Abstract
Introduction
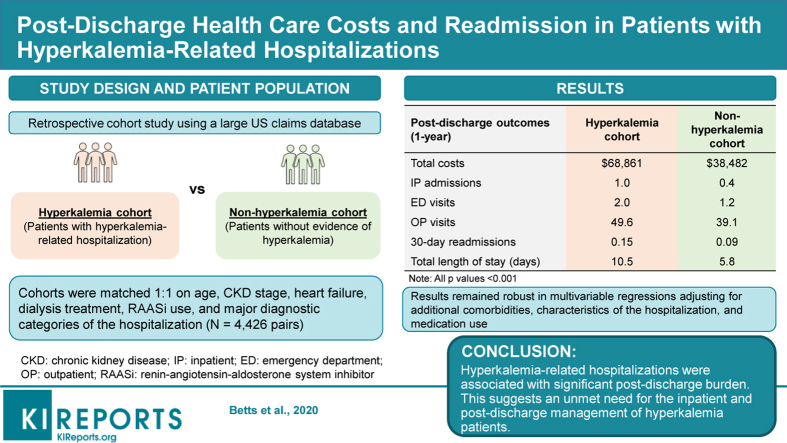
Limited evidence is available regarding the postdischarge economic and readmission burdens of hyperkalemia.
Methods
Using the IBM MarketScan Commercial and Medicare-Supplemental Claims database (January 1, 2010–December 31, 2014), adult patients with a hospitalization with a hyperkalemia diagnosis (ICD-9-CM 276.7, hyperkalemia cohort) were 1:1 matched with patients with a hospitalization without evidence of hyperkalemia (nonhyperkalemia cohort) on age, chronic kidney disease stage, heart failure, dialysis, renin-angiotensin-aldosterone system inhibitor use, and major diagnostic categories of the hospitalization. All-cause health care costs and health care resource utilization measures were compared between cohorts during the 1-year postdischarge period. Postdischarge readmission and length of stay (LOS) were compared between hyperkalemia-related hospitalizations from the hyperkalemia cohort and matched hospitalizations unrelated to hyperkalemia from the nonhyperkalemia cohort.
Results
Patients with hyperkalemia-related hospitalizations (n = 4426) incurred $30,379 (95% confidence interval, $25,423–$35,335) higher 1-year total all-cause costs ($68,861 vs. $38,482) and had higher rates of inpatient admissions (1.0 vs. 0.4), emergency department visits (2.0 vs. 1.2), and outpatient visits (49.6 vs. 39.1) than the nonhyperkalemia cohort during the 1-year postdischarge study period (all P < 0.001). Hyperkalemia-related hospitalizations (n = 5377) were associated with significantly higher readmission rates (within 30 days: 0.15 vs. 0.09; 60 days: 0.25 vs. 0.16; 90 days: 0.36 vs. 0.23; all P < 0.001), longer LOS per readmission (8.1 vs. 7.1 days), and longer total inpatient days (10.5 vs. 5.8 days) compared with hospitalizations unrelated to hyperkalemia (all P < 0.001). Similar trends were observed across comorbidity subgroups.
Conclusion
Hyperkalemia-related hospitalizations were associated with significant economic and readmission burdens during the 1-year postdischarge period.
Keywords: cost, postdischarge, health care resource utilization, hospitalizations, hyperkalemia, readmission
Graphical abstract
Hyperkalemia is an electrolyte abnormality defined as abnormally high serum potassium levels (>5.0 mEq/l).1, 2, 3, 4 Although hyperkalemia may be asymptomatic, abnormally high potassium levels can manifest as muscle cramps and weakness, and, in some cases, can lead to life-threatening cardiac arrhythmias and sudden death.5, 6, 7 The annual prevalence of hyperkalemia in 2014 in a US adult patient population was 1.6% with a higher prevalence of 6.4% observed in adult patients with chronic kidney disease (CKD) and heart failure (HF).8 Among US Medicare beneficiaries, the estimated prevalence of hyperkalemia was 2.6%–2.7% in the overall population and 8.9%–9.3% in patients with CKD and/or HF.9
Hyperkalemia is primarily caused by renal dysfunction leading to reduced excretion of potassium.5,9 Patients with an advanced stage of CKD are at greatest risk of developing hyperkalemia.10 In addition, patients with chronic HF are at an increased risk of hyperkalemia as a result of reduced cardiac output and compromised renal perfusion.2 Among patients with diabetes mellitus, insulin deficiency leading to elevated serum potassium concentrations resulting from suboptimal intracellular potassium transport may also increase the risk of hyperkalemia.10 Impairments in the renin-angiotensin-aldosterone system (RAAS), in the case of Addison's disease, or adrenal enzyme deficiencies can also cause hyperkalemia.11 RAAS inhibitors (including aldosterone receptor antagonists [ARAs], angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and direct renin inhibitors), which are commonly prescribed for patients with CKD and HF, can also increase the frequency and severity of hyperkalemia.2,4,11, 12, 13
In addition to clinical consequences, hyperkalemia is associated with increased health care costs and health care resource utilization (HRU). This burden is largely attributed to inpatient stays and varies significantly by patient subgroups (e.g., patients with CKD or HF).14, 15, 16 A recent study by Betts et al.15 using a large US claims database found that patients with hyperkalemia incurred $15,983 (2015 USD) higher total health care costs and $9293 higher inpatient costs (58% of the total cost difference) than patients without hyperkalemia within 1 year. The average LOS per inpatient admission was 1.5 days longer for patients with hyperkalemia, and when hospitalized, patients with hyperkalemia were 40% more likely to be readmitted within 1 year compared with matched patients without hyperkalemia.15 Another study by Betts et al.14 in a Medicare population observed that patients with hyperkalemia incurred $19,349 higher 1-year all-cause medical costs compared with matched patients without hyperkalemia ($34,362 vs. $15,013), with $13,219 (68%) of the total cost difference being attributed to cost difference in inpatient admissions. A study by Fitch et al.16 also reported that patients with hyperkalemia had consistently higher costs compared with patients without hyperkalemia in the Medicare ($4945 vs. $2137 per-patient-per-month) and commercially insured ($7247 vs. $2879 per-patient-per-month) patient populations. Both Betts et al.15 and Fitch et al.16 showed that HRU and health care costs increased with CKD severity with inpatient care being the main driver of costs among patients with CKD and hyperkalemia.
