Abstract
Background
During a novel virus pandemic, predicting emergency department (ED) volume is crucial for arranging the limited medical resources of hospitals for balancing the daily patient- and epidemic-related tasks in EDs. The goal of the current study was to detect specific patterns of change in ED volume and severity during a pandemic which would help to arrange medical staff and utilize facilities and resources in EDs in advance in the event of a future pandemic.
Methods
This was a retrospective study of the patients who visited our ED between November 1, 2019 and April 30, 2020. We evaluated the change in ED patient volume and complexity of patients in our medical record system. Patient volume and severity during various periods were identified and compared with data from the past 3 years and the period that SARS occurred.
Results
A reduction in ED volume was evident. The reduction began during the early epidemic period and increased rapidly during the peak period of the epidemic with the reduction continuing during the late epidemic period. No significant difference existed in the percentages of triage levels 1 and 2 between the periods. The admission rate, length of stay in the ED, and average number of patients with out-of-hospital cardiac arrest increased during the epidemic periods.
Conclusion
A significant reduction in ED volume during the COVID-19 pandemic was noted and a predictable pattern was found. This specific change in pattern in the ED volume may be useful for performing adjustments in EDs in the future during a novel virus pandemic. The severity of patients visiting the ED during epidemic periods was inconclusive.
Keywords: Emergency medicine, Patient volume, COVID-19
1. Introduction
Coronavirus disease 2019 (COVID-19) first arose in Wuhan, China in December 2019 before spreading rapidly and developing into a global epidemic emergency [[1], [2], [3], [4]]. Governments and world health systems have adopted emergency measures to control the COVID-19 pandemic. Emergency departments (EDs) have been the most affected departments in hospitals. Multiple measures have been reported for managing patients suspected of having COVID-19 and preventing infection during their treatment [5,6]. Normal tasks in the ED have remained critical during pandemic management and prevention. Predicting the ED volume is vital for arranging limited medical resources in hospitals for balancing daily patient- and epidemic-related tasks in EDs. Reports from various countries have found a reduction in ED patient volume during the epidemic period, but further analysis was limited [[7], [8], [9]]. The degree of ED volume reduction and parameters including severity, disposition, and outcomes during the epidemic were less studied.
The goal of our study was to analyze the above mentioned reduction during the COVID-19 pandemic using time-series patterns and comparing the results with those of studies on previous epidemics, such as severe acute respiratory syndrome (SARS). This study established a specific pattern for ED volume change during a pandemic, which is necessary for arranging medical staff and utilizing facilities and resources appropriately, and may be useful in the future in the event of other novel virus pandemics.
2. Material and methods
2.1. Study design
This was a retrospective study conducted at a university-affiliated tertiary teaching hospital in Taiwan with a 3600-bed capacity and an estimated annual ED volume of 180,000 patient visits. The study was approved by our institutional review board (IRB no.202000628B1).
2.2. Study setting and population
Our ED is composed of a medical ED (MED), trauma ED (TED), and pediatric ED (PED). Nontraumatic adult patients presented to the MED and nontraumatic pediatric patients (age < 18 years) were presented to the PED. All trauma patients—adults and children—were sent to the TED.
The study period was from November 1, 2019–April 30, 2020 and was divided into four periods according to the COVID-19 epidemic condition in Taiwan. The first patient with COVID-19 in Taiwan was confirmed on January 11, 2020. We defined the pre-epidemic period (P1) occurring from November 1, 2019 to January 10, 2020. The early epidemic period (P2) was defined occurring from January 11, 2020–February 27, 2020 because the first cluster of COVID-19 infection in a hospital occurred on February 28, 2020. The peak epidemic (P3) was defined occurring from February 28 to April 12, 2020, which was the date of the last confirmed local case until the time this article was written. The late-epidemic period (P4) was defined as the period since April 13, 2020. Data of patients visiting our ED during the study period, over the past 3 years, and the SARS period were extracted from the medical record system of our hospital. The data of the SARS period were divided into the same four periods with the same definition (the first SARS case occurred on March 13, 2003; the first cluster of SARS infection happened on April 21, 2003; the final SARS case was diagnosed on July 7, 2003). The patient volume and characteristics, including their age, sex, triage acuity level, disposition, and length of stay (LOS) in the ED were collected and analyzed.
