Abstract
The global challenge presented by COVID‐19 is unparalleled. Shortages in healthcare staff and manpower bring the practical skills of medical students under the spotlight. However, before they can be placed on hospital frontlines, it is crucial to assess their preparedness for patient interaction. This can be achieved by comparing their behavioral dynamics to those of physicians. An online questionnaire was administered between March 20, 2020 and March 27, 2020. The preventive strategies adopted by medical students and physicians at different ages and levels of education were compared by using chi‐square test where a p value of <0.05 was considered statistically significant. We report that the demonstration of preventive behaviors increased with educational attainment and age. Older age groups avoided crowded areas, wore more masks, used disinfectants and did not touch their faces as compared to the younger participants (p < 0.001). Similarly, postgraduate doctors used more masks and disinfectants as compared to graduate doctors and medical students (p < 0.001). Based on our results, the lack of preventive behavior shown by medical students has implications for policy makers. We recommend short‐ and long‐term changes to medical programs and admissions policies to equip medical students with the personal and professional skills to better contribute to the healthcare system in the present pandemic and beyond.
Keywords: active learning, behavior, COVID‐19, medical education, pandemic, public health, risk, teaching in medical schools
1. INTRODUCTION
The rapid global spread of COVID‐19 has been unprecedented. The World Health Organization (WHO) has raised alarm by declaring it a pandemic since March 11, 2020. 1 As of April 25, 2020, more than 200 countries have been affected. 2 Within a short period of few months, this state of emergency has undermined the stability of healthcare systems worldwide. In the absence of any treatment or vaccine, the only way to counter the outbreak is by adopting preventative measures. Therefore, national and international governments are promoting social distancing strategies to prevent disease.
While most of the population remains at home, healthcare professionals continue to manage patients at hospitals, putting themselves in the line of fire in the fight against coronavirus. As a consequence, their risk of acquiring infection remains high. The latest data suggest that healthcare workers comprise nearly a third of all infected cases worldwide. 3 As the number of infected care providers continue to rise, the outbreak is increasingly overwhelming resources. Medical efforts against the coronavirus are further limited by significant hospital staff shortages. 4
To reduce the impact of these shortages, extraordinary measures are being imposed: annual leaves are being cancelled for doctors, junior doctors are managing specialist duties and even medical students are being considered to support response efforts against COVID‐19. 5 , 6
Desperate circumstances demand desperate measures. In the current pandemic, employing future physicians to support understaffed and overworked healthcare teams seems logical. However, before we consider placing medical students at the forefront of this battlefield, it is important to gauge their preparedness to support response efforts. Many have questioned the benefits of involving medical students with their limited knowledge and clinical exposure. In fact, some argue that their inexperience can turn them into vectors of transmission contributing further to the problem. 7 , 8
Recent efforts by medical schools to modify pedagogy have promoted competency‐based learning globally. However, medical curricula in most of the developing world still focus on academic knowledge and classroom‐based didactic teaching. The applicability of evidence‐based knowledge is limited. Insufficient emphasis on public health education deprives students of a broad outlook on healthcare systems. 9 Studies suggest that instead of improving, perceptions of medical students about the importance of preventive strategies diminish during their undergraduate years. 10 , 11 In the current health crisis, transmission control mainly relies on human behavior. Healthcare professionals are considered role models by their patients. 12 Evidence suggests that lifestyle followed by doctors influences their treatment of the patients. 13 Doctors who adopt and exhibit healthy behaviors provide better advice and motivation to their patients. 14 As prevention is currently our only way to counter disease transmission, the behavior and advice of doctors and medical students treating patients at the hospital will play a fundamental role in control efforts against COVID‐19. However, a lack of healthful behavior has been reported widely in medical students worldwide and in Pakistan. 15 , 16
These reports are concerning and require prompt action from medical educators. The current crisis has underscored a need for student training in public health like never before. The inability of students to support response efforts against COVID‐19 because of their limited knowledge, lack of skill, and deficient preventive health education raises questions about the practical utility of current medical curricula. 17 , 18
It is clear that insufficient knowledge affects student behavior negatively. Additionally, the age and maturity of medical students has also shown to affect their competency. 19
Scientists recognize medical students, junior doctors and senior doctors as behaviorally distinct groups based on their knowledge and age. 20 Despite that, there are only a few reports of comparative data on their preventive behavior. To address this gap, for the first time in the region, we seek to compare the preventative strategies adopted by future physicians and current doctors at varying levels of education and ages.
The present health crisis and a constantly increasing burden of infectious diseases in the region 21 give a completely new perspective to the future of medical education. By comparing the most significant determinants of behavior we aim to develop an educational map to better prepare undergraduate students to work alongside healthcare teams in current and future emergency health situations.
