Abstract
Cardiac angiosarcomas are a rare group of soft tissue sarcomas, characterized by aggressive local growth and early spread. Because this is an uncommon disease, there is currently no standard treatment approach. When localized, surgery appears to lead to the best outcomes, but this can be technically challenging and not always feasible. Upfront chemoradiotherapy provides an alternative that may shrink the tumor to enable definitive surgical resection. We report a case of primary cardiac angiosarcoma with a complete metabolic and pathological response after upfront chemoradiotherapy with paclitaxel, who then underwent surgery, as a potential treatment option for patients with this rare condition.
<Learning objective: Cardiac angiosarcoma can present with non-specific symptoms and signs making early diagnosis difficult. When localized, surgery provides the best survival outcomes for patients, but may not be possible due to the extent of invasion into surrounding critical structures. In this case of locally advanced disease in a young patient, there was the opportunity to treat this tumor aggressively with upfront combined chemoradiotherapy followed by surgery, with a dramatic response observed.>
Keywords: Cardiac angiosarcoma, Right heart sarcoma, Chemoradiotherapy
Introduction
Cardiac angiosarcoma is a rare endothelial cell tumor, characterized by an aggressive permeating growth within the surrounding myocardial wall. The majority occur in the right atrium, and can infiltrate into neighboring structures and spread distantly [1].
The diagnosis of cardiac angiosarcoma can be difficult as early symptoms are often nonspecific. Furthermore, severe manifestations can occur, including right heart failure, myocardial rupture, and cardiac tamponade [2]. Multiple investigations can aid in the diagnosis, including echocardiogram, computed tomography (CT), cardiac magnetic resonance imaging (MRI), and positron emission tomography (PET) CT.
Surgical resection is the mainstay of treatment where possible. However, upfront chemoradiotherapy may be an alternative treatment option for unresectable tumors, and paclitaxel has demonstrated activity against angiosarcoma of other sites [3], [4].
Case report
We report a 46-year-old female with a good performance status, who is a lifelong non-smoker. Her intercurrent medical history includes hypertension, Hashimoto's thyroiditis, and factor V Leiden deficiency.
She presented to the Royal Adelaide Hospital with fevers, dyspnea, and a cough. At that time, she was diagnosed with pericarditis. Echocardiogram showed a small-to-moderate pericardial effusion, and no cardiac mass was detected. C-reactive protein level was 334 mg/L and white cell count was 16.7 × 109/L. Anti-inflammatory therapy was commenced, her symptoms resolved, and the patient was discharged after repeat echocardiogram showed a stable effusion. She re-presented three months later with chest pain, dysphagia, dyspnea, and night sweats. Electrocardiogram showed sinus tachycardia. Echocardiogram showed no pericardial effusion, although a right atrial mass was now visible. CT and cardiac MRI showed a 7 × 11 × 10 cm mass in the right atrium and also encasing the right coronary artery (Fig. 1). PET scan showed strong fluorodeoxyglucose avidity, and no evidence of metastatic disease. Initial cardiac biopsy was equivocal, however repeat biopsy confirmed the diagnosis of cardiac angiosarcoma (Fig. 2).
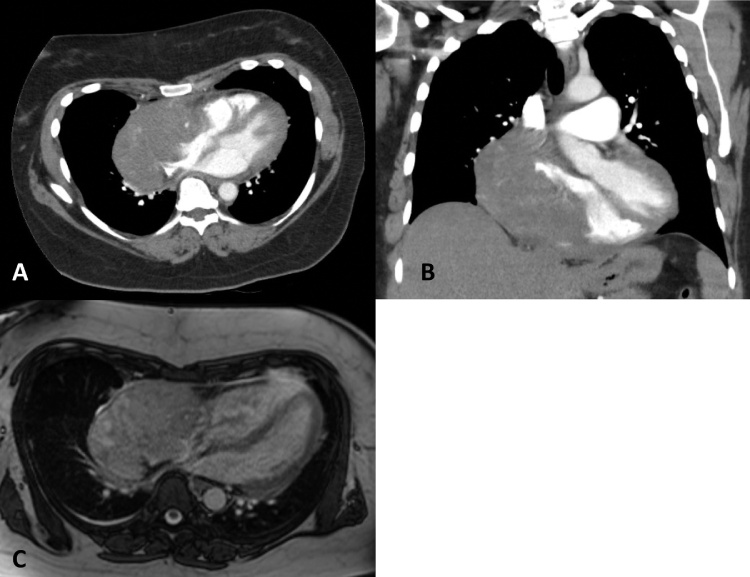
Fig. 1.
Computed tomography (A and B) and magnetic resonance imaging (C) at the time of second presentation showing right atrial mass.
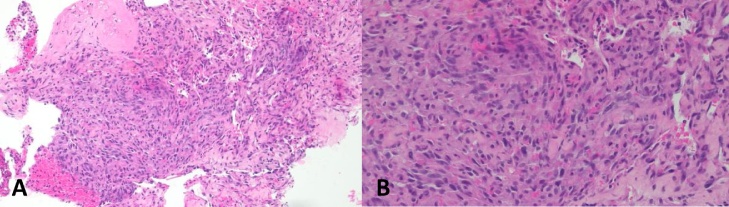
Fig. 2.
