Introduction
As severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spreads worldwide, nonrespiratory manifestations of coronavirus disease 2019 (COVID-19) are being reported with greater frequency. A variety of dermatologic eruptions associated with this viral infection have been recognized. Although urticaria has been reported several times in association with COVID-19, angioedema has rarely been reported. We present a case of angioedema and urticaria occurring in the setting of COVID-19 infection and review cases published in the medical literature.
Case summary
A 40-year-old previously healthy man presented to the emergency department with a 1-day history of lip and bilateral eyelid swelling and a generalized pruritic rash, all starting simultaneously. The patient described the lesions as migratory, each lasting for a few hours. The rash started on the back and subsequently spread to his extremities within hours, sparing his face and scalp. The eyelid swelling decreased on the same day without treatment, whereas the lip swelling persisted. Clinically, there was no clear association with ingestion of any food or medication. He denied recent ingestion of newly prescribed or over-the-counter medications, herbal supplements, or home remedies. He denied similar previous presentations or history of allergies, except for an episode of generalized rash after receiving an antibiotic 4 years before presentation. The patient had no medical conditions and denied receiving any medications, including angiotensin-converting enzyme 2 inhibitors.
Before the symptoms occurred, he had a 5-day history of mild, nonproductive cough and dyspnea with low-grade fever. He reported ingesting 2 g (4 tablets) of acetaminophen for the fever within 2 days before his presentation, but with no improvement. He had regularly received acetaminophen in the past without any rashes or adverse reactions. He did not report a history of smoking or alcohol consumption and also denied family history of allergies or angioedema. The patient denied contact with any individuals with a confirmed positive case of COVID-19. He was employed as support staff for a designated COVID-19 hospital.
On examination, the patient was in mild respiratory distress. Vital signs on admission were as follows: temperature 37.4°C, blood pressure 118/67 mm Hg, respiratory rate 22/min, and oxygen saturation 97% on room air. Erythematous generalized urticarial welts were noted, more prominent on the trunk (Fig 1), whereas the palms and soles were spared. Dermographism was not detected. His lips were markedly swollen (Fig 2); eyelid swelling was resolving at presentation. No other skin abnormalities were found. There were no wheezes or crackles on chest examination.
Fig 1.

Welts on the trunk.
Fig 2.

Angioedema of the lips.
Laboratory investigation results were within normal limits, except for a significantly elevated D-dimer level of 15.05 μg/mL (normal value <0.50 μg/mL). Nasopharyngeal swab result for COVID-19 reverse transcriptase–polymerase chain reaction test was positive. Chest radiograph showed bilateral lower-zone opacities and infiltrations typical for COVID pneumonia of moderate severity. Electrocardiogram showed possible S1, Q3, and T3 changes that were suggestive of pulmonary embolism. Therefore, a therapeutic dose of low-molecular-weight heparin (enoxaparin at 1 mg/kg/d) was started. Despite the high probability of pulmonary embolism, computed tomographic pulmonary angiography was not performed because of the potential risk of serious contrast reaction in a patient with angioedema.
After giving consent, the patient received loading doses of favipiravir at 1200 mg twice a day and hydroxychloroquine at 400 mg twice a day on day 1, followed by favipiravir 600 mg twice daily and hydroxychloroquine 200 mg twice daily, starting on day 2 for a total of 7 days in accordance with hospital protocol for treatment of moderate COVID-19 pneumonia. Urticaria and angioedema were treated with oral desloratadine 5 mg 3 times daily.