2. MATERIAL AND METHODS
2.1. Study design and settings
This is a descriptive cross‐sectional survey carried out during the last week of March 2020. The study was ethically approved by the Institutional Review Board (IRB) of HITEC‐IMS, Taxila.
2.2. Participants
This study included adults above 18 years of age who were either studying at a medical university or had completed graduate or postgraduate medical education. Informed consent was obtained, and random convenient sampling was used to select participants. The participants were invited through email to fill and submit the attached questionnaire.
2.3. Questionnaire
Questionnaire was developed and a pilot study was conducted on a sample of 30 participants. Feedback was used to modify the items and finalized instrument was administered electronically. Preventive measures advertised by National Institute of Health (NIH) on its official website were employed to assess the precautionary behavior. 22 Participants' responses were dichotomous (yes/no). The survey consisted of two sections. The first section collected demographic information about age, gender, and location. The second section comprised eight preventive strategies propagated widely through campaigns over the country. The Cronbach's alpha coefficient for the questionnaire was more than 0.7.
The study was ethically approved by the Institutional Review Board of HITEC‐IMS, Taxila.
2.4. Data and analysis
Data were collected electronically and analyzed using SPSS Version 23. Descriptive analysis was done to report frequencies and percentages. The preventive behavior was compared between different ages and education levels by employing chi‐square test. A p value of <0.5 was considered significant.
3. RESULTS
Responses were submitted by 704 participants (response rate = 78%) out of which 62% (n = 436) were females and males were 38% (n = 268). Figure 1 presents information about education levels based on the gender of the participants. A total of 306 responses were submitted by undergraduate students (43%), while graduate and postgraduate participants provided 250 (35%) and 148 (21%) responses, respectively.
FIGURE 1.
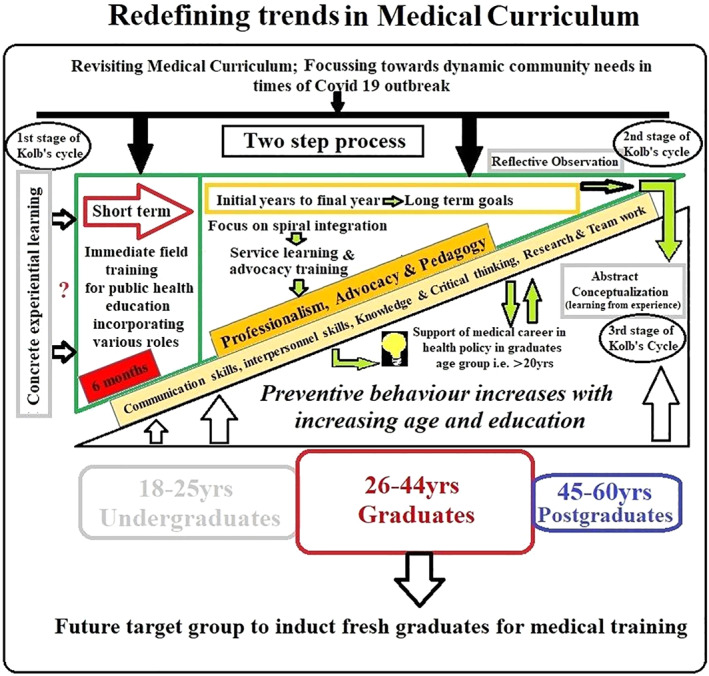
A conceptual model of reviewing medical curriculum displaying stepwise progression through three successive stages of Kolb's cycle. The impetus for the growth of new impressions is provided by firsthand experiences. The author's recommend practising spiral curriculum with revisions and recommendations of curricular reform committee's to achieve the competencies required in our graduates according to the guidelines of ACGME, Canadian Medical Education Directives for Specialists (CanMEDS), Foundation for Advancement of International Medical Education and Research (FAIMER), Association for Medical Education in Europe (AMEE), and World Health Organization (WHO)
The comparison of the age and education is shown in Figure 2. Out of 306 undergraduate students, 97% (297) were between 18 and 25 years of age and 3% (9) were between 26 and 44 years. Similarly, 99% (248) of graduate respondents were aged between 26 and 44 years and less than 1% (2) were between 45 and 60 years of age. The number of postgraduate participants aged between 26 and 44 years was 17% (27) and those between 45 and 60 years were 83% (121).
The difference in preventive behavior shown by participants based on their education is shown in Table 1. Responses indicate that there is no significant difference between the preventive measures being taken by undergraduate college students, compared to those who have graduated (p > 0.05, Table 1). However, it can be seen that postgraduate professionals use face masks and antiseptics significantly more than both undergraduate students and graduates (p < 0.05, Table 1). With regard to other preventive measures, there is no considerable difference between the groups.
