onrust S, Cuijpers P. Mood and anxiety disorders in widowhood: a systematic review. Aging & Mental Health. 2006;10(4):327–34. [DOI] [PubMed] [Google Scholar]
- 21.Robbins-Welty G, Stahl S, Zhang J, Anderson S, Schenker Y, Shear MK et al. Medical comorbidity in complicated grief: Results from the HEAL collaborative trial. Journal of Psychiatric Research. 2018;96:94–9. doi: 10.1016/j.jpsychires.2017.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. Lancet. 2007;370(9603):1960–73. doi: 10.1016/S0140-6736(07)61816-9. [DOI] [PubMed] [Google Scholar]
- 23.Vidarsdottir H, Fang F, Chang M, Aspelund T, Fall K, Jonsdottir MK et al. Spousal loss and cognitive function in later life: a 25-year follow-up in the AGES-Reykjavik study. Am J Epidemiol. 2014;179(6):674–83. doi: 10.1093/aje/kwt321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aartsen MJ, Van Tilburg T, Smits CH, Comijs HC, Knipscheer KC. Does widowhood affect memory performance of older persons? Psychol Med. 2005;35(2):217–26. [DOI] [PubMed] [Google Scholar]
- 25.Perez HCS, Ikram MA, Direk N, Tiemeier H. Prolonged Grief and Cognitive Decline: A Prospective Population-Based Study in Middle-Aged and Older Persons. Am J Geriatr Psychiatry. 2018;26(4):451–60. doi: 10.1016/j.jagp.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 26.Elwert F, Christakis NA. The effect of widowhood on mortality by the causes of death of both spouses. Am J Public Health. 2008;98(11):2092–8. doi: 10.2105/AJPH.2007.114348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Einiö E, Martikainen P. Risk of Hospitalization for Cancer, Musculoskeletal Disorders, Injuries, or Poisonings Surrounding Widowhood. American journal of epidemiology. 2019;188(1):110–8. doi: 10.1093/aje/kwy184. [DOI] [PubMed] [Google Scholar]
- 28.Ornstein KA, Garrido MM, Siu AL, Bollens-Lund E, Rahman OK, Kelley AS. An Examination of Downstream Effects of Bereavement on Healthcare Utilization for Surviving Spouses in a National Sample of Older Adults. Pharmacoeconomics. 2019;37(4):585–96. doi: 10.1007/s40273-019-00787-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Szanto K, Galfalvy H, Vanyukov PM, Keilp JG, Dombrovski AY. Pathways to Late-Life Suicidal Behavior: Cluster Analysis and Predictive Validation of Suicidal Behavior in a Sample of Older Adults With Major Depression. J Clin Psychiatry. 2018;79(2). doi: 10.4088/JCP.17m11611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Galfalvy H, Dombrovski A, Szanto K. Prospective predictors of all-cause mortality and suicide in late-life depression. Biological Psychiatry. 2018;83(9):S129. [Google Scholar]
- 31.Prior A, Fenger-Gron M, Davydow DS, Olsen J, Li J, Guldin MB et al. Bereavement, multimorbidity and mortality: a population-based study using bereavement as an indicator of mental stress. Psychol Med. 2018;48(9):1437–43. doi: 10.1017/s0033291717002380. [DOI] [PubMed] [Google Scholar]
- 32.King M, Vasanthan M, Petersen I, Jones L, Marston L, Nazareth I. Mortality and medical care after bereavement: a general practice cohort study. PLoS One. 2013;8(1):e52561. doi: 10.1371/journal.pone.0052561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burton AM, Haley WE, Small BJ. Bereavement after caregiving or unexpected death: effects on elderly spouses. Aging Ment Health. 2006;10(3):319–26. doi: 10.1080/13607860500410045. [DOI] [PubMed] [Google Scholar]
- 34.Jacobson NC, Lord KA, Newman MG. Perceived emotional social support in bereaved spouses mediates the relationship between anxiety and depression. J Affect Disord. 2017;211:83–91. doi: 10.1016/j.jad.2017.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ghesquiere AR, Bazelais KN, Berman J, Greenberg RL, Kaplan D, Bruce ML. Associations between recent bereavement and psychological and financial burden in homebound older adults. Omega: Journal of Death and Dying. 2016;73(4):326–39. [Google Scholar]
- 36.Thompson GN, Roger K. Understanding the needs of family caregivers of older adults dying with dementia. Palliat Support Care. 2014;12(3):223–31. doi: 10.1017/s1478951513000461. [DOI] [PubMed] [Google Scholar]