Although previous studies have demonstrated that hyperkalemia is associated with a significant economic burden, with inpatient admission as the main driver of costs, there is limited evidence regarding outcomes following discharge from a hyperkalemia-related hospitalization. Postdischarge readmission rates are important hospital quality metrics to measure the effectiveness of hospital care and the postdischarge economic burden has important implications to payers. Moreover, given that previous studies showed that the burden of hyperkalemia varies by patient subgroups, an assessment of the postdischarge burden of hyperkalemia among different patient subgroups is needed. To help fill this gap in knowledge, the present study was conducted to assess real-world postdischarge costs and HRU, including readmissions associated with hyperkalemia-related hospitalizations, in the overall patient population as well as in subgroups defined by hyperkalemia-related comorbidities.
Methods
Data Source
This study used data from a large US insurance claims database (the IBM MarketScan Commercial and Medicare-Supplemental Claims database [January 1, 2010 to December 31, 2014]). The database captures health services claims for more than 170 million insured active employees and their dependents, including early retirees, and Medicare-eligible retirees with employer-provided Medicare Supplemental plans. The database includes demographic characteristics, insurance enrollment history, diagnoses and procedures, and claims for medical and pharmacy services. The laboratory database clinically enriches the medical and pharmacy services data of patients in the MarketScan database by linking patients’ claims data with outpatient laboratory test results. The data are available for a subset of patients in the database. Both databases are fully compliant with the Health Insurance Portability and Accountability Act of 1996 and its implementing regulations, and thus, no ethics board review was required.
The IBM MarketScan Commercial and Medicare-Supplemental Claims database has been used in multiple studies for the assessment of prevalence, clinical burden, and economic burden of hyperkalemia.8,15,16 The multiple strengths of this database made it the most suitable database for the present study. For example, all medical claims covering inpatient, outpatient, and emergency room visits were recorded during each patient’s eligibility period, making it feasible to capture all of a patient’s HRU and costs. In addition, the MarketScan database captures laboratory tests for a subset of the covered lives, including tests ordered in office-based practices, which made it possible to include some laboratory information such as measurements of serum potassium and estimated glomerular filtration rate (eGFR), which may be used to identify hyperkalemia and CKD. Lastly, the large sample size and representativeness of data would allow the results of the study to be generalizable to the US commercially insured population.
Study Design and Sample Selection
The objective of this study was to assess the incremental postdischarge economic and readmission burden of hyperkalemia. To address this study objective, the postdischarge outcomes among patients with hyperkalemia-related hospitalizations (hyperkalemia cohort) were compared with hospitalizations from nonhyperkalemia patients (nonhyperkalemia cohort).
Adult patients with 1 or more hospitalizations with a hyperkalemia diagnosis (International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM] code 276.7) were identified as the hyperkalemia cohort. The first hospitalization with hyperkalemia was selected as the hospitalization of interest (i.e., the index hospitalization). Patients’ postdischarge outcomes were assessed during the 1-year period following discharge from the index hospitalization. The day after discharge was defined as the index date (i.e., the date patients’ postdischarge outcomes were first evaluated).
Adult patients with at least 1 hospitalization were included in the nonhyperkalemia cohort if they did not have any evidence of hyperkalemia including elevated potassium laboratory results (identified by Logical Observation Identifiers Names and Code 2823–3; >5.0 mEq/l), hyperkalemia diagnoses, or sodium polystyrene sulfonate prescriptions during the entire claims history. A randomly selected eligible hospitalization was identified as the index hospitalization for the nonhyperkalemia cohort, and the day after discharge was defined as the index date.
Continuous insurance enrollment from 6 months before the index hospitalization (i.e., baseline period) to 12 months after the index hospitalization discharge (i.e., study period) was required for both cohorts. The hyperkalemia cohort and the nonhyperkalemia cohort were matched 1:1 on age group (18–64 or >65 years), CKD stage (stage 3, stage 4, stage 5, and unspecified CKD stage), HF, dialysis treatment, and RAAS inhibitor (RAASi) use during the baseline period as well as major diagnostic categories (MDCs) and HF, acute myocardial infarction, and pneumonia diagnosis-related groups during the index hospitalization.
Patient Characteristics and Outcomes Assessment
Patient characteristics measured during the baseline period included (i) demographic characteristics, including age, sex, region, and insurance type; (ii) disease and clinical characteristics including hyperkalemia-related comorbidities (such as CKD, HF, diabetes, and hypertension), Charlson Comorbidity Index, selected comorbidities by diagnosis-related group, and MDCs; and (iii) medication use, including RAASi and sodium polystyrene sulfonate.
All-cause health care costs (in 2016 US dollars) included all-cause medical costs (inpatient, emergency department [ED], and outpatient costs) and pharmacy costs during the 1-year study period and by each quarter. HRU outcomes included inpatient admissions, ED visits, and outpatient visits during the 1-year study period.
Readmissions were assessed as the number of all-cause hospital readmissions and presence of at least one inpatient readmission within 30, 60, and 90 days of the discharge date of the index hospitalization. LOS per readmission and total inpatient days were also assessed during the 1-year postdischarge study period.
