Abstract
Background
More than 2 months have passed since the novel coronavirus disease 2019 (COVID-19) first emerged in Wuhan, China. With the migration of people, the epidemic has rapidly spread within China and throughout the world. Due to the severity of the epidemic, undiscovered transmission of COVID-19 deserves further investigation. The aim of our study hypothesized possible modes of SARS-CoV-2 transmission and how the virus may have spread between two family clusters within a residential building in Guangzhou, China.
Methods
In a cross-sectional study, we monitored and traced confirmed patients and their close contacts from January 11 to February 5, 2020 in Guangzhou, China, including 2 family cluster cases and 61 residents within one residential building. The environmental samples of the building and the throat swabs from the patients and from their related individuals were collected for SARS-CoV-2 and tested with real-time reverse transcriptase polymerase chain reaction (RT-PCR). The relevant information was collected and reported using big data tools.
Results
There were two notable family cluster cases in Guangzhou, which included 3 confirmed patients (family No.1: patient A, B, C) and 2 confirmed patients (family No.2: patient D, E), respectively. None of patients had contact with other confirmed patients before the onset of symptoms, and only patient A and patient B made a short stop in Wuhan by train. Home environment inspection results showed that the door handle of family No.1 was positive of SARS-CoV-2. The close contacts of the 5 patients all tested negative of SARS-CoV-2 and in good health, and therefore were released after the official medical observation period of 14-days. Finally, according to the traceability investigation through applying big data analysis, we found an epidemiological association between family No.1 and family No.2, in which patient D (family No.2) was infected through touching an elevator button contaminated by snot with virus from patient A (family No.1) on the same day.
Conclusions
Contaminants with virus from confirmed patients can pollute the environment of public places, and the virus can survive on the surface of objects for a short period of time. Therefore, in addition to the conventional droplet transmission, there is also indirect contact transmission such as snot-oral transmission that plays a crucial role in community spread of the virus.
Keywords: Novel coronavirus disease, Severe acute respiratory syndrome coronavirus 2, Snot-oral transmission, Indirect transmission
Background
In late December 2019, an outbreak of the novel coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was reported by the local health facilities in Wuhan, China [1, 2]. The epidemic has been spreading to many other Chinese cities [3–5]. As the spread escalated, the World Health Organization (WHO) declared that the SARS-CoV-2 outbreak constitutes a “Public Health Emergency of International Concern” on January 30, 2020, and the epidemic has escalated to a pandemic since March 11, 2020.
With the information from epidemiological investigation and clinical manifestation accumulating, evidence indicated that there existed person-to-person transmission of COVID-19 [6, 7]. In order to elucidate the reason for the rapid spread of the disease, the researchers examined whether the virus could survive in external environment and found detectable nucleic acid of SARS-CoV-2 in environmental sample gathered from South China Seafood Market in Wuhan, the place where the virus first broke out. Other studies also showed that the virus was also found in patients’ feces and urine [8]. The pre-existing evidence suggests that contaminants from patients can pollute the environment of public places and indirectly indicates the possibility of contact transmission. Due to the fact that the Chinese government had invested a lot of resources and adopted various measures to manage the impact of the outbreak, the number of confirmed COVID-19 cases and suspected cases has begun to decline slowly since 15 February 2020, and there has been no new cases for days in several provinces and cities [9]. But the epidemic has not completely come to an end and we still need to remain vigilant continuously especially because of the migration of large populations and the gradual reopening of public places. New reports have shown that the virus continues to spread, yet we still have very few understandings of the characteristics of the virus, and therefore need further investigation. As reported in this study, there were two interesting family cluster cases reported in Guangzhou, providing the evidence of snot-oral indirect transmission of SARS-CoV-2.