- 37.Carr DC, Ureña S, Taylor MG. Adjustment to Widowhood and Loneliness Among Older Men: The Influence of Military Service. The Gerontologist. 2018;58(6):1085–95. doi: 10.1093/geront/gnx110. [DOI] [PubMed] [Google Scholar]
- 38.Bonavita A, Yakushko O, Morgan Consoli ML, Jacobsen S, Mancuso RLL. Receiving Spiritual Care: Experiences of Dying and Grieving Individuals. Omega (Westport). 2018;76(4):373–94. doi: 10.1177/0030222817693142. [DOI] [PubMed] [Google Scholar]
- 39.Jones SM, Amtmann D, Gell NM. A psychometric examination of multimorbidity and mental health in older adults. Aging Ment Health. 2016;20(3):309–17. doi: 10.1080/13607863.2015.1008988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.O’Neil M Depression in the elderly. J Contin Educ Nurs. 2007;38(1):14–5. [DOI] [PubMed] [Google Scholar]
- 41.Holm AL, Berland AK, Severinsson E. Factors that influence the health of older widows and widowers-A systematic review of quantitative research. Nurs Open. 2019;6(2):591–611. doi: 10.1002/nop2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sanders S, Ott CH, Kelber ST, Noonan P. The experience of high levels of grief in caregivers of persons with Alzheimer’s disease and related dementia. Death Stud. 2008;32(6):495–523. doi: 10.1080/07481180802138845. [DOI] [PubMed] [Google Scholar]
- 43.Sallim AB, Sayampanathan AA, Cuttilan A, Ho RC-MJJotAMDA. Prevalence of mental health disorders among caregivers of patients with Alzheimer disease. 2015;16(12):1034–41. [DOI] [PubMed] [Google Scholar]
- 44.Nseir S, Larkey LK. Interventions for spousal bereavement in the older adult: an evidence review. Death Stud. 2013;37(6):495–512. doi: 10.1080/07481187.2011.649941. [DOI] [PubMed] [Google Scholar]
- 45.Ghesquiere A, Shear MK, Duan N. Outcomes of bereavement care among widowed older adults with complicated grief and depression. J Prim Care Community Health. 2013;4(4):256–64. doi: 10.1177/2150131913481231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Johannsen M, Damholdt M, Zachariae R, Lundorff M, Farver-Vestergaard I, O’Connor MJJoad. Psychological Interventions for Grief in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. 2019. [DOI] [PubMed] [Google Scholar]
- 47.Waller A, Turon H, Mansfield E, Clark K, Hobden B, Sanson-Fisher RJPM. Assisting the bereaved: A systematic review of the evidence for grief counselling. 2016;30(2):132–48. [DOI] [PubMed] [Google Scholar]
- 48.Shear K, Frank E, Houck PR, Reynolds CFJJ. Treatment of complicated grief: a randomized controlled trial. 2005;293(21):2601–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kissane DW, McKenzie M, Bloch S, Moskowitz C, McKenzie DP, O’Neill I. Family focused grief therapy: a randomized, controlled trial in palliative care and bereavement. Am J Psychiatry. 2006;163(7):1208–18. doi: 10.1176/appi.ajp.163.7.1208. [DOI] [PubMed] [Google Scholar]
- 50.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. 2016;104(3):240–3. doi: 10.3163/1536-5050.104.3.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kealy D, Sierra-Hernandez CA, Piper WE, Joyce AS, Weideman R, Ogrodniczuk JS. Short-Term Group Therapy for Complicated Grief: The Relationship Between Patients’ In-Session Reflection and Outcome. Psychiatry. 2017;80(2):125–38. doi: 10.1080/00332747.2016.1220231.• A randomized-controlled trial investigating the preliminary efficacy of an insight-oriented, group psychodynamic therapy which demonstrated superior preliminary efficacy in reducing complicated grief symptoms over supportive psychotherapy
- 53.Knowles LM, Stelzer E-M, Jovel KS, O’Connor M-F. A pilot study of virtual support for grief: Feasibility, acceptability, and preliminary outcomes. Computers in Human Behavior. 2017;73:650–8. doi: 10.1016/j.chb.2017.04.005.•• Study illustrating preliminary efficacy for a virtual reality group for bereaved older adults on improving depression over an online psychoeducational control arm.