TABLE 1.
Comparison of preventive behavior for COVID‐19 shown by undergraduates (n = 306), graduates (n = 250), and postgraduates (n = 148)
| Responses | N (%) | Chi‐square/p | N (%) | Chi‐square/p | N (%) | Chi‐square/p | |||
|---|---|---|---|---|---|---|---|---|---|
| Undergraduates | Graduates | Undergraduates | Postgraduates | Graduates | Postgraduates | ||||
| Covered cough/sneeze | |||||||||
| Yes | 278 (91) | 230 (92) | 0.06 | 278 (91) | 137 (92) | 0.06 | 230 (92) | 137 (92) | 0 |
| No | 28 (9) | 20 (8) | p = 0.79 | 28 (9) | 11 (8) | p = 0.79 | 20 (8) | 11 (8) | 1 |
| Avoided close contacts | |||||||||
| Yes | 288 (94) | 228 (91) | 0.64 | 288 (94) | 136 (92) | 0.30 | 228 (91) | 136 (92) | 0.06 |
| No | 18 (6) | 22 (9) | p = 0.42 | 18 (6) | 12 (8) | p = 0.57 | 22 (9) | 12 (8) | 0.79 |
| Wear face masks | |||||||||
| Yes | 217 (71) | 189 (75) | 0.40 | 217 (71) | 136 (92) | 14.6 | 189 (75) | 136 (92) | 10.48 |
| No | 89 (19) | 61 (25) | p = 0.52 | 89 (29) | 12 (8) | p < 0.001** | 61 (25) | 12 (8) | p = 0.001** |
| Avoid crowded areas | |||||||||
| Yes | 290 (95) | 234 (93) | 0.35 | 290 (95) | 138 (93) | 0.35 | 234 (93) | 138 (93) | 0 |
| No | 16 (5) | 16 (7) | p = 0.55 | 16 (5) | 10 (7) | p = 0.55 | 16 (7) | 10 (7) | p = 1 |
| Washed hands for 20 s with soap | |||||||||
| Yes | 289 (94) | 238 (95) | 0.09 | 289 (94) | 142 (95) | 0.09 | 238 (95) | 142 (95) | 0 |
| No | 17 (6) | 12 (5) | p = 0.75 | 17 (6) | 6 (5) | p = 0.75 | 12 (5) | 6 (5) | p = 1 |
| Use disinfectants | |||||||||
| Yes | 219 (71) | 199 (80) | 2.18 | 219 (72) | 134 (90) | 11.49 | 199 (80) | 134 (90) | 3.92 |
| No | 87 (29) | 51 (20) | p = 0.13 | 87 (28) | 14 (10) | p < 0.001** | 51 (20) | 14 (10) | p < 0.04* |
| Avoid touching face | |||||||||
| Yes | 259 (85) | 214 (86) | 0.04 | 259 (85) | 131 (88) | 0.38 | 214 (86) | 131 (88) | 0.20 |
| No | 47 (15) | 36 (14) | p = 0.84 | 47 (15) | 17 (12) | p = 0.53 | 36 (14) | 17 (12) | p = 0.65 |
| Stay home | |||||||||
| Yes | 272 (89) | 215 (86) | 0.41 | 272 (89) | 132 (89) | 0 | 215 (86) | 132 (89) | 0.41 |
| No | 34 (11) | 35 (14) | p = 0.52 | 34 (11) | 16 (11) | p = 1 | 35 (14) | 16 (11) | p = 0.52 |
*Significant; **Highly significant.
The variation in adopting preventive strategies with age is shown in Table 2. Based on the responses, participants above the age of 45 were significantly more cautious. They used more masks, avoided overcrowded places, used antiseptics, and avoided touching their face significantly more than other age groups (p < 0.05, Table 2).
TABLE 2.