(A and B) Biopsy result showing histopathological appearance of cardiac angiosarcoma tumor.
Treatment
Given the location of the tumor, and its close proximity to the heart and large blood vessels, it was thought that upfront surgery would carry significant technical difficulties and risk. Therefore, upfront chemotherapy and radiotherapy was used as a way to shrink the tumor, and thus possibly make it more amenable to surgical resection. She was commenced on concurrent chemoradiotherapy, and received 60 Gy in 30 fractions, with weekly paclitaxel 80 mg/m2. She completed a total of 18 cycles of weekly paclitaxel. This was complicated by severe esophagitis requiring a period of nasoenteric feeding. She also had a brief hospital admission one week after completing radiotherapy, presenting with fevers, cough, and dyspnea. Chest X-ray showed a new patchy air space opacity in the right mid-to-lower zones consistent with radiation pneumonitis. There was clinical improvement with dexamethasone and radiographic improvement on repeat CT chest five weeks later.
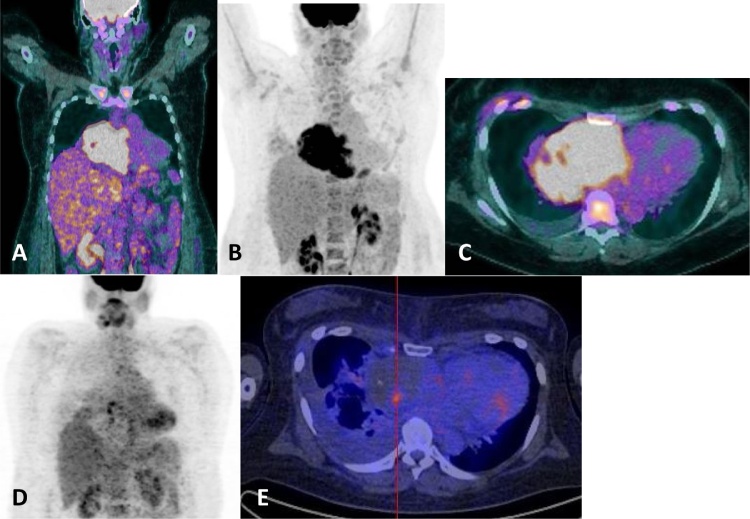
Repeat cardiac MRI following chemoradiotherapy showed a reduction in the size of the primary cardiac angiosarcoma. Repeat PET scan showed a significant improvement in the tumor mass, with only small foci of residual fluorodeoxyglucose activity and otherwise a complete metabolic response (Fig. 3).
Fig. 3.
Fluorodeoxyglucose positron emission tomography (PET) scan prior to chemoradiotherapy (A, B, and C), and follow-up PET scan following chemoradiotherapy (D and E).
The patient was evaluated by a multidisciplinary team at Cleveland Clinic, including oncology, cardiology, and cardiothoracic surgery. After much deliberation, she was deemed suitable for surgery, and she underwent resection of the tumor. Intra-operatively, it was noted that the tumor appeared avascular and necrotic. The tumor mass filled the entire right atrium with the free wall of the atrium being the base and was close to the lateral aspect of the tricuspid annulus and surrounding the right coronary artery in that same area. The mass was removed with a small margin of normal atrial wall but only peeled off the tricuspid annulus, right coronary artery, and right ventricle. The defect was closed with a generous bovine pericardial patch. Post-operatively, she developed a recurrent right pleural effusion requiring insertion of a chest drain, but otherwise recovered well.
Outcome and follow up
Surgical pathology from her resection confirmed a complete pathological response, with fully necrotic tumor present surrounded by normal myocardium and fibrous tissue.
At latest follow up five months post-surgery and eight months post-chemoradiotherapy, the patient remains asymptomatic, and has no ongoing toxicities from treatment, apart from mild dysphagia.
Discussion
Primary tumors of the heart are extremely rare, and the majority are benign. Cardiac angiosarcoma is the most common primary malignant tumor of the heart [1], [5]. It is a rare subgroup of soft tissue sarcomas, and is associated with a poor prognosis due to its aggressive nature and high rates of local recurrence and systemic metastases [2]. The rapid infiltrating growth of this tumor can lead to emergency clinical presentations including pericardial effusions, cardiac tamponade, and myocardial rupture [6]. This case demonstrates how the nonspecific symptoms of cardiac angiosarcoma can contribute to a delayed diagnosis.
Over time, improvements have been made in the ability to visualize and diagnose these tumors. Echocardiogram is still highly useful in detection, in conjunction with the use of cardiac MRI to better define the exact location, size, and local extension of the tumor [7]. CT and PET scans have a role for detecting distant metastatic disease.
Because cardiac angiosarcoma is an uncommon disease, there is currently no standard treatment approach. Most published studies are retrospective case series and case reports, with heterogeneous populations that include patients with angiosarcomas from other primary sites and other subtypes of cardiac tumors. Several studies have shown that when localized, surgical resection leads to the best chance of long-term survival [5], [7], [8]. However, surgery is often technically challenging, particularly since these tumors occur within the heart or in close proximity to the great vessels. Furthermore, the rapidly progressive nature of this disease can mean surgery is not an option for some patients.