Definition of Comorbidities and Patient Subgroups
Subgroups of patients were formed based on key comorbidities.17 CKD was identified by diagnosis code (Supplementary Table S1) or eGFR indicating stages 3 to 5, and categorized as follows: CKD stage 3, diagnosis code (585.3) or eGFR 30 to 59 ml/min per 1.73 m2; CKD stage 4, diagnosis code (585.4) or eGFR 15 to 29 ml/min per 1.73 m2; CKD stage 5, diagnosis code (403 except for 403.x0, 404 except for 404.x0, 404.x1, 585.5, and 585.6) or eGFR below 15 ml/min per 1.73 m2. The unspecified CKD stage group included patients with an ICD-9-CM code for unspecified CKD (585.9, 403.x0, 404.x0, and 404.x1) (Supplementary Table S1). Dialysis treatment was identified using relevant procedure codes (Supplementary Table S2), and patients on dialysis were included in their own group. HF, diabetes, and hypertension were identified by ICD-9-CM diagnosis codes (Supplementary Table S1).
Statistical Analysis
Matched Comparisons of Patient Characteristics, Costs, and HRU
Patient characteristics, health care costs, and HRU were described and compared between the matched hyperkalemia and nonhyperkalemia cohorts using generalized estimating equation models. Health care costs and HRU were also compared in the subgroup populations, including patients with CKD, HF, CKD and/or HF, dialysis treatment, diabetes, and hypertension.
Matched Comparisons of Readmissions and LOS
The postdischarge readmission burden was assessed among a second sample consisting of all the hyperkalemia-related hospitalizations from the hyperkalemia cohort and all of the hospitalizations from the nonhyperkalemia cohort. The hyperkalemia-related hospitalizations and hospitalizations unrelated to hyperkalemia were matched using the same patient characteristics/comorbidities/treatments as previously described. In this sample, patients could contribute to more than 1 hospitalization, with each treated as an index hospitalization.
Readmission rates within 30, 60, and 90 days postdischarge, LOS per readmission, and total inpatient days within 1 year of discharge were compared between cohorts using generalized estimating equation models. The analyses were also conducted in the subgroups of patients with key hyperkalemia-related comorbidities. In addition, the proportion of readmissions related to hyperkalemia were described among all hyperkalemia-related hospitalizations and in the CKD and/or HF subgroup.
Adjusted Multivariable Comparisons
Multivariable generalized estimating equation regression models were used to compare the postdischarge outcomes between cohorts, adjusting for diabetes, hypertension, age, sex, insurance type, region, and Charlson Comorbidity Index, in addition to the matching variables. The 95% confidence intervals (CIs) and P values for the adjusted comparisons were obtained using a bootstrap with 1000 replications.
Adjusted comparisons of total all-cause health care costs were performed among patient subgroups including CKD, HF, CKD and/or HF, CKD stage (stages 3–5 and unspecified), dialysis treatment, diabetes, and hypertension.
All analyses were conducted using SAS version 9.4 (SAS Institute, Inc., Cary, NC).
Sensitivity Analysis
The following sensitivity analyses were implemented to assess the robustness of the results. First, patients on dialysis were excluded to evaluate the impact of this group of patients on the cost and readmission rate difference between cohorts. Second, the characteristics of hospitalization may be different between patients with and without hyperkalemia. Thus, the discharge status, LOS, index year, index month, and index day of the week of the index hospitalization were further adjusted to assess the robustness of the difference in total all-cause health care costs. Compared with an earlier time point during the baseline period, use of potassium-altering medications and other medications at the hospital admission may be more related to the admission and its outcomes. Therefore, an additional sensitivity analysis for the 1-year cost and HRU with further adjustment for individual RAASi classes (ARAs, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and direct renin inhibitors), potassium supplements, loop diuretics, and overall medication burden (i.e., total number of unique medications) at the time of the index hospital admission was conducted.
Results
Patient Characteristics
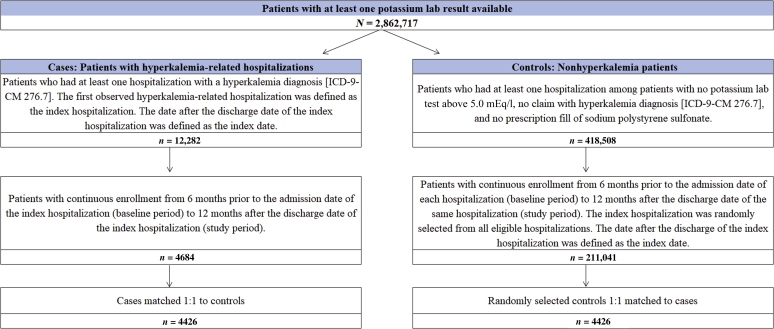
A total of 4426 patients from the hyperkalemia cohort were identified and matched to 4426 controls (Figure 1). CKD stage, dialysis treatment, HF, diagnosis-related group-defined comorbidities, MDCs, and RAASi use were exactly balanced as a result of the matching. The matched pairs were similar with respect to age (mean, 63.7 vs. 62.8 years; P = 0.701) and a greater proportion of the hyperkalemia cohort were male compared with controls (54.0% vs. 45.2%; P < 0.001). The hyperkalemia cohort had a significantly higher prevalence of diabetes (52.6% vs. 40.8%; P < 0.001) and higher Charlson Comorbidity Index (3.7 vs. 3.0; P < 0.001) compared with controls. The proportions for diagnosis-related group-defined HF, pneumonia, and acute myocardial infarction were 3.1%, 1.6%, and 1.2%, respectively. The most common MDCs were disorders of the kidney and urinary tract (20.8%), disorders of the circulatory system (17.6%), and endocrine, nutritional, and metabolic diseases and disorders (12.6%). RAASi use among the hyperkalemia cohort and the nonhyperkalemia cohort during the baseline period was 58.9%, and 12.8% of the hyperkalemia cohort used sodium polystyrene sulfonate. The proportions of patients using angiotensin-converting enzyme inhibitors, ARAs, and loop diuretics were slightly higher in the hyperkalemia cohort than the nonhyperkalemia cohort at the time of index hospital admission; whereas the use of direct renin inhibitors and potassium supplements were similar between the 2 cohorts. Patients in the hyperkalemia cohort had a significantly longer LOS and a smaller percentage discharged to home or self-care (Table 1).
Figure 1.