2.3. Outcome measures
The main outcome was daily ED visits between various periods divided according to the epidemic. Patient volume was compared with the average volume on the same date in each of the past 3 years and the volume of similar SARS periods. The demographics and characteristics were analyzed between various periods.
2.4. Statistical analysis
Data were analyzed using SPSS software (version 13.0 for Windows; SPSS, Chicago, IL). Categorical variables were presented as numbers and percentages during the descriptive analysis. The data were compared using the Mann–Whitney U test for continuous variables and Pearson's chi-square or Fisher's exact tests for categorical variables. The discrpancies between different periods were reported using an analysis of variance test. A p value <.05 was considered to be statistically significant.
3. Results
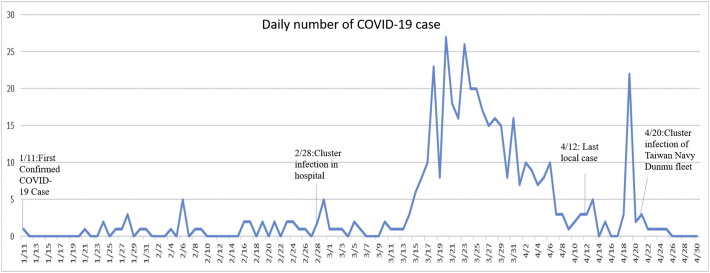
Fig. 1 presents the number of patients infected with COVID-19. The first local patient infected with COVID-19 in Taiwan was confirmed on January 11, 2020. The daily number of patients was initially low but rapidly increased after the first event of nosocomial infection. The peak of the epidemic appeared in March 2020 and decreased gradually in April 2020. The last local case of COVID-19 was diagnosed on April 12, 2020. A cluster infection with 21 cases occurred among the Taiwan Navy's Dunmu fleet between April 14 and April 18. As of the writing of this article, 429 COVID-19 cases had been confirmed, including six deaths (mortality rate 1.3%), as reported by Taiwan's Central Epidemic Command Center.