Methods
A cross-sectional study was conducted to investigate the possible modes of SARS-CoV-2 transmission between 2 family clusters within the same residential building in Guangzhou, China. Between January 11, 2020 and February 5, 2020, two family cluster cases included 5 confirmed patients reported in one residential building. We investigated cases, close contacts, the residents,security guards and janitors of this building. On January 30, we sampled aerosol and surface samples from the elevator and the houses of the two families. On February 1, we sampled blood samples and throat swabs from the residents of this building, and throat swabs collected from the security guards and janitors. On February 3, 2020, the second batch of surface samples from the elevator and the houses of the two families were collected. The environmental samples of the building and the throat swabs from the patients and their related individuals were tested with real-time reverse transcriptase polymerase chain reaction (RT-PCR) for SARS-CoV-2. The relevant information was collected and analyzed using big data tools.
Data collection
All information of traceability investigation was collected using big data tools and reported by Guangzhou Center for Disease Control and Prevention (Guangzhou CDC), and the field epidemiological investigations were conducted by the staff of Guangzhou municipal and Baiyun district centers for disease control and prevention based on the “questionnaire on individual case of COVID-19 cases” and the “questionnaire on Individual case of suspected COVID-19 cases”. The pharyngeal swabs, blood samples, aerosol samples and surface samples were collected by medical staff in hospitals or during the field investigation, and safely sent to Guangzhou Centre for Disease Control and Prevention. The real-time reverse-transcriptase–polymerase-chain-reaction (RT-PCR) assay was performed to confirm the infection caused by the SARS-Cov-2 virus. The informed consent was obtained from each participant and this epidemiological study was approved by the Ethical Committee of Guangzhou Centre for Disease Control and Prevention.
Study definitions
Big data tools
The “big data tools” is a database containing information about monitored and traced cases and close contacts accumulated and managed by Guangzhou CDC, from which we get the information of 2 family cluster cases and 61 residents of same residential building from January 11 to February 5, 2020 in Guangzhou, China.
Sample collection
3 aerosol samples and 21 surface samples were collected from the elevator and the houses of the two families. In addition to collecting throat swabs from 5 confirmed patients, there were 61 blood samples and 61 throat swabs collected from the residents of this building, and 14 throat swabs collected from security guards and janitors, as shown in Table 2.
Table 2.
The outcome of environmental samples tested
| Sample number | Sampling area | Sample type | Outcomes |
|---|---|---|---|
| The first sampling of environmental samples on the 30 January, 2020. | |||
| 1 | Up and down Button of 01 floor outside of elevator | Object surface swab | Negative |
| 2 | Button of close and open inside of elevator | Object surface swab | Negative |
| 3 | Button of 01-B1 floor inside of elevator | Object surface swab | Negative |
| 4 | Button of 02–11 floor inside of elevator | Object surface swab | Negative |
| 5 | The ground of elevator | Object surface swab | Negative |
| 6 | The wall of elevator | Object surface swab | Negative |
| 7 | Both sides of elevator door | Object surface swab | Negative |
| 8 | The door of elevator | Object surface swab | Negative |
| 9 | Button of 10 floor | Object surface swab | Negative |
| 10 | The door handle of No.1 family | Object surface swab | Positive* |
| 11 | Button of 11 floor | Object surface swab | Negative |
| 12 | The door handle of No.2 family | Object surface swab | Negative |
| 13 | The door handle of the big door of building | Object surface swab | Negative |
| 14 | Button of 02 floor outside of elevator | Object surface swab | Negative |
| 15 | Button of 03 floor outside of elevator | Object surface swab | Negative |
| 16 | Button of 04 floor outside of elevator | Object surface swab | Negative |
| 17 | Button of 05 floor outside of elevator | Object surface swab | Negative |
| 18 | Button of 06 floor outside of elevator | Object surface swab | Negative |
| 19 | Button of 07 floor outside of elevator | Object surface swab | Negative |
| 20 | Button of 08 floor outside of elevator | Object surface swab | Negative |