- 54.Newsom C, Schut H, Stroebe MS, Wilson S, Birrell J, Moerbeek M et al. Effectiveness of bereavement counselling through a community-based organization: A naturalistic, controlled trial. Clinical Psychology & Psychotherapy. 2017;24(6):O1512–O23. doi: 10.1002/cpp.2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stahl ST, Emanuel J, Albert SM, Dew MA, Schulz R, Robbins-Welty G et al. Design and Rationale for a Technology-based Healthy Lifestyle Intervention in Older Adults Grieving the Loss of a Spouse. Contemp Clin Trials Commun. 2017;8:99–105. doi: 10.1016/j.conctc.2017.09.002.•• A study in which a behavioral self-monitoring intervention focusing on sleep, diet, and exercise with and without motivational interviewing showed preliminary efficacy for reducing symptoms of depression and anxiety but not complicated grief in widowed OAs.
- 56.Ando M, Sakaguchi Y, Shiihara Y, Izuhara K. Universality of bereavement life review for spirituality and depression in bereaved families. Am J Hosp Palliat Care. 2014;31(3):327–30. doi: 10.1177/1049909113488928. [DOI] [PubMed] [Google Scholar]
- 57.Miller MD, Stack J, Reynolds CF. A Two-Tiered Strategy for Preventing Complications of Bereavement in the First Thirteen Months Post-Loss: A Pilot Study Using Peer Supports with Professional Therapist Back-up. American Journal of Geriatric Psychiatry. 2018;26(3):350–7. doi: 10.1016/j.jagp.2017.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hershenberg R, Paulson D, Gros DF, Acierno R. Does Amount and Type of Activity Matter in Behavioral Activation? A Preliminary Investigation of the Relationship between Pleasant, Functional, and Social Activities and Outcome. Behav Cogn Psychother. 2015;43(4):396–411. doi: 10.1017/s1352465813001185.• A single arm study in which a small sample of bereaved OAs reported reductions in complicated grief and depression symptoms after receiving a psychoeducational and behavioral activation intervention.
- 59.Nappa U, Lundgren AB, Axelsson B. The effect of bereavement groups on grief, anxiety, and depression - a controlled, prospective intervention study. BMC Palliat Care. 2016;15:58. doi: 10.1186/s12904-016-0129-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Solaimani Khashab A, Ghamari Kivi H, Fathi D. Effectiveness of Cognitive Behavioral Therapy on Spiritual Well-Being and Emotional Intelligence of the Elderly Mourners. Iran J Psychiatry. 2017;12(2):93–9.• An investigation on a group-delivered CBT intervention which demonstrated preliminary evidence in improving spiritual well-being and emotional intelligence in widowed OAs in a nursing home.
- 61.Nam I(a) Restoration-focused coping reduces complicated grief among older adults: A randomized controlled study. European Journal of Psychiatry. 2017;31(3):93–8. doi: 10.1016/j.ejpsy.2017.07.002.•• A randomized-controlled trial investigating a Dual-Process Model-based intervention that demonstrated preliminary efficacy in reducing complicated grief in older adults.
- 62.Bryant RA, Kenny L, Joscelyne A, Rawson N, Maccallum F, Cahill C et al. Treating prolonged grief disorder: a randomized clinical trial. JAMA Psychiatry. 2014;71(12):1332–9. doi: 10.1001/jamapsychiatry.2014.1600. [DOI] [PubMed] [Google Scholar]
- 63.Cotter P, Meysner L, Lee CW. Participant experiences of eye movement desensitisation and reprocessing vs. Cognitive behavioural therapy for grief: Similarities and differences. European Journal of Psychotraumatology Vol 8(1), 2017, ArtID 1375838. 2017;8(1). doi: 10.1080/20008198.2017.1375838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Meysner L, Cotter P, Lee CW. Evaluating the efficacy of EMDR with grieving individuals: A randomized control trial. Journal of EMDR Practice and Research. 2016;10(1):2–12. doi: 10.1891/1933-3196.10.1.2. [DOI] [Google Scholar]
- 65.Litz BT, Schorr Y, Delaney E, Au T, Papa A, Fox AB et al. A randomized controlled trial of an internet-based therapist-assisted indicated preventive intervention for prolonged grief disorder. Behav Res Ther. 2014;61:23–34. doi: 10.1016/j.brat.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wenn JA, O’Connor M, Kane RT, Rees CS, Breen LJ. A pilot randomised controlled trial of metacognitive therapy for prolonged grief. BMJ Open. 2019;9(1). doi: 10.1136/bmjopen-2017-021409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chow AYM, Caserta M, Lund D, Suen MHP, Xiu D, Chan IKN et al. Dual-Process Bereavement Group Intervention (DPBGI) for Widowed Older Adults. Gerontologist. 2018. doi: 10.1093/geront/gny095.•• A randomized-controlled trial of a Chinese group-based intervention, Dual-Process Bereavement Group Intervention-Chinese (DPBGI-C) which showed preliminary efficacy in improving complicated grief and depression in widowed older adults.