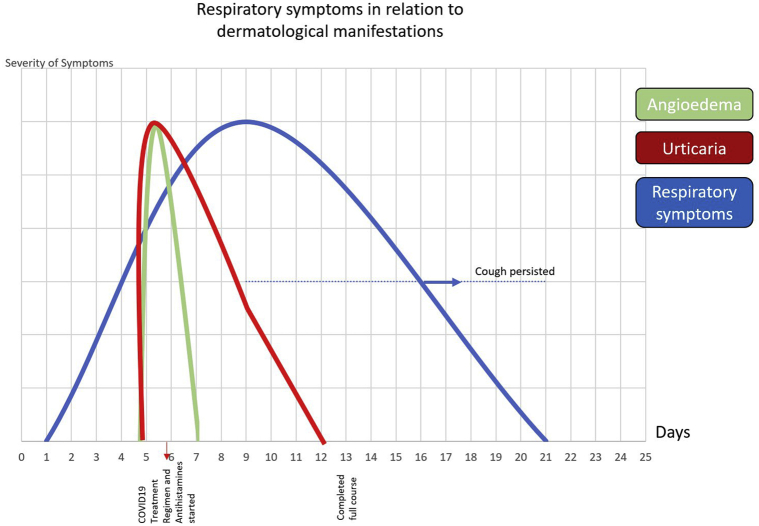
During hospitalization, the patient remained vitally and hemodynamically stable and did not require oxygen support. Lip swelling and urticaria resolved within 3 days and desloratadine was discontinued. Fever and shortness of breath resolved within 5 days, whereas the cough persisted for another 10 days. D-dimer levels decreased to 1.01 μg/mL during 5 days. There was no recurrence of angioedema or urticaria, and the patient was discharged to a quarantine facility in accordance with posthospitalization protocol for patients discharged with a positive COVID-19 polymerase chain reaction test result. The timeline of his symptoms is depicted in Fig 3.
Fig 3.
Timeline of patient's symptoms.
Discussion
COVID-19 infection can present with several distinctive symptoms, including dermatologic manifestations of various morphologies, such as vesicles, petechiae, acral chilblain lesions, exanthems, and urticaria.1 Although the exact etiology of COVID-19–related skin manifestations is still unclear, it is possible that SARS-CoV-2 acts like other viruses by initiating a state of mast cell activation, leading to histamine release.2
We conducted a search of PubMed and Scopus databases for articles, including case reports, published between December 1, 2019, and July 15, 2020, using the following search terms: COVID-19, coronavirus 2019, SARS-CoV-2, urticaria, angioedema, skin manifestations, and dermatology.
One of the first studies that described cutaneous manifestations in COVID-19 was performed by a group of dermatologists in Italy. It analyzed 88 COVID-19 patients and found different types of skin lesions in 20.4%.3 The main symptoms included erythematous rashes (14 cases), urticarial eruptions (3 cases), and vesicular rash (1 case). Another report from Indonesia described a 51-year-old patient who suddenly developed a generalized pruritic urticarial rash 3 days posthospitalization for COVID-19–related pneumonia.4 A Spanish study describing urticarial lesions in a COVID-19–positive patient did not find any difference between “common urticaria” and COVID-19–related urticaria on histologic examination.5
Although urticarial lesions have been described in patients with COVID-19 pneumonia, associated angioedema was rarely reported (Table I). Cohen at al6 described a case of a 61-year-old hypertensive man with COVID-19 who presented with a 12-hour history of lip and facial swelling, which occurred after 12 days of fever, chills, and dry cough. No other skin lesions or pruritus were present. All symptoms except cough improved after 2 days of methylprednisolone and diphenhydramine. Moreover, Adeliño and colleagues7 reported a 30-year-old woman who developed acute urticaria and angioedema 11 days after the onset of COVID-19 respiratory symptoms. Those manifestations quickly resolved after she received 3 days of ebastine 10 mg. Similar swift resolution of angioedema was observed in our case, which resolved within 3 days.
Table I.
Reported presentations of angioedema in coronavirus disease 2019 patients
| Author | Urticaria | Angioedema | Respiratory symptoms | Timeline | Treatment received for dermatologic manifestations |
|---|---|---|---|---|---|
| Current study | Yes | Yes, mainly lips and eyelids | Yes | Respiratory symptoms preceded urticaria and angioedema by 5 d | Desloratadine |
| Cohen6 | No | Yes, mainly facial and periorbital with upper lip involvement | Yes | Respiratory symptoms preceded urticaria and angioedema by 12 d | Methylprednisolone and diphenhydramine |
| Adeliño7 | Yes | Yes, mainly periorbital with mild lip involvement | Yes | Respiratory symptoms preceded urticaria and angioedema by 11 d and resolved before cutaneous manifestations appeared | Ebastine |
| Hassan8 | Yes | Yes, lips and hand swelling | Yes | Angioedema and urticaria preceded respiratory symptoms by 1 and 2 d, respectively | Fexofenadine hydrochloride and prednisolone |
| Azmy9 | No | Yes, tongue swelling | Yes | Respiratory symptoms preceded angioedema by 5 d | Diphenhydramine Methylprednisolone C1 esterase inhibitor |
In addition, Hassan8 described a case of a 46-year-old woman who initially presented with angioedema and urticaria, preceding respiratory symptoms of fever and dry cough, which developed on the second day of illness. She was treated successfully with diphenhydramine and methylprednisolone.