| 21 | Button of 09 floor outside of elevator | Object surface swab | Negative |
| 22 | Inside the elevator | aerosol | Negative |
| 23 | The house of No.1 family | aerosol | Negative |
| 24 | The house of No.2 family | aerosol | Negative |
| The second sampling of environmental samples on the 3 February, 2020. | |||
| 1 | Button inside of elevator | Object surface swab | Negative |
| 2 | Button of 08 floor outside of elevator | Object surface swab | Negative |
| 3 | First floor stair railing | Object surface swab | Negative |
| 4 | The door handle of No.2 family | Object surface swab | Negative |
| 5 | Third floor stair railing | Object surface swab | Negative |
| 6 | First floor stair railing outside of big door of building | Object surface swab | Negative |
| 7 | The door handle of 702 household | Object surface swab | Negative |
| 8 | The door handle of 1102 household | Object surface swab | Negative |
| 9 | The door handle of No.1 family | Object surface swab | Negative |
| 10 | Button of 02 floor outside of elevator | Object surface swab | Negative |
Viral nucleic acid test
Laboratory confirmation of the SARS-CoV-2 by RT-PCR assay (Shanghai BioGerm Medical Biotechnology) was conducted in Guangzhou Center for Disease Prevention and Control (Guangzhou CDC). The RT-PCR assay was performed in accordance with the protocol established by the World Health Organization. SARS-CoV-2 nucleic acid testing was performed using RT-PCR assay according to the National Health Commission guidelines for laboratory testing of pneumonia with novel coronavirus infection [10, 11].
The COVID-19 patient
The case is determined by a positive result by real-time reverse-transcriptase–polymerase-chain-reaction (RT-PCR) assay of the SARS-Cov-2 virus in patient’s pharyngeal and anal swab specimens. Only the laboratory-confirmed patients were included in the final analysis.
Asymptomatic patient
An asymptomatic case is defined as someone who shows no clinical symptoms within 14 days before the diagnosis, tests positive for SARS-CoV-2 on RT-PCR or serum-specific IgM antibodies, and is identified through close contact screening, cluster epidemic investigation and traceback investigation.
The exposure
The exposure is defined as the following situations within 14 days before the onset of illness applicable to individuals: 1) traveling to or living in Wuhan or other regions with severe epidemics abroad; 2) having contact with SARS-CoV-2 infected individuals whose nucleic acid test was positive or with patients who had fever or respiratory symptoms coming from Wuhan or other regions abroad that have been severely affected by the epidemic; 3) having been to 2 or more cases occurred fever or respiratory symptoms in a small area (such as home, office, school class, workshop, construction site, etc.).
Cluster outbreak
The cluster outbreak is defined as 2 or more presumptive confirmed cases reported with fever or respiratory symptoms within 14 days after having been in the same confined space (such as home, office, school class, workshop, construction site, etc.), which provides the possibility of interpersonal transmission and being infected due to co-exposure.
Close contact
Close contact refers to an individual who has not taken effective protection when in proximity of suspected or confirmed cases 2 days before the onset of symptoms or 2 days before the collection of asymptomatic specimens.
Statistical analysis
We setup the EXCEL databases to include all questionnaires, clinic and laboratory data of two family COVID-19 patients. The continuous variables were shown as medians and interquartile ranges (Q1-Q4), Median (IQR), or medians and ranges, Median (min-max). The categorical variables were summarized as counts and percentages, no. (%). All the figures were drawn using Graphad Prism 8 software, and all the analyses were performed using SPSS software (Statistical Package for the Social Sciences, version 26.0).
Results
Characteristics of two family cluster cases
In the cross-sectional study of COVID-19 in Guangzhou, we found that there were two notable family cluster cases, which included 3 (family No.1: patient A, B and C) and 2 (family No.2: patient D and E) cases of COVID-19 patients, respectively. As listed in Table 1, patient A was male and 70 years old; patient B and C were female and were 68 and 38 years old. Patient D was a 64 year old female, and patient E was male and 66 years of age. All patients had fever at onset, except for patient E, who was symptomless.
Table 1.