Comparison of preventive behavior for COVID‐19 shown by ages 18–25 (n = 297), 26–44 (n = 284), and 45–50 (n = 123)
| N (%) | Chi‐square/p | N (%) | Chi square/p | N (%) | Chi square/p | ||||
|---|---|---|---|---|---|---|---|---|---|
| Responses | 18–25 (years) | 26–44 (years) | 18‐25 (years) | 45‐60 (years) | 26‐44 (years) | 45‐60 (years) | |||
| Covered cough/sneeze | |||||||||
| Yes | 257 (87) | 254 (89) | 0.14 | 257 (87) | 115 (93) | 2.60 | 254 (89) | 115 (93) | 0.97 |
| No | 40 (13) | 30 (11) | p = 0.52 | 40 (13) | 8 (7) | p = 0.10 | 30 (11) | 8 (7) | p = 0.3 |
| Avoided close contacts | |||||||||
| Yes | 249 (84) | 246 (87) | 0.34 | 249 (84) | 116 (94) | 5.10 | 246 (87) | 116 (94) | 2.84 |
| No | 48 (16) | 38 (13) | p = 0.55 | 48 (16) | 7 (6) | p < 0.02* | 38 (13) | 7 (6) | p = 0.09 |
| Wear face masks | |||||||||
| Yes | 192 (65) | 233 (82) | 7.4 | 192 (65) | 117 (95) | 9.8 | 233 (82) | 117 (95) | 8.3 |
| No | 105 (35) | 51(18) | p = 0.001** | 105 (35) | 6 (5) | p < 0.001** | 51 (18) | 6 (5) | p < 0.001** |
| Avoid crowded areas | |||||||||
| Yes | 283 (95) | 263 (95) | 0.35 | 283 (95) | 116 (94) | 0.09 | 263 (93) | 116 (94) | 4.8 |
| No | 14 (5) | 21 (7) | p = 0.55 | 14 (5) | 7 (6) | p = 0.74 | 21 (7) | 7 (6) | p < 0.02* |
| Washed hands for 20 s with soap | |||||||||
| Yes | 283 (95) | 269 (95) | 0.09 | 283 (95) | 117 (95) | 0.09 | 269 (95) | 117 (95) | 0.09 |
| No | 14 (5) | 15 (5) | p = 0.75 | 14 (5) | 6 (5) | p = 0.75 | 15 (5) | 6 (5) | p = 0.75 |
| Use disinfectants | |||||||||
| Yes | 221 (74) | 215 (76) | 0.10 | 221 (74) | 116 (94) | 14.88 | 215 (76) | 116 (94) | 12.7 |
| No | 76 (26) | 69 (24) | p = 0.74 | 76 (26) | 7 (6) | p < 0.001** | 69 (24) | 7 (6) | p < 0.001** |
| Avoid touching face | |||||||||
| Yes | 251 (84) | 236 (83) | 0.14 | 251 (84) | 117 (95) | 6.43 | 236 (83) | 117 (95) | 7.3 |
| No | 46 (16) | 48 (17) | p = 0.69 | 46 (16) | 6 (5) | p < 0.01* | 48 (17) | 6 (5) | p < 0.006** |
| Stay home | |||||||||
| Yes | 260 (88) | 243 (86) | 0.17 | 260 (88) | 116 (94) | 2.19 | 243 (86) | 116 (94) | 3.5 |
| No | 37 (12) | 41 (14) | p = 0.67 | 37 (12) | 7 (6) | p = 0.13 | 41 (14) | 7 (6) | p = 0.06 |
*Significant; **Highly significant.
The most common preventive strategy followed by participants was to wash their hands (>90%).
4. DISCUSSION
According to our data, preventive behavior improves with increasing levels of medical education and clinical exposure. Postgraduate participants adopted the most preventive measures to protect themselves. They used more masks and disinfectants than graduates and undergraduates (p < 0.5). Similarly, graduate respondents used more masks and disinfectants than undergraduates, but the difference was not significant (p > 0.5, Table 1). These results are consistent with studies associating educational attainment with healthful practices 23 , 24 and can be explained on the basis of a number of possible mechanisms.
It is well documented that higher education and experience improve cognitive abilities. 25 , 26 Indeed, physicians' clinical experience and exposure has been shown to impact patient safety. 27 The relation between education level and preventive behavior has also been described in previous epidemics. 28 This association is understandable as during their postgraduate years, doctors are constantly exposed to complex tasks and challenges which require flexible thinking. In order to perform their clinical duties, they learn to strategize, plan, and implement solutions. Furthermore, a greater acquaintance with health advocacy and community service in the field makes graduates more conscious of their health and aware of the consequences of nonprevention. 29
To prepare medical students for a frontline role in public health emergencies like COVID‐19, there is a need to increase their knowledge and skills. Studies suggest that experiential learning through community involvement can contribute to this, improving health attitudes and behaviors. 30 , 31 , 32 To this end, there have been efforts to incorporate community engagement and real patient experience into medical education, internationally. 33
Nonetheless, deficits in medical curricula regarding health advocacy and service learning are still widely recognized. 34 This is especially notable in the developing world, where most teaching is still traditional and teacher centered with limited patient interaction. 35
Based on our results, we propose a novel conceptual model to bring curricular reforms. These would allow for short‐term possibilities to deal with the current crisis and long‐term strategies to establish permanent changes in medical education (Figure 1).