Selection of patients with hyperkalemia-related hospitalizations and patients with hospitalizations unrelated to hyperkalemia. ICD-9-CM, International Classification of Diseases, 9th Revision, Clinical Modification.
Table 1.
Baseline characteristics of patients with hyperkalemia-related hospitalizations and matched patients with index hospitalization unrelated to hyperkalemia
| Patient characteristics | Patients with hyperkalemia-related hospitalizations |
Patients with index hospitalization unrelated to hyperkalemia |
P |
|---|---|---|---|
| n = 4426 | n = 4426 | ||
| Demographics | |||
| Age, mean (SD) | 63.7 (15.6) | 62.8 (16.3) | 0.701 |
| Men, n (%) | 2391 (54.0) | 2002 (45.2) | <0.001a |
| Region, n (%) | 0.09 | ||
| North Central | 1906 (43.1) | 1721 (38.9) | |
| South | 1224 (27.7) | 1269 (28.7) | |
| Northeast | 796 (18.0) | 798 (18.0) | |
| West | 499 (11.3) | 637 (14.4) | |
| Unknown | 1 (0.0) | 1 (0.0) | |
| Health insurance type, n (%) | 0.012a | ||
| Comprehensive | 1553 (35.1) | 1367 (30.9) | |
| Preferred provider organization | 1450 (32.8) | 1484 (33.5) | |
| Health maintenance organization | 923 (20.9) | 1030 (23.3) | |
| Noncapitated point-of-service | 280 (6.3) | 289 (6.5) | |
| Exclusive provider organization | 40 (0.9) | 35 (0.8) | |
| Consumer-driven health plan | 35 (0.8) | 68 (1.5) | |
| Health deductible health plan | 20 (0.5) | 33 (0.7) | |
| Capitated or partially-capitated point-of-service | 7 (0.2) | 5 (0.1) | |
| Unknown | 118 (2.7) | 115 (2.6) | |
| Disease characteristics | |||
| Hyperkalemia-related comorbidities, n (%) | |||
| Chronic kidney disease (CKD) | 1809 (40.9) | 1809 (40.9) | — |
| CKD stage 3 | 736 (16.6) | 736 (16.6) | — |
| CKD stage 4 | 355 (8.0) | 355 (8.0) | — |
| CKD stage 5 | 301 (6.8) | 301 (6.8) | — |
| CKD stage unspecified | 417 (9.4) | 417 (9.4) | — |
| Dialysis treatment | 407 (9.2) | 407 (9.2) | — |
| HF | 1473 (33.3) | 1473 (33.3) | — |
| Diabetes | 2327 (52.6) | 1808 (40.8) | <0.001a |
| Hypertension | 3573 (80.7) | 3488 (78.8) | 0.67 |
| Charlson Comorbidity Index, mean (SD) | 3.7 (2.5) | 3.0 (2.4) | <0.001a |
| Length of stay, d, mean (SD) | 9.6 (16.2) | 6.3 (8.7) | <0.001a |
| Selected comorbidities by diagnosis-related group, n (%) | — | ||
| HF | 138 (3.1) | 138 (3.1) | — |
| Pneumonia | 70 (1.6) | 70 (1.6) | — |
| Acute myocardial infarction | 51 (1.2) | 51 (1.2) | — |
| Major diagnostic categories of the index hospitalization | — | ||
| Diseases and disorders of the kidney and urinary tract | 921 (20.8) | 921 (20.8) | — |
| Diseases and disorders of the circulatory system | 778 (17.6) | 778 (17.6) | — |
| Endocrine, nutritional, and metabolic diseases and disorders | 558 (12.6) | 558 (12.6) | — |
| Diseases and disorders of the digestive system | 405 (9.2) | 405 (9.2) | — |
| Diseases and disorders of the respiratory system | 370 (8.4) | 370 (8.4) | — |
| Diseases and disorders of the musculoskeletal system and connective tissue | 346 (7.8) | 346 (7.8) | — |
| Other | 1048 (23.7) | 1048 (23.7) | — |
| Discharge status | <0.001a | ||
| Discharged to home or self-care | 2849 (64.4) | 3311 (74.8) | |
| Discharged/Transferred to home health service | 735 (16.6) | 546 (12.3) | |
| Discharged/Transferred to SNF | 417 (9.4) | 278 (6.3) | |
| Transferred to inpatient rehab facility | 142 (3.2) | 71 (1.6) | |
| Others | 179 (4.0) | 96 (2.2) | |
| Missing | 104 (2.3) | 124 (2.8) | |
| Medication use during the baseline period, n (%) | |||
| Renin-angiotensin-aldosterone system inhibitors (RAASi) use | 2609 (58.9) | 2609 (58.9) | — |
| Sodium polystyrene sulfonate | 566 (12.8) | 0 (0.0) | — |
| Medication use at the time of the index admission | |||
| Number of unique medications at baseline, mean (SD) | 5.6 (4.1) | 4.9 (3.8) | <0.001a |
| RAASi use, n (%) | 2027 (45.8) | 1976 (44.7) | 0.092 |
| ACEi | 1283 (29.0) | 1145 (25.9) | <0.001a |
| ARBs | 645 (14.6) | 794 (17.9) | <0.001a |
| ARAs | 369 (8.3) | 124 (2.8) | <0.001a |
| Direct renin inhibitors | 28 (0.6) | 25 (0.6) | 0.675 |
| Potassium supplement, n (%) | 9 (0.2) | 12 (0.3) | 0.514 |
| Loop diuretics, n (%) | 903 (20.4) | 739 (16.7) | <0.001a |
ACEi, angiotensin-converting enzyme inhibitors; ARAs, aldosterone receptor antagonists; ARBs, angiotensin receptor blockers; HF, heart failure; SNF, skilled nursing facility.
P < 0.05 is significant.