The basic information of 5 patients with COVID-19
| Patients | Occupation | Symptoms | Temperature | Blood leukocyte count (*109/L) |
Lymphocyte count(*109/L) |
Lymphocyte percentage(%) |
Neutrophil percentage(%) |
CT | Onset date | Admission date | Out date |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient A | Retiree | Fever, running nose | 38 °C | 4.25 | 0.74 | 17.4 | 75.1 | B + | Jan13 2020 | Jan24 2020 | Feb13 2020 |
| Patient B | Retiree | Fever, dry cough | 37.5 °C | 6.05 | 2.1 | 34.7 | 56.8 | B - | Jan23 2020 | Jan24 2020 | Feb23 2020 |
| Patient C | Civil servants | Fever | 38.5 °C | 5.66 | 1.47 | 26.04 | 65.4 | B + | Jan19 2020 | Jan24 2020 | Feb8 2020 |
| Patient D | Retiree | Fever | 37.8 °C | 5.42 | 1.21 | 22.34 | 66.44 | B + | Jan21 2020 | Jan27 2020 | Feb21 2020 |
| Patient E | Retiree | – | Normal | Normal | Normal | Normal | Normal | R up + | asymptomatic | Jan27 2020 | Feb21 2020 |
Note: Age (range, 38–70 years); CT Computerized tomography, B Bilateral lung, R up the upper lobe of the right lung
Information of family No.1
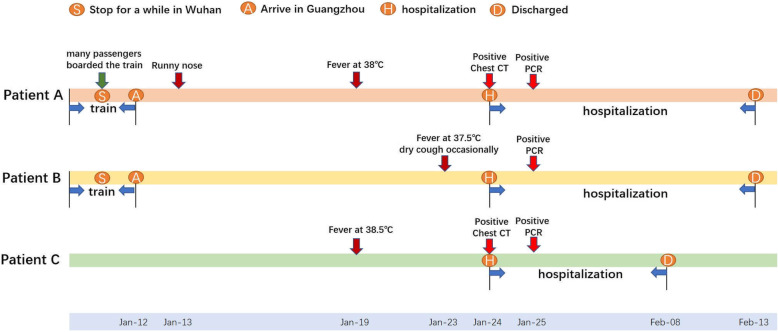
Patient A, 70 years old, developed a fever at 38 °C accompanied with runny nose on January 19th, 2020, as shown in Fig. 1. Patient B, patient A’s wife, developed a fever at 37.5 °C with an occasional dry cough on January 23th. Patient C, their daughter, developed a fever at 38.5 °C without other symptoms on January 19th. On January 24th, the three patients visited Jinshazhou Hospital of Guangzhou Chinese Medicine University for treatment. The chest CT of patient A showed bilateral lung inflammation and emphysema and blood test showed decreased lymphocyte count. The chest CT result of patient C also showed bilateral lung inflammation, while that of patient B was normal. On the night of the same day, they were admitted to the isolation ward of hospital as suspected cases of COVID-19. At 9:00 a.m. on January 25, their throat swabs were collected by Guangzhou CDC and tested for SARS-CoV-2 virus nucleic acid test, all of which were reported to be positive on the same day, so they were immediately transported by ambulance to the designated COVID-19 hospital for isolation treatment. These three patients were in mild severity. After isolation and treatment in the designated hospital, they were cured and discharged. A total of 18 individuals were identified as close contacts of this family by Guangzhou CDC and so far, all of them were healthy without any symptoms and thus are all relieved of medical observation.
Fig. 1.
