Abstract
This cross-sectional study examines changes in the number of patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic in the United States.
Introduction
In response to the coronavirus disease (COVID-19) pandemic, the American Society of Clinical Oncology recommends, “to conserve health system resources and reduce patient contact with health care facilities,… that cancer screening procedures that require clinic/center visits, such as screening mammograms and colonoscopy, be postponed for the time being.”1 A Washington Post headline reported, “Patients with heart attacks, strokes, and even appendicitis vanish from hospitals.”2 A study from 9 high-volume US cardiac catheterization laboratories3 found a 38% decrease in patients treated for ST-elevation myocardial infarction, considered a life-threatening condition. In this study, we analyzed weekly changes in the number of patients with newly identified cancer before and during the COVID-19 pandemic.
Methods
This cross-sectional study included patients across the United States who received testing for any cause by Quest Diagnostics and whose ordering physicians assigned them International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes associated with any of 6 cancer types (ie, breast, colorectal, lung, pancreatic, gastric, and esophageal) from January 1, 2018, to April 18, 2020. Each patient was counted once, at the first instance of each ICD-10 code starting in January 2018. The weekly count was tracked starting with the first full calendar week of 2019 through April 18, 2020. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cross-sectional studies. This study was deemed exempt by the Western Institutional Review Board in accordance with 45 CFR §160 and §164 because no study participant provided specimens or information not already existing as part of health care operations.
Mean (SD) weekly numbers of newly diagnosed patients (Poisson regression for count), along with mean ages (2-sided t test) and sex distributions (χ2 test), were compared between baseline period (January 6, 2019, to February 29, 2020) and the COVID-19 period (March 1 to April 18, 2020) at a significance level of P < .05. Data analyses were performed using SAS Studio 3.6 on SAS version 9.4 (SAS Institute).
Results
This study included 278 778 patients, 258 598 (92.8%) from the baseline period and 20 180 (7.8%) from the COVID-19 period. Among all patients, 209 478 (75.1%) were women, and the mean (SD) age was 66.1 (12.7) years. During baseline, the mean (SD) weekly number of newly identified patients was 2208 (335) with breast cancer, 946 (134) with colorectal cancer, 695 (88) with lung cancer, 271 (39) with pancreatic cancer, 96 (14) with gastric cancer, and 94 (14) with esophageal cancer. During the pandemic, the weekly number fell 46.4% (from 4310 to 2310) for the 6 cancers combined, with significant declines in all cancer types, ranging from 24.7% for pancreatic cancer (from 271 to 204; P = .01) to 51.8% for breast cancer (from 2208 to 1064; P < .001) (Figure). The mean age of cancer patients in the COVID-19 period was within 1 year of that for patients in the baseline period; patients diagnosed with esophageal cancer in the COVID-19 period were slightly older than those diagnosed in the baseline period (mean [SD] age, 69.5 [11.0] years vs 68.4 [11.4] years; P = .04), but patients with all other cancers were younger (eg, breast cancer: mean [SD] age, 63.0 [13.0] years vs 64.3 [12.7] years; P < .001). Statistically, sex distribution in the 2 periods was the same in all cancers except for pancreatic, which had fewer women in the baseline group than the COVID-19 group (8083 of 16 268 [49.8%] vs 820 of 1547 [53.0%]; P = .01) (Table). The decrease had generally leveled beginning the week starting March 29, 2020 (Figure).
Figure. Newly Identified Cancers, Baseline Mean and Weekly During the Coronavirus Disease 2019 Pandemic.
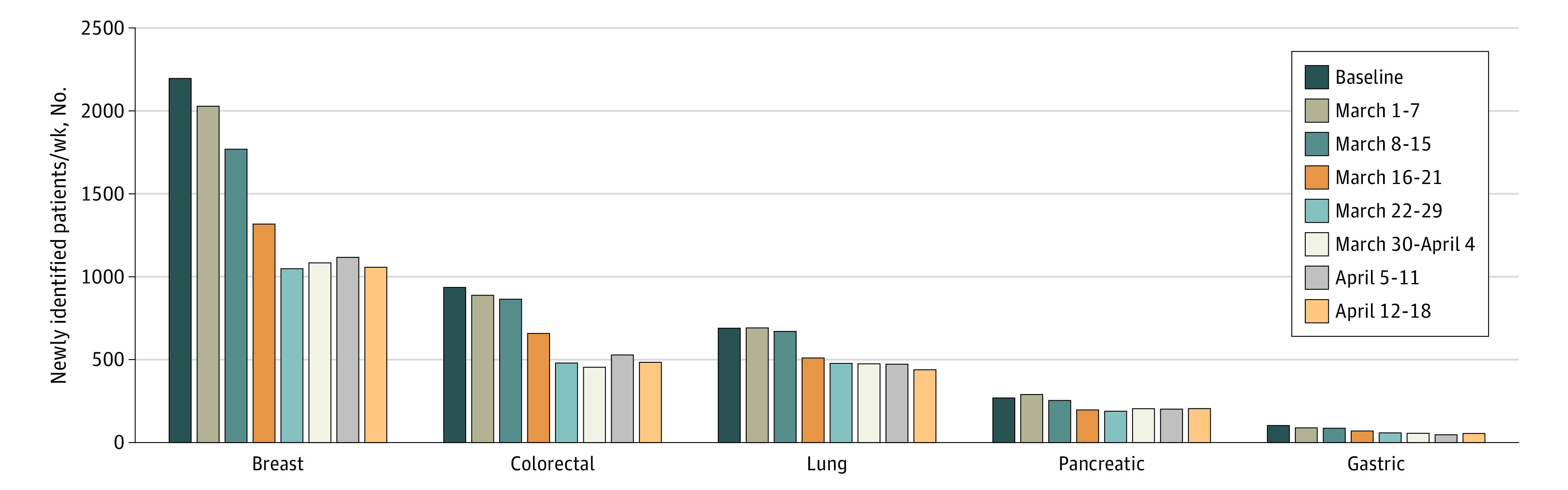
Table. Demographic Information for Patients With Newly Identified Cancer.