Fig. 1.
Daily number of patients diagnosed with COVID-19 in Taiwan.
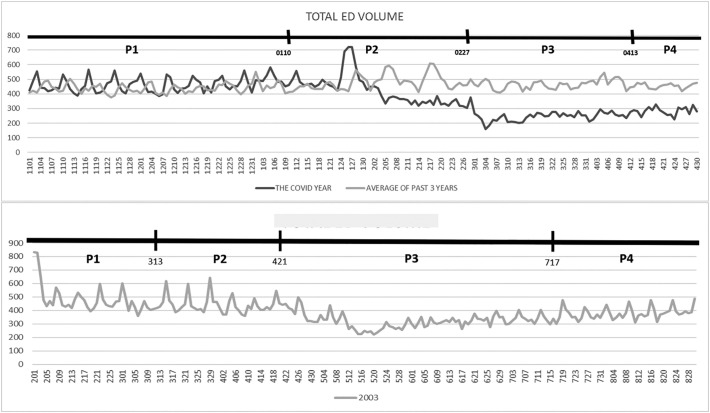
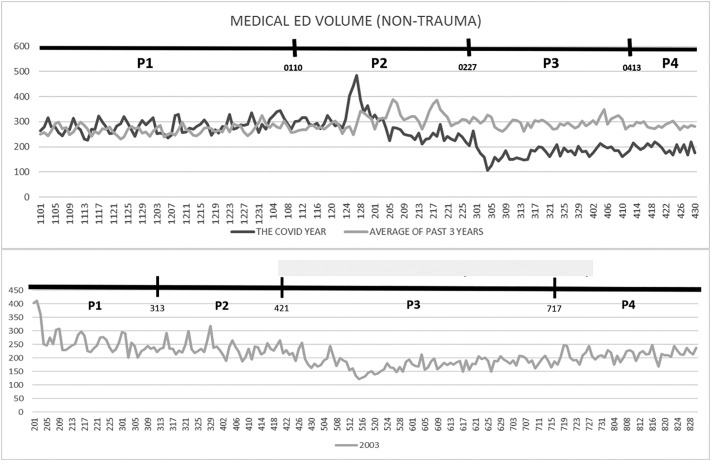
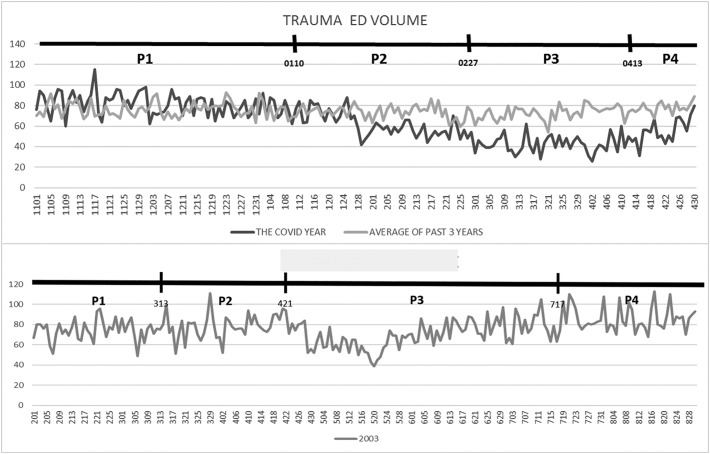
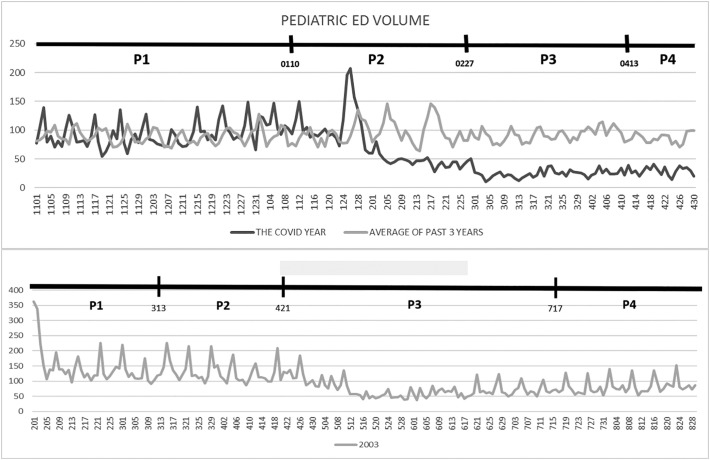
Fig. 2 shows the daily ED volume in the epidemic year and the average volumes from the past 3 years and the same defined SARS period. The total daily patient volume and proportions in the MED, TED, and PED are independently illustrated in Fig. 3 , Fig. 4 , and Fig. 5 . All patient volume proportions decreased during the early epidemic period and dropped rapidly to approximately half the volume during the peak epidemic period. The reduction persisted into the late-epidemic period. A similar pattern was noted in the periods divided according to our definition for SARS. Table 1 describes the mean values in various periods; the reduction in patient volume can be observed to have been significant. The decreases in total patients and proportions in the MED and TED began during the early epidemic period and reached half volumes during the peak epidemic period. The pediatric patient number was affected the most at less than 30% of the volume of the pre-epidemic period. A similar trend of ED volume was found during the SARS period, and the pattern was very similar according to our defined periods except for the patient volume of TED. The volume of TED in the SARS period only mildly decreased during the peak epidemic period.
Fig. 2.
Emergency department (ED) volume during the epidemic year, past 3 years, and the SARS period.
Fig. 3.