Azmy et al9 described an interesting approach to COVID-19–associated angioedema in a patient who developed angioedema and tongue swelling postintubation secondary to SARS-CoV-2–induced acute respiratory distress syndrome. Her angioedema was not associated with urticaria and was refractory to diphenhydramine and methylprednisolone. Although the patient had normal C1 esterase inhibitor levels and denied personal or family history of inherited angioedema, she was treated with a single dose of C1 esterase inhibitor (C1 esterase inhibitor at 20 units/kg), with resolution of her symptoms. Further studies are needed to determine whether this is an effective treatment for refractory COVID-19–related angioedema.
A plausible explanation for the development of angioedema lies in the established correlation between SARS-CoV-2 and angiotensin-converting enzyme 2, a receptor for the virus to enter the epithelial cells of the lungs.10 It is known that angiotensin-converting enzyme 2 has a crucial role in the inhibition of des-Arg9 bradykinin, which is a potent ligand of bradykinin receptor 1. Hence, the inhibition of angiotensin-converting enzyme 2 leads to excessive activation of the bradykinin pathway, and subsequently increases vascular permeability leading to angioedema.11,12 This is similar to the proposed mechanism by which this virus causes acute pulmonary edema and acute respiratory distress syndrome.12
Urticaria and angioedema are often triggered by various viral or bacterial infections, and COVID-19 infection is not an exception, adding a new member to the array of cutaneous manifestations of this enigmatic infection. Therefore, in the setting of this pandemic, these lesions should prompt early viral testing and infection control precautions when clinically relevant.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Galván Casas C., Català A., Carretero Hernández G. Classification of the cutaneous manifestations of COVID 19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020;183(1):71–77. doi: 10.1111/bjd.19163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wedi B., Raap U., Wieczorek D., Kapp A. Urticaria and infections. Allergy Asthma Clin Immunol. 2009;5(1):10. doi: 10.1186/1710-1492-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Recalcati S. Cutaneous manifestations in COVID 19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34(5):e212–e213. doi: 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]
- 4.Gunawan C., Angela A., Widysanto A. Urticarial eruption in coronavirus disease 2019 (COVID 19) infection: a case report in Tangerang, Indonesia. J Eur Acad Dermatol Venereol. 2020;34(8):e372–e373. doi: 10.1111/jdv.16622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Quintana-Castanedo L., Feito-Rodríguez M., Valero-López I., Chiloeches-Fernández C., Sendagorta-Cudós E., Herranz-Pinto P. Urticarial exanthem as early diagnostic clue for COVID 19 infection. JAAD Case Rep. 2020;6(6):498–499. doi: 10.1016/j.jdcr.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen A.J., DiFrancesco M.F., Solomon S.D., Vaduganathan M. Angioedema in COVID 19. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adeliño R., Andrés-Cordón J., Aracelis De La Cruz Martínez C. Acute urticaria with angioedema in the setting of coronavirus disease 2019. J Allergy Clin Immunol. 2020;8(7):2386–2387. doi: 10.1016/j.jaip.2020.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hassan K. Urticaria and angioedema as a prodromal cutaneous manifestation of SARS-CoV-2 (COVID 19) infection. BMJ Case Rep. 2020;13(7):e236981. doi: 10.1136/bcr-2020-236981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azmy V., Benson J., Love K., Steele R. Idiopathic nonhistaminergic acquired angioedema in a patient with COVID 19. Ann Allergy Asthma Immunol. 2020 doi: 10.1016/j.anai.2020.06.039. S1081-1206(20)30447-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choudhury A., Mukherjee S. In silico studies on the comparative characterization of the interactions of SARS-CoV-2 spike glycoprotein with ACE-2 receptor homologs and human TLRs. J Med Virol. 2020 doi: 10.1002/jmv.25987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hofman Z.L.M., van den Elzen M.T., Kuijpers J. Evidence for bradykinin release in chronic spontaneous urticaria. Clin Exp Allergy. 2020;50(3):343–351. doi: 10.1111/cea.13558. [DOI] [PubMed] [Google Scholar]
- 12.van de Veerdonk F.L., Netea M.G., van Deuren M. Kallikrein-kinin blockade in patients with COVID 19 to prevent acute respiratory distress syndrome. Elife. 2020;9:e57555. doi: 10.7554/eLife.57555. [DOI] [PMC free article] [PubMed] [Google Scholar]