Introduction
Noninfectious complications of peritoneal dialysis (PD) are increasing in relative importance with success in decreasing the rate of infections such as PD peritonitis.1 Noninfectious complications of PD include obstructions, fistulas, as well as unusual exit site complications.2 Obstructions can result from various causes including omental wraps and fallopian tube wraps,3, 4, 5 and can also lead to communications/fistulas between the bladder and colonic walls.6,7 Dialysate leaks represent 1 of the major noninfectious complications of PD.
Case Presentation
The patient is a 42-year-old African American woman with a past medical history of lupus nephritis and end-stage renal disease on continuous cycler (automated) PD for 5 years, with poor compliance with dialysis and recurrent episodes of peritonitis. Her last prescription was 2 liter exchanges, 4 cycles overnight, no last fill with 1.5% and 2.5% alternating concentrations. There had been 2 known prior episodes in the past 2 years; however, details were not available because of changes in providers and patient’s inability to recall the exact time course. The patient reported a new episode of abdominal pain worse than ever before, and also reported intermittent incontinence and increasing painless vaginal discharge. She was treated for repeat peritonitis and vaginitis/cervicitis. There was some improvement in her pain for a short period, but she continued to report nonresolving vaginal discharge. She also reported that the discharge occurred mostly during the fill cycle of PD. She was admitted for possible nonresolving peritonitis needing further investigation. Peritoneal dialysis was resumed in the hospital to continue dialysis. Within 1 hour of resuming dialysis, she had a large amount of vaginal discharge, wetting the bed despite having pads in place. This fluid was tested by bedside urine dipstick, which was positive for glucose, raising concern for PD fluid leak. Gynecology services were urgently consulted, but their detailed pelvic examination did not reveal an overt fistula or opening in the vaginal vault. Urgent noncontrast magnetic resonance imaging was done, which showed the PD catheter in the left lower quadrant, looping posterior to the uterus in the rectouterine space, around multiloculated T2 hyperintense fluid pockets. The radiologist reported that this represented a combination of fallopian tubes and loculated pockets of peritoneal fluid/cocooning. Significant distension of the vagina with complex T2 heterogeneous material was seen, which, per history, was consistent with dialysate or menstrual fluid. No perforation of the uterus or vagina was seen. A small fluid-filled tract coursing in the rectovaginal space from the 9 o’clock to 12 o’clock positions of the rectum, coming into close contact with the right posterior vaginal fornix, was seen. This was presumed to represent a potential site of fistulous communication. For confirmation, a computed tomography (CT) scan with contrast was performed. This also showed the PD catheter to be coiled in the pouch of Douglas. However, the contrast medium traveled through the catheter and then through the right fallopian tube, entered the uterus, and extended through the cervix into the vagina (Figure 1). It appears that the patient had formed loculated pouches on the pelvic floor, and that 1 pouch had the PD catheter in direct communication with the fallopian tube. The PD dialysate was traveling directly through the anatomically intact fallopian tube. The patient then underwent an open exploratory laparotomy, which showed multiple adhesions requiring surgical enterolysis and drainage of the pseudocysts with right salpingectomy. The PD catheter was a double-cuff swan-neck Tenckhoff catheter with a coiled tip. The patient was transitioned to hemodialysis.
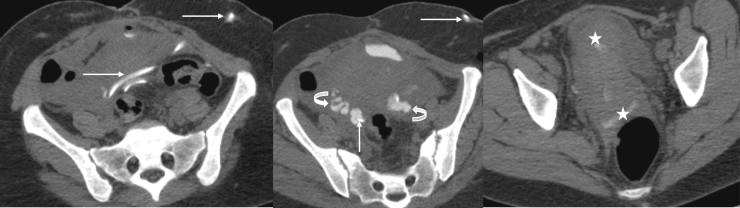
Figure 1.
Contiguous axial computed tomography images after instillation of contrast medium through the peritoneal dialysis catheter (straight arrows) shows an accumulation of contrast medium within both fallopian tubes (curved arrows), with subsequent communication into the endometrium and finally through the vagina (asterisks).
Following salpingectomy, the patient was transitioned to hemodialysis. There were no further episodes of vaginal discharge. She was followed for 1.5 years postoperatively, and continued to report no ongoing issues.