In the short term, we propose that medical students are enrolled in an intensive public health education course with immediate effect. The formal medical syllabus could be suspended for 6 months. Initially, students would undergo a month of intensive online training on infectious disease epidemiology, control, and prevention. This should continue into field training for the next 2 months in which students support the health response to COVID‐19 through various roles. 36 For example, they may provide guidance to individuals about symptoms through hotline services. Moreover, they can be involved in research activities at national laboratories to develop vaccines and ventilators, support awareness campaigns, and help plan strategies for contact tracing and effective quarantine. Finally, they could be deployed at healthcare facilities to shadow healthcare workers in their response efforts against the pandemic. A few institutions have started to incorporate this training throughout their curricula 37 ; however, such changes should be enforced by policy makers as a part of a unified national effort against coronavirus.
Involving thousands of trained medical students can help immensely with response efforts and limit sustained transmission of COVID‐19. Nonetheless, interrupting the medical curriculum might appear counterproductive in the short‐term. One problem could be that by delaying graduation, less house officers will be available to work as residents in hospitals next year. However, this issue can be resolved if capable final year students are offered an early graduation by licencing authorities.
In the long‐term, we propose (Figure 1) important changes to the medical curriculum with the integration of public health education through service‐learning opportunities and advocacy training. Medical educators have emphasized the value of inculcating civic responsibility in medical students through working with communities in real life settings. In Pakistan, the current curriculum does not provide learning opportunities in a real life context. 38 In addition to a formal public health curriculum, early and frequent clinical exposure should start from year one of medical college. Students should have opportunity to shadow general practitioners and volunteer at health camps for underserved populations. Research shows that if lifestyle health priorities are addressed early in medical education, this not only improves the health behavior of medical students, but also strengthens their clinical skills. 17 Beyond the public health academic curriculum, small groups of students should be involved in multiyear community‐based projects. This may include health fairs and awareness campaigns for vulnerable communities. These changes are achievable in both developed and developing countries with minimal resource requirements. If adopted, they will provide students with the opportunity to understand the social determinants of health and available resources, as well as the importance of preventive behavior. The inclusion of project‐based learning will help students to better understand the importance of preventive behavior, improving their engagement with public health while building their research and analysis skills. 39 The long‐term goal of service learning and advocacy training in medical curricula is to develop skilled and committed groups of students who can contribute to their communities whenever the need arises. This would inculcate students with a sense of responsibility, empathy, and interpersonal skills in the earliest years of their medical training. Moreover, it would enable medical students—who constitute a valuable yet underutilized resource—to benefit society and act as positive role models for healthful practices.
Another long‐term measure which we suggest according to our findings is to alter the age of students applying to medical school. This study demonstrates that the strong influence of age on preventive behavior has implications for policy makers and medical school authorities. Since healthful behavior improved with aging, irrespective of medical education, the authors propose (Figure 1) to increase the required age for the medical entrants. This could be achieved by delaying the entry into medical school until after the completion of an undergraduate degree.
Doctors who aged between 45 and 60 years undertook significantly more protective measures and avoided close contact with those who were sick. Similarly, they used considerably more masks and disinfectants and avoided crowded areas more than other experimental groups. Regarding these measures, there was also a noticeable difference between 26‐ and 44‐year‐old doctors and medical students younger than 25 years of age (Table 2). There is empirical evidence of the effect of age on preventative behavior. 40 It is also well known that middle age is when an individual is at the peak of his career and confidence. Assuming multiple roles, they are not only contributing to the society, but are also leading families as responsible adults. They are more in control than young or older adults. 41 , 42 , 43 The influence of perceived control on health‐related behavior has been described previously. 44 As decision makers, participants belonging to this age group may have acted more responsibly by taking more preventive measures to prevent the outbreak in their families and community.