Patient volume in the medical ED during the epidemic year, the averages from the past 3 years, and the SARS period.
Fig. 4.
Patient volume in the trauma ED during the epidemic year, the averages from the past 3 years, and the SARS period.
Fig. 5.
Patient volume in the pediatric ED during the epidemic year, the averages from the past 3 years, and the SARS period.
Table 1.
Comparison of emergency department volumes between different periods
| Pre-epidemic, P1 | Early epidemic, P2 | Peak epidemic, P3 | Late epidemic, P4 | p value | |
|---|---|---|---|---|---|
| Cumulative numbers of COVID-19 patients (average number per day) | 0 (0) | 215 (4.48) | 518 (11.51) | 360 (20.0) | |
| Daily ED visits, total, mean ± SD | 463.92 ± 47.88 | 425.98 ± 102.35 | 248.67 ± 34.87 | 283.24 ± 28.56 | p < .001 |
| Average daily ED visits of past 3 years, mean ± SD | 439.6 ± 32.62 | 482.2 ± 52.82 | 465.8 ± 31.72 | 455.4 ± 17.62 | |
| Daily ED visits of SARS, mean ± SD | 489.5 ± 112.02 | 444.9 ± 65.4 | 324.9 ± 54.82 | 381.5 ± 45.22 | |
| Daily visits, medical ED, mean ± SD | 282.52 ± 27.53 | 284.75 ± 58.33 | 176.75 ± 26.29 | 196 ± 17.56 | p < .001 |
| Average daily visits of past 3 years, medical ED, mean ± SD | 268.4 ± 18.28 | 306.3 ± 33.54 | 295.4 ± 19.27 | 285.1 ± 10.39 | |
| Daily visits of SARS, medical ED, mean ± SD | 263.8 ± 47.99 | 236.15 ± 26.92 | 180.68 ± 25.2 | 212.36 ± 20.03 | |
| Daily visits, trauma ED, mean ± SD | 81.23 ± 10.86 | 61.88 ± 11.66 | 42.7 ± 8.36 | 55.67 ± 12.09 | p < .001 |
| Average daily visits of past 3 years, trauma ED, mean ± SD | 76.2 ± 7.2 | 73.9 ± 6.25 | 72.7 ± 6.62 | 78 ± 5.26 | |
| Daily visits of SARS, trauma ED, mean ± SD | 74.95 ± 10.44 | 77.97 ± 11.74 | 70.82 ± 13.73 | 85.58 ± 12.44 | |
| Daily visits, pediatric ED, mean ± SD | 94.15 ± 21.94 | 74.58 ± 41.85 | 25.18 ± 7.80 | 29.06 ± 7.26 | p < .001 |
| Average daily visits of past 3 years, pediatric ED, mean ± SD | 89.1 ± 12.39 | 96.2 ± 20.45 | 92.1 ± 11.11 | 86.8 ± 8.99 | |
| Daily visits of SARS, pediatric ED, mean ± SD | 150.76 ± 65.96 | 130.77 ± 36.4 | 73.40 ± 27.77 | 83.56 ± 26.59 |
ED: emergency department; SD: standard deviation; SARS: severe acute respiratory syndrome.
Table 2 lists the characteristics of patients in the different periods. The volume of male and elderly patients increased during the epidemic periods. No significant difference existed in the percentages of patients with triage levels 1 and 2 among the four periods. The admission rate was significantly elevated during the epidemic periods. Furthermore, the ED LOS decreased during the early epidemic period and then increased during the peak and late-epidemic periods. Moreover, the average number of patients with out-of-hospital cardiac arrest (OHCA) per day significantly increased during the early epidemic period.
Table 2.