Discussion
This case highlights the differential diagnosis of vaginal discharge in a young PD patient. The case also calls attention to an unusual presentation of a relatively common, noninfectious complication of a patient on PD, namely, that of PD fluid leak.
A small amount of vaginal discharge (<5 ml) is normal in women of reproductive age, varying in amount and character based on hormonal influences.S1 Initial evaluation of a patient with vaginal discharge needs a dedicated history with physical examination including speculum examination with cystoscopy testing, whiff test, and wet mount microscopy.S2
If the diagnosis is unclear, further evaluations are recommended. Differential diagnosis of abnormal vaginal discharges includes vaginal and cervical infections, retained foreign body, and abnormal fistulas.
Most commonly, vaginal infections are trichomoniasis, candidiasis, and bacterial vaginosis, each with its own characteristic presentation. Trichomoniasis is characterized by a purulent malodorous discharge that is usually accompanied by dyspareunia, pruritus, or dysuria. Candidiasis discharge is scant, yogurt-like, and thick, whereas vaginosis has thin malodorous gray discharge.S3 In sexually active women, sexually transmitted diseases such as gonorrhea and chlamydia are also a concern. Common causes of cervicitis can be ascending vaginal/vulvovaginal infections or noninfectious causes such as spermicides and chemical douches.S4
Retained foreign bodies may include tampons and pessaries. This patient reported no such history, and the dedicated examination by the gynecologist did not reveal any such pathology.
With this history and a normal examination, an abnormal fistula was the next differential diagnosis needing further evaluation.
Women with vaginal discharge secondary to urogenital fistulas may have a history of obstructed labor, severe pelvic pathologies such as pelvic inflammatory disease, history of radiation, or history of gynecological surgery. Formation of urogenital fistulas can be expected in patients with a history of systemic inflammatory diseases (e.g., inflammatory bowel disease) where the tissue is already friable and prone to poor healing. Genital fistula, the pathology of highest concern, in this case, could have multiple anatomical pathways. The vaginal vault being flanked anteriorly by the bladder and the urethra, and posteriorly by the rectum, can have fistulous connections from various anatomical sites. Anterior connections lead to vesicovaginal fistulas, which are the most common, whereas ureterovaginal, vesicouterine, vesicoperitoneal, and vesicocolonic fistulas are quite rare and are associated with intraabdominal malignancies. Enterovaginal fistulas such as anovaginal, rectovaginal, and colo-vaginal fistulas usually occur after obstructed labor, nonhealing traumatic perineal laceration or episiotomy infection, Crohn’s disease, or radiation. These patients present with a fecal vaginal discharge, gas through the vagina, and fecal soiling and incontinence. This condition is easily diagnosed during a vaginal examination. Rarely, very small fistulas may need enhanced examination using a colposcope. Small fistulas may be managed conservatively, but usually, the symptoms are quite distressing and thus need surgical corrections.S5 This patient reported no such symptoms.
This patient, with a history of prior episodes of peritonitis, was at risk for having friable tissue, although she had no history of any systemic illness such as Crohn’s disease that could lead to intrabdominal friable tissue.
This patient had reported unusual symptoms such as intermittent incontinence with nonodorous discharge and sudden vaginal discharge. These symptoms were not considered to be related to PD, thus delaying diagnosis (Table 1). Eventually, she was diagnosed with a PD fluid leak through the vagina.
Table 1.
Teaching points
| Abdominal pain and vaginal discharge in a peritoneal dialysis (PD) patient should lead to detailed examination and imaging. |
| Although infectious complications are common, noninfective complications such as obstructions and fistulas are not uncommon. |
| Abnormal fistulas such as catheter−fallopian tube fistulas are possible with excoriations and infections leading to friable organs and also communications through normal anatomy. |
Peritoneal dialysis fluid can leak externally through the exit site, or internally through different communicating anatomical compartments. An external leak is easy to diagnose using a bedside urine dipstick. A high glucose content of the fluid is a hallmark of PD fluid. Interestingly, the dipstick also has additional advantage in certain other cases. Urine dipstick has been used to help diagnose PD peritonitis by the presence of nitrites and leucocyte-esterase.S6 It can also show the presence of blood and bilious leaks. It is used to detect exit site leaks while trying to differentiate serous discharge from that of exit site PD fluid leak, especially when a fluid leak is noted with urgent start PD. In this case, also, the dipstick provided a quick bedside assessment of the origin of this patient’s fluid leak, which prompted further evaluation.