The diagram of epidemiological survey in family No.1
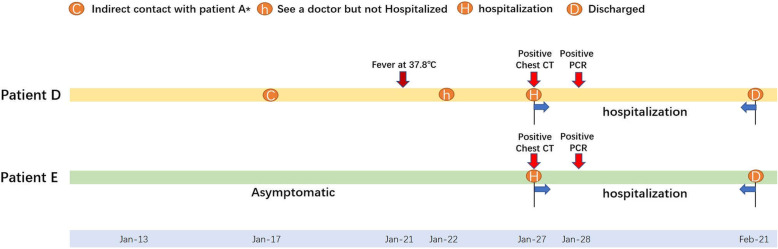
Information of family No.2
As described in Fig. 2, Patient D, a 64-year-old woman, experienced the onset of fever at 37.8 °C without other symptoms on January 21th, and went to Jinsha Street Community Health Service Center for treatment on January 22th. Patient E, patient D’s husband, without any respiratory symptoms, he went to Jinshazhou Hospital of Guangzhou Chinese Medicine University with his wife on January 27th. The chest CT test of patient D showed bilateral lung inflammation and that of patient E showed inflammation in the upper lobe of the right lung. Both patients were admitted to the isolation ward of hospital as suspected cases of COVID-19 on the same day. On January 28th, the outcomes of virus nucleic acid test were both positive of SARS-CoV-2 so that they were transported by ambulance to the designated hospital of COVID-19 for isolation treatment on January 29th. They were both mild patients in stable condition. After isolation and treatment in the designated hospital, they were cured and discharged. Three other individuals were identified as close contacts of this family by Guangzhou CDC and so far, all were in good health without any symptoms so that they were all relieved of medical observation.
Fig. 2.
The diagram of epidemiological survey in family No.2
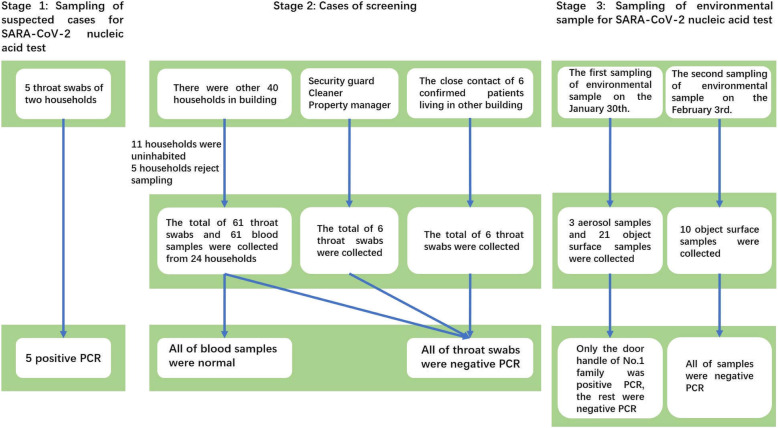
The results of viral nucleic acid test
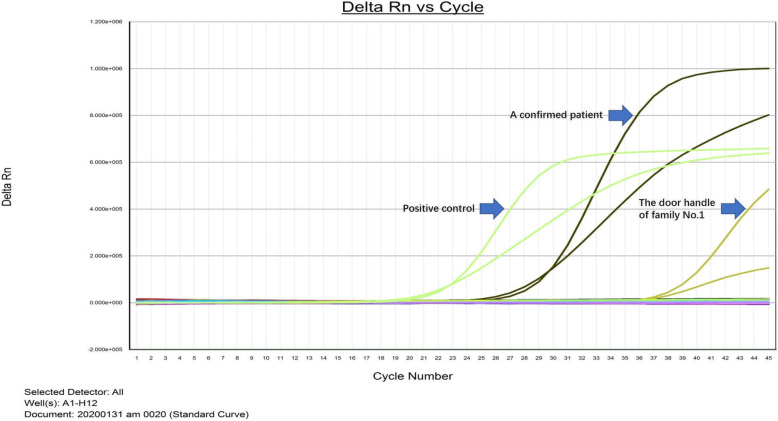
As presented in Figs. 3, 5 patients from the above two families were positive of SARS-CoV-2, while the test results of throat swabs and blood samples collected from relevant individuals were all negative, as listed in Table S 1 and S 2. Of all environmental samples, only the door handle of family No.1 tested positive of SARS-CoV-2(shown in Fig. 4), and the rest were negative that listed in Table 2.
Fig. 3.