Currently, the students joining medical school in Pakistan and other countries like the United Kingdom are coming straight from high school and are 18–19 years of age. The present system of recruiting medical students places older or graduate applicants at a disadvantage. 45 However, in the United States entry to medical school is restricted to graduates who are usually in their 20s. Research shows that students who enter medical school after graduating are more motivated, mature, and hardworking. 46 The age of the medical student has shown to bring certainty and motivation. 45 , 47 , 48 In fact it has been observed that older incoming medical students, whether they have an undergraduate degree or not, are better able to handle responsibilities and are more ready to become future doctors than 18‐year olds. 45
Following the theory of creating knowledge by transformation of experience presented by David Allen Kolb, 49 our educational model shows that in terms of both short‐ and long‐term proposed goals we will be at Stage 1 of Kolb's cycle (Figure 1). In this stage, our learner will actively experience an activity such as field work in early and later years of clinical training. The second stage of Kolb's cycle, which is reflective observation, is represented during and towards the end of the program. These reflective observations would be made by the academicians, educationists and the students themselves through formative and summative assessments. The students ultimately will be modeling a change, representing the third stage of Kolb's cycle (i.e., abstract conceptualization of field training) after graduation, as depicted in Figure 1. Achieving the third stage of Kolb's cycle is vital, as experiences learned during the course will change behaviors. This will manifest as improvement in acquiring competencies such as professionalism, advocacy and pedagogy as demonstrated by Kirkpatrick's model. 50 The result will be an inculcation of what the World Health Organization calls essential skills of a “five‐star doctor”. 51
5. CONCLUSIONS
As the current outbreak is rapidly exhausts healthcare resources, the importance of a prompt and effective response cannot be understated. The vast potential of medical students, as a force for change, is limited by their current training. The challenges in involving willing, energetic, and enthusiastic students in emergency health responses are substantial and can be overcome in the short‐term by initiating training courses, and in the long‐term through incorporating changes in admission policies and curricula. Indeed, medical education must be tailored it to enable the students to synchronize with evolving and emerging infectious diseases. Unless measures are taken to better prepare undergraduate students to deal with situations like the COVID‐19 pandemic, their supporting role will always be uncertain and associated with risk.
5.1. Limitations
There are certain limitations to our study. We collected data mainly from three provinces (Federal capital, Punjab, and Sindh) with less representation of others; hence geographical limitations should be considered. There is no such study available on health education intervention in our region before this pandemic, so a comparison cannot be done. However, implementing a health education program in future may lead to an empirically effective evidence by comparing with our study. Even though the questionnaire was developed following preventive measures advertised by NIH and piloted, the results may still be deviated from the real situation; however, this does not affect the overall results of our study as feedback was used to modify the items. In spite of these limitations, our study provides future directions to academicians, medical educationists, and health policy makers to make swift curricular interventions and research ideas for advancement in service learning and health advocacy.
Lessons for practice.
Preventive behaviors differ with age and level of educational attainment.
Long‐term solution to improve public health exposure is through experiential learning.
Short courses in public health are essential to prepare medical students for COVID‐19 support.
Increase the required age for the medical entrants to improve preventive behavior.
Curricular reforms can build medical students' potential to support healthcare systems in health emergencies.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
ACKNOWLEDGMENT
The authors would like to express their gratitude to our participants who shared their valuable time to complete our questionnaire.
Haque A, Mumtaz S, Khattak O, Mumtaz R, Ahmed A. Comparing the preventive behavior of medical students and physicians in the era of COVID‐19: Novel medical problems demand novel curricular interventions. Biochem Mol Biol Educ. 2020;48:473–481. 10.1002/bmb.21406
REFERENCES
- 1. Word Health Organization . (2020) WHO Director‐General's opening remarks at the media briefing on COVID‐19. [cited 2020 Apr 8]. Available from: https://www.who.int/dg/speeches/detail/who‐director‐general‐s‐opening‐remarks‐at‐the‐media‐briefing‐on‐covid‐19‐‐‐20‐april‐2020.
- 2. Coronavirus Disease (COVID‐2019) Situation Reports . (2020). Situation report 107. [cited 2020 Apr 3]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- 3. Centre for Evidence Based Medicine: COVID‐19 (2020) How many healthcare workers are infected? [cited 2020 Apr 6]. Available from: https://www.cebm.net/covid-19/covid-19-how-many-healthcare-workers-are-infected/.
- 4. Dunhill L. Intensive care staffing ratios dramatically diluted. Essex, UK: HSJ Wilmington Healthcare Limited. [cited 2020 Apr 14]. Available from:, 2020. https://www.hsj.co.uk/exclusive‐intensive‐care‐staffing‐ratios‐dramatically‐diluted/7027214. [Google Scholar]
- 5. Khan AA. (2020) Medical university students called in to fight pandemic. University World News. [cited 2020 Apr 06]. Available from: https://www.universityworldnews.com/post.php?story=20200409084747835.
- 6. Farber ON. (2020) Medical students can help combat Covid‐19. Don't send them home. STAT. [cited 2020 Apr 06]. Available from: https://www.statnews.com/2020/03/14/medical-students-can-help-combat-covid-19/.
- 7. Krieger P, Goodnough A. (2020) Medical students, sidelined for now, find new ways to fight coronavirus. The New York Times. [cited 2020 Apr 06]. Available from: https://www.nytimes.com/2020/03/23/health/medical‐students‐coronavirus.html.