Internal leakage of peritoneal fluid through acquired or congenital communications is a well-known complication of PD. The internal communications are commonly between peritoneum and the pleura, or between the peritoneum and the abdominal wall. Less commonly, PD catheter can excoriate through bowel wall, or form fistulous connections with bladder or uterovaginal vault.S7
Leakage in the pleural space usually presents with symptoms of dyspnea and inadequate ultrafiltration. The chest X-ray of such a patient would show a nonresolving or recurrent hydrothorax or pleural effusion, which is usually right-sided. This PD hydrothorax is considered to form through natural pleuro-peritoneal diaphragmatic communications, lymphatic drainage abnormalities, or due to pleuro-peritoneal pressure differences.S8 Investigation includes thoracentesis, an examination of the pleural fluid, and CT peritoneography or peritoneal scintigraphy.S9,S10 Management of pleural effusion depends on the acuity and severity of the clinical presentation. Treatment ranges from temporary withholding of dialysis to chemical or surgical pleurodesis.
Abdominal wall PD fluid leak usually presents with symptoms of widening girth, peau d’orange appearance of the abdominal wall, and ultrafiltration failure. The edema can extend to the genitalia following natural peritoneal reflections, and can also cause sudden scrotal swelling in men. Investigations include magnetic resonance imaging, in which the PD fluid can serve as a contrast medium and most abdominal pathologies can be well visualized.S11 The treatment of these complications ranges from a temporary withholding of PD to a complete transition to hemodialysis.8 Intestinal perforations can occur with PD catheter excoriation over a bowel segment and may present with fecal peritonitis, usually quite severe in clinical presentation. The patient may present with dialysate diarrhea, and X-ray may show air in the peritoneal cavity.S12 The diagnosis is supported by PD fluid culture showing multiorganisms, especially enteric organisms. A CT scan may be needed to best define the perforation. Management includes laparotomy and surgical correction of the perforation. These patients are commonly transitioned to hemodialysis.
This patient’s abdominal pain was related to peritonitis and loculations in the abdomen, also raising concern for another differential diagnosis, namely, that of encapsulating peritoneal sclerosis (EPS). The CT scan showed unremarkable bowel loops, which was not congruent with EPS presentation. The open laparotomy did appear to be worrisome for a grim diagnosis; however, no dedicated peritoneal biopsies were performed at the time to confirm or to exclude EPS. Because the fallopian tube was sent for pathology, this specimen could be used to further assess the concern for EPS. Sections of the fallopian tube demonstrated acute and chronic inflammation (Figure 2). High-power examination showed cytologic atypia consistent with reactive epithelial changes (Figure 3). In EPS, the normal mesothelial layers of the peritoneum will be replaced by fibroblasts, fibrin, and acute and chronic inflammation, whereas the CT scan would have shown the typical bunched-up appearance due to bowel adhesions and peritoneal thickening.
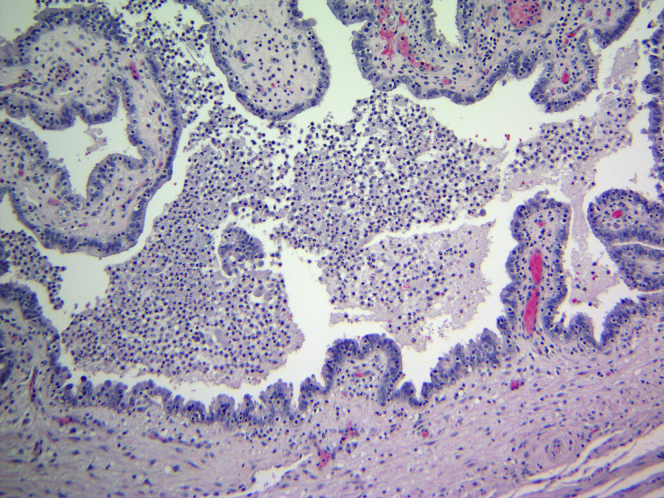
Figure 2.
Sections of the fallopian tube demonstrate acute and chronic inflammation.