The graphical of detecting steps of SARS-CoV-2 among the patients and their close contacts, and their surroundings
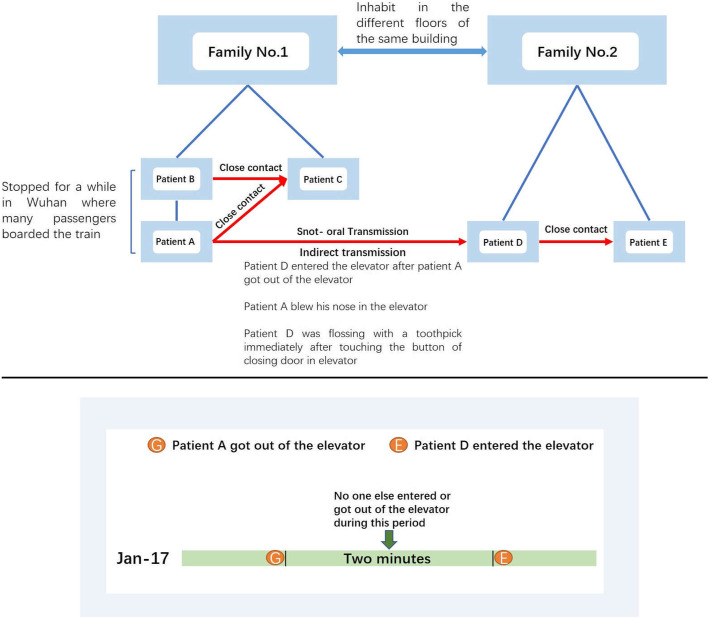
Fig. 5.
The epidemiological investigation and their relationship between family No.1 and family No.2
Fig. 4.
The result of SARS-CoV-2 viral nucleic acid test for the door handle
Epidemiological investigation
All three members of family No.1 said that they had no contact with COVID-19 patients nor individuals from Hubei province. However, patient A and patient B had traveled to Guangzhou by train from other province to visit their children (patient C). The train stopped in Wuhan for several minutes. That stop was a crowded and compact hub where many passengers boarded the train. Therefore, as shown in Fig. 5, it was inferred that patient A and patient B were infected through close contact to passengers who might be unknown patients of COVID-19. Later they passed on the COVID-19 to their daughter (patient C) as close family contact. Both members of family No.2 said that they had no contact with the patients in family No.1 or individuals from Hubei province, and had no link to Wuhan city.
Epidemiological relationship between family No.1 and family No.2
According to the traceability investigation through applying the big data tools, we found that patient A had a bad habit in personal hygiene that he often blew nose using his own hand, which was what he again did before touching the button of closing door in elevator. As shown in Fig. 5, on January 17th, patient A blew nose using his own hand before touching the button of closing door in elevator, then 2 min after patient A got out of the elevator, patient D entered the same elevator and touched the same button. The most important thing is that patient D immediately flossed with a toothpick after touching the elevator button. Therefore, it was speculated that patient D (family No.2) was infected for COVID-19 by means of snot-oral indirect transmission of touching the button of elevator contaminated by snot with virus from patient A (family No.1).
Discussion
Although the epidemic of COVID-19 has been going on for months, the epidemiological characteristics of the SARS-CoV-2 virus are not yet fully understood. With the import of COVID-19 cases, there were many new local patients in the cities outside of Hubei province [5, 12]. Some cities have a high proportion of clustering cases, such as Beijing, where, as of February 11, a total of 77 clustered cases involving 251 patients accounted for 71% of a total of 352 patients [13]. A point worth noting about this epidemic is that some local cases have no clear source of infection in the cities outside of Hubei province.
Recently, there were several reports that the new coronavirus could spread via droplets, contact and natural aerosols from human-to-human [1, 4, 14, 15], causing a high possibility of a pandemic. As more and more new cases with COVID-19 are reported worldwide [16, 17], it seems to be a gloomy reality. To contain the spread of the COVID-19 epidemic without delay, a deeper understanding of the SARS-CoV-2 virus should be presented [18]. To reduce the impact and spread of the disease, it is essential to limit human-to-human transmission to reduce secondary infections among close contacts and health care workers.