- 68.Utz RL, Caserta M, Lund D. An Evaluation of the Living After Loss Intervention - Part 1: Do Bereavement-Related Outcomes Vary by the Content of Support Groups? Grief Matters. 2013;16(2):32–5. [PMC free article] [PubMed] [Google Scholar]
- 69.Shear MK, Wang Y, Skritskaya N, Duan N, Mauro C, Ghesquiere A. Treatment of complicated grief in elderly persons: a randomized clinical trial. JAMA Psychiatry. 2014;71(11):1287–95. doi: 10.1001/jamapsychiatry.2014.1242.•• A randomized-controlled trial of Complicated Grief Treatment with older adults that demonstrated efficacy in reducing complicated grief symptoms
- 70.Shear MK, Reynolds CF 3rd, Simon NM, Zisook S, Wang Y, Mauro C et al. Optimizing Treatment of Complicated Grief: A Randomized Clinical Trial. JAMA Psychiatry. 2016;73(7):685–94. doi: 10.1001/jamapsychiatry.2016.0892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nam I (b) Complicated Grief Treatment for older adults: The critical role of a supportive person. Psychiatry Res. 2016;244:97–102. doi: 10.1016/j.psychres.2016.07.044.• A randomized-controlled trial investigating efficacy of Complicated Grief Treatment (CGT) in Korean older adults, using a therapist phone call to replace a support provider for isolated participants. CGT with a support provider was more effective than standard supportive counseling.
- 72.Orgeta V, Qazi A, Spector A, Orrell M. Psychological treatments for depression and anxiety in dementia and mild cognitive impairment: systematic review and meta-analysis. Br J Psychiatry. 2015;207(4):293–8. doi: 10.1192/bjp.bp.114.148130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Richardson VE. The Dual Process Model of Coping with Bereavement: A decade later. Omega: Journal of Death and Dying. 2010;61(4):269–71. doi: 10.2190/OM.61.4.a. [DOI] [PubMed] [Google Scholar]
- 74.Stroebe M, Schut H. The dual process model of coping with bereavement: rationale and description. Death Stud. 1999;23(3):197–224. doi: 10.1080/074811899201046. [DOI] [PubMed] [Google Scholar]
- 75.Pfoff MK, Zarotney JR, Monk TH. Can a function-based therapy for spousally bereaved seniors accrue benefits in both functional and emotional domains? Death Stud. 2014;38(6–10):381–6. doi: 10.1080/07481187.2013.766658.•• A randomized-controlled trial that found Functional Therapy, a behavioral intervention, demonstrated greater improvements in depression and sleep than emotion-focused therapy in a small sample of spousal/partner-bereaved OAs
- 76.Pishvaei M, Moghanloo RA, Moghanloo VA. The Efficacy of Treatment Reminders of Life with Emphasis on Integrative Reminiscence on Self-Esteem and Anxiety in Widowed Old Men. Iranian Journal of Psychiatry. 2015;10(1):19–24.•• This study investigates the effect of a group-based life review intervention in a small sample of OA widowers. Compared to a time-only control group, the intervention group experienced improvements in self-esteem and anxiety.
- 77.Nam IS. (c) Effects of psychoeducation on helpful support for complicated grief: a preliminary randomized controlled single-blind study. Psychol Med. 2016;46(1):189–95. doi: 10.1017/s0033291715001658.• This study assessed the impact of psychoeducation about grief and social support alone or psychoeducation paired with an interview about interpersonal conflicts and found the addition of the interview resulted in greater improvements in complicated grief and depression than psychoeducation alone in a sample that included OAs.