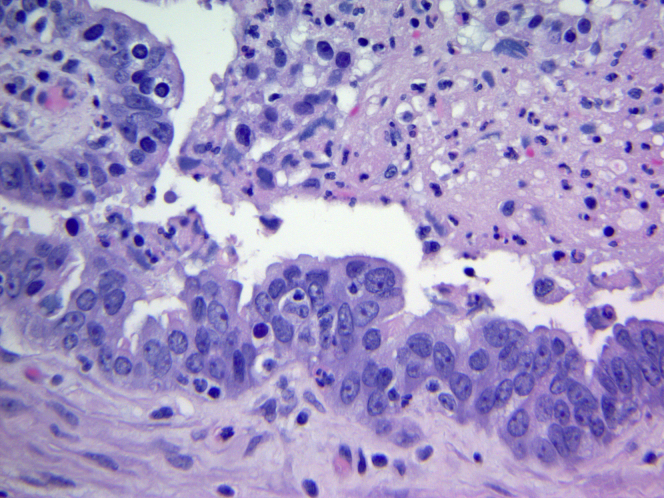
Figure 3.
High-power examination showing cytologic atypia consistent with reactive epithelial changes.
Peritoneal dialysis fluid leakage into the pleural space, abdominal wall, or intestinal perforations are known complications of peritoneal dialysis.8 Vaginal PD fluid leak is not as well known a complication, although there are some very rare case reports of such leaks with a history of some surgical manipulation.9 Abnormal fistulas are possible and can be expected with excoriations and infections leading to friable organs and vaginal PD fluid leak; these are 1 such complication of which nephrologists should be aware. In PD patients, the significance of a bedside urine dipstick in assessing for PD fluid leak is of considerable importance over different scenarios.
This case is unique in that the painless vaginal discharge was occurring through natural communications among the peritoneum, fallopian tube, and vagina. Vaginal discharge in PD patients should lead to detailed examination and imaging.
Disclosure
All the authors declared no competing interests.
Footnotes
Supplementary References.
Supplementary Material
References
- 1.McCormick B.B., Bargman J.M. Noninfectious complications of peritoneal dialysis: implications for patient and technique survival. J Am Soc Nephrol. 2007;18:3023. doi: 10.1681/ASN.2007070796. [DOI] [PubMed] [Google Scholar]
- 2.Siddiqui M., Bradford L., Kaley J. Noninfectious peritoneal dialysis exit site rash—an unusual case report and review of the literature. Kidney Int Rep. 2018;3:11–13. doi: 10.1016/j.ekir.2017.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gudsoorkar P.S., Penner T., Jassal S.V., Bargman J.M. The enigmatic fallopian tube: a more common cause of catheter malfunction than previously recognized. Perit Dial Int. 2016;36:459–461. doi: 10.3747/pdi.2015.00125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cobelo C., Ros S., Trujillo C., Garcia P. An unusual case of vaginal leak in a patient on peritoneal dialysis. Perit Dial Int. 2010;30:665–666. doi: 10.3747/pdi.2010.00016. [DOI] [PubMed] [Google Scholar]
- 5.Moreiras-Plaza M., Caceres-Alvarado M. Peritoneal dialysis catheter obstruction caused by fallopian tube wrapping. Am J Kidney Dis. 2004;44:e28–e30. doi: 10.1053/j.ajkd.2004.04.046. [DOI] [PubMed] [Google Scholar]
- 6.Fleisher A.G., Kimmelstiel F.M., Lattes C.G., Miller R.E. Surgical complications of peritoneal dialysis catheters. Am J Surg. 1985;149:726. doi: 10.1016/s0002-9610(85)80174-4. [DOI] [PubMed] [Google Scholar]
- 7.Yanai K., Ueda Y., Minato S. Delayed peritoneal dialysis catheter-intestinal fistula. Nephrology. 2018;23:890–891. doi: 10.1111/nep.13204. [DOI] [PubMed] [Google Scholar]
- 8.Leblanc M., Ouimet D., Pichette V. Dialysate leaks in peritoneal dialysis. Semin Dial. 2001;14:50–54. doi: 10.1046/j.1525-139x.2001.00014.x. [DOI] [PubMed] [Google Scholar]
- 9.Harrison R., Weber LeBrun E. Repair of vagino-peritoneal fistula caused by vaginal cuff fixation of peritoneal dialysis catheter: a case report. Perit Dial Int. 2015;35:363–365. doi: 10.3747/pdi.2014.00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.