| Cancer type | January 6, 2019, to February 29, 2020 | March 1 to April 18, 2020 | ||||
|---|---|---|---|---|---|---|
| Patients, No. | Women, No. (%) | Age, mean (SD), y | Patients, No. | Women, No. (%) | Age, mean (SD), y | |
| Breast | 132 513 | 132 513 (100) | 64.3 (12.7) | 9475 | 9475 (100) | 63.0 (13.0) |
| Colorectal | 56 744 | 28 056 (49.6) | 66.7 (13.4) | 4377 | 2109 (48.2) | 65.4 (13.3) |
| Lung | 41 671 | 22332 (53.7) | 70.1 (10.6) | 3753 | 1960 (52.3) | 69.3 (11.0) |
| Pancreatic | 16 268 | 8083 (49.8) | 67.6 (12.7) | 1547 | 820 (53.0) | 66.8 (12.8) |
| Gastric | 5744 | 2454 (42.8) | 67.4 (13.5) | 471 | 180 (38.2) | 66.7 (13.8) |
| Esophageal | 5658 | 1354 (24.0) | 68.4 (11.4) | 557 | 142 (25.5) | 69.5 (11.0) |
Discussion
Our prepandemic data represented a good share of the National Cancer Institute weekly incidence estimates of the 6 cancers, ranging from 16% (lung cancer) to 42% (breast cancer).4 A potential limitation of this study is that the association of delayed diagnoses of cancer with outcomes likely depends on the final stage of disease at diagnosis, relative to baseline, and associated treatment implications (curative vs palliative).
Our results indicate a significant decline in newly identified patients with 6 common types of cancer, mirroring findings from other countries.5 The Netherlands Cancer Registry has seen as much as a 40% decline in weekly cancer incidence, and the United Kingdom has experienced a 75% decline in referrals for suspected cancer since COVID-19 restrictions were implemented.5
While residents have taken to social distancing, cancer does not pause. The delay in diagnosis will likely lead to presentation at more advanced stages and poorer clinical outcomes. One study suggests a potential increase of 33 890 excessive cancer deaths in the Untied States.6 Our findings are consistent with previous research,1,2,3,5 and they call for urgent planning to address the consequences of delayed diagnoses. Planning may entail more robust digital technology to strengthen clinical telehealth offerings and other patient-clinician interactions, including self-service scheduling across specialties and well-designed collection processes.
References
- 1.American Society of Clinical Oncology . Cancer screening, diagnosis, staging, and surveillance. Updated June 22, 2020. Accessed July 13, 2020. https://www.asco.org/asco-coronavirus-resources/care-individuals-cancer-during-covid-19/cancer-screening-diagnosis-staging
- 2.Bernstein L, Sellers FS. Patients with heart attacks, strokes and even appendicitis vanish from hospitals. Published April 19, 2020. Accessed April 27, 2020. https://www.washingtonpost.com/health/patients-with-heart-attacks-strokes-and-even-appendicitis-vanish-from-hospitals/2020/04/19/9ca3ef24-7eb4-11ea-9040-68981f488eed_story.html
- 3.Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871-2872. doi: 10.1016/j.jacc.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Surveillance, Epidemiology, and End Results Program. Cancer stat facts: esophageal cancer. Accessed April 27, 2020. https://seer.cancer.gov/statfacts/html/esoph.html
- 5.IJzerman M, Emery J. Is a delayed cancer diagnosis a consequence of COVID-19? Published April 30, 2020. Accessed May 1, 2020. https://pursuit.unimelb.edu.au/articles/is-a-delayed-cancer-diagnosis-a-consequence-of-covid-19
- 6.Lai A, Pasea L, Banerjee A, et al. . Estimating excess mortality in people with cancer and multimorbidity in the COVID-19 emergency. medRxiv. Preprint posted online June 1, 2020. doi: 10.13140/RG.2.2.34254.82242 [DOI] [Google Scholar]