Health Care Costs and Resource Use
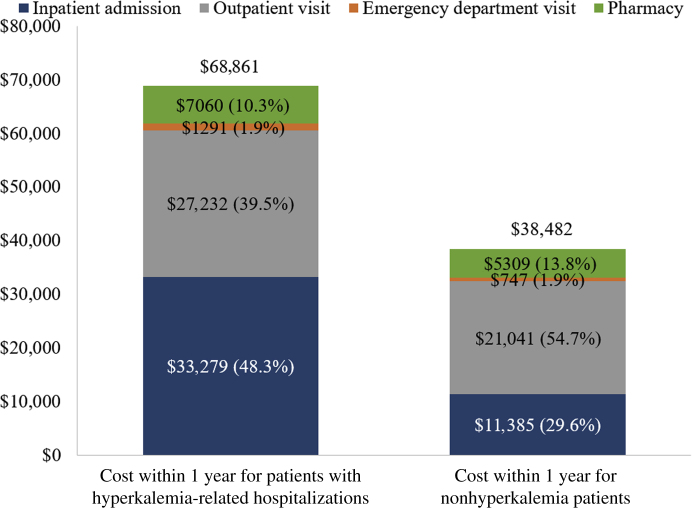
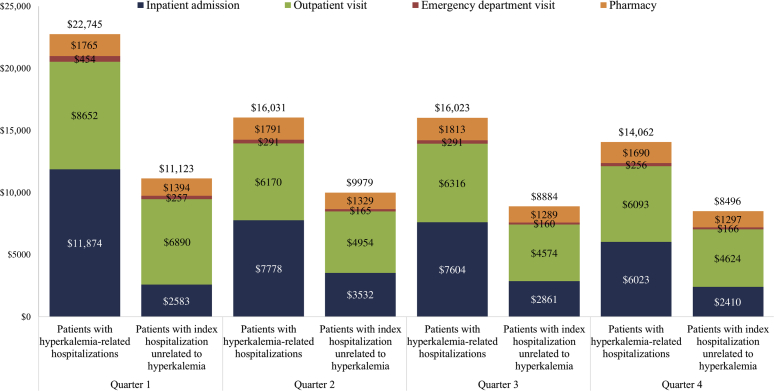
During the 1-year study period, the hyperkalemia cohort incurred $30,379 (95% CI, $25,423–$35,335) higher total all-cause health care costs compared with controls ($68,861 vs. $38,482; P < 0.001). Inpatient costs were the main cost driver among the hyperkalemia cohort, who incurred $21,894 higher inpatient costs compared with controls ($33,279 vs. $11,385) (Figure 2). Moreover, the hyperkalemia cohort had consistently higher total all-cause health care costs in each quarter, with the greatest cost difference within the first quarter after discharge (difference Q1: $11,622; Q2: $6051; Q3: $7139; Q4: $5566; all P < 0.001) (Figure 3). In the adjusted analyses, the 1-year and quarterly cost results were largely consistent with the matched unadjusted analyses. The hyperkalemia cohort incurred $29,161 (95% CI, $24,634–$33,730) higher total all-cause health care costs compared with controls within the 1-year study period. This cost difference was robust to further adjustments for discharge status, LOS, index year, index month, and index day of the week ($28,057 [95% CI, $23,659–$32,209]). The cost difference was similar after adjusting for the use of individual RAASi classes, loop diuretics, potassium supplements, and total number of unique medications at the time of the hospital admission ($26,640 [95% CI, $22,551–$30,892], P < 0.001). The hyperkalemia cohort also incurred higher total all-cause health care costs in each quarter compared with controls (Q1: $10,255, Q2: $6496, Q3: $6784, Q4: $5376; all P < 0.001).
Figure 2.
Comparison of postdischarge total all-cause health care costs between overall patients with hyperkalemia-related hospitalizations and matched patients with hospitalizations unrelated to hyperkalemia during the 1-year postdischarge period.
Figure 3.
Comparison of postdischarge total all-cause health care costs between patients with hyperkalemia-related hospitalizations and matched patients with hospitalizations unrelated to hyperkalemia by quarter.
Compared with the nonhyperkalemia cohort, the hyperkalemia cohort had significantly higher rates of inpatient admissions (1.0 vs. 0.4), outpatient visits (49.6 vs. 39.1), and ED visits (2.0 vs. 1.2) during the 1-year study period after discharge from the index hospitalization (all P < 0.001). Similarly, more patients in the hyperkalemia cohort had at least 1 inpatient visit (49.6% vs. 26.2%; P < 0.001) and at least 1 ED visit (61.3% vs. 46.7%; P < 0.001) compared with controls (Table 2). The comparisons of HRU remained robust in the adjusted analyses: patients in the hyperkalemia cohort had significantly higher rates of inpatient admissions (1.0 vs. 0.4, P < 0.001), outpatient visits (48.2 vs. 40.3, P < 0.001), and ED visits (1.9 vs. 1.2, P < 0.001). The comparisons of HRU were similar after adjusting for the use of individual RAASi classes, loop diuretics, potassium supplements and total number of unique medications at the time of the hospital admission, with patients in the hyperkalemia cohort demonstrating significantly higher rates of inpatient admissions (0.9 vs. 0.4, P < 0.001), outpatient visits (47.9 vs. 40.5, P < 0.001), and ED visits (1.9 vs. 1.2, P < 0.001).
Table 2.
Comparison of postdischarge all-cause health care resource utilization of overall patients with hyperkalemia-related hospitalizations and matched patients with index hospitalization unrelated to hyperkalemia
| Resource utilization within 1 year | Patients with hyperkalemia-related hospitalizations |
Patients with index hospitalization unrelated to hyperkalemia |
Difference (95% CI) | P |
|---|---|---|---|---|
| n = 4426 | n = 4426 | |||
| Number of all-cause health care visits, mean (SD) | ||||
| Inpatient admission | 1.00 (1.61) | 0.41 (0.88) | 0.59 (0.54–0.65) | <0.001a |
| Outpatient visit | 49.62 (45.55) | 39.11 (41.83) | 10.51 (8.69–12.33) | <0.001a |
| Emergency department visit | 1.97 (3.28) | 1.18 (2.45) | 0.79 (0.67–0.91) | <0.001a |
| Presence of at least 1 all-cause health care visit, % mean (SD) | ||||
| Inpatient admission | 49.57 (50.00) | 26.23 (43.99) | 23.34 (21.38–25.30) | <0.001a |
| Outpatient visit | 99.80 (4.50) | 99.75 (4.98) | 0.05 (−0.15 to 0.24) | 0.654 |
| Emergency department visit | 61.32 (48.70) | 46.70 (49.89) | 14.62 (12.56–16.67) | <0.001a |
CI, confidence interval.