Characteristics of patients in different periods
| P1 (pre-epidemic) | P2 (early epidemic) | P3 (peak epidemic) | P4 (late epidemic) | p value | |
|---|---|---|---|---|---|
| Gender, male, % | 52.0% | 52.6% | 53.6% | 53.6% | p = .001 |
| Gender, the past three years, male, % | 53.1% | 52.1% | 52.0% | 52.4% | |
| Age, year, mean ± SD | 41.71 ± 26.79 | 43.18 ± 25.76 | 46.28 ± 23.85 | 46.76 ± 24.23 | p < .001 |
| Age, the past 3 years, year, mean ± SD | 41.61 ± 26.94 | 42.78 ± 26.83 | 42.66 ± 26.89 | 42.55 ± 26.61 | |
| Triage level I and level II, % | 20.0% | 19.5% | 19.3% | 19.3% | p = .311 |
| Triage level I and level II, %, the past 3 years | 27.6% | 26.1% | 25.9% | 23.9% | |
| Admission rate, % | 27.6% | 27% | 30.8% | 32.6% | p < .001 |
| Admission, rate, the past 3 years, % | 28.5% | 25.5% | 27.3% | 26.9% | |
| Length of stay, mins, median(IQR) | 152.94 (83.60–442.96) | 139.57 (75.06–377.94) | 151.32 (76.08–483.20) | 167.47 (84.23–579.81) | p = .01 |
| Length of stay, the past 3 years, median(IQR) | 138.97 (73.32–404.5) | 134.59 (71.57–385.03) | 141.93 (74.53–423.27) | 138.18 (72.2–405.23) | |
| Average OHCA number per day | 0.93 ± 0.96 | 1.48 ± 1.05 | 0.96 ± 1.02 | 0.5 ± 0.86 | p = .002 |
OHCA: Out-of-hospital cardiac arrest; SD: standard deviation; IQR: Interquartile range.
4. Discussion
Epidemic prevention during the COVID-19 pandemic includes the rearrangement of the flow line and subdivision of medical staff, which are essential; furthermore, the appropriate distribution of medical staff and resources for regular and epidemic duties is crucial to avoid ED collapse [6]. Preparedness for the COVID-19 pandemic may displace the utilization of medical staff and resources for regular duties in hospitals; therefore, predicting the ED volume during a pandemic will be essential for reasonably arranging the assignments of ED staff, including physicians and nurses. Studies on the correlation of ED volume and time factors have reported high predictability under general conditions [[10], [11], [12], [13]]. The current study established a specific pattern using time series of the epidemic and demonstrated a correlation between ED volume and the epidemic. The specific pattern consists of three phases. The first phase, the early epidemic period, is defined as occurring from the first infected case to the first cluster infection in our study and exhibited the beginning of a decrease in ED volume. The second phase, the peak epidemic period, occurred from the outbreak of the first cluster infection and exhibited a rapid reduction in ED volume with a rapid decrease compared with the pre-epidemic period. The third phase, the late-epidemic period, occurred after the last local case and exhibited a persistent reduction before a gradual increase. The time and rate of patient volume return depended not only on the local but also global epidemic conditions because the media is highly developed. We divided the SARS period using the same definition and a similar pattern was found. This pattern was also noted in previous studies on both COVID-19 and SARS [7,14,15]. Novel virus pandemics may again occur in the future, and this simple, specific pattern, using the date of the first infected case and first cluster infection episode, may be used in the future as a reference for adjusting the schedules of medical staff and distributing medical resources in advance.
There was one difference in the change of patient volume between the COVID-19 and SARS periods. The patient volume of TED during the SARS period did not decrease significantly, and only a small reduction was noted during the peak epidemic period. A possible explanation is that the economics and daily activities during SARS were not affected as much as during the COVID-19 pandemic and the quarantine policy was not as strict as it currently is. The TED patient volume may be used as an indicator of economic activities, however, further study is necessary.
The severity of the ED patients was another concern and should be considered beyond the volume of such patients. The problem of overcrowding and utilization of ED resources were not only related to patient volume but also to the severity and complexity of symptoms in patients [16]. Medical behavior changes in people during a pandemic because they fear becoming infected by the novel virus, which is not well understood and represents an unnecessary burden on health systems [9,[17], [18], [19]]. Psychological stress and fear causes people to avoid going to hospitals and EDs even when critically ill. An increased proportion of critical patients in the ED during the epidemic period was expected; however, our study obtained diverse results regarding severity.