Given the aggressive nature of these tumors, combined modality therapies have emerged as a potential way to achieve better survival outcomes. There are several case reports and case series of patients treated with adjuvant radiotherapy, as well as neoadjuvant or adjuvant chemotherapy (see Online Tables 1 and 2). Upfront chemotherapy can shrink the tumor mass, allowing for radical surgery [9]. Various chemotherapeutic agents have been used, including paclitaxel, doxorubicin, ifosfamide, docetaxel, gemcitabine, cyclophosphamide, vincristine, and dacarbazine. There are also case reports showing that angiosarcomas of various sites may respond to pazopanib, imatinib, recombinant interleukin-2, and bevacizumab (see Online Tables 1 and 2). Studies in unresectable and metastatic angiosarcoma have shown paclitaxel to be a well-tolerated and effective agent, with objective responses seen in over half the patients [3], [4]. In the only phase II study of angiosarcoma, the ANGIOTAX study, paclitaxel treatment was associated with a median overall survival of 8 months in patients with unresectable angiosarcoma, and 10% of patients had a partial response that enabled a curative-intent surgery [4].
Although there are several reports of responses to paclitaxel, to our knowledge this is the first case of a complete metabolic and pathologic response to upfront chemoradiotherapy with paclitaxel, followed by surgery. In this case, a complete metabolic response was noted on the repeat PET scan after chemoradiotherapy, and no viable tumor was found at the time of surgery (complete pathological response). The decision to offer surgery was based on the patient's response to upfront chemoradiotherapy, the tumor being in essence avascular, her symptoms of right ventricular inflow obstruction, and the fact that resection did not require removal of too much of the right ventricle. At surgery, the tumor was circumscribed and seemed completely necrotic. The patient has recovered well, with no evidence of tumor recurrence, now five months after surgery.
Upfront chemoradiotherapy with weekly paclitaxel, followed by surgical resection may be an effective treatment for patients with cardiac angiosarcoma, and can result in significant pathological responses. Validation in prospective studies is required.
Funding
No financial support to disclose.
Conflict of interest
The authors declare that there are no conflicts of interest.
Acknowledgments
Laura Sullivan, International Nurse Coordinator, Cleveland Clinic.
Footnotes
Supplementary material related to this article can be found, in the online version, at https://doi.org/10.1016/j.jccase.2020.04.010.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Patel S.D., Peterson A., Bartczak A., Lee S., Chojnowski S., Gajewski P. Primary cardiac angiosarcoma – a review. Med Sci Monit. 2014;20:103–109. doi: 10.12659/MSM.889875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antonuzzo L., Rotella V., Mazzoni F., Doni L., Bianchini D., Garbini F. Primary cardiac angiosarcoma: a fatal disease. Case Rep Med. 2009;2009:591512. doi: 10.1155/2009/591512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Byeon S., Song H.N., Kim H.K., Ham J.S., Lee S.J., Lee J. A Korean single-center, real-world, retrospective study of first-line weekly paclitaxel in patients with metastatic angiosarcoma. Clin Sarcoma Res. 2016;6:8. doi: 10.1186/s13569-016-0048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Penel N., Bui B.N., Bay J.O., Cupissol D., Ray-Coquard I., Piperno-Neumann S. Phase II trial of weekly paclitaxel for unresectable angiosarcoma: the ANGIOTAX Study. J Clin Oncol. 2008;26:5269–5274. doi: 10.1200/JCO.2008.17.3146. [DOI] [PubMed] [Google Scholar]
- 5.Randhawa J.S., Budd G.T., Randhawa M., Ahluwalia M., Jia X., Daw H. Primary cardiac sarcoma: 25-year Cleveland Clinic experience. Am J Clin Oncol. 2016;39:593–599. doi: 10.1097/COC.0000000000000106. [DOI] [PubMed] [Google Scholar]
- 6.Chaves V.M., Pereira C., Andrade M., von Hafe P., Almeida J.S. Cardiac angiosarcoma: from cardiac tamponade to ischaemic stroke – a diagnostic challenge. Eur J Case Rep Intern Med. 2019;6:001079. doi: 10.12890/2019_001079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simpson L., Kumar S.K., Okuno S.H., Schaff H.V., Porrata L.F., Buckner J.C. Malignant primary cardiac tumors: review of a single institution experience. Cancer. 2008;112:2440–2446. doi: 10.1002/cncr.23459. [DOI] [PubMed] [Google Scholar]
- 8.Blackmon S.H., Reardon M.J. Surgical treatment of primary cardiac sarcomas. Tex Heart Inst J. 2009;36:451–452. [PMC free article] [PubMed] [Google Scholar]
- 9.Abu Saleh W.K., Ramlawi B., Shapira O.M., Al Jabbari O., Ravi V., Benjamin R. Improved outcomes with the evolution of a neoadjuvant chemotherapy approach to right heart sarcoma. Ann Thorac Surg. 2017;104:90–96. doi: 10.1016/j.athoracsur.2016.10.054. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.