P values < 0.05 are significant.
Among all subgroups, patients with hyperkalemia-related hospitalizations incurred significantly higher total all-cause costs during the 1-year study period compared with controls. The total all-cause health care cost difference between the matched pairs was $29,397 ($74,351 vs. $44,955; P < 0.001) among patients with CKD and/or HF, $28,794 ($66,961 vs. $38,166) among patients with CKD, $29,109 ($94,336 vs. $65,227) among patients with CKD stage 5, $20,516 ($55,446 vs. $34,929) among patients with CKD stage 4, $30,927 ($65,064 vs. $34,137) among patients with CKD stage 3, and $31,850 ($60,351 vs. $28,500) among patients with unspecified CKD stage, $29,878 ($82,486 vs. $52,608) among patients with HF, $30,507 ($72,083 vs. $41,577) among patients with diabetes, $29,268 ($70,187 vs. $40,919) among patients with hypertension, and $42,146 ($147,310 vs. $105,164) among patients with dialysis treatment (all P < 0.001) (Table 3). After the baseline characteristics were further adjusted, the results remained largely unchanged from the unadjusted results in all subgroups. In addition, the difference in 1-year postdischarge health care cost was similar among patients without dialysis ($29,187 [$60,917 vs. $31,729]), compared with the difference observed in the overall population.
Table 3.
Comparison of postdischarge total all-cause health care costs of patients with hyperkalemia-related hospitalizations and matched patients with index hospitalization unrelated to hyperkalemia during the 1-year postdischarge period by subgroups
| Patient subgroups | Number of pairs | Patients with hyperkalemia-related hospitalizations, $ |
Patients with index hospitalization unrelated to hyperkalemia, $ |
Difference, $ (95% CI) | P |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | ||||
| Patients with CKD and/or HF | 2509 | 74,351 (145,478) | 44,955 (120,621) | 29,397 (22,004–36,790) | <0.001a |
| Patients with CKD | 1809 | 66,961 (135,515) | 38,166 (74,066) | 28,794 (21,680–35,909) | <0.001a |
| CKD stage 5 | 301 | 94,336 (135,750) | 65,227 (122,738) | 29,109 (8,469–49,750) | 0.006a |
| CKD stage 4 | 355 | 55,446 (76,012) | 34,929 (55,386) | 20,516 (10,747–30,286) | <0.001a |
| CKD stage 3 | 736 | 65,064 (148,342) | 34,137 (66,168) | 30,927 (19,200–42,654) | <0.001a |
| Unspecified CKD stage | 417 | 60,351 (148,398) | 28,500 (44,392) | 31,850 (17,001–46,699) | <0.001a |
| Patients with dialysis | 407 | 147,310 (188,949) | 105,164 (136,889) | 42,146 (19,506–64,786) | <0.001a |
| Patients with HF | 1473 | 82,486 (163,305) | 52,608 (146,277) | 29,878 (18,686–41,070) | <0.001a |
| Patients with diabetes | 2327 | 72,083 (117,550) | 41,577 (119,038) | 30,507 (23,711–37,303) | <0.001a |
| Patients with hypertension | 3573 | 70,187 (130,871) | 40,919 (107,871) | 29,268 (23,708–34,829) | <0.001a |
| Other patients | 362 | 55,568 (104,157) | 22,732 (92,314) | 32,836 (18,518–47,153) | <0.001a |
CI, confidence interval; CKD, chronic kidney disease; HF, heart failure.
P values < 0.05 are significant.
Readmission and LOS
The readmission and LOS were assessed in 5377 pairs of matched hospitalizations. Compared with hospitalizations unrelated to hyperkalemia, hyperkalemia-related hospitalizations had higher rates of readmission within 30 days (0.15 vs. 0.09), 60 days (0.25 vs. 0.16), and 90 days (0.36 vs. 0.23) of index discharge date (all P < 0.001). A higher proportion of hyperkalemia-related hospitalizations had at least 1 readmission within 30 days (12.5% vs. 8.4%), 60 days (18.3% vs. 12.7%), and 90 days (24.3% vs. 16.8%) of the index discharge date compared with controls (all P < 0.001). Consistently, hyperkalemia-related hospitalizations in patients with CKD and/or HF had higher rates of readmission within 30 days (0.16 vs. 0.11), 60 days (0.28 vs. 0.18), and 90 days (0.41 vs. 0.26) of the index hospitalization (all P < 0.001), and a higher proportion with at least one readmission within 30 days (13.8% vs. 9.4%), 60 days (19.8% vs. 14.3%), and 90 days (26.5% vs. 19.2%) of the index discharge date (all P < 0.001). The adjusted analyses identified similar results. The results for the overall population were robust to the exclusion of patients with dialysis treatment.
Patients with hyperkalemia-related hospitalizations had longer LOS per readmission (8.1 vs. 7.1 days; P < 0.001) and more total inpatient days within the 1-year study period (10.5 vs. 5.8 days; P < 0.001) compared with hospitalizations unrelated to hyperkalemia (Table 4). In addition, hyperkalemia-related hospitalizations in patients with CKD and/or HF also had a longer LOS per readmission (8.4 vs. 7.4 days) and more total inpatient days (12.4 vs. 7.2 days) compared with control hospitalizations (all P < 0.001). The adjusted analyses identified similar results.
Table 4.