The proportions of triage levels 1 and 2, which are the most severe patients, remained the same during the epidemic period, but both the admission rate and LOS increased in our study, which is similar to a previous report on SARS [14]. Additionally, the average number of patients with OHCA per day increased significantly during the early epidemic period, which may be an indicator of delayed medical treatment. One possible explanation is that the triage level could not completely represent the severity and complexity of patient symptoms [16]. Another possible reason is that many patients with a lower triage level in our hospitals were referred by local hospitals and clinics because of specialty problems such as ophthalmology and otolaryngology, and these referred patients may not decrease as much as other patients during an epidemic and may increase the portion of a lower triage level. This may explain that the portion of triage levels 1 and 2 during the epidemic period was not significantly increased in our study. To avoid the limitations of single indicators, other indicators of patient severity, such as admission rate and average OHCA numbers were included in the study. The admission rate began to increase in the peak epidemic period and may indicate an increased severity and complexity of patients which were not presented by the portion of triage levels 1 and 2 in our study. Another important finding is the increased average number of OHCA patients in the early epidemic period which is probably an essential indicator of delayed medical treatment of patients and this phenomenon was most obvious in the early epidemic period. The public health systems may need to adopt certain measures to avoid similar issues during a future pandemic.
LOS decreased in the early epidemic period. Dropped patient volume decreased waiting times for treatment and examinations and increased ward availability, so shortened LOS was found in the early epidemic period, although it began to increase during the peak epidemic period. Some wards and ICUs were restructured to treat isolated patients of suspected COVID-19 infection. Physicians also had patient number limitations according to the infection control policy. These changes may be responsible for increased LOS in the peak and late epidemic periods.
This study had several limitations. First, this study was a single-hospital study in one country and the results may not represent the general worldwide conditions. Second, our study design was restricted to a medical center and may not reflect the conditions in regional or local hospitals. Third, some parameters were not included in the study, such as the chief complaint and diagnosis, and thus the detailed data of patients during the epidemic were not completely studied. Finally, the COVID-19 pandemic persists as of the writing of this article; therefore, the effect of a prolonged epidemic was not included in this study.
5. Conclusions
This study revealed a significant reduction in ED volume during the COVID-19 pandemic, and a predictable pattern has been found in similar novel virus epidemics. The reduction in patient volume began during the early epidemic period and increased rapidly during the peak epidemic period, persisting into the late epidemic period. This specific pattern of change in ED volume will be useful for adjusting medical staff and resources in advance of a novel virus pandemic. Some indicators showed increased severity and delayed medical treatment of patients during the epidemic, however, the results were inconsistent in our study and thus further research will be necessary.
Funding sources/Disclosures
This research received no funding.
Declaration of Competing Interest
There are no conflicts of interest to declare.
Acknowledgments
This research was supported by Chang-Gung Memorial Hospital. We are thankful to our colleagues who provided their expertise, which greatly assisted the research, although they may not agree with all the interpretations provided in this paper.