- 78.Holtslander L, Duggleby W, Teucher U, Cooper D, Bally JM, Solar J et al. Developing and pilot-testing a Finding Balance Intervention for older adult bereaved family caregivers: A randomized feasibility trial. Eur J Oncol Nurs. 2016;21:66–74. doi: 10.1016/j.ejon.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 79.Currier JM, Neimeyer RA, Berman JS. The effectiveness of psychotherapeutic interventions for bereaved persons: A comprehensive quantitative review. Psychol Bull. 2008;134(5):648–61. doi: 10.1037/0033-2909.134.5.648. [DOI] [PubMed] [Google Scholar]
- 80.Constantino RE, Sekula LK, Rubinstein EN. Group intervention for widowed survivors of suicide. Suicide Life Threat Behav. 2001;31(4):428–41. [DOI] [PubMed] [Google Scholar]
- 81.Wampold BE. How important are the common factors in psychotherapy? An update. World Psychiatry. 2015;14(3):270–7. doi: 10.1002/wps.20238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Maciejewski PK, Maercker A, Boelen PA, Prigerson HG. “Prolonged grief disorder” and “persistent complex bereavement disorder”, but not “complicated grief”, are one and the same diagnostic entity: an analysis of data from the Yale Bereavement Study. World Psychiatry. 2016;15(3):266–75. doi: 10.1002/wps.20348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Roberts K, Holland J, Prigerson HG, Sweeney C, Corner G, Breitbart W et al. Development of the Bereavement Risk Inventory and Screening Questionnaire (BRISQ): Item generation and expert panel feedback. Palliat Support Care. 2017;15(1):57–66. doi: 10.1017/S1478951516000626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Holland JM, Neimeyer RA. Separation and traumatic distress in prolonged grief: The role of cause of death and relationship to the deceased. Journal of Psychopathology and Behavioral Assessment. 2011;33(2):254–63. [Google Scholar]
- 85.Bingham KS, Flint AJ, Mulsant BH. Management of Late-Life Depression in the Context of Cognitive Impairment: a Review of the Recent Literature. Curr Psychiatry Rep. 2019;21(8):74. doi: 10.1007/s11920-019-1047-7. [DOI] [PubMed] [Google Scholar]
- 86.Morthland M, Shah A, Meadows JT, Scogin F. Development of an audio and computer cognitive behavioral therapy for depression in older adults. Aging Ment Health. 2019:1–9. doi: 10.1080/13607863.2019.1609901. [DOI] [PubMed] [Google Scholar]
- 87.Pepin R, Segal DL, Coolidge FL. Intrinsic and extrinsic barriers to mental health care among community-dwelling younger and older adults. Aging Ment Health. 2009;13(5):769–77. doi: 10.1080/13607860902918231. [DOI] [PubMed] [Google Scholar]
- 88.Schulz R, Wahl HW, Matthews JT, De Vito Dabbs A, Beach SR, Czaja SJ. Advancing the Aging and Technology Agenda in Gerontology. Gerontologist. 2015;55(5):724–34. doi: 10.1093/geront/gnu071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Czaja SJ, Boot WR, Charness N, Rogers WA, Sharit J. Improving Social Support for Older Adults Through Technology: Findings From the PRISM Randomized Controlled Trial. Gerontologist. 2018;58(3):467–77. doi: 10.1093/geront/gnw249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kim SH. The influence of finding meaning and worldview of accepting death on anger among bereaved older spouses. Aging Ment Health. 2009;13(1):38–45. doi: 10.1080/13607860802154457. [DOI] [PubMed] [Google Scholar]
- 91.Neimeyer RA, Holland JM. Bereavement in later life: Theory, assessment, and intervention. APA handbook of clinical geropsychology, Vol 2: Assessment, treatment, and issues of later life. Washington, DC: American Psychological Association; US; 2015. p. 645–66. [Google Scholar]
- 92.Lichtenthal WG, Breitbart W. The central role of meaning in adjustment to the loss of a child to cancer: implications for the development of meaning-centered grief therapy. Curr Opin Support Palliat Care. 2015;9(1):46–51. doi: 10.1097/SPC.0000000000000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lichtenthal WG, Catarozoli C, Masterson M, Slivjak E, Schofield E, Roberts KE et al. An open trial of meaning-centered grief therapy: Rationale and preliminary evaluation. Palliat Support Care. 2019;17(1):2–12. doi: 10.1017/S1478951518000925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Vincent GK, Velkoff VA. The next four decades: The older population in the United States: 2010 to 2050. vol 1138 US Department of Commerce, Economics and Statistics Administration, US; …; 2010. [Google Scholar]
- 95.Wang H, Zhao E, Fleming J, Dening T, Khaw KT, Brayne C et al. Is loneliness associated with increased health and social care utilisation in the oldest old? Findings from a population-based longitudinal study. BMJ Open. 2019;9(5):e024645. doi: 10.1136/bmjopen-2018-024645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lichtenthal WG, Maciejewski PK, Craig Demirjian C, Roberts KE, First MB, Kissane DW et al. Evidence of the clinical utility of a prolonged grief disorder diagnosis. World Psychiatry. 2018;17(3):364–5. doi: 10.1002/wps.20544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Eymard AS, Douglas DH. Ageism among health care providers and interventions to improve their attitudes toward older adults: an integrative review. J Gerontol Nurs. 2012;38(5):26–35. doi: 10.3928/00989134-20120307-09. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.