Comparison of inpatient readmissions between hyperkalemia-related hospitalizations and matched hospitalizations unrelated to hyperkalemia
| Inpatient readmissions, mean (SD) | Hyperkalemia-related hospitalizations |
Hospitalizations unrelated to hyperkalemia |
Difference (95% CI) | P |
|---|---|---|---|---|
| n hospitalizations = 5377 | n hospitalizations = 5377 | |||
| Number of inpatient readmissions | ||||
| Within 30 days of index discharge date | 0.15 (0.42) | 0.09 (0.32) | 0.05 (0.04–0.07) | <0.001a |
| Within 60 days of index discharge date | 0.25 (0.62) | 0.16 (0.47) | 0.09 (0.07–0.11) | <0.001a |
| Within 90 days of index discharge date | 0.36 (0.79) | 0.23 (0.59) | 0.13 (0.11–0.16) | <0.001a |
| Presence of at least 1 inpatient readmission, % | ||||
| Within 30 days of index discharge date | 12.5 (33.05) | 8.4 (27.78) | 4.1 (2.9–5.2) | <0.001a |
| Within 60 days of index discharge date | 18.3 (38.67) | 12.7 (33.34) | 5.6 (4.2–6.9) | <0.001a |
| Within 90 days of index discharge date | 24.3 (42.88) | 16.8 (37.38) | 7.5 (6.0–9.0) | <0.001a |
| Length of stay/total inpatient days | ||||
| Length of stay per readmission | 8.1 (9.0) | 7.1 (7.0) | 1.0 (0.5–1.4) | <0.001a |
| Total inpatient days | 10.5 (23.5) | 5.8 (13.8) | 4.7 (4.0–5.4) | <0.001a |
CI, confidence interval.
P < 0.05 is significant.
In the group for hyperkalemia-related hospitalizations, hyperkalemia-related readmissions accounted for 22.65% of all readmissions by 30 days (178 of 786), 21.38% of all readmissions by 60 days (289 of 1352), and 20.27% of all readmissions by 90 days (393 of 1939). Among patients with CKD and/or HF, hyperkalemia-related readmissions accounted for 26.98% readmissions by 30 days (143 of 530), 25.05% of readmissions by 60 days (228 of 910), and 23.18% readmissions by 90 days (308 of 1329).
Discussion
Hyperkalemia is an electrolyte abnormality associated with a high economic burden.14, 15, 16 Given that the inpatient burden was a major driver of the incremental burden of hyperkalemia, the present study focused specifically on the time period after discharge from hyperkalemia-related hospitalizations. This study is among the first to evaluate the postdischarge economic and readmission burdens associated with hyperkalemia-related hospitalizations in the real world.
This study found persistent postdischarge economic burden of hyperkalemia over the 1-year study period with inpatient admissions contributing to 72% of the total all-cause health care cost difference between the matched pairs. Compared with hospitalizations unrelated to hyperkalemia, hyperkalemia-related hospitalizations had 56% to 58% higher rates of readmission within 30, 60, and 90 days of the index discharge date (44%–48% higher in the presence of at least 1 inpatient readmission), a longer LOS per readmission, and nearly twice the total inpatient days within the 1-year study period compared with control hospitalizations. In addition, 23.4% of patients were rehospitalized following 90 days of a hyperkalemia-related hospitalization. Although patients on dialysis may have a higher range of costs compared with nondialysis patients, the sensitivity analyses of removing patients on dialysis suggest that the cost and readmission comparisons in the 2 cohorts were robust and not driven by patients on dialysis.
The unadjusted differences between hyperkalemia and nonhyperkalemia cohorts may be driven by underlying conditions or their severity, thus we carefully accounted for this through multiple measures. First, matching on key hyperkalemia-related comorbidities minimized baseline differences between cohorts. Matching on MDCs during the index hospitalization further balanced differences between hyperkalemia-related hospitalizations and hospitalizations unrelated to hyperkalemia. In addition to matching, adjusting for other potential confounders further mitigated the difference of the comparisons. Considering the between-cohort differences in the characteristics of the index hospitalization, the present study also performed an adjusted analysis to further adjust for discharge status, LOS, index year, index month, and index day of the week. However, discharge status and LOS could be downstream effects from the index hyperkalemia event and thus adjusting for these variables would present conservative estimates. The fact that such further adjustments only slightly decrease the cost difference estimates suggest the robustness of the results. Furthermore, to account for differences in medication use between the cohorts, the present study conducted an additional sensitivity analysis adjusting for individual RAASi classes, potassium supplements, loop diuretics, and total number of unique medications used at the time of the index hospital admission. The results were again robust to the additional adjustments. Although residual confounding due to unmeasured or unobserved variables is possible, the consistent finding that a hyperkalemia-related hospitalization was associated with a significantly higher postdischarge burden from the adjusted regression results (including results from multiple sensitivity analyses) strengthened the findings.
The high incremental postdischarge economic and readmission burdens may be attributable to lack of monitoring and the absence of outpatient treatment following discharge. Close monitoring and timely treatment after discharge from a hyperkalemia-related hospitalization should be considered and may help to reduce the economic burden, particularly among patients who are at a high risk of recurrence.
Clinical practice guidelines regarding potassium monitoring in patients with hyperkalemia are needed. Therefore, future studies are warranted to evaluate predictors of hyperkalemia recurrence and hyperkalemia-related readmissions. Additional studies are also needed to evaluate postdischarge treatment patterns for hyperkalemia (e.g., sodium polystyrene sulfonate prescriptions and other potassium-binding agents) to shed light on potential treatment gaps following hyperkalemia-related hospitalizations.
This study fills an important gap in the current literature regarding the economic and readmission burden of hyperkalemia during the postdischarge period. Notable strengths of this study include the use of a large sample of patients with a hyperkalemia-related hospitalization, which is representative of the US commercially insured population. Furthermore, a comprehensive evaluation of health care costs, HRU, and readmission outcomes within patient subgroups may be used as quality metrics to evaluate hospitalization performance.