References
- 1.Wu Z., McGoogan J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. Jama. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Y.C., Chen C.S., Chan Y.J. The outbreak of COVID-19: an overview. J Chin Med Assoc. 2020;83(3):217–220. doi: 10.1097/jcma.0000000000000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cucinotta D., Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Noble J., Degesys N.F., Kwan E., Grom E., Brown C., Fahimi J., et al. Emergency department preparation for COVID-19: accelerated care units. Emerg Med J. 2020 doi: 10.1136/emermed-2020-209788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cao Y., Li Q., Chen J., Guo X., Miao C., Yang H., et al. Hospital emergency management plan during the COVID-19 epidemic. Acad Emerg Med. 2020;27(4):309–311. doi: 10.1111/acem.13951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bjørnsen L.P., Næss-Pleym L.E., Dale J., Laugsand L.E. Patient visits to an emergency department in anticipation of the COVID-19 pandemic. Tidsskr Nor Laegeforen. 2020;140(8) doi: 10.4045/tidsskr.20.0277. [DOI] [PubMed] [Google Scholar]
- 8.Guo H., Zhou Y., Liu X., Tan J. The impact of the COVID-19 epidemic on the utilization of emergency dental services. J Dent Sci. 2020 doi: 10.1016/j.jds.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.COVID-19 Webinar: a unique insight in highly impacted countries. 2020. https://academy.eusem.org/eusem/2020/covid-19/290502/session.speakers.covid-19.webinar.a.unique.insight.in.highly.impacted.countries.html?fmenu=8*browseby=8*sortby=2*label=19798 Sharing experiences of high COVID-19 impact countries. Accessed 13.4.2020.
- 10.Ong M.E.H., Ho K.K., Tan T.P., Koh S.K., Almuthar Z., Overton J., et al. Using demand analysis and system status management for predicting ED attendances and rostering. Am J Emerg Med. 2009;27(1):16–22. doi: 10.1016/j.ajem.2008.01.032. [DOI] [PubMed] [Google Scholar]
- 11.Atherton W.G., Harper W.M., Abrams K.R. A year’s trauma admissions and the effect of the weather. Injury. 2005;36(1):40–46. doi: 10.1016/j.injury.2003.10.027. [DOI] [PubMed] [Google Scholar]
- 12.Rotstein Z., Wilf-Miron R., Lavi B., Shahar A., Gabbay U., Noy S. The dynamics of patient visits to a public hospital ED: a statistical model. Am J Emerg Med. 1997;15(6):596–599. doi: 10.1016/s0735-6757(97)90166-2. [DOI] [PubMed] [Google Scholar]
- 13.McCarthy M.L., Zeger S.L., Ding R., Aronsky D., Hoot N.R., Kelen G.D. The challenge of predicting demand for emergency department services. Acad Emerg Med. 2008;15(4):337–346. doi: 10.1111/j.1553-2712.2008.00083.x. [DOI] [PubMed] [Google Scholar]
- 14.Boutis K., Stephens D., Lam K., Ungar W.J., Schuh S. The impact of SARS on a tertiary care pediatric emergency department. CMAJ. 2004;171(11):1353–1358. doi: 10.1503/cmaj.1031257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang C.C., Yen D.H., Huang H.H., Kao W.F., Wang L.M., Huang C.I., et al. Impact of severe acute respiratory syndrome (SARS) outbreaks on the use of emergency department medical resources. J Chin Med Assoc. 2005;68(6):254–259. doi: 10.1016/s1726-4901(09)70146-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hahn B., Zuckerman B., Durakovic M., Demissie S. The relationship between emergency department volume and patient complexity. Am J Emerg Med. 2018;36(3):366–369. doi: 10.1016/j.ajem.2017.08.023. [DOI] [PubMed] [Google Scholar]
- 17.Man C.Y., Yeung R.S., Chung J.Y., Cameron P.A. Impact of SARS on an emergency department in Hong Kong. Emerg Med (Fremantle) 2003;15(5–6):418–422. doi: 10.1046/j.1442-2026.2003.00495.x. [DOI] [PubMed] [Google Scholar]
- 18.Blendon R.J., Benson J.M., DesRoches C.M., Raleigh E., Taylor-Clark K. The public’s response to severe acute respiratory syndrome in Toronto and the United States. Clin Infect Dis. 2004;38(7):925–931. doi: 10.1086/382355. [DOI] [PubMed] [Google Scholar]
- 19.Lew T.W., Kwek T.K., Tai D., Earnest A., Loo S., Singh K., et al. Acute respiratory distress syndrome in critically ill patients with severe acute respiratory syndrome. Jama. 2003;290(3):374–380. doi: 10.1001/jama.290.3.374. [DOI] [PubMed] [Google Scholar]