COVID-19 has placed respiratory medicine at the centre of health responses worldwide, but lung health was a major global challenge long before the current pandemic. More than 1000 people die of asthma and more than 2000 children die of pneumonia daily, and lung cancer is the most common cancer type in terms of incidence and mortality. Most of this enormous burden has fallen on people in the south and vulnerable populations in high-income economies. These are diseases of poverty, and disadvantages further compound inequity through increased disability, loss of productivity, and high health costs.1 As a major driver of ill health and poverty, the burden of respiratory disease remains a global rate-limiting step towards achieving health equity, economic growth, and Sustainable Development Goals.2
Even before the COVID-19 pandemic, this respiratory burden was set to increase.3 As urbanisation and climate change intensifies, global exposure to the key risk factors of tobacco smoking, indoor and outdoor air pollution from biomass fuels, traffic exhaust and occupational pollutants, and allergens, is likely to increase. Infants and young children are at particular risk. The complex relationships between biological, sociocultural, and environmental causes of respiratory disease mean that there are many gaps in the understanding of how best to address these factors, especially in settings with poor and unequal availability of respiratory health services.
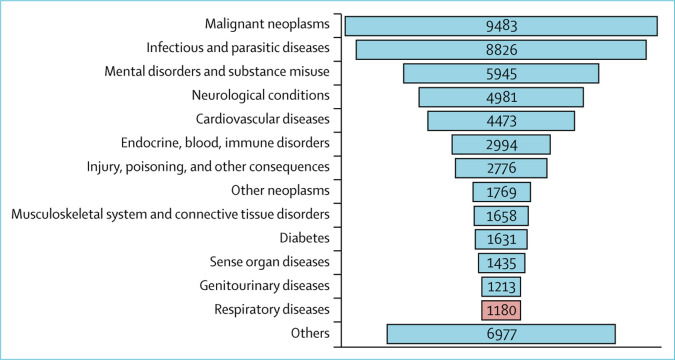
Health financing is under greater pressure now than ever, therefore research is needed to understand which resources can be released or better used. Examples include unwarranted variation in the use of medication including pronounced underuse of nicotine replacement therapy in treating tobacco dependence, overuse of bronchodilators, and underuse of highly effective inhaled corticosteroids in asthma, and poor adherence to tuberculosis treatment. Yet, in the latest WHO analysis of research expenditure from 12 major funders, between 2012 and 2017,4 respiratory diseases were low down on the list (figure ).
Figure.
Grants awarded for non-communicable diseases in 2012–2017
Total 55 341 (72%) grants were for non-communicable diseases. Data taken from WHO Global Observatory World RePORT.4
Almost three-quarters of grants were for non-communicable diseases (NCD), but respiratory disease lies 13th in the NCD category list with just 2% of the total number of grants. When listed according to disease: tuberculosis lies 19th, asthma is 27th, and chronic obstructive pulmonary disease is in 50th place. Only 0·2% of research funding went to low-income countries. Of the 450 grants received by African countries, grants for respiratory diseases included: 39 for tuberculosis, seven for lower respiratory infections, and two for asthma. In southeast Asia only two of 19 grants were for respiratory-related infections.
There has been a substantial mismatch between burden and research investment, which has not improved in over a decade.5 Although limited by data availability, our analysis suggests that advocacy for respiratory research has not been successful in communicating the urgency or scale of the problem, or the potential impact of research investment. An improved response is needed at an international and national scale.
Some countries such as the UK with South Asia, and Uganda have started to invest in research to identify the size of the problem and to reprioritise research funding.6 However, there is no global research strategy that aligns the interests of all stakeholders: governmental and commercial research funders, academic institutions, global and national health agencies, clinicians, patients, and the public. Global funding also needs to be rebalanced towards low-income and middle-income countries that bear the greatest burden but have the least resource available. In the focus on transmissibility and epidemic preparedness that will probably follow once the COVID-19 pandemic has resolved, the contribution of tobacco dependence, air pollution, and nutrition to respiratory morbidity should not be forgotten. To have a lasting impact, respiratory health research needs to increasingly expand its focus and partnerships beyond the health sector and health systems.
There is an urgent need for the respiratory research community to work more effectively with other stakeholders to increase recognition of the terrible burden of respiratory disease and to develop, test, implement, and scale-up the necessary multiple and multisectoral strategies to improve respiratory health. In its first call for global health bids, the UK National Institute for Health Research (NIHR) committed 12% of the total grant allocation to responsive respiratory research in the Development Assistance Committee listed countries. This allocation has triggered the formation of a Global Health Respiratory Network (GHRN), a meta-collaboration of UK respiratory research institutions, and their global health partners.7 The GHRN has created opportunities for synergistic working between research programmes across countries and the spectrum of respiratory diseases.
The future requires well funded, long term, large-scale implementation science collaborations. We call on all funders to review and publish their investment in research on respiratory health. We also ask funders to work synergistically to build up current activity and to develop and share a research roadmap which would minimise the risk of duplication and maximise the effect on health, wellbeing, and economic growth. The WHO Coordinated Global Research Roadmap for COVID-19 might be a model to emulate.
Acknowledgments
We declare no competing interests. The National Institute for Health Research (NIHR) groups and units that form the Global Health Respiratory Network are funded by Research Councils UK as part of the Global Challenges Research Fund (GCRF) or by the NIHR using aid from the UK government to support global health research. The views expressed are those of the authors and not necessarily those of the GCRF, NIHR, or the UK Department of Health and Social Care.
References
- 1.Squire SB, Thomson R, Namakhoma I, El Sony A, Kritski A, Madan J. Catastrophic care-seeking costs as an indicator for lung health. BMC Proc. 2015;9(suppl 10):4. doi: 10.1186/1753-6561-9-S10-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nugent R, Bertram MY, Jan S. Investing in non-communicable disease prevention and management to advance the Sustainable Development Goals. Lancet. 2018;391:2029–2035. doi: 10.1016/S0140-6736(18)30667-6. [DOI] [PubMed] [Google Scholar]
- 3.Institute for Health Metrics and Evaluation (IHME) IHME; Seattle, WA: 2018. Findings from the Global Burden of Disease Study 2017. [Google Scholar]
- 4.WHO Number of grants for biomedical research by funder, type of grant, duration and recipients (World RePORT) 2019. https://www.who.int/research-observatory/monitoring/inputs/world_report/en/
- 5.Stuckler D, King L, Robinson H, McKee M. WHO's budgetary allocations and burden of disease: a comparative analysis. Lancet. 2008;372:1563–1569. doi: 10.1016/S0140-6736(08)61656-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang C, Xu J, Yang L. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet. 2018;391:1706–1717. doi: 10.1016/S0140-6736(18)30841-9. [DOI] [PubMed] [Google Scholar]
- 7.Sheikh A, Campbell H, Balharry D. The UK's global health respiratory network: improving respiratory health of the world's poorest through research collaborations. J Glob Health. 2019;9 doi: 10.7189/jogh.09.020104. [DOI] [PMC free article] [PubMed] [Google Scholar]