As reported in this study, we found two family clusters infected with SARS-CoV-2 in the same building in Guangzhou, China. Through testing the external environment samples, we found that the sample taken from door handle of family No.1 tested positive of SARS-CoV-2, which indicated that contaminants with virus from confirmed patients can pollute the environment of public places. Furthermore, the patient D of family No.2 was infected via the snot-oral indirect transmission, indicating that SARS-CoV-2 virus can survive in the environment for at least a short period of time. As previously reported by Zou LR et al., higher viral loads were detected soon after symptom onset, with higher viral loads detected in the nose than in the throat [19, 20], which further demonstrated that indirect contact transmission by means of snot-oral Transmission might be an effective way to spread the epidemic disease. For the surface survival of virus, SARS-CoV-2 can remain viable and infectious on surfaces up to days, so common surface transmission of the virus is highly possible [21]. Although the elevator buttons were detected as negative for viral nucleic acid, the possible reason is that the buttons have been used many times and the time interval from contamination to sampling is too long. During this period, the interior of the elevator has been disinfected several times. With the return to work and the gradual opening of public places, the migration of large population is a huge challenge for prevention and control of the epidemic. Therefore, it is also still important for the prevention and control of the epidemic to pay attention to personal hygiene, taking measures such as wearing a facemask, washing hands frequently and not touching nose and mouth before washing hands and so on, as well as disinfection of public places in the coming time period.
Our study had some obvious limitations. First, on January 17, no samples were collected on the day of the elevator button pollution and our elevator button sampling took place on January 30. Second, according to the weak positive test of patient A’s home handle and his poor hygiene habits, it is our inference that the infection of patient D was caused by the transmission of the elevator button polluted by patient A’s nose. Third, we cannot exclude the possibility of transmission of the virus by unknown infected persons, such as asymptomatic carriers [22].
Conclusions
In summary, this study provides direct evidence substantiating that SARS-CoV-2 can infect other individuals by means of snot-oral transmission as one mode of indirect contact transmission. This finding is of significance for the prevention and control of COVID-19 and the formulation of the public health policies and measures. Based on previous reports and the evidence provided in this study, it is important to pay attention to personal hygiene and disinfection in public places.
Supplementary information
Additional file 1: Table S1. The outcome of whole blood samples tested. Table S2. The outcome of throat swabs tested.
Acknowledgements
We thank Boqi Rao, Yingyi Feng, Yujie Pan, Zhi Li, Chun Mao, Wenhui Lun, Zeqin Huang, and Junyi Ye from Guangzhou Medical University (Guangzhou, China) for assisting with data collection. We thank Boqi Rao for his assistance in preparing the figures. We thank Fuman Qiu from Guangzhou Medical University (Guangzhou, China) for his assistance in writing the manuscript. We are very grateful to all staff at Guangzhou Center for Disease Control and Prevention for providing the data and all medical staff members and field workers who are working on the frontline of caring for patients and collecting the data.
Abbreviations
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2; COVID-19: Corona virus disease 2019
- RT-PCR
Real-time reverse transcriptase polymerase chain reaction
- IQR
Interquartile ranges
- CT
Computerized tomography
- B
Bilateral lung
- Rup
Upper lobe of the right lung
Authors’ contributions
HZ, LZ and JL designed the study. CX, KL, ZZ, HP, DW, JC and XZ collated the data. HZ analyzed epidemiologic data. HZ, CX, YG and JY contributed to interpreting the results. HZ wrote the manuscript. XL, JL and LZ revised the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported by the National Natural Science Foundation of China.