Findings from this study should be interpreted in light of its limitations. First, although the hyperkalemia-related hospitalizations and hospitalizations were matched by demographic characteristics, key hyperkalemia-related comorbidities, and other comorbidities, some potentially relevant comorbidities and demographic factors (e.g., race) could not be matched between cohorts due to unavailability of data in the MarketScan database. Second, comorbidities were identified using diagnostic codes that are intended for administrative purposes; thus, the prevalence of some comorbidities may be underestimated. Third, the study population was specific to commercially insured patients, and therefore, results may not be generalizable to the entire US population, including the uninsured.
Conclusion
Hyperkalemia-related hospitalizations were associated with substantial postdischarge economic and readmission burdens 1-year postdischarge, in both the overall population and patient subgroups. Almost one-quarter of hyperkalemia-related hospitalizations resulted in readmission within 90 days, with the readmission rate within 90 days 58% higher than hospitalizations unrelated to hyperkalemia. These postdischarge outcomes have important financial implications for payers. The high postdischarge burden of hyperkalemia-related hospitalizations indicates an unmet need for safe and effective treatment options and improved management of hyperkalemia after inpatient care.
Disclosure
JMW is a former employee of AstraZeneca and owns stock/stock options. KAB, FM, YaoW, YanW, AD, and EQW are employees of Analysis Group Inc., which has received consultancy fees from AstraZeneca.
Acknowledgments
The authors thank Sneha Kelkar and Cheryl Xiang for their contribution to the manuscript. This study was funded by AstraZeneca. Medical writing assistance was provided by Gloria DeWalt, PhD, an employee of Analysis Group, Inc. Funding for this support was provided by the sponsor.
Footnotes
Table S1. ICD-9-CM code for hyperkalemia-related comorbidities.
Table S2. Procedure codes for dialysis and hemodialysis.
Supplementary Material
References
- 1.An J.N., Lee J.P., Jeon H.J. Severe hyperkalemia requiring hospitalization: predictors of mortality. Crit Care. 2012;16:R225. doi: 10.1186/cc11872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dunn J.D., Benton W.W., Orozco-Torrentera E., Adamson R.T. The burden of hyperkalemia in patients with cardiovascular and renal disease. Am J Manag Care. 2015;21(15 Suppl):s307–s315. [PubMed] [Google Scholar]
- 3.Goyal A., Spertus J.A., Gosch K. Serum potassium levels and mortality in acute myocardial infarction. JAMA. 2012;307:157–164. doi: 10.1001/jama.2011.1967. [DOI] [PubMed] [Google Scholar]
- 4.Jain N., Kotla S., Little B.B. Predictors of hyperkalemia and death in patients with cardiac and renal disease. Am J Cardiol. 2012;109:1510–1513. doi: 10.1016/j.amjcard.2012.01.367. [DOI] [PubMed] [Google Scholar]
- 5.Allon M. Hyperkalemia in end-stage renal disease: mechanisms and management. J Am Soc Nephrol. 1995;6:1134–1142. doi: 10.1681/ASN.V641134. [DOI] [PubMed] [Google Scholar]
- 6.Kovesdy C.P. Management of hyperkalaemia in chronic kidney disease. Nat Rev Nephrol. 2014;10:653–662. doi: 10.1038/nrneph.2014.168. [DOI] [PubMed] [Google Scholar]
- 7.Hayes J., Kalantar-Zadeh K., Lu J.L. Association of hypo- and hyperkalemia with disease progression and mortality in males with chronic kidney disease: the role of race. Nephron Clin Pract. 2012;120:c8–c16. doi: 10.1159/000329511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Betts K.A., Woolley J.M., Mu F. The prevalence of hyperkalemia in the United States. Curr Med Res Opin. 2018;34:971–978. doi: 10.1080/03007995.2018.1433141. [DOI] [PubMed] [Google Scholar]
- 9.Acker C.G., Johnson J.P., Palevsky P.M., Greenberg A. Hyperkalemia in hospitalized patients: causes, adequacy of treatment, and results of an attempt to improve physician compliance with published therapy guidelines. Arch Intern Med. 1998;158:917–924. doi: 10.1001/archinte.158.8.917. [DOI] [PubMed] [Google Scholar]
- 10.Nyirenda M.J., Tang J.I., Padfield P.L., Seckl J.R. Hyperkalaemia. BMJ. 2009;339:b4114. doi: 10.1136/bmj.b4114. [DOI] [PubMed] [Google Scholar]
- 11.Mushiyakh Y., Dangaria H., Qavi S. Treatment and pathogenesis of acute hyperkalemia. J Community Hosp Intern Med Perspect. 2011;1(4) doi: 10.3402/jchimp.v1i4.7372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khanagavi J., Gupta T., Aronow W.S. Hyperkalemia among hospitalized patients and association between duration of hyperkalemia and outcomes. Arch Med Sci. 2014;10:251–257. doi: 10.5114/aoms.2014.42577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McMahon G.M., Mendu M.L., Gibbons F.K., Christopher K.B. Association between hyperkalemia at critical care initiation and mortality. Intensive Care Med. 2012;38:1834–1842. doi: 10.1007/s00134-012-2636-7. [DOI] [PubMed] [Google Scholar]
- 14.Betts KA, Woolley JM, Mu F, et al. Economic burden of hyperkalemia in Medicare patients. American Society of Nephrology Annual Meeting; October 31–November 05, 2017; New Orleans.
- 15.Betts K.A., Woolley J.M., Mu F. The cost of hyperkalemia in the United States. Kidney Int Rep. 2018;3:385–393. doi: 10.1016/j.ekir.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fitch K., Woolley J.M., Engel T., Blumen H. The clinical and economic burden of hyperkalemia on medicare and commercial payers. Am Health Drug Benefits. 2017;10:202–210. [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Medicare & Medicaid Services ICD-10-CM/PCS MS-DRG v34.0 Definitions Manual. https://www.cms.gov/ICD10Manual/version34-fullcode-cms/fullcode_cms/P0372.html Available at: [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.