- 8. Association of American Medical Colleges . (2020) Guidance on medical students' clinical participation: effective immediately. [cited 2020 Apr 06]. Available from: https://www.aamc.org/system/files/2020‐04/meded‐April‐14‐Guidance‐on‐Medical‐Students‐Participation‐in‐Direct‐Patient‐Contact‐Activities.pdf.
- 9. Jawed S, Khaliq S, Abid M, Shaikh JR, Salam O, Abid Z. Knowledge of Chikungunya fever among medical students of Jinnah Sindh Medical University, Karachi. Pak Cureus. 2018;10(8):e3179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Daher AM, Osman MT, Selamat MI, Noor AM. Students' evaluation of health promotion learning outcomes, a case from a Malaysian Institute. Int J Community Med Public Health. 2015;4:472–477. [Google Scholar]
- 11. Jones PR, Brooks JH, Wylie A. Realising the potential for an Olympic legacy; teaching medical students about sport and exercise medicine and exercise prescribing. Br J Sports Med. 2013;47(17):1090–1094. [DOI] [PubMed] [Google Scholar]
- 12. Debra Wood . (2018) How physicians can be healthy role models for patients. [cited 2020 May 12]. Available from: https://www.merritthawkins.com/news‐and‐insights/blog/lifestyle/how‐physicians‐can‐be‐healthy‐role‐models‐for‐patients/.
- 13. Belfrage ASV, Grotmol KS, Tyssen R, et al. Factors influencing doctors' counselling on patients' lifestyle habits: A cohort study. BJGP Open. 2018;2(3):bjgpopen18X101607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lobelo F, Duperly J, Frank E. Physical activity habits of doctors and medical students influence their councelling practices. Br J Sports Med. 2009;43:89–92. [DOI] [PubMed] [Google Scholar]
- 15. Nacar M, Cetinkaya F, Baykan Z, Yilmazei G, Elmali F. Hazrdous health behaviour among medical students: A study from Turkey. Asian Pac J Cancer Prev. 2016;16:7675–7681. [DOI] [PubMed] [Google Scholar]
- 16. Karamat A, Arif N, Malik AK, Chaudhry A, Cheema MA, Rauf A. Cigarette smoking and medical students at King Edward Medical University, Lahore (Pakistan). J Pak Med Assoc. 2011;61:509–512. [PubMed] [Google Scholar]
- 17. Barss P, Grivna M, Al‐Maskari F, Kershaw G. Strengthening public health medicine training for medical students: Development and evaluation of a lifestyle curriculum. Med Teach. 2008;30(9–10):e196–e218. [DOI] [PubMed] [Google Scholar]
- 18. Duperly J, Lobelo F, Segura C, et al. The association between Colombian medical students' healthy personal habits and a positive attitude toward preventive counseling: Cross‐sectional analyses. BMC Public Health. 2009;9:218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shacklady J, Holmes E, Mason G, Davies I, Dornan T. Maturity and medical students' ease of transition into the clinical environment. Med Teach. 2009;31(7):621–626. [DOI] [PubMed] [Google Scholar]
- 20. McDougall R. The junior doctor as ethically unique. J Med Ethics. 2008;34(4):268–270. [DOI] [PubMed] [Google Scholar]
- 21. World Health Statistics (2019) Monitoring health for the SDGs, sustainable development goals. [cited 2020 Apr 06]. Available from: https://apps.who.int/iris/bitstream/handle/10665/324835/9789241565707‐eng.pdf?ua=1.
- 22. National Strategic Framework for Containment of Antimicrobial Resistance . (2018). [cited 2020 Apr 06]. Available from: https://www.nih.org.pk/wp-content/uploads/2018/08/national-strategic-framework-AMR.pdf.