81872694, 81673267 and 81473040 (J. Lu); Local Innovative and Research Teams Project of Guangdong Pearl River Talents Program 2017BT01S155 (J Lu); Health Industry Scientific Research Project of Gansu Province GSWSKY2018–18(H Zhao). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was approved by the Ethical Committee of Guangzhou Center for Disease Control and Prevention (No. GZCDC20200311). Because of the urgent need to collect data on this emerging infectious disease, the requirement for written informed consent was waived. The oral informed consent was obtained from each participant and this form of consent was confirmed by the Ethical Committee.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Chaojun Xie, Hongjun Zhao, Kuibiao Li and Zhoubin Zhang contributed equally to this work.
Contributor Information
Lin Zhang, Email: 378563318@qq.com.
Jiachun Lu, Email: jclu@gzhmu.edu.cn.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12889-020-09296-y.
References
- 1.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Du Z, Wang L, Cauchemez S, Xu X, Wang X, Cowling BJ, Meyers LA. Risk for transportation of coronavirus disease from Wuhan to other cities in China. Emerg Infect Dis. 2020;26(5):1049–1052. doi: 10.3201/eid2605.200146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deng SQ, Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med. 2020;9(2):575. doi: 10.3390/jcm9020575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tong ZD, Tang A, Li KF, Li P, Wang HL, Yi JP, Zhang YL, Yan JB. Potential Presymptomatic transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerg Infect Dis. 2020;26(5):1052–1054. doi: 10.3201/eid2605.200198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Phan LT, Nguyen TV, Luong QC, Nguyen TV, Nguyen HT, Le HQ, et al. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med. 2020;382(9):872–874. doi: 10.1056/NEJMc2001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan JF, Yuan S, Kok KH, To KK. Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CCTV news, http://news.cctv.com/. [cited 2020 Feb 22].
- 9.National Health Commission of the People's Republic of China. http://wwwnhcgovcn. [cited 2020 Feb 23]. [DOI] [PMC free article] [PubMed]
- 10.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: interim guidance. https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf. opens in new tab. [cited 2020 Jan 28].
- 12.Wu J, Liu J, Zhao X, Liu C, Wang W, Wang D, et al. Clinical Characteristics of Imported Cases of COVID-19 in Jiangsu Province: A Multicenter Descriptive Study. Clin Infect Dis. 2020:ciaa199. 10.1093/cid/ciaa199. [DOI] [PMC free article] [PubMed]
- 13.Beijing city health commission, http://wjw.beijing.gov.cn/. [cited 2020 Feb 11].
- 14.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang D, Lin M, Wei L, Xie L, Zhu G, Dela Cruz CS, Sharma L. Epidemiologic and clinical characteristics of novel coronavirus infections involving 13 patients outside Wuhan, China. JAMA. 2020;323(11):1092–1093. doi: 10.1001/jama.2020.1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim JY, Ko JH, Kim Y, Kim YJ, Kim JM, Chung YS, et al. Viral load kinetics of SARS-CoV-2 infection in first two patients in Korea. J Korean Med Sci. 2020;35(7):e86. doi: 10.3346/jkms.2020.35.e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anzai A, Kobayashi T, Linton NM, Kinoshita R, Hayashi K, Suzuki A, et al. Assessing the impact of reduced travel on exportation dynamics of novel coronavirus infection (COVID-19) J Clin Med. 2020;9(2):601. doi: 10.3390/jcm9020601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sun P, Lu X, Xu C, Sun W, Pan B. Understanding of COVID-19 based on current evidence. J Med Virol. 2020;92(6):548–551. doi: 10.1002/jmv.25722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xie C, Lu J, Wu D, Zhang L, Zhao H, Rao B, Yang Z. False negative rate of COVID-19 is eliminated by using nasal swab test. Travel Med Infect Dis. 2020;101668. 10.1016/j.tmaid.2020.101668. [DOI] [PMC free article] [PubMed]
- 21.Neeltje D, Trenton B, Dylan H. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao H, Lu X, Deng Y, Tang Y, Lu J. COVID-19: asymptomatic carrier transmission is an underestimated problem. Epidemiol Infect. 2020;148:E116. doi: 10.1017/S0950268820001235. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. The outcome of whole blood samples tested. Table S2. The outcome of throat swabs tested.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.