- 23. Margolis R. Educational differences in healthy behaviour changes and adherence among middle‐aged Americans. J Health Soc Behavior. 2013;54:353–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hahn RA, Truman BI. Education improves health and promotes health equity. Int J Health Serv. 2015;45:657–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Turner BJ, Laine C. Differences between generalists and specialists: Knowledge, realism, or primum non nocere? J Gen Intern Med. 2001;16:422–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nilson MS, Pilhammar E. Professional approaches in clinical judgements among senior and junior doctors: Implications for medical education. BMC Med Educ. 2009;21:9–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bahl A, Hixson CC. July phenomenon impacts efficiency of emergency care. West J Emerg Med. 2019;20:157–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Alves AC, Fabbro AL, Passos AD, Carneiro AF, Jorge TM, Martinez EZ. Knowledge and practices related to dengue and its vector: A community‐based study from Southeast Brazil. Rev Soc Bras Med Trop. 2016;49:222–226. [DOI] [PubMed] [Google Scholar]
- 29. Wiskar K. Physician health: A review of lifestyle behaviors and preventive health care among physicians. BCMJ. 2012;54(8):419–423. [Google Scholar]
- 30. Belkowitz J, Sanders LM, Zhang C, et al. Teaching health advocacy to medical students: A comparison study. J Public Health Manag Pract. 2014;20:10–19. [DOI] [PubMed] [Google Scholar]
- 31. McIntosh S, Block RC, Kapsak G, Pearson TA. Training medical students in community health: A novel required fourth‐year clerkship at the University of Rochester. Acad Med. 2008;83:357–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Paterniti DA, Pan RJ, Smith LF, Horan NM, West DL. From physician‐centered to community‐oriented perspectives on health care: Assessing the efficacy of community‐based training. Acad Med. 2006;81:347–353. [DOI] [PubMed] [Google Scholar]
- 33. Carney JK, Hackett R. Community‐academic partnerships: A “community‐first” model to teach public health. Educ Health (Abingdon). 2008;21(1):166. [PubMed] [Google Scholar]
- 34. Douglas A, Mak D, Bulsara C, Macey D, Samarawickrema I. The teaching and learning of health advocacy in an Australian medical school. Int J Med Educ. 2018;9:26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Latif ZM, Wajid G. Reforming medical education in Pakistan through strengthening departments of medical education. Pak J Med Sci. 2018;34:1439–1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ashleigh Peoples . (2020) Medical students can give vital help in the COVID‐19. [cited 2020 May 12]. Available from: https://blogs.scientificamerican.com/observations/medical‐students‐can‐give‐vital‐help‐in‐the‐covid‐19‐crisis/.
- 37. Agha Khan University . (2020) AKU introduces COVID‐19 course for its medical students. [cited 2020 Apr 08]. Available from: https://www.aku.edu/news/Pages/News_Details.aspx?nid=NEWS-002142.
- 38. Aslam R, Jaffery T, Zaidi Z. Service learning: Increasing civic responsibility in Pakistani students. Med Educ. 2011;45(5):524. [DOI] [PubMed] [Google Scholar]
- 39. Kershaw G, Grivna M, Elbarazi I, AliHassan S, Aziz F, Al Dhaheri A. Integrating public health and health promotion practice in the medical curriculum: A self‐directed team‐based project approach. Front Public Health. 2017;21:00193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Deeks A, Lombard C, Michelmore J, Teede H. The effects of gender and age on health related behaviors. BMC Public Health. 2009;9:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wahl H‐W, Kruse A. Historical perspectives of middle age within the life span. In: Willis SL, Martin M, editors. Middle adulthood: A lifespan perspective. Thousand Oaks, CA: Sage, 2005; p. 3–34. [Google Scholar]
- 42. Willis SL, Martin M, Rocke C. Longitudinal perspectives on midlife development: Stability and change. Eur J Ageing. 2010;7:131–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lachman ME, Teshale S, Agrigoroaei S. Midlife as a pivotal period in life course: Balancing growth and decline at the crossroads of youth and old age. Int J Behav Dev. 2015;39:20–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gerstorf D, Rocke C, Lachman ME. Antecedent‐consequent relations of perceived control to health and social support: Longitudinal evidence for between‐domain associations across adulthood. J Gerontol B Psychol Sci Soc Sci. 2011;66:61–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Powis D, Hamilton J, Gordon J. Are graduate entry programmes the answer to recruiting and selecting tomorrow's doctors? Med Educ. 2004;38:1147–1153. [DOI] [PubMed] [Google Scholar]
- 46. Peile E. Should all medical students be graduates first? Yes. BMJ. 2007;24:1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Wilkinson TJ, Wells JE, Bushnell JA. Are differences between graduates and undergraduates in a medical course due to age or prior degree? Med Educ. 2004;38:1141–1146. [DOI] [PubMed] [Google Scholar]
- 48. McCrorie P. Graduate students are more challenging, demanding, and questioning. BMJ. 2002;28:676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kolb DA. Experiential learning: Experience as the source of learning and development. Englewood Cliffs NJ: Prentice‐Hall Inc., 1984. [Google Scholar]
- 50. Kirkpatrick DL, Kirkpatrick JD. Evaluating training programs: The four levels. 3rd ed. San Francisco, CA: Berrett‐Koechler Publication, 2006. [Google Scholar]
- 51. Doctors for Health . A WHO global strategy for changing medical education and medical practice for health for all. Geneva, Switzerland: Division of Organization and Management of Health Systems, 1996; [cited 2020 Apr 04]. Available from: https://apps.who.int/iris/handle/10665/62997. [Google